Abstract
Background
Patients who miss scheduled appointments without notifying office staff––“no-shows”––disrupt practice workflow and decrease access for others, resulting in misuse of resources and lost revenue. The primary purpose of this study was to identify factors associated with no-shows in a hospital-based outpatient hand office. Secondarily, we studied factors associated with cancelations.
Methods
Of the 14,793 new adult patient appointments to our outpatient hand surgery office scheduled between January 2011 and December 2013, 880 (5.9 %) were no-shows and 2715 (18 %) were cancelations. Data on patient demographics and timing of the visit were collected to construct a multinomial logistic regression model of determinants of appointment no-shows and cancelations.
Results
Factors independently associated with no-shows included younger age, Hispanic or black race, unmarried status (single or divorced), appointment on a Monday or Tuesday, and residence near the office. Factors associated with cancelations were female sex, unmarried status (widowed or divorced), winter season, and appointment on a weekday other than Friday.
Conclusions
Non-attendees are more likely to be younger, unmarried, non-white, to have their appointments at the start of the week, and to live near the office. Knowledge of these factors might prove useful for implementation of tailored quality improvement initiatives to reduce non-attendance and maximize productivity in the hand surgery office setting.
Type of study/level of evidence: Prognostic IV.
Keywords: Appointments, No-shows, Cancelations, Hand surgery
Introduction
Non-attendance at outpatient clinics is a vexing and common phenomenon in healthcare, with rates ranging between 5 and 39 % [7, 19, 24]. Patients who miss scheduled appointments without notifying office staff––“no-shows”––disrupt practice workflow and decrease access for others, resulting in misuse of resources, suboptimal quality of care, longer waiting lists, and higher patient dissatisfaction [9, 18, 21, 27, 28].
Studies in numerous settings of healthcare delivery suggest that patients who do not keep physician appointments tend to be younger, non-white, and socio-economically disadvantaged [11, 12, 14, 15, 25, 26]. Other factors associated with non-attendance include long waiting times to get an appointment and the timing of the visit within the day and week [1, 9, 13].
In the hand clinic setting, ten Berg and Ring [32] noted that patients with a metacarpal fracture who did not return for a scheduled 1-month follow-up visit were more likely to be unemployed, unmarried, and uninsured. This study, however, was specific to patients with relatively minor skeletal trauma––a diagnosis associated with high absenteeism rates [31]––and may therefore not be representative of patients with elective hand conditions or more severe trauma; furthermore, it lacked data on the timing of the appointment [32]. A more comprehensive understanding of the characteristics of hand surgery patients who fail to keep scheduled appointments might aid in the formulation of interventions to improve attendance rates and maximize clinic efficiency.
The primary purpose of this study was therefore to identify factors associated with no-shows in a busy hospital-based outpatient hand office. Secondarily, we studied factors associated with cancelations.
Materials and Methods
Using an Institutional Review Board approved protocol, we identified all new patient appointments to our outpatient hand surgery office scheduled between January 1, 2011 and December 31, 2013. Our office is located in a large urban academic hospital in the USA and uses the IDX system (General Electric, Connecticut, USA) for appointment scheduling. Appointment status was categorized into three groups: (1) attended, (2) canceled, and (3) no-show. Visits for individuals aged less than 18 years old were excluded from analysis. The final cohort had 14,793 records, with 2715 (18 %) cancelations and 880 (5.9 %) no-shows.
Our institutional database was queried to collect data on patient demographics and timing of the appointment. Demographic and appointment-related characteristics were compared among patients who attended, canceled, and failed to show without notice to their appointments (Table 1). Explanatory variables included age, sex, race/ethnicity (White, Black, Hispanic, Asian, other, and unknown), marital status (single, married, divorced, widowed, and unknown), place of residence according to patient’s zip code (zip codes in the same city as our office were defined as living near the office, while the remaining zip codes were defined as residing far from the office), season of the year, and weekday.
Table 1.
