Abstract
Objectives
The evidence base to inform the management of Achilles tendon rupture is sparse. The objectives of this research were to establish what current practice is in the United Kingdom and explore clinicians’ views on proposed further research in this area. This study was registered with the ISRCTN (ISRCTN68273773) as part of a larger programme of research.
Methods
We report an online survey of current practice in the United Kingdom, approved by the British Orthopaedic Foot and Ankle Society and completed by 181 of its members. A total of ten of these respondents were invited for a subsequent one-to-one interview to explore clinician views on proposed further research in this area.
Results
The survey showed wide variations in practice, with patients being managed in plaster cast alone (13%), plaster cast followed by orthoses management (68%), and orthoses alone (19%). Within these categories, further variation existed regarding the individual rehabilitation facets, such as the length of time worn, the foot position within them and weight-bearing status. The subsequent interviews reflected this clinical uncertainty and the pressing need for definitive research.
Conclusions
The gap in evidence in this area has resulted in practice in the United Kingdom becoming varied and based on individual opinion. Future high-quality randomised trials on this subject are supported by the clinical community.
Cite this article: Bone Joint Res 2015;4:65–9
Keywords: Achilles tendon, Rupture, Rehabilitation, Plaster Cast, Orthotics
Article focus
The evidence base for Achilles tendon rupture management is sparse
What is current management across the United Kingdom?
Key messages
Limited research in the area of Achilles tendon management has resulted in wide variations in practice across the United Kingdom
Clinicians’ views support the need for further research in this area in order to decrease variation and optimise patient care
Strengths and limitations
This is the first study to survey the practice in the United Kingdom of Achilles tendon rupture management
This research represents a ‘snapshot’ of current practice in the United Kingdom. Broader generalisation to other healthcare systems and practices is limited
Introduction
The Achilles is the largest tendon in the human body and transmits the powerful contractions of the calf muscles that are required for walking and running.1 Achilles tendon rupture affects over 11 000 people each year in the United Kingdom, and the incidence is increasing as the population remains more active into older age.2 When the tendon ruptures it is painful and has an immediate and serious detrimental impact on daily activities of living. This can result in restricted daily activities in the early phase and reduced physical activity, with associated negative health and social consequences in the longer term.3
Following non-operative management, patients have traditionally been treated in plaster casts, with the cast immobilising the foot and ankle while the tendon heals.4 However, there are potential problems with this approach. Firstly, there is the immediate impact on mobility for a period of around eight weeks. This is compounded if the patient is non-weight bearing. Secondly, there are the complications and risks associated with prolonged immobilisation including muscle atrophy, deep vein thrombosis and joint stiffness.5 Finally, there are the potential long-term consequences which include prolonged gait abnormalities, persistent calf muscle weakness and an inability to return to previous activity levels.3,6,7 Functional bracing (involving immediate, protected weight-bearing in a brace) was designed to address these issues.8 However, the only guideline on this topic, by the American Academy of Orthopaedic Surgeons,9 concluded that:
‘For patients treated non-operatively, we are unable to recommend for or against the use of immediate functional bracing for patients with acute Achilles tendon rupture’.
Systematic reviews have demonstrated that not only is there a gap in evidence regarding whether plaster cast or functional bracing should be used, but also of what exactly these treatments consist.4,8 For example, for how long is the plaster cast worn? Which functional bracing system is used? And in what position should the foot and ankle be maintained? Such reviews have provided a summary of the published protocols being used in research, but it is not known if these published research protocols reflect what is actually happening in hospitals across the United Kingdom.
With the support of the British Foot and Ankle Society (BOFAS), the aims of this mixed methods study were to survey orthopaedic consultants to ascertain current practice in the United Kingdom for non-operatively managed Achilles tendon ruptures, and interview orthopaedic consultants to explore clinicians’ views on the proposed protocols to be used in future research comparing plaster cast immobilisation with functional bracing, following an Achilles tendon rupture.
