Abstract
INTRODUCTION
Despite available, effective therapies, racial and ethnic disparities in care and outcomes of hypertension persist. Several interventions have been tested to reduce disparities; however, their translation into practice and policy is hampered by knowledge gaps and limited collaboration among stakeholders.
METHODS
We characterized factors influencing disparities in blood pressure (BP) control by levels of an ecological model. We then conducted a literature search using PubMed, Scopus, and CINAHL databases to identify interventions targeted toward reducing disparities in BP control, categorized them by the levels of the model at which they were primarily targeted, and summarized the evidence regarding their effectiveness.
RESULTS
We identified 39 interventions and several state and national policy initiatives targeted toward reducing racial and ethnic disparities in BP control, 5 of which are ongoing. Most had patient populations that were majority African-American. Of completed interventions, 27 demonstrated some improvement in BP control or related process measures, and 7 did not; of the 6 studies examining disparities, 3 reduced, 2 increased, and 1 had no effect on disparities.
CONCLUSIONS
Several effective interventions exist to improve BP in racial and ethnic minorities; however, evidence that they reduce disparities is limited, and many groups are understudied. To strengthen the evidence and translate it into practice and policy, we recommend rigorous evaluation of pragmatic, sustainable, multilevel interventions; institutional support for training implementation researchers and creating broad partnerships among payers, patients, providers, researchers, policymakers, and community-based organizations; and balance and alignment in the priorities and incentives of each stakeholder group.
Keywords: blood pressure, disparities, hypertension, interventions, prevention, policy, racial inequities, research translation.
DISPARITIES IN HYPERTENSION CONTROL AND PREVENTION
Despite the availability of effective therapy, hypertension remains a significant cause of morbidity and mortality in the United States and a major contributor to cardiovascular disease (CVD), stroke, and chronic kidney disease.1 Recent estimates from the National Health and Nutrition Examination Survey (NHANES) data suggest that the prevalence of hypertension in African-Americans remains significantly higher than in white or Mexican-American adults.2,3 Racial disparities in hypertension prevalence have persisted over time.2,4 Similarly, racial disparities in BP control persist despite longstanding awareness and the development of targeted initiatives to reduce disparities.2,5–7 Available evidence indicates that, compared with whites, African-Americans receiving adequate treatment should achieve similar declines in overall BP and experience lower rates of hypertension-related morbidity and mortality.8,9 However, despite improvements in awareness and treatment in the general population, hypertension continues to be poorly diagnosed, treated, and controlled among African-Americans and Hispanics, who suffer disproportionately from hypertension-related morbidity and mortality.1,2 Furthermore, NHANES data from 2003 to 2010 suggests that blood pressure (BP) control was achieved in fewer African-Americans (62%) when compared with Mexican-Americans (74%) and Caucasians (75%) even though awareness of hypertension was not significantly different between Caucasians and African-Americans.2 A study conducted in a Medicaid population in North Carolina from 2005–2006 showed that African-Americans with high BP were more likely to have four or more antihypertensives prescribed and more likely to have received provider responses to hypertension and medication adjustments; however, they were less likely to have attained goal BP.6 Disparities are also apparent in preventable hospitalizations for hypertension, where the gap in admission rates for hypertension widened between African-American and Caucasian patients from 2004 to 2009.10
MULTILEVEL BARRIERS TO REDUCING DISPARITIES IN BLOOD PRESSURE CONTROL
Barriers to reducing disparities in BP control are complex and include factors related to individual patients; family and social support systems; health care providers; organization and practice settings in which health care occurs; the local community environment; and local, state, and national health policy environments. If interventions to reduce disparities are to be successfully designed, targeted, and implemented, it is critical to understand these multifactorial barriers. In this article, we review known barriers to reducing racial disparities in hypertension prevention and control. We present a modified version of the ecological model based on Bronfenbrenner’s work11,12 to describe these barriers, which shows the different levels at which health disparities can be understood (Figure 1). Finally, we highlight innovative interventions to overcome these barriers and present recommendations for translating research findings into practice and policy.
Figure 1.
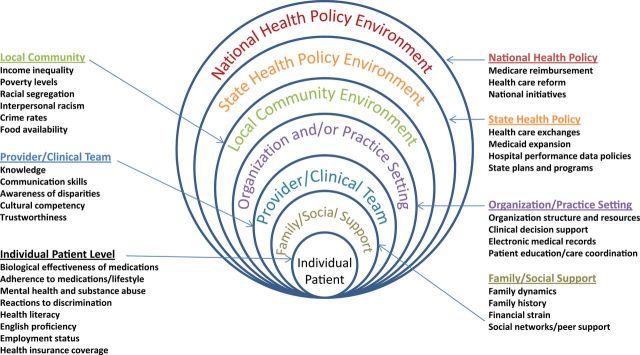
Multilevel influences on disparities in hypertension prevention and control.
Individual patient level barriers
Factors affecting BP control at the individual level include genetic (e.g., differences in biological responses to treatment), behavioral (e.g., medication adherence and lifestyle factors), cognitive and affective (e.g., knowledge, abilities, and attitudes), and sociodemographic (e.g., socioeconomic status and language proficiency) influences.
Genetic factors.
Racial differences in intrinsic biological factors account for only a small amount of observed disparities. Indeed, within racial groups, wide variations in drug-associated changes in BP have been observed, suggesting that many blacks and whites have similar responses to specific drugs.13
Behavioral factors.
Patient behaviors are believed to contribute significantly to hypertension disparities. Recent studies have demonstrated that adherence is lower in African-American patients than whites,14–16 and differences in medication adherence are associated with BP control disparities.15,17 Other behavioral and lifestyle factors (e.g., poor adherence to recommendations about weight management and low-salt diet, heavy drinking and alcoholism, smoking, and use of illicit drugs) may also contribute to disparities in BP control.18–20
Cognitive and affective factors.
Patient behaviors and acceptance of medical advice may be influenced by emotional reactions to the environment, cognitive styles and abilities, and beliefs about individual health. A recent study found that being “labeled” as hypertensive was associated with poorer mental health and greater depressive symptoms among African-Americans.21 Studies of race consciousness show that African-Americans are more likely than whites to think about race, and those who do are more likely to have elevated BP than their white counterparts.22 Studies of health literacy, another cognitive factor, demonstrate that patients with lower literacy levels are less likely to engage in participatory decision-making with their providers and have worse BP control than those with higher literacy levels.23
Sociodemographic factors.
Language proficiency may also present a barrier to hypertension control. In 2000, 18% of the total US population reported that they spoke a language other than English at home,24 and lack of English proficiency has been cited as a barrier to hypertension control in Korean-Americans.25 Socioeconomic barriers (e.g., unemployment and lack of health insurance) have been shown to be associated with inadequate BP care and control among young African-American men with hypertension.18 A recent study using national data reported a higher prevalence of no health insurance and poorer access to care among Hispanics and low-income persons with hypertension.26
Family/social support level barriers
Family-level factors such as marital status, living arrangements, family dynamics, social support for care, and financial strain impact BP through their influences on stress and adherence to medications.27 More expensive medications such as calcium channel blockers may result in increased financial strain on families when compared to cheaper, antihypertensives.28 Additionally, a study reported that many hypertension patients attributed their hypertension to family history and suggested that there was a relationship between this attribution and medication-taking behavior.29 Findings from the same study also showed that a large percentage of patients rated stress at home as a cause of their hypertension.29
Health system and provider level barriers
Racial minorities may also encounter barriers to optimal BP care and control at the health system, provider, and organizational team levels. Barriers include lower quality of care, poorer provider-patient communication, and lower levels of trust in health professionals.27,30–32
Lower quality of care.
Healthcare settings where many racial minorities receive care have fewer resources and less access to specialists and newer technologies, which may be associated with poorer outcomes.30 One study of African-Americans with uncontrolled hypertension found that a majority of patients were not receiving diuretics, despite widely publicized recommendations for their use.33
Communication barriers.
Disparities also exist in the quality of patient–provider communication. Physicians tend to be more verbally dominant and less likely to engage in participatory decision making with African-American patients.34 African-Americans with uncontrolled BP have shorter visits containing fewer biomedical, psychosocial, and rapport-building statements when compared with whites with controlled BP.31
Lower levels of trustworthiness.
Studies of hypertensive African-Americans suggest that distrust of health care professionals may pose a significant barrier to medication adherence,27 and higher levels of perceived discrimination in the health care system have been reported in African-American patients.32 Increased participatory decision making and rapport building may improve patient trust in physicians, which may mitigate concerns about BP medications and increase uptake of lifestyle changes.35,36
Local community environment level barriers
Many community and local environmental factors, such as neighborhood poverty, crime rates, proportion of families living in poverty, availability of healthy foods, residential segregation, and racial isolation contribute to disparities in BP control.27,37,38 These social determinants of health play a significant role in racial disparities in BP. To illustrate, Kingsbury et al.39 present a conceptual model in which social and environmental factors such as psychosocial stressors, occupational stressors, and environmental stressors may affect sleep quality in a way that would disproportionately affect BP control in African-Americans. Additionally, neighborhood violence has been implicated as a key contextual factor negatively associated with BP medication adherence due to the impact of increased stress on patients.27 Finally, perceived interpersonal racism has been shown to correlate with increased ambulatory BP measures.37
Local, state, and national policy environments level barriers
Pay-for-performance models have been theorized to carry risks of worsening health disparities. Karve et al.40 demonstrated that the percentage of African-American patients served by hospitals is inversely related to performance measures for MI and pneumonia, raising concern that pay-for-performance may place hospitals that serve large minority populations at financial risk. Major pay-for-performance programs in the UK41 have had no effects on racial disparities in hypertension management. Models of effects of pay-for-performance programs in the United States have not shown increases in disparities.42 Nevertheless, the risk remains, and experts suggest these programs should consider both overall quality and disparities. Additionally, policy initiatives and wide social programs to improve health may result in worsening of health inequities through a “staircase effect” in which wide-based interventions to improve health may be less likely to be taken up by those with lower socioeconomic status.43,44 As a result, health inequities may increase by socioeconomic status, and these inequities may translate to increases in racial disparities. With population-wide initiatives such as Healthy People 2020 in place, the risk remains that disparities in BP control may be paradoxically increased.
