Abstract
Background.
The assessment of mobility is essential to both aging research and clinical geriatric practice. A newly developed self-report measure of mobility, the mobility assessment tool-short form (MAT-sf), uses video animations as an innovative method to improve measurement accuracy/precision. The primary aim of the current study was to evaluate whether MAT-sf scores can be used to identify risk for major mobility disability (MMD).
Methods.
This article is based on data collected from the Lifestyle Interventions and Independence for Elders study and involved 1,574 older adults between the ages of 70–89. The MAT-sf was administered at baseline; MMD, operationalized as failure to complete the 400-m walk ≤ 15 minutes, was evaluated at 6-month intervals across a period of 42 months. The outcome of interest was the first occurrence of MMD or incident MMD.
Results.
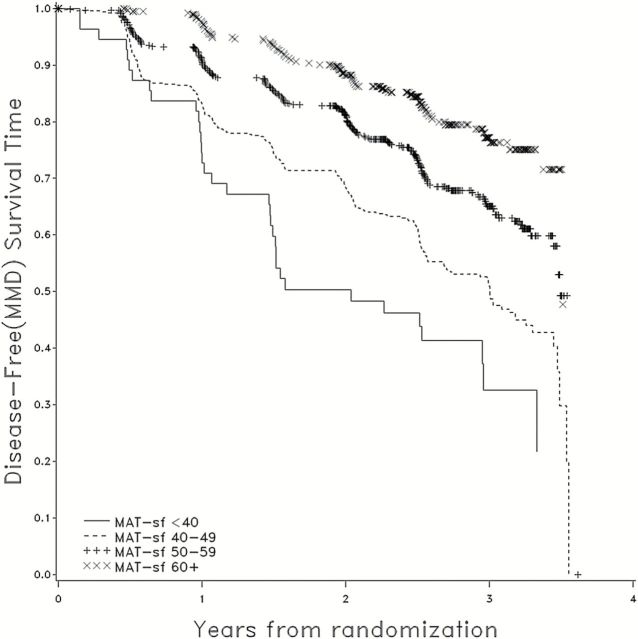
After controlling for age, sex, clinic site, and treatment arm, baseline MAT-sf scores were found to be effective in identifying risk for MMD (p < .0001). Partitioning the MAT-sf into four groups revealed that persons with scores <40, 40–49, 50–59, and 60+ had failure rates across 42 months of follow-up of 66%, 52%, 35%, and 22%, respectively.
Conclusions.
The MAT-sf is a quick and efficient way of identifying older adults at risk for MMD. It could be used to clinically identify older adults that are in need of intervention for MMD and provides a simple means for monitoring the status of patients’ mobility, an important dimension of functional health.
Key Words: MAT-sf, Mobility disability, LIFE study, Geriatric assessment, Physical function.
Mobility is central to sustaining independence in aging (1–4) as the loss of mobility threatens quality of life (5) and confers an increased risk for morbidity, institutionalization, and death (6–9). The clinical importance of mobility takes on added significance when considering the rapidly growing population of older adults in the United States (10). An appropriate means of identifying those at risk for mobility disability is central to addressing this looming public health threat (3,11,12). The current study took advantage of data collected as part of a large multicenter clinical trial of older adults to examine the ability of a novel, video-animated self-report measure of mobility, the mobility assessment tool-short form (MAT-sf) (4), to prospectively identify risk for objectively defined incident major mobility disability (MMD).
Recently, the Lifestyle Interventions and Independence for Elders (LIFE) study (13) examined the effect of a long-term structured physical activity program (PA), as compared with a successful aging education control program (SA), on preventing the loss of the ability to walk 400 m. Preserving the ability to walk 400 m is an excellent proxy for being ambulatory in the community and the loss of this capacity constitutes MMD (14). In the LIFE study, incident MMD was experienced by 30.2% of participants in the PA group and by 35.5% in the SA group, hazard ratio (HR) = 0.82; 95% CI [0.69, 0.98], p = .03. The current secondary analysis of the LIFE data examined the ability of a novel, brief, video-animated self-report measure of mobility—the MAT-sf—to identify risk for MMD across 42 months of follow-up. The primary aim of this analysis was to test the hypothesis that scores on the MAT-sf would yield a graded, increasing risk for incident MMD, allowing for the possibility of an interaction between baseline MAT-sf scores and intervention assignment. A secondary aim was to evaluate whether the effect of the MAT-sf on MMD would remain after adjustment for scores on a well-known performance-based measure of physical function, the short physical performance battery (SPPB) (15).
