At the end of 2012, more than 402,000 end-stage renal disease (ESRD) patients in the United States were receiving hemodialysis (HD) therapy.1 By current estimates, more than 700,000 Americans will have ESRD by 2015.2 HD vascular access dysfunction is a major cause of morbidity and mortality in this population, and results in a significant component of the overall health care cost in the United States.3 4 Arteriovenous (AV) fistula use in HD patients has surpassed alternative access options during the past decade as a result of the National Vascular Access Improvement Initiative, or Fistula First program.5 6 Fistulas are associated with better clinical outcomes and decreased morbidity, including lower infection rates and shorter lengths of hospitalization, compared with AV grafts. However, both AV fistulas and grafts are prone to dysfunction and eventual failure.7 8
Neointimal hyperplasia associated with HD access causes significant morbidity such as disruption of adequate flow rates for HD, suboptimal HD, arm swelling, prolonged bleeding after the removal of dialysis sheaths, extremity swelling caused by diversion of flow, pseudoaneurysms, and frank thrombosis.9 Percutaneous transluminal angioplasty (PTA) is a standard, first-line treatment for venous stenosis and is known to prolong the lifespan of HD access, but indications such as occlusions, frequent or early restenosis, and PTA-induced rupture have resulted in the frequent use of stents to supplement or replace PTA. Several retrospective series and multicenter, randomized, prospective trials10 11 12 have examined the effectiveness of PTA, bare metal stents (BMS), and stent grafts (SGs) for a variety of indications related to the maintenance of HD access. This article provides guidance on the use of stents to preserve HD access from the perspective of our busy academic practice, as well as an updated review of the relevant published literature.
General Tips to Avoid Stent-Related Complications and Treatment Failure
Avoiding Stent Migration, Fracture, and Deformation
“Measure twice and stent once.” The best defense against stent migration is strict adherence to the practice of oversizing based on an increase of 10 to 15% over the estimated normal vessel diameter to ensure adequate apposition of the stent to the vessel wall. Excessive oversizing should be avoided to prevent associated neointimal hyperplasia, early in-stent restenosis, and in the case of SGs, “corduroy” deformity of the stent wall caused by incomplete expansion. The length of the stent should cover the length of the diseased segment plus short segments of adjacent normal vessel upstream and downstream to the lesion.
Balloon-expandable stents are easily and permanently crushed when exposed to minimal trauma. To avoid the known complication of crushed stents, in our practice, all stents used for peripheral indications to preserve vascular access are self-expanding. The published use of balloon-expandable stents for dialysis vascular access has been limited to select cases of highly elastic central venous stenoses where precise placement is essential and the risk of traumatic stent compression is minimal. Dialysis shunts are superficial, sometimes cross joints, and are thus exposed to recurrent trauma, compression, and repetitive movement. Self-expanding stents are the only option in peripheral vessels since they more readily resume their shape after compression.
If at all possible, we avoid stent placement in cannulation zones or across joints to minimize the risks of fracture and fragmentation of stents, and infection of SGs.13 Repeated punctures of BMS can cause stenosis or pseudoaneurysm formation leading to access dysfunction. That said, in some cases, cannulation zones or joints cannot be practically avoided, and we prefer to select SGs (see below) in this setting due to their resistance to fracture demonstrated in the limited published literature.14 15 16
Selecting Covered versus Uncovered Stents
Stents can be further categorized as bare versus covered, and the advantages of each are discussed later in section “Specific Applications of Stents.” To review, a stent is made of a mesh-like metallic scaffold, typically nitinol (a nickel titanium alloy) or stainless steel. The advantage of nitinol stents over stainless steel stents is “shape memory”—the propensity to maintain stent length and shape throughout deployment. Covered stents, or SGs, are surfaced, either internally with polytetrafluoroethylene (PTFE) or externally with Dacron. At our institution, we prefer Viabahn SGs (Gore, Flagstaff, AZ) when crossing the elbow joint, covering cannulation sites, or spanning long venous segments. Viabahn is quite flexible, resistant to fracture, and available in longer sizes intended for their application to peripheral arterial disease. In addition, the low-profile Viabahn SG (Gore) allows for a smaller sheath caliber compared with that required for other SGs. Alternatively, despite its larger introducer, we use the Fluency SG (Bard, Tempe, AZ) without a sheath for these indications. When considering stents used in the treatment of the venous anastomosis of an AV graft, our preference is the FLAIR SG (Bard) due to favorable published results of this device for this specific indication (see section “Specific Applications of Stents”). For BMS, we typically use either Zilver (Bard) or Epic (Boston Scientific, Natick, MA) BMS for most indications because of their flexibility and shape memory.
Preserving Future Access Options
Stents have several significant drawbacks, and in our practice, we use them sparingly, particularly when their use places alternative access sites at risk. In such cases, despite frequent episodes of restenosis (up to 1 per month in our practice), we may continue to re-employ PTA as our secondary therapy and refer the case for future surgical revision or creation of new access. In such cases, exhausted access sites, the frequency of restenosis, and even social issues may play a role in the decision to continue repeating PTA more frequently instead of revising or replacing the access; the value of maintaining a multidisciplinary dialysis access conference for review of these cases is clear. The goal of any intervention should include preservation of not only current vascular access but also of future access options.