INTERVENTIONS TO REDUCE DISPARITIES IN HYPERTENSION CARE AND CONTROL
Interventions developed to improve management of hypertension in racial minorities are numerous. We provide our detailed search strategy for identifying effective interventions in Supplementary Table S1. When possible, we categorized identified interventions by the level of Bronfenbrenner’s Ecological Model at which they were primarily targeted. Overall, we identified and reviewed 39 interventions in the literature as well as several state and national policy initiatives targeted toward reducing racial disparities in BP control, 5 of which are ongoing. Most (51.5%) completed and reviewed interventions had patient populations that were majority African-American. Of completed interventions, 27 demonstrated some improvement in BP control or in related process measures, and 7 did not; 23 studies improved BP levels or control rates, 4 improved lifestyle behaviors, 3 improved medication adherence, 2 improved knowledge, and 1 improved participatory decision-making. Of the six studies for which effects on disparities are available, three reduced, two increased, and one had no effect on disparities. We describe these interventions, targeted at multiple levels, and their effects, below and within Tables 1, 2.
Table 1.
Intervention study characteristics
| Study | Intervention type | Location | Setting | Sample size | Patient population |
|---|---|---|---|---|---|
| Individual patient interventions | |||||
| Bosworth et al. 45 | Home BP monitoring; Behavioral intervention | North Carolina | Home environment | 636 | Minority groups: 49% AA |
| Mean age: 61 years | |||||
| Sex: 66% female | |||||
| Income: 19% “inadequate” | |||||
| Ogedegbe et al. 46 | Patient Education; motivational Interviewing | New York City | Clinic | 256 | Minority groups: 100% AA |
| Mean age: 58 years | |||||
| Sex: 79% female | |||||
| Income: NR | |||||
| Schneider et al. 47 | Stress reduction; behavioral intervention | Milwaukee, WI | Group education | 201 | Minority groups: 100% AA |
| Mean age: 59 years | |||||
| Sex: 42% female | |||||
| Income: 50% <$10,000/year | |||||
| Rigsby et al. 48 | Patient education; behavioral intervention | Alabama | Church | 36 | Minority groups: 100% AA |
| Age: NR | |||||
| Sex: 80.6% female | |||||
| Income: NR | |||||
| Jackson et al. 49 | Medication management; behavioral intervention | Durham, NC | Telemedicine | 573 | Minority groups: 49.5% AA |
| Mean age: 63.5 years | |||||
| Sex: 8.2% female | |||||
| Income: 18.2% “inadequate income” | |||||
| Migneault et al. 50 | Behavioral intervention; patient education | Urban US | Telemedicine | 337 | Minority groups: 100% AA |
| Mean age: 56.3 years | |||||
| Sex: 70% female | |||||
| Income: median household income $10–20,000/year (range) | |||||
| Giuse et al. 51 | Patient education | Nashville, TN | Emergency room | 196 | Minority groups: 33.6% nonwhite |
| Mean age: 50.5 years (intervention group 1) | |||||
| Sex: 55% female | |||||
| Income: NR | |||||
| Family/social support interventions | |||||
| Houston et al. 52 | Culturally appropriate storytelling intervention | Southern United States | Community | 299 | Minority groups: 100% AA |
| Mean age: 53.7 years | |||||
| Sex: 71.4% female | |||||
| Income: 61.8% household <$12,000/year | |||||
| Rocha-Goldberg et al. 53 | Group education sessions | Durham, NC | Community | 17 | Minority groups: 100% Hispanic |
| Mean age: 46 | |||||
| Sex: 59% female | |||||
| Income: NR | |||||
| Rodriguez et al. 54 | Group education sessions | Boston, MA | Community | 34 | Minority groups: 100% AA |
| Mean age: 48 years | |||||
| Sex: 100% female | |||||
| Income: NR | |||||
| Shaya et al. 55 | Group education; social networks | Baltimore, MD | Community | 441 | Minority groups: 100% AA |
| Mean age: 48 years (intervention group) | |||||
| Sex: 41.3% female | |||||
| Income: NR | |||||
| Turner et al. 56 | Peer support; patient education | Nationwide | Telephone | 280 | Minority groups: 100% AA |
| Mean age: 61.9 years | |||||
| Sex: 65% female | |||||
| Income: NR | |||||
| Provider/team interventions | |||||
| Thom et al. 57 | Physician education; cultural competency training | Northern California | Clinic | 429 patients | Minority groups: 23.2% AA, 25.3% |
| Hispanic, 13.1% Asian (intervention group) | |||||
| Mean age: 54.9 years (intervention group) | |||||
| Sex: 49% female (intervention group) | |||||
| Income: NR | |||||
| Organization/practice interventions | |||||
| Hicks et al. 58 | Electronic medical records (EMRs) | Urban population | Clinic (EMR) | 2,027 | Minority groups: 33% AA |
| Median age: 64 years (intervention group 1) | |||||
| Sex: 66.1% female | |||||
| Income: NR | |||||
| Hebert et al. 59 | Clinical support model | Southern United States | Clinic | 898 | Minority groups: 36.3% AA, 21.6% Hispanic |
| Mean age: 57 years | |||||
| Sex: 35.6% female | |||||
| Income: NR | |||||
| Samal et al. 60 | EMRs | Nationwide | Clinic (EMR) | 17,016 | Minority groups: 14% AA, 15% Hispanics |
| Mean age: 51 years | |||||
| Sex: 67% female | |||||
| Income: NR | |||||
| Song et al. 61 | New clinic model | Boston, MA | Mobile clinic (delivery design) | 5,900 | Minority groups: 68.3% AA, 13.9% Hispanic (returners) |
| Mean age: 56.8 years (returners) | |||||
| Sex: 51% female (returners) | |||||
| Income: NR | |||||
| Local community environment interventions | |||||
| Ravenell et al. 62 | Increased screening; Motivational Interviewing; Patient Navigation | New York City | Community (barbershops) | Ongoing 480 planned | Minority groups: 100% AA |
| Age: Ongoing | |||||
| Sex: 100% male | |||||
| Income: Ongoing | |||||
| Zoellner et al. 63 | Community-based participatory research (CBPR), Multicomponent Lifestyle Intervention | Southern Mississippi | Community | 269 | Minority groups: 94% AA |
| Mean age: 44.3 years | |||||
| Sex: 85% female | |||||
| Income: 28.3% household income< $20,000/year | |||||
| Troyer et al. 64 | Home delivered Dietary Approaches to Stop Hypertension (DASH) diet meals | Not reported | Community | 210 | Minority groups: 39% nonwhite |
| Age: 100% >60 years | |||||
| Sex: 82.9% female | |||||
| Income: 43% < 165% of poverty line | |||||
| National health policy interventions | |||||
| Hicks et al. 65 | Organizational change; quality improvement | Nationwide | Nationwide database review (community health centers) | 10,153 | Minority groups: 13% AA |
| Mean Age: 56 | |||||
| Sex: 56% female | |||||
| Income: NR | |||||
| Landon et al. 66 | Organizational change; quality improvement | Nationwide | Nationwide database review (community health centers) | 9,658 (3,362 with HTN) | Minority groups: 13.2% AA, 23% Hispanic (HTN intervention) |
| Mean age: 56.1 years (HTN intervention) | |||||
| Sex: 56.2% female (HTN intervention) | |||||
| Income: NR | |||||
| Multilevel: individual patient and provider/team setting interventions | |||||
| Johnson et al. 67 | Patient education; provider education | Baltimore, MD | Clinic | 552 | Minority groups: 91.3% AA |
| Mean age: 55 years (intervention group 1) | |||||
| Sex: 65.3% female | |||||
| Income: NR | |||||
| Pezzin et al. 68 | Telemedicine; home BP monitoring; patient education | Urban US area | Telemedicine | 845 | Minority groups: 100% AA |
| Mean age: 64.3 years | |||||
| Sex: 66% female | |||||
| Income: NR | |||||
| Bove et al. 69 | Nurse management system; telemedicine | Urban and rural sites | Telemedicine/clinic | 388 | Minority groups: 1% AA (rural); 76.5% AA (urban) |
| Mean age: 62.5 years (rural); 57.9 years (urban) | |||||
| Sex: 44.4% female (rural), 47.5% (urban) | |||||
| Income: 43% < $25,000/year | |||||
| Han et al. 25 | Nurse management system; telemedicine | Baltimore, MD | Telemedicine | 360 | Minority groups: 100% Asian (Korean-American) |
| Mean age: 51.9 years | |||||
| Sex: 53% female | |||||
| Income: NR | |||||
| Multilevel: individual patient and local community environment interventions | |||||
| Cene et al. 70 | Community-based nurse practitioner/ community health worker team care; enhanced clinical care | Baltimore, MD | Community/clinic | 363 | Minority groups: 100% AA |
| Mean age: 47.8 years | |||||
| Sex: 63% female | |||||
| Income: NR | |||||
| Balcazar et al. 71 | Family-centered and CBPR/community feasibility program; patient education | El Paso, TX | Community | 98 | Minority groups: 100% Hispanic (Mexican-Americans) |
| Mean age: 54.9 years (intervention group) | |||||
| Sex: 78.5% female | |||||
| Income: 79% household income< $15,000/year | |||||
| Zarate-Abbott et al. 72 | Health education; workplace intervention | South Texas | Workplace | 21 | Minority groups: 100% Hispanic (Mexican-American) |
| Mean age: 50 | |||||
| Sex: 100% female | |||||
| Income: NR | |||||
| Kim et al. 73 | Multimodal self-help program; patient education | Baltimore-Washington metro area | Community | 440 | Minority groups: 100% Asian (Korean-American) |
| Mean age: 70.9 years | |||||
| Sex: 72.4% female | |||||
| Income: NR | |||||
| Multilevel: family/social support and local community environment interventions | |||||
| Victor et al. 74 | Community involvement; patient education; peer-based health messaging | Dallas, TX | Community (barbershops) | 1,297 | Minority groups: 100% AA |
| Mean age: 49.5 years (intervention group) | |||||
| Sex: 100% male | |||||
| Income: 14.3% < 100% of poverty level | |||||
| Multilevel: individual patient and organization/practice setting interventions | |||||
| Glasgow et al. 75 | Patient HTN self- management education; weight loss intervention | Boston, MA | Community Health Center | 365 | Minority groups: 71.2% AA, 13.1% Hispanic |
| Mean age: 54.6 years | |||||
| Sex: 71% female | |||||
| Income: 54.5% <$25,000/year | |||||
| Multilevel: provider/team and organization/practice setting interventions | |||||
| Cooper et al. 76 | Physician communication skills training; patient activation | Baltimore, MD | Clinic | 279 | Minority groups: 62% AA |
| Mean age: 59.7 years (intervention group 1) | |||||
| Sex: 65.9% female | |||||
| Income: 68% < $35,000/year | |||||
| Kim et al. 77 | Home BP monitoring; telemedicine | Baltimore, MD | Telemedicine | 359 | Minority groups: 100% Korean-American |
| Age: 52 | |||||
| Sex: 53% female | |||||
| Income: NR | |||||
| Ogedegbe et al. 78 | Patient education; motivational interviewing; Home BP monitoring; lifestyle counseling; physician feedback; monthly hypertension case rounds | New York City | Community Health Center | 1,059 | Minority groups: 100% AA |
| Mean age: 56.5 years | |||||
| Sex: 71.6% female | |||||
| Income: 72.4% household income< $20,000/year | |||||
| Cooper et al. 79 | Improved BP measurement; organizational change (care management staff added); audit/ feedback and communication skills training for physicians | Baltimore, MD | Clinic/system | ~45,000 (~16,000 with HTN) | Minority groups: 42% AA, 2% Hispanic, 2% Asian, 3% multiracial |