Methods
Participants
From February 2010 to December 2011, 14,831 participants were screened for the LIFE study at eight different field centers (see Supplementary Material for information on clinic sites); 1,635 of these potential participants were eligible and randomized to intervention, 818 to PA and 817 to SA. Details regarding screening, recruitment yields, and baseline characteristics have been published (16) as has the CONSORT diagram (13). For the purposes of this secondary analysis, data were available on 1,574 participants, with the small loss to follow-up of 3.7% due to early technical problems with computers used to deliver the MAT-sf.
The LIFE study eligibility criteria were designed to target older persons (age 70–89 years) who were: (a) sedentary (spending <20 minutes per week in the past month getting regular physical activity and reporting <125min/wk of moderate physical activity); (b) at risk for mobility disability (SPPB score of ≤9); (c) able to walk 400 m in ≤15 minutes without sitting, using a walker, or needing the help of another person; and (d) able to safely participate in the intervention. Persons with a SPPB score ≤7 were preferentially enrolled to enrich the sample with individuals at higher risk for MMD.
The study protocol was approved by the institutional review boards at all participating sites. Written informed consent was obtained from all study participants. The trial was monitored by a data and safety monitoring board appointed by the National Institute on Aging. The trial is registered at ClinicalsTrials.gov with the identifier NCT01072500.
Measures
The 400-m walk was assessed every 6 months at clinic visits. Home, telephone, and proxy assessments were attempted if the participants could not come to the clinic. Due to concerns with participant burden from the extensive testing in the LIFE study, the MAT-sf was only administered at baseline, 18 months, and 30 months. In the current analyses, we only use the baseline MAT-sf scores. The assessment staff were blinded to the intervention and remained separate from the intervention team. Participants were asked not to disclose their assigned group and not to talk about their interventions during the assessment.
Major mobility disability
The 400-m walk test served as our criterion indicator of MMD. This test is a modified version of a walking test originally developed by Newman and colleagues (9). Participants were instructed to walk at their usual pace for 400 m (10 laps of a 20-m course defined by two cones) (14). The maximum time allowed for the test was 15 minutes without sitting and without the help of another person; in successfully completing the test, participants were allowed to stop and stand to rest for up to 1 minute and could use a cane, but they were not allowed to lean against any object to support their weight. They were not allowed to use a walker or to seek help from another person. Time to complete the 400-m walk was recorded in minutes and seconds and then converted to seconds.
When MMD could not be objectively measured because of the inability of the participant to come to the clinic and absence of a suitable walking course at the participant’s home, institution, or hospital, the outcome was adjudicated based on objective inability to walk 4 m in ≤10 seconds or self-, proxy-, or medical record-reported inability to walk across a room. It would not be feasible for a participant who met any of these latter criteria to complete the 400-m walk within 15 minutes. A total of 17% of the MMD outcomes in PA and 11% in SA were determined via adjudication.
The mobility assessment tool short form
The MAT-sf is a 10-item computer-based, self-administered assessment of mobility that uses animated video clips of each task to illustrate various mobility-related challenges. Participants provide an assessment of their ability to perform each task on the computer by clicking the appropriate response (4,17). The 10 items in the MAT-sf cover a broad range of functioning. The items include walking on level ground, a slow jog, walking uphill outdoors on uneven terrain, walking up a ramp with and without using a handrail, stepping over hurdles, ascending and descending stairs with and without the use of a handrail, and climbing stairs while carrying one or two bags. The items were selected based on individual response and information curves derived from item response theory (4,17). Each item was accompanied by an animated video clip together with the responses for that question (number of minutes, number of times, yes/no). The possible range of scores is from 30 to 80. The MAT-sf has been found to have excellent test–retest reliability (intraclass correlation coefficient = .93) and validity (4,17). Also, the test items have improved accuracy/precision compared with items found on traditional self-reported disability measures because the actual task is presented visually and contextual features can be manipulated. For example, by comparing responses on MAT-sf items that pertain to the same task but within different contexts, Marsh and colleagues (17) demonstrated that differences in gait speed, terrain, as well as the presence or absence of a handrail and varying the number of steps on a flight of stairs, led to statistically significant and clinically meaningful differences in a participants’ responses to test items.
