Abstract
Little is known about the genetic characteristics, distribution, and transmission cycles of Cryptosporidium species that cause human disease in New Zealand. To address these questions, 423 fecal specimens containing Cryptosporidium oocysts and obtained from different regions were examined by the PCR-restriction fragment length polymorphism technique. Indeterminant results were resolved by DNA sequence analysis. Two regions supplied the majority of isolates: one rural and one urban. Overall, Cryptosporidium hominis accounted for 47% of the isolates, with the remaining 53% being the C. parvum bovine genotype. A difference, however, was observed between the Cryptosporidium species from rural and urban isolates, with C. hominis dominant in the urban region, whereas the C. parvum bovine genotype was prevalent in rural New Zealand. A shift in transmission cycles was detected between seasons, with an anthroponotic cycle in autumn and a zoonotic cycle in spring. A novel Cryptosporidium sp., which on DNA sequence analysis showed a close relationship with C. canis, was detected in two unrelated children from different regions, illustrating the genetic diversity within this genus.
Almost seventy years elapsed between the first observation of Cryptosporidium by Edward Tyzzer in 1907 (37) and the realization in 1976 that it was a human pathogen (9). Cryptosporidium is an apicomplexan parasite that causes gastrointestinal illness in as many as 152 mammals (10) and numerous other vertebrates. Immunocompetent humans are usually parasitized only by either the Cryptosporidium hominis or the C. parvum bovine genotype (2, 8, 19, 21, 23, 24, 29, 31, 35, 40, 42); however, an increasing number of Cryptosporidium species and genotypes are being implicated as a cause of diarrheal disease in the immunocompetent human population. These include C. meleagridis (30), C. felis (44), C. canis (44), C. parvum cervine genotype (28), and a C. parvum pig genotype (28). We add to this list a novel Cryptosporidium genotype that phylogenetically clustered closest to C. canis and was isolated from two unrelated immunocompetent children. The rapid increase in Cryptosporidium research since 1976 has seen the number of valid species increase to 20 (27) and decrease to 10 (10), and it is now on the rise again to 13 (32). Clearly, there is great genetic diversity within the genus with more species, genotypes, and variants likely to be uncovered by more-sensitive molecular techniques (6, 12, 13, 15-17, 22, 25, 41).
New Zealand's economy is based on primary food production with dairy, beef, and sheep farming playing the largest role. A preliminary study (unpublished) of the national dairy herd as a potential reservoir for human infection found that 8.8% of 385 calves and 0.7% of 572 cows tested were infected with the C. parvum bovine genotype. In the present study we characterize 423 human Cryptosporidium-positive fecal specimens from New Zealand by β-tubulin PCR-restriction fragment length polymorphism (PCR-RFLP), 18S ribosomal DNA (rDNA) PCR-RFLP, and 18S rDNA sequencing.
MATERIALS AND METHODS
Fecal specimens.
Between August 2000 and August 2003 several medical diagnostic laboratories in the North Island of New Zealand and one in the South Island forwarded 423 human fecal specimens found to contain Cryptosporidium oocysts to the Protozoa Research Unit (PRU) (Table 1). Since it is not a medical diagnostic laboratory, the PRU had to rely on fecal specimens that tested positive for the presence of Cryptosporidium oocysts that were referred to it. Two laboratories referred the majority of fecal specimens. One was in Hamilton, a city that services a large intensively dairy farmed region, and the other was in Wellington, a metropolitan district. The fecal specimens did not contain any preservatives and were stored at 4°C until examined.
TABLE 1.
Geographic distribution of Cryptosporidium spp. from human infections in New Zealand
| Locality | No. of isolates
|
|||
|---|---|---|---|---|
| C. hominis | C. parvum bovine genotype | Novel genotype | Totala | |
| Wellington | 109 | 13 | 122 | |
| Hamilton | 40 | 72 | 1 | 113 |
| Hawkes Bay | 21 | 15 | 36 | |
| Southland | 1 | 34 | 35 | |
| Bay of Plenty | 6 | 27 | 33 | |
| Hutt Valley | 12 | 12 | 1 | 25 |
| All others | 9 | 50 | 59 | |
Only localities that referred more than 20 fecal specimens are included.
From time to time the PRU surveys animal populations. Cryptosporidium oocysts from a wild rabbit fecal specimen were isolated, characterized, and used for phylogenetic purposes in the present study.
