Abstract
Background
Ultrasound (US) is a good first-line alternative for the diagnosis of bone fractures in adults as well as children. Our study shows that, compared to X-ray, in a resource-constrained environment, on-site US has a high sensitivity (98%) and specificity (96%) in the diagnosis of bone fractures.
Purpose
To compare the accuracy of on-the-spot US with conventional radiography in the screening for bone fractures during the Paris–Dakar rally raid.
Material and Methods
Eighty-three patients (81 men, 2 women) with clinically suspected bone fractures were included in 2013 and 2014. They underwent X-ray and US on the spot, blindly interpreted by two musculoskeletal radiologists. Using X-ray as gold standard, we calculated sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for US, for each anatomic location. The accuracy of US and radiography were also assessed, as were the number of fragments and their degree of displacement (Student’s t-test).
Results
Compared with X-ray, sensitivity, specificity, PPV, and NPV of on-site US were, respectively, for the presence (or absence) of fractures: 98%, 98%, 100%, and 95%. The accuracy of US was 99%. Only one radial styloid process fracture was misdiagnosed with US. There was no significant difference between US and X-ray (P > 0.93) concerning the number of fragments and their degree of displacement.
Conclusion
Bedside musculoskeletal ultrasound performed by trained musculoskeletal radiologists is a useful method in determining and assessing bone fractures in a resource constrained environment.
Keywords: Ultrasound, bone, fracture, X-ray, accuracy
Introduction
The Dakar rally (or “The Dakar”, formerly Paris–Dakar rally) is a professional rally, launched for the first time in December 1978 and held every year since then between late December and mid-January. While initially set partly in Europe and mainly in Africa, the competition has been organized in South America since 2009. The main categories are motorcycles, cars, trucks, and quads (since 2009). Life and navigation conditions can be difficult and the rally raid is subject to a number of mild, serious, or fatal accidents. Various injuries marred the course of the caravan, for competitors and non-competitors like organizers, journalists, or others.
Since 1987, a complete and organized medical team comprising a control center, emergency physicians, surgeons, nurses, and radiologists provides on-site support or evacuates patients to hospitals close to the rally site to permit optimal management, particularly in case of trauma. Every year, several dozen participants or accompanying people have medical or surgical problems but, to our knowledge, no previous medical study has focused on the epidemiological criteria of those, or more particularly on the interest of an on-site radiology ward with X-ray and ultrasonography (US) equipment for bone trauma screening.
Indeed, fractures are very common injuries regardless of age or sex, and particularly in professional racers. X-ray is the reference method for diagnosing and assessing bone fractures. However, this technique exposes the patient to potentially harmful radiation, e.g. to the thyroid in case of fractured clavicle or lung in case of fractured rib, which is frequently found in motorcycle drivers.
US may represent a good first-line alternative for the diagnosis of fractures. It is currently already being used in adults as well as children for suspected skeletal fractures and injuries to the scaphoid, ankle, hand or long bones, with excellent sensitivity and specificity (1–4).
Therefore, the purpose of this study was to compare the accuracy of on-the-spot US with X-ray in the screening for bone fractures among competitors (car drivers, motorcyclists, truck, and quad drivers) and non-competitors during the Paris–Dakar rally in South America.
Material and Methods
Patients
During the Dakar Rally raid in 2013 and 2014 (a period of 21 days in 2013 and 2014), we conducted a single-center observational cohort study. All patients with clinical suspicion of a bone fracture were referred to our on-site imaging department by clinicians (emergency physicians and surgeons) for radiographs and a sonographic evaluation.
Exclusion criteria were: patients under the age of 18 years; patients with suspicion of a vertebral fracture; patients who had to be immediately evacuated because of unstable vital signs; and patients with non-traumatic problems or a clinical diagnosis that did not warrant imaging. All patients were informed of the study procedure and gave their informed consent.
X-ray, US, and data analysis
All patients underwent radiographic and sonographic evaluation by two musculoskeletal (MSK) radiologists (BD and DJ) with 5 and 25 years of experience, respectively.