The test can be completed on any laptop computer and scores are saved to an exportable file. Also, for ease of administration, the software was designed for use on touch-screen computers and the iPad. The time required to complete the test with instructions from the examiner is ~5 minutes. Reading comprehension was designed at an 8-grade reading level and versions are available in English, Spanish, French, and Portuguese.
The short physical performance battery
The SPPB is a summary performance measure consisting of three increasingly difficult standing balance tests, usual pace walking speed over a 4-m distance, and time for five repeated chair stands performed as quickly as possible. Each performance measure is assigned a categorical score ranging from 0 (inability to complete the test) to 4 (best performance). A summary score ranging from 0 (worst performers) to 12 (best performers) was calculated by summing the three component scores. Support for the measurement properties of the SPPB has been provided by Guralnik and colleagues (15).
Intervention Groups
Because our interest in the current investigation was to evaluate whether the baseline MAT-sf score was able to assess risk for incident MMD independent of any intervention effect, we have not included a description of the two intervention groups in this article. The interested reader is referred to a prior publication on the study design for details of the LIFE study interventions (18).
Statistical Analyses
Descriptive statistics (means, standard deviations, and proportions) were used to characterize the LIFE sample. Proportional hazards models were used to examine the association between baseline MAT-sf scores and time to the initial MMD event. A continuous version of the MAT-sf was used in model fitting, but for ease of interpretation and plotting, MAT-sf scores were grouped into four categories: category 1, scores <40; category 2, scores ranging between 40 and 49; category 3, scores ranging between 50 and 59; and category 4, scores 60+. These four 10-unit categories were used because the MAT-sf is based on a T-scale with a mean of 50 and a SD of 10. The initial model in our survival analysis was adjusted for age, sex, clinical site, and intervention arm with the SPPB added as a covariate in a second model to evaluate whether inclusion of this performance test mitigated the impact of the MAT-sf on evaluation of risk for incident MMD. In addition, in a preliminary analysis, an intervention arm by MAT-sf interaction term was examined to insure that this effect was not important to interpretation of the study results. Comparisons were considered significant if p < .05. All analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC).
Results
As shown in Table 1, there was a broad range of educational backgrounds within the cohort; 67% were women and 76.7% were non-Hispanic white. The most common comorbidity was hypertension at 70.7%, followed by diabetes at 25.4%, and cancer at 22.4%. Participants varied considerably in body mass index; however, only a small percentage were either underweight (<18.5kg/m2; 0.4%) or morbidly obese (40+ kg/m2; 7.1%). The MAT-sf had a mean of 53.6 with a range of 33–76. The distribution of participants across MAT-sf categories that were used to facilitate interpretation of the data included 3.6% from 30 to 39, 33.7% from 40 to 49, 38.4% from 50 to 59, and 24.3% at 60+.
Table 1.
Participant Characteristics (N = 1,574)
| Characteristic | Mean (±SD) or N (%) |
|---|---|
| Age (y) | 78.9 (5.2) |
| Gender | |
| Male | 519 (33.0%) |
| Female | 1,055 (67.0%) |
| Race | |
| White | 1,207 (76.7%) |
| Black | 293 (18.6%) |
| Hispanic | 37 (2.4%) |
| Other | 37 (2.4%) |
| Education | |
| Less than high school | 27 (1.8%) |
| High school (any) | 472 (31.2%) |
| Any postsecondary education (excluding graduate education) | 622 (41.1%) |
| Graduate education (any) | 392 (25.9%) |
| BMI* | |
| <18.5 | 7 (0.4%) |
| 18.5–24.9 | 282 (17.9%) |
| 25–29.9 | 558 (35.4%) |
| 30–34.9 | 419 (26.6%) |
| 35–39.9 | 196 (12.4%) |
| 40+ | 112 (7.1%) |
| Self-reported comorbidities | |
| Myocardial infarction | 123 (7.8%) |
| Hypertension | 1,103 (70.7%) |
| Congestive heart failure | 68 (4.4%) |
| Arthritis | 302 (19.3%) |
| Diabetes | 398 (25.4%) |
| Cancer | 352 (22.4%) |
| Physical health status | |
| MAT-sf score | 53.6 (8.0) |
| 400-m walk (s) | 488.8 (151.7) |
| SPPB score | 7.4 (1.6) |
Notes: BMI = body mass index; MAT-sf = mobility assessment tool-short form; SPPB = short physical performance battery.