Certain anatomical locations are suboptimal for stent placement due to possible long-standing sequelae that interfere with that goal. If at all possible, stents should not “cage” venous branches that may serve as the outflow of future shunts or as a pathway for future catheter placement. Examples include coverage of the median cubital vein in the forearm, extension from the cephalic vein into the subclavian vein, and extension from the subclavian vein or brachiocephalic vein across the jugular vein confluence or contralateral brachiocephalic vein, respectively (Fig. 1). Such measures may preserve future brachial–basilic or axillary fistula formation, future dialysis catheter placement, or even future access options in the entire contralateral limb.
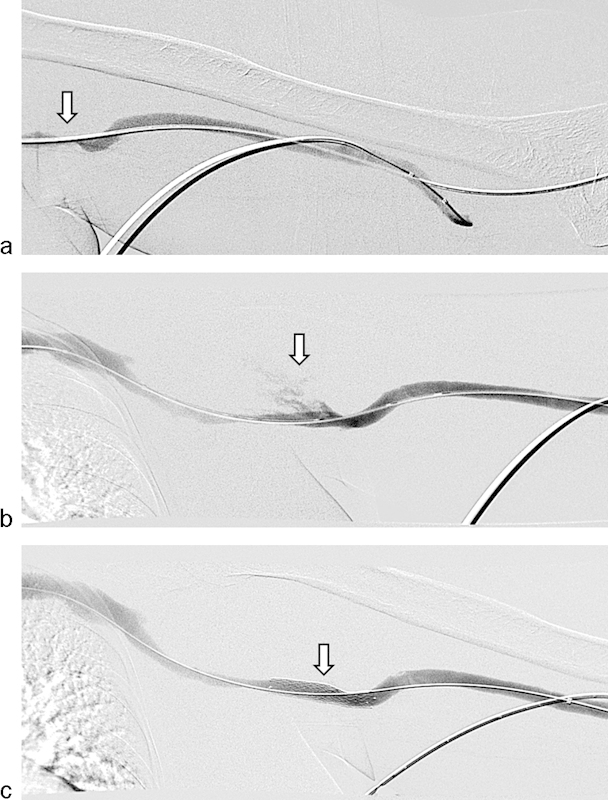
Fig. 1.
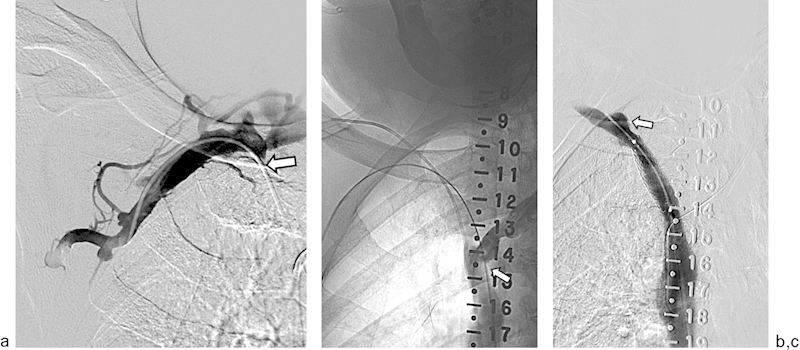
(a) An 82-year-old man with a right arm brachiocephalic fistula and chronic obstruction of the right brachiocephalic vein (arrow). The femoral vein was accessed for recanalization and stent placement. (b) Venography of the left brachiocephalic vein was performed with a radiopaque ruler in place to avoid caging this inflow vein (arrow) during stent deployment. (c) After stent deployment (12 × 40 mm Zilver), the inflows of the right internal jugular (arrow) and left brachiocephalic veins have been spared to preserve future access options.
Avoiding Infection
The authors' preference is to administer a single intravenous dose of prophylactic antibiotic before stent deployment. No published evidence supports periprocedural prophylactic antibiotics for stent deployment, but stents are foreign bodies, and rigorous adherence to aseptic technique is recommended. For those deemed to be at high risk for infection (e.g., long procedures, thrombolysis procedures, immune-compromised patients), antibiotics are administered by some interventionalists to cover skin pathogens, particularly when the case involves a synthetic graft rather than a fistula. Specifically for SGs, prophylactic antibiotics are recommended when stents are placed across pseudoaneurysms and aneurysms, as chronic clot within them has been shown to be colonized by bacteria.17 18
Follow-up
Following stent placement to maintain HD access, routine follow-up is performed by our nephrology colleagues at the time of dialysis via physical exam and standard hemodynamic surveillance techniques. Complex or recurring cases are discussed at our multidisciplinary vascular access conference. We do not routinely recommend anticoagulation after stent placement since the incidence of early thrombosis is low. However, we recommend immediate and long-term anticoagulation in cases of early thrombosis following stent deployment, particularly in cases involving chronically low blood pressure or absence of an identifiable anatomic cause of thrombosis.
Specific Applications of Stents
Venous stenosis along the HD vascular access circuit is a common and often difficult clinical entity to treat. In our practice, we treat all dialysis access stenoses with PTA first and reserve BMS and SGs for elastic stenoses or early recurrent (< 1 month) stenoses. If at all possible, we attempt to adhere to KDOQI clinical practice guidelines,19 which recommend that stents should be considered in the setting of unsuccessful PTA for peripheral venous stenosis resulting in either elastic recoil or early recurrent stenosis within 3 months. That said, the role of stents is evolving, as increasingly improved and robust studies over the past decade have demonstrated promising results, particularly for AV graft venous anastomotic stenosis and in-stent stenosis.
