Abstract
Background
Assessment of joint range of motion (ROM) is an accepted evaluation of disability as well as an indicator of recovery from musculoskeletal injuries. Many goniometric techniques have been described to measure ROM, with variable validity due to inter-rater reliability. In this report, we assessed the validity of photograph-based goniometry in measurement of ROM and its inter-rater reliability and compared it to two other commonly used techniques.
Methods
We examined three methods for measuring ROM in the upper extremity: manual goniometry (MG), visual estimations (VE), and photograph-based goniometry (PBG). Eight motions of the upper extremity were measured in 69 participants at an academic medical center.
Results
We found visual estimations and photograph-based goniometry to be clinically valid when tested against manual goniometry (r avg. 0.58, range 0.28 to 0.87). Photograph-based measurements afforded a satisfactory degree of inter-rater reliability (ICC avg. 0.77, range 0.28 to 0.96).
Conclusions
Our study supports photograph-based goniometry as the new standard goniometric technique, as it has been clinically validated, is performed with greater consistency and better inter-rater reliability when compared with manual goniometry. It also allows for better documentation of measurements and potential incorporation into medical records in direct contrast to visual estimation.
Keywords: Range of motion, Visual estimation, Photograph, Goniometry
Introduction
Joint range of motion (ROM) is a fundamental measure in orthopedic practice, with widespread applications in rehabilitation, clinical decision-making, outcome analysis, and determination of disability rating [6, 9, 11, 14, 18, 22]. Measurements of joint ROM have become common means of communication among medical practitioners who care for the same patient. Similarly, joint ROM has become an integral measurement in determining patient outcomes both before and after surgical intervention in scientific literature [1].
Goniometry is commonly used for measurement of ROM. There are various valid goniometric techniques including use of a standard mechanical goniometer placed across the joint [8], visual estimations made by orthopedic professionals [4], computer-based measurements from photographs taken of the joint [5, 21], and devices worn that span the joint [2]. The standard goniometer is the most frequently used technique, as it is simple, inexpensive, portable, and durable [7, 15, 19]. Yet, it has been criticized for its poor inter-rater reliability [7]. Available evidence suggests that the measurements with standard goniometry are most accurate if taken by the same person each time [16]. In a large healthcare setting, this notion becomes infeasible, and signifies the importance of a facile technique with great inter-rater reliability.
Photograph-based goniometry has been best studied for its use in the elbow [5, 12, 14] and knee [3, 10, 13, 21, 22, 24], with possible utility in the hand [17, 23]. In this study, we compared three different techniques for measuring joint ROM at the elbow and wrist. The purpose was to identify a technique that yields a combination of accuracy, inter-rater reliability, cost-effectiveness, and efficiency. The goal was to identify the technique that allows for the most accurate and reliable assessment of joint ROM in the clinic by various examiners. Our hypothesis was that photograph-based goniometry would show equally valid measures of joint ROM as manual goniometry and offer acceptable inter-rater reliability.
Materials and Methods
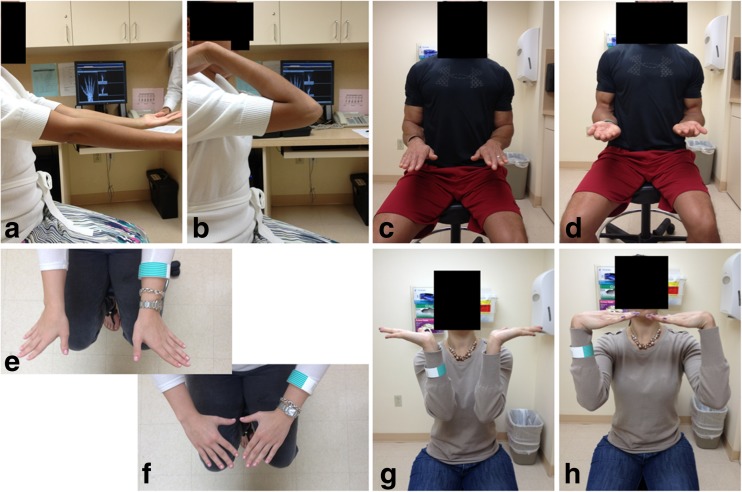
Patients seen in an orthopedic hand surgery clinic in an academic institution from May to June 2014 were considered for inclusion in the study. Prisoners, pregnant women, patients under the age of 18, and those unable to perform the upper extremity movements required were excluded from the final study sample. The patients enrolled in the study were asked to perform eight exercises: elbow extension and flexion, pronation and supination, wrist ulnar and radial deviation, and wrist extension and flexion (Fig. 1). All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5). Informed consent was obtained from all patients for being included in the study. Additional informed consent was obtained from all patients for whom identifying information is included in this article.
