Abstract
Lipodystrophy is a group of metabolic disorders, possibly caused by autoimmune disease. In this report, we describe a case of adult-onset acquired partial lipodystrophy accompanied by rheumatoid arthritis without a family history. Interestingly, immunohistochemical staining revealed dense infiltration of IL-27-producing cells as well as MMP-7-and MMP-28-expressing cells, both of which have been reported to facilitate the development of autoimmune disease. Our present case might suggest possible mechanisms for acquired partial lipodystrophy.
Key Words: Acquired partial lipodystrophy, IL-27, MMP-7, MMP-28
Introduction
Lipodystrophy is a group of metabolic disorders, which can be divided into generalized, partial or local type [1]. Although the exact pathogenesis of lipodystrophy is still unknown, autoimmunity could be a cause, particularly noted in acquired partial lipodystrophy (APL; Barraquer-Simons syndrome) and acquired generalized lipodystrophy (Lawrence syndrome) [1]. In this report, we describe a case of adult-onset APL accompanied by rheumatoid arthritis (RA) and with absence of a family history. In addition, we employed immunohistochemical staining for IL-27 as well as MMP-7 and MMP-28, both of which have been reported to facilitate the development of autoimmune scleroderma [2, 3, 4, 5].
Case Report
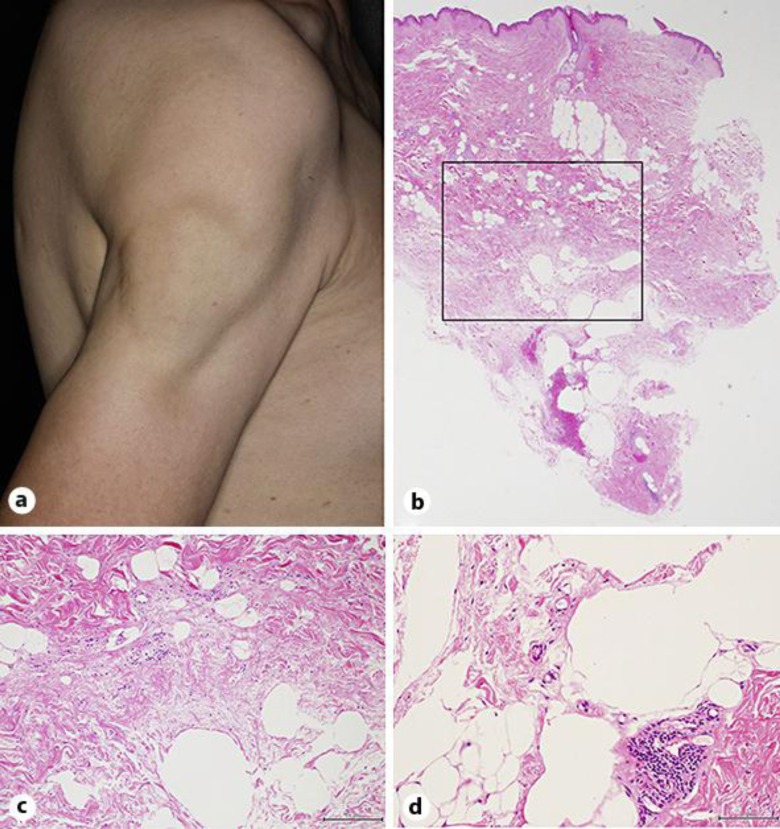
A 54-year-old Japanese woman visited our outpatient clinic with a 20-year history of loss of subcutaneous fat on her left upper limb. She had been treated for hypothyroidism for 22 years and for chronic RA for 11 years. There was no family history of lipodystrophy. On her initial visit, physical examination revealed multifocal loss of subcutaneous fat on her bilateral upper limbs, shoulders, back, abdomen and left lower limb (fig. 1a). A biopsy specimen from the right shoulder revealed a decrease in adipose tissue (fig. 1b), a prominent increase in collagen fibers (fig. 1c) and dense infiltration of lymphocytes around the vesicles (fig. 1d). A full blood count was within the normal range. The biochemical profile revealed increased levels of anti-CCP (31.6 U/ml), MMP-3 (148 ng/ml) and CH50 (72.4 U/ml) as well as prominently decreased levels of TSH (0.23 μU/ml). The serum levels of leptin and adiponectin were within the normal range. From the above findings, we diagnosed the patient as having adult-onset APL accompanied by RA without a family history.