Characteristics of hand surgery appointments; (n = 14,793)
| Parameter | All patients | Appointment status | P | ||
|---|---|---|---|---|---|
| Attended | Canceled | No-show | |||
| Total, n (%) | 14,793 | 11,198 (76) | 2715 (18) | 880 (5.9) | |
| Age in years, mean ± SD | 51 ± 17 | 52 ± 17 | 52 ± 17 | 45 ± 16 | <0.001 |
| Age in years, n (%) | |||||
| 18–35 | 3262 (22) | 2430 (22) | 547 (20) | 285 (32) | <0.001 |
| 36–55 | 5194 (35) | 3852 (34) | 980 (36) | 362 (41) | |
| 56–70 | 4302 (29) | 3326 (30) | 805 (30) | 171 (19) | |
| >70 | 2035 (14) | 1590 (14) | 383 (14) | 62 (7.0) | |
| Sex, n (%) | |||||
| Female | 7892 (53) | 5885 (53) | 1560 (58) | 447 (51) | <0.001 |
| Male | 6901 (47) | 5313 (47) | 1155 (43) | 433 (49) | |
| Race/ethnicity, n (%) | |||||
| White | 11,580 (78) | 8910 (80) | 2131 (79) | 539 (61) | <0.001 |
| Black | 722 (4.9) | 509 (4.5) | 122 (4.5) | 91 (10) | |
| Hispanic | 1229 (8.3) | 863 (7.7) | 206 (7.6) | 160 (18) | |
| Asian | 651 (4.4) | 487 (4.3) | 132 (4.9) | 32 (3.6) | |
| Other | 155 (1.0) | 114 (1.0) | 26 (1.0) | 15 (1.7) | |
| Unknown | 456 (3.1) | 315 (2.8) | 98 (3.6) | 43 (4.9) | |
| Marital status, n (%) | |||||
| Single | 5228 (35) | 3865 (35) | 927 (34) | 436 (50) | <0.001 |
| Married | 7275 (49) | 5661 (51) | 1308 (48) | 306 (35) | |
| Separated or divorced | 1188 (8.0) | 864 (7.7) | 237 (8.7) | 87 (9.9) | |
| Widowed | 635 (4.3) | 478 (4.3) | 137 (5.1) | 20 (2.3) | |
| Unknown | 446 (3.0) | 314 (2.8) | 102 (3.8) | 30 (3.4) | |
| Season of the year, n (%) | |||||
| Summer | 3639 (25) | 2783 (25) | 658 (24) | 198 (23) | 0.15 |
| Fall | 3622 (25) | 2755 (25) | 656 (24) | 211 (24) | |
| Winter | 3492 (24) | 2591 (23) | 688 (25) | 214 (24) | |
| Spring | 4039 (27) | 3069 (27) | 713 (26) | 257 (29) | |
| Weekday, n (%) | |||||
| Monday | 2922 (20) | 2202 (20) | 526 (19) | 194 (22) | <0.001 |
| Tuesday | 4086 (28) | 3011 (27) | 800 (30) | 275 (31) | |
| Wednesday | 3781 (26) | 2874 (26) | 695 (26) | 212 (24) | |
| Thursday | 2940 (20) | 2259 (20) | 539 (20) | 142 (16) | |
| Friday | 1064 (7.2) | 852 (7.6) | 155 (5.7) | 57 (6.5) | |
| Place of residence, n (%) | |||||
| Boston | 6479 (44) | 4904 (44) | 1105 (41) | 470 (53) | <0.001 |
| Outside of Boston | 8314 (56) | 6294 (56) | 1610 (59) | 410 (47) | |
Assuming normal distribution of the data based on the large sample size, Pearson’s chi-square test was employed for analysis of categorical variables, and one-way analysis of variance (ANOVA) for continuous variables. Multinomial logistic regression modeling was used to determine factors independently associated with appointment no-shows and cancelations. Appointment attendance was set as the reference dependent outcome. All explanatory variables were included in the regression model [3]. Results were reported as odds ratios (OR) with 95 % confidence intervals (CI). The statistical threshold for type I error was set at 0.05.