Fig. 1.
Upper extremity motions measured included a elbow extension, b elbow flexion, c pronation, d supination, e ulnar deviation, f radial deviation, g wrist extension, and h wrist flexion. Range of motion was assessed for each exercise and recorded in degrees from neutral motion with the exception of extension/flexion of the elbow, which was recorded in degrees from complete extension (0°)
Measurement Techniques
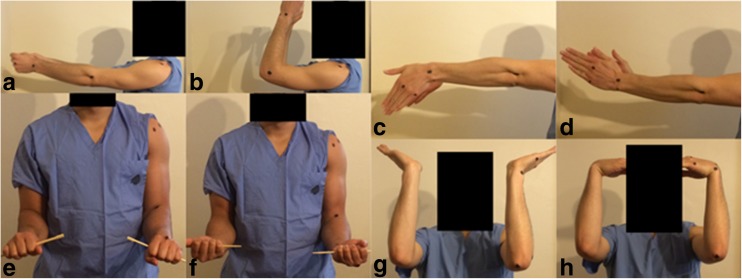
Range of motion for each exercise was measured by three techniques: clinical goniometric measurements made by trained volunteer medical students, visual estimations made by a fellowship-trained hand surgeon, and measurements of angles from pictures made by volunteer medical students (Fig. 2).
Fig. 2.
Measurement techniques included a T1—manual goniometry, b T2—visual estimations, and c T3—picture measurements
Technique 1—Manual Goniometry
Goniometric measurements were made using a standard goniometer. Elbow extension and flexion were measured with arm externally rotated. The three reference points used for this measurement were mid-point on the lateral arm over the humeral shaft, lateral epicondyle, and radial styloid. Pronation and supination were measured with arms at the patient’s sides and elbows flexed 90°. The angle of the plane of hand with metacarpophalangeal joints in extension relative to the shaft of the humerus was measured. Ulnar and radial deviation of the wrist were measured in a similar arm and elbow position with wrist in 90° of pronation. Extension and flexion of the wrist were measured on the ulnar side of the wrist; with reference points of the olecranon process, the ulnar styloid, and the fifth metacarpal (Fig. 1).
Technique 2—Visual Estimations
All estimations were made by a fellowship-trained hand surgeon using the aforementioned points of reference for each motion.
Technique 3—Photograph-Based Goniometry
Digital photographs were taken of the patients’ upper extremities at the endpoint of their range of motion. The photographer faced the patient for wrist exercises and stood on the side of the patient for elbow exercises with camera at the level of the moving joint. Computer software (ImageJ, Bethesda, MA) was used to calculate angles of the joints. Each arm of the angle measurement tool was placed in similar fashion as described above for the manual goniometry measurements. Apple iPhone 4s camera (Apple, Cupertino, CA) was used for all photographs taken in this study.
Data Analysis
Each measurement technique was evaluated for its validity by comparing it against the current standard, manual goniometry. Comparisons were made using Pearson product-moment correlation coefficients (r) as calculated in SPSS (SPSS, Chicago, IL). Significant correlation was signified by an r value of greater than 0.50.
Each photographic measurement was taken twice, once by each of two different observers. An intraclass correlation coefficient (ICC) was calculated using SPSS for each exercise to quantify the inter-rater reliability for the measurement. Significant correlation was signified by an ICC value of greater than 0.75 [20].
Results
Study participants were patients seen in an orthopedic hand surgery clinic in an academic institution over a 2-month period. There were a total of 69 patients included in our study; the age range was 18 to 63. Thirty-eight were female and 31 were male.