Oocyst isolation.
Oocysts were concentrated and removed from the majority of the fecal debris by the formal saline-diethyl ether method (1). A Dynabeads G/C-Combo immunomagnetic bead separation kit (Dynal Biotech ASA, Oslo, Norway) was used to isolate the concentrated oocysts from the remaining heavy fecal debris by following the manufacturer's instructions with minor modifications. Briefly, the oocyst concentrate was made up to 1 ml with water in a microcentrifuge tube, and 100-μl volumes of 10× buffers A and B, plus 25 μl of anti-Cryptosporidium-coated paramagnetic beads, were added to the oocysts. The mixture was gently rotated for 1 h at 8 rpm on a Labquake shaker/rotisserie (Barnstead/Thermolyne, Dubuque, Iowa). A magnet, fixed in a housing capable of holding a microcentrifuge tube (made in house), was used to capture the oocyst-bead complex. Debris was removed by washing the oocyst-bead complex twice with 1 ml of 1× buffer A. Oocysts were separated from the beads by the addition of 50 μl of 0.1 M HCl for 10 min with 10 s of vortexing at the start and end of the incubation period. The beads were captured with the magnet before the oocyst suspension was collected and neutralized with 5 μl of 1 M NaOH. Oocysts were stored at 4°C until processed.
Nucleic acid extraction.
To each 55 μl of oocyst suspension, 75 μl of TE buffer (1 mM Tris-HCl and 0.5 mM EDTA) containing 1% Nonidet-P 40 and 20 μl of a 20% suspension of Chelex 100 resin (Bio-Rad Laboratories, Hercules, Calif.) were added. The oocysts were subjected to five freeze-thaw cycles of 2 min in liquid air, followed by 2 min in water at 96°C. Cell debris and Chelex 100 resin were deposited by centrifugation at 10,000 × g for 1 min. The supernatant containing the nucleic acid was stored at 4°C until processed.
PCR amplification.
Initially, all specimens were amplified with the primers for the β-tubulin gene as previously described (5). A PCR product of 592 bp was expected. Any specimens that did not produce a PCR product were reexamined with a nested primer technique targeting the variable region of the 18S rRNA gene. The β-tubulin gene is thought to exist as a single-copy gene per sporozoite (38), and as such it is does not provide as large a DNA template for PCR amplification as did the five-copy 18S rDNA. Each oocyst will thus have 4 copies of the β-tubulin gene available for PCR amplification but 20 copies of the 18S rDNA. The nested primer PCR technique helps to increase the sensitivity of oocyst detection in specimens that contain small numbers of oocysts. Primers for the 18S rDNA were designed by using Primer3 (version 0.9; http://www-genome.wi.mit.edu/genomesoftware/other/primer3.html). The outer primer pair of CRY-L1 (5′-GTT AAA CTG CGA ATG GCT CA) and Cry-L2 (5′-CCA TTT CCT TCG AAA CAG GA) and the inner primer pair of CRY-S1 (5-CTC GAC TTT ATG GAA GGG TTG) and CRY-S2 (5′-CCT CCA ATC TCT AGT TGG CAT A) amplified a 1,397-bp fragment and an 832-bp fragment, respectively. Each 20-μl volume of PCR mixture contained 1× PCR reagent buffer (Invitrogen Life Technologies, Carlsbad, Calif.), 250 μM concentrations of each deoxynucleoside triphosphate, 1.5 mM MgCl2, 100 nM concentrations of each primer, 2.5 U of Taq polymerase, and 1 μl of DNA template. Cycling conditions consisted of an initial denaturation step of 96°C for 2 min, followed by 35 cycles of 94°C for 30 s, 56°C for 30 s, and 72°C for 45 s, and finally elongation at 72°C for 5 min. PCR amplification was performed in a Perkin-Elmer GeneAmp PCR System 9700 thermal cycler. All PCR products were analyzed by electrophoresis in 1.6% ultrapure DNA-grade agarose (Bio-Rad), stained with ethidium bromide, and visualized on a UV transilluminator.
PCR-RFLP analysis.
All β-tubulin PCR products were digested with the restriction enzyme DdeI at 37°C for 3 h (5) and fractionated by electrophoresis in a 3.5% Metaphor agarose gel (BioWhittaker Molecular Applications, Rockland, Maine), stained with ethidium bromide, and visualized on a UV transilluminator. The C. parvum bovine genotype PCR product contains a DdeI restriction site that gives two bands of 178 and 414 bp. This site is not present in C. hominis, so a single band of 592 bp is observed.