Results
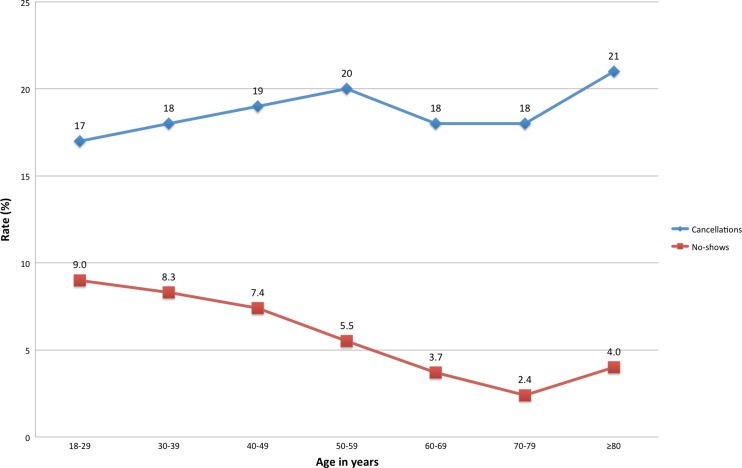
Patients who did not attend and did not call in advance to cancel were more likely (p < 0.001) to be younger (45 ± 16 years) than patients who kept their appointments (52 ± 17 years), and were also more likely (p < 0.001) to be men (49 vs. 47 %), Hispanic (18 vs. 7.7 %) or black (10 vs. 4.5 %), single (50 vs. 35 %) or divorced (9.9 vs. 7.7 %), to have their appointments scheduled at the beginning of the week, and to live relatively close to the hospital (53 vs. 44 %; Table 1). Patients who canceled their appointments were of similar age and race compared to those who attended, but were more likely (p < 0.001) to be women (58 vs. 53 %), widowed (5.1 vs. 4.3 %) or divorced (8.7 vs. 7.7 %), to have their appointment scheduled during winter (25 vs. 23 %), and to reside far from the hospital (59 % vs. 56 %; Table 1). With increasing patient age, there was a downward trend in appointment no-show rates and an upward trend in appointment cancelation rates (Fig. 1).
Fig. 1.
Rates of cancelations and no-shows by patient age
In multinomial regression modeling (Table 2), factors independently associated with appointment no-shows included younger age, Hispanic race (OR 2.4, 95% CI 2.0–3.0, p < 0.001) or black race (OR 2.5, 95% CI 1.9–3.1, p < 0.001), being single (OR 1.6, 95% CI 1.3–1.9, p < 0.001) or divorced (OR 1.8, 95% CI 1.4–2.3, p < 0.001), appointment on a Monday (OR 1.4, 95% CI 1.001–1.9, p = 0.05) or Tuesday (OR 1.5, 95% CI 1.1–2.0, p = 0.008), and residence near the hospital (OR 1.2, 95% CI 1.002–1.3, p = 0.047). Factors associated with appointment cancelations were female sex (OR 1.2, 95% CI 1.1–1.3, p < 0.001), being widowed (OR 1.2, 95% CI 1.01–1.5, p = 0.044) or divorced (OR 1.2, 95% CI 1.01–1.4, p = 0.042), winter season (OR 1.2, 95% CI 1.03–1.3, p = 0.014), and appointment on a weekday other than Friday.
Table 2.