The X-ray exams were performed and interpreted using the following equipment: X-ray tube – Poskom®, PXP-40HF (100KV); cassette reader – FCR CAPSULA X (CR-IR 357); console – NetPix (CR-IR 348). US exams were performed with the following equipment: Ultrasound Scan Logic E (GE Healthcare, Milwaukee, WI, USA), using a 17 MHz linear golf club-shaped probe.
The radiographs and ultrasound studies were interpreted separately either by BD or DJ, who were blinded to the results of the other modality.
Demographic data, clinical, and first-line imaging observations indicating injuries were collected. The US and X-ray results were recorded in separate forms. For both modalities, the presence or absence of fracture was noted. In case of a positive exam, the fracture was classified as being displaced or not. The greatest gap between the fragments and the number of fragments were also noted.
Then, the results of both diagnostic tests were compared.
Statistical analysis
Statistical analysis was performed using the SAS® software. The accuracy of US was compared to radiography. To compare US and X-ray data, we calculated sensitivity, specificity, and positive and negative predictive values (PPV, NPV).
We used Student's t-test to compare the assessment of the number of fragments and their degree of displacement with X-ray and US.
P < 0.05 was considered as statistically significant.
Results
Patients and clinical data
During Paris–Dakar 2013 and 2014, 127 patients (125 men, 2 women) were referred to our on-site Radiology department. Forty-four were excluded because of polytrauma (n = 9), abdominal surgical indications (n = 3; 2 appendicitis and 1 low speed abdominal pain), renal colic type pain (n = 4), pulmonary infection (n = 16), spine fractures (n = 6), lower extremity phlebitis (n = 4), orchitis (n = 1), and cervical painful mass (n = 1).
Of the 83 included patients (81 men, 2 women), 14 were part of the rally organization and 69 were competitors (n = 48 motorcyclists, n = 5 truck drivers, n = 4 race car pilots, n = 5 quad drivers, n = 7 assistant drivers). Mean age was 40.6 years (SD, 9.9 years), mean pain duration before the X-ray and US exams was 0.8 days (±0.5 days).
Of all clinically suspected upper extremity fractures (n = 47), seven concerned the clavicle, 21 concerned the forearm, wrist, or hand, 15 concerned the shoulder, and four concerned the elbow. Of all clinically suspected lower extremity fractures (n = 20), 13 concerned the leg, ankle, or foot, and seven concerned the femur or knee. As for clinically suspected chest fractures (n = 12), 10 concerned the ribs and two concerned the scapula. Two clinically suspected nasal bone fractures were also included.
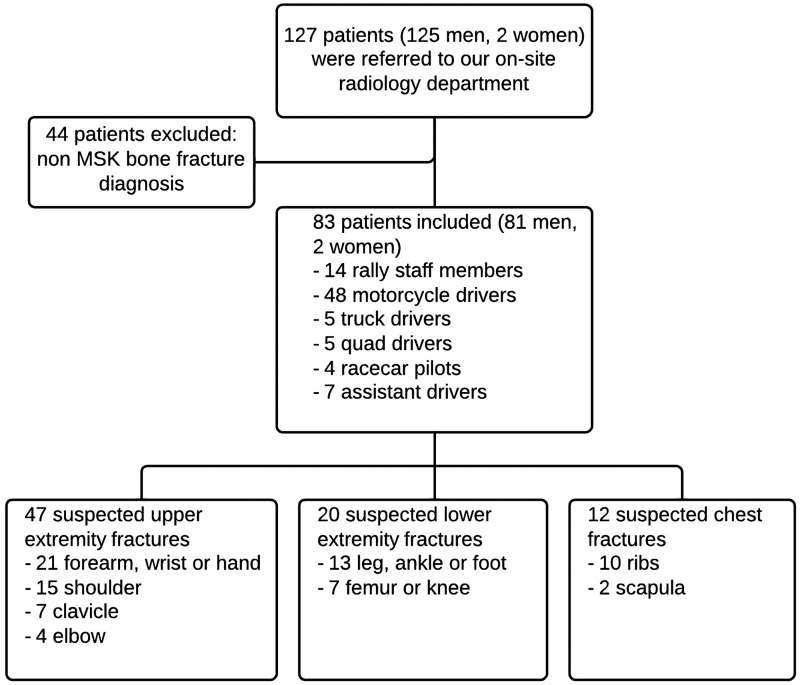
The study design is summarized in Fig. 1.