*BMI was computed as weight in kg divided by height in meters squared.
Table 2 provides the results of the survival analyses using baseline MAT-sf scores to evaluate risk for incident MMD. In a preliminary model, we examined for the possibility of a baseline MAT-sf by treatment interaction term. Because this term was not statistically significant (p = .78), it was eliminated from further consideration. Across 42 months of follow-up, there were a total of 522 persons determined to have MMD. Panel A of Table 2 presents the results without SPPB scores in the model and illustrates that the MAT-sf score was strongly related to the risk of MMD (p < .0001). As shown in Figure 1, at 24 months of follow-up, the graded rates of failure for categories 1–4 were 51%, 32%, 17%, and 10%, respectively; at 36 months, the rates were 66%, 52%, 35%, and 22%, respectively. Following this analysis, HRs were computed comparing the first three categories of the MAT-sf with category 4 (scores of 60+). These analyses illustrated that there was a graded risk moving from category 1 to category 4 (all p values < .001): HR (1 vs 4) = 4.51, 95% CI [2.94, 6.91]; HR (2 vs 4) = 2.73, 95% CI [2.12, 3.68]; and HR (3 vs 4) = 1.73, 95% CI [1.31, 2.29].
Table 2.
Survival Analyses for MAT-sf and Covariates: Free of Major Mobility Disability
| Variable | df | Panel A | Panel B |
|---|---|---|---|
| Chi-Square; p Value | Chi-Square; p Value | ||
| Without SPPB in Model | With SPPB in Model | ||
| MAT-sf | 3 | 75.87; p < .0001 | 51.64; p < .0001 |
| Clinic site | 10 | 7.92; p = .6365 | 9.28; p = .5053 |
| Age | 1 | 14.92; p = .0001 | 9.32; p = .0023 |
| Sex | 1 | 0.16; p = .6876 | 0.07; p = .7890 |
| Intervention | 1 | 3.67; p = .0553 | 3.62; p = .0568 |
| SPPB | 1 | — | 24.20; p < .0001 |
Notes: df = degrees of freedom; MAT-sf = mobility assessment tool-short form; SPPB = short physical performance battery.
Figure 1.
Mobility assessment tool-short form (MAT-sf) categories and survival without major mobility disability (MMD) by time from randomization.
Panel B of Table 2 provides the results of the model when SPPB was included as a covariate. In this model, there was a slight attenuation in the HRs for the 3 individual comparisons (all p values < .001): HR (1 vs 4) = 3.57, 95% CI [2.31, 5.52]; HR (2 vs 4) = 2.40, 95% CI [1.81, 3.19]; and HR (3 vs 4) = 1.59, 95% CI [1.20, 2.11], though all remained statistically significant. The MAT-sf and SPPB were related to one another in the expected direction, although the strength of this relationship was modest, r = .35, p < .0001. As shown in Table 2, the SPPB had an independent relationship with MMD (p < .0001).
Discussion
This secondary analysis of the LIFE study data examined whether baseline MAT-sf scores were useful in evaluating risk for incident MMD. The MAT-sf is a brief, novel, video-animated method for assessing mobility that has substantial advantages over existing self-report measures (4,17). Most important is the fact that respondents are able to visualize the tasks rather than having to make judgments about what is implied in tasks such as walking a block or climb stairs. In addition, the MAT-sf provides animated videos of complex, real-world tasks such as stepping over objects and walking on uneven paths outdoors. As shown in Figure 1, across a period of 42 months, there was a progressive increase in the risk of developing incident MMD with each 10-unit decrease in MAT-sf scores. For example, the risk of MMD after 3 years of follow-up was 22% for those with scores 60+, 35% for those with scores 50–59, 52% for those with scores 40–49, and 66% for those with scores <40.
