Abstract
Background/Aims:
Information on eye diseases in blind school children in Allahabad is rare and sketchy. A cross-sectional study was performed to identify causes of blindness (BL) in blind school children with an aim to gather information on ocular morbidity in the blind schools in Allahabad and in its vicinity.
Study Design and Setting:
A cross-sectional study was carried out in all the four blind schools in Allahabad and its vicinity.
Materials and Methods:
The students in the blind schools visited were included in the study and informed consents from parents were obtained. Relevant ocular history and basic ocular examinations were carried out on the students of the blind schools.
Results:
A total of 90 students were examined in four schools of the blind in Allahabad and in the vicinity. The main causes of severe visual impairment and BL in the better eye of students were microphthalmos (34.44%), corneal scar (22.23%), anophthalmos (14.45%), pseudophakia (6.67%), optic nerve atrophy (6.67%), buphthalmos/glaucoma (3.33%), cryptophthalmos (2.22%), staphyloma (2.22%), cataract (2.22%), retinal dystrophy (2.22%), aphakia (1.11%), coloboma (1.11%), retinal detachment (1.11%), etc. Of these, 22 (24.44%) students had preventable causes of BL and another 12 (13.33%) students had treatable causes of BL.
Conclusion:
It was found that hereditary diseases, corneal scar, glaucoma and cataract were the prominent causes of BL among the students of blind schools. Almost 38% of the students had preventable or treatable causes, indicating the need of genetical counseling and focused intervention.
Keywords: Blind schools, cataract, corneal scar, hereditary diseases, ocular morbidity, prevention of blindness
Visual impairment (VI) is a worldwide problem that has a significant socioeconomic impact. Childhood blindness (BL) is a priority area because of the number of years of BL that ensues. Data on the prevalence and causes of BL and severe VI (SVI) in children are needed for planning and evaluating preventive and curative services, including planning special education and low vision services.[1]
Considering the fact that 30% of India's blind lose their eyesight before the age of 20 years and many of them are under five when they become blind, the importance of early detection and treatment of ocular disease and VI among young children is obvious.[2] Although BL in children is relatively uncommon, this age group is also considered a priority as severe visual loss in children can affect their development, mobility, education, and employment opportunities, which can have far reaching implications on the quality-of-life of children and affected families.[3,4]
India has an estimated 320,000 blind children, more than any other country in the world.[5] Even though this represents a small fraction of the total BL, the control of BL in children is one of the priority areas of the World Health Organization's (WHO) “vision 2020: The right to sight” program. This is a global initiative, which was launched by WHO in 1999 to eliminate avoidable BL worldwide by the year 2020.[6] The aim of vision 2020 is to reduce the current projection of 75 million blind people by the year 2020 to a target of 25 million. To achieve this, all the stakeholders, particularly the ophthalmologists and pediatricians, must play a leadership role.[7]
Information on the major causes of BL in children is required to design effective prevention of BL (PBL) programs.[8] Reliable, population-based data on the causes of BL in children are difficult to obtain in developing countries as registers of the blind do not exist, and very large sample sizes would be required for formal cross-sectional surveys. Alternative sources include the use of key informants and examination of children identified as blind in community-based rehabilitation programs. Examination of children in the special institution has increasingly been used to provide data on the causes of BL in children, but possible sources of bias need to be borne in mind. The standard reporting form for recording the causes of visual loss in children, developed by the International Centre for Eye Health, London for the WHO/PBL program[9] has been used in various states of India.[10,11]
Regrettably, there are inadequate data on causes and prevalence of ocular morbidities among children of the developing world. We aim in this paper to study the prevalence and causes of ocular morbidity among children with a view to amassing data that can be used to plan interventional measures that can stem the tide of avoidable BL.
Materials and Methods
This cross-sectional study was carried out in total 90 students of all four schools of the blind in Allahabad and in its vicinity from April 2012 to August 2013, a list of which was obtained from District Handicapped Welfare Officer, Allahabad. The required permission for screening of the children was obtained from the principal/headmaster of each school. The concerned authorities of each school were briefed about the aims and objectives of the study. The school authorities were requested to inform the parents of the children at the time of screening.
UNICEF defines childhood as 0–16 years inclusive. All students aged 16 years or less in the schools were included in the study. Students older than 16 years but who became blind before that age was also included.