Historically, initial studies that looked at BMS versus PTA alone reported mixed results with no clear benefit for stents over PTA alone.11 20 21 22 However, nitinol BMS offer a clear advantage over PTA alone for a select patient population that has failed PTA because of elastic recoil, rapidly recurrent stenosis, or vessel rupture. In a prospective nonrandomized trial of patients that failed PTA, Vogel and Parise demonstrated significant reduction of restenosis using the SMART BMS (Cordis Corporation, Bridgewater, NJ) versus PTA, and also improved mean primary graft patency for its use specifically at the venous anastomosis,12 but difficulties with in-stent restenosis persisted. This study was limited by a small sample size and nonrandomization.
Venous Anastomotic Stenosis
The majority of AV grafts occlude due to progressive stenosis at the venous anastomosis. When venous anastomotic stenosis is clinically suspected, treatment considerations are based on the age of the graft, the timing and frequency of past interventions, the angiographic appearance of the stenosis, and its response to initial attempts at PTA. For focal, hemodynamically significant narrowing at the venous anastomosis, the first-line initial therapy consists of PTA. However, the time interval since graft creation should exceed 1 month to minimize the risk of rupture with PTA. If there is elastic recoil or early recurrence of the focal stenosis within 1 month, we proceed with primary SG placement. If the venous anastomotic site demonstrates a focal occlusion or a long, complex stenosis with a poor response to PTA, stent placement is again strongly considered.
In most cases, when stents are required at the venous anastomosis, we deploy a FLAIR SG (Fig. 2). For this indication, these stents offer the patency advantages described below, and they are manufactured in distally flared and unflared configurations that can be chosen when the diameter of the outflow vein central to the stenosis is larger than or equal to that of the AV graft, respectively. It is critical that a “landing zone” of nondiseased segment measuring at least 10 mm be incorporated into the SG length at both the proximal end (intragraft) and distal end (native outflow vein) to SG stability. This in addition to the length of stenosis determines the SG length chosen. Again, it is important to avoid caging potential future site of access that would use the brachial or basilic veins as outflow vessels. For the FLAIR SG, we predilate the stenosis to allow for full stent deployment and easy removal of the delivery sheath. There have been anecdotal cases of stent deployment in which the delivery sheath could not be removed or dislodged the stent during removal.
Fig. 2.
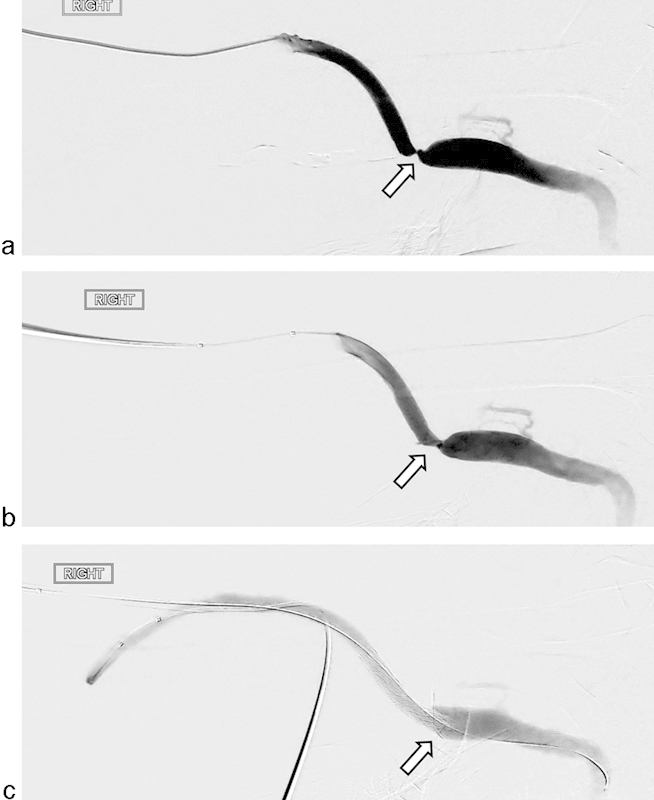
(a) A 35-year-old woman with a tight stenosis of the venous anastomosis (arrow) of a right brachial-axillary arteriovenous graft. (b) Minimal improvement (arrow) following angioplasty with a 7-mm balloon is noted. (c) There has been resolution of the stenosis after the placement of a flared FLAIR stent (8–12 mm diameter, 5 cm long). The flared component (arrow) allows better apposition to the wall of the relatively larger axillary vein lumen.
After deployment of the flared version of the FLAIR SG, the distal end of the SG is angioplastied with a larger balloon diameter to ensure apposition of the flared end to the native vein wall. The remainder of the stent is angioplastied using a balloon equal to or 1 mm greater than the SG diameter. A final angiogram is always performed to assess the caliber of the venous anastomosis poststent deployment and to verify improvement in flow.