Fig. 1.
a Multifocal loss of subcutaneous fat on the right upper limb and shoulder. In the subcutaneous area, there was a decrease in adipose tissue (b), a prominent increase in collagen fibers (c) and dense infiltration of lymphocytes around the vesicles (d). Original magnification: b ×50, c ×200, d ×400.
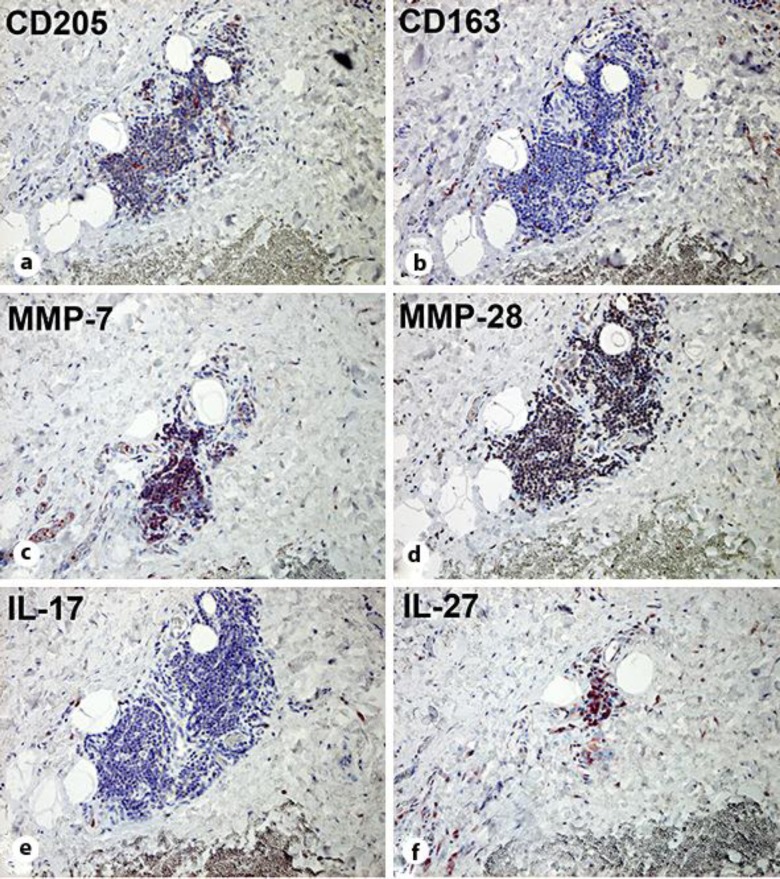
To investigate the immunological background of the local skin area, we employed immunohistochemical staining, which revealed that these infiltrating lymphocytes were mainly composed of CD205+ matured dendritic cells (fig. 2a), and these cells produced MMP-7 (fig. 2c), MMP-28 (fig. 2d) and IL-27 (fig. 2f). CD163+ macrophages (fig. 2b) and IL-17-producing cells (fig. 2e) were scattered in the same area.
Fig. 2.
Paraffin-embedded tissue samples from the right shoulder were deparaffinized and stained with anti-CD205 Ab (a), anti-CD163 Ab (b), anti-MMP-7 Ab (c), anti-MMP-28 Ab (d), anti-IL-17 Ab (e) or anti-IL-27 Ab (f). The sections were developed with liquid permanent red. Original magnification: ×200.
Discussion
In the subcutaneous sclerosing areas of APL, dense infiltrating leukocytes, most of which were CD205+ matured dendritic cells, were observed in our present case. Interestingly, in the same areas, IL-27-producing cells as well as MMP-7-and MMP-28-expressing cells were prominent. Since IL-27 has been reported to facilitate the development of various autoimmune diseases, such as psoriasis, systemic lupus erythematosus and scleroderma, and since MMP-7 and MMP-28 have also been reported to contribute to autoimmune diseases [2, 3, 4, 5], our present immunohistochemical findings might suggest that APL is an autoimmune-related disorder.
IL-27, a member of the IL-12 family, is composed of EBI3 and p28 subunits and activates both STAT1 and STAT3 through a distinct IL-27 receptor [6]. IL-27 is mainly produced by activated antigen-presenting cells and is involved in priming T helper 1 (Th1) cells [3, 6, 7]. Recently, IL-27 has been reported in various Th1/Th17-mediated inflammatory diseases and autoimmune diseases [3, 4, 8]. For instance, patients with scleroderma show increased serum levels of IL-27, which suggests that IL-27 contributes to the pathogenesis of scleroderma [4]. As previously reported by us, in the lesional skin of autoimmune diseases such as systemic lupus erythematosus, IL-27-producing cells could be observed within the epidermal-dermal junction area [8]. These reports suggest that the IL-27-producing cells could be a center of inflammation in the lesional skin of autoimmune diseases. Concerning our present case, IL-27-producing cells were detected in the sclerosed adipose tissue, which suggested that IL-27 might be one of the factors that facilitate the liposclerosis of APL.