Fig. 1.
Flowchart showing clinical information and study design.
X-ray and US were performed selectively on the clinically suspected fracture sites.
Imaging data
X-ray examinations showed 33 upper extremity fractures, 15 lower extremity fractures, and 10 chest and nasal bone fractures whereas US demonstrated only 32 upper extremity fractures, 15 lower extremity fractures, and 10 chest and nasal bone fractures. Not strictly limited to assessing the cortical bone, US permitted in the upper extremities the diagnosis of six acromio-clavicular joint dislocations, one rotator cuff tear, one subacromial bursitis, three sterno-clavicular dislocations, two cases of wrist common extensor tendinitis, and one ulnar collateral ligament tear in the first metatarso-phalangeal joint without Stener effect.
In the lower extremity and chest, it also revealed three lateral ankle ligament tears (2 in the anterior talo-fibular part and 1 in the calcaneo-fibular part), one medial ligament and one lateral retinaculum lesion in the knee, and two rib cartilage fractures. US also made the diagnosis of one flexor retinaculum osseous avulsion initially missed on radiography in a case of medial ankle joint pain.
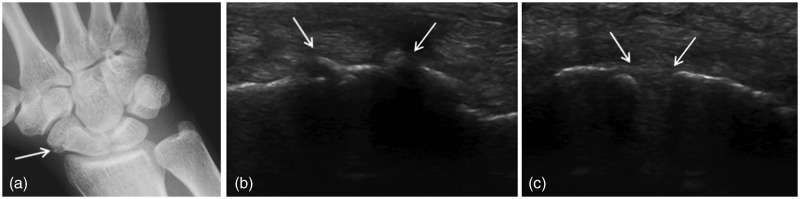
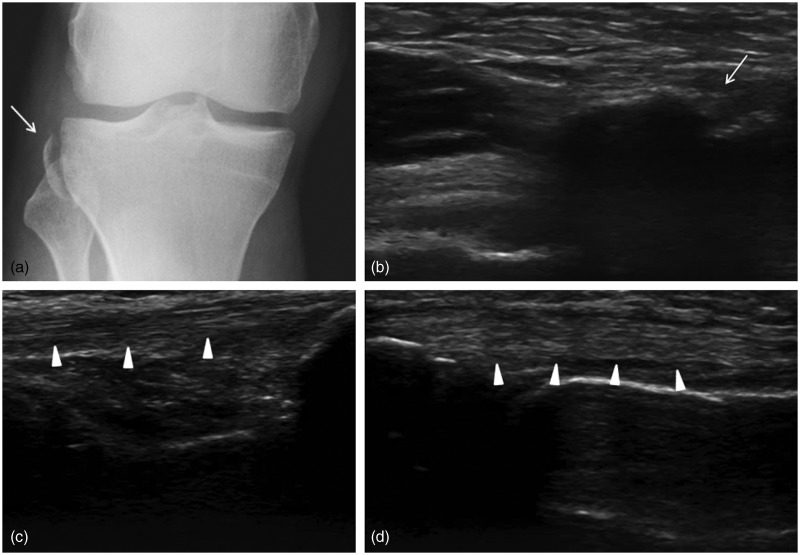
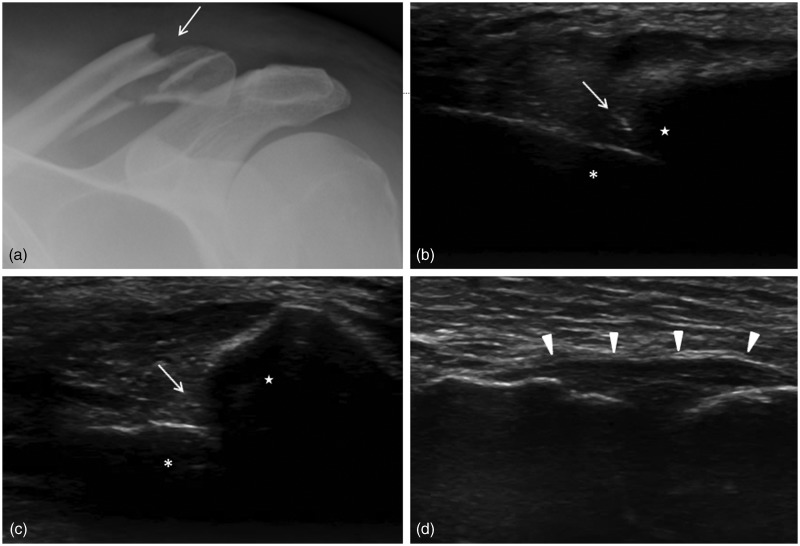
All imaging data are summarized in Table 1. Figs. 2–4 show, respectively, a scaphoid fracture, a Segond fracture of the knee, and a clavicle fracture, both on US and radiographs.
Table 1.
Number of fractures detected by X-Ray and US.
| X-Ray | US | |
|---|---|---|
| Upper extremity fractures | 33 | 32 |
| Lower extremity fractures | 15 | 15 |
| Chest/nasal bone fractures | 10 | 10 |
Fig. 2.
Scaphoid fracture (white arrows) of the right wrist on X-ray (a) and on US (b: palmar view). Normal dorsal part of the scapho-lunar ligament (white arrows) on US (c: dorsal view).
Fig. 3.