There has been a recurring clinical research interest in whether the assessment of physical function in older adults could be used to identify risk for subsequent physical disability, but with one exception, virtually all of the evidence to date is based on self-report as opposed to objectively measured performance-based outcomes. Whereas two early studies found that decline in self-reported mobility was associated with downstream difficulty reported in both basic and instrumental activities of daily living (1,2), more recent epidemiological evidence has targeted healthy older adults and evaluated the prognostic value of objective performance-based measures of function in evaluating risk for self-reported disability. For example, a study of 1,122 older adults (mean age = 77.1 years) who had no evidence of disability completed the SPPB and then were followed for 4 years. There was an incremental, elevated risk for disability at the 4-year assessment visit associated with the SPPB; individuals having lower scores had higher risk. Furthermore, the association existed whether disability was defined as either self-reported limitations with mobility—the inability to walk ½ mile or needing help when climbing stairs—or the need for help from another person to perform one or more basic activities of daily living (12). Similarly, studying 3,075 community dwelling, well-functioning older adults aged 70–79 years across a mean follow-up of 4.9 years, investigators in the Health ABC study reported that poorer performance on the 400-m walk was associated with higher risk of both moderate and severe difficulty with self-reported mobility, again based on both walking ½ mile and climbing stairs (9). Finally, in functionally healthy older woman aged 70–79 years (N = 436), Fried and colleagues (3) examined whether the self-reported need to modify the method or frequency to perform tasks in daily life as a result of a health condition, or the time to climb a set of 14 steps, was related to the risk for perceived difficulty in walking ½ mile or climbing 10 steps at an 18-month follow-up visit. Both self-reported modification in the performance of daily tasks and slower stair climb time at the initial assessment visit were independently related to the risk for self-reported limitations with mobility.
The current findings build on this existing research in several important ways. First, the outcome of interest was a performance-based measure of incident MMD, the loss in the ability to walk 400 m (18). Preserving the ability to walk 400 m is central to maintaining a high quality of life and required for many activities to be fully independent, such as shopping and community engagement (13). To date, the only large-scale study to evaluate risk for MMD using failure to complete the 400 m as the criterion has been an observational study conducted in Italy (19). They reported that lower scores on the SPPB were associated with an increased risk for MMD 3 years later. Second, we employed a brief and psychometrically sound computerized measure of self-reported mobility to estimate the risk for developing MMD—the MAT-sf (4,17,20). Among the advantages of this measure are its brevity and increased measurement precision (17). In addition to reducing human error, the computerized format eliminates the need for extensive assessor training. In contrast to objective tests such as the SPPB, there is no need for dedicated space and concerns surrounding patient safety are eliminated. The MAT-sf can be easily used in clinic settings to assess risk and it can even be administered remotely to patients with data being electronically delivered to a central data management site. And third, the LIFE study was restricted to older adults who had evidence of some functional limitation at the time of baseline testing; that is, participants had to have an SPPB score ≤9 to be included in the study. Thus, the MAT-sf was found to be valuable in identifying older adults at risk for incident MMD despite a truncated distribution.
A secondary aim of this study was to evaluate whether the ability of the MAT-sf to identify risk for incident MMD would be diminished if a performance-based measure of physical function, the SPPB, was included as a covariate. Although the HRs for the individual MAT-sf comparisons declined after the inclusion of the SPPB, far more striking was the low covariation between the two measures and the independent information that the SPPB contributed to the risk for MMD. This is the first investigation to illustrate the independent effect that self-report and performance-based measures of function have on the identification of risk for MMD. This finding is critically important because it suggests that interventions designed to counter MMD should target patients’ perceptions of their capacities (20–23). In one longitudinal study of older adults with knee pain, we found that patients who had poor quadriceps strength combined with low confidence in their capacity to climb stairs had dramatically greater decreases in stair climbing performance across a period of 30 months than those who had equally poor strength yet remained confident in their ability to climb stairs (24). Furthermore, in a recent community-based trial involving weight loss and physical activity, we found that confidence in one’s capacity to walk was a partial mediator for the effect that the intervention had on 400-m walk time (23). It would seem that what older adults think they can do is an important determinant of maintaining independence in the community. Parenthetically, we also recognize that a host of other factors including activity history, cultural norms, lack of motivation, and negative emotions contribute to sedentary behavior in aging and to functional decline.