The 18S rRNA gene PCR products were digested with SspI and VspI, as previously described (40), and then analyzed as described above.
18S rDNA PCR sequence and phylogenetic analysis.
The 832-bp band containing the 18S rDNA was purified by using a QIAquick gel extraction kit (Qiagen GmbH, Hilden, Germany) by following the manufacturer's instructions. An ABI 3730 DNA analyzer (Applied Biosystems) was used to sequence overlapping bidirectional strands of PCR product with at least two PCR products from each fecal specimen sequenced to ensure accuracy. Sequences were assembled with Perkin-Elmer's MT Navigator software and aligned by using CLUSTAL X (36). To aid phylogenetic analysis, 18S rDNA sequences obtained from GenBank were used in a multiple sequence alignment along with human, bovine, dog, and rabbit Cryptosporidium sequences from New Zealand isolates. A phylogenetic tree was constructed with PAUP software (34) by using the neighbor-joining method and a general time-relative model to calculate genetic distances. The reliability of branches in the tree were tested by bootstrap values obtained from 1,000 pseudoreplications, with C. serpentis as an outgroup.
Nucleotide sequence accession numbers.
Published 18S rDNA sequences used for phylogenetic analysis included the following: C. andersoni, accession number AB089285; C. baileyi, AF093495 (40); C. canis, AF112576 (42); C. felis, AF112575 (42); C. meleagridis, AF112574 (42); C. muris, AF093498] (40); C. hominis, AF093489 (40); C. parvum bovine genotype, AF108864 (26); C. parvum pig genotype, AF115377 (42); C. serpentis, AF093502 (40); and C. wrairi, AF115378 (42). The two novel Cryptosporidium sequences and a C. parvum rabbit genotype sequence used to interpret results have been deposited with GenBank under the accession numbers AY458612 to AY458614.
RESULTS
β-Tubulin PCR-RFLP.
Of the 423 specimens, 405 gave the expected 592-bp PCR product for the β-tubulin gene. PCR-RFLP analysis of this fragment showed that 188 isolates (46%) were C. hominis and 217 isolates (54%) were C. parvum bovine genotype.
18S rDNA PCR-RFLP and sequencing.
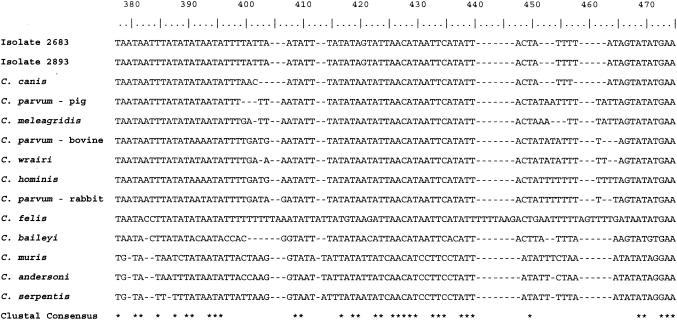
The 18 human Cryptosporidium isolates that failed to produce a β-tubulin product were amplified by using the 18S rDNA primers. PCR-RFLP analysis was carried out, and the products were sequenced, showing 10 to be C. hominis, 6 to be C. parvum bovine genotype, and 2 to be a novel genotype. All 18 products were sequenced and aligned over ca. 734 bp, depending on the variation in length of the individual sequences, by using CLUSTAL X (Fig. 1). The two novel isolates were most similar to sequences obtained from dog isolates. A search of the GenBank database did not find an exact match for the two novel Cryptosporidium 18S rDNA sequences which differed from each other only by an A-to-G substitution at position 587. Phylogenetic analysis of the Cryptosporidium genus by neighbor joining also grouped the novel isolate most closely with C. canis (Fig. 2).
FIG. 1.
DNA sequence alignment through the variable region of the Cryptosporidium 18S rDNA, including the novel isolates 2683 and 2893 and the rabbit isolate. Nucleotide position is based on the 734-bp length of aligned sequence and, depending on gaps in the individual sequences, the actual positions are an approximation.
FIG. 2.
