Abstract
Background
Impairment in instrumental activities of daily living (IADL) emerges in the transition from mild cognitive impairment (MCI) to Alzheimer’s disease (AD) dementia. Some IADL scales are sensitive to early deficits in MCI, but none have been validated for detecting subtle functional changes in clinically normal (CN) elderly at risk for AD.
Methods
Data from 624 subjects participating in the Alzheimer’s Disease Neuroimaging Initiative and 524 subjects participating in the Massachusetts Alzheimer’s Disease Research Center, which are two large cohorts including CN elderly and MCI subjects, were used to determine which Functional Activities Questionnaire items best discriminate between and predict progression from CN to MCI.
Results
We found that “Remembering appointments” and “assembling tax records” best discriminated between CN and MCI subjects, while worse performance on “paying attention and understanding a TV program”, “paying bills/balancing checkbook”, and “heating water and turning off the stove” predicted greater hazard of progressing from a diagnosis of CN to MCI.
Conclusions
These results demonstrate that certain questions are especially sensitive in detecting the earliest functional changes in CN elderly at risk for AD. As the field moves toward earlier intervention in preclinical AD, it is important to determine which IADL changes can be detected at that stage and track decline over time.
Keywords: Activities of daily living, Alzheimer’s disease, clinical assessment, daily functioning, clinically normal elderly, mild cognitive impairment
Introduction
Impairment in activities of daily living (ADL) is a major feature of Alzheimer’s disease (AD) dementia and a significant source of caregiver burden. Basic ADL consist of activities such as dressing, grooming, bathing, toileting, and feeding oneself, while instrumental ADL (IADL) consist of activities such as preparing meals, performing household chores, running errands, traveling outside of one’s neighborhood, keeping track of one’s schedule and appointments, managing the finances, and doing the taxes.
Many IADL scales have been validated for the assessment of functional impairment in dementia, but few have been shown to be helpful in earlier disease stages such as amnestic mild cognitive impairment (MCI) [1]. Indeed, the total impairment score from the Functional Activities Questionnaire (FAQ) [2], a commonly used subjective IADL scale, has been helpful in MCI, but has usually failed to demonstrate early functional changes in clinically normal (CN) elderly at risk for AD due to significant floor effects noted on the total score of CN individuals [3,4].
However, the notion that IADL impairment starts only at the stage of mild dementia has been challenged. Several studies using large well-characterized cohorts have shown that mild impairment in IADL is already present at the stage of MCI, preceding mild dementia [3–5]. This is also reflected in the revised criteria for MCI that allow for the presence of mild IADL changes [6]. IADL depend on multiple cognitive functions, which are affected early on in the AD trajectory; therefore, it is not surprising that changes in IADL could be detected early on if sensitive enough assessments are used [1,3,7]. However, in the recently issued guidance by the Food and Drug Administration (FDA) for the design of clinical trials in early AD, recommendations were made to use a global functioning scale (combining cognition and IADL) at the stage of prodromal AD (MCI due to AD) and a sensitive cognitive measure alone at the stage of preclinical AD because of the lack of sensitive IADL scales for those early AD stages [8]. Therefore, better IADL scales, capturing vital concerns of individuals with early AD, need to be developed in order to address this important gap.
A study employing the Alzheimer’s Disease Neuroimaging Initiative (ADNI) data, assessed individual FAQ items and showed that “remembering appointments” and “assembling tax records” were most sensitive in differentiating CN from MCI subjects at baseline [5]. However, this study did not adjust for various covariates and did not determine the longitudinal potential of those items in predicting disease progression. We therefore decided to extend these analyses in the ADNI cohort, as well as replicate them in a separate well-characterized cohort from the Massachusetts Alzheimer’s Disease Research Center (MADRC). The objective of the current study was to determine which of the 10 FAQ items are most sensitive to early IADL changes by assessing which items best discriminate between CN and MCI diagnoses cross-sectionally and which items best predict longitudinal progression from CN to MCI after adjusting for important demographic characteristics. We hypothesized that items which involve more complex tasks that rely on multiple cognitive functions (ex: managing the finances) and items that depend on intact memory (ex: remembering appointments), which is affected the earliest in AD, will emerge from these analyses. The results of the current study could then serve as the basis for the development of a more sensitive IADL scale for preclinical AD.
Methods
Subjects
The study sample consisted of two separate cohorts. For one cohort, data were obtained from the ADNI study (adni.loni.usc.edu, PI Michael W. Weiner), a large multi-center, observational, biomarker study previously described in detail [3,9].
For the other cohort, data were obtained from the MADRC clinical core longitudinal research cohort at a single site previously described in detail [10]. The MADRC is one of 29 National Institute on Aging Alzheimer’s Disease Centers (ADC) with each center collecting longitudinal clinical and biomarker data from its subjects. Annual evaluations follow the ADC Uniform Data Set (UDS) protocol and consist of a standard medical history, neurological exam, neuropsychological test battery, and the Clinical Dementia Rating (CDR) [11,12].
Six hundred and twenty four subjects (229 CN, 395 MCI) participating in ADNI evaluated every 6 to 12 months, and 524 subjects (335 CN, 189 MCI) participating in the MADRC longitudinal cohort evaluated annually were included in the current analyses. The two cohorts were analyzed separately.
ADNI and MADRC subjects at baseline were generally in good health and medically stable, and had a study partner able to provide collateral information about the subject’s daily functioning, cognition, and behavior. ADNI subjects at baseline were ages 55 to 90 (inclusive), did not have significant cerebrovascular disease and had a Modified Hachinski Ischemic Score [13] ≤ 4, and did not have active psychiatric disorders and had a Geriatric Depression Scale, short form [14] ≤ 5. In contrast, MADRC subjects at baseline were ages 43 to 95 years old (inclusive), and there were no specific cerebrovascular or psychiatric exclusion criteria for those subjects.
For ADNI, subjects were assigned to diagnostic groups (CN or amnestic MCI) by site investigators at baseline as previously described [3,9]. CN subjects had a CDR [15] global score of 0, Mini-Mental State Examination (MMSE) [16] score of 25–30 (inclusive), and no significant memory impairment (performed within 1.5 standard deviations of education adjusted cut-off scores on the delayed recall portion of one Logical Memory story (LM-IIa) of the Wechsler Memory Scale-Revised (WMS-R) [17]). MCI subjects were amnestic, single or multiple domain, had a CDR global score of 0.5 and memory box score ≥ 0.5, MMSE score of 24–30 (inclusive), a memory complaint, objective memory loss on the WMS-R LM-IIa, essentially preserved IADL (no cut-off on a specific test was used to determine this; it was based on qualitative clinical judgment by the site investigator), and were not demented.
