Abstract
Background
Data are limited regarding the use of peripheral nerve blockade at the level of the forearm, and most studies regard these procedures as rescue techniques for failed or incomplete blocks. The purpose of the study was to investigate patients undergoing hand surgery with distal peripheral nerve (forearm) blocks and compare them with patients having similar procedures under more proximal brachial plexus blockade. No investigations comparing distal nerve blockade to proximal approaches are currently reported in the literature.
Methods
Medical records were retrospectively reviewed for patients who had undergone hand surgery with a peripheral nerve block between November 2012 and October 2013. The primary outcome was the ability to provide a primary anesthetic without the need for general anesthesia or local anesthetic supplementation by the surgical team. Secondary outcome measures included narcotic administration during the block and intraoperative procedures, block performance times, and the need for rescue analgesics in the post anesthesia care unit (PACU).
Results
No statistical difference in conversion rates to general anesthesia was observed between the two groups. Total opiate administration for the block and surgical procedure was lower in the forearm block group. There was no difference in block performance times or need for rescue analgesics in the PACU.
Conclusions
Forearm blocks are viable alternatives to proximal blockade and are effective as a primary anesthetic technique in patients undergoing hand surgery. Compared to the more proximal approaches, these blocks have the benefits of not causing respiratory compromise, the ability to be performed bilaterally, and may be safer in anticoagulated patients.
Keywords: Regional anesthesia, Forearm blocks, Median (or) ulnar (or) radial nerve blocks, Ultrasound-guided, Hand surgery
Introduction
Multiple approaches exist for ultrasound-guided peripheral nerve blockade of the upper extremity. These include the interscalene, supraclavicular, infraclavicular, and axillary blocks, all which carry specific risks and benefits.
Distal peripheral nerve ultrasonographic studies of the median, ulnar, and radial nerves have been documented in the anesthesiology literature [2, 4, 6]. Most studies present these as rescue techniques for a failed or incomplete upper extremity block, with only one study documenting the use of the distal peripheral nerve block as a primary anesthetic technique [1, 2, 4, 6]. These blocks have been demonstrated to be efficacious and safe in patients undergoing hand procedures such as laceration repairs, incision and drainage, and fracture reductions in the emergency department [5].
The current literature is limited regarding forearm blocks as an anesthetic technique for hand surgery. This technique may have advantages over traditionally performed proximal approaches, such as maintenance of respiratory function, decreased bleeding complications at noncompressible sites, and the ability to be used for bilateral procedures.
Materials and Methods
After obtaining approval from the Institutional Review Board, the electronic medical records of all patients undergoing hand surgery with a peripheral nerve block between November 2012 and October 2013 were reviewed. Exclusion criteria included any patients receiving monitored anesthesia care (MAC) with local infiltration by the surgical team or a general anesthetic without a peripheral nerve block.
The forearm block group was comprised of patients receiving median, radial, and ulnar nerve blocks at the level of the proximal to mid-forearm. It is important for the reader to note that we are referring to the superficial sensory branch of the radial nerve. No attempt was made to identify or block the deep motor branch. For the sake of simplicity, we will use terms such as “radial nerve” and “superficial sensory branch of the radial nerve” interchangeably. The comparison group consisted of patients receiving an ultrasound-guided supraclavicular, infraclavicular, or axillary nerve block. All blocks were performed in a designated block area or performed in the operating room by an attending regional anesthesiologist or a resident or fellow under direct supervision prior to the surgical procedure. Intravenous sedation using midazolam or propofol, in combination with a narcotic, was administered during the block procedure in all subjects. Of the 30 forearm blocks, 29 were performed by a single anesthesiologist (JRS) or a trainee under his supervision. In the comparison group, there was variability in the block site, choices, and doses of local anesthetic, as well as the presence of additives; this variability reflects normative practice in a typical busy clinical environment with multiple anesthesiologists.