Validity was calculated using Pearson product-moment correlation coefficients (r) comparing the correlation of visual estimations (VE) or photograph-based goniometry (PBG) to manual goniometry (MG). The validity for both VE and PBG showed medium (r = 0.3–0.5) to strong (r = 0.5–1.0) correlations with MG measurements (Table 1). The average correlation for VE was 0.54 (range 0.33 to 0.73). The average correlation for PBG was 0.58 (range 0.28 to 0.87). The average variance for VE was 2° (range 0° to 4°) and for PBG was 2° (range 0° to 5°).
Table 1.
Validity
| Motion | T1 (MG) | T2 (VE) | T3 (PBG) | |||||
|---|---|---|---|---|---|---|---|---|
| Avg. (°) | Avg. | r | Correl. | Avg. (°) | r | Correl. | ||
| Elbow extension | R | 1 | 0 | 0.40 | Medium | 4 | 0.77 | Strong |
| L | 1 | 0 | 0.47 | Medium | 4 | 0.71 | Strong | |
| Elbow flexion | R | 131 | 128 | 0.72 | Strong | 132 | 0.54 | Strong |
| L | 132 | 129 | 0.51 | Strong | 131 | 0.67 | Strong | |
| Pronation | R | 85 | 86 | 0.54 | Strong | 82 | 0.57 | Strong |
| L | 86 | 86 | 0.57 | Strong | 84 | 0.39 | Medium | |
| Supination | R | 83 | 84 | 0.56 | Strong | 84 | 0.87 | Strong |
| L | 84 | 85 | 0.73 | Strong | 85 | 0.53 | Strong | |
| Ulnar deviation | R | 43 | 42 | 0.46 | Medium | 40 | 0.34 | Medium |
| L | 43 | 42 | 0.33 | Medium | 42 | 0.58 | Strong | |
| Radial deviation | R | 17 | 21 | 0.48 | Medium | 18 | 0.44 | Medium |
| L | 17 | 21 | 0.43 | Medium | 19 | 0.28 | Small | |
| Wrist extension | R | 54 | 58 | 0.65 | Strong | 51 | 0.67 | Strong |
| L | 54 | 57 | 0.59 | Strong | 52 | 0.68 | Strong | |
| Wrist flexion | R | 71 | 74 | 0.65 | Strong | 71 | 0.72 | Strong |
| L | 71 | 74 | 0.59 | Strong | 66 | 0.57 | Strong | |
T1 technique 1, T2 technique 2, T3 technique 3
Inter-rater reliability for PBG was assessed using ICC values across two separate observers for each joint motion. About half of the motions assessed showed excellent (ICC 0.75–1.00) correlation values, which were considered significant [20]. The remaining ranged from poor (ICC < 0.40) to good (ICC 0.60–0.74) (Table 2). The average ICC was 0.77 with the range from 0.28 to 0.96. Pronation measurements offered lowest inter-rater reliability (ICC 0.28–0.39).
Table 2.
Inter-rater reliability of PBG
| Motion | Rater 1 (°) | Rater 2 (°) | Average (°) | ICC Value | ||
|---|---|---|---|---|---|---|
| Elbow extension | R | 4 | 4 | 4 | 0.96 | Excellent |
| L | 4 | 5 | 4 | 0.95 | Excellent | |
| Elbow flexion | R | 134 | 130 | 132 | 0.83 | Excellent |
| L | 132 | 130 | 131 | 0.86 | Excellent | |
| Pronation | R | 80 | 85 | 82 | 0.39 | Poor |
| L | 83 | 84 | 84 | 0.28 | Poor | |
| Supination | R | 84 | 83 | 84 | 0.94 | Excellent |
| L | 85 | 84 | 85 | 0.69 | Good | |
| Ulnar deviation | R | 42 | 39 | 40 | 0.78 | Excellent |
| L | 43 | 40 | 42 | 0.78 | Excellent | |
| Radial deviation | R | 18 | 18 | 18 | 0.74 | Good |
| L | 21 | 17 | 19 | 0.28 | Poor | |
| Wrist extension | R | 50 | 52 | 51 | 0.96 | Excellent |
| L | 51 | 53 | 52 | 0.93 | Excellent | |
| Wrist flexion | R | 74 | 68 | 71 | 0.95 | Excellent |
| L | 71 | 61 | 66 | 0.96 | Excellent | |
Discussion
Assessment of joint ROM is an accepted evaluation of disability as well as an indicator of recovery from musculoskeletal injuries. Many goniometric techniques have been described to measure ROM, with variable utility due to inter-rater reliability. The present study focused on the validity and reliability of PBG as an emerging goniometric technique. Previous studies have shown that goniometric measurements of ±5° are clinically acceptable and do not affect conclusions drawn from the data [21]. Both visual estimation (VE) and photograph-based goniometry (PBG) show clinically acceptable measures of validity, as the average variance for VE was 2° (range 0° to 4°) and for PBG was 2° (range 0° to 5°).