For MADRC, subjects were assigned to diagnostic groups (CN or amnestic MCI) by an experienced clinician and then a consensus diagnosis was made. Diagnoses were based on clinical history, UDS neuropsychological test battery results, and the CDR. However, unlike in ADNI, strict cut-offs for neuropsychological tests were not followed to determine diagnosis. CN subjects performed normally on neuropsychological testing in all domains and the majority (92%) had a CDR global score of 0. MCI subjects amnestic, single or multiple domain, had subjective memory complaints (either by self or informant report), objective memory impairment on either the WMS-R LM-IIa, the Free and Cued Selective Reminding Test [18], or the California Verbal Learning Test [19], essentially preserved IADL (determined by a clinician without a strict cut-off), and did not meet criteria for dementia.
The study was approved by the Institutional Review Board (IRB) of each participating ADNI site and by the Partners IRB for the MADRC. Written informed consent was obtained from all subjects and study partners prior to initiation of any study procedures in accordance with local IRB guidelines.
Clinical assessments
The Functional Activities Questionnaire (FAQ) is a subjective scale consisting of 10 items assessing IADL [2]. It is administered to an informant. The score range for each item is 0–3 (higher scores indicate greater impairment; 0 = normal or never did but could do now; 1 = has difficulty but does by self or never did but would have difficulty now; 2 = requires assistance; 3 = dependent). There is no established cut-off score for IADL impairment on the FAQ. However, one study reported that a total FAQ score (sum of all 10 item scores; range 0–30) of ≥ 6 is suggestive of functional impairment [20]. Moreover, recent studies have shown that the total FAQ score can discriminate well between CN, MCI, and mild AD dementia subjects [3,4].
Statistical analyses
Statistical and graphical analyses were performed using SAS Version 9.3 and JMP Pro Version 10. We performed a parallel set of analyses on the ADNI and MADRC cohorts with the intention of replicating the results in two independent cohorts.
Cross-sectional analyses
In order to determine which FAQ items best differentiated subjects with baseline diagnoses of CN versus MCI, we conducted a backward elimination (cutoff p≤0.01) linear discriminant analysis of the two groups using all 10 FAQ items as the initial pool of discriminators. Covariates associated with diagnosis (see Table 1) were included in the model—baseline age, sex, years of education, and the American National Adult Reading Test intelligence quotient (AMNART IQ) [21] (an estimate of premorbid intelligence, serving as a proxy of cognitive reserve). Because the FAQ items have only a few discrete values, which may violate the normality assumptions of discriminant analyses, backward elimination logistic regression, which does not require that assumption, was conducted to confirm the results of the discriminant analysis using all the previous discriminator variables and covariates as predictors of a diagnosis of CN versus MCI.
Table 1.
Baseline demographics and characteristics of subjects.
| Cohort | ADNI | MADRC | ||||
|---|---|---|---|---|---|---|
| Group | All | CN | MCI | All | CN | MCI |
| n | 624 | 229 | 395 | 524 | 335 | 189 |
| Age | 75.3 ± 6.7† | 76.0 ± 5.0 | 74.8 ± 7.4 | 72.6 ± 9.7*† | 70.1 ± 9.8 | 76.9 ± 8.0 |
| Sex (% male) | 59.8%**† | 52.0% | 64.3% | 35.5%*† | 28.7% | 47.6% |
| Education | 15.8 ± 3.0 | 16.0 ± 2.9 | 15.7 ± 3.1 | 16.1 ± 2.6 | 16.3 ± 2.4 | 15.7 ± 2.9 |
| AMNART IQ | 118.2 ± 11.4* | 121.1 ± 10.6 | 116.6 ± 11.5 | 121.8 ± 8.8* | 123.0 ± 7.5 | 119.5 ± 10.4 |
| MMSE | 27.8 ± 1.8* | 29.1 ± 1.0 | 27.0 ± 1.8 | 28.5 ± 2.0* | 29.2 ± 1.0 | 27.2 ± 2.6 |
| CDR sum of boxes | 1.0 ± 1.0*† | 0.0 ± 0.1 | 1.6 ± 0.9 | 0.8 ± 1.2*† | 0.1 ± 0.3 | 2.0 ± 1.1 |
ADNI (Alzheimer’s Disease Neuroimaging Initiative), AMNART IQ (American National Adult Reading Test intelligence quotient), CDR (Clinical Dementia Rating), CN (clinically normal), MADRC (Massachusetts Alzheimer’s Disease Research Center), MCI (mild cognitive impairment), MMSE (Mini-Mental State Examination).
All values represent mean ± standard deviation (except n and sex).
p<0.001 for CN vs. MCI within cohort.
p<0.01 for CN vs. MCI within cohort.
p<0.001 between cohorts.
Longitudinal analyses
We employed Cox proportional hazards regression models to assess time to change in diagnosis from a baseline diagnosis of CN to an endpoint diagnosis of MCI. Subjects who remained stable at CN were treated in the analyses as “censored” observations providing partial information on time to change in diagnosis (i.e., we at least know they had not transitioned to a diagnosis of MCI up until the time of their last study visit). Predictors were tested in a backward elimination algorithm (cutoff p≤0.01). The initial pool of predictors in the Cox regressions was the same as that used in the cross-sectional analyses. After backward elimination produced an optimal subset of predictors, the validity of the proportional hazard model assumption was tested for each of the retained predictors using a Kolmogorov test comparing residuals with simulations under a null hypothesis.
Results
Table 1 provides baseline demographics and characteristics of all subjects and for each diagnostic group (CN, MCI) by cohort. Within the ADNI and MADRC cohorts, there were significant differences between diagnostic groups for MMSE, CDR Sum of Boxes, and AMNART in expected directions. For both cohorts, there was a significantly higher proportion of males for the MCI than CN group. For the MADRC cohort, the MCI group was significantly older than the CN group. These latter differences were among those adjusted for in our analyses. ADNI subjects were significantly older than MADRC subjects (driven by the CN group), had a significantly higher proportion of males, and had significantly lower CDR Sum of Boxes scores.
Table 2 shows the baseline individual FAQ item scores and total FAQ score. For both the ADNI and MADRC cohorts, coefficient alpha (“Cronbach’s alpha”) for the 10 FAQ items was moderately high, just under 0.9, with the “heating water and turning off the stove” item having the lowest item total correlation reflecting the fact that it was skewed toward zero for both the CN and MCI more so than was any other FAQ item.
Table 2.