Forearm Block Technique
After administration of intravenous sedation and application of a chlorhexidine/alcohol skin preparation, a SonoSite S-Nerve Ultrasound System (Bothell, WA) L25 14 MHz probe was placed on the mid-forearm to identify the pertinent structures. The median nerve was easily identified in most patients (Fig. 1). The ulnar nerve was also readily identified medially to the ulnar artery (Fig. 2). The radial nerve was challenging to identify in some patients. While it is located lateral to the radial artery, its distance from and relationship with the corresponding artery was not always uniform, and its location varied as one traced its course in the forearm. Figure 3 illustrates variations of the radial nerve in different subjects. When the nerves were clearly visible, they were traced to the proximal forearm and blocked. If a nerve was not easily seen in the proximal forearm, it was followed distally and blocked where a favorable image was found. All blocks were performed at the level of or proximal to the mid-forearm.
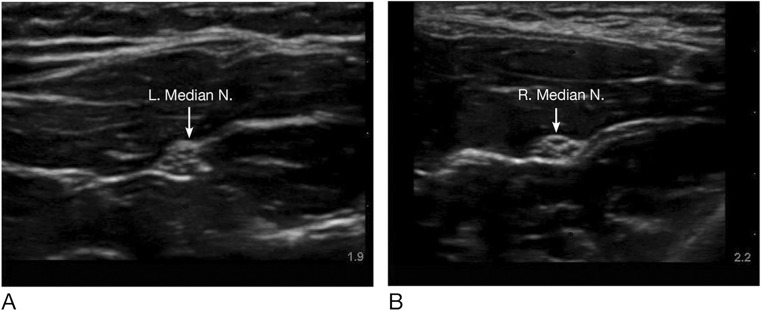
Fig. 1.
a–b Images of the median nerve in two different subjects prior to injection of local anesthetic. L left, R right, N nerve
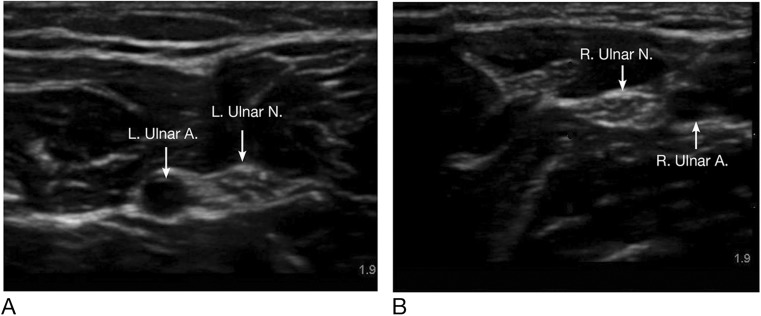
Fig. 2.
a–b Images of the ulnar nerve in two different subjects prior to injection of local anesthetic. L left, R right, N nerve, A artery
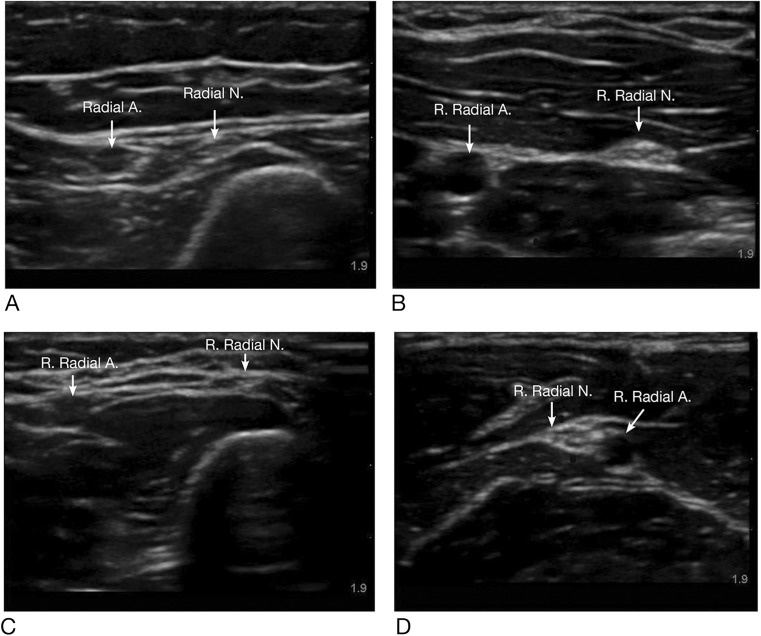
Fig. 3.