Segond fracture (white arrows) of the right knee on X-ray (a) and on US (b: sagittal fragment on lateral view). Normal collateral lateral ligament (white arrowheads) on US (c) and lateral patellar retinaculum (white arrowheads) on US (d).
Fig. 4.
Clavicle fracture (white arrows) of the left shoulder on X-ray (a) and on US (b: coronal view, c: sagittal view) with superior-proximal fragment (white star) and distal- inferior fragment (white asterisk). Normal dorsal part of the acromio-clavicular ligament (white arrowheads) on US (d: dorsal view).
X-ray and US assessment
Overall, compared with X-ray, sensitivity, specificity, PPV, and NPV of on-site US were, respectively, for the presence (or absence) of fractures: 98%, 98%, 100%, and 95%. US accuracy was 99%. No false positive US examinations were found.
For the upper extremities, the sensitivity, specificity, PPV and NPV of on-site US were 97%, 100%, 100%, and 93%, respectively. US accuracy was 99%. For the lower extremity, the sensitivity, specificity, PPV, and NPV, of on-site US were 100%, 100%, 100%, and 100%, respectively. US accuracy was 100%. Finally, for axial skeleton and nasal bones, the sensitivity, specificity, PPV, and NPV, of on-site US were 100%, 100%, 100%, and 100%, respectively. US accuracy was 100%.
Concerning the kind of the fracture (displaced or not), accuracy was 100%, both globally and for the different anatomical locations.
The mean gap between the bone fragments was 5.47 mm (SD, 3.84) on X-ray and 5.47 mm (SD, 3.56) in US, with no statistically significant difference. The minimum and maximum diastasis were the same on X-ray and US: 2 mm and 15 mm, respectively.
The mean number of fragments was 3.28 on radiography (SD, 1.49) and 3.31 on US (SD, 1.49) with no significant difference (P = 0.93). The minimum and maximum numbers of fragments were the same on X-ray and US: 2 and 8, respectively.
The comparison between X-ray and US is summarized in Table 2.
Table 2.