Baseline individual FAQ item and total FAQ score (mean ± standard deviation).
| Cohort | ADNI | MADRC | ||||
|---|---|---|---|---|---|---|
| FAQ Items | All | CN | MCI | All | CN | MCI |
| “Paying bills/balancing checkbook”* | 0.35 ± 0.74 | 0.03 ± 0.24 | 0.53 ± 0.87 | 0.16 ± 0.49 | 0.02 ± 0.15 | 0.41 ± 0.75 |
| “Assembling tax records”** | 0.44 ± 0.82 | 0.03 ± 0.26 | 0.68 ± 0.93 | 0.17 ± 0.55 | 0.03 ± 0.19 | 0.48 ± 0.84 |
| “Shopping alone for clothes or groceries” | 0.16 ± 0.49 | 0.00 ± 0.07 | 0.25 ± 0.59 | 0.11 ± 0.41 | 0.01 ± 0.08 | 0.29 ± 0.64 |
| “Playing a game of skill such as bridge or chess/working on a hobby” | 0.17 ± 0.47 | 0.00 ± 0.07 | 0.27 ± 0.57 | 0.10 ± 0.40 | 0.01 ± 0.10 | 0.29 ± 0.66 |
| “Heating water and turning off stove”* | 0.07 ± 0.32 | 0.00 ± 0.00 | 0.10 ± 0.40 | 0.06 ± 0.27 | 0.01 ± 0.11 | 0.15 ± 0.42 |
| “Preparing a balanced meal” | 0.16 ± 0.45 | 0.00 ± 0.07 | 0.25 ± 0.55 | 0.06 ± 0.29 | 0.00 ± 0.06 | 0.18 ± 0.47 |
| “Keeping track of current events” | 0.20 ± 0.53 | 0.00 ± 0.07 | 0.32 ± 0.64 | 0.08 ± 0.32 | 0.01 ± 0.09 | 0.22 ± 0.50 |
| “Paying attention and understanding a TV program”* | 0.16 ± 0.43 | 0.00 ± 0.07 | 0.25 ± 0.52 | 0.10 ± 0.34 | 0.02 ± 0.13 | 0.25 ± 0.51 |
| “Remembering appointments”** | 0.52 ± 0.79 | 0.05 ± 0.27 | 0.80 ± 0.86 | 0.26 ± 0.54 | 0.04 ± 0.21 | 0.65 ± 0.70 |
| “Driving or traveling out of the neighborhood” | 0.25 ± 0.63 | 0.01 ± 0.09 | 0.39 ± 0.75 | 0.17 ± 0.47 | 0.03 ± 0.18 | 0.41 ± 0.68 |
| Total FAQ Score | 2.48 ± 3.99 | 0.14 ± 0.60 | 3.84 ± 4.46 | 1.22 ± 2.72 | 0.17 ± 0.67 | 3.06 ± 3.79 |
ADNI (Alzheimer’s Disease Neuroimaging Initiative), CN (clinically normal), FAQ (Functional Activities Questionnaire), MADRC (Massachusetts Alzheimer’s Disease Research Center), MCI (mild cognitive impairment).
FAQ item score range: 0–3 (higher scores indicate greater impairment; 0 = normal or never did but could do now; 1 = has difficulty but does by self or never did but would have difficulty now; 2 = requires assistance; 3 = dependent).
All values represent mean ± standard deviation.
FAQ items that best predicted progression from CN to MCI.
FAQ items in that best discriminated between CN and MCI subjects.
Cross-sectional analyses
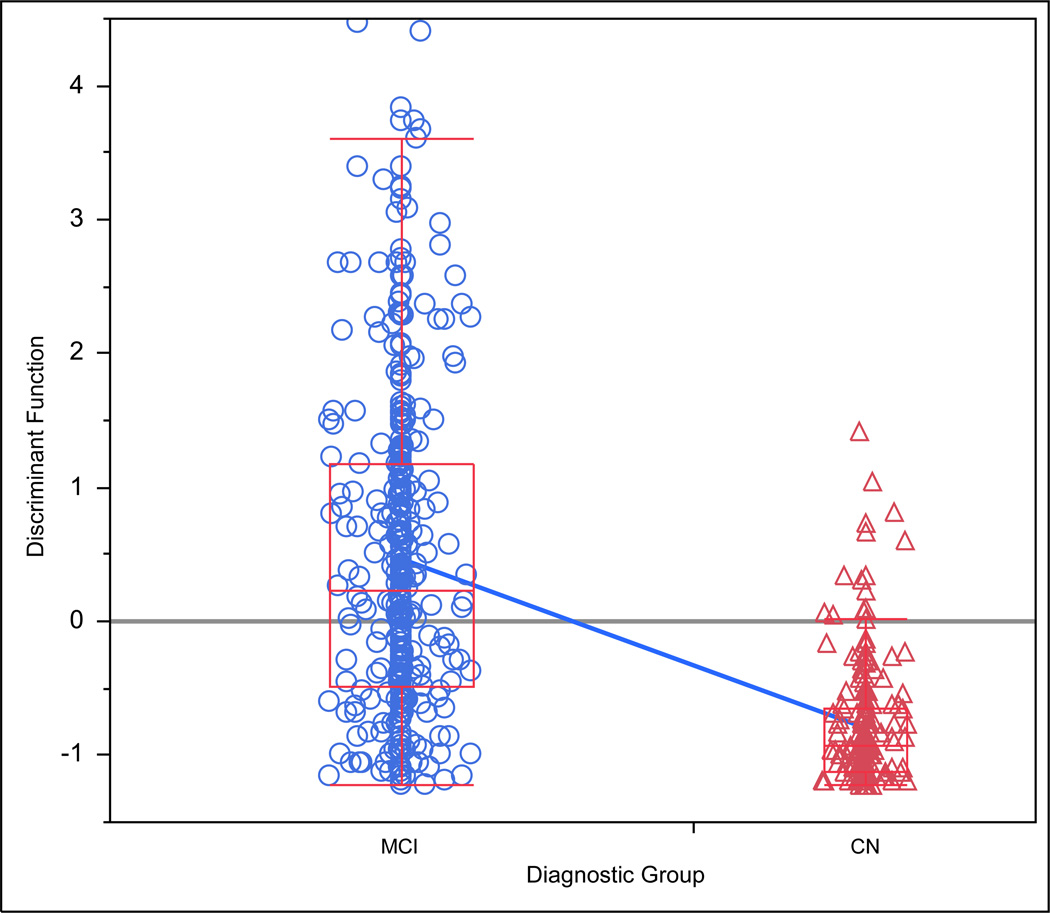
In ADNI, the discriminant analysis showed that of the FAQ items only “remembering appointments” (standardized discriminant coefficient=0.70, p<0.0001) and “assembling tax records” (coefficient=0.42, p<0.0001) significantly discriminated between CN and MCI subjects with MCI subjects performing worse than CN, see Table 2. Estimated premorbid intelligence (AMNART IQ) was also retained in the model (coefficient=−0.37, p<0.0001) with CN subjects having higher scores then MCI. The canonical correlation (between the derived discriminant linear combination versus dummy coded group status) was 0.52 (p<0.0001), see Figure 1. The logistic regression results confirmed the discriminant analysis results with the addition of “playing a game of skill such as bridge or chess/working on a hobby” as a significant predictor with MCI subjects performing worse than CN (p=0.007; p<0.0001 for the model as a whole). The area under the receiver operating characteristic (ROC) curve was 0.87.
