Abstract
Background
Multiple wrist x-ray images have been described to assess for scapholunate (SL) instability. Some views may be redundant. The purpose of this study was to compare three plain x-ray views in identifying a traumatic diastasis of the SL interval.
Methods
Nineteen patients (19 wrists) with a positive scaphoid shift test and surgically confirmed SL ligament damage were identified. There were 15 males and 4 females with a mean age of 39 years. Pre-operative x-rays were reviewed, including posteroanterior (PA) neutral and PA ulnar deviation views of the injured wrist, and PA clenched fist views of the injured and uninjured wrists. Dynamic SL instability was defined by an SL mid-interval gap of <3 mm and static SL instability by a gap of ≥3 mm in the PA neutral views. The mid-interval measurements were compared between x-ray images.
Results
There were 10 dynamic and 9 static SL instability cases. The PA ulnar deviation and the PA clenched fist views showed significantly greater SL gaps in comparison to the PA neutral views in dynamic but not static SL instability cases. In both categories of instability, there was no significant difference in the SL gaps between the two stress images. The PA clenched fist view of the uninjured wrist revealed SL gapping of >3 mm in 50% of patients but with generally greater gapping in the clenched fist view of the injured wrist.
Conclusions
The PA ulnar deviation and clenched fist stress views were equally effective in showing a dynamic SL diastasis following wrist injury. Neither view was more effective than a neutral PA view in diagnosing static SL instability.
Keywords: Carpal instability, Scapholunate instability, Wrist radiography
Introduction
The scapholunate (SL) interosseous ligament, secondary scaphoid ligamentous restraints, the flexor carpi radialis muscle, and joint conformity play interrelated roles in maintaining normal scapholunate alignment and carpal kinematics [12, 16, 17, 20, 23, 26, 28]. Dynamic SL interval instability represents an injury primarily to the SL ligament and may require stress x-ray imaging for diagnostic confirmation [12, 19]. Static SL interval instability, in the absence of bone injury and/or joint deformity, results from damage to both the SL ligament and secondary soft tissue restraints and will often be evident on routine posteroanterior (PA) and lateral x-ray projections [3, 17, 23].
Multiple stress x-ray imaging positions have been described to assess for SL instability, including clenched fist PA and anteroposterior, PA clenched pencil, PA thumb-finger traction, and ulnar deviation projections (PA and anteroposterior) [2, 4–6, 9–11, 13, 14, 21]. Lee et al. [14] performed a cadaveric study to evaluate eight different stress x-ray views and determined that the PA clenched pencil view was the most effective in showing dynamic SL instability. Sulkers et al. [24, 25] carried out two retrospective studies of patients suspected to have carpal instability and found cineradiography with the wrist in various positions useful in the diagnosis of SL dissociation. To our knowledge, there are no in vivo comparative studies of plain stress x-ray imaging in the assessment of SL instability. In a cost-conscious health-care environment, and without an accessible fluoroscopy machine, limiting the number of plain x-ray images completed to diagnose carpal malalignment may be important.
The purpose of this study was to compare the effectiveness of the PA neutral, the PA ulnar deviation, and the PA clenched fist x-ray images in depicting an SL diastasis in patients with clinically suspected and surgically proven SL ligament damage. We hypothesized that the PA ulnar deviation and the PA clenched fist stress x-ray views would reveal similar SL interval gaps in dynamic and static SL instability cases.
Materials and Methods
Twenty-one patients (21 wrists) with symptomatic SL instability following trauma who underwent surgery by six fellowship-trained hand surgeons between 2006 and 2011 were identified. After obtaining institutional review board approval, the office charts and pre-operative wrist x-rays were reviewed in each case. Two patients with a concomitant wrist fracture were excluded from the analysis. There were no patients with a known history of gout or pseudogout, rheumatoid arthritis, a remote wrist fracture, or previous surgery performed on either wrist. The final study population of 19 patients (19 wrists) included 15 males and 4 females with a mean age of 39 years (range, 23 to 56 years). Records in each case reflected SL interval tenderness and a painful scaphoid shift test [5].