The quality and quantity of published evidence for the use of anastomotic SG is growing. Two recently conducted randomized, prospective, multicenter controlled clinical trials, RENOVA and REVISE (FLAIR and Viabahn SGs, respectively), have shown that deployment of SGs at the venous anastomosis resulted in superior postintervention treatment area primary patency (TAPP) and overall access circuit primary patency (ACPP) at 6, 12, and 24 months as compared with PTA alone.23 24 25 26 Although both trials included patients with stenoses at the venous anastomosis, the REVISE trial also included shunts with complete thrombotic occlusion and stenoses at the elbow. The results from the FLAIR/RENOVA trials demonstrated SG ACPP at 6, 12, and 24 months of 38, 24, 9.5% versus PTA of 20, 10, 5.5%, respectively (p = 0.01).23 24 25 In addition, access circuit stenosis warranting reintervention within 24 months occurred significantly more often in the PTA group (83%) versus the SG group (63%; p < 0.001). The REVISE trial demonstrated similar results to the RENOVA trial, with SG ACPP at 6, 12, and 24 months of 43, 21, and 10% versus PTA ACPP of 29, 15, and 7% (p = 0.035) with SGs resulting in greater primary patency for both thrombotic and nonthrombotic patients.26 Interestingly, in the REVISE trial, prior intervention did not affect the outcomes of the SG group but predicted unfavorable outcomes for the PTA group. The absence of detected SG fractures, especially at the crossing of the elbow, highlighted another promising advancement of SG technology. Although the financial cost benefit of SGs versus PTA for venous anastomotic stenosis has yet to be determined, the REVISE trial estimated a cost reduction of $2,000 per patient in the SG arm over the course of the study.26 27
Recurrent Stenosis
Overutilization of stents has increased the incidence of in-stent stenosis in the HD population. In our practice, to maintain maximal luminal diameter and minimize procedural cost, we treat mild, hemodynamically significant in-stent restenosis with PTA using either high-pressure balloons such as the Conquest (Boston Scientific) or using cutting balloons (Boston Scientific) in refractory cases. For more severe cases, stents are required. The choice of BMS versus SGs for this indication is highly operator dependent, since no published data offer conclusive advantages of BMS versus SGs in this setting. The PTFE or Dacron covering of SGs excludes neointimal hyperplasia development and prevents migration of smooth muscle cells, acting as a barrier between the potentially thrombogenic wall and luminal blood flow.28 Therefore, we do not hesitate to rescue a poor PTA result with a SG. But SGs are no panacea and are prone to “edge stenosis” that tends to occur within 5 mm of each end of the SG, with neointimal formation from the ends of the stent migrating toward the center.29
Our staged approach to mild in-stent stenosis is subject to change with further support from the published data. A recent robust multicenter prospective clinical trial, RESCUE, evaluated PTA versus the Fluency SG for recurrent in-stent stenosis and demonstrated superiority of SGs.30 The 6-month postintervention TAPP was 65% for SGs versus 10% for PTA (p < 0.001), and the 6-month ACPP was 17 versus 3%, respectively (p < 0.001). Of note, superiority of SGs was demonstrated for both AVG and AVF, and did not affect postintervention lesion patency (central or peripheral). The study excluded thrombosed grafts and in-stent stenoses in the cephalic arch and elbow regions.
Cephalic Arch Stenosis
Cephalic arch stenosis is another frequent problem encountered in malfunctioning HD access, particularly in the setting of brachiocephalic fistulas for which the estimated prevalence is up to 40%.31 The management of cephalic stenosis is challenging due to the resistant nature of the stenosis, early restenosis, and high rupture rates during PTA.31 32 33 In addition, when PTA-induced rupture occurs, bleeding is difficult to manually compress, and large, axillary hematomas can cause significant morbidity and threaten access viability. For this reason, we take a delicate approach to the treatment of this entity with precautions similar to those employed during peripheral arterial PTA. We access with vascular sheaths large enough to deploy a rescue SG, should it be required to treat rupture. In addition, we maintain wire access across the cephalic arch when performing our post-PTA angiogram to allow for appropriate rescue interventions. In our experience, these precautions have not been as critical when performing angiography after PTA of other segments of the peripheral venous outflow.
When stents are required, our practice has seen a gradual shift from BMS toward Viabahn SGs for this indication, again related to the evolving published literature. A prospective, randomized study by Shemesh et al compared PTA with either SG or BMS for recurrent cephalic arch stenosis (within 3 months of successful PTA).34 Only patients with brachiocephalic fistulae were included. Six-month and 1-year patency rates for SG and BMS were 82 and 32% versus 39 and 0%, respectively (p = 0.002). Although the authors concluded that restenosis rates were significantly better for SG versus BMS, this study was limited by its extremely small size (only 12 and 13 patients in BMS and SG, respectively). However, another prospective, randomized, multicenter study is underway comparing outcomes between PTA and Viabahn SGs for cephalic arch stenosis and central venous stenosis/occlusions, with an expected completion date in early 2015. Given the reported high incidence of BMS fracture at the cephalic arch and within the subclavian vein, it remains to be seen if SGs are also at risk for fracture at these sites.
Finally, all cases of recurring or refractory cephalic arch stenosis are discussed at our multidisciplinary vascular access conference for consideration of possible future salvage surgical intervention. A recent study compared surgical transposition of recurring cephalic arch stenosis plus PTA with SGs. One-year primary patency was 39 versus 32% for surgical revision plus PTA versus SG, respectively, demonstrating equivalence of the treatment modalities.33
Exclusion of Aneurysms and Pseudoaneurysms
Aneurysms and pseudoaneurysm formations are significant complications of AV shunts that can potentially jeopardize access longevity. In addition, rare progressive enlargement due to repeated punctures may lead to compromise of the overlying skin and, if not addressed timely, rupture and death by exsanguination can occur. While aneurysms and pseudoaneurysms are frequently grouped together to describe enlargement of fistulas and grafts, our treatment approach to these two pathological entities differs. In both entities, outflow vein stenosis is thought to contribute by increasing intragraft or fistula pressure.35 36 37
A true aneurysm contains all three layers of the vessel wall—intima, media, and adventitia—and is the most common form of dilatation encountered in AV fistulas. In a native fistula, dialysis access usually remains functional despite gross enlargement and deformity of the access. Despite this appearance, we never recommend the use of SGs as a cosmetic treatment for AV fistulas. However, SGs may be indicated in cases of aneurysms causing frequent, recurrent shunt thrombosis, difficult access for dialysis, or compromise of the overlying skin.