Figure 1.
Dot-Box plot of discriminant function (linear combination of product of discriminating variables and their respective coefficients) versus diagnostic group in the ADNI cohort. FAQ items “remembering appointments” and “assembling tax records”, and AMNART IQ remained as significant predictors in the model that best discriminated between a diagnosis of CN and MCI. The blue diagonal line connecting the boxes for the respective diagnostic groups indicates the diagnostic group mean in each box, whereas the grey horizontal line across the entire figure indicates the grand mean. ADNI (Alzheimer’s Disease Neuroimaging Initiative), AMNART IQ (American National Adult Reading Test intelligence quotient), CN (clinically normal), FAQ (Functional Activities Questionnaire), MCI (mild cognitive impairment).
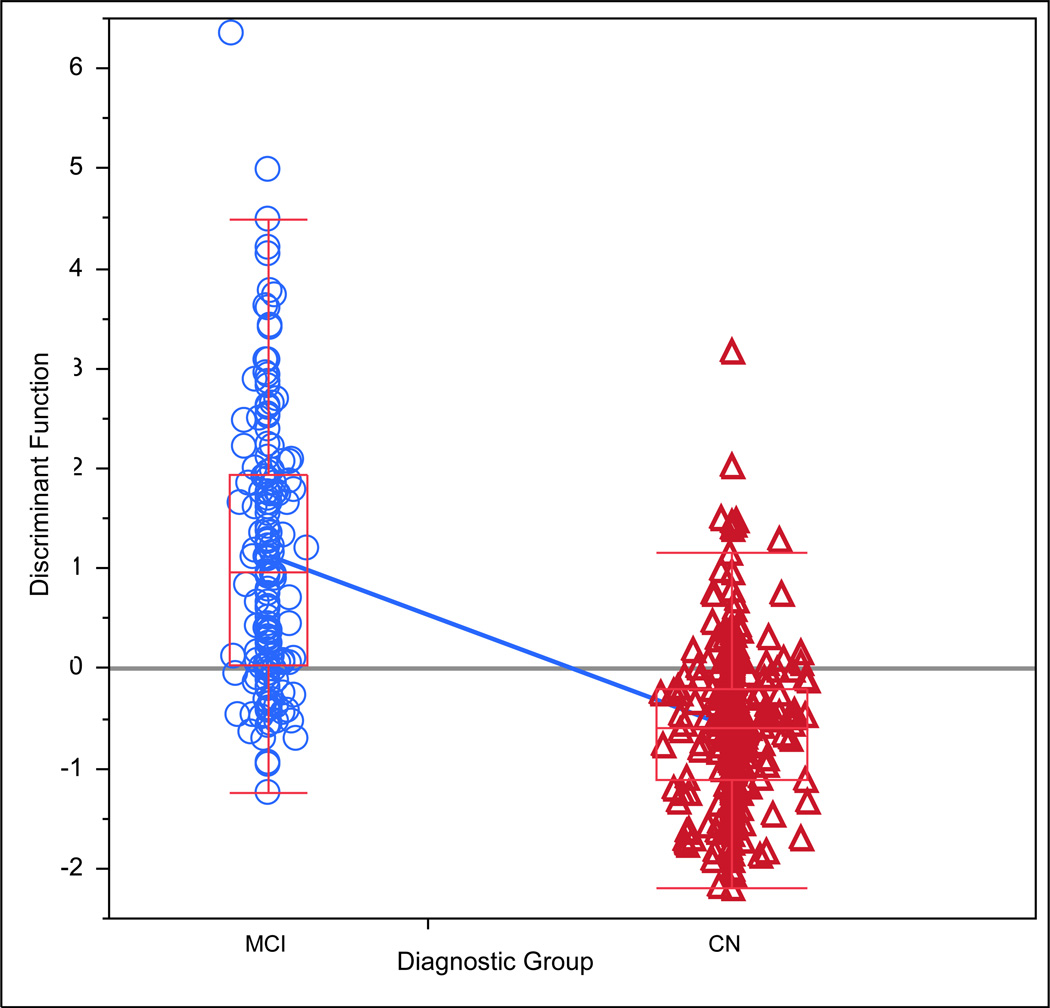
In MADRC, the discriminant analysis showed that of the FAQ items only “remembering appointments” (discriminant coefficient=0.82, p<0.0001) significantly discriminated between CN and MCI subjects with MCI subjects performing worse than CN, see Table 2. Estimated premorbid intelligence (coefficient=−0.34, p<0.0001; CN subjects having higher scores than MCI), age (coefficient=0.50, p<0.0001; MCI subjects being older than CN), and sex (coefficient for dummy coded sex=−0.25, p=0.0008; greater proportion of males among MCI subjects when compared to CN) were also retained in the model. The canonical correlation for the model was 0.63 (p<0.0001), see Figure 2. The logistic regression results confirmed the discriminant analysis results (p<0.0001 for the model as a whole). The area under the ROC curve was 0.88.
Figure 2.
Dot-Box plot of discriminant function versus diagnostic group in the MADRC cohort. FAQ item “remembering appointments”, AMNART IQ, age, and sex remained as significant predictors in the model that best discriminated between a diagnosis of CN and MCI. The blue diagonal line connecting the boxes for the respective diagnostic groups indicates the diagnostic group mean in each box, whereas the grey horizontal line across the entire figure indicates the grand mean. AMNART IQ (American National Adult Reading Test intelligence quotient), CN (clinically normal), FAQ (Functional Activities Questionnaire), MADRC (Massachusetts Alzheimer’s Disease Research Center), MCI (mild cognitive impairment).
After collapsing the data across both cohorts, a logistic regression confirmed the results of the analyses of the separate cohorts with “remembering appointments” (p<0.0001) and “assembling tax records” (p<0.0001) as significant predictors with MCI subjects performing worse than CN, as well as “keeping track of current events” (p=0.004), which was not seen with the separate cohorts.
Longitudinal analyses
In ADNI, 11 out of 223 (5%) subjects progressed from CN to MCI after a mean of 3 years, while in MADRC, 42 out of 323 (13%) subjects progressed from CN to MCI after a mean of 2 years.
