Abstract
We describe an unusual case of trans-scaphoid perilunate injury where the proximal half of the scaphoid avulsed from all attaching ligaments and extruded into the forearm. Treatment involved anatomic reduction and internal fixation of the fracture, scapholunate (SL) ligament repair, temporary K-wire fixation, and prolonged immobilization. At 19-month follow-up, the fracture healed, SL ligament remained intact, and the patient recovered much of his hand function.
Keywords: Perilunate fracture dislocation, Perilunate injury, Trans-scaphoid perilunate avulsion fracture, Treatment of trans-scaphoid perilunate avulsion fracture
Introduction
Perilunate dislocations and perilunate fracture dislocations are a spectrum of injuries that result from high-energy trauma leading to disruption of the integrity of the ligamentous support of the wrist [1]. Untreated perilunate fracture dislocations can have devastating effects on the function of the wrist including posttraumatic arthritis, decreased range of motion (ROM), chronic carpal tunnel syndrome, and attritional rupture of flexor tendons [2]. Mayfield and colleagues [3] described four stages of progressive carpal destabilization. As the wrist extends by the high-energy external force, the scaphoid goes into extension. The lunate is held by the short and long radial lunate ligaments and resists extension. The scapholunate (SL) ligament becomes strained and may tear. As more energy is applied, the lunocapitate dislocation occurs next, followed by lunotriquetral (LT) disruption, and finally lunate dislocation (Fig. 1). If during the first stage, the wrist is radially deviated, the force transmits through the scaphoid waist instead, and a trans-scaphoid perilunate fracture dislocation occurs. This is also the most common type of perilunate fracture dislocation. Our case, however, did not follow the pattern described. Instead of one or the other, the force was transmitted between both the SL ligament and scaphoid waist, resulting in a complete disruption of SL ligament and a fracture of the scaphoid, with the proximal half of the scaphoid extruding through the volar wrist capsule. We present our surgical treatment and outcome of this unusual and complex injury.
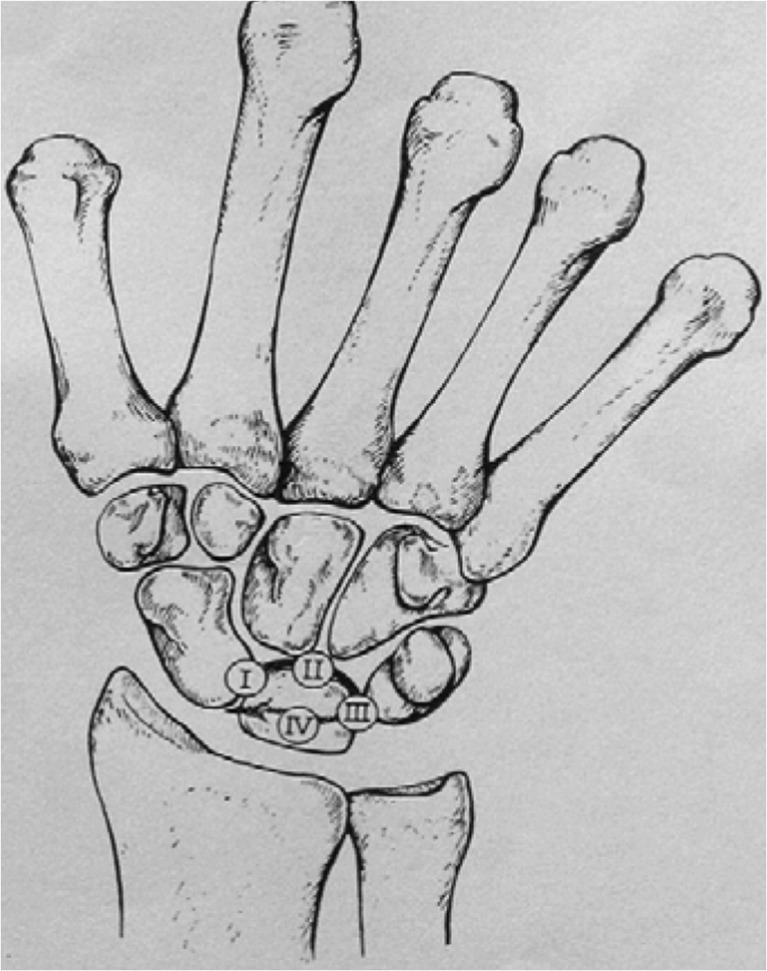
Fig. 1.