| Mean age: 48 years | |||||
| Sex: 62% female | |||||
| Multilevel: organization/practice setting and local community environment interventions | |||||
| Halladay et al. 80 | Community health coach; home BP monitoring; patient education; phone coaching; practice- level HTN care quality improvement | North Carolina | Clinic/community | Ongoing | Ongoing |
| Multilevel: individual, family/social support, and local community environment interventions | |||||
| Ephraim et al. 81 | Community health workers; patient self- management and communication skills training; home BP monitoring | Baltimore, MD | Clinic/community | Ongoing | Ongoing |
| Cooper (Miller) et al. 82 | Dietary advice; facilitated access to healthy foods | Baltimore, MD | Clinic/community | Ongoing | Ongoing |
Abbreviations: AA, African-American; BP, blood pressure; HTN, hypertension; NR, not reported.
Table 2.
Intervention study results
| Study | Design | Primary outcomes | Improvement in blood pressure control or related outcomes? |
|---|---|---|---|
| Individual patient interventions | |||
| Bosworth et al. 45 | Randomized controlled trial | Systolic blood pressure | Yes: Significant decreases in BP in nonwhite patients at 24 months after receiving a combined self-management/ home BP monitoring intervention |
| Ogedegbe et al. 46 | Randomized controlled trial | Medication adherence | Yes: Positive-affect induction leads to significantly improved medication adherence at 12 months in AA patients with HTN |
| Schneider et al. 47 | Randomized controlled trial | Time to first event: mortality, MI, or stroke | Yes: Significant decrease of 4.9mm Hg in systolic blood pressure in patients randomized to receive transcendental meditation |
| Rigsby et al. 48 | Prepost study | Increased knowledge of hypertension, risk factors | Yes: 96% of participants who submitted daily BP logs reductions in blood pressure |
| Jackson et al. 49 | Randomized controlled trial | Mean systolic, diastolic blood pressure | Yes: Decreased systolic blood pressure at 18 months postintervention after receiving a combined medication management/behavioral intervention |
| Reduced disparities: Decreased systolic and diastolic blood pressure in African-Americans compared to whites | |||
| Migneault et al. 50 | Randomized controlled trial | Changes in physical activity, diet index score | No: No statistically significant reduction in systolic or diastolic BP among patients who received culturally tailored behavior intervention (vs. education-only controls) |
| Giuse et al. 51 | Sequential randomized trial | Improvements in hypertension knowledge | Yes: Significant increases in hypertension knowledge after receiving emergency room discharge instructions tailored to health literacy |
| Family/social support interventions | |||
| Houston et al. 52 | Randomized controlled trial | Change in blood pressure | Yes: A storytelling intervention produced improved blood pressure control at 3 months in a population of AA patients with HTN |
| Rocha-Goldberg et al. 53 | Prepost study | Systolic BP, dietary changes, BMI | Yes: A culturally adapted group behavioral intervention resulted in significant improvements in systolic blood pressure in Hispanic/Latino adults |
| Rodriguez et al. 54 | Prepost study | Blood pressure, body weight, BMI, waist circumference | Yes: A 12-week nutrition and physical activity intervention produced a 38% relative reduction in hypertension prevalence in AA women |
| Shaya et al. 55 | Nonrandomized study | Blood pressure | Yes: A hypertension education program focused on clustering in social networks resulted in improved systolic and diastolic BPs at 18 months |
| Turner et al. 56 | Randomized controlled trial | Coronary heart disease risk; systolic BP | Yes: A peer patient behavioral support system resulted in significant reductions in systolic blood pressure |
| Provider/team interventions | |||
| Thom et al. 57 | Nonrandomized study | Patient reported physician cultural competency | No: No statistically significant changes in systolic BP in patients after physicians were randomized to a cultural competence curriculum |
| Organization/practice interventions | |||
| Hicks et al. 58 | Randomized study | Blood pressure | Yes: Clinical decision support improves HTN outcomes across all ethnicities |
| Hebert et al. 59 | Pre-post study | Blood pressure | Yes: Patients enrolled in heart failure disease management programs had reductions in BP |
| Reduced disparities: Reduction of racial disparities in control | |||
| Samal et al. 60 | Observational study | Blood pressure control | No: Increased disparities in BP control in African-Americans in clinics that did not use EMRs |
| Song et al. 61 | Longitudinal prepost study | Blood pressure control | Yes: Average reduction of 10.7mm Hg in SBP, 6.2mm Hg in DBP in patients returning to a mobile health clinic |
| Local community environment interventions | |||
| Ravenell et al. 62 | Randomized controlled trial | Blood pressure control; medication adherence | Ongoing |
| Zoellner et al. 63 | Pre-post study | Blood pressure | Yes: Statistically significant decreases in systolic and diastolic BP at 6 months; sugar intake after enrolling patients in a community-based blood pressure management program |
| Troyer et al. 64 | Randomized controlled trial | Dietary adherence to Dietary Approaches to Stop Hypertension (DASH) guidelines | Yes: Elderly patients receiving DASH-adherent meals were more likely to become DASH adherent in their overall diets |
| Impact on disparities: Improvements in DASH adherence were marginally larger in whites and patients with higher income | |||
| National health policy interventions | |||
| Hicks et al. 65 | Observational study | Disparity scores on quality of care indicators | Impact on disparities: Health disparities collaboratives at community health centers do not reduce disparities in hypertension care or outcomes |
| Landon et al. 66 | Nonrandomized control study | Improvements in quality of care indicators and outcomes | No: No improvement in processes of care or clinical outcomes for hypertension in community health centers participating in quality improvement collaboratives |
| Multilevel: individual patient and provider/team setting interventions | |||
| Johnson et al. 67 | Randomized controlled trial | Blood pressure control | Yes: Statistically significantly better improvements in BP control over 6 months for patients in the intervention group (patient and provider education) vs. usual care group |
| Pezzin et al. 68 | Randomized controlled trial | Blood pressure control | Yes: A combination of home monitoring and a nurse-led medication management intervention improved BP control in AA patients with stage 2 hypertension |
| Bove et al. 69 | Randomized controlled trial | Weight, BP, physical activity | Yes: A nurse management system resulted in improvements in BP control in urban and rural populations. Telemedicine did not improve outcomes. |
| Han et al. 25 | Randomized controlled trial | Medication adherence; smoking cessation; alcohol consumption; exercise | Yes: A bilingual nurse telephone counseling program in Korean-Americans resulted in improvements in medication adherence, alcohol consumption, and exercise, with frequency of counseling related to intervention effect |
| Multilevel: individual patient and local community environment interventions | |||
| Cene et al. 70 | Randomized controlled trial | Low density lipoprotein levels, smoking cessation, blood pressure | No: No significant differences in BP control between high-risk AA patients who received a community-based intervention vs. those who received enhanced clinical care |
| Balcazar et al. 71 | Randomized controlled trial | BP, waist circumference, BMI, attitudes toward BP, BP self-management behaviors | Yes: A family and community intervention using NHLBI educational modules resulted in improvements in dietary behavioral outcomes and perceived benefits of healthy behaviors in Hispanic/Latino patients |
| Zarate-Abbott et al. 72 | Prepost study | Blood pressure control, BP self-management behavioral change | Yes: A workplace educational intervention among Hispanic housekeepers yielded significant improvements in systolic and diastolic BPs 17 months post-intervention |
| Kim et al. 73 | Randomized controlled trial | Blood pressure control | Yes: Significant changes in blood pressure control over 12 months; attenuated at 18 months |
| Multilevel: family/social support and local community environment interventions | |||
| Victor et al. 74 | Randomized controlled trial | Blood pressure control rates | Yes: AA barbershops in which barbers were enabled to act as health educators/BP screeners had higher blood pressure control rates in hypertensive patients |
| Multilevel: individual patient and organization/practice setting interventions | |||
| Glasgow et al. 75 | Randomized controlled trial | Weight, blood pressure | Yes: Statistically significant improvements in BP control over 24 months for patients enrolled in a blood pressure self- management intervention using the RE-AIM framework |
| Multilevel: individual patient, provider/team and organization/practice setting interventions | |||
| Cooper et al. 76 | Randomized controlled trial | Blood pressure control; patient and physician participatory decision making (PDM); physician communication skill changes | Yes: Significant changes in patient involvement in care/ participatory decision-making; significant reductions in BP among patients with uncontrolled BP |
| Impact on disparities: Improvements in patient communication and PDM larger in blacks than whites but smaller in persons with low vs. adequate health literacy (personal communication) | |||
| Kim et al. 77 | Randomized controlled trial | Blood pressure control | Yes: A 6-week behavioral education program followed by blood pressure telemonitoring and bilingual nurse telephone counseling was effective in improving BP control in a Korean-American immigrant population |
| Ogedegbe et al. 78 | Cluster- randomized clinical trial | Blood pressure control | No: No statistically significant difference in BP control for patients randomized to a practice-based multicomponent educational intervention (vs. usual care) |
| Multilevel: organization/practice setting and local community environment interventions | |||
| Halladay et al. 80 | Nonrandomized observational trial | Blood pressure change | Ongoing |
| Disparity in blood pressure change | |||
| Multilevel: individual, family/social support, and local community environment interventions | |||
| Ephraim et al. 81 | Randomized controlled trial | Blood pressure control | Ongoing |
| Cooper (Miller) et al. 82 | Randomized controlled trial | Blood pressure control | Ongoing |
Abbreviations: BP, blood pressure; BMI, body mass index; HTN, hypertension; LDL, low density lipoprotein.