An ophthalmologist and an optometrist examined the students in the respective school premises. The relevant information was collected from the class teachers and parents (whenever possible). The study included all the students of the blind school irrespective of age. Brief demographic details, medical and family history of each child were recorded. The ophthalmologists carried out a detailed eye examination of each student.
Visual acuity was assessed in each eye using a Snellen tumbling ‘E’ visual acuity test chart. The students who did not cooperate with the ‘E’ chart, were assessed for the ability to fix and follow light. Near vision were assessed using figures equivalent to N. The visual status of students was recorded using WHO categories of VI before and after refraction.
To categorize a student under low visual category, simple tests of functional vision were used as the ability to navigate around two chairs set 2 m apart unaided with a visual acuity of <20/60 to light perception; to recognize faces at a distance of 3 m and to recognize the shape of three two-cm symbols at any near distance. The students who failed to cooperate with these tests due to additional handicaps were judged on their visual behavior.
Refraction and low vision aid assessment were performed in all students who were able to perform the tests of functional vision by an optometrist. Anterior segments of the eye were examined using a light and loupe magnifier and/or with a handheld slit-lamp. The posterior segment was examined using direct and indirect ophthalmoscope after dilatation of the pupil.
The WHO/PBL program's eye examination record for children with BL and low vision was used to categorize the causes of BL and to record the findings using the definitions in the coding instructions.[9]
The anatomical classification of causes of visual loss defined that part of the eye which had been damaged leading to visual loss (such as cornea, lens, retina, optic nerve, whole globe). Where two or more anatomical sites were involved the major site was selected, or where two sites contributed equally, the most treatable condition was selected. For each student, the need of optical, medical or surgical interventions was recorded, and the visual prognosis was assessed. Students requiring further investigations and treatment procedures were referred. The data were entered into a database and analyzed using SPSS 11.0 for Windows. A report of the findings and recommendations was given to the principal of each school.
Definitions
The WHO in 1972 proposed a uniform criterion and defined BL as, “visual acuity of <20/400 (Snellen) or its equivalent.” In order to facilitate the screening of visual acuity by nonspecialized persons, in the absence of appropriate vision charts, the WHO in 1979 added the “Inability to count fingers in day-light at a distance of 3 m” to indicate vision <20/400 or its equivalent.
Results
A total of 90 students were examined in four schools of the blind in Allahabad and in its vicinity. The list of schools for blind visited is as follows:
Raj Blind School, Elgin Road, Allahabad
Arunima Blind School, Darbhanga Colony, Allahabad
The School and Home for the Blind (Blind Asylum), Naini, Allahabad
Bachpan Day Care Centre, Swaroop Rani Hospital Road, Allahabad.
In all 90 students who participated in the study, 65 (72.22%) were males and 25 (27.78%) were females. There is male preponderance in the study with the sex ratio (male:Female ratio) being 2.6:1. Of the 90, 2 students (2.22%) belonged to age ≤5 years, 26 students (28.89%) were between ages 6 and 10 years, 42 students (46.67%) were between ages 11 and 15 years, 20 students (22.22%) were belonged to age ≥16 years. The majority, that is, 71 (78.89%) students were from the rural area, and 19 (21.11%) students were from the urban area. Most of the students that is, 84 (93.33%) were Hindu and remaining, that is, 6 (6.67%) students were Muslim.
Only 3 (3.33%) students in blind schools were having an associated disability while the remaining 87 (96.67%) students were not having any associated disability. Among the 90 students who participated in the study, 6 (6.67%) students gave history of BL in the family members and rest 84 (93.33%) did not have had history of BL in family members. Parental consanguinity was identified in 5 cases (5.56%); no indication of consanguinity was reported in 57 cases (63.33%); and 28 cases (31.11%) were unknown because of lack of information. Almost all students (94.44%) were fluent in Braille.
We classified students in blind schools by socioeconomic status according to modified B. J. Prasad classification. We found that 56 (62.22%) students were from lower socioeconomic class, that is, Class IV and Class V [Table 1 and Fig. 1].
Table 1.
Distribution of students in blind schools by socioeconomic status according to modified B. J. Prasad classification
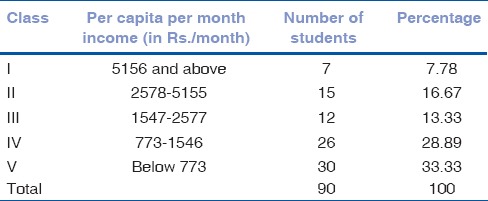
Figure 1.