Multinomial logistic regression of predictors of missed appointments in hand surgery
| Predictor | No-shows | Cancelations | ||||||
|---|---|---|---|---|---|---|---|---|
| OR | 95 % CI | P | OR | 95 % CI | P | |||
| Lower | Upper | Lower | Upper | |||||
| Age (reference: >70 year) | ||||||||
| 18–35 | 2.1 | 1.5 | 2.9 | <0.001 | 0.97 | 0.82 | 1.1 | 0.74 |
| 36–55 | 2.0 | 1.5 | 2.6 | <0.001 | 1.1 | 0.95 | 1.3 | 0.23 |
| 56–70 | 1.2 | 0.89 | 1.6 | 0.23 | 1.0 | 0.88 | 1.2 | 0.83 |
| Female sex | 1.0 | 0.84 | 1.1 | 0.97 | 1.2 | 1.1 | 1.3 | <0.001 |
| Race/ethnicity (reference: white) | ||||||||
| Black | 2.5 | 1.9 | 3.1 | <0.001 | 1.0 | 0.83 | 1.3 | 0.87 |
| Hispanic | 2.4 | 2.0 | 3.0 | <0.001 | 1.0 | 0.87 | 1.2 | 0.73 |
| Asian | 1.0 | 0.69 | 1.4 | 0.99 | 1.2 | 0.95 | 1.4 | 0.16 |
| Other | 1.9 | 1.1 | 3.3 | 0.020 | 1.0 | 0.63 | 1.5 | 0.87 |
| Unknown | 2.1 | 1.48 | 3.0 | <0.001 | 1.2 | 0.98 | 1.6 | 0.08 |
| Marital status (reference: married) | ||||||||
| Single | 1.6 | 1.3 | 1.9 | <0.001 | 1.1 | 1.0 | 1.2 | 0.096 |
| Separated or divorced | 1.8 | 1.4 | 2.3 | <0.001 | 1.2 | 1.01 | 1.4 | 0.042 |
| Widowed | 1.1 | 0.66 | 1.8 | 0.76 | 1.2 | 1.01 | 1.5 | 0.044 |
| Unknown | 1.4 | 0.89 | 2.1 | 0.16 | 1.3 | 1.0 | 1.7 | 0.023 |
| Season of the year (reference: Spring) | ||||||||
| Summer | 0.86 | 0.71 | 1.0 | 0.86 | 1.0 | 0.92 | 1.2 | 0.62 |
| Fall | 0.89 | 0.73 | 1.1 | 0.89 | 1.0 | 0.91 | 1.2 | 0.64 |
| Winter | 1.0 | 0.81 | 1.2 | 0.99 | 1.2 | 1.03 | 1.3 | 0.014 |
| Weekday (reference: Friday) | ||||||||
| Monday | 1.4 | 1.001 | 1.9 | 0.050 | 1.3 | 1.1 | 1.6 | 0.0080 |
| Tuesday | 1.5 | 1.1 | 2.0 | 0.0080 | 1.5 | 1.2 | 1.8 | <0.001 |
| Wednesday | 1.1 | 0.8 | 1.5 | 0.44 | 1.3 | 1.10 | 1.6 | 0.0040 |
| Thursday | 1.0 | 0.7 | 1.4 | 0.99 | 1.3 | 1.06 | 1.6 | 0.010 |
| Residence near the office | 1.2 | 1.002 | 1.3 | 0.047 | 0.87 | 0.79 | 0.95 | 0.0020 |
Reference dependent outcome: appointment attendance
P-values in italic denote statical significance
Discussion
Missed outpatient appointments contribute to inefficient resource allocation and lost revenue [27, 28]. Although rates and risk factors for non-attendance have been documented in various clinical settings, there is little published regarding hand surgery patients [32]. In an era of increasing cost containment, knowledge of predictors of missed appointments might help reduce healthcare expenditure while improving the quality and efficiency of care. We therefore set out to determine if variables from our scheduling and institutional database could be used to predict patients likely to miss hand surgery office appointments. In this study, non-attendees were more likely to be younger, unmarried and non-white, to have their appointments at the start of the week and to live near the hospital.