Individual patient interventions
Interventions targeting individual patient level barriers (e.g., socioeconomic and lifestyle issues) include patient self-management education, counseling, and motivational strategies (Tables 1, 2).
Patient self-management education strategies.
Bosworth et al.45 used home BP monitoring and self-management techniques via telephone, and found that non-white patients had sustained decreases in systolic BP lasting 24 months after the intervention. Glasgow et al. 75 demonstrated statistically significant improvements in BP control over 24 months using a self-management intervention developed using an implementation science framework; however, the self-management program was not sustained beyond the study period. Discharge instructions tailored for health literacy level have been demonstrated to be effective in improving postdischarge knowledge about hypertension in emergency room patients who present with hypertension.51 One self-management program consisting of written educational materials along with BP, exercise, and food consumption logs resulted in improvements in self-reported BP measurements from 96% of patients who returned BP logs.48 Jackson et al. 49 demonstrated that medication and behavioral management interventions delivered through a telephone-based system were effective in reducing systolic and diastolic BP 12 and 18 months after the start of the intervention. Migneault et al. 50 found that an automatic, culturally adapted telemedicine system was effective in improving dietary quality, although there were no effects on BP. Balcazar et al. 71 demonstrated that a model in which community health workers disseminated NHLBI-produced BP education modules yielded statistically significant dietary behavioral outcomes and perceived benefits of healthy behaviors in Hispanic patients. Zarate-Abbott et al. 72 developed a culturally sensitive workplace health education program targeted at low-income Hispanic immigrant housekeepers and demonstrated improvements in systolic and diastolic BP at 17 months. Kim et al. 73 tested a self-help multimodal behavioral intervention and showed improvements in BP control, knowledge, self-efficacy, medication adherence, and depression over 12 months in older Korean-Americans.
Counseling strategies.
Programs in stress reduction help improve BP control; a transcendental meditation program showed significant reductions in all-cause mortality, MI, stroke, systolic BP, and anger expression in African-American patients with coronary artery disease.47 The Five Plus Nuts and Beans study is an ongoing randomized trial that looks to compare the effectiveness of general written dietary advice vs. neighborhood-specific counseling regarding food purchasing and dietary behaviors on BP control in African-American patients with medication-controlled hypertension in an urban practice.79
Motivational strategies.
One study used positive-affect induction and self-affirmation with patient education in African-Americans, demonstrating improvements in medication adherence, but no significant changes in BP control at 12 months.46
Family/social support system interventions
Several interventions have also been developed to address barriers to BP control at the level of the family and social support systems (Tables 1, 2).
Targeting family members.
Flynn et al. 83 conducted focus groups of African-American patients with hypertension and found that patients often cited family members as facilitators in engagement in hypertension self-management. As such, one of the interventions being tested in the Achieving Blood Pressure Control Together (ACT) study will include communication activation for patients and family members.81
Targeting peer support.
In one intervention, 147 African-Americans with hypertension received a DVD with culturally appropriate stories from peer patients to discuss BP control. The program was noted to improve BP control in these patients up to three months postintervention.52 Peer-to-peer phone calls from patients with well-controlled hypertension were demonstrated to be effective in reducing systolic BP in African-American patients with uncontrolled hypertension.56 Rodriguez et al. 54 demonstrated that a group education course, which contained information on dietary and lifestyle changes, was effective in reducing systolic BP at 6 and 12 weeks postintervention. In addition, a hypertension education program targeted to African-Americans with CVD focused around peer groups and social networks was more effective in decreasing systolic and diastolic BP when compared with usual care.55 One 6-week culturally tailored group behavioral intervention for Hispanic/Latino adults resulted in improvements in systolic BP, weight, body mass index, and physical activity as compared with preintervention baseline measures.53
Targeting extended social networks.
The ACT study56 is currently ongoing and involves community health workers to leverage individual patient factors along with family and social support factors to improve patient participation in hypertension self-management. Victor et al. 74 demonstrated that an intervention targeting African-American owned barbershops where barbers were enabled to work as health educators and provide BP checks improved BP control and marginally decreased systolic BP in clients with hypertension.
Provider/team interventions
Several interventions have addressed patient–provider communication as a major means of improving BP control (Tables 1, 2). One intervention did not demonstrate any statistically significant differences in BP among patients whose primary physicians were randomized to a cultural competence curriculum.57 However, Cooper et al. tested physician communication skills training and patient activation by community health workers and showed improvements in participatory decision making and systolic BP.76 The latter interventions reduced racial disparities in participatory decision-making and patient positive affect (personal communication with author), but widened disparities in patient question-asking between patients with low and adequate health literacy.23 Johnson et al. 67 demonstrated that a combined approach of physician education by hypertension specialists as well as patient counseling on BP management resulted in statistically significant improvements in BP control over 6 months in a primarily African-American patient population. A nurse-driven program to facilitate CVD self-management behaviors was effective in decreasing systolic and diastolic BP; these changes were not enhanced by a concomitant telephone-based intervention.69 Bilingual nurse counseling in Korean-Americans has shown to be effective in improving medication adherence, alcohol consumption, and exercise, with frequency of counseling related to intervention effect.25 Finally, Pezzin et al. 68 demonstrated that a home-based nurse and health educator counseling intervention improved BP control among recently discharged African-American patients with stage 2 hypertension.
ORGANIZATION/PRACTICE SETTING INTERVENTIONS
Several interventions examined the effectiveness of changes in organizational setting or practices in helping to control BP (Tables 1, 2). Song et al. 61 demonstrated significant decreases in BP among patients who followed-up at mobile health clinics for BP care. The role of electronic medical records (EMRs) was examined in two studies; both showed that clinics without EMR systems had greater racial disparities in BP control.58,60 Use of clinical decision support technology in EMR systems has been shown to improve BP control across all ethnicities.58 In addition, Kim et al. 77 demonstrated that a 6-week behavioral education program followed by BP telemonitoring and bilingual nurse telephone counseling was effective in markedly improving BP control in a Korean-American immigrant population. Furthermore, use of intensive outpatient health services, such as heart failure management clinics, was also demonstrated to reduce racial disparities in BP control.59 Ogedegbe et al. 78 randomized community health centers in NC to a practice-based multicomponent educational intervention or usual care, and did not observe significant changes in patients’ BP control. Project ReD CHiP is an ongoing, multilevel health system quality improvement intervention that includes training in accurate BP measurement by staff; provider education (including audit and feedback of panel data stratified by race/ethnicity and communication skills focused on enhancing medication adherence); and access to improved wraparound care management services for patients in a large urban primary care network.82 Project ReD CHiP incorporates multiple individual level and provider or health system-level components, which have been guided by significant stakeholder engagement throughout development and implementation in order to ensure sustainability. The Heart Healthy Lenoir project combines practice-level quality improvement interventions to improve BP control with patient-directed interventions, using a health coach to improve BP control.80 The latter two projects, funded by the National Institutes of Health (NIH) Centers for Population Health and Health Disparities, are using principles of community-based participatory research (CBPR) and implementation science throughout intervention planning and development and adapting the interventions to local context to enhance sustainability.