All 19 patients underwent open wrist surgery from a dorsal approach, 17 of whom also underwent wrist arthroscopy preceding or concurrent with the open wrist procedure. The open procedures included SL interval pinning, SL ligament repair, and dorsal capsulodesis. A Geissler grade IV SL tear (i.e., small-joint camera passed through the SL interval) was detected in 11 cases, and a Geissler grade III SL tear (i.e., small-joint probe passed through the SL interval) was detected in 6 cases [7]. Complete tears of the dorsal component of the SL ligament were documented in 15 cases, and partial tears with attenuation of the dorsal component of the SL ligament were noted in the remaining 4 cases. We were unable to determine the presence of bony ligamentous avulsions or the integrity of the volar component of the SL ligaments from the operative reports.
Pre-operative digitized x-rays included a PA neutral view of the injured wrist, a PA ulnar deviation of the injured wrist, and PA clenched fist views of both the injured and uninjured wrists (Fig. 1). The technical quality of each image was gauged by assessing the position of the ulnar groove in relationship to the ulnar styloid [14, 15]. A true PA neutral view was defined by the positioning of the extensor carpi ulnaris groove radial to the midline of the ulnar styloid and roughly parallel alignment of the third carpometacarpal joint with the longitudinal axis of the radius. Standard PA stress views (PA ulnar deviation and PA clenched fist) were defined by the extensor carpi ulnaris groove situated radial to the midline of the ulnar styloid.
Fig. 1.
a True posteroanterior neutral, b standard posteroanterior ulnar deviation, and c standard posteroanterior clenched fist x-ray images of an injured wrist with dynamic scapholunate instability. d Standard posteroanterior clenched fist x-ray view of the uninjured wrist in the same patient. The true posteroanterior neutral view is defined by the location of the extensor carpi ulnaris groove radial to the midline of the ulnar styloid and roughly parallel alignment of the third carpometacarpal joint with the longitudinal axis of the radius. Standard posteroanterior stress views (ulnar deviation and PA clenched fist) are defined by the situation of the extensor carpi ulnaris groove radial to the midline of the ulnar styloid [14, 15]
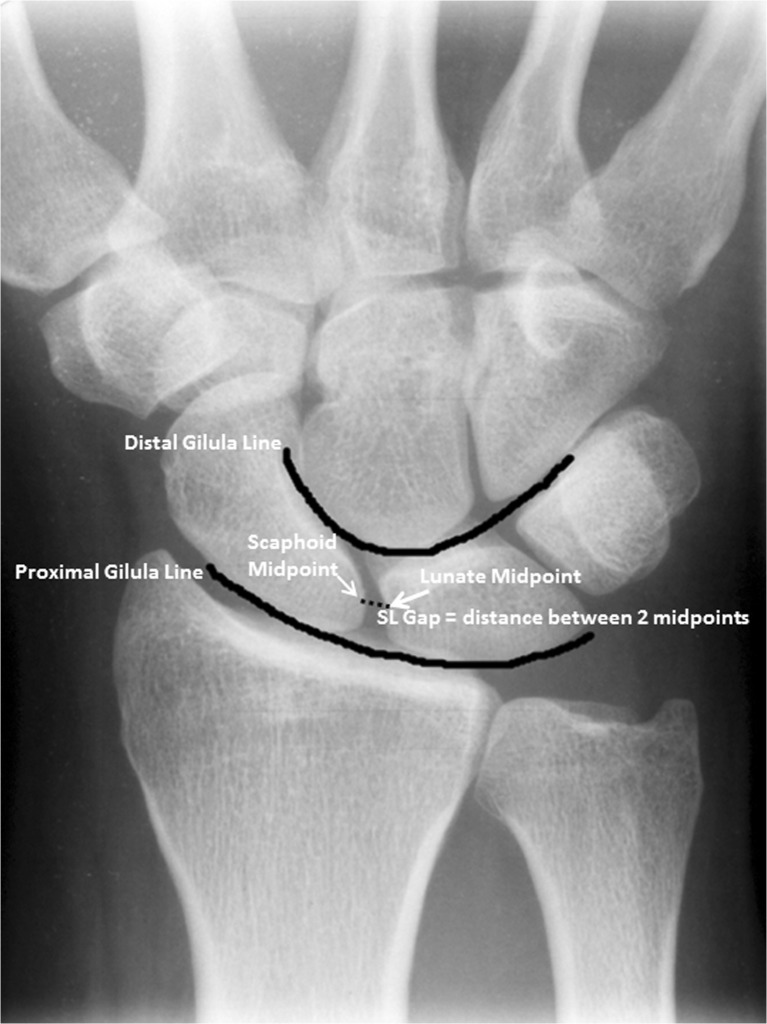
Carpal angulation and mid-interval SL distances were measured using previously described techniques [14]. Carpal angulation signified the angle between the longitudinal axes of the distal radius and the third metacarpal. The midpoints between the Gilula lines of the proximal and distal borders of the proximal carpal row were marked on the scaphoid and lunate surfaces of the SL joint, and the distance between these two points denoted the mid-interval SL gap (Fig. 2). When the SL joint was not well profiled, the mid-interval SL gap was measured from the most clearly visible edges of the scaphoid and lunate at the joint line [14].