Neighbor-joining tree analysis of Cryptosporidium 18S rDNA showing the phylogenetic relationship of two novel isolates to others in the genus. Analysis was based on genetic distances calculated by the general time-reversible model. C. serpentis was used as an outgroup with 1,000 bootstrap pseudoreplications.
Genotype geographic distribution.
Geographic distribution of the two main Cryptosporidium species causing human infection reflected the land use of the regions from which specimens were referred. The isolates recovered from the Hamilton specimens consisted of 40 (35%) C. hominis, 72 (64%) C. parvum bovine genotype, and 1 novel C. canis-like genotype. Isolates from Wellington were in direct contrast with 109 (89%) C. hominis and 13 (11%) C. parvum bovine genotypes. The remaining isolates were all from provincial New Zealand: 49 (26%) C. hominis, 138 (73%) C. parvum bovine genotype, and 1 novel C. canis-like genotype (Table 1). All provincial centers referred more C. parvum bovine genotype than C. hominis with the exception of Hawke's Bay, which referred 21 C. hominis-positive specimens during the autumn cryptosporidiosis peak and 15 C. parvum bovine genotype-positive specimens during the spring cryptosporidiosis peak. Southland, which is undergoing a boom in dairy farming, referred 35 positive specimens, 34 of which were of the C. parvum bovine genotype.
Cryptosporidium species seasonality.
There was a marked seasonal shift in transmission route between spring, when almost all human infections were caused by the zoonotic C. parvum bovine genotype, and autumn, when the anthroponotic C. hominis was dominant (Fig. 3). This pattern has been noted previously (14, 18).
FIG.3.
Seasonal shift in transmission route between C. parvum and C. hominis human infections.
DISCUSSION
We examined the distribution and transmission cycles of Cryptosporidium species in New Zealand's human population and evaluated the implications for public health. The results were similar to those of previous studies (18, 29).
One laboratory in Hamilton and another in Wellington forwarded their Cryptosporidium-positive fecal samples to the PRU over the period of the study. Other laboratories provided specimens on a more sporadic basis for a total of 423 specimens. Enough specimens were received by the PRU for conclusions to be postulated.
PCR-RFLP of the β-tubulin gene was successful for 405 of the 423 human isolates, differentiating them into C. hominis and the C. parvum bovine genotype. Early in the study the 18S rRNA region of 20 of the 405 isolates was amplified and sequenced to check for agreement between the two methods. In every case, the results from β-tubulin PCR-RFLP and the sequenced 18S rDNA concurred. Also, there was no variation within the C. hominis sequences or the C. parvum bovine genotype sequences. PCR-RFLP of the β-tubulin gene is therefore a consistent, reliable, and rapid method that can be used with confidence for speciating isolates from human fecal samples.
In the present study, an isolate from the colon of a shot wild rabbit was characterized. Multilocus PCR-RFLP was performed on 18S rDNA, rDNA internal transcribed spacer region 1 (20), β-tubulin gene (5), Cryptosporidium oocyst wall protein gene (35), a polythreonine repeat motif (7), and the ribonucleotide reductase R1 subunit locus (39), with all of the results indicating C. hominis. The sequence, however, from the 18S rDNA region of this isolate was not identical to that of C. hominis (Fig. 1). This sequence was included in the phylogenetic analysis of strains for the present study (Fig. 2, C. parvum-rabbit). Although the sequence is unique and first published by Xiao, it is still most similar to the human genotype (32, 43).
A novel Cryptosporidium genotype that clustered closely to C. canis was detected in fecal specimens from two children (24 and 14 months of age): one in Hamilton and one in Upper Hutt (close to Wellington). Both strains were detected by nested 18S rDNA PCR, and then only a small amount of PCR product was produced, indicating a light oocyst load with a genotype that may have accidentally infected humans.