Patients and Methods
Firstly, this study used an online survey (approved by the BOFAS scientific committee) to document which management techniques are being used across hospitals in the United Kingdom by orthopaedic consultants. Secondly, this study used one-to-one interviews to explore clinicians’ views on a proposed plaster cast and functional bracing protocol to be used in a future planned randomised controlled trial (RCT) comparing the two protocols. Approval for the study was granted by the National Research Ethics Committee West Midlands (12/WM/0083) and registered with the International Standard Randomised Controlled Trial Number (ISRCTN) 68273773 as part of a larger programme of research.
The survey was emailed to all BOFAS members. This population was chosen because in the United Kingdom NHS setting, patients with Achilles tendon rupture will typically be referred from accident and emergency departments to the next available fracture clinic for an opinion from an orthopaedic specialist. In fracture clinic, the orthopaedic specialist and patient will discuss management options, and in some cases, pre-defined protocols will be used. These are usually developed by orthopaedic consultants with a special interest in foot and ankle management. Therefore, this survey specifically targeted those orthopaedic consultants with a special interest in foot and ankle management in order to establish what protocols are being implemented across the United Kingdom.
An online survey of closed-ended questions was administered via a link to SurveyMonkey10 from the initial invitation email to all BOFAS members. The survey questions were formulated based on international clinical guidelines, a systematic review of rehabilitation protocols completed by the authors and consultation with the BOFAS scientific committee. Following initial development of the questionnaire, it was piloted by five BOFAS members to gain feedback on content and ease of use.
The survey comprised three sections. Part one contained questions about what proportion of patients with an Achilles tendon rupture the orthopaedic consultant typically manages non-operatively and the criteria they use to make this decision. Part two contained questions about the plaster cast or functional bracing protocol they use, and part three contained questions regarding the post-treatment physiotherapy received. All survey responses were categorical.
All survey data were collected in SurveyMonkey and transferred to Microsoft Excel 2013 (Redmond, Washington) for analysis. Frequency distributions for the closed-ended questions were generated. Missing data were not imputed.
A total of 181 members completed the survey. Subsequently, these participants were invited to take part in a one-to-one interview. Of these, 36 agreed to be contacted for an interview. From these 36 responses, ten were chosen using maximum variation sampling techniques to ensure a wide range of perspectives were captured. Criteria considered included the participants’ current practice, size of their catchment area and previous engagement in research.
We recorded ten semi-structured key informant interviews with orthopaedic clinicians who responded to the survey and consented to be contacted. The interviews were carried out by the lead author within the participant’s place of practice, or alternatively, at a place of their choice.
A semi-structured methodology was used to ensure core areas were explored with all interviewees, while allowing the interviewer to be responsive to the participants’ comments to investigate emerging themes further. One-to-one interviews were used to ensure that opinion leaders in the field of foot and ankle management did not influence responses from other colleagues. Furthermore, one-to-one interviews allowed greater flexibility regarding scheduling of data collection, which was a key consideration to ensure consent to participation.
The interviewees were asked to describe their context and experiences in relation to Achilles tendon rupture rehabilitation. They were then provided with a summary of current evidence about rehabilitation, current practice in the United Kingdom (informed by the survey results) and the rationale for future research. Interviewees were invited to comment. They were then given a summary of a proposed trial methodology and asked again to comment.
All interviews were transcribed and the responses to the questions were explored using conventional content analysis, allowing names for categories to flow from the data to be discussed later in relation to current practice and future research.