Fig. 2.
Scapholunate mid-interval measurement. The midpoints between the Gilula lines of the proximal and distal borders of the proximal carpal row are marked on the scaphoid and lunate surfaces at the scapholunate joint. The distance between these points is defined as the mid-interval gap. When the scapholunate joint is not well profiled, the mid-interval scapholunate distance is measured from the most clearly visible edges of the scaphoid and lunate at the joint [14]
Dynamic instability was defined by a mid-interval SL gap of less than 3 mm on the PA neutral image that widened with stress x-ray imaging. Static SL instability was characterized by a mid-interval SL gap of 3 mm or more on the PA neutral image [2]. Arthritic changes were categorized as joint space narrowing, subchondral sclerosis, subchondral cyst formation, and osteophyte formation.
Two blinded authors reviewed and completed measurements on all x-rays independently and came to a consensus on the technical quality of the images and the presence of arthritic changes. The distal radius to third metacarpal angles was measured to the nearest degree, and mid-interval SL distances were measured to the nearest tenth of a millimeter. Statistical analysis was performed using Microsoft Excel software (version 14.0, Redmond, WA). The independent x-ray measurements were averaged and summarized by means, standard deviations, and ranges. The averaged mid-interval SL gaps were compared using the two-tailed Student t test with a level of significance set at P < .05.
Results
There were 10 dynamic and 9 static SL instability cases. A true PA neutral view was confirmed in 17 of 19 injured wrists. Completion of a standard PA stress view was determined for 18 injured wrist ulnar deviation views, 17 injured wrist clenched fist views, and 18 uninjured wrist clenched fist views. Angulation of the carpus was in an ulnar direction in nearly all cases, averaging 8° ± 1° (range, 0° to 18°) in the PA neutral views of the injured wrists, 31° ± 3° (range, 13° to 49°) in the PA ulnar deviation views of the injured wrists, 6° ± 2° (range, 9° radial to 19° ulnar) in PA clenched fist views of the injured wrists, and 11° ± 1° (range, 2° to 21°) in the PA clenched fist views of the uninjured wrists.
Tables 1 and 2 include the average mid-interval SL measurements. In the dynamic SL instability cases, the mid-interval SL measurements in both stress views of the injured wrists were significantly greater than the mid-interval SL measurements obtained from the PA neutral views of the same wrists (P < .001, Table 3). The SL interval measurement increased with stress imaging in all dynamic instability cases. There were no significant differences in the SL gaps between the two stress images or between the PA clenched fist views of the injured and uninjured wrists.