Local community environment interventions
Several interventions have sought to improve BP control on the community level (Tables 1, 2). An ongoing community screening intervention for BP control targeting African-American males in barbershops seeks to identify patients from local communities with high BP and randomize them to subsequent motivational interviewing and patient navigator interventions.62 Zoellner et al. 63 used a CBPR approach to enroll patients from a Mississippi town into a BP management program including group education sessions, weekly pedometer log compliance, and motivational enhancement sessions. This study demonstrated statistically significant decreases in systolic and diastolic BP and sugar intake in participants, who were primarily African-American. Cene et al. 70 evaluated a community-based self-management program provided by community health workers and a nurse practitioner for African-Americans patients with high CVD risk; this intervention did not produce significant changes in systolic or diastolic BP. A Dietary Approaches to Stop Hypertension (DASH) meal delivery program to older adults with CVD was effective in making recipient diets Dietary Approaches to Stop Hypertension (DASH)-adherent; however, this program was more effective in white and higher income patients.64
State/national policy environment interventions
Several interventions have been developed to address disparities in BP management and control at state and national levels (Tables 1, 2). Many of these policy initiatives are relatively new and evidence of long-term effectiveness and best practices for sustaining and disseminating these interventions are not yet clear. For example, the Health Services and Research Administration (HRSA) has sponsored health disparities collaboratives in community health centers. Of the centers that had health disparities collaboratives, there was no significant improvement in intermediate outcomes or composite quality measures for hypertension,66 although they were successful in improving process of care measures for asthma and diabetes. To date, large-scale analyses of health disparities collaboratives have shown no effect on composite quality outcomes or disparities for hypertension.65,66 The reasons for this may be multifactorial. For instance, it is unclear how effective interventions are being disseminated from practice to practice. Initiatives such as the Million Hearts Project will be helpful in elucidating this information; the project is convening broad groups of stakeholders from provider professional organizations, health care system leaders, community-based organizations, advocacy groups, retail pharmacy and medical technology vendors, pharmaceutical and biotech companies, policy makers, funders, and the public health sector to encourage sharing of best practices, technical support, tools, and collaborations on demonstrations that can be scaled up and spread (MillionHearts.org). Specific to hypertension control, the Million Hearts Project seeks to prevent one million heart attacks and strokes by 2017 through quality improvement initiatives; increasing awareness; and improving access to care.84
Similarly, the Department of Health and Human Services and the CDC have sponsored multiple initiatives to reduce racial disparities in BP control, both directly and indirectly. The Affordable Care Act has also provided multiple provisions to reduce health disparities, including the expansion of Medicaid coverage to improve access; requiring that all federally funded programs collect data on race, ethnicity, primary language, disability status, and gender; expanding funding for the National Health Service Corps and creating Health Professional Training Grants for underserved areas; and by providing $11 billion for community health center programs to expand coverage through FQHCs. In addition, the HHS has made data collection to track disparities a priority through the Healthy People 2020 project, and the CDC has implemented multiple initiatives to reduce health disparities through its Office of Minority Health and Health Equity, by providing support to the Community Preventive Services Task Force and the National Prevention Council, and by providing funding for further community initiatives through Community Transformation Grants.85
Several state initiatives also focus on reductions in health disparities. In 2009, the Institute of Medicine held a roundtable on health disparities, from which a four-pronged summary of recommendations was released.86 This broad-based set of recommendations included suggestions on capacity-building and enhancement of access to quality resources at the community level; within health care services; and at the level of the health care system; as well as overarching recommendations on how to support local efforts at local, state, and national policy levels.86 Minnesota launched an Eliminating Health Disparities Initiative (EHDI) in 2001 to focus on reducing disparities in eight key areas, one of which is CVD.87 Concomitantly, CVD death rate decreased significantly in African-Americans over the 1999–2004 time period when compared to 1995–1999.87 Massachusetts has spearheaded several initiatives to reduce disparities, including a Health Disparities Council to track the progress of statewide health care reform programs in reducing disparities, revision of Mass Health Medicaid financial incentives to reduce disparities, and stratification of healthcare effectiveness quality measures by race and ethnicity.86 In Maryland, the 2012 Health Improvement and Disparities Reduction Act provided $4 million to fund the development of Health Enterprise Zones (HEZs) to improve health outcomes and reduce health disparities, as well as provisions for additional tax credits and loan repayment assistance within the HEZs.88 The law also encourages reporting and analysis of health disparities data, as well as continued cultural competency training for health care providers.88 To our knowledge, the initiatives in Massachusetts and Maryland have not yet reported their results.
RECOMMENDATIONS FOR TRANSLATING EFFECTIVE INTERVENTIONS INTO PRACTICE AND POLICY
Several effective interventions exist to improve BP in racial and ethnic minorities; however, evidence that they will reduce disparities is limited. To strengthen the evidence and translate it into practice and policy, we recommend implementation and rigorous evaluation of pragmatic, multilevel interventions; institutional support for broad stakeholder partnerships that include payers, patients, researchers, policymakers, and community-based organizations; and balance and alignment in the priorities and incentives of each stakeholder group. Table 3 enumerates these recommendations.
Table 3.
Recommendations
| Funders |
|---|
| Continue to promote research with broad stakeholder engagement and with plans for sustainability through all agencies, including National Institutes of Health, Agency for Healthcare Research and Quality, and PCORI and private foundations |
| Provide mechanisms to implement and test dissemination of effective interventions not just to researchers and healthcare delivery organizations, but to patients and community-based organizations |
| Communicate with patients and community-based organizations to align their priorities, values, and goals with those of researchers and payers |
| Policymakers |
| Develop and expand Current Procedural Terminology (CPT®) billing codes for wraparound and preventive services including patient education, telemedicine, mid-level provider driven, and team-based interventions |
| Encourage reporting of data to identify and address disparities |
| Provide funding and other incentives for multilevel community-based initiatives |
| Payers |
| Provide clear provisions for reimbursement for wraparound and preventive services including patient education, telemedicine, mid-level provider driven and team-based interventions |
| Design pay-for-performance and other reimbursement models that incentivize both quality and disparities reduction |
| Partner with researchers and healthcare providers to align incentives and reimbursement policies to support evidence-based effective interventions |
| Researchers |
| Continue development and innovation of multilevel interventions to reduce racial disparities |
| Assess community capacities as part of sustainability assessments in developing interventions |
| Maintain effective dialogue with patients and community-based organizations not just to disseminate best practices, but also to establish common sets of priorities, values, and goals |
| Communicate with payers about effective evidence-based practices and other evidence needed to inform changes to reimbursement |
| Provide training to the next generation of health disparities and implementation science researchers |
| Patients |
| Provide feedback to researchers and community-based organizations about effectiveness of interventions |
| Provide input to providers and community-based organizations about priorities, values, and goals |
| Community-based organizations |
| Communicate with researchers, payers, and patients about community priorities, values, and goals, and provide feedback on research, health system, and public health interventions |
| Work with researchers to build capacity to study, measure and disseminate effective interventions |
| Providers and healthcare organizations |
| Enroll in programs that reimburse for delivering covered services to low-income patients |
| Become familiar with community-based resources that enhance patient access to medications, specialty services, health promotion programs, and other social services |
| Incorporate sliding scale and/or flexible payment plans when possible |
| Include equity in healthcare delivery as a pillar of your quality improvement strategy and measure quality of care in all domains, stratified by groups/ethnicity |
| Explore and improve climate, policies, and training related to diversity within your practice or organization |
| Use culturally and linguistically appropriate signage, language services, and printed patient information for your patient population, and provide cultural and linguistic competence training for all providers and staff |
| Provide training for providers and clinical staff in patient-centered communication skills |
| Share best practices with colleagues, researchers, payers, community-based organizations, and policymakers |
Successful strengthening of the evidence base for implementation research and subsequent translation into practice in real world settings for the reduction of disparities calls for the training of a new cadre of individuals with relevant expertise and skill sets.89 In particular, the ability to integrate data from a wide variety of sources and embrace the analytic rigor required for solving complex, multilevel challenges typical in the health disparities arena will be essential. Training for this work must not only be transdisciplinary but must explicitly go beyond the traditional biomedical construct of health to include the social, psychological, cultural, behavioral, and ecological domains. It will be crucial to link this training with the appropriate communities where racial and ethnic disparities are most profound.89
Because barriers to reducing disparities in BP control are encountered at multiple levels of influence (Figure 1), interventions targeting barriers at several levels of the ecological model may be more effective at addressing disparities than those targeting barriers at only one or two levels.90,91 For researchers, we recommend designing and testing pragmatic interventions in real-world settings using implementation research methods to describe contextual influences and examine multilevel effects; and incorporating process measures, cost and economic analyses, and outcomes important to patients and communities. This may inform key stakeholders actively working to translate research findings into policy and practice. This work may also mobilize policy makers, providers, and organizations to implement and support these interventions on a broad scale, leading to sustainability of existing initiatives.
Assessing and increasing capacity at individual, organizational, and community levels is critical to intervention success.92 Collaborative efforts with full transparency with respect to aligning incentives and setting common priorities, values, and goals from all involved stakeholders will be important in producing sustained reductions in racial disparities in hypertension. From the payer perspective, measuring and tracking quality of care stratified by race, ethnicity and primary language and being cognizant of the potential for disparities with pay-for-performance models are important, as is the development of new Current Procedural Terminology (CPT®) codes to allow for adequate reimbursement for new and innovative models of care.
Similarly, continued active monitoring of progress across racial, ethnic, and sociodemographic groups at local, state, and national levels will be helpful in ensuring equity effectiveness and in preventing the development of further disparities. Our work has confirmed the observation made by others that certain populations that suffer disproportionate morbidity and mortality are relatively underrepresented in disparities-focused health services research.91 In the National Institutes of Health-funded study of 1,268 disparities-focused health services research initiatives conducted between 2007 and 2011, fewer research projects were designed to detect, understand, or eliminate disparities affecting American Indians/Native Americans (3%) and Pacific Islanders/Native Hawaiians (<1%) than in Blacks/African-Americans (24%) or in Hispanics/Latinos (18%).93
Finally, patients and community-based organizations should continue to communicate their priorities and work with researchers, healthcare provider organizations, and policy-makers to build their own capacities, mobilize resources, and advocate for change.