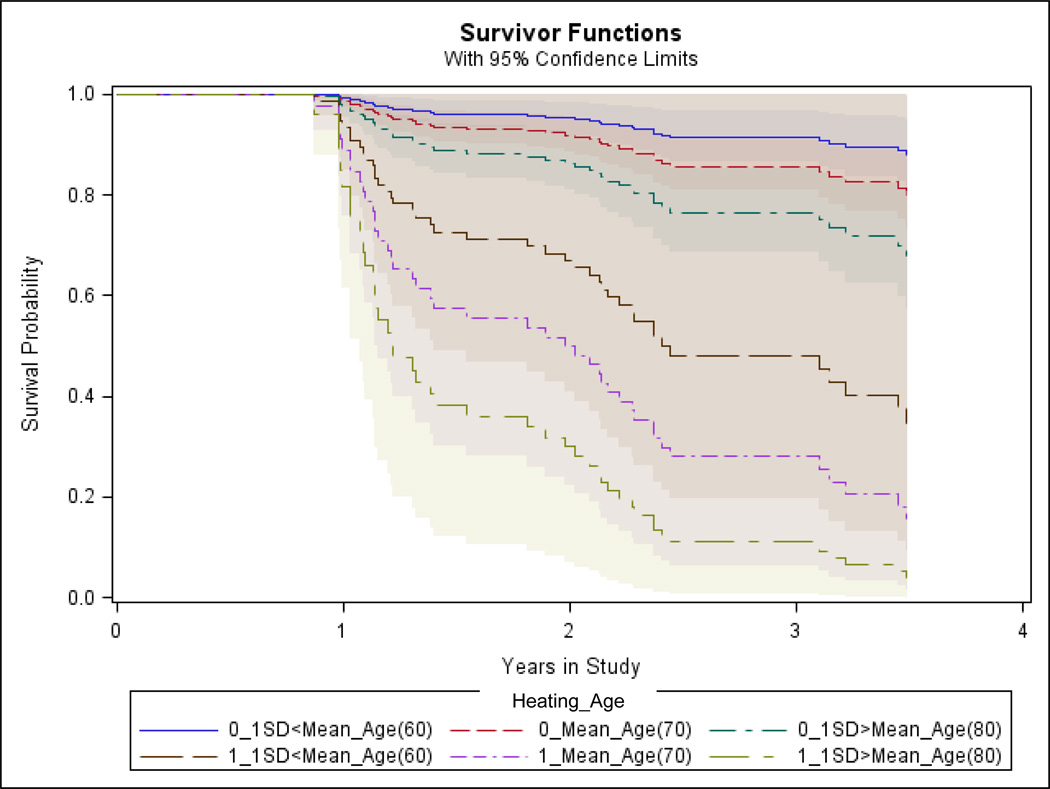
In ADNI, we found that worse performance on “paying attention and understanding a TV program” (Hazard Ratio (HR) for a one unit increase=58.4, p=0.0003, 95% confidence interval (CI) for HR=2.96, 406.08) and “paying bills/balancing checkbook” (HR=3.0, p=0.004, 95% CI for HR=1.06, 5.47) predicted greater hazard of progressing from CN to MCI (p=0.007 for the model as a whole), see Figure 3.
Figure 3.
Survival curves predicted by the Cox regression model in the ADNI cohort showing predictors retained in the model (FAQ items “paying bills/balancing checkbook” and “paying attention and understanding a TV program”). “Survival” means maintenance of a stable diagnosis of CN as opposed to progression from CN to MCI. Different FAQ item score combinations are illustrated (score range 0–3; higher scores indicate greater impairment; the first number in the legend refers to the score of FAQ item “Understanding” and second number refers to the score of FAQ item “Bills”). ADNI (Alzheimer’s Disease Neuroimaging Initiative), CN (clinically normal), FAQ (Functional Activities Questionnaire), MCI (mild cognitive impairment).
In MADRC, we found that “heating water and turning off the stove” (HR=8.2, p=0.0006, 95% CI for HR=1.96, 23.48) predicted greater hazard of progressing from CN to MCI, see Figure 4. Older age at baseline (HR for a year=1.06, p=0.002, 95% CI for HR=1.02, 1.10; HR for a decade=1.74, 95% CI= 1.2, 2.5) also predicted greater hazard of progressing from CN to MCI (p=0.0002 for the model as a whole).
Figure 4.
Survival curves predicted by the Cox regression model in the MADRC cohort showing predictors retained in the model (FAQ item “heating water and turning off the stove” and age). “Survival” means maintenance of a stable diagnosis of CN as opposed to progression from CN to MCI. Different FAQ item score (“Heating”; range 0–1; higher scores indicate greater impairment; appears as the first number in the legend) and age (mean and 1 standard deviation (SD) below and above mean) combinations are illustrated. CN (clinically normal), FAQ (Functional Activities Questionnaire), MADRC (Massachusetts Alzheimer’s Disease Research Center), MCI (mild cognitive impairment).
For both ADNI and MADRC, all predictors retained in the model passed the test for the proportional hazard assumption.
After collapsing the data across both cohorts, a Cox regression confirmed the results of the analyses of the separate cohorts with “heating water and turning off the stove” (p=0.008) significantly predicting greater hazard of progressing from CN to MCI and “paying bills/balancing checkbook” (p=0.02) marginally predicting progression.
Discussion
Utilizing cross-sectional and longitudinal data from two well characterized aging and AD cohorts, we demonstrated that a few sensitive questions can be employed to successfully discriminate between CN elderly and individuals with MCI, as well as predict progression from CN to MCI over time. These questions could be used in future research studies, for more sensitive IADL scales, and possibly for screening purposes in the primary care setting. Additionally, among various demographic characteristics adjusted for including age, sex, and education, a proxy of cognitive reserve stood out in contributing to the finer discrimination between CN and MCI.
The two FAQ items that best distinguished between CN and MCI were “remembering appointments” and “assembling tax records”. The first item was identified in both the ADNI and MADRC cohort, while the second item was only identified in the ADNI cohort. When collapsing the data across both cohorts, the same two FAQ items were identified. Difficulties in both of these items were reported in MCI most frequently when compared to the rest of the FAQ items. These results are in line with the previously reported unadjusted ADNI analyses of the FAQ items [5]. Another recent analysis using a subsequent ADNI cohort examining individual IADL-related Everyday Cognition (ECog) items showed that “Remembering appointments, meetings, or engagements” reported by self or informant discriminated well between CN and MCI subjects [22]. “Remembering appointments” clearly relies on memory, which is usually the earliest cognitive function to be affected in AD and has been shown to contribute to IADL impairment [3,7]. “Assembling tax records” is a more complex task that likely relies on multiple cognitive domains including executive function, which among the different cognitive domains has been shown to frequently contribute to IADL, including to total FAQ score [3,7,23]. That said, in the current analyses, we did not examine the direct association between individual FAQ items and different cognitive domains.