Results
Percentage of patients managed non-operatively and reasons for choosing this management
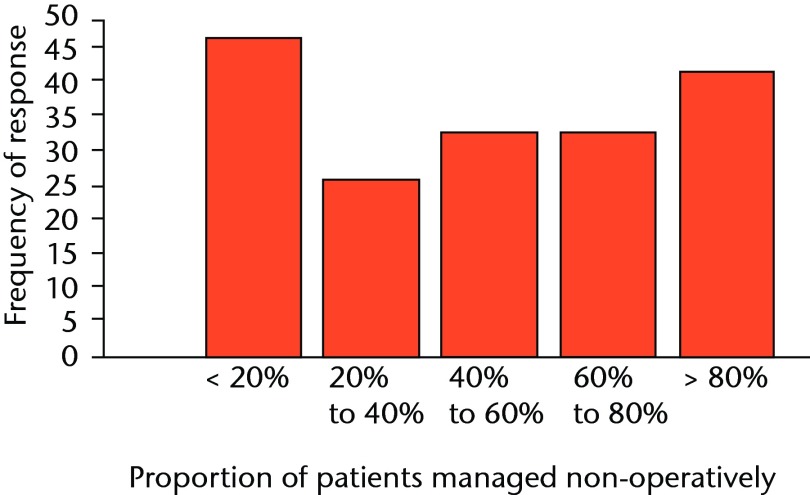
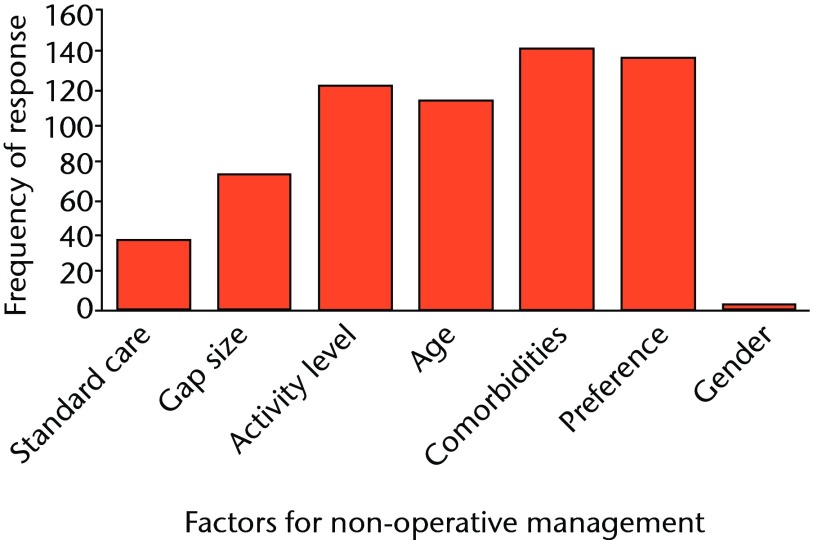
Figure 1 shows the frequency of responses for each categorical response to the question asking clinicians ‘What proportion of patients do you manage non-operatively?’ Figure 2 highlights the most common factors influencing the decision to manage the patient non-operatively, which include patient preference, presence of comorbidities, patient activity level, and age. Less common factors included the gender of the patient, the tendon ‘gap’ size on ultrasound and ‘following unit protocol’.
Fig. 1.
Response 181/181: bar graph showing the percentage of patients managed non-operatively.
Fig. 2.
Response 181/181: bar graph showing factors for non-operative management.
Type of rehabilitation method used
The subsequent survey questions referred to the individual rehabilitation methods used by clinicians. The most popular was the combined management of plaster cast immobilisation followed by application of orthoses management (124; 69%); the second most popular was orthoses alone (34; 19%), followed by plaster cast immobilisation alone (23; 12%).
Plaster cast rehabilitation
Of those who use plaster cast alone, the majority initially place the foot in a minimum of 20º, gradually moving the foot to plantigrade. The plaster casts were worn for between < four and 11 weeks, most commonly between six and nine weeks. Weight-bearing status while wearing the plaster cast ranged from immediate full weight-bearing to no weight being permitted. The majority reported starting with no weight being permitted, but allowing progression to full weight-bearing during the period the plaster cast was worn (10; 48%).