SUPPLEMENTARY MATERIAL
Supplementary materials are available at American Journal of Hypertension (http://ajh.oxfordjournals.org).
FUNDING
Dr Mueller is supported by Health Resources and Services Administration (HRSA-11–156). Dr Purnell was supported by the National Heart, Lung and Blood Institute of the National Institutes of Health (NHLBI, 5T32HL007180). Dr Cooper is supported by NHLBI (K24 HL083113, P50 HL0105187).
DISCLOSURE
There are no affiliations or financial involvement with any organization or entity with a direct financial interest in the subject matter or materials discussed in the manuscript. The authors have no financial or nonfinancial conflict to disclose.
Supplementary Material
REFERENCES
- 1.Agency for Healthcare Research and Quality (AHRQ) National Healthcare Disparities Report. Rockville, MD:: AHRQ Publication; 2013. [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) Racial/Ethnic disparities in the awareness, treatment, and control of hypertension - United States, 2003–2010. Morb Mortal Wkly Rep. 2013;62:351–355. [PMC free article] [PubMed] [Google Scholar]
- 3.Egan BM, Li J, Hutchison FN, Ferdinand KC. Hypertension in the United States 1999–2012: progress toward healthy people 2020 Goals. Circulation. 2014;130:1692–1699. doi: 10.1161/CIRCULATIONAHA.114.010676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bleich SN, Jarlenski MP, Bell CN, LaVeist TA. Health inequalities: trends, progress, and policy. Annu Rev Public Health. 2012;33:7–40. doi: 10.1146/annurev-publhealth-031811-124658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cooper ES. Cardiovascular diseases and stroke in African Americans: a call for action. J Natl Med Assoc. 1993;85:97–100. [PMC free article] [PubMed] [Google Scholar]
- 6.Downie DL, Schmid D, Plescia MG, Huston SL, Bostrom S, Yow A, Lawrence WW, Jr, DuBard CA. Racial disparities in blood pressure control and treatment differences in a Medicaid population, North Carolina, 2005-2006. Prev Chronic Dis. 2011;8:A55. [PMC free article] [PubMed] [Google Scholar]
- 7.Delgado J, Jacobs EA, Lackland DT, Evans DA, de Leon CF. Differences in blood pressure control in a large population-based sample of older African Americans and non-Hispanic whites. J Gerontol A Biol Sci Med Sci. 2012;67:1253–1258. doi: 10.1093/gerona/gls106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hypertension Detection and Follow-up Program Cooperative G. Five-year findings of the hypertension detection and follow-up program: mortality by race-sex and blood pressure level. A further analysis. Hypertension Detection and Follow-up Program Cooperative Group. J Commun Health. 1984;9 [PubMed] [Google Scholar]
- 9.Ooi WL, Budner NS, Cohen H, Madhavan S, Alderman MH. Impact of race on treatment response and cardiovascular disease among hypertensives. Hypertension. 1989;14:227–234. doi: 10.1161/01.hyp.14.3.227. [DOI] [PubMed] [Google Scholar]
- 10.Will JC, Nwaise IA, Schieb L, Zhong Y. Geographic and racial patterns of preventable hospitalizations for hypertension: Medicare beneficiaries, 2004-2009. Public Health Rep (Washington, D.C.: 1974) 2014;129:8–18. doi: 10.1177/003335491412900104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bronfenbrenner U. International Encyclopedia of Education. 2nd edn. Vol. 3. Oxford:: Elsevier; (1994). Ecological models of human development. [Google Scholar]
- 11a.Gauvain M., Col M, editors. 2nd edn. NY: Freeman; 1993. Readings on the development of children; pp. 37–43. [Google Scholar]
- 12.Gorin SS, Badr H, Krebs P, Prabhu Das I. Multilevel interventions and racial/ethnic health disparities. J Natl Cancer Inst Monogr. 2012;2012:100–111. doi: 10.1093/jncimonographs/lgs015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sehgal AR. Overlap between whites and blacks in response to antihypertensive drugs. Hypertension. 2004;43:566–572. doi: 10.1161/01.HYP.0000118019.28487.9c. [DOI] [PubMed] [Google Scholar]
- 14.Ndumele CD, Shaykevich S, Williams D, Hicks LS. Disparities in adherence to hypertensive care in urban ambulatory settings. J Health Care Poor Underserved. 2010;21:132–143. doi: 10.1353/hpu.0.0259. [DOI] [PubMed] [Google Scholar]
- 15.Kressin NR, Orner MB, Manze M, Glickman ME, Berlowitz D. Understanding contributors to racial disparities in blood pressure control. Circ Cardiovasc Qual Outcomes. 2010;3:173–180. doi: 10.1161/CIRCOUTCOMES.109.860841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kyanko KA, Franklin RH, Angell SY. Adherence to chronic disease medications among New York City Medicaid participants. J Urban Health. 2013;90:323–328. doi: 10.1007/s11524-012-9724-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bosworth HB, Powers B, Grubber JM, Thorpe CT, Olsen MK, Orr M, Oddone EZ. Racial differences in blood pressure control: potential explanatory factors. J Gen Intern Med. 2008;23:692–698. doi: 10.1007/s11606-008-0547-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hill MN, Bone LR, Kim MT, Miller DJ, Dennison CR, Levine DM. Barriers to hypertension care and control in young urban black men. Am J Hypertens. 1999;12:951–958. doi: 10.1016/s0895-7061(99)00121-1. [DOI] [PubMed] [Google Scholar]
- 19.Pawlak R, Colby S. Benefits, barriers, self-efficacy and knowledge regarding healthy foods; perception of African Americans living in eastern North Carolina. Nutr Res Pract. 2009;3:56–63. doi: 10.4162/nrp.2009.3.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Warren-Findlow J, Seymour RB. Prevalence rates of hypertension self-care activities among African Americans. J Natl Med Assoc. 2011;103:503–512. doi: 10.1016/s0027-9684(15)30365-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Spruill TM, Gerber LM, Schwartz JE, Pickering TG, Ogedegbe G. Race differences in the physical and psychological impact of hypertension labeling. Am J Hypertens. 2012;25:458–463. doi: 10.1038/ajh.2011.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brewer LC, Carson KA, Williams DR, Allen A, Jones CP, Cooper LA. Association of race consciousness with the patient-physician relationship, medication adherence, and blood pressure in urban primary care patients. Am J Hypertens. 2013;26:1346–1352. doi: 10.1093/ajh/hpt116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aboumatar HJ, Carson KA, Beach MC, Roter DL, Cooper LA. The impact of health literacy on desire for participation in healthcare, medical visit communication, and patient reported outcomes among patients with hypertension. J Gen Intern Med. 2013;28:1469–1476. doi: 10.1007/s11606-013-2466-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shin H, Bruno R. 2000. Language use and English-speaking ability. http://www.census.gov.ezproxy.welch.jhmi.edu/prod/2003pubs/c2kbr-29.pdf .