Table 1.
Dynamic scapholunate instability
| Cases (10) | Mid-interval SL (mm) |
|---|---|
| PA neutral injured wrist | 2.1 ± 0.3 (1.4–2.9) |
| PA ulnar deviation injured wrist | 3.8 ± 0.4 (2.4–4.9) |
| PA clenched fist injured wrist | 3.6 ± 0.3 (2.3–5.4) |
| PA clenched fist uninjured wrist | 3.1 ± 0.2 (1.7–5.0) |
Data presented as means, standard deviations, and ranges
SL scapholunate, PA posteroanterior
Table 2.
Static scapholunate instability
| Cases (9) | Mid-interval SL (mm) |
|---|---|
| PA neutral injured wrist | 4.6 ± 0.9 (3.3–7.3) |
| PA ulnar deviation injured wrist | 5.1 ± 0.7 (1.8–7.6) |
| PA clenched fist injured wrist | 4.8 ± 0.6 (3.1–7.4) |
| PA clenched fist uninjured wrist | 3.6 ± 0.4 (1.6–5.1) |
Data presented as means, standard deviations, and ranges
SL scapholunate, PA posteroanterior
Table 3.
Comparisons of stress radiographic views
| SL interval comparisons | Dynamic cases (P value) | Static cases (P value) |
|---|---|---|
| PA ulnar deviation injured wrist vs. PA neutral injured wrist | <.001 | .32 |
| PA clenched fist injured wrist vs. PA neutral injured wrist | <.001 | .67 |
| PA ulnar deviation injured wrist vs. PA clenched fist injured wrist | .47 | .54 |
| PA clenched fist injured wrist vs. PA clenched fist uninjured wrist | .32 | .003 |
SL scapholunate, PA posteroanterior
In the static SL instability cases, the SL gap in the injured wrists increased with stress imaging in all but one patient. The mid-interval distance in this case decreased from 4.7 mm in the PA neutral view to 1.8 mm in the PA ulnar deviation view (the carpal angle in this projection measured 14° in an ulnar direction and the image was standardized). The were no significant differences in the SL diastases between the stress x-ray images and the PA neutral views (P ≥ .32) nor was there a significant difference in the SL diastases between the two stress radiographic views (Table 3). In contrast to the dynamic instability cases, the SL gaps in the PA clenched fist views of the injured wrists were significantly greater than the SL gaps in the PA clenched fist images of the uninjured wrists (P = .003).
The PA clenched fist views of the uninjured wrists revealed abnormal SL gaps of greater than 3 mm in 9 of 19 patients (Table 4). In four dynamic SL instability cases, there was generally a small increase in the SL interval measurements between the injured and uninjured PA clenched fist views; however, this was not significant. In the five static SL instability cases, there was a significant difference in SL gap between the injured and uninjured PA clenched fist views with a mean gap difference measuring more than 1 mm (P = .03).
Table 4.
Uninjured wrists with scapholunate interval widening
| PA clenched fist | Uninjured wrist mid-interval SL (mm) | Injured wrist mid-interval SL (mm) |
|---|---|---|
| Dynamic SL instability (4 cases) | 3.8 ± 0.8 (3.2–5.0) | 3.8 ± 0.3 (3.4–4.0) |
| Static SL instability (5 cases) | 4.3 ± 0.7 (3.3–5.1) | 5.7 ± 1.0 (4.8–7.4) |
Data presented as means, standard deviations, and ranges
SL scapholunate, PA posteroanterior
Degenerative arthritic changes were present in six patients: three dynamic SL instability cases, three static SL instability cases, and three uninjured wrists in the same subgroup of patients. Arthritis was characterized by a narrowed radioscaphoid articulation in all but one patient who was found to have a subchondral cyst in the proximal pole of each scaphoid bone. There were no arthritic changes involving the scaphotrapeziotrapezoid or capitolunate articulations.