A pseudoaneurysm, also referred to as false aneurysm, is the most common form of dilatation encountered with synthetic AV grafts, and usually results from a leaking hole in a vessel wall with a hematoma contained by the surrounding neointimal or fibrous tissue. This results from repeated punctures during dialysis and is usually limited to the area of the graft. We use SGs when signs of impending rupture are present (rapid increase in size or spontaneous bleeding), when there is threatened viability of overlying skin, or when the size of the pseudoaneurysm limits the availability of cannulation sites. Pseudoaneurysms can occur with both native fistulas and grafts when arterial anastomotic breakdown occurs, which constitutes a surgical emergency. Temporary placement of a high-compliance balloon across the arterial anastomosis may be necessary to bridge the gap for many minutes to perform emergent surgical intervention.
Endovascular exclusion of aneurysms or pseudoaneurysms requires adequate landing zones of at least 10 mm at both ends of the lesion to avoid the complications of endoleak and stent dislodgment leading to access thrombosis. At our institution, we typically deploy either a Fluency or a Viabahn SG for this indication. After stent deployment, we occasionally puncture and aspirate the excluded dilated segment with an 18-G needle to remove residual blood, and perform an angiogram with extended delayed imaging to rule out an endoleak (Fig. 3). The removal of residual blood seems to improve the cosmetic result and may reduce the risks associated with residual dead space in the excluded sac such as infection or endoleak. Type 3 endoleaks occur when SGs placed across cannulation zones are repeatedly punctured for dialysis and leakage into the excluded aneurysm or pseudoaneurysm recurs (Fig. 4).
Fig. 3.
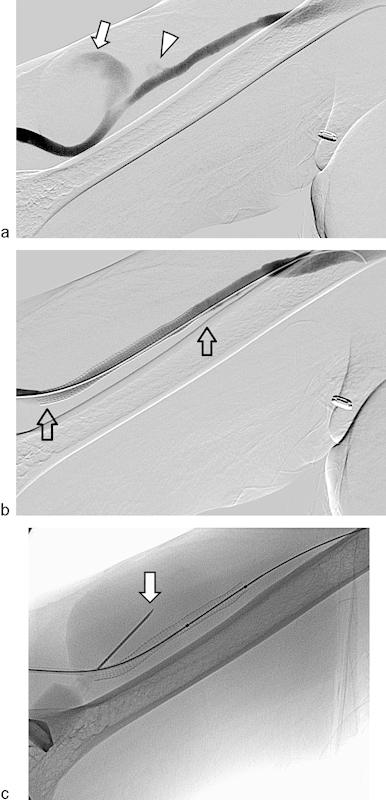
(a) A 59-year-old man with large (arrow) and small (arrowhead) aneurysms in the cannulation zone of a right brachiobasilic fistula. (b) A Viabahn stent graft (7 × 100 mm) (arrows) was used to exclude both aneurysms. (c) An 18-G needle (arrow) was used to aspirate the contents of the aneurysms to improve the cosmetic result and decrease the risks of infection and endoleak associated with repeated punctures for dialysis.
Fig. 4.
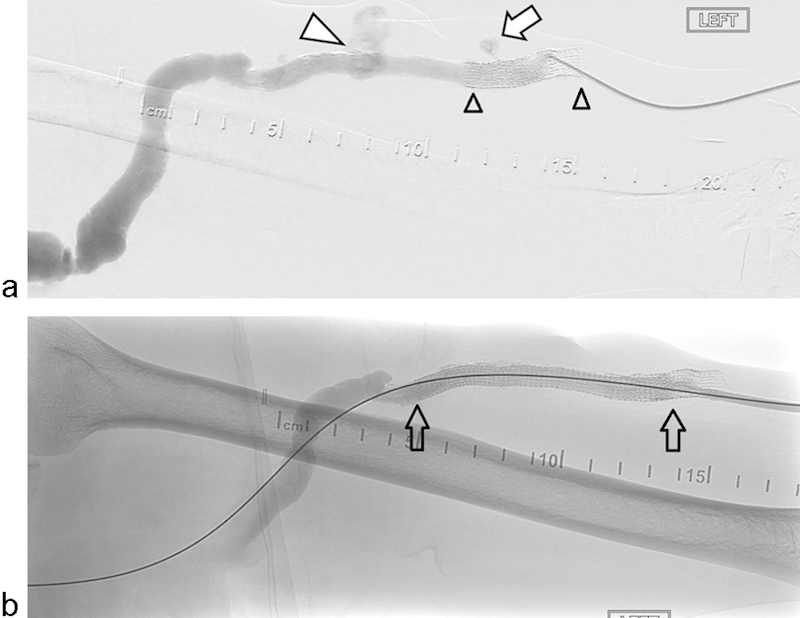
(a) A 65-year-old man with a right brachial–brachial arteriovenous graft presents with repeat episodes of thrombosis caused by a pseudoaneurysm (white arrowhead). In addition, a previously placed Viabahn stent graft (small black open arrowheads) placed for pseudoaneurysm exclusion exhibits a Type 3 endoleak (arrow) caused by dialysis access punctures. (b) Revision was performed with a new Viabahn stent graft (8 × 100 mm) (arrows). The new stent graft was intentionally overlapped with the prior Viabahn.