- 25.Han HR, Kim J, Kim KB, Jeong S, Levine D, Li C, Song H, Kim MT. Implementation and success of nurse telephone counseling in linguistically isolated Korean American patients with high blood pressure. Patient Educ Couns. 2010;80:130–134. doi: 10.1016/j.pec.2009.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fang J, Yang Q, Ayala C, Loustalot F. Disparities in Access to Care Among US Adults With Self-Reported Hypertension. Am J Hypertens. 2014;27:1377–1386. doi: 10.1093/ajh/hpu061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lewis LM, Askie P, Randleman S, Shelton-Dunston B. Medication adherence beliefs of community-dwelling hypertensive African Americans. J Cardiovasc Nurs. 2010;25:199–206. doi: 10.1097/JCN.0b013e3181c7ccde. [DOI] [PubMed] [Google Scholar]
- 28.Flack JM, Sica DA, Bakris G, Brown AL, Ferdinand KC, Grimm RH, Jr, Hall WD, Jones WE, Kountz DS, Lea JP, Nasser S, Nesbitt SD, Saunders E, Scisney-Matlock M, Jamerson KA. International Society on Hypertension in Blacks Management of high blood pressure in Blacks: an update of the International Society on Hypertension in Blacks consensus statement. Hypertension. 2010;56:780–800. doi: 10.1161/HYPERTENSIONAHA.110.152892. [DOI] [PubMed] [Google Scholar]
- 29.Patel RP, Taylor SD. Factors affecting medication adherence in hypertensive patients. Ann Pharmacother. 2002;36:40–45. doi: 10.1345/aph.1A046. [DOI] [PubMed] [Google Scholar]
- 30.Chan PS, Nichol G, Krumholz HM, Spertus JA, Jones PG, Peterson ED, Rathore SS, Nallamothu BK. American Heart Association National Registry of Cardiopulmonary Resuscitation (NRCPR) Investigators Racial differences in survival after in-hospital cardiac arrest. JAMA. 2009;302:1195–1201. doi: 10.1001/jama.2009.1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cené CW, Roter D, Carson KA, Miller ER, 3rd, Cooper LA. The effect of patient race and blood pressure control on patient-physician communication. J Gen Intern Med. 2009;24:1057–1064. doi: 10.1007/s11606-009-1051-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Benjamins MR. Race/ethnic discrimination and preventive service utilization in a sample of whites, blacks, Mexicans, and Puerto Ricans. Med Care. 2012;50:870–876. doi: 10.1097/MLR.0b013e31825a8c63. [DOI] [PubMed] [Google Scholar]
- 33.Gerber LM, Mann SJ, McDonald MV, Chiu YL, Sridharan S, Feldman PH. Diuretic use in black patients with uncontrolled hypertension. Am J Hypertens. 2013;26:174–179. doi: 10.1093/ajh/hps029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Johnson RL, Roter D, Powe NR, Cooper LA. Patient race/ethnicity and quality of patient-physician communication during medical visits. Am J Public Health. 2004;94:2084–2090. doi: 10.2105/ajph.94.12.2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jones DE, Carson KA, Bleich SN, Cooper LA. Patient trust in physicians and adoption of lifestyle behaviors to control high blood pressure. Patient Educ Couns. 2012;89:57–62. doi: 10.1016/j.pec.2012.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Martin KD, Roter DL, Beach MC, Carson KA, Cooper LA. Physician communication behaviors and trust among black and white patients with hypertension. Med Care. 2013;51:151–157. doi: 10.1097/MLR.0b013e31827632a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Finkelstein EA, Khavjou OA, Mobley LR, Haney DM, Will JC. Racial/ethnic disparities in coronary heart disease risk factors among WISEWOMAN enrollees. J Womens Health (Larchmt) 2004;13:503–518. doi: 10.1089/1540999041280963. [DOI] [PubMed] [Google Scholar]
- 38.Brondolo E, Love EE, Pencille M, Schoenthaler A, Ogedegbe G. Racism and hypertension: a review of the empirical evidence and implications for clinical practice. Am J Hypertens. 2011;24:518–529. doi: 10.1038/ajh.2011.9. [DOI] [PubMed] [Google Scholar]
- 39.Kingsbury JH, Buxton OM, Emmons KM. Sleep and its Relationship to Racial and Ethnic Disparities in Cardiovascular Disease. Curr Cardiovasc Risk Rep. 2013;7 doi: 10.1007/s12170-013-0330-0. (5). doi:10.1007/s12170-013-0330-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Karve AM, Ou FS, Lytle BL, Peterson ED. Potential unintended financial consequences of pay-for-performance on the quality of care for minority patients. Am Heart J. 2008;155:571–576. doi: 10.1016/j.ahj.2007.10.043. [DOI] [PubMed] [Google Scholar]
- 41.Lee JT, Netuveli G, Majeed A, Millett C. The effects of pay for performance on disparities in stroke, hypertension, and coronary heart disease management: interrupted time series study. PLoS One. 2011;6:e27236. doi: 10.1371/journal.pone.0027236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Weissman JS, Hasnain-Wynia R, Weinick RM, Kang R, Vogeli C, Iezzoni L, Landrum MB. Pay-for-performance programs to reduce racial/ethnic disparities: what might different designs achieve? J Health Care Poor Underserved. 2012;23:144–160. doi: 10.1353/hpu.2012.0030. [DOI] [PubMed] [Google Scholar]
- 43.Capewell S, Graham H. Will cardiovascular disease prevention widen health inequalities? PLoS Med. 2010;7:e1000320. doi: 10.1371/journal.pmed.1000320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tugwell P, de Savigny D, Hawker G, Robinson V. Applying clinical epidemiological methods to health equity: the equity effectiveness loop. BMJ (Clinical Research Ed.) 2006;332:358–361. doi: 10.1136/bmj.332.7537.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bosworth HB, Olsen MK, Grubber JM, Powers BJ, Oddone EZ. Racial differences in two self-management hypertension interventions. Am J Med. 2011;124:468.e1–468.e8. doi: 10.1016/j.amjmed.2010.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ogedegbe GO, Boutin-Foster C, Wells MT, Allegrante JP, Isen AM, Jobe JB, Charlson ME. A randomized controlled trial of positive-affect intervention and medication adherence in hypertensive African Americans. Arch Intern Med. 2012;172:322–326. doi: 10.1001/archinternmed.2011.1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schneider RH, Grim CE, Rainforth MV, Kotchen T, Nidich SI, Gaylord-King C, Salerno JW, Kotchen JM, Alexander CN. Stress reduction in the secondary prevention of cardiovascular disease: randomized, controlled trial of transcendental meditation and health education in Blacks. Circ Cardiovasc Qual Outcomes. 2012;5:750–758. doi: 10.1161/CIRCOUTCOMES.112.967406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rigsby BD. Hypertension improvement through healthy lifestyle modifications. ABNF J. 2011;22:41–43. [PubMed] [Google Scholar]
- 49.Jackson GL, Oddone EZ, Olsen MK, Powers BJ, Grubber JM, McCant F, Bosworth HB. Racial differences in the effect of a telephone-delivered hypertension disease management program. J Gen Intern Med. 2012;27:1682–1689. doi: 10.1007/s11606-012-2138-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Migneault JP, Dedier JJ, Wright JA, Heeren T, Campbell MK, Morisky DE, Rudd P, Friedman RH. A culturally adapted telecommunication system to improve physical activity, diet quality, and medication adherence among hypertensive African-Americans: a randomized controlled trial. Ann Behav Med. 2012;43:62–73. doi: 10.1007/s12160-011-9319-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Giuse NB, Koonce TY, Storrow AB, Kusnoor SV, Ye F. Using health literacy and learning style preferences to optimize the delivery of health information. J Health Commun. 2012;17(Suppl 3):122–140. doi: 10.1080/10810730.2012.712610. [DOI] [PubMed] [Google Scholar]
- 52.Houston TK, Allison JJ, Sussman M, Horn W, Holt CL, Trobaugh J, Salas M, Pisu M, Cuffee YL, Larkin D, Person SD, Barton B, Kiefe CI, Hullett S. Culturally appropriate storytelling to improve blood pressure: a randomized trial. Ann Intern Med. 2011;154:77–84. doi: 10.7326/0003-4819-154-2-201101180-00004. [DOI] [PubMed] [Google Scholar]
- 53.Rocha-Goldberg Mdel P, Corsino L, Batch B, Voils CI, Thorpe CT, Bosworth HB, Svetkey LP. Hypertension Improvement Project (HIP) Latino: results of a pilot study of lifestyle intervention for lowering blood pressure in Latino adults. Ethn Health. 2010;15:269–282. doi: 10.1080/13557851003674997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rodriguez F, Christopher L, Johnson CE, Wang Y, Foody JM. Love your heart: a pilot community-based intervention to improve the cardiovascular health of African American women. Ethn Dis. 2012;22:416–421. [PubMed] [Google Scholar]
- 55.Shaya FT, Chirikov VV, Daniel Mullins C, Shematek J, Howard D, Foster C, Saunders E. Social networks help control hypertension. J Clin Hypertens (Greenwich, Conn.) 2013;15:34–40. doi: 10.1111/jch.12036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Turner BJ, Hollenbeak CS, Liang Y, Pandit K, Joseph S, Weiner MG. A randomized trial of peer coach and office staff support to reduce coronary heart disease risk in African-Americans with uncontrolled hypertension. J Gen Intern Med. 2012;27:1258–1264. doi: 10.1007/s11606-012-2095-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Thom DH, Tirado MD, Woon TL, McBride MR. Development and evaluation of a cultural competency training curriculum. BMC Med Educ. 2006;6:38. doi: 10.1186/1472-6920-6-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hicks LS, Sequist TD, Ayanian JZ, Shaykevich S, Fairchild DG, Orav EJ, Bates DW. Impact of computerized decision support on blood pressure management and control: a randomized controlled trial. J Gen Intern Med. 2008;23:429–441. doi: 10.1007/s11606-007-0403-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hebert K, Julian E, Alvarez J, Dias A, Tamariz L, Arcement L, Quevedo HC. Eliminating disparities in hypertension care for Hispanics and blacks using a heart failure disease management program. South Med J. 2011;104:567–573. doi: 10.1097/SMJ.0b013e318224dd18. [DOI] [PubMed] [Google Scholar]
- 60.Samal L, Lipsitz SR, Hicks LS. Impact of electronic health records on racial and ethnic disparities in blood pressure control at US primary care visits. Arch Intern Med. 2012;172:75–76. doi: 10.1001/archinternmed.2011.604. [DOI] [PubMed] [Google Scholar]