Discussion
Plain radiographs remain a valuable tool in the diagnosis of SL instability. Various SL stress radiographic techniques have been advocated; however, there is no universally accepted best view. Several methods for measuring the SL interval have been reported with abnormal values ranging from 2 to 4 mm [19, 22]. We adopted the mid-interval SL measurement technique described by Lee et al. [14], and we defined an abnormal gap in our static SL instability cases as 3 mm or greater on a neutral PA x-ray view [2]: a threshold value commonly used in our clinical practices.
Lee et al. [14] performed a cadaveric experiment to assess eight stress x-ray images and concluded that the PA clenched pencil view consistently showed the widest SL gap. All ligaments surrounding the scaphoid were sectioned in their study. Since cadaveric testing will not predictably simulate in vivo kinematics, and because cineradiography may not be readily available in all physician practices [24, 25], we sought to assess the effectiveness of the PA ulnar deviation and the PA clenched fist views in depicting SL diastases in patients with surgically confirmed SL ligament damage. An increase in SL joint spacing was depicted in all dynamic SL instability cases using either stress x-ray image. In contrast, the stress x-rays in our static SL instability cases showed no significant increase in SL gapping when compared to the PA neutral views.
The SL gap unexpectedly decreased in 1 static SL instability case when the wrist was imaged with the carpus in 14° of ulnar deviation. The average ulnar deviation angle of the injured carpus was approximately twice this number in the compilation of PA ulnar deviation views. We suspect that near neutral alignment of the carpus and possibly slight rotation of the wrist (although the image met the criteria for a standard stress view) factored into the appearance of SL joint space narrowing in this case. Lee et al. [14] found that the maximum SL gap occurred with the wrist positioned in 30° of ulnar deviation, whereas smaller gaps developed with the wrist positioned in greater or lesser angles of ulnar deviation. Moneim [18] reported that overlap of the scaphoid and lunate on a PA projection without 20° of forearm pronation could obscure recognition of an SL gap.
An SL gap of more than 3 mm was depicted in 50% of the uninjured wrist PA clenched fist views in our series, including both dynamic and static SL instability cases. The SL interval increase was generally greater in the PA clenched fist view of the injured wrist in each case; however, the difference in SL gapping between wrists was only significant in the static SL cases. Atraumatic SL interval widening has been reported in asymptomatic individuals [8, 27], and the clinical relevance of this x-ray finding remains uncertain. There were no patients in our study with a known history of gout or pseudogout: two recognized risk factors for SL dissociation [1].
This study has several limitations. The participating hand surgeons did not routinely order other stress radiographs of the injured wrist, a PA neutral view of the uninjured wrist, or comparative lateral wrist images. Failure to obtain standard PA stress and true PA neutral views in a few cases and underlying degenerative arthritic changes may have influenced the SL interval measurements. The angle of flexion or extension of the wrist, a variable which will conceivably affect imaging of the SL joint, was not monitored [14, 22]. Only patients with surgically confirmed SL ligament damage were included; consequently, the findings may not be applicable to all patients with SL instability. Finally, the number of cases studied was relatively small, precluding statistical power. We determined that 64 cases in each group would have been necessary to detect a difference of 0.5 mm in the SL interval measurements between stress views with a statistical power level of .8 and a probability level of .05.
Based on the findings from our study, both PA ulnar deviation and PA clenched fist views were equally effective in depicting dynamic SL instability. One rather than both of these stress x-ray views may be adequate in assessing for an abnormally increased SL interval in a suspected case of dynamic SL instability. In patients with static SL instability, the PA neutral view was as useful as either stress view at showing an SL gap. An SL diastasis in the PA grip view of the uninjured wrist was a common finding, underscoring the importance of standardized stress imaging and corroborative clinical examination findings in diagnosing clinically relevant SL instability.
Acknowledgments
Grant Support
None.
Conflict of Interest
Ronak M. Patel declares that he has no conflict of interest.
David M. Kalainov has received consulting fees from Acumed and Skeletal Kinetics unrelated to this study.