This study is not without limitations. First, it would have been clinically valuable to have had sequential assessments of the MAT-sf at each 6-month interval to evaluate whether short-term decline was an additional diagnostic for risk of MMD. Unfortunately, due to concerns for excessive subject burden in the LIFE trial associated with numerous planned outcome measurements, we were unable to conduct such high frequency assessments. Second, patients can and do recover from failure on the 400-m walk, thus MMD is not necessarily a persistent condition. However, MMD is similar to other medical events such as a heart attack in that failure marks a serious change in health status and places these individuals at increased risk for further decline, hospitalization, and mortality (6,8,9).
In summary, data from this investigation provide evidence that the MAT-sf is a valuable and potential cost-efficient clinical tool for use in evaluating the risk for incident MMD. The information provided by the MAT-sf relative to risk for MMD is reasonably independent of information provided by the SPPB, a well-known performance-based measure of physical function. Future research should consider using the MAT-sf as a means of triaging older persons for intervention to reduce the incidence of MMD and as a tool for monitoring the functional health of older adults within health care and in community settings such as, retirement communities, assisted living facilities, area agencies on aging, and Young Men’s Christian Association.
Supplementary Material
Supplementary material can be found at: http://biomedgerontology.oxfordjournals.org/
Funding
The Lifestyle Interventions and Independence for Elders study is funded by a National Institutes of Health/National Institute on Aging Cooperative Agreement #UO1 AG22376 and a supplement from the National Heart, Lung and Blood Institute 3U01AG022376-05A2S and sponsored in part by the Intramural Research Program, National Institute on Aging, National Institutes of Health. The research was partially supported by the Claude D. Pepper Older Americans Independence Centers at the University of Florida (1 P30 AG028740), Wake Forest University (1 P30 AG21332), Tufts University (1P30AG031679), University of Pittsburgh (P30 AG024827), and Yale University (P30AG021342) and the National Institutes of Health/National Center for Research Resources Clinical and Translational Science Awards at Stanford University (UL1 RR025744), at University of Florida (U54RR025208), and at Yale University (UL1 TR000142). Tufts University is also supported by the Boston Rehabilitation Outcomes Center (1R24HD065688-01A1). W.J.R. was supported, in part, from the following mechanisms: National Heart, Lung, and Blood Institute (R18 HL076441), National Institutes for Aging (P30 AG021332), and General Clinical Research Center (M01-RR007122); T.M.G. is the recipient of an Academic Leadership Award (K07AG043587) from the National Institutes on Aging.
Conflict of Interest
None of the authors declare any conflict of interest related to this manuscript.
Supplementary Material
References
- 1. Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919. 10.1001/jama.1963.03060120024016 [DOI] [PubMed] [Google Scholar]
- 2. Rosow I, Breslau N. A Guttman health scale for the aged. J Gerontol. 1966;21:556–559. 10.1093/geronj/21.4.556 [DOI] [PubMed] [Google Scholar]
- 3. Fried LP, Bandeen-Roche K, Chaves PH, Johnson BA. Preclinical mobility disability predicts incident mobility disability in older women. J Gerontol A Biol Sci Med Sci. 2000;55:M43–M52. [DOI] [PubMed] [Google Scholar]
- 4. Rejeski WJ, Ip EH, Marsh AP, Barnard RT. Development and validation of a video-animated tool for assessing mobility. J Gerontol A Biol Sci Med Sci. 2010;65:664–671. 10.1093/gerona/glq055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rejeski WJ, Lang W, Neiberg RH, et al. Correlates of health-related quality of life in overweight and obese adults with type 2 diabetes. Obesity. 2006;14:870–883. 10.1038/oby.2006.101 [DOI] [PubMed] [Google Scholar]