Repair of Angioplasty-Induced Vascular Rupture
Angioplasty-induced venous rupture is a common and well-known complication of AV fistulas and grafts. In most cases, external manual compression or prolonged tamponade with an angioplasty balloon at the rupture site controls extravasation and preserves the dialysis access. However, for extravasation not controlled by conservative measures or those that are inaccessible to manual compression, both BMS and SGs have been shown to be an effective bailout strategy to salvage access and control antegrade flow.38 39 The choice between devices is operator dependent in our practice. Although BMS may be effective for this indication (Fig. 5), most of our interventionalists prefer SGs, which have been reported to have better short-term results and superior patency rates.39
Fig. 5.
(a) A 45-year-old man with a tight stenosis (arrow) involving the venous anastomosis of a brachial–brachial arteriovenous graft. (b) Active extravasation (arrow) into the axilla immediately after angioplasty to 8 mm is noted. (c) There is complete cessation of extravasation after the placement of an Epic bare metal stent (8 × 40 mm) (arrow).
Central Venous Stenosis
Central venous stenosis or occlusion ipsilateral to a dialysis shunt is a relatively common problem with an incidence ranging from 4 to 40%.40 41 The most common etiology in this patient population is repeated placement of central venous catheters. The majority of the affected patients remain asymptomatic. However, in some cases, high venous pressure and blood flow reductions from limited collateral venous drainage compromise dialysis delivery. Consequences include development of dilated and tortuous collateral veins, and symptomatic ipsilateral upper extremity and facial edema.40 41
Treatment options depend on the location, severity, and chronicity of the stenosis. For mild-to-moderate stenoses, we use PTA as our first-line treatment option with early and close follow-up during dialysis. Stent placement for central venous lesions is generally reserved for cases of PTA failure, early recurrence within 3 months after initially successful PTA, or in cases of rupture after PTA. However, for severe central venous stenosis or occlusion, we commonly proceed with primary stent placement since immediate elastic recoil and early restenosis are common in our experience. Admittedly, literature support for this approach is sparse. PTA alone has demonstrated variable technical success ranging from 70 to 90%; however, this strategy has resulted in a primary patency at 6 months of only 23 to 63%,40 emphasizing the need for careful patient selection and a low threshold for stent utilization.
Central venous disease is often highly elastic, requiring a stent with high radial force. In addition, precise placement is essential to avoid caging branch vessels and prevent the stent from extending into the right atrium. Therefore, balloon-expandable stents are sometimes used for this indication to exploit their high radial force and precise placement with minimal foreshortening. Central venous stent placement has demonstrated very high technical success rates, approaching 100%, and low complications rates.40 A recent retrospective study evaluated long-term outcomes of SG placement in patients with symptomatic central venous lesions and ipsilateral dialysis accesses, and demonstrated 6, 12, and 36 month lesion patency rates of 60, 40, and 28%, and access patency rates of 96, 94, and 72%, respectively. For this study, the indications for SG placement were poor PTA results, rapid recurrence of stenoses, or total occlusion. It was concluded that SG placement in these clinical scenarios is associated with prolonged access patency.41
Conclusion
In the last two decades, there has been a dramatic increase in stent placement for dialysis access venous stenosis, in-stent stenosis, aneurysms and pseudoaneuryms, and angioplasty-induced vascular rupture. At this point, there is level 1 evidence for SG superiority over PTA for venous stenosis in AV grafts and in-stent stenosis in both AV grafts and AV fistulae. Given significant updates in evidence for stent use and considerable advancement in stent technology, we feel that an update of KDOQI clinical practice guidelines, which have not been revised in over 8 years, is in order. Although recent data for stent use in AV fistula lesions are promising, at present, we do not routinely deploy stents in this setting as a primary treatment. Until further large prospective, randomized controlled trials are conducted to assess primary stenting of venous stenosis in the setting of AV fistulas, our preference remains PTA as a primary treatment for AV fistula dysfunction.