Validity was assessed as described above, with strong correlations signified by r > 0.5. For VE, the motions of elbow flexion, pronation, supination, wrist extension, and wrist flexion were considered to have strong correlations with MG. For PBG, the motions of elbow extension, elbow flexion, supination, wrist extension, and wrist flexion were all considered to have strong correlations with MG. The difference between this group was that elbow extension correlated strongly with MG as measured by PBG, but not by VE; suggesting superiority of PBG for this measurement. However, pronation was strongly correlated between VE and MG but not by PBG and MG, suggesting superiority of VE for this measurement. It appears that neither method was valid when measuring ulnar or radial deviation (Table 1).
Measurements of radial and ulnar deviation using VE and PBG correlated least closely with the standard goniometric measurements. Some participants inadvertently added wrist flexion, supination, and/or shoulder abduction, which resulted in less consistent measurements. When a camera is used to make measurements, its lens must be perpendicular to the joint. If it is not held perpendicular, the resultant deviation results in a parallax effect that obscures the measurements that can be made from the picture. In this study, parallax effect could have contributed to poorer correlation, and may be more simply controlled with a camera with an accelerometer, such as a smartphone [13], or use of a simple tripod.
Inter-rater reliability was assessed as described above, with significant correlation defined as ICC > 0.75. As only a single rater assessed VE, ICC could not be assessed. For PBG, two raters measured the motions. The motions of elbow extension, elbow flexion, supination, wrist extension, and wrist flexion were thus considered significantly reliable (Table 2).
Previous studies have demonstrated a high level of inter-rater reliability when photographic methods have been employed to measure joint ROM [3, 5, 10, 14, 17, 21–24]. Yet, no study had used photograph-based goniometry to measure all eight motions of the upper extremity measured. Recently, Blonna et al. used photograph-based goniometry and have reported ICC values of 0.98 for elbow extension, and 0.96 for elbow flexion [5], which are comparable to our values of 0.96 and 0.85, respectively. To our knowledge, no study has validated the use of PBG for measurements of wrist extension and flexion, though our results show promising accuracy and inter-rater reliability (r = 0.68, ICC = 0.95 and r = 0.65, ICC = 0.96, respectively).
The advantages to utilizing a photograph-based method for goniometry over the standard manual technique are vast. Photographs allow for telemedicine, a permanent and printable report, can be taken and measured at any time, show obvious benefit in the inter- and intra-assessor settings, and can be shown to the patient to demonstrate ROM improvement over time [3, 5, 21, 22, 24]. In our study, PBG revealed ideal efficiency and optimization of both surgeon and patient time during each visit. While PBG was performed quickly during the patient visit in the exam room, the photographs had to be transferred to a computer, subsequently analyzed, and measurements made before obtaining the goniometric data. However, PBG potentially requires less in-office time as compared to the other two techniques. This saves time for both physician and patient and is thus the superior method from an optimization of care standpoint.
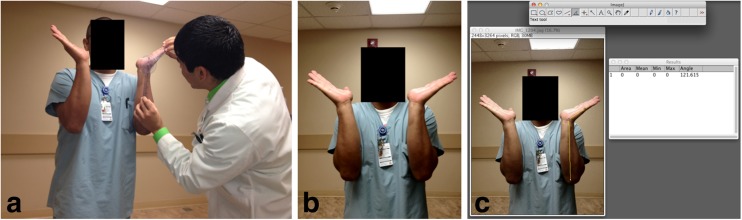
There are several limitations in this study. Goniometric and visual estimations made using MG and VE were rounded to the nearest 5° increments, whereas PBG measurements were measured to the tenth of a degree. As PBG gains favor, standardization of techniques will ensure accurate measurements. Positions should visualize the joint motion in perpendicular, as well as clearly depict bony landmarks (Fig. 3). Elbow extension and flexion photographs are taken from the side, with clear view of the acromion, lateral epicondyle, and capitate depression [8, 14]. Radial and ulnar deviation photographs are taken similarly, with clear view of the third metacarpal as well. Pronation and supination photographs are taken from the front, with the patients’ elbows at their sides and pins marking the plane of the hand, with clear view of the bicipital groove of the humerus and the antecubital fossa [2]. Wrist extension and flexion are also assessed from the front, with the forearms held perpendicular to the ground, with clear view of the olecranon, ulnar styloid, and fifth metacarpal.