Plaster cast followed by orthoses rehabilitation
The majority of respondents were in this category (124/181). Of these 124, 118 provided further details regarding their rehabilitation protocols. As for plaster cast rehabilitation alone, the foot was most commonly reported to be placed in a minimum of 20º of plantarflexion (108; 92%), with 101 (86%) then moving the foot gradually towards plantigrade. The plaster cast was worn for shorter duration than above, with most reporting a period less than six weeks. There was again a range in weight-bearing status from immediate full weight-bearing to no weight being permitted.
The orthoses part of the management showed that two orthoses types were most commonly used, the rigid rocker bottom style (65, 55%), and the adjustable CAM style (50, 42%). Again, the majority initially place the foot in a minimum of 20º, gradually moving to plantigrade. The orthoses were reported to be worn up to a maximum of ten weeks by some; the most common length of time was < four weeks. In contrast to the plaster cast phase, immediate full was the most common weight-bearing status.
During the orthosis wearing phase, the patient could also begin early range of movement exercises as the orthoses could be removed intermittently. This was not an option with plaster cast rehabilitation. In the orthoses phase, 72 of the 105 consultants that responded to this question (68%) allowed removal of the orthoses for this purpose. They were most commonly removed more than three times a day to complete as many repetitions as the patient felt able.
Orthoses rehabilitation
Two types of orthoses were used: the rigid rocker bottom type (17, 50%) and the adjustable cam type (17, 50%). All patients were kept in a minimum of 20º of plantarflexion or had two or more heel wedge inserts. They were worn for between five and ten weeks. Immediate full weight-bearing was used by the majority in this group.
In contrast to the above, only 13 consultants (38%) allowed removal of the orthoses to complete range of movement exercises. Of those, most recommended completing the exercises only two or three times a day and imposed limits on the number of repetitions.
Post-immobilisation advice
Following any of three rehabilitation methods described above, 62 clinicians reported providing patients with advice sheets and 149 clinicians also refer to physiotherapy. In physiotherapy, 96 clinicians reported that patients followed a protocol designed by the foot and ankle team.
Clinicians’ views on rehabilitation protocols designed for a future RCT
The interviewees were all at consultant level with a special interest in foot and ankle research. Clinical experience ranged from newly appointed to more than 20 years in a post. Previous research experience ranged from those who had led audit/service evaluation only, to those who were actively participating in large multi-centre RCTs.
Throughout the interviews, a common discussion arose that any future RCTs comparing rehabilitation methods need to be pragmatic to the NHS setting, and not prescriptive. The main reasons discussed were related to the research needing to reflect what actually happens in practice, rather than what should happen. For example, instead of imposing a rigid rehabilitation protocol, tolerances should be used. Therefore, instead of stating the exact orthoses to be used, the intervention would instead be ‘orthoses management’, with an accompanying quality criteria checklist to quantify what was acceptable under this heading. This then would reflect what actually happens in practice. It was also linked in with what clinicians felt would be feasible to implement:
‘...Our unit would have to use the Vacuped boot – otherwise it will be too much of a culture change. The intervention is weight bearing, not the specific boot... Need to add the lee-way’
‘…If you let all centres use any boot – you need a pre-defined list of brands and exclude centres that don’t use them...’
‘… I use an articulated boot – but would be happy to use any. Ideally the protocol should be the same across every centre, but I recognise that this would be problematic…’
Alongside the specific issues related to implementing rehabilitation protocols across the NHS in a multi-centre trial, three further themes emerged including financial drivers to participate, external support drivers to participate and approval from colleagues for research feasibility.
All interviewees raised issues surrounding the current economic climate, most specifically that the acceptability and feasibility of conducting a future large multi-centre RCT would require financial incentive for the department to justify the additional pressures in an already busy service. This was closely linked to the second theme of the requirement for ongoing external support:
‘…the trust needs to be paid – if there is no money the trust is unlikely to sign up…’
‘...financial support for staff time is required to take part in the study… support with training requirements.’