Performance of US in the detection of fractures (globally and for each anatomical region) compared with X-ray as gold standard.
| Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Accuracy (%) | |
|---|---|---|---|---|---|
| Presence of fractures | 98,3 | 96 | 98,3 | 96 | 99,2 |
| Upper extremity | 96,9 | 100 | 100 | 93,3 | 99,2 |
| Lower extremity | 100 | 80 | 93,8 | 100 | 100 |
| Axial skeleton/nasal bone | 100 | 100 | 100 | 100 | 100 |
NPV, negative predictive value; PPV, positive predictive value.
Discussion
This study shows that, compared to X-ray, on-site US has a high sensitivity (98%) and specificity (96%) in the diagnosis of bone fractures. Only one upper extremity fracture was misdiagnosed with US. It was a radial styloid process fracture in a patient who was sent for scaphoid fracture. US was negative and X-ray showed the fractured radius.
Our results are in concordance with the recent literature. Recent studies have focused on the reliability and interest of US for the diagnosis of bone fractures in adults and children. They show that US could also be recommended in routine use in the emergency department in selected cases. According to Patel et al., bedside US of long bones is a rapid, efficient, and non-invasive method of evaluating patients with suspected orthopedic trauma, with an agreement of 96% with radiography (5). Moreover, as shown by Atighechi et al., US can replace radiography in the early diagnosis of nasal bone fractures, because of significantly better results of US compared with radiography (P = 0.004) (6). Warkentine et al. demonstrated the use of US for early identification and assessment of occult or unsuspected fractures in case of child abuse (7). Hubner et al. have focused on the fact that in expert hands, an accurate diagnosis of long bone fractures could be made in 86% of cases. However, these authors were less enthusiastic in case of comminuted fractures because of a lack of sensitivity (8).
Despite these series in which US was a reliable tool for diagnosis of fractures, there is a discordance concerning the need for a MSK US education. Indeed, according to Hedelin et al., Ekinci et al., and Rabiner et al, limited and standardized training in adults and children is enough to permit US-guided triage for bone fractures with a highly sensitive technique (100%) with a 99% specificity in adults (9–11). On the contrary, Bolandparvaz et al. concluded that bedside US (with 1 month of training) is not a reliable method for diagnosing upped and lower limb fractures, compared with radiography (12). Since the two radiologists participating in our study were specialized in MSK pathology for 5 and 25 years, respectively, a US course was deemed unnecessary and its utility was not evaluated.
In the absence of bone fractures, US permitted, on site, the analysis of tendons, ligaments, muscles, and hypodermal tissue. More particularly, it enabled the evaluation of the rotator cuff, wrist tendons, acromioclavicular and sterno-clavicular joints, and ankle ligaments – structures that are frequently injured structures during a rally. Indeed, according to the literature, in case of normal X-ray with suspected occult fracture in children and in adults, US had a specificity to detect radiographically undiagnosed fractures, notably in adults, with 30% more diagnostic information in patients for bone and soft tissue (13,14).
By assessing US in a quite large population (n = 83) that systematically underwent US and X-ray, our study provides strong evidence that on-site US by trained MSK practitioners is a useful method in determining and assessing bone fractures. We strictly used X-ray as gold standard and not medical history or clinical examination. In our study, all processing steps have been completely standardized and documented from the X-ray up to the follow-up US. Therefore, in addition to our results, this controlled methodology may also serve as a template to design future prospective studies assessing the efficacy of US in monitoring fracture healing.
We acknowledge that our study has several limitations. First, our protocol was based on conventional radiography and not CT or MRI as the gold standard. In case of false positive results with US, these modalities might have shown a cortical fracture (CT) or bone marrow edema (MRI). However, we chose on-site CR because of the impossibility to perform CT or MRI in all included patients. Second, no long-term follow-up was performed, not even by means of a telephone survey. This means that we do not have any information about the clinical and radiological evolution beyond the acute stage. Third, all exams were blindly interpreted by trained musculoskeletal radiologists and as such, no dedicated US course was needed. It could be interesting to evaluate the usefulness of such a dedicated course, and to evaluate the learning curve of junior radiologists. Lastly, 44 of the initial 127 patients were excluded from this study. A larger patient population would probably have increased the statistical power of our results. This study is, however, to our knowledge, the most important prospective on-site pilot study in an international Rally performed by two MSK radiologists to assess the efficacy of US in the diagnosis of bone fractures.