- 6. Branch LG, Jette AM. A prospective study of long-term care institutionalization among the aged. Am J Public Health. 1982;72:1373–1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Branch LG, Guralnik JM, Foley DJ, et al. Active life expectancy for 10,000 Caucasian men and women in three communities. J Gerontol. 1991;46:M145–M150. 10.1093/geronj/46.4.M145 [DOI] [PubMed] [Google Scholar]
- 8. Hirvensalo M, Rantanen T, Heikkinen E. Mobility difficulties and physical activity as predictors of mortality and loss of independence in the community-living older population. J Am Geriatr Soc. 2000;48:493–498. [DOI] [PubMed] [Google Scholar]
- 9. Newman AB, Simonsick EM, Naydeck BL, et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. JAMA. 2006;295:2018–2026. 10.1001/jama.295.17.2018 [DOI] [PubMed] [Google Scholar]
- 10. Manton KG, Vaupel JW. Survival after the age of 80 in the United States, Sweden, France, England, and Japan. N Engl J Med. 1995;333:1232–1235. 10.1056/NEJM199511023331824 [DOI] [PubMed] [Google Scholar]
- 11. Fried LP, Guralnik JM. Disability in older adults: evidence regarding significance, etiology, and risk. J Am Geriatr Soc. 1997;45:92–100. [DOI] [PubMed] [Google Scholar]
- 12. Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332:556–561. 10.1056/NEJM199503023320902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pahor M, Guralnik JM, Ambrosius WT, et al. Effect of structured physical activity on prevention of major mobility disability in older adults: the LIFE study randomized clinical trial. JAMA. 2014;311:2387–2396. 10.1001/jama.2014.5616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pahor M, Blair SN, Espeland M, et al. Effects of a physical activity intervention on measures of physical performance: results of the Lifestyle Interventions and Independence for Elders Pilot (LIFE-P) study. J Gerontol A Biol Sci Med Sci. 2006;61:1157–1165. [DOI] [PubMed] [Google Scholar]
- 15. Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. 10.1093/geronj/49.2.M85 [DOI] [PubMed] [Google Scholar]
- 16. Marsh AP, Lovato LC, Glynn NW, et al. Lifestyle Interventions and Independence for Elders study: recruitment and baseline characteristics. J Gerontol A Biol Sci Med Sci. 2013;68:1549–1558. 10.1093/gerona/glt064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Marsh AP, Ip EH, Barnard RT, Wong YL, Rejeski WJ. Using video animation to assess mobility in older adults. J Gerontol A Biol Sci Med Sci. 2011;66:217–227. 10.1093/gerona/glq209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fielding RA, Rejeski WJ, Blair S, et al. The Lifestyle Interventions and Independence for Elders study: design and methods. J Gerontol A Biol Sci Med Sci. 2011;66:1226–1237. 10.1093/gerona/glr123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Vasunilashorn S, Coppin AK, Patel KV, et al. Use of the Short Physical Performance Battery Score to predict loss of ability to walk 400 meters: analysis from the InCHIANTI study. J Gerontol A Biol Sci Med Sci. 2009;64:223–229. 10.1093/gerona/gln022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rejeski WJ, Marsh AP, Anton S, et al. ; LIFE Research Group. The MAT-sf: clinical relevance and validity. J Gerontol A Biol Sci Med Sci. 2013;68:1567–1574. 10.1093/gerona/glt068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rejeski WJ, Ettinger WH, Jr, Martin K, Morgan T. Treating disability in knee osteoarthritis with exercise therapy: a central role for self-efficacy and pain. Arthritis Care Res. 1998;11:94–101. 10.1002/art.1790110205 [DOI] [PubMed] [Google Scholar]
- 22. Rejeski WJ, Brawley LR, Ambrosius WT, et al. Older adults with chronic disease: benefits of group-mediated counseling in the promotion of physically active lifestyles. Health Psychol. 2003;22:414–423. 10.1037/0278-6133.22.4.414 [DOI] [PubMed] [Google Scholar]
- 23. Brawley L, Rejeski WJ, Gaukstern JE, Ambrosius WT. Social cognitive changes following weight loss and physical activity interventions in obese, older adults in poor cardiovascular health. Ann Behav Med. 2012;44:353–364. 10.1007/s12160-012-9390-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rejeski WJ, Miller ME, Foy C, Messier S, Rapp S. Self-efficacy and the progression of functional limitations and self-reported disability in older adults with knee pain. J Gerontol B Psychol Sci Soc Sci. 2001;56:S261–S265. 10.1093/geronb/56.5.S261 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.