References
- 1.U.S. Renal Data System . Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2010. USRDS 2010 Annual Data Report. Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. [Google Scholar]
- 2.Gilbertson D T, Liu J, Xue J L. et al. Projecting the number of patients with end-stage renal disease in the United States to the year 2015. J Am Soc Nephrol. 2005;16(12):3736–3741. doi: 10.1681/ASN.2005010112. [DOI] [PubMed] [Google Scholar]
- 3.Konner K, Hulbert-Shearon T E, Roys E C, Port F K. Tailoring the initial vascular access for dialysis patients. Kidney Int. 2002;62(1):329–338. doi: 10.1046/j.1523-1755.2002.00436.x. [DOI] [PubMed] [Google Scholar]
- 4.The economic cost of ESRD, vascular access procedures, and Medicare spending for alternative modalities of treatment. Am J Kidney Dis. 1997;30:160–177. doi: 10.1016/s0272-6386(97)90187-6. [DOI] [PubMed] [Google Scholar]
- 5.Vassalotti J A, Jennings W C, Beathard G A. et al. Fistula first breakthrough initiative: targeting catheter last in fistula first. Semin Dial. 2012;25(3):303–310. doi: 10.1111/j.1525-139X.2012.01069.x. [DOI] [PubMed] [Google Scholar]
- 6.The Fistula First Breakthrough Initiative Available at: http://esrdncc.org/ffcl/. Accessed December 20, 2012
- 7.Lacson E Jr, Wang W, Hakim R M, Teng M, Lazarus J M. Associates of mortality and hospitalization in hemodialysis: potentially actionable laboratory variables and vascular access. Am J Kidney Dis. 2009;53(1):79–90. doi: 10.1053/j.ajkd.2008.07.031. [DOI] [PubMed] [Google Scholar]
- 8.Xue H, Ix J H, Wang W. et al. Hemodialysis access usage patterns in the incident dialysis year and associated catheter-related complications. Am J Kidney Dis. 2013;61(1):123–130. doi: 10.1053/j.ajkd.2012.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee T, Roy-Chaudhury P. Advances and new frontiers in the pathophysiology of venous neointimal hyperplasia and dialysis access stenosis. Adv Chronic Kidney Dis. 2009;16(5):329–338. doi: 10.1053/j.ackd.2009.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yevzlin A, Asif A. Stent placement in hemodialysis access: historical lessons, the state of the art and future directions. Clin J Am Soc Nephrol. 2009;4(5):996–1008. doi: 10.2215/CJN.04040808. [DOI] [PubMed] [Google Scholar]
- 11.Chan M R, Bedi S, Sanchez R J. et al. Stent placement versus angioplasty improves patency of arteriovenous grafts and blood flow of arteriovenous fistulae. Clin J Am Soc Nephrol. 2008;3(3):699–705. doi: 10.2215/CJN.04831107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vogel P M, Parise C. Comparison of SMART stent placement for arteriovenous graft salvage versus successful graft PTA. J Vasc Interv Radiol. 2005;16(12):1619–1626. doi: 10.1097/01.RVI.0000179792.23867.01. [DOI] [PubMed] [Google Scholar]
- 13.Zaleski G X, Funaki B, Rosenblum J, Theoharis J, Leef J. Metallic stents deployed in synthetic arteriovenous hemodialysis grafts. AJR Am J Roentgenol. 2001;176(6):1515–1519. doi: 10.2214/ajr.176.6.1761515. [DOI] [PubMed] [Google Scholar]
- 14.Rhodes E S, Silas A M. Dialysis needle puncture of Wallgrafts placed in polytetrafluoroethylene hemodialysis grafts. J Vasc Interv Radiol. 2005;16(8):1129–1134. doi: 10.1097/01.RVI.0000167852.14245.05. [DOI] [PubMed] [Google Scholar]
- 15.Vesely T M. Use of stent grafts to repair hemodialysis graft-related pseudoaneurysms. J Vasc Interv Radiol. 2005;16(10):1301–1307. doi: 10.1097/01.RVI.0000175903.38810.13. [DOI] [PubMed] [Google Scholar]
- 16.Pandolfe L R, Malamis A P, Pierce K, Borge M A. Treatment of hemodialysis graft pseudoaneurysms with stent grafts: institutional experience and review of the literature. Semin Intervent Radiol. 2009;26(2):89–95. doi: 10.1055/s-0029-1222451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ayus J C, Sheikh-Hamad D. Silent infection in clotted hemodialysis access grafts. J Am Soc Nephrol. 1998;9(7):1314–1317. doi: 10.1681/ASN.V971314. [DOI] [PubMed] [Google Scholar]
- 18.Delorme J M, Guidoin R, Canizales S. et al. Vascular access for hemodialysis: pathologic features of surgically excised ePTFE grafts. Ann Vasc Surg. 1992;6(6):517–524. doi: 10.1007/BF02000823. [DOI] [PubMed] [Google Scholar]
- 19.National Kidney Foundation KDOQI clinical practice guidelines and clinical practice recommendations for 2006. Updates: Hemodialysis adequacy, peritoneal dialysis adequacy and vascular access Available at: http://www.kidney.org/sites/default/files/docs/12-50-0210_jag_dcp_guidelines-hd_oct06_sectiona_ofc.pdf. Accessed April 15, 2015
- 20.Quinn S F, Schuman E S, Demlow T A. et al. Percutaneous transluminal angioplasty versus endovascular stent placement in the treatment of venous stenoses in patients undergoing hemodialysis: intermediate results. J Vasc Interv Radiol. 1995;6(6):851–855. doi: 10.1016/s1051-0443(95)71200-3. [DOI] [PubMed] [Google Scholar]
- 21.Beathard G A. Gianturco self-expanding stent in the treatment of stenosis in dialysis access grafts. Kidney Int. 1993;43(4):872–877. doi: 10.1038/ki.1993.122. [DOI] [PubMed] [Google Scholar]