The three FAQ items that best predicted progression from CN to MCI over time were “paying attention and understanding a TV program” and “paying bills/balancing checkbook” identified in the ADNI cohort and “heating water and turning off the stove” identified in the MADRC cohort. Unlike in the cross-sectional analyses, the results did not line up in both cohorts when the analyses were performed separately. This could potentially be due to the larger sample of CN elderly in the MADRC cohort where there was also a greater proportion of progression to MCI over time. However, when collapsing the data across both cohorts, 2 of these 3 FAQ items were obtained. Difficulties in “paying attention and understanding a TV program” and “heating water and turning off the stove” are likely not early manifestations of MCI and in fact at baseline were not noted to happen that frequently among MCI subjects in either cohort. However, poor performance on both of these items at baseline in CN conveyed a very high risk of progression to MCI (HR of 58.4 and 8.2, respectively), suggesting that the few individuals who manifest these difficulties early on are at extreme risk of developing MCI. On the other hand, difficulties in “paying bills/balancing checkbook” is likely an early manifestation of MCI and were found to occur frequently among MCI subjects in either cohort at baseline. Poor performance on this item conveyed a high risk of progression to MCI (HR of 3.0) but not as high as the other rare items, suggesting that this common manifestation can serve as an important indicator of the risk of developing MCI. Prior studies focusing on financial tasks, using a performance-based IADL instrument, the Financial Capacity Instrument (FCI), have similarly shown that difficulties performing the finances, including difficulties with paying bills and balancing the checkbook, distinguished between CN and MCI, as well as predicted progression from MCI to AD dementia [24,25]. More recently, another study showed that self but not informant report of difficulties in balancing the checkbook discriminate between CN and MCI [22]. As with the cross-sectional analyses in the current study, the FAQ items identified in the longitudinal analyses here heavily rely on executive function and memory. However, they also rely more on attention unlike the items identified in the cross-sectional analyses. It is therefore possible that early IADL changes due to inattention in CN elderly are more predictive of future decline to MCI, while IADL changes relying on multiple, complex cognitive functions are better at distinguishing between CN and MCI.
IADL are most commonly assessed using subjective scales usually relying on informant report; some performance-based IADL instruments have been developed as well thought to be more objective and potentially more ecologically valid than the subjective scales [1]. Several subjective IADL scales have been used to successfully distinguish between CN and MCI: the total score of the FAQ, the CDR, the Structured Interview and Scoring Tool—MADRC Informant Report (SIST-M-IR), the ADL-Prevention Instrument (ADL-PI), and the ECog [3,4,26–28]. Four of the SIST-M-IR items in particular have been shown to best discriminate between CN and MCI [29]. Moreover, the SIST-M-IR and ADL-PI total scores have been shown to successfully predict progression from CN to MCI and future cognitive decline in CN elderly [27,28]. Fewer performance-based IADL instruments have been shown to differentiate between CN and MCI: the FCI and the University of California, San Diego Performance-Based Skills Assessment [24,30]. In the current study we were able to demonstrate that 5 simple questions had equivalent sensitivity to early IADL changes in AD like the above scales and instruments—these questions could potentially be used more easily for screening purposes by primary care physicians, who do not have the time and expertise to perform more extensive clinical assessments. Moreover, diagnostic assessments, such as various imaging modalities and cerebrospinal fluid, though likely are more sensitive for the detection of early AD, are expensive, sometimes invasive, and not always widely available. Therefore, a brief and accurate screening clinical assessment employing IADL questions such as those identified here can be of great use.
An important confound to consider in subjective IADL scales is that before reaching late MCI, self-report of IADL changes may potentially be more accurate than informant report. Using the ECog, equivalent information was obtained from self-report and informant report versions about IADL in individuals with CN and MCI, while demented individuals under-reported the degree of their IADL impairment when compared to their informants [31]. In contrast, another study showed a lack of agreement in reporting of IADL, such as driving and managing the finances, by self versus informant in individuals with MCI [32]. CN individuals or those with subjective cognitive concerns usually have intact or even increased awareness of cognitive changes; in those individuals self-report is reliable and often more useful than informant report [33]. On the other hand, individuals with MCI and mild dementia often have a decrease in awareness; therefore, in those individuals informant report is likely more reliable than self-report. Thus, new subjective IADL scales targeting early AD will likely require assessment of both subjects and informants.
In multiple studies, IADL impairment has been associated with amyloid and tau pathology, as well as regional atrophy, hypometabolism, and hypoperfusion across the early AD spectrum [34–41]. Temporal and parietal findings on imaging studies traditionally associated with early AD and memory and semantic processing impairment have been associated with IADL impairment in the above referenced studies. Moreover, frontal findings usually associated with executive dysfunction but not necessarily with early AD have also been associated with IADL impairment. As suggested by the complexity of the 5 FAQ items identified as sensitive markers of early AD in the current study, multiple cognitive domains contribute to high level IADL and therefore are likely to involve multiple regions in the brain.
The current study had several limitations. First, only 1 of the 5 FAQ items identified in the analyses was found across both cohorts. Therefore, our results need to be interpreted with caution. That said, ADNI subjects were older than MADRC subjects, had a higher proportion of males, had more MCI than CN subjects, had lower scores on CDR Sum of Boxes, and had a smaller proportion of subjects progressing from CN to MCI. Those differences could have accounted for the different results observed in the two cohorts. However, when collapsing the data across both cohorts, similar items were identified for both cross-sectional and longitudinal analyses. Second, both the ADNI and MADRC samples are highly characterized and are not representative of the general population. Both samples consist of highly educated and highly intelligent individuals. However, those demographic characteristics were adjusted for in our analyses. Moreover, this is typical of multicenter clinical trial samples. Therefore, these results could be informative of future clinical trials assessing sensitive IADL outcome measures in early AD. More studies in the general population will be required before the current findings could be potentially implemented for early AD screening by primary care providers. Third, as discussed above, IADL impairment in early AD has been associated with multiple AD biomarkers, but the current study did not assess the association between the FAQ items and AD biomarkers. Future studies, focusing on various sensitive IADL questionnaire items forming a new and improved subjective scale will be related to AD biomarkers for the purpose of further validation. Since the FAQ items have only a few discrete values, the normality assumptions of discriminant analyses were likely violated in the cross-sectional analyses used to determine which items best distinguished between CN and MCI subjects. We therefore confirmed the results of the discriminant analyses with logistic regression models, which do not require a normality assumption, and similar results were obtained. Fourth, the FAQ is informant-based, which as discussed above is appropriate for MCI but may not be appropriate for CN elderly for whom self-report may be more accurate. Moreover, a performance-based instrument maybe preferable to a subjective scale altogether since it is more objective and may in fact simulate real life. However, most performance-based instruments are time consuming and may require extensive training to administer as opposed to the subjective scales.
Conclusions
These results demonstrate that after adjusting for demographics including age, certain questions are especially sensitive in detecting the earliest functional changes in CN elderly at risk for AD. As the field is moving toward earlier intervention, it is imperative to develop new sensitive subjective scales and performance-based instruments for assessing IADL in order to better predict the progression in preclinical AD and early prodromal AD (early MCI) that is most meaningful to affected individuals and their loved ones.