The overall numeric distribution of Cryptosporidium species was almost equally divided: 198 (46.8%) C. hominis specimens and 223 (52.7%) C. parvum bovine genotype specimens, along with 2 C. canis-like genotype specimens (0.5%). This distribution of Cryptosporidium species does not give the full picture, since when the provincial regions are compared to metropolitan Wellington there is a marked difference. Wellington had 109 (89%) C. hominis isolates and 13 (11%) C. parvum bovine genotype isolates, whereas the provincial regions included 89 (30%) C. hominis and 210 (70%) C. parvum bovine genotype isolates, with 2 C. canis-like genotype specimens. New Zealand's temperate climate allows livestock to remain outdoors on pasture year-round, with the Hamilton region having two calving seasons, resulting in a potential for an increase in the environmental load of oocysts. The spreading of ponded milking shed washings and meat-processing plant effluent as fertilizer onto the land, plus frequent mild rainfall, also disperses the oocysts over pastures and ultimately into rivers and streams. An earlier study found Cryptosporidium oocysts to be present in 12.6% of environmental and treated waters tested from throughout New Zealand (4). With today's better sampling, recovery, and detection procedures, this number would be expected to be higher. People living in Wellington have less opportunity for contact with farm animals but would have more chance of being involved in outbreak situations, be it transmitted person to person, water borne, or food borne. The lack of access to farm animals rather than the lack of animals has previously been suggested as an explanation for a decline in cryptosporidiosis caused by C. parvum bovine genotype (11).
Cryptosporidiosis has been a notifiable disease in New Zealand since July 1996, with case numbers rising each year. New Zealand's infection rate (i.e., cases per 100,000) for the years 2001 and 2002 were 32.3 and 26.1, respectively; however, the rates for both Hamilton (61.2 and 40) and Wellington (37.4 and 61) were above the national rate (3). Although the national infection rate fell during 2002, Wellington's infection rate increased to 61 as it experienced 2 swimming pool outbreaks resulting in 72 cases of cryptosporidiosis with C. hominis. Notified cases have a distinct seasonal pattern, usually showing two clear peaks during spring and autumn (3) (Fig. 4). The autumns of 2000 and 2002, however, did not show peaks, which might be attributed to below average rainfall during autumn for those years (33), and showed a lack of outbreaks. Spring is the main calving and lambing season and, since Cryptosporidium is a disease of young animals, this is the time of year when there is a high environmental load with the C. parvum bovine genotype. The C. parvum bovine genotype was responsible for almost all of the spring cryptosporidiosis cases before a complete change of transmission cycle saw C. hominis becoming dominant in the autumn. This seasonality was reflected in the Hamilton specimens, with C. hominis prevalent in the autumn and C. parvum bovine genotype prevalent in the spring. Wellington referred fewer positive fecal specimens in the spring, which may reflect the lack of access to young infected animals by its population. Figure 3 shows this seasonal shift in transmission cycles. Since humans are usually infected only by C. hominis or C. parvum bovine genotype, a more discriminating method, other than PCR-RFLP and 18S rDNA sequencing, may be needed to investigate outbreaks for potential sources.
FIG.4.
National monthly number of human cryptosporidiosis cases since the disease became notifiable in July 1996.
New Zealand's climate and animal husbandry and farming practices are ideally suited to the spread and survival of Cryptosporidium oocysts. Fencing off rivers and streams or planting riparian buffer zones along stream banks could restrict the access of livestock and their excreta to natural waterways. At present, the government is considering submissions on public access across private land to natural waterways, with the fencing of buffer zones being one possibility. Fonterra, New Zealand's largest dairy company, which is a cooperative owned by farmers, is actively encouraging its shareholders to fence off esplanade strips along natural waterways to reduce the concept of “dirty dairying.” Effective wastewater management of effluent from farms, meat-processing plants, settlements, towns, and cities could interrupt the transmission cycle, along with keeping the water reticulation of toddlers' public swimming pools separate from the main swimming pool. The tracing of outbreak sources requires molecular techniques capable of discriminating differences within Cryptosporidium species and genotypes. Vigilance with public health education programs and strict adherence to the New Zealand Drinking Water Standards would also help to lower the infection rate.
Acknowledgments
We gratefully acknowledge the continued financial support and cooperation of the New Zealand Ministry of Health.
We thank Jan Bird (formerly of MedLab Hamilton) and Vicki McKnight (Wellington Medical Laboratory), along with many other medical laboratory scientists, for providing specimens. We also thank Trish McLenachan and Matthew Phillips of the Alan Wilson Centre for Molecular Ecology and Evolution for phylogenetic advice and help with the manuscript.