Mayfield described four stages of perilunate instability. The first stage (I) is disruption of the scapholunate articulation. The second (II) and third (III) stages are separation of the capitolunate and lunotriquetral joints. The fourth (IV) stage is a volar lunate dislocation (with permission from Mayfield JK. Wrist ligamentous anatomy and pathogenesis of carpal instability. Ortho Clin North Am 1984;15(2):209–216)
Case report
A 26-year-old, right-hand-dominant male presented to our emergency department after falling 12 ft onto his left outstretched hand. He was initially evaluated at an outside hospital, splinted, and transferred to our institution. The patient complained of left-hand swelling, pain, and paresthesias. On physical exam, the left wrist demonstrated marked edema and a palpable bony fragment in the volar forearm, just proximal to the distal wrist crease. Left wrist ROM was diminished.
Initial radiographs (Fig. 2a, b) demonstrated a trans-scaphoid perilunate fracture dislocation with extrusion of the proximal scaphoid fragment into the forearm and dorsal subluxation of the carpus.
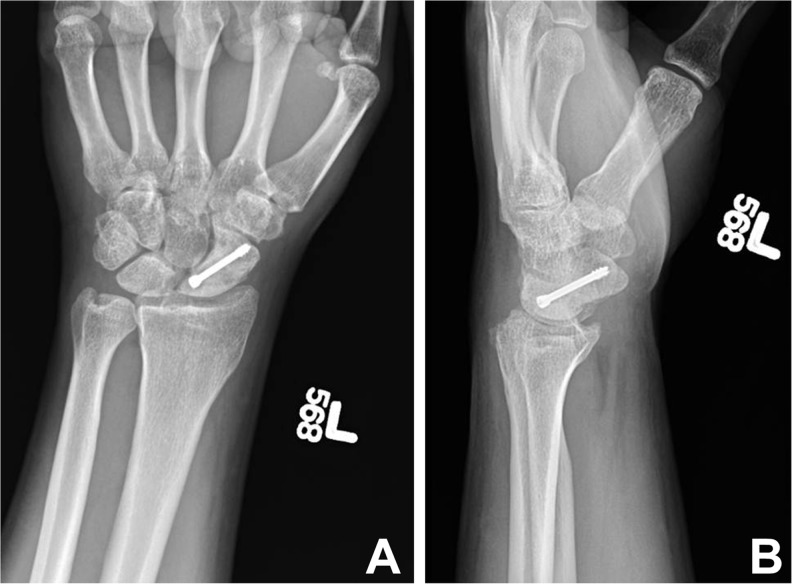
Fig. 2.
a Trans-scaphoid avulsion fracture dislocation with migration of proximal scaphoid fragment, AP view. b Trans-scaphoid perilunate avulsion fracture dislocation with migration of proximal scaphoid fragment, lateral view
The patient was taken back to the operating room urgently for open carpal tunnel release, open reduction internal fixation of the scaphoid fracture using a cannulated compression screw, repair of the dorsal SL ligament, and pinning of the radiocarpal joint. An extended open carpal tunnel release was performed. The incision was extended proximally to retrieve the proximal fracture fragment. The proximal half of the scaphoid was lying freely within the volar forearm (Fig. 3). A large perforation was noted in the volar wrist capsule near the anatomic position of the proximal half of the scaphoid. There were no injuries to the midcarpal or ulnar aspect of the volar wrist capsule. A dorsal approach was then used to access the carpal bones. A large rent was noted in the extensor retinaculum over the fourth dorsal compartment (Fig. 4). The EPL was translocated out of the third compartment, exposing a large rent in the dorsal wrist capsule. A dorsal ligament-sparing incision incorporating the capsular tear was made to expose the underlying carpus. The distal half of the scaphoid remained in situ. The proximal segment was placed in an anatomic position, and fixation of the scaphoid fracture was performed with a 3.0 cannulated screw. A complete midsubstance tear of the SL ligament was identified and repaired with three over-and-over sutures using 2-0 FiberWire® (Fig. 5). The SL ligament repair was reinforced by placing a 0.045 Kirschner wire (K-wire) through the scaphoid into the lunate. Another K-wire was used to stabilize the radiocarpal joint because the wrist was subluxing dorsally. A third K-wire was placed from the triquetrum to lunate and distal radius (Fig. 6). Subsequently, the wrist capsule was repaired with 2-0 FiberWire®. A volar splint was applied at the end of the case.