Acknowledgements
This study was supported by ADNI (U01 AG024904), DOD ADNI (W81XWH-12-2-0012), the MADRC (P50 AG005134), R01 AG027435, K23 AG033634, K24 AG035007, and the Harvard Aging Brain Study (P01 AGO36694). ADNI is funded by the National Institute on Aging, the National Institute of Biomedical Imaging and Bioengineering, and through generous contributions from the following: Alzheimer’s Association; Alzheimer’s Drug Discovery Foundation; BioClinica, Inc.; Biogen Idec Inc.; Bristol-Myers Squibb Company; Eisai Inc.; Elan Pharmaceuticals, Inc.; Eli Lilly and Company; F. Hoffmann-La Roche Ltd and its affiliated company Genentech, Inc.; GE Healthcare; Innogenetics, N.V.; IXICO Ltd.; Janssen Alzheimer Immunotherapy Research & Development, LLC.; Johnson & Johnson Pharmaceutical Research & Development LLC.; Medpace, Inc.; Merck & Co., Inc.; Meso Scale Diagnostics, LLC.; NeuroRx Research; Novartis Pharmaceuticals Corporation; Pfizer Inc.; Piramal Imaging; Servier; Synarc Inc.; and Takeda Pharmaceutical Company. The Canadian Institutes of Health Research is providing funds to support ADNI clinical sites in Canada. Private sector contributions are facilitated by the Foundation for the National Institutes of Health (www.fnih.org). The grantee organization is the Northern California Institute for Research and Education, and the study is coordinated by the Alzheimer's Disease Cooperative Study at the University of California, San Diego. ADNI data are disseminated by the Laboratory for Neuro Imaging at the University of Southern California.
Conflicts of Interest
The authors have received research salary support from Janssen Alzheimer Immunotherapy (GAM, REA), Wyeth/Pfizer Pharmaceuticals (GAM, REA), Eisai Inc. (GAM), Eli Lilly and Company (GAM), Avid Radiopharmaceuticals (KAJ), and Bristol-Myers-Squibb (GAM, RAS).
References
- 1.Marshall GA, Amariglio RE, Sperling RA, Rentz DM. Activities of daily living: Where do they fit in the diagnosis of Alzheimer’s disease. Neurodegener Dis Manag. 2012;2(5):483–491. doi: 10.2217/nmt.12.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pfeffer RI, Kurosaki TT, Harrah CH, Jr, Chance JM, Filos S. Measurement of functional activities in older adults in the community. J Gerontol. 1982;37(3):323–329. doi: 10.1093/geronj/37.3.323. [DOI] [PubMed] [Google Scholar]
- 3.Marshall GA, Rentz DM, Frey MT, Locascio JJ, Johnson KA, Sperling RA, et al. Executive function and instrumental activities of daily living in mild cognitive impairment and Alzheimer’s disease. Alzheimers Dement. 2011;7(3):300–308. doi: 10.1016/j.jalz.2010.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morris JC. Revised Criteria for Mild Cognitive Impairment May Compromise the Diagnosis of Alzheimer Disease Dementia. Arch Neurol. 2012 doi: 10.1001/archneurol.2011.3152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brown PJ, Devanand DP, Liu X, Caccappolo E. Functional impairment in elderly patients with mild cognitive impairment and mild Alzheimer disease. Arch Gen Psychiatry. 2011;68(6):617–626. doi: 10.1001/archgenpsychiatry.2011.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011;7(3):270–279. doi: 10.1016/j.jalz.2011.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Royall DR, Lauterbach EC, Kaufer D, Malloy P, Coburn KL, Black KJ, et al. The cognitive correlates of functional status: a review from the Committee on Research of the American Neuropsychiatric Association. J Neuropsychiatry Clin Neurosci. 2007;19(3):249–265. doi: 10.1176/jnp.2007.19.3.249. [DOI] [PubMed] [Google Scholar]
- 8.Kozauer N, Katz R. Regulatory innovation and drug development for early-stage Alzheimer's disease. N Engl J Med. 2013;368(13):1169–1171. doi: 10.1056/NEJMp1302513. [DOI] [PubMed] [Google Scholar]
- 9.Weiner MW, Veitch DP, Aisen PS, Beckett LA, Cairns NJ, Green RC, et al. The Alzheimer's Disease Neuroimaging Initiative: a review of papers published since its inception. Alzheimers Dement. 2012;8(1 Suppl):S1–S68. doi: 10.1016/j.jalz.2011.09.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Donovan NJ, Amariglio RE, Zoller AS, Rudel RK, Gomez-Isla T, Blacker D, et al. Subjective cognitive concerns and neuropsychiatric predictors of progression to the early clinical stages of Alzheimer’s disease. Am J Geriatr Psychiatry. 2014;22(12):1642–1651. doi: 10.1016/j.jagp.2014.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morris JC, Weintraub S, Chui HC, Cummings J, Decarli C, Ferris S, et al. The Uniform Data Set (UDS): clinical and cognitive variables and descriptive data from Alzheimer Disease Centers. Alzheimer Dis Assoc Disord. 2006;20(4):210–216. doi: 10.1097/01.wad.0000213865.09806.92. [DOI] [PubMed] [Google Scholar]
- 12.Weintraub S, Salmon D, Mercaldo N, Ferris S, Graff-Radford NR, Chui H, et al. The Alzheimer's Disease Centers' Uniform Data Set (UDS): the neuropsychologic test battery. Alzheimer Dis Assoc Disord. 2009;23(2):91–101. doi: 10.1097/WAD.0b013e318191c7dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosen WG, Terry RD, Fuld PA, Katzman R, Peck A. Pathological verification of ischemic score in differentiation of dementias. Ann Neurol. 1980;7(5):486–488. doi: 10.1002/ana.410070516. [DOI] [PubMed] [Google Scholar]
- 14.Sheikh JI, Yesavage JA. Clinical Gerontology : A Guide to Assessment and Intervention. New York: The Haworth Press; 1986. Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version; pp. 165–173. [Google Scholar]
- 15.Morris JC. The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology. 1993;43(11):2412–2414. doi: 10.1212/wnl.43.11.2412-a. [DOI] [PubMed] [Google Scholar]
- 16.Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 17.Wechsler D. WMS-R Wechsler Memory Scale Revised Manual. New York: The Psychological Corporation, Harcourt Brace Jovanovich, Inc; 1987. [Google Scholar]
- 18.Buschke H. Cued recall in amnesia. J Clin Neuropsychol. 1984;6(4):433–440. doi: 10.1080/01688638408401233. [DOI] [PubMed] [Google Scholar]
- 19.Delis DC, Kramer JH, Kaplan E, Ober BA. California Verbal Learning Test. Second ed. San Antonio, TX: Psychological Corporation; 2000. [Google Scholar]
- 20.Nitrini R, Caramelli P, Herrera E, Jr, Bahia VS, Caixeta LF, Radanovic M, et al. Incidence of dementia in a community-dwelling Brazilian population. Alzheimer Dis Assoc Disord. 2004;18(4):241–246. [PubMed] [Google Scholar]