a–d Images of the radial nerve in four different subjects prior to injection of local anesthetic. R right, N nerve, A artery
The blocks were performed with the needle inserted in the plane of the ultrasound beam to allow for simultaneous visualization of the needle and target structure. The forearm blocks were performed using a 22-gauge, five-centimeter Stimuplex needle (B. Braun Medical Inc., Melsungen, Germany). The median, radial, and ulnar nerves were systematically blocked in every patient. For most patients, 5 mL of 0.5 % bupivacaine was injected around each nerve with the goal of obtaining circumferential spread. Block performance time was defined as the time required to place the ultrasound probe, acquire the desired images, and perform perineural injections for all three nerves. Figure 4 shows images of various nerves after the local anesthetic injection.
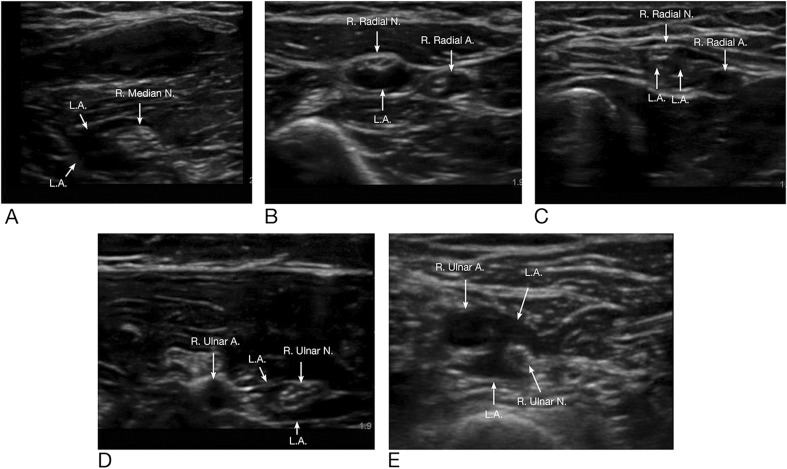
Fig. 4.
a–e Images of various nerves after injection of local anesthetic. R right, N nerve, A artery, L.A. local anesthetic
There were no paresthesias with local anesthetic injection, local anesthetic toxicity, or other complications reported during the block procedures. A propofol infusion was initiated for patient comfort prior to starting the surgical procedure. Administration of narcotics was left to the discretion of the anesthesia providers. Patients were queried by their surgeons regarding sensorimotor function during their follow-up visits, and the anesthesiologist was notified if a nerve injury was suspected.
Statistical Analysis
Our intention was to present a descriptive study showing the efficacy of the distal peripheral nerve blocks compared to traditional proximal brachial plexus blocks. Preliminary statistical analyses indicated that 26 patients per group would be needed to determine a 30 % difference in conversion rate to general anesthesia between the two groups. A delta value of less than 0.3 would suggest equivalence of technique. Categorical variables were presented as percentages, and differences between the groups were assessed using chi-square or Fisher’s exact tests. Continuous variables with skewed distributions were presented as median and 25–75 % interquartile range (IQR25–75%), with differences between groups assessed by the Wilcoxon rank-sum test. P values <0.05 were taken to signify statistical significance.
Results
Thirty patients were included for analysis in each group. Patient demographics were similar between the two groups. Ten out of 30 forearm block group patients were female, while 14 out of 30 in the comparison group were female. There was no statistical difference in the ages of the patients in both groups. No significant difference was found in body mass indices (BMI) among the two groups. All nerve blocks were performed instead of local infiltration and sedation after discussing this with our surgical colleagues, and procedures that were performed under local anesthetic infiltration and sedation were not included in this investigation.
Forearm Block Group
Thirty-three patients received ultrasound-guided distal peripheral nerve blocks of the median, radial, and ulnar nerves at the level of the mid to proximal forearm. Three of these patients were excluded from further analysis. One was excluded because of a missing block note and incomplete anesthetic record, and the other two experienced unexpected delays of greater than 4 h between the block placement and the time of surgery. One patient had bilateral hand surgery performed using bilateral forearm blocks. Because two blocks were performed, these were counted as two separate blocks. A list of the surgical procedures, the types of blocks performed, and the number of patients receiving them are shown in Table 1.