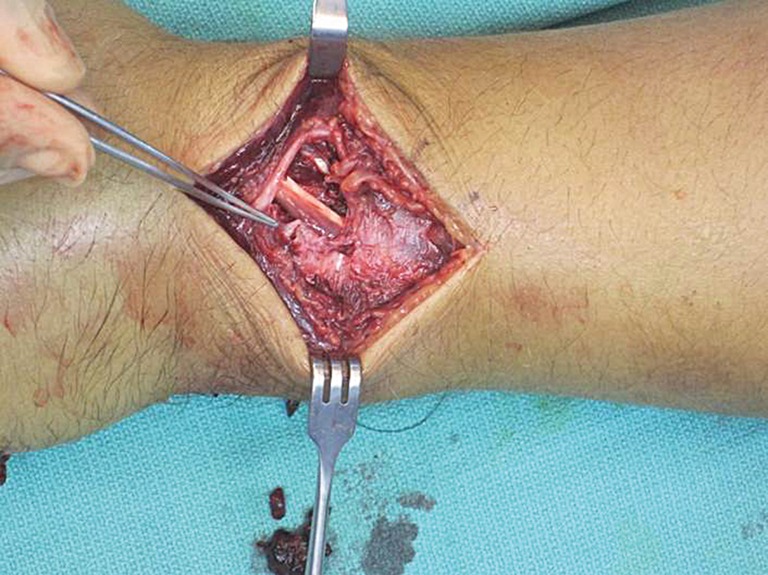
Fig. 3.

Exposure of median nerve after an extended open carpal tunnel release and retrieval of the proximal scaphoid fragment in distal volar forearm
Fig. 4.
Large rent in extensor retinaculum
Fig. 5.
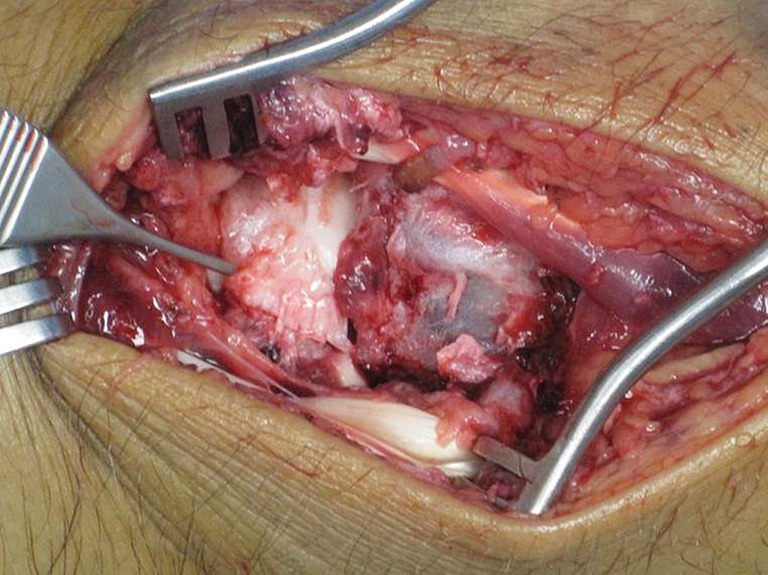
Midsubstance tear of dorsal scapholunate ligament
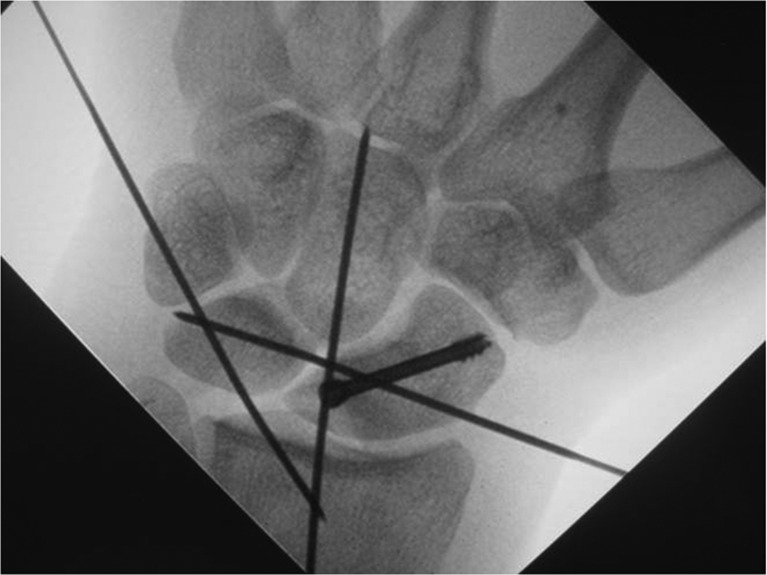
Fig. 6.
Intraoperative imaging of left scaphoid and radiocarpal reduction and fixation
The patient was initially immobilized for 8 weeks postoperatively. After X-rays showed bridging bone formation across the fracture site and lack of clinical tenderness, the K-wires were removed, and ROM was started. Initial ROM measurements showed 27 degrees of flexion, 25 degrees of extension, 10 degrees of ulnar deviation, and 5 degrees of radial deviation. The patient demonstrated full supination and pronation. Grip strength was measured at 15 lbs with the Jamar dynamometer. One month after starting ROM, the patient complained of increasing pain in his left wrist. He was noted to have tenderness in the left snuff box overlying the scaphoid fracture site. The patient was immobilized for another 8 weeks in a short-arm cast. A 3-month follow-up CT scan (Fig. 7) demonstrated new bone formation without suspicion of nonunion. During immobilization, the patient received ultrasound bone stimulation. At 1-year follow-up, the patient returned to work as a manual laborer. The patient reported no pain with rest and ADLs and 1/10 pain with radial and ulnar deviation during power grip and hammering. He was nontender over the fracture site with improved function of his wrist. X-rays at 1 year demonstrated bony union with some sclerosis of the proximal scaphoid. SL interval is intact with stress views (Fig. 8). His left wrist ROMs at 1-year follow-up were as follows: wrist flexion, 40 degrees; wrist extension, 35 degrees; full supination, full pronation, and radial deviation, 11 degrees; and ulnar deviation, 13 degrees. Left grip strength was measured at 60 lbs (75 % of right). The patient had a QuickDASH score of 4.5. At 19-month follow-up, radiographs demonstrated bony union, maintenance of the SL interval, stable screw position, and some expected sclerosis of the proximal half of the scaphoid (Fig. 9a–c). The patient’s clinical exam remained the same.
Fig. 7.
Left-hand CT scan at 3-month follow-up showing bony bridging across the scaphoid fracture site
Fig. 8.