REFERENCES
- 1.Allen, A. V. H., and D. S. Ridley. 1970. Further observations on the formal ether concentration technique for faecal parasites. J. Clin. Pathol. 23:545-546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Awad-El-Kariem, F. M., H. A. Robinson, D. A. Dyson, D. Evans, S. Wright, M. T. Fox, and V. McDonald. 1995. Differentiation between animal and animal strains of Cryptosporidium parvum using isoenzyme typing. Parasitology 110:129-132. [DOI] [PubMed] [Google Scholar]
- 3.Baker, M. 2003. Monthly surveillance reports: September 2003. [Online.] Environmental Science and Research, Ltd., Wellington, New Zealand. http://www.esr.cri.nz.
- 4.Brown, T. J., G. Ionas, J. J. Learmonth, E. A. Keys, and P. A. McLenachan. 1998. The distribution of Giardia and Cryptosporidium in New Zealand waters: a nationwide study. Water Waste New Zealand 101:60-63. (Erratum, 102:58.) [Google Scholar]
- 5.Caccio, S., W. Homan, K. van Dijk, and E. Pozio. 1999. Genetic polymorphism at the β-tubulin locus among human and animal isolates of Cryptosporidium parvum. FEMS Microbiol. Lett. 170:173-179. [DOI] [PubMed] [Google Scholar]
- 6.Caccio, S., F. Spano, and E. Pozio. 2001. Large sequence variation at two microsatellite loci among zoonotic (genotype C) isolates of Cryptosporidium parvum. Int. J. Parasitol. 31:1082-1086. [DOI] [PubMed] [Google Scholar]
- 7.Carraway, M., S. Tzipori, and G. Widmer. 1997. A new restriction length polymorphism from Cryptosporidium parvum identifies genetically heterogeneous parasite populations and genotypic changes following transmission from bovine to human hosts. Infect. Immun. 65:3958-3960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carraway, M., S. Tzipori, and S. Widmer. 1996. Identification of genetic heterogeneity in the Cryptosporidium parvum ribosomal repeat. Appl. Environ. Microbiol. 62:712-716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Casemore, D. P., S. E. Wright, and R. L. Cook. 1997. Cryptosporidiosis: human and animal epidemiology, p. 65-92. In R. Fayer (ed.), Cryptosporidium and cryptosporidiosis. CRC Press, Inc., Boca Raton, Fla.
- 10.Fayer, R., U. Morgan, and S. J. Upton. 2000. Epidemiology of Cryptosporidium: transmission, detection and identification. Int. J. Parasitol. 30:1305-1322. [DOI] [PubMed] [Google Scholar]
- 11.Hunter, P. R., R. M. Chalmers, Q. Syed, L. S. Hughes, S. Woodhouse, and L. Swift. 2003. Foot and mouth disease and cryptosporidiosis: possible interaction between two emerging infectious diseases. Emerg. Infect. Dis. 9:109-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khramtsov, N. V., P. Chung, C. C. Dykstra, J. K. Griffiths, U. M. Morgan, M. J. Arrowood, and S. J. Upton. 2000. Presence of double-stranded RNAs in human and calf isolates of Cryptosporidium parvum. J. Parasitol. 86:275-282. [DOI] [PubMed] [Google Scholar]
- 13.Khramtsov, N. V., K. M. Woods, M. V. Nesterenko, C. C. Dykstra, and S. J. Upton. 1997. Virus-like, double-stranded RNAs in the parasite protozoan Cryptosporidium parvum. Mol. Microbiol. 26:289-300. [DOI] [PubMed] [Google Scholar]
- 14.Learmonth, J. J., G. Ionas, A. B. Pita, and R. S. Cowie. 2001. Seasonal shift in Cryptosporidium parvum transmission cycles in New Zealand. J. Eukaryote Microbiol. 48:34S-35S. [DOI] [PubMed]
- 15.Leoni, F., C. I. Gallimore, J. Green, and J. McLauchlin. 2003. Molecular epidemiological analysis of Cryptosporidium isolates from humans and animals by using a heteroduplex mobility assay and nucleic acid sequencing based on a small double-stranded RNA element. J. Clin. Microbiol. 41:981-992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leoni, F., C. I. Gallimore, J. Green, and J. Mc Lauchlin. 2003. A rapid method for identifying diversity within PCR amplicons using a heteroduplex mobility assay and synthetic polynucleotides: application to characterisation of dsRNA elements associated with Cryptosporidium. J. Microbiol. Methods 54:95-103. [DOI] [PubMed] [Google Scholar]
- 17.Mallon, M., A. MacLeod, J. Wastling, H. Smith, B. Reilly, and A. Tait. 2003. Population structures and the role of genetic exchange in the zoonotic pathogen Cryptosporidium parvum. J. Mol. Evol. 56:407-417. [DOI] [PubMed] [Google Scholar]