- 61.Song Z, Hill C, Bennet J, Vavasis A, Oriol NE. Mobile clinic in Massachusetts associated with cost savings from lowering blood pressure and emergency department use. Health Affairs (Project Hope) 2013;32:36–44. doi: 10.1377/hlthaff.2011.1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ravenell J, Thompson H, Cole H, Plumhoff J, Cobb G, Afolabi L, Boutin-Foster C, Wells M, Scott M, Ogedegbe G. A novel community-based study to address disparities in hypertension and colorectal cancer: a study protocol for a randomized control trial. Trials. 2013;14:287. doi: 10.1186/1745-6215-14-287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zoellner J, Connell C, Madson MB, Thomson JL, Landry AS, Fontenot Molaison E, Blakely Reed V, Yadrick K. HUB city steps: a 6-month lifestyle intervention improves blood pressure among a primarily African-American community. J Acad Nutr Diet. 2014;114:603–612. doi: 10.1016/j.jand.2013.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Troyer JL, Racine EF, Ngugi GW, McAuley WJ. The effect of home-delivered Dietary Approach to Stop Hypertension (DASH) meals on the diets of older adults with cardiovascular disease. Am J Clin Nutr. 2010;91:1204–1212. doi: 10.3945/ajcn.2009.28780. [DOI] [PubMed] [Google Scholar]
- 65.Hicks LS, O’Malley AJ, Lieu TA, Keegan T, McNeil BJ, Guadagnoli E, Landon BE. Impact of health disparities collaboratives on racial/ethnic and insurance disparities in US community health centers. Arch Intern Med. 2010;170:279–286. doi: 10.1001/archinternmed.2010.493. [DOI] [PubMed] [Google Scholar]
- 66.Landon BE, Hicks LS, O’Malley AJ, Lieu TA, Keegan T, McNeil BJ, Guadagnoli E. Improving the management of chronic disease at community health centers. N Engl J Med. 2007;356:921–934. doi: 10.1056/NEJMsa062860. [DOI] [PubMed] [Google Scholar]
- 67.Johnson W, Shaya FT, Khanna N, Warrington VO, Rose VA, Yan X, Bailey-Weaver B, Mullins CD, Saunders E. The Baltimore Partnership to Educate and Achieve Control of Hypertension (The BPTEACH Trial): a randomized trial of the effect of education on improving blood pressure control in a largely African American population. J Clin Hypertens (Greenwich, Conn.) 2011;13:563–570. doi: 10.1111/j.1751-7176.2011.00477.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pezzin LE, Feldman PH, Mongoven JM, McDonald MV, Gerber LM, Peng TR. Improving blood pressure control: results of home-based post-acute care interventions. J Gen Intern Med. 2011;26:280–286. doi: 10.1007/s11606-010-1525-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bove AA, Santamore WP, Homko C, Kashem A, Cross R, McConnell TR, Shirk G, Menapace F. Reducing cardiovascular disease risk in medically underserved urban and rural communities. Am Heart J. 2011;161:351–359. doi: 10.1016/j.ahj.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 70.Cene CW, Yanek LR, Moy TF, Levine DM, Becker LC, Becker DM. Sustainability of a multiple risk factor intervention on cardiovascular disease in high-risk African American families. Ethn Dis. 2008;18:169–175. [PubMed] [Google Scholar]
- 71.Balcazar HG, Byrd TL, Ortiz M, Tondapu SR, Chavez M. A randomized community intervention to improve hypertension control among Mexican Americans: using the promotoras de salud community outreach model. J Health Care Poor Underserved. 2009;20:1079–1094. doi: 10.1353/hpu.0.0209. [DOI] [PubMed] [Google Scholar]
- 72.Zarate-Abbott P, Etnyre A, Gilliland I, Mahon M, Allwein D, Cook J, Mikan V, Rauschhuber M, Sethness R, Muñoz L, Lowry J, Jones ME. Workplace health promotion–strategies for low-income Hispanic immigrant women. AAOHN J. 2008;56:217–222. doi: 10.3928/08910162-20080501-01. [DOI] [PubMed] [Google Scholar]
- 73.Kim KB, Han HR, Huh B, Nguyen T, Lee H, Kim MT. The effect of a community-based self-help multimodal behavioral intervention in Korean American seniors with high blood pressure. Am J Hypertens. 2014;27:1199–1208. doi: 10.1093/ajh/hpu041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Victor RG, Ravenell JE, Freeman A, Leonard D, Bhat DG, Shafiq M, Knowles P, Storm JS, Adhikari E, Bibbins-Domingo K, Coxson PG, Pletcher MJ, Hannan P, Haley RW. Effectiveness of a barber-based intervention for improving hypertension control in black men: the BARBER-1 study: a cluster randomized trial. Arch Intern Med. 2011;171:342–350. doi: 10.1001/archinternmed.2010.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Glasgow RE, Askew S, Purcell P, Levine E, Warner ET, Stange KC, Colditz GA, Bennett GG. Use of RE-AIM to Address Health Inequities: Application in a low-income community health center based weight loss and hypertension self-management program. Transl Behav Med. 2013;3:200–210. doi: 10.1007/s13142-013-0201-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cooper LA, Roter DL, Carson KA, Bone LR, Larson SM, Miller ER, 3rd, Barr MS, Levine DM. A randomized trial to improve patient-centered care and hypertension control in underserved primary care patients. J Gen Intern Med. 2011;26:1297–1304. doi: 10.1007/s11606-011-1794-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kim MT, Han HR, Hedlin H, Kim J, Song HJ, Kim KB, Hill MN. Teletransmitted monitoring of blood pressure and bilingual nurse counseling-sustained improvements in blood pressure control during 12 months in hypertensive Korean Americans. J Clin Hypertens (Greenwich, Conn.) 2011;13:605–612. doi: 10.1111/j.1751-7176.2011.00479.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ogedegbe G, Tobin JN, Fernandez S, Cassells A, Diaz-Gloster M, Khalida C, Pickering T, Schwartz JE. Counseling African Americans to Control Hypertension: cluster-randomized clinical trial main effects. Circulation. 2014;129:2044–2051. doi: 10.1161/CIRCULATIONAHA.113.006650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Cooper LA, Boulware LE, Miller ER, 3rd, Golden SH, Carson KA, Noronha G, Huizinga MM, Roter DL, Yeh HC, Bone LR, Levine DM, Hill-Briggs F, Charleston J, Kim M, Wang NY, Aboumatar H, Halbert JP, Ephraim PL, Brancati FL. Creating a transdisciplinary research center to reduce cardiovascular health disparities in Baltimore, Maryland: lessons learned. Am J Public Health. 2013;103:e26–e38. doi: 10.2105/AJPH.2013.301297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Halladay JR, Donahue KE, Hinderliter AL, Cummings DM, Cene CW, Miller CL, Garcia BA, Tillman J, DeWalt D Heart Healthy Lenoir Research Team. The Heart Healthy Lenoir project–an intervention to reduce disparities in hypertension control: study protocol. BMC Health Serv Res. 2013;13:441. doi: 10.1186/1472-6963-13-441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ephraim PL, Hill-Briggs F, Roter DL, Bone LR, Wolff JL, Lewis-Boyer L, Levine DM, Aboumatar HJ, Cooper LA, Fitzpatrick SJ, Gudzune KA, Albert MC, Monroe D, Simmons M, Hickman D, Purnell L, Fisher A, Matens R, Noronha GJ, Fagan PJ, Ramamurthi HC, Ameling JM, Charlston J, Sam TS, Carson KA, Wang NY, Crews DC, Greer RC, Sneed V, Flynn SJ, DePasquale N, Boulware LE. Improving urban African Americans’ blood pressure control through multi-level interventions in the Achieving Blood Pressure Control Together (ACT) study: a randomized clinical trial. Contemp Clin Trials. 2014;38:370–382. doi: 10.1016/j.cct.2014.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Cooper LA, Marsteller JA, Noronha GJ, Flynn SJ, Carson KA, Boonyasai RT, Anderson CA, Aboumatar HJ, Roter DL, Dietz KB, Miller ER, 3rd, Prokopowicz GP, Dalcin AT, Charleston JB, Simmons M, Huizinga MM. A multi-level system quality improvement intervention to reduce racial disparities in hypertension care and control: study protocol. Implement Sci. 2013;8:60. doi: 10.1186/1748-5908-8-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Flynn SJ, Ameling JM, Hill-Briggs F, Wolff JL, Bone LR, Levine DM, Roter DL, Lewis-Boyer L, Fisher AR, Purnell L, Ephraim PL, Barbers J, Fitzpatrick SL, Albert MC, Cooper LA, Fagan PJ, Martin D, Ramamurthi HC, Boulware LE. Facilitators and barriers to hypertension self-management in urban African Americans: perspectives of patients and family members. Patient Prefer Adher. 2013;7:741–749. doi: 10.2147/PPA.S46517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Million Hearts website. http://millionhearts.hhs.gov/about_mh.html . Accessed 8 July 2014.
- 85.Meyer PA, Penman-Aguilar A, Campbell VA, Graffunder C, O’Connor AE, Yoon PW Centers for Disease Control and Prevention (CDC) Conclusion and future directions: CDC Health Disparities and Inequalities Report - United States, 2013. MMWR Surveill Summ. 2013;62(Suppl 3):184–186. [PubMed] [Google Scholar]
- 86.Karen M. Washington, DC: The National Academies Press; 2011. Anderson, Rapporteur; Roundtable on the Promotion of Health Equity and the Elimination of Health Disparities; Institute of Medicine: State and Local Policy Initiatives to Reduce Health Disparities: Workshop Summary. [Google Scholar]
- 87.Minnesota Office of Minority and Multicultural Health. “Minnesota’s Eliminating Health Disparities Initiative (EHDI), Report 4: Programmatic Results Achieved by EHDI Grantees. http://www.health.state.mn.us/ommh/grants/ehdi/ehdireport4080812.pdf. Accessed 7 November 2014.
- 88. Maryland Department of Health and Mental Hygiene website: “About HEZs”. http://dhmh.maryland.gov/healthenterprisezones/SitePages/About_Hezs.aspx . Accessed 8 July 2014.
- 89.Golden SH, Purnell T, Halbert JP, Matens R, Miller ER, Levine DM, Nguyen TH, Gudzune KA, Crews DC, Mahlangu-Ngcobo M, Cooper LA. A community-engagedcardiovascular health disparities research training curriculum: implementation and preliminary outcomes. Acad Med. 2014;89:1348–56. doi: 10.1097/ACM.0000000000000426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Clarke AR, Goddu AP, Nocon RS, Stock NW, Chyr LC, Akuoko JA, Chin MH. Thirty years of disparities intervention research: what are we doing to close racial and ethnic gaps in health care? Med Care. 2013;51:1020–26. doi: 10.1097/MLR.0b013e3182a97ba3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Glasgow L, Ashok M, Porterfield D, Morris L, Zheng Z. Understanding options to reduce disparities in CVD through comparative effectiveness research: a landscape review. http://www.pcori.org/assets/2014/01/PCORI-Landscape-Review-Understanding-Options-to-Reduce-Disparities-in-Cardiovascular-Disease-Dec-2013.pdf . Accessed 8 July 2014.
- 92.Flaspohler P, Duffy J, Wandersman A, Stillman L, Maras MA. Unpacking prevention capacity: an intersection of research-to-practice models and community-centered models. Am J Community Psychol. 2008;41:182–196. doi: 10.1007/s10464-008-9162-3. [DOI] [PubMed] [Google Scholar]
- 93.Association of American Medical Colleges. The State of Health Equity Research: Closing Knowledge Gaps to Address Inequities. https://members.aamc.org/eweb/upload/14-009%20HEALTH%20DISPARITIES_FINAL1.pdf . Accessed 27 October 2014.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