Left-hand radiographs at 1-year follow-up. Left radiograph was a clenched fist view
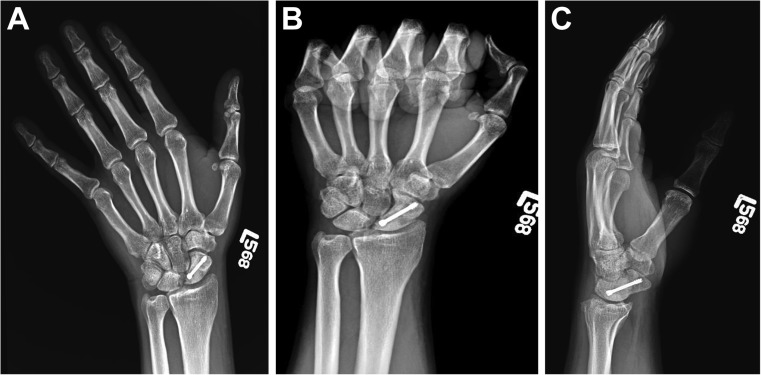
Fig. 9.
a Left-hand AP radiograph with ulnar deviation at 19-month follow-up. b Left-hand clenched fist view at 19-month follow-up. c Left-hand lateral view at 19-month follow-up
Discussion
High-energy traumatic injuries of the wrist can result in complex perilunate ligamentous and osseous disruption. Perilunate ligamentous dislocations result from transmission of force through the lesser arc of the wrist and have been classified by Mayfield [3]. Trans-scaphoid perilunate fracture dislocations are the most commonly described perilunate fracture dislocations [4]. Our case report describes an unusual trans-scaphoid perilunate fracture dislocation with complete disruption of both the SL ligament and scaphoid. In our case, with all its blood supply cutoff, the proximal half of the scaphoid was in fact a large autologous bone graft. In addition to fracture healing, the SL ligament also needed to heal to provide good functional outcome. Several alternative surgical options were considered such as proximal row carpectomy, four-corner fusion, and simple removal of the avulsed fragment. Our thought was that by performing open reduction and internal fixation (ORIF) and ligament repair whereby restoring normal anatomy, we would give the patient the best chance for a good functional outcome and at the same time preserve all these other salvage options if they fail. To our knowledge, these fracture pattern and treatment have not been described previously in the literature. The treatment of perilunate fracture dislocations has evolved over time and includes closed reduction with or without pinning, open reduction and stabilization of fractures or dislocations with or without ligamentous repair, and salvage procedures consisting of proximal row carpectomy [1, 2, 5, 6]. Closed reduction with or without pinning has been associated with unsatisfactory carpal alignment and poor functional outcomes. Therefore, surgical treatment has emerged as the standard of care for definitive treatment of these complex perilunate injuries in order to sustain adequate fracture and dislocation reduction, restoration of ligament integrity, and improvement of functional outcomes. Closed reduction now serves as a temporizing treatment to prevent progression of median nerve neuropathy until the patient can undergo appropriate imaging studies and be taken to the operating room.
Dorsal, volar, and combined approaches have been described for the surgical treatment of perilunate injuries. Although better visualization can be achieved with a combined approach, there is suspicion of increased risk of wound healing complications, swelling, and interruption of blood supply to the carpus [7]. The dorsal approach is known for allowing good exposure of the proximal carpal row, midcarpal joints, and proximal pole of scaphoid. The volar approach is best suited for patients with suspected volar ligament injury and acute carpal tunnel syndrome because this allows access for volar ligament repair and release of the transverse carpal ligament. Kremer et al. [8] reported suboptimal outcomes of patients with perilunate injuries who were treated with a combined approach. However, it is unclear whether the suboptimal outcome is due to the combined approach or the severity of the injury. In this case report, we utilized a combine approach. The volar exposure was performed to allow release of the transverse carpal ligament, retrieval of the proximal segment of the scaphoid, and evaluation of the volar wrist ligaments. Through the dorsal approach, we performed an ORIF of the scaphoid fracture with a compression screw, repaired the SL ligament, and stabilized the radiocarpal joint with K-wires in a triangular pattern. Our patient proceeded on to bony union of the scaphoid fracture with functional outcomes of his left wrist and minimal pain with significant upper extremity weight bearing.
Timing of repair of perilunate dislocations and perilunate fracture dislocations can significantly affect clinical outcomes. Surgical treatment of perilunate dislocations in the acute setting has been associated with improved clinical outcomes including better wrist motion and grip strength and decreased severity of arthrosis on radiographs [1, 9]. However, it is important to mention that radiographic evidence of arthrosis does not necessarily correlate with clinical outcomes or manifested symptoms [1, 2, 10].