All interviewees also expressed a need for wider departmental approval from colleagues. Interviewees often discussed the needs for all research projects to be a team activity within the trust, not just an individual endeavour.
‘…need for good communication when doctors rotate – that’s when things go wrong in other studies...’
‘…team acceptability is the main barrier, the best strategy would be to present to ED and present to the orthopaedic department…’
‘…just need clinician buy in…’
Discussion
This is the first study to survey practice in the United Kingdom among orthopaedic consultants regarding the management of patients with an Achilles tendon rupture. Our results show there is wide variation in practice.
There was disparity among clinicians at the very first decision of which patients should be managed non-operatively and why. There was, however, agreement regarding those patients with comorbidities (which would preclude them from surgery) and patient preference.
Following the decision to operate or not, rehabilitation methods fell into three categories: plaster cast alone, plaster cast followed by orthoses management, and orthoses management alone. However, within these categories there was again wide variation in the duration for which the cast/orthotic device was worn and the position of the ankle joint. This variation in practice reflects the variation in current literature.8,9
Historically, all patients were immobilised and non-weight bearing in a plaster cast. However, recent research has led to newer methods involving early movement and loading. These newer methods were developed from initial animal models that were able to demonstrate positive effects of load and movement on tendon characteristics, healing orientation of collagen fibres and calf strength.11,12
The first randomised trials using these principles were reported by Saleh et al,13 leading to further comparative studies and subsequent meta-analyses on the topic by the Cochrane Collaboration in 2004,14 Suchak in 2006,4 and more recent systematic reviews for the development of national guidelines by the American Academy of Orthopaedic Surgeons (AAOS) in 2009.9 However, a definitive opinion on what rehabilitation method should be used has not been reached in the literature, and this is clearly reflected in this United Kingdom-wide survey of clinicians.
In response to the need for further research in this important area, the authors interviewed clinicians who responded to the survey in order to explore their views on a proposed plaster cast and functional bracing protocol to be used in a future trial comparing the two protocols. The interviews were also used to explore their views on the acceptability and feasibility of the proposed future trial. The emerging themes highlighted the need for research to reflect clinical practice, alongside common barriers to conducting clinical multi-centre studies.
Many of these themes have previously been identified and, more recently, integrated into a framework for developing interventions which contain different interacting facets, such as Achilles tendon rehabilitation.15 Further research in this area was supported by the 181 clinicians involved in this study and there was a consensus regarding the need for a pragmatic study design and adequate resources to run a large multi-centre trial. This highlights the clinical need to address this proposed research question.
This United Kingdom-wide survey and follow-up interviews represent a ‘snapshot’ of current practice. Broader generalisation to other healthcare systems and practices is limited, and the results of this research should therefore be extrapolated to other healthcare systems with caution.
Although research based on animal models has consistently shown the benefits of movement and load on healing tendons, evidence from clinical application is limited. This gap in the research literature has resulted in practice in the United Kingdom becoming varied and based on individual opinion. Future high-quality randomised trials on this subject are supported by the clinical community.
Funding Statement
The authors would like to thank R. Grant and K. Keates in their role as lay representatives, providing critical oversight for the project, and the British Orthopaedic Foot and Ankle Society for critically reviewing the survey and its distribution among its members. The lead author would also like to thank the National Institute for Health Research. This project was funded by a National Institute for Health Research Clinical Lectureship award. This article presents independent research funded by the National Institute for Health Research. The views expressed are those of the authors and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health.