- 18.McLauchlin, J., C. Amar, S. Pedraza-Diaz, and G. Nichols. 2000. Molecular epidemiological analysis of Cryptosporidium spp. in the United Kingdom: results of genotyping Cryptosporidium spp. in 1,705 fecal samples from humans and 105 fecal samples from livestock animals. J. Clin. Microbiol. 38:3984-3990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McLauchlin, J., S. Pedraza-Diaz, C. Amar-Hoetzeneder, and G. L. Nichols. 1999. Genetic characterization of Cryptosporidium strains from 218 patients with diarrhea diagnosed as having sporadic cryptosporidiosis. J. Clin. Microbiol. 37:3153-3158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morgan, U., P. Deplazes, D. A. Forbes, F. Spano, H. Hertzberg, K. D. Sargent, A. Elliot, and R. C. A. Thompson. 1999. Sequence and PCR-RFLP analysis of the internal transcribed spacers of the rRNA repeat unit in isolates of Cryptosporidium parvum from different hosts. Parasitology 118:49-58. [DOI] [PubMed] [Google Scholar]
- 21.Morgan, U., K. D. Sargent, P. Deplazes, D. A. Forbes, F. Spano, H. Hertzberg, A. Elliot, and R. C. A. Thompson. 1998. Molecular characterisation of Cryptosporidium from various hosts. Parasitology 117:31-37. [DOI] [PubMed] [Google Scholar]
- 22.Morgan, U., L. Xiao, R. Fayer, A. A. Lal, and R. C. A. Thompson. 1999. Variation in Cryptosporidium: towards a taxonomic revision of the genus. Int. J. Parasitol. 29:1733-1751. [DOI] [PubMed] [Google Scholar]
- 23.Morgan, U. M., C. C. Constantine, D. A. Forbes, and R. C. A. Thompson. 1997. Differentiation between human and animal isolates of Cryptosporidium parvum using rDNA sequencing and direct PCR analysis. J. Parasitol. 83:825-830. [PubMed] [Google Scholar]
- 24.Morgan, U. M., C. C. Constantine, P. O'Donoghue, B. P. Meloni, P. A. O'Brien, and R. C. A. Thompson. 1995. Molecular characterization of Cryptosporidium isolates from humans and other animals using random amplified polymorphic DNA analysis. Am. J. Trop. Med. Hyg. 52:559-564. [DOI] [PubMed] [Google Scholar]
- 25.Morgan, U. M., P. T. Monis, R. Fayer, P. Deplazes, and R. C. A. Thompson. 1999. Phylogenetic relationships among isolates of Cryptosporidium: evidence for several new species. J. Parasitol. 85:1126-1133. [PubMed] [Google Scholar]
- 26.Morgan, U. M., L. Xiao, R. Fayer, T. K. Graczyk, A. A. Lal, P. Deplazes, and R. C. A. Thompson. 1999. Phylogenetic analysis of Cryptosporidium isolates from captured reptiles using 18S rDNA sequence data and random amplified polymorphic DNA analysis. J. Parasitol. 85:525-530. [PubMed] [Google Scholar]
- 27.O'Donoghue, P. J. 1995. Cryptosporidium and cryptosporidiosis in man and animals. Int. J. Parasitol. 25:139-195. [DOI] [PubMed] [Google Scholar]
- 28.Ong, C. S. L., D. L. Eisler, A. Alikhani, V. W. K. Fung, J. Tomblin, W. R. Bowie, and J. L. Isaac-Renton. 2002. Novel Cryptosporidium genotypes in sporadic cryptosporidiosis cases: first report of human infections with a cervine genotype. Emerg. Infect. Dis. 8:263-268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ong, C. S. L., D. L. Eisler, S. H. Goh, J. Tomblin, F. M. Awad-El-Kariem, C. B. Beard, L. Xiao, I. Sulaiman, A. Lal, M. Fyfe, A. King, W. R. Bowie, and J. Isaac-Renton. 1999. Molecular epidemiology of cryptosporidiosis outbreaks and transmission in British Columbia, Canada. Am. J. Trop. Med. Hyg. 61:63-69. [DOI] [PubMed] [Google Scholar]
- 30.Pedraza-Diaz, S., C. Amar, and J. McLauchlin. 2000. The identification and characterization of an unusual genotype of Cryptosporidium from human feces as Cryptosporidium meleagridis. FEMS Microbiol. Lett. 189:189-194. [DOI] [PubMed] [Google Scholar]
- 31.Peng, M. M., L. Xiao, A. R. Freeman, M. J. Arrowood, A. A. Escalante, A. C. Weltman, C. S. L. Ong, W. B. McKenzie, A. A. Lal, and C. B. Beard. 1997. Genetic polymorphism among Cryptosporidium parvum isolates: evidence of two distinct human transmission cycles. Emerg. Infect. Dis. 3:567-573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ryan, U., L. Xiao, C. Read, L. Zhou, A. A. Lal, and I. Pavlasek. 2003. Identification of novel Cryptosporidium genotypes from the Czech Republic. Appl. Environ. Microbiol. 69:4302-4307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Salinger, J. 2002. Climate summaries. National Institute of Water and Atmospheric Research. [Online.] http://www.niwa.cri.nz.