Fig. 3.
Proposed enhancement of positioning and marking of bony landmarks for the each motion measurement including a elbow extension, b elbow flexion, c ulnar deviation, d radial deviation, e pronation, f supination, g wrist extension, and h wrist flexion
Our study supports photograph-based goniometry as a valid goniometric technique to improve clinical efficiency. It also allows for much better documentation of the measurements when contrasted with visual estimation. Photograph-based goniometry has the valuable benefit of incorporation into medical records to allow for the motion to be measured directly by multiple healthcare members without having to take the physical measurements themselves. The ease with which these measurements can be made and enhanced inter-rater reliability supports this technique as the new standard in goniometric measurements.
Acknowledgments
Conflict of Interest
Jared A. Crasto declares that he has no conflict of interest.
Arash J. Sayari declares that he has no conflict of interest.
Robert R-L. Gray declares that he has no conflict of interest.
Morad Askari declares that he has no conflict of interest.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5). Informed consent was obtained from all patients for being included in the study.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study. Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Contributor Information
Jared A. Crasto, Email: Jared.Crasto@osumc.edu
Arash J. Sayari, Email: ASayari@med.miami.edu
Robert R-L. Gray, Email: RGreezy@gmail.com
Morad Askari, Phone: (305) 243-4500, Email: Maskari@med.miami.edu.
References
- 1.Amadio PC, Berquist TH, Smith DK, Ilstrup DM, Cooney WP, Linscheid RL. Scaphoid malunion. J Hand Surg [Am] 1989;14A(4):679–87. doi: 10.1016/0363-5023(89)90191-3. [DOI] [PubMed] [Google Scholar]
- 2.Armstrong AD, MacDermid JC, Chinchalkar S, Stevens RS, King GJW. Reliability of range-of-motion measurement in the elbow and forearm. J Shoulder Elb Surg. 1998;7:573–80. doi: 10.1016/S1058-2746(98)90003-9. [DOI] [PubMed] [Google Scholar]
- 3.Bennett D, Hanratty B, Thompson N, Beverland D. Measurement of knee joint motion using digital imaging. Int Orthop. 2009;33(6):1627–31. doi: 10.1007/s00264-008-0694-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blonna D, Zarkadas PC, Fitzsimmons JS, O’Driscoll SW. Accuracy and inter-observer reliability of visual estimation compared to clinical goniometry of the elbow. Knee Surg Sport Traumatol Arthrosc. 2012;20(7):1378–85. doi: 10.1007/s00167-011-1720-9. [DOI] [PubMed] [Google Scholar]
- 5.Blonna D, Zarkadas PC, Fitzsimmons JS, O’Driscoll SW. Validation of a photography-based goniometry method for measuring joint range of motion. J Shoulder Elb Surg. 2012;21(1):29–35. doi: 10.1016/j.jse.2011.06.018. [DOI] [PubMed] [Google Scholar]
- 6.Boone DC, Azen SP. Normal range of motion of joints in male subjects. J Bone Joint Surg. Am. 1979;61(5):756–9. [PubMed] [Google Scholar]
- 7.Boone DC, Azen SP, Lin C-M, Spence C, Baron C, Lee L. Reliability of goniometric measurements. Phys Ther. 1978;58(11):1355–60. doi: 10.1093/ptj/58.11.1355. [DOI] [PubMed] [Google Scholar]
- 8.Carter TI, Pansy B, Wolff AL, Hillstrom HJ, Backus SI, Lenhoff M, et al. Accuracy and reliability of three different techniques for manual goniometry for wrist motion: a cadaveric study. J Hand Surg [Am] 2009;34(8):1422–8. doi: 10.1016/j.jhsa.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 9.Cleffken B, van Breukelen G, van Mameren H, Brink P, Olde Damink S. Test-retest reproducibility of elbow goniometric measurements in a rigid double-blinded protocol: intervals for distinguishing between measurement error and clinical change. J Shoulder Elb Surg. 2007;16(6):788–794.e2. doi: 10.1016/j.jse.2007.02.134. [DOI] [PubMed] [Google Scholar]