Table 1.
Surgical procedures and respective blocks performed
| Surgical procedure | Distal peripheral nerve block | Supraclavicular block | Infraclavicular block | Axillary block |
|---|---|---|---|---|
| Carpal tunnel release | 1 | |||
| Carpal tunnel revision | 1 | |||
| Closed reduction of finger fracture | 1 | |||
| Closed reduction and percutaneous pinning of finger fracture | 1 | 1 | ||
| Endoscopic carpal tunnel release | 1 | |||
| Finger amputation | 2 | |||
| Finger amputation/bilateral hand incision and drainage | 1 | |||
| Finger arthroplasty | 1 | |||
| Finger arthroplasty and tendon repair | 1 | |||
| Finger manipulation | 1 | |||
| Finger mass excision/biopsy | 2 | 1 | ||
| Hand foreign body removal | 1 | |||
| Hand hardware removal | 3 | 1 | ||
| Hand incision and drainage | 6 | 2 | 1 | |
| Hand ligament repair | 1 | 1 | ||
| Hand mass excision | 3 | 1 | ||
| Hand tendon reconstruction | 1 | |||
| Hand tendon repair | 2 | 2 | ||
| Hand tendon transfer | 1 | |||
| Incision and drainage of thumb or digits | 1 | 1 | ||
| Metacarpal fracture repair | 1 | 1 | ||
| ORIF of finger fracture | 4 | 4 | 1 | 1 |
| Trigger finger release | 1 | 1 | ||
| Release of multiple trigger fingers | 1 | |||
| Trigger finger revision | 1 | |||
| Trigger finger and thumb IP joint fusion | 1 | |||
| Total number of patients | 30 | 19 | 7 | 4 |
Number quantity of patients receiving the respective surgical procedure and block
Plain 0.5 % bupivacaine was used in 27 out of 30 forearm blocks. Two patients received 0.75 % ropivacaine, and 0.5 % bupivacaine with 1:300,000 epinephrine was administered to one patient. Total local anesthetic doses for blockade of all three nerves ranged from 12 to 20 mL, with the average dose being 15.5 mL.
Of the 30 patients receiving the forearm blocks, two were converted to a general anesthetic and one required local anesthetic supplementation by the surgical team. One of these was induced after 86 min of tourniquet time for what was anticipated to be a short procedure. While the forearm blocks did not provide anesthetic coverage for tourniquets, tourniquet intolerance was not an issue in the remaining patients. The median tourniquet time in the forearm block group was 24 min, and even upper arm tourniquets were well tolerated with propofol sedation. The second patient requiring conversion to general anesthesia was undergoing an endoscopic carpal tunnel release after forearm block placement. The patient appeared uncomfortable after the initial incision, and general anesthesia was administered per the surgeon’s preference and request. A third patient undergoing a carpal tunnel revision under a forearm block required local anesthetic supplementation by the surgical team.
Comparison Group
Thirty-five patients received an ultrasound-guided supraclavicular, infraclavicular, or axillary block for hand surgery. Five of these patients were excluded because of missing block notes or incomplete records relating to the block procedure. No bilateral surgical procedures or blocks were performed in this group.
One patient in the supraclavicular block group undergoing a flexor digitorum superficialis slide at the musculotendinous junction of long, ring, and small fingers as well as pinning of the index, long, ring, and small finger MP joints required conversion to general anesthesia per the surgeon’s request for immobility; it is unclear if block failure was a factor in this request.
Ropivacaine 0.5 %, ropivacaine 0.75 %, mepivacaine 1.5 %, bupivacaine 0.5 %, and various combinations thereof, with and without epinephrine, were used for the comparison group blocks. Doses of local anesthetic ranged from 20 to 40 mL, corresponding to an average volume of 29.5 mL. Average local anesthetic doses for supraclavicular, infraclavicular, and axillary blocks were 28.2 mL, 31.4 mL, and 32.5 mL, respectively.