- 34.Softord, D. L. 1999. PAUP, 4.65 ed. Sinauer Associates, Sutherland, Mass.
- 35.Spano, F., L. Putignani, J. McLauchlin, D. P. Casemore, and A. Crisanti. 1997. PCR-RFLP analysis of the Cryptosporidium oocyst wall protein (COWP) gene determines between C. wrairi and C. parvum, and between C. parvum isolates of human and animal origin. FEMS Microbiol. Lett. 150:209-217. [DOI] [PubMed] [Google Scholar]
- 36.Thompson, J. D., T. J. Gibson, G. Plewnaik, F. Jeanmougin, and D. G. Higgins. 1997. The ClustalX Windows interface: flexible strategies for multiple sequence alignment aided by quality analysis tools. Nucleic Acids Res. 24:4876-4882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tyzzer, E. E. 1907. A sporozoon found on the peptic glands of the common mouse. Proc. Soc. Exp. Biol. Med. 5:12-13. [Google Scholar]
- 38.Widmer, G., L. Tchack, C. Chappell, and S. Tzipori. 1998. Sequence polymorphism in the β-tubulin gene reveals heterogeneous and variable population structures in Cryptosporidium parvum. Appl. Environ. Microbiol. 64:4477-4481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Widmer, G., S. Tzipori, C. J. Fitchenbaum, and J. K. Griffiths. 1998. Genotypic and phenotypic characterisation of Cryptosporidium parvum isolates from people with AIDS. J. Infect. Dis. 178:834-840. [DOI] [PubMed] [Google Scholar]
- 40.Xiao, L., L. Escalante, C. Yang, I. Sulaiman, A. A. Escalante, R. J. Montali, R. Fayer, and A. A. Lal. 1999. Phylogenetic analysis of Cryptosporidium parasites based on the smaller subunit rRNA gene locus. Appl. Environ. Microbiol. 65:1578-1583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xiao, L., J. Limor, C. Bern, and A. A. Lal. 2001. Tracking Cryptosporidium parvum by sequence analysis of small double-stranded RNA. Emerg. Infect. Dis. 7:141-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Xiao, L., U. M. Morgan, J. Limor, L. J. Escalante, M. J. Arrowood, W. Shulaw, R. C. A. Thompson, R. Fayer, and A. A. Lal. 1999. Genetic diversity within Cryptosporidium parvum and related Cryptosporidium species. Appl. Environ. Microbiol. 65:3386-3391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Xiao, L., I. M. Sulaiman, U. M. Ryan, L. Zhou, E. R. Atwill, M. L. Tischler, X. Zhang, R. Fayer, and A. A. Lal. 2002. Host adaptation and host-parasite co-evolution in Cryptosporidium: implications for taxonomy and public health. Int. J. Parasitol. 32:1773-1785. [DOI] [PubMed] [Google Scholar]
- 44.Xiao, L. H., C. Bern, J. Limor, I. Sulaiman, J. Roberts, W. Checkley, L. Cabrera, R. H. Gilman, and A. A. Lal. 2001. Identification of 5 types of Cryptosporidium parasites in children in Lima, Peru. J. Infect. Dis. 183:492-497. [DOI] [PubMed] [Google Scholar]