Although our analysis benefits from access to large numbers and associated power, we acknowledge several important shortcomings. First, the retrospective nature of the study does not allow ascertainment of the exact reasons for which patients missed their appointments. Second, in line with other studies [4, 11, 20, 34], we limited our analysis to new patient appointments. Third, although we included important data on the timing of the appointment including weekday and season of the year, we were unable to adjust for the waiting time for an appointment and the specific time of the appointment within the day, both factors known to contribute to absenteeism in other settings [5, 6, 9, 13]. Fourth, another drawback was our inability to control for the diagnosis or presenting problem and its severity; however, illness severity has been shown to be unrelated to non-attendance [23, 30]. Fifth, proximity to care was assessed as a dichotomous variable relying on zip code analysis; although this is a valid approach, it would have been perhaps better to evaluate the distance from home to the office as a continuous variable [2]. Finally, this study was conducted at a single institution in the USA and our findings may not be generalizable to other populations.
In line with previous research on this topic [8, 11, 12, 14, 15], younger age was an independent predictor of appointment no-shows. The effect of race and sex on appointment absenteeism is inconsistent in the literature [10, 16, 17, 27]. In our study, we found that Hispanic and black patients were more likely to miss appointments, but there was no difference with regard to sex. Single or divorced patients were at increased odds of not keeping their scheduled appointments. Similarly, ten Berg and Ring [32] found that unmarried patients were more likely to miss follow-up visits after metacarpal fractures.
In agreement with a study by Ellis and Jenkins [13] performed in outpatient clinics across Scotland, we found that appointments at the beginning of the week were more likely to be missed than those at the end of the week. As suggested in their work [13], the observation that attendance rates are higher on days that elicit emotionally positive associations (e.g., Friday) than on days that elicit emotionally negative associations (e.g., Monday or Tuesday) may indicate that attendance patterns echo those of emotional responses to weekdays [33].
Patients living closer to the office were more likely to miss their appointments. This finding, which is consistent with a recent study by Giunta and colleagues [15] in a primary care setting in Argentina, might seem counterintuitive at first. Additional confirmatory research on this issue is warranted, but it may be possible that patients living near the office feel that they don’t necessarily have to show for their scheduled appointments if they have other unexpected obligations to take care of, as they can more easily come to the office on a more convenient day for them. On the other hand, there may be socioeconomic differences between city dwellers and others.
The reasons for hand surgery no-shows remain incompletely understood and warrant further research. Studies in other settings have shown that reasons for patients to miss appointments include forgetfulness, logistical issues (e.g., family or work commitments, lack of transportation, no access to a telephone), psychological distress, resolution of symptoms, fear of bad news, and lack of understanding of the scheduling system [8, 21, 22, 30].
We were also able to identify a number of factors associated with appointment cancelations. Consistent with a study conducted in dermatology [29], female patients were more likely to cancel appointments than male patients. Furthermore, the likelihood of cancelations was higher in widowed and divorced patients, on weekdays other than Friday, and during the winter season. Research to date has given little attention to the study of determinants of appointment cancelations, perhaps because they have less financial and health implications than no-shows.
Understanding the characteristics of patients who are likely to miss scheduled appointments is an important first step towards developing tailored quality improvement initiatives to reduce non-attendance and maximize productivity in the hand surgery office setting, and to ensure follow-up or needed care in higher risk patients. More research is needed to [1] gain insight into the actual reasons––some of which may be potentially modifiable––for hand surgery patients to miss appointments and to [2] test whether existing interventions (e.g., reminders, managed overbooking, no-show fees) can reduce non-attendance rates on at-risk patients [24].
Acknowledgments
Conflict of Interest
Mariano Menendez declares that he has no conflict of interest.
David Ring declares that he has no conflict of interest.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent
This study was a retrospective database analysis, and no individual informed consent was required.
Contributor Information
Mariano E. Menendez, Email: memenendez@partners.org
David Ring, Phone: 617 724 3953, Email: dring@partners.org.