In conclusion, bedside musculoskeletal sonography, when performed by trained radiologists, is a useful technique to assess bone fractures when compared to radiography. It is especially of value in a resource-constrained environment such as the Paris–Dakar rally where CT and MRI are unavailable. However, it could also be recommended for routine use in the emergency department in selected cases. Additional randomized clinical studies comparing US to other more contemporary imaging modalities such as CT scan or MRI will be of great interest to consolidate clinical practice.
Conflict of interest
None declared.
References
- 1.Herneth AM, Siegmeth A, Bader TR, et al. Scaphoid fractures: evaluation with high-spatial-resolution US initial results. Radiology 2001; 220: 231–235. [DOI] [PubMed] [Google Scholar]
- 2.Simanovsky N, Lamdan R, Hiller N, et al. Sonographic detection of radiographically occult fractures in pediatric ankle and wrist injuries. J Pediatr Orthop 2009; 29: 142–145. [DOI] [PubMed] [Google Scholar]
- 3.Yesilaras M, Aksay E, Atilla OD, Sever M, et al. The accuracy of bedside ultrasonography as a diagnostic tool for the fifth metatarsal fractures. Am J Emerg Med 2014; 32: 171–174. [DOI] [PubMed] [Google Scholar]
- 4.Bischoff A. Distal forearm fractures – ultrasonography for diagnosis in children is very helpful. Rofo 2013; 184: 920–920. [DOI] [PubMed] [Google Scholar]
- 5.Patel RM, Tollefson BJ. Bedside ultrasound detection of long bone fractures. J Miss State Med Assoc 2013; 54: 159–162. [PubMed] [Google Scholar]
- 6.Atighechi S, Baradaranfar MH, Karimi G, et al. Diagnostic value of ultrasonography in the diagnosis of nasal fractures. J Craniofac Surg 2014; 25: 51–53. [DOI] [PubMed] [Google Scholar]
- 7.Warkentine FH, Horowitz R, Pierce MC. The use of ultrasound to detect occult or unsuspected fractures in child abuse. Pediatr Emerg Care 2014; 30: 43–46. [DOI] [PubMed] [Google Scholar]
- 8.Hubner U, Schlicht W, Outzen S, et al. Ultrasound in the diagnosis of fractures in children. J Bone Joint Surg Br 2000; 82: 1170–1173. [DOI] [PubMed] [Google Scholar]
- 9.Hedelin H, Goksor LA, Karlsson J, et al. Ultrasound-assisted triage of ankle trauma can decrease the need for radiographic imaging. Am J Emerg Med 2013; 31: 1686–1689. [DOI] [PubMed] [Google Scholar]
- 10.Ekinci S, Polat O, Gunalp M, et al. The accuracy of ultrasound evaluation in foot and ankle trauma. Am J Emerg Med 2013; 31: 1551–1555. [DOI] [PubMed] [Google Scholar]
- 11.Rabiner JE, Friedman KM, Khine H, et al. Accuracy of point-of-care ultrasound for diagnosis of skull fractures in children. Pediatrics 2013; 131: 1757–1764. [DOI] [PubMed] [Google Scholar]
- 12.Bolandparvaz S, Moharamzadeh P, Jamali K, et al. Comparing diagnostic accuracy of bedside ultrasound and radiography for bone fracture screening in multiple trauma patients at the ED. Am J Emerg Med 2013; 31: 1583–1585. [DOI] [PubMed] [Google Scholar]
- 13.Marshburn T, Legome E, Sargsyan A, et al. Goal-directed ultrasound in the detection of long-bone fractures. J Trauma 2004; 57: 329–332. [DOI] [PubMed] [Google Scholar]
- 14.Abi KS, Haddad-Zebouni S, Roukoz S, et al. Ultrasound as an adjunct to radiography in minor musculoskeletal pediatric trauma. J Med Liban 2011; 59: 70–74. [PubMed] [Google Scholar]