Author contributions:R. S. Kearney: Contribution to study design, acquisition, analysis and interpretation of data. Drafted the manuscript, Gave final approval, Agrees to be accountable for all aspects of the work
N. Parsons: Contribution to study design, analysis and interpretation of data, Critically revised the article and gave final approval, Agrees to be accountable for all aspects of the work
M. Underwood: Contribution to study design and interpretation of data, Critically revised the article and gave final approval, Agrees to be accountable for all aspects of the work
M. L. Costa: Contribution to study design, analysis and interpretation of data, Critically revised the article and gave final approval, Agrees to be accountable for all aspects of the work
ICMJE Conflict of Interest:None declared
Supplementary material. A table providing rehabilitation facets for plaster cast only, plaster cast followed by orthoses, and orthoses only is available alongside the online version of this article at www.bjr.boneandjoint.org.uk
References
- 1.Evans NA, Stanish WD. The basic science of tendon injuries. Curr Orthop 2000;14:403–412. [Google Scholar]
- 2.Maffulli N, Waterston SW, Squair J, Reaper J, Douglas AS. Changing incidence of Achilles tendon rupture in Scotland: a 15-year study. Clin J Sport Med 1999;9:157–160. [DOI] [PubMed] [Google Scholar]
- 3.Costa ML, MacMillan K, Halliday D, et al. Randomised controlled trials of immediate weight-bearing mobilisation for rupture of the tendo Achillis. J Bone Joint Surg [Br] 2006;88-B:69–77. [DOI] [PubMed] [Google Scholar]
- 4.Suchak AA, Spooner C, Reid DC, Jomha NM. Postoperative rehabilitation protocols for Achilles tendon ruptures: a meta-analysis. Clin Orthop Relat Res 2006;445:216–221. [DOI] [PubMed] [Google Scholar]
- 5.Healy B, Beasley R, Weatherall M. Venous thromboembolism following prolonged cast immobilisation for injury to the tendo Achillis. J Bone Joint Surg [Br] 2010;92-B:646–650. [DOI] [PubMed] [Google Scholar]
- 6.Costa ML, Kay D, Donell ST. Gait abnormalities following rupture of the tendo Achillis: a pedobarographic assessment. J Bone Joint Surg [Br] 2005;87-B:1085–1088. [DOI] [PubMed] [Google Scholar]
- 7.Kearney RS, Lamb SE, Achten J, Parsons NR, Costa ML. In-shoe plantar pressures within ankle-foot orthoses: implications for the management of achilles tendon ruptures. Am J Sports Med 2011;39:2679–2685. [DOI] [PubMed] [Google Scholar]
- 8.Kearney RS, McGuinness KR, Achten J, Costa ML. A systematic review of early rehabilitation methods following a rupture of the Achilles tendon. Physiotherapy 2012;98:24–32. [DOI] [PubMed] [Google Scholar]
- 9.No authors listed. The Diagnosis and Treatment of Acute Achilles Tendon Rupture: Guideline and Evidence Report December 2009. AAOS. http://www.aaos.org/research/guidelines/atrguideline.pdf (date last accessed 23 February 2015).
- 10.No authors listed. Survey Monkey. http://www.surveymonkey.com/ (date last accessed 23 February 2015).
- 11.Enwemeka CS. Functional loading augments the initial tensile strength and energy absorption capacity of regenerating rabbit Achilles tendons. Am J Phys Med Rehabil 1992;71:31–38. [DOI] [PubMed] [Google Scholar]
- 12.Enwemeka CS, Spielholz NI, Nelson AJ. The effect of early functional activities on experimentally tenotomized Achilles tendons in rats. Am J Phys Med Rehabil 1988;67:264–269. [PubMed] [Google Scholar]
- 13.Saleh M, Marshall PD, Senior R, MacFarlane A. The Sheffield splint for controlled early mobilisation after rupture of the calcaneal tendon: a prospective, randomised comparison with plaster treatment. J Bone Joint Surg [Br] 1992;74-B:206–209. [DOI] [PubMed] [Google Scholar]
- 14.Khan RJ, Fick D, Brammar TJ, Crawford J, Parker MJ. Interventions for treating acute Achilles tendon ruptures. Cochrane Database Syst Rev 2004;3:CD003674. [DOI] [PubMed] [Google Scholar]
- 15.No authors listed. Developing and evaluating complex interventions: new guidance. MRC. http://www.mrc.ac.uk (date last accessed 23 February 2015).