MMP-7 is involved in the degradation of extracellular matrix protein in the remodeling of fibrotic tissue in systemic scleroderma [5]. MMP-28 plays a role in the remodeling of the newly formed basement membrane during wound repair [9]. In dermal lesions, as previously reported by us, both MMP-7-and MMP-28-expressing cells were detected in the perivascular areas of morphea and lichen sclerosus et atrophicus [2]. Although the precise mechanisms of MMP-7 and MMP-28 in scleroderma are still unknown, these reports suggested the possible contribution of these MMPs to the pathogenesis of this sclerosing disease.
In this report, we describe a case of adult-onset APL accompanied by RA without a family history. Interestingly, biopsy specimens from areas with decreased adipocytes were densely infiltrated with CD205+ matured dendritic cells, which could be IL-27-producing, MMP-7-and MMP-28-expressing cells. Our present case might suggest possible mechanisms for APL. Since we present a single case, further cases are needed to gain additional insight into the pathomechanisms of APL.
References
- 1.Nolis T. Exploring the pathophysiology behind the more common genetic and acquired lipodystrophies. J Hum Genet. 2014;59:16–23. doi: 10.1038/jhg.2013.107. [DOI] [PubMed] [Google Scholar]
- 2.Kakizaki A, Fujimura T, Furudate S, Kambayashi Y, Aiba S. Immunohistochemical similarities between lichen sclerosus et atrophicus and morphea: a case study. Case Rep Dermatol. 2015;7:39–45. doi: 10.1159/000381010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shibata S, Tada Y, Kanda N, Nashiro K, Kamata M, Karakawa M, Miyagaki T, Kai H, Saeki H, Shirakata Y, Watanabe S, Tamaki K, Sato S. Possible roles of IL-27 in the pathogenesis of psoriasis. J Invest Dermatol. 2010;130:1034–1039. doi: 10.1038/jid.2009.349. [DOI] [PubMed] [Google Scholar]
- 4.Yoshizaki A, Yanaba K, Iwata Y, Komura K, Ogawa A, Muroi E, Ogawa F, Takenaka M, Shimizu K, Hasegawa M, Fujimoto M, Sato S. Elevated serum interleukin-27 levels in patients with systemic sclerosis: association with T cell, B cell and fibroblast activation. Ann Rheum Dis. 2011;70:194–200. doi: 10.1136/ard.2009.121053. [DOI] [PubMed] [Google Scholar]
- 5.Moinzadeh P, Krieg T, Hellmich M, Brinckmann J, Neumann E, Müller-Ladner U, Kreuter A, Dumitrescu D, Rosenkranz S, Hunzelmann N. Elevated MMP-7 levels in patients with systemic sclerosis: correlation with pulmonary involvement. Exp Dermatol. 2011;20:770–773. doi: 10.1111/j.1600-0625.2011.01321.x. [DOI] [PubMed] [Google Scholar]
- 6.Pflanz S, Hibbert L, Mattson J, Rosales R, Vaisberg E, Bazan JF, Phillips JH, McClanahan TK, de Waal Malefyt R, Kastelein RA. WSX-1 and glycoprotein 130 constitute a signal-transducing receptor for IL-27. J Immunol. 2004;172:2225–2231. doi: 10.4049/jimmunol.172.4.2225. [DOI] [PubMed] [Google Scholar]
- 7.Trinchieri G, Pflanz S, Kastelein RA. The IL-12 family of heterodimeric cytokines: new players in the regulation of T cell responses. Immunity. 2003;19:641–644. doi: 10.1016/s1074-7613(03)00296-6. [DOI] [PubMed] [Google Scholar]
- 8.Tojo G, Fujimura T, Kambayashi Y, Mizuashi M, Aiba S. Systemic lupus erythematosus accompanied by psoriasis induces IL-27-producing cells in both affected areas of the skin. Case Rep Dermatol. 2012;4:181–185. doi: 10.1159/000342803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Illman SA, Lohi J, Keski-Oja J. Epilysin (MMP-28) – structure, expression and potential functions. Exp Dermatol. 2008;17:897–907. doi: 10.1111/j.1600-0625.2008.00782.x. [DOI] [PubMed] [Google Scholar]