In contrast, patients with higher American Society of Anesthesiologists Physical Status classifications (III and IV) underwent more forearm blocks (14/30 procedures) when compared to the comparison group. More patients underwent forearm blocks inside of the operating rooms immediately prior to their surgical procedure (20/30 procedures). Median times to perform the blocks were not statistically significant. Twenty-four out of 30 proximal block patients (80 %) had a tourniquet used during their procedure, whereas the remaining six had surgery without a tourniquet. Similarly, a tourniquet was used in 24 out of 30 forearm block patients (80 %). Four forearm block patients had surgery without a tourniqet and tourniquet use was not documented in two patients receiving forearm blocks. No statistical significance was found comparing median tourniquet or surgical times between the two groups. Total fentanyl administration for both the block and intraoperative procedure was significantly lower in the forearm block group. Postoperatively, recovery room nurses queried patients to report their pain on a scale of 0 (no pain) to 10 (worst pain imaginable) upon arrival to the PACU. Patient complaints of pain upon arrival to the post anesthesia care unit or the need for rescue analgesics were not statistically different between the groups. These results are summarized in Tables 2 and 3.
Table 2.
Demographics of control and forearm/distal block group
| Control group n = 30 | Forearm/distal arm block group n = 30 | P value | |
|---|---|---|---|
| Age, years [IQR] | 44.5 [28.75–62.5] | 50 [34.5–67.25] | 0.24 |
| Gender, F (%) | 14 (46.6 %) | 10 (33.3 %) | 0.29 |
| BMI, kg/M2 [IQR] | 26.1 [22.8–29.9] | 28.4 [24.9–31.25] | 0.13 |
| ASA PS | |||
| I | 6 | 2 | 0.0012* |
| II | 23 | 14 | |
| III | 0 | 9 | |
| IV | 1 | 5 | |
Chi-square was utilized for contingency analysis
n number of patient; F female; mean, IQR 25–75 % interquartile range; BMI body mass index; ASA PS American Society of Anesthesiologists Physical Status
*Signifies statistical significance
Table 3.
Characteristics of control and forearm/distal block group
| Control group n = 30 | Forearm/distal arm block group n = 30 | P value | |
|---|---|---|---|
| Time to perform block procedure, min [IQR] | 10 [7–13] | 8 [6–12] | 0.14 |
| OR tourniquet time, min [IQR] | 38 [19–68] | 24 [18–39] | 0.28 |
| Surgical time, min [IQR] | 48 [26–72] | 42 [25–66] | 0.41 |
| Total fentanyl administration for block and procedure, mcg [IQR] | 125 [100–200] | 100 [50–100] | 0.01* |
Chi-square was utilized for contingency analysis
n number of patient; median, IQR 25–75 % interquartile range
*Signifies statistical significance
Patients were queried by their surgeons postoperatively regarding nerve injury, and the anesthesiologist was contacted when a nerve injury was suspected. One patient who had a forearm block for a long finger trigger finger release and a thumb IP joint fusion complained of numbness in the radial nerve distribution of the hand, and EMG studies confirmed a radial neuropathy at the level of the proximal forearm, which was subsequently attributed to the block procedure. She reported her symptoms to be improving at telephone follow-up 6 months after surgery. There were no other instances of suspected nerve injury reported in the remaining patients.
Discussion
Our results suggest that this technique is as effective as traditional techniques, across the outcomes of conversion to general anesthesia, the need for local anesthetic supplementation by the surgical team, and opioid consumption.
Familiarity with the surgical procedure is paramount to the successful use of the distal peripheral nerve blocks. Previous experience with these blocks prior to this investigation at our institution suggested that these blocks were most reliable in surgeries limited to the hand, with variable results in procedures involving the wrist and distal forearm. Given the complex innervation of the forearm and wrist, it was not surprising that patients having surgery in this region with a forearm block sometimes required local anesthetic supplementation or conversion to general anesthesia. Both endoscopic and open carpal tunnel surgeries involve incisions of varying lengths, which may extend from the base of the hand to the distal forearm [7]. Our experience mirrors that of Anagnostopoulou et al., where at least part of the forearm was spared in spite of successful deposition of local anesthetic around the target nerve(s) [1]. Additionally, while a more proximal block technique or general anesthesia may be considered in cases with prolonged tourniquet times, forearm blocks are better suited for cases with short tourniquet times.