References
- 1.Adams LA, Pawlik J, Forbes GM. Nonattendance at outpatient endoscopy. Endoscopy. 2004;36(5):402–4. doi: 10.1055/s-2004-814329. [DOI] [PubMed] [Google Scholar]
- 2.Bliss RL, Katz JN, Wright EA, et al. Estimating proximity to care: are straight line and zipcode centroid distances acceptable proxy measures? Med Care. 2012;50(1):99–106. doi: 10.1097/MLR.0b013e31822944d1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clarke H, Soneji N, Ko DT, et al. Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. BMJ. 2014;348:g1251. doi: 10.1136/bmj.g1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cohen AD, Goldbart AD, Levi I, et al. Health provider factors associated with nonattendance in pediatric dermatology ambulatory patients. Pediatr Dermatol. 2007;24(2):113–7. doi: 10.1111/j.1525-1470.2007.00354.x. [DOI] [PubMed] [Google Scholar]
- 5.Cohen AD, Kaplan DM, Kraus M, et al. Nonattendance of adult otolaryngology patients for scheduled appointments. J Laryngol Otol. 2007;121(3):258–61. doi: 10.1017/S0022215106003653. [DOI] [PubMed] [Google Scholar]
- 6.Cohen AD, Kaplan DM, Shapiro J, et al. Health provider determinants of nonattendance in pediatric otolaryngology patients. Laryngoscope. 2005;115(10):1804–8. doi: 10.1097/01.mlg.0000175202.50499.63. [DOI] [PubMed] [Google Scholar]
- 7.Collins J, Santamaria N, Clayton L. Why outpatients fail to attend their scheduled appointments: a prospective comparison of differences between attenders and non-attenders. Aust Health Rev. 2003;26(1):52–63. doi: 10.1071/ah030052. [DOI] [PubMed] [Google Scholar]
- 8.Cosgrove MP. Defaulters in general practice: reasons for default and patterns of attendance. Br J Gen Pract. 1990;40(331):50–2. [PMC free article] [PubMed] [Google Scholar]
- 9.Cronin PR, DeCoste L, Kimball AB. A multivariate analysis of dermatology missed appointment predictors. JAMA Dermatol. 2013;149(12):1435–7. doi: 10.1001/jamadermatol.2013.5771. [DOI] [PubMed] [Google Scholar]
- 10.Deyo RA, Inui TS. Dropouts and broken appointments. A literature review and agenda for future research. Med Care. 1980;18(11):1146–57. doi: 10.1097/00005650-198011000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Dreiher J, Froimovici M, Bibi Y, et al. Nonattendance in obstetrics and gynecology patients. Gynecol Obstet Invest. 2008;66(1):40–3. doi: 10.1159/000115844. [DOI] [PubMed] [Google Scholar]
- 12.Dreiher J, Goldbart A, Hershkovich J, et al. Factors associated with non-attendance at pediatric allergy clinics. Pediatr Allergy Immunol. 2008;19(6):559–63. doi: 10.1111/j.1399-3038.2007.00691.x. [DOI] [PubMed] [Google Scholar]
- 13.Ellis DA, Jenkins R. Weekday affects attendance rate for medical appointments: large-scale data analysis and implications. PLoS One. 2012;7(12):e51365. doi: 10.1371/journal.pone.0051365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Feitsma WN, Popping R, Jansen DE. No-show at a forensic psychiatric outpatient clinic: risk factors and reasons. Int J Offender Ther Comp Criminol. 2012;56(1):96–112. doi: 10.1177/0306624X10389435. [DOI] [PubMed] [Google Scholar]
- 15.Giunta D, Briatore A, Baum A, et al. Factors associated with nonattendance at clinical medicine scheduled outpatient appointments in a university general hospital. Patient Prefer Adherence. 2013;7:1163–70. doi: 10.2147/PPA.S51841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goldman L, Freidin R, Cook EF, et al. A multivariate approach to the prediction of no-show behavior in a primary care center. Arch Intern Med. 1982;142(3):563–7. [PubMed] [Google Scholar]
- 17.Goodhart GL, Kramer M, Zaidi AA. Characteristics of defaulters in treatment for infection with Neisseria gonorrhoeae. J Infect Dis. 1979;140(4):649–51. doi: 10.1093/infdis/140.4.649. [DOI] [PubMed] [Google Scholar]