Brian J. Chilelli declares that he has no conflict of interest.
Richard L. Makowiec has received consulting fees from Skeletal Kinetics unrelated to this study.
Statement of Human and Animal Rights
This article does not contain any studies with human or animal subjects. Nevertheless, all potentially applicable procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as reviewed in 2008. Approval was obtained for this study from the Institutional Review Board of Northwestern University.
Statement of Informed Consent
Informed patient consent was waived by the Institutional Review Board of Northwestern University given the retrospective design of the study with no patient interaction or published personal identifying information.
Funding Received
We received no funding directly or indirectly related to this study.
References
- 1.Beck JD, Deegan JH, Riehl JT, et al. Incidence of scapholunate ligament dissociation in patients with aspiration-confirmed gout. J Hand Surg [Am] 2010;35:1938–1942. doi: 10.1016/j.jhsa.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 2.Belsole RJ. Radiography of the wrist. Clin Orthop Relat Res. 1986;202:50–56. [PubMed] [Google Scholar]
- 3.Berger RA, Imeada T, Berglund L, et al. Constraint and material properties of the subregions of the scapholunate interosseous ligament. J Hand Surg [Am] 1999;24:953–962. doi: 10.1053/jhsu.1999.0953. [DOI] [PubMed] [Google Scholar]
- 4.Cautilli GP, Wehbe MA. Scapho-lunate distance and cortical ring sign. J Hand Surg [Am] 1991;16:501–503. doi: 10.1016/0363-5023(91)90022-4. [DOI] [PubMed] [Google Scholar]
- 5.Chen F, Kalainov DM. Examination, imaging, staging, and conservative treatment options. Atlas Hand Clin. 2003;8:201–208. doi: 10.1016/S1082-3131(03)00045-1. [DOI] [Google Scholar]
- 6.Frot B, Alnot JY, Folinais D, et al. Visualization of the scapholunate space. Description of a simple radiologic image. Ann Chir Main. 1986;5:335–338. doi: 10.1016/S0753-9053(86)80013-8. [DOI] [PubMed] [Google Scholar]
- 7.Geissler WB, Freeland AE, Savoie FH, et al. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg Am. 1996;78:357–365. doi: 10.2106/00004623-199603000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Gharbaoui IS, Netscher DT, Kessler FB. Chronic asymptomatic contralateral wrist scapholunate dissociation. Plast Reconstr Surg. 2005;116:1672–1678. doi: 10.1097/01.prs.0000187138.31451.79. [DOI] [PubMed] [Google Scholar]
- 9.Gilula LA. Carpal injuries: analytic approach and case exercises. AJR Am J Roentgenol. 1979;133:503–517. doi: 10.2214/ajr.133.3.503. [DOI] [PubMed] [Google Scholar]
- 10.Gilula LA. Commentary: the clenched pencil view. J Hand Surg [Am] 2003;28:419–420. doi: 10.1053/jhsu.2003.50066. [DOI] [PubMed] [Google Scholar]
- 11.Kindynis P, Resnick D, Kang HS, et al. Demonstration of the scapholunate space with radiography. Radiology. 1990;175:278–280. doi: 10.1148/radiology.175.1.2315496. [DOI] [PubMed] [Google Scholar]
- 12.Kitay A, Wolfe SW. Scapholunate instability: current concepts in diagnosis and management. J Hand Surg [Am] 2012;37:2175–2196. doi: 10.1016/j.jhsa.2012.07.035. [DOI] [PubMed] [Google Scholar]
- 13.Lawand A, Foulkes GD. The “clenched pencil” view: a modified clenched fist scapholunate stress view. J Hand Surg [Am] 2003;28:414–418. doi: 10.1053/jhsu.2003.50046. [DOI] [PubMed] [Google Scholar]