- 22.Hoffer E K, Sultan S, Herskowitz M M, Daniels I D, Sclafani S JA. Prospective randomized trial of a metallic intravascular stent in hemodialysis graft maintenance. J Vasc Interv Radiol. 1997;8(6):965–973. doi: 10.1016/s1051-0443(97)70695-x. [DOI] [PubMed] [Google Scholar]
- 23.Haskal Z J, Trerotola S, Dolmatch B. et al. Stent graft versus balloon angioplasty for failing dialysis-access grafts. N Engl J Med. 2010;362(6):494–503. doi: 10.1056/NEJMoa0902045. [DOI] [PubMed] [Google Scholar]
- 24.Haskal Z J. Twelve month results of the RENOVA trial: a prospective multicenter randomized, concurrently-controlled comparison of the Flair® endovascular stent graft vs. balloon angioplasty in dialysis access grafts. J Vasc Interv Radiol. 2013;24(4):S5. [Google Scholar]
- 25.Haskal Z. 24-month final results from the RENOVA study: a randomized controlled comparison of stent grafts and balloon angioplasty for dialysis access graft preservation. J Vasc Interv Radiol. 2014;25(3):S6. [Google Scholar]
- 26.Vesely T DaCanzo W Behrend T Dwyer A Aruny J REVISE Clinical Trial: Presentation at the ASDIN 10th Annual Scientific Meeting; 2014
- 27.Salman L, Asif A. Stent graft for nephrologists: concerns and consensus. Clin J Am Soc Nephrol. 2010;5(7):1347–1352. doi: 10.2215/CJN.02380310. [DOI] [PubMed] [Google Scholar]
- 28.Sick P B, Brosteanu O, Niebauer J, Hehrlein C, Schuler G. Neointima formation after stent implantation in an experimental model of restenosis: polytetrafluoroethylene-covered versus uncovered stainless steel stents. Heart Dis. 2002;4(1):18–25. doi: 10.1097/00132580-200201000-00004. [DOI] [PubMed] [Google Scholar]
- 29.Dolmatch B L, Tio F O, Li X D, Dong Y H. Patency and tissue response related to two types of polytetrafluoroethylene-covered stents in the dog. J Vasc Interv Radiol. 1996;7(5):641–649. doi: 10.1016/s1051-0443(96)70822-9. [DOI] [PubMed] [Google Scholar]
- 30.Falk A, Maya I D, Yevzlin A S. Six-month results of the RESCUE trial: FLUENCY® PLUS Endovascular Stent Graft versus PTA for In-stent Restenosis. J Vasc Interv Radiol. 2014;25(4):661. [Google Scholar]
- 31.Rajan D K, Clark T WI, Patel N K, Stavropoulos S W, Simons M E. Prevalence and treatment of cephalic arch stenosis in dysfunctional autogenous hemodialysis fistulas. J Vasc Interv Radiol. 2003;14(5):567–573. doi: 10.1097/01.rvi.0000071090.76348.bc. [DOI] [PubMed] [Google Scholar]
- 32.Kian K, Asif A. Cephalic arch stenosis. Semin Dial. 2008;21(1):78–82. doi: 10.1111/j.1525-139X.2007.00387.x. [DOI] [PubMed] [Google Scholar]
- 33.Kian K, Unger S W, Mishler R, Schon D, Lenz O, Asif A. Role of surgical intervention for cephalic arch stenosis in the “fistula first” era. Semin Dial. 2008;21(1):93–96. doi: 10.1111/j.1525-139X.2007.00388.x. [DOI] [PubMed] [Google Scholar]
- 34.Shemesh D Goldin I Zaghal I Berlowitz D Raveh D Olsha O Angioplasty with stent graft versus bare stent for recurrent cephalic arch stenosis in autogenous arteriovenous access for hemodialysis: a prospective randomized clinical trial J Vasc Surg 20084861524–1531., 1531.e1–1531.e2 [DOI] [PubMed] [Google Scholar]
- 35.Barshes N R, Annambhotla S, Bechara C. et al. Endovascular repair of hemodialysis graft-related pseudoaneurysm: an alternative treatment strategy in salvaging failing dialysis access. Vasc Endovascular Surg. 2008;42(3):228–234. doi: 10.1177/1538574408314443. [DOI] [PubMed] [Google Scholar]
- 36.Shemesh D, Goldin I, Zaghal I, Berelowitz D, Verstandig A G, Olsha O. Stent graft treatment for hemodialysis access aneurysms. J Vasc Surg. 2011;54(4):1088–1094. doi: 10.1016/j.jvs.2011.03.252. [DOI] [PubMed] [Google Scholar]
- 37.Pasklinsky G, Meisner R J, Labropoulos N. et al. Management of true aneurysms of hemodialysis access fistulas. J Vasc Surg. 2011;53(5):1291–1297. doi: 10.1016/j.jvs.2010.11.100. [DOI] [PubMed] [Google Scholar]
- 38.Funaki B, Szymski G X, Leef J A, Rosenblum J D, Burke R, Hackworth C A. Wallstent deployment to salvage dialysis graft thrombolysis complicated by venous rupture: early and intermediate results. AJR Am J Roentgenol. 1997;169(5):1435–1437. doi: 10.2214/ajr.169.5.9353476. [DOI] [PubMed] [Google Scholar]
- 39.Dale J D, Dolmatch B L, Duch J M, Winder R, Davidson I J. Expanded polytetrafluoroethylene-covered stent treatment of angioplasty-related extravasation during hemodialysis access intervention: technical and 180-day patency. J Vasc Interv Radiol. 2010;21(3):322–326. doi: 10.1016/j.jvir.2009.10.042. [DOI] [PubMed] [Google Scholar]
- 40.Kundu S. Review of central venous disease in hemodialysis patients. J Vasc Interv Radiol. 2010;21(7):963–968. doi: 10.1016/j.jvir.2010.01.044. [DOI] [PubMed] [Google Scholar]
- 41.Verstandig A G Berelowitz D Zaghal I et al. Stent grafts for central venous occlusive disease in patients with ipsilateral hemodialysis access J Vasc Interv Radiol 20132491280–1287., quiz 1288 [DOI] [PubMed] [Google Scholar]