- 18.Grover S, Gagnon G, Flegel KM, et al. Improving appointment-keeping by patients new to a hospital medical clinic with telephone or mailed reminders. Can Med Assoc J. 1983;129(10):1101–3. [PMC free article] [PubMed] [Google Scholar]
- 19.Hamilton W, Round A, Sharp D. Patient, hospital, and general practitioner characteristics associated with non-attendance: a cohort study. Br J Gen Pract. 2002;52(477):317–9. [PMC free article] [PubMed] [Google Scholar]
- 20.Kruse GR, Rohland BM, Wu X. Factors associated with missed first appointments at a psychiatric clinic. Psychiatr Serv. 2002;53(9):1173–6. doi: 10.1176/appi.ps.53.9.1173. [DOI] [PubMed] [Google Scholar]
- 21.Lacy NL, Paulman A, Reuter MD, et al. Why we don’t come: patient perceptions on no-shows. Ann Fam Med. 2004;2(6):541–5. doi: 10.1370/afm.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lawson VL, Lyne PA, Harvey JN, et al. Understanding why people with type 1 diabetes do not attend for specialist advice: a qualitative analysis of the views of people with insulin-dependent diabetes who do not attend diabetes clinic. J Health Psychol. 2005;10(3):409–23. doi: 10.1177/1359105305051426. [DOI] [PubMed] [Google Scholar]
- 23.Lloyd M, Bradford C, Webb S. Non-attendance at outpatient clinics: is it related to the referral process? Fam Pract. 1993;10(2):111–7. doi: 10.1093/fampra/10.2.111. [DOI] [PubMed] [Google Scholar]
- 24.Molfenter T. Reducing appointment no-shows: going from theory to practice. Subst Use Misuse. 2013;48(9):743–9. doi: 10.3109/10826084.2013.787098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Neal RD, Hussain-Gambles M, Allgar VL, et al. Reasons for and consequences of missed appointments in general practice in the UK: questionnaire survey and prospective review of medical records. BMC Fam Pract. 2005;6:47. doi: 10.1186/1471-2296-6-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Neal RD, Lawlor DA, Allgar V, et al. Missed appointments in general practice: retrospective data analysis from four practices. Br J Gen Pract. 2001;51(471):830–2. [PMC free article] [PubMed] [Google Scholar]
- 27.Oppenheim GL, Bergman JJ, English EC. Failed appointments: a review. J Fam Pract. 1979;8(4):789–96. [PubMed] [Google Scholar]
- 28.Parikh A, Gupta K, Wilson AC, et al. The effectiveness of outpatient appointment reminder systems in reducing no-show rates. Am J Med. 2010;123(6):542–8. doi: 10.1016/j.amjmed.2009.11.022. [DOI] [PubMed] [Google Scholar]
- 29.Penneys NS, Glaser DA. The incidence of cancellation and nonattendance at a dermatology clinic. J Am Acad Dermatol. 1999;40(5 Pt 1):714–8. doi: 10.1016/s0190-9622(99)70152-0. [DOI] [PubMed] [Google Scholar]
- 30.Sharp DJ, Hamilton W. Non-attendance at general practices and outpatient clinics. BMJ. 2001;323(7321):1081–2. doi: 10.1136/bmj.323.7321.1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stone CA, Palmer JH, Saxby PJ, et al. Reducing non-attendance at outpatient clinics. J R Soc Med. 1999;92(3):114–8. doi: 10.1177/014107689909200304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.ten Berg PW, Ring D. Patients lost to follow-up after metacarpal fractures. J Hand Surg [Am] 2012;37(1):42–6. doi: 10.1016/j.jhsa.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 33.Tugade MM, Fredrickson BL. Resilient individuals use positive emotions to bounce back from negative emotional experiences. J Pers Soc Psychol. 2004;86(2):320–33. doi: 10.1037/0022-3514.86.2.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zirkle MS, McNelles LR. Nonattendance at a hospital-based otolaryngology clinic: a preliminary analysis within a universal healthcare system. Ear Nose Throat J. 2011;90(8):E32–4. [PubMed] [Google Scholar]