Our hand surgeons have been pleased with their experience with these blocks and routinely request them for appropriate patients. They have successfully been used in patients where local anesthetic infiltration is contraindicated, such as in cases of infection or suspected malignancy. Our experience has also been favorable in patients having multiple soft tissue procedures or significant bony surgery (such as metacarpal surgery) to limit local anesthetic volumes. By choosing a forearm block over local infiltration, the surgical site anatomy is preserved and may provide for better operating conditions by not causing tissue distortion and edema.
Our hand surgeons have reported that it is not uncommon for patients who receive proximal brachial plexus blocks to voice displeasure about an insensate extremity and lack of motor control after surgery and they have received no such complaints from patients receiving the forearm blocks. Additionally, while all three nerves were blocked in every patient, many hand operations occur in the distribution of only one or two of these nerves. Selective blockade of the specific nerve(s) may shorten the time for anesthetic administration, decrease the risk of unnecessary nerve injury, and minimize sensorimotor impairment postoperatively. Bupivacaine with epinephrine administered via infiltration has an approximate duration of action of 5–8 h, whereas its effects may last as long as 16–18 h if administered via a single-injection brachial plexus block [3]. The duration of forearm blocks is currently unknown, but the potential of a long duration of action, decreased motor blockade, preservation of surgical site anatomy, and ability to provide anesthesia for a wide variety of hand surgeries (including cases with suspected infection or malignancy) may make them an attractive alternative to local infiltration and proximal brachial plexus blocks.
Table 1 illustrates the variety of procedures and patient populations that received forearm blocks as an anesthetic. When considering the performance of these blocks, the anesthesiologist should—as in all cases—be familiar with the operative plan and communicate with all members of the perioperative team. Providers unfamiliar with these blocks may interpret the motor-sparing properties of these blocks preoperatively as block failure and needlessly administer a general anesthetic to the patient.
A limitation of this investigation is that formal sensorimotor assessments were not performed. The onset times of these blocks are currently unknown and undocumented in the literature. Most of these blocks were performed in the operating room immediately prior to their surgical procedure, so a fast onset could be inferred. While the great majority of the distal block patients had intact gross motor function of the upper extremity, sensorimotor function in the PACU and the need for a sling were not clearly documented in many patients. This facet of the forearm blocks could hold tremendous promise for particular hand surgeries, such as following flexor tenolysis, where it is very helpful to have the patient actively flex the finger to demonstrate the extent of finger flexion obtained by the procedure. Further research, particularly comparing sensorimotor function between the proximal and distal approaches, is warranted.
Other potential weaknesses of our investigation, by virtue of its retrospective nature, include variations in local anesthetic types, dosages, and additives; lack of blinding and randomization; as well as lack of patient feedback regarding their surgical and anesthetic experience. One patient in our study had a nerve injury which was attributed to the block procedure. Although our surgeons routinely inquire about numbness and weakness during postoperative follow-up appointments, it is possible that subtle neurologic injuries were not reported by the patients or not relayed to the anesthesiology team for further evaluation. A prospective, randomized study comparing proximal techniques to the forearm blocks for hand surgery is currently underway at our institution. Determination of block onset, sensorimotor testing, standardization of block medications, patient satisfaction, and incidence of nerve injury will be evaluated in this investigation.
In summary, selective blockade of the median, ulnar, and radial nerves at the level of the forearm provides an efficacious alternative to more proximal techniques for patients undergoing hand surgery. While the more proximal techniques will likely remain the gold standard for brachial plexus blockade, the forearm blocks can be promoted from their status as “rescue blocks” to a useful technique in the regionalist’s armamentarium.
Acknowledgments
We would like to thank the Ochsner Clinic Foundation Publishing Services team and Dr. Lauren D. Vazquez for proofreading this submission. We also thank Barbara Siede, MS, from the Ochsner Clinic Foundation Medical Illustration Services for her assistance in the labeling of our images.
Conflict of Interest
José R. Soberón, Jr. received research funding from Pacira Pharmaceuticals (Parsippany, NJ). His institution received an unrestricted research grant from Pacira Pharmaceuticals in 2013. It was not used to fund this investigation, and Pacira Pharmaceuticals’ products and services are not discussed in this manuscript.