- 21.Nelson HE, O'Connell A. Dementia: the estimation of premorbid intelligence levels using the New Adult Reading Test. Cortex. 1978;14(2):234–244. doi: 10.1016/s0010-9452(78)80049-5. [DOI] [PubMed] [Google Scholar]
- 22.Marshall GA, Zoller AS, Kelly KE, Amariglio RE, Locascio JJ, Johnson KA, et al. Everyday Cognition scale items that best discriminate between and predict progression from clinically normal to mild cognitive impairment. Curr Alzheimer Res. 2014;11(9):853–861. doi: 10.2174/1567205011666141001120903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Boyle PA, Malloy PF, Salloway S, Cahn-Weiner DA, Cohen R, Cummings JL. Executive dysfunction and apathy predict functional impairment in Alzheimer disease. Am J Geriatr Psychiatry. 2003;11(2):214–221. [PubMed] [Google Scholar]
- 24.Triebel KL, Martin R, Griffith HR, Marceaux J, Okonkwo OC, Harrell L, et al. Declining financial capacity in mild cognitive impairment: A 1-year longitudinal study. Neurology. 2009;73(12):928–934. doi: 10.1212/WNL.0b013e3181b87971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Griffith HR, Belue K, Sicola A, Krzywanski S, Zamrini E, Harrell L, et al. Impaired financial abilities in mild cognitive impairment: a direct assessment approach. Neurology. 2003;60(3):449–457. doi: 10.1212/wnl.60.3.449. [DOI] [PubMed] [Google Scholar]
- 26.Farias ST, Mungas D, Harvey DJ, Simmons A, Reed BR, DeCarli C. The measurement of everyday cognition: Development and validation of a short form of the Everyday Cognition scales. Alzheimers Dement. 2011:7593–7601. doi: 10.1016/j.jalz.2011.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Galasko D, Bennett DA, Sano M, Marson D, Kaye J, Edland SD. ADCS Prevention Instrument Project: assessment of instrumental activities of daily living for community-dwelling elderly individuals in dementia prevention clinical trials. Alzheimer Dis Assoc Disord. 2006;20(4 Suppl 3):S152–S169. doi: 10.1097/01.wad.0000213873.25053.2b. [DOI] [PubMed] [Google Scholar]
- 28.Okereke OI, Pantoja-Galicia N, Copeland M, Hyman BT, Wanggaard T, Albert MS, et al. The SIST-M: predictive validity of a brief structured clinical dementia rating interview. Alzheimer Dis Assoc Disord. 2012;26(3):225–231. doi: 10.1097/WAD.0b013e318231cd30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zoller AS, Gaal IM, Royer CA, Locascio JJ, Amariglio RE, Blacker D, et al. SIST-M-IR activities of daily living items that best discriminate clinically normal elderly from those with mild cognitive impairment. Curr Alzheimer Res. 2014;11(8):785–791. doi: 10.2174/156720501108140910122220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goldberg TE, Koppel J, Keehlisen L, Christen E, Dreses-Werringloer U, Conejero-Goldberg C, et al. Performance-based measures of everyday function in mild cognitive impairment. Am J Psychiatry. 2010;167(7):845–853. doi: 10.1176/appi.ajp.2010.09050692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Farias ST, Mungas D, Jagust W. Degree of discrepancy between self and other-reported everyday functioning by cognitive status: dementia, mild cognitive impairment, and healthy elders. Int J Geriatr Psychiatry. 2005;20(9):827–834. doi: 10.1002/gps.1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Okonkwo OC, Griffith HR, Vance DE, Marson DC, Ball KK, Wadley VG. Awareness of functional difficulties in mild cognitive impairment: a multidomain assessment approach. J Am Geriatr Soc. 2009;57(6):978–984. doi: 10.1111/j.1532-5415.2009.02261.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Caselli RJ, Chen K, Locke DE, Lee W, Roontiva A, Bandy D, et al. Subjective cognitive decline: self and informant comparisons. Alzheimers Dement. 2014;10(1):93–98. doi: 10.1016/j.jalz.2013.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Landau SM, Harvey D, Madison CM, Koeppe RA, Reiman EM, Foster NL, et al. Associations between cognitive, functional, and FDG-PET measures of decline in AD and MCI. Neurobiol Aging. 2011;32(7):1207–1218. doi: 10.1016/j.neurobiolaging.2009.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Marshall GA, Lorius N, Locascio JJ, Hyman BT, Rentz DM, Johnson KA, et al. Regional cortical thinning and cerebrospinal biomarkers predict worsening daily functioning across the Alzheimer disease spectrum. J Alzheimers Dis. 2014;41(3):719–728. doi: 10.3233/JAD-132768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marshall GA, Olson LE, Frey MT, Maye J, Becker JA, Rentz DM, et al. Instrumental activities of daily living impairment is associated with increased amyloid burden. Dement Geriatr Cogn Disord. 2011;31(6):443–450. doi: 10.1159/000329543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Okonkwo OC, Alosco ML, Griffith HR, Mielke MM, Shaw LM, Trojanowski JQ, et al. Cerebrospinal fluid abnormalities and rate of decline in everyday function across the dementia spectrum: normal aging, mild cognitive impairment, and Alzheimer disease. Arch Neurol. 2010;67(6):688–696. doi: 10.1001/archneurol.2010.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Roy K, Pepin LC, Philiossaint M, Lorius N, Becker JA, Locascio JJ, et al. Regional fluorodeoxyglucose metabolism and instrumental activities of daily living across the Alzheimer’s disease spectrum. J Alzheimers Dis. 2014;42(1):291–300. doi: 10.3233/JAD-131796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.de Gois Vasconcelos L, Jackowski AP, Oliveira MO, Flor YM, Bueno OF, Brucki SM. Voxel-based morphometry findings in Alzheimer's disease: neuropsychiatric symptoms and disability correlations - preliminary results. Clinics (Sao Paulo) 2011;66(6):1045–1050. doi: 10.1590/S1807-59322011000600021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nadkarni NK, Levy-Cooperman N, Black SE. Functional correlates of instrumental activities of daily living in mild Alzheimer's disease. Neurobiol Aging. 2012;33(1):53–60. doi: 10.1016/j.neurobiolaging.2010.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vidoni ED, Honea RA, Burns JM. Neural correlates of impaired functional independence in early Alzheimer's disease. J Alzheimers Dis. 2010;19(2):517–527. doi: 10.3233/JAD-2010-1245. [DOI] [PMC free article] [PubMed] [Google Scholar]