Sotereanos et al. [7] reported 11 cases with perilunate injuries, 8 of which were trans-scaphoid perilunate injuries. These trans-scaphoid perilunate injuries were treated with open reduction and fixation of the scaphoid fractures. They reported wrist flexion of 39 degrees, wrist extension of 50 degrees, radial deviation of 12 degrees, ulnar deviation of 25 degrees, and grip strength of 23 kg (77 % of contralateral side). Herzberg and Forissier [2] reported an average wrist flexion of 64 degrees and wrist extension of 49 degrees in 14 patients treated for trans-scaphoid perilunate injuries.
At 1-year follow-up, our patient obtained wrist flexion of 40 degrees, wrist extension of 35 degrees, radial deviation of 11 degrees, ulnar deviation of 13 degrees, and full supination and pronation, and grip strength was measured at 60 lbs (75 % of right). These results are similar to those reported by Sotereanos et al. [7]. However, it is difficult to provide direct comparisons of our results because of differences in injury pattern and fracture fixation techniques.
In conclusion, trans-scaphoid perilunate fracture dislocations can present unique fracture patterns that can be challenging to hand surgeons such as in this case with both SL ligament and scaphoid disrupted. However, adherence to basic principles including adequate exposure, early intervention, stable fracture fixation, obtaining adequate carpal alignment, and restoring the integrity of the ligaments can provide our patient with functional ROM to the wrist, decreased incidence of early arthritis, and improved quality of life.
Acknowledgments
Conflict of Interest
Lisa Moody declares that she has no conflict of interest.
Andrew Y. Zhang declares that he has no conflict of interest.
Statement of Human and Animal Rights
This article does not contain any studies with human or animal subjects.
Statement of Informed Consent
Informed consent was not required from the patient prior to commencing work on this case report.
References
- 1.Herzberg G, Comtet JJ, Linscheid RL, et al. Perilunate dislocations and fracture-dislocations: a multicenter study. J Hand Surg Am. 1993;18:768–79. [DOI] [PubMed]
- 2.Herzberg G, Forissier D. Acute dorsal trans-scaphoid perilunate fracture-dislocations: medium-term results. J Hand Surg Br. 2002;27:498–502. [DOI] [PubMed]
- 3.Mayfield JK. Patterns of injury to carpal ligaments. A spectrum. Clin Orthop Relat Res 1984;36-42 [PubMed]
- 4.Mayfield JK, Johnson RP, Kilcoyne RK. Carpal dislocations: pathomechanics and progressive perilunar instability. J Hand Surg Am. 1980;5:226–41. [DOI] [PubMed]
- 5.DiGiovanni B, Shaffer J. Treatment of perilunate and transscaphoid perilunate dislocations of the wrist. Am J Orthop (Belle Mead NJ). 1995;24:818–26. [PubMed]
- 6.Hee HT, Wong HP, Low YP. Transscaphoid perilunate fracture/dislocations—results of surgical treatment. Ann Acad Med Singapore. 1999;28:791–4. [PubMed]
- 7.Sotereanos DG, Mitsionis GJ, Giannakopoulos PN, et al. Perilunate dislocation and fracture dislocation: a critical analysis of the volar-dorsal approach. J Hand Surg Am. 1997;22:49–56. [DOI] [PubMed]
- 8.Kremer T, Wendt M, Riedel K, et al. Open reduction for perilunate injuries—clinical outcome and patient satisfaction. J Hand Surg Am. 2010;35:1599–606. [DOI] [PubMed]
- 9.Komurcu M, Kurklu M, Ozturan KE, et al. Early and delayed treatment of dorsal transscaphoid perilunate fracture-dislocations. J Orthop Trauma. 2008;22:535–40. [DOI] [PubMed]
- 10.Souer JS, Rutgers M, Andermahr J, et al. Perilunate fracture-dislocations of the wrist: comparison of temporary screw versus K-wire fixation. J Hand Surg Am. 2007;32:318–25. [DOI] [PubMed]