- 10.Dunlevy C, Cooney M, Gormely J. Procedural considerations for photographic-based joint angle measurements. Physiother Res Int. 2005;10(4):190–200. doi: 10.1002/pri.9. [DOI] [PubMed] [Google Scholar]
- 11.Ellis B, Bruton A, Goddard JR. Joint angle measurement: a comparative study of the reliability of goniometry and wire tracing for the hand. Clin Rehabil. 1997;11(4):314–20. doi: 10.1177/026921559701100408. [DOI] [PubMed] [Google Scholar]
- 12.Ferriero G, Sartorio F, Foti C, Primavera D, Brigatti E, Vercelli S. Reliability of a new application for smartphones (DrGoniometer) for elbow angle measurement. Phys Med Rehabil. 2011;3(12):1153–4. doi: 10.1016/j.pmrj.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 13.Ferriero G, Vercelli S, Sartorio F, Muñoz Lasa S, Ilieva E, Brigatti E, et al. Reliability of a smartphone-based goniometer for knee joint goniometry. Int J Rehabil Res. 2013;36(2):146–51. doi: 10.1097/MRR.0b013e32835b8269. [DOI] [PubMed] [Google Scholar]
- 14.Fish DR, Wingate L. Sources of goniometric error at the elbow. Phys Ther. 1985;65(11):1666–70. doi: 10.1093/ptj/65.11.1666. [DOI] [PubMed] [Google Scholar]
- 15.Fleiss JL. The design and analysis of clinical experiments. Toronto: Wiley; 1986. [Google Scholar]
- 16.Gajdosik RL, Bohannon RW. Clinical measurement of range of motion: review of goniometry emphasizing reliability and validity. Phys Ther. 1987;67(12):1867–72. doi: 10.1093/ptj/67.12.1867. [DOI] [PubMed] [Google Scholar]
- 17.Georgeu GA, Mayfield S, Logan AM. Lateral digital photography with computer-aided goniometry versus standard goniometry for recording finger joint angles. J Hand Surg [Am] 2002;27-B(2):184–6. doi: 10.1054/jhsb.2001.0692. [DOI] [PubMed] [Google Scholar]
- 18.Lenssen AF, van Dam EM, Crijns YHF, Verhey M, Geesink RJT, van den Brandt PA, et al. Reproducibility of goniometric measurement of the knee in the in-hospital phase following total knee arthroplasty. BMC Musculoskelet Disord. 2007;8:83. doi: 10.1186/1471-2474-8-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Low JL. The reliability of joint measurement. Physiotherapy. 1976;62(7):227–9. [PubMed] [Google Scholar]
- 20.Müller R, Büttner P. A critical discussion of intraclass correlation coefficients. Stat Med. 1994;13(23–24):2465–76. doi: 10.1002/sim.4780132310. [DOI] [PubMed] [Google Scholar]
- 21.Naylor JM, Ko V, Adie S, Gaskin C, Walker R, Harris IA, et al. Validity and reliability of using photography for measuring knee range of motion: a methodological study. BMC Musculoskelet Disord. 2011;12:77–86. doi: 10.1186/1471-2474-12-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Russell TG, Jull GA, Wootton R. Can the internet be used as a medium to evaluate knee angle? Man Ther. 2003;8(4):242–6. doi: 10.1016/S1356-689X(03)00016-X. [DOI] [PubMed] [Google Scholar]
- 23.Smith RP, Dias JJ, Ullah A, Bhowal B. Visual and computer software-aided estimates of Dupuytren’s contractures: correlation with clinical goniometric measurements. Ann R Coll Surg Engl. 2009;91(4):296–300. doi: 10.1308/003588409X359259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Verhaegen F, Ganseman Y, Arnout N, Vandenneucker H, Bellemans J. Are clinical photographs appropriate to determine the maximal range of motion of the knee? Acta Orthop Belg. 2010;76(6):794–8. [PubMed] [Google Scholar]