Neil R. Bhatt reported no conflicts of interest.
Bobby D. Nossaman reported no conflicts of interest.
Scott F. Duncan reported no conflicts of interest.
Matthew E. Patterson reported no conflicts of interest.
Leslie E. Sisco-Wise reported no conflicts of interest.
José R. Soberón, Jr. had seen the original study data, reviewed the analysis of the data, approved the final manuscript, and is the author responsible for archiving the study files. Neil R. Bhatt had seen the original study data, reviewed the analysis of the data, and approved the final manuscript. Bobby D. Nossaman had seen the original study data, reviewed the analysis of the data, and approved the final manuscript. Scott F. Duncan had seen the original study data, reviewed the analysis of the data, and approved the final manuscript. Matthew E. Patterson had seen the original study data, reviewed the analysis of the data, and approved the final manuscript. Leslie E. Sisco-Wise had seen the original study data, reviewed the analysis of the data, and approved the final manuscript.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Statement of Informed Consent
The requirement for written informed consent was waived by the Institutional Review Board.
Footnotes
This report describes human research. IRB contact information:
Ochsner Clinic Foundation Institutional Review Board
1514 Jefferson Highway
New Orleans, LA 70121
(504) 842-3535
The requirement for written informed consent was waived by the Institutional Review Board.
This report describes an observational clinical study.
This report describes a cross-sectional observational study. The author states that the report includes every item in the STROBE checklist for cross-sectional observational studies.
This manuscript was screened for plagiarism using CrossRefMe.
Contributor Information
José R. Soberón, Phone: (504) 842-4028, Email: jsoberon@ochsner.org
Neil R. Bhatt, Email: nbhatt@ochsner.org
Bobby D. Nossaman, Email: nossaman@mac.com
Scott F. Duncan, Email: scduncan@ochsner.org
Matthew E. Patterson, Email: mpatterson@ochsner.org
Leslie E. Sisco-Wise, Email: lsiscowise@ochsner.org
References
- 1.Anagnostopoulou S, Saranteas T, Chantzi C, Dimitriou V, Karabinis A, Kostopanagiotou G. Ultrasound identification of the radial nerve and its divisions. Is rescue nerve block at or below the elbow possible? Anaesth Intensive Care. 2008;36(3):457–459. [PubMed] [Google Scholar]
- 2.Gray AT, Schafhalter-Zoppoth I. Ultrasound guidance for ulnar nerve block in the forearm. Reg Anesth Pain Med. 2003;28(4):335–339. doi: 10.1016/s1098-7339(03)00196-2. [DOI] [PubMed] [Google Scholar]
- 3.Hadzic, A. Textbook of regional anesthesia and acute pain management. 1st ed. McGraw-Hill Professional; 2007.
- 4.Kathirgamanathan A, French J, Foxall GL, Hardman JG, Bedforth NM. Delineation of distal ulnar nerve anatomy using ultrasound in volunteers to identify an optimum approach for neural blockade. Eur J Anaesthesiol. 2009;26(1):43–46. doi: 10.1097/EJA.0b013e328318c5b6. [DOI] [PubMed] [Google Scholar]
- 5.Liebmann O, Price D, Mills C, Gardner R, Wang R, Wilson S, et al. Feasibility of forearm ultrasonography-guided nerve blocks of the radial, ulnar, and median nerves for hand procedures in the emergency department. Ann Emerg Med. 2006;48(5):558–562. doi: 10.1016/j.annemergmed.2006.04.014. [DOI] [PubMed] [Google Scholar]
- 6.McCartney CJ, Xu D, Constantinescu C, Abbas S, Chan VW. Ultrasound examination of peripheral nerves in the forearm. Reg Anesth Pain Med. 2007 Sep-Oct;32(5):434–439. Erratum in: Reg Anesth Pain Med. 2008 Mar-Apr;33(2):188. [DOI] [PubMed]
- 7.Mintalucci DJ, Leinberry CF., Jr Open versus endoscopic carpal tunnel release. Orthop Clin North Am. 2012;43(4):431–437. doi: 10.1016/j.ocl.2012.07.012. [DOI] [PubMed] [Google Scholar]