- 14.Lee SK, Desai H, Silver B, et al. Comparison of radiographic stress views for scapholunate dynamic instability in a cadaver model. J Hand Surg [Am] 2011;36:1149–1157. doi: 10.1016/j.jhsa.2011.05.009. [DOI] [PubMed] [Google Scholar]
- 15.Levis CM, Yang Z, Gilula LA. Validation of the extensor carpi ulnaris groove as a predictor for the recognition of standard posteroanterior radiographs of the wrist. J Hand Surg [Am] 2002;27:252–257. doi: 10.1053/jhsu.2002.31150. [DOI] [PubMed] [Google Scholar]
- 16.Mayfield JK, Johnson RP, Kilcoyne RK. Carpal dislocations: pathomechanics and progressive perilunar instability. J Hand Surg. 1980;5:226–241. doi: 10.1016/S0363-5023(80)80007-4. [DOI] [PubMed] [Google Scholar]
- 17.Mitsuyasu H, Patterson RM, Shah MA, et al. The role of the dorsal intercarpal ligament in dynamic and static scapholunate instability. J Hand Surg [Am] 2004;29:279–288. doi: 10.1016/j.jhsa.2003.11.004. [DOI] [PubMed] [Google Scholar]
- 18.Moneim MS. The tangential posteroanterior radiograph to demonstrate scapholunate dissociation. J Bone Joint Surg Am. 1981;63:1324–1326. [PubMed] [Google Scholar]
- 19.Pliefke J, Stengel D, Rademacher G, et al. Diagnostic accuracy of plain radiographs and cineradiography in diagnosing traumatic scapholunate dissociation. Skeletal Radiol. 2008;37:139–145. doi: 10.1007/s00256-007-0410-7. [DOI] [PubMed] [Google Scholar]
- 20.Salva-Coll G, Garcia-Elias M, Llusa-Perez M, et al. The role of the flexor carpi radialis muscle in scapholunate instability. J Hand Surg [Am]. 2011;36:31-36 [DOI] [PubMed]
- 21.Schernberg F. Roentgenographic examination of the wrist: a systematic study of the normal, lax and injured wrist. Part 1: the standard and positional views. J Hand Surg [Br]. 1990;15:210–9. [DOI] [PubMed]
- 22.Schimmerl-Metz SM, Metz VM, Totterman SM, et al. Radiologic measurement of the scapholunate joint: implications of biologic variation in scapholunate joint morphology. J Hand Surg [Am] 1999;24:1237–1244. doi: 10.1053/jhsu.1999.1237. [DOI] [PubMed] [Google Scholar]
- 23.Short WH, Werner FW, Green JK, et al. Biomechanical evaluation of the ligamentous stabilizers of the scaphoid and lunate: part III. J Hand Surg [Am] 2007;32:297–309. doi: 10.1016/j.jhsa.2006.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sulkers GSI, Schep NWL, Mass M, et al. Intraobserver and interobserver variability in diagnosing scapholunate dissociation by cineradiography. J Hand Surg [Am] 2014;39:1050–1054. doi: 10.1016/j.jhsa.2014.03.014. [DOI] [PubMed] [Google Scholar]
- 25.Sulkers GSI, Schep NWL, Mass M, et al. The diagnostic accuracy of wrist cineradiography in diagnosing scapholunate dissocation. J Hand Surg [Eur]. 2014;39:263–71. [DOI] [PubMed]
- 26.Thienpont E, Mulier T, De Smet L. Radiographic analysis of anatomic risk factors for scapholunate dissociation. Acta Orthop Belg. 2003;69:246–251. [PubMed] [Google Scholar]
- 27.Vance RM, Gelberman RH, Braun RM. Chronic bilateral scapholunate dissociation without symptoms. J Hand Surg. 1979;4:178–180. doi: 10.1016/S0363-5023(79)80138-0. [DOI] [PubMed] [Google Scholar]
- 28.Werner FW, Short WH, Green JK, et al. Severity of scapholunate instability is related to joint anatomy and congruency. J Hand Surg [Am] 2007;32:55–60. doi: 10.1016/j.jhsa.2006.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]