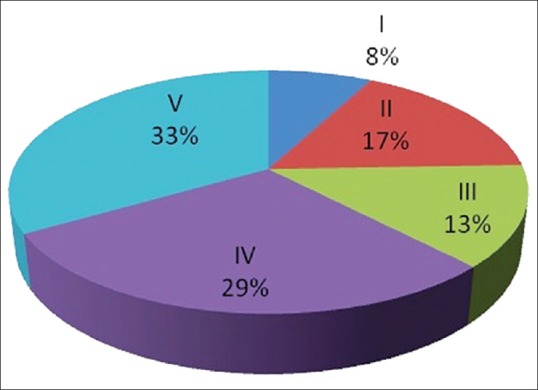
Distribution of students in blind schools by socioeconomic status according to modified B. J. Prasad classification in percentage
A total of 81 (90.00%) students were blind, 7 (7.78%) students were severely visually impaired and 2 (2.22%) students had no VI [Table 2 and Fig. 2].
Table 2.
Visual acuity (better eye) in blind school students
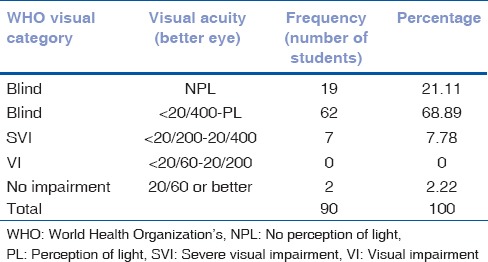
Figure 2.
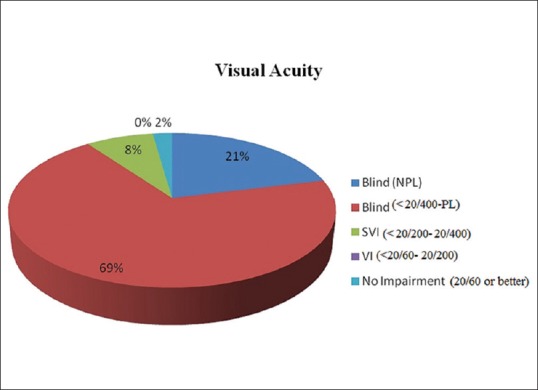
Visual acuity (better eye) in blind school students
In all 90 students who participated in the study, the whole globe 49 (54.44%), cornea 22 (24.45%), lens (10.00%), optic nerve 6 (6.67%), retina 3 (3.33%), and uvea 1 (1.11%) were found to be the affected sites causing BL or VI [Table 3 and Fig. 3].
Table 3.
Anatomical classification of the causes of VI in the better eye of blind school students
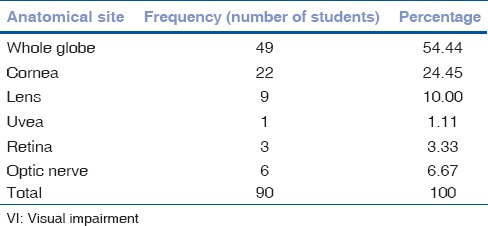
Figure 3.
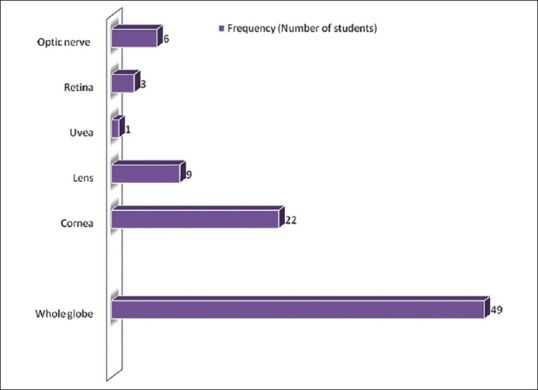
Anatomical classification of the causes of visual impairment in the better eye of blind school students
The main causes of SVI and BL in the better eye of blind school students were microphthalmos (34.44%), anophthalmos (14.45%), buphthalmos/glaucoma (3.33%), cryptophthalmos (2.22%), staphyloma (2.22%), nutritional corneal scar (22.23%), cataract (2.22%), aphakia (1.11%), pseudophakia (6.67%), coloboma (1.11%), retinal dystrophy (2.22%), retinal detachment (1.11%), optic nerve atrophy (6.67%) etc [Table 4].
Table 4.
The main causes of SVI and BL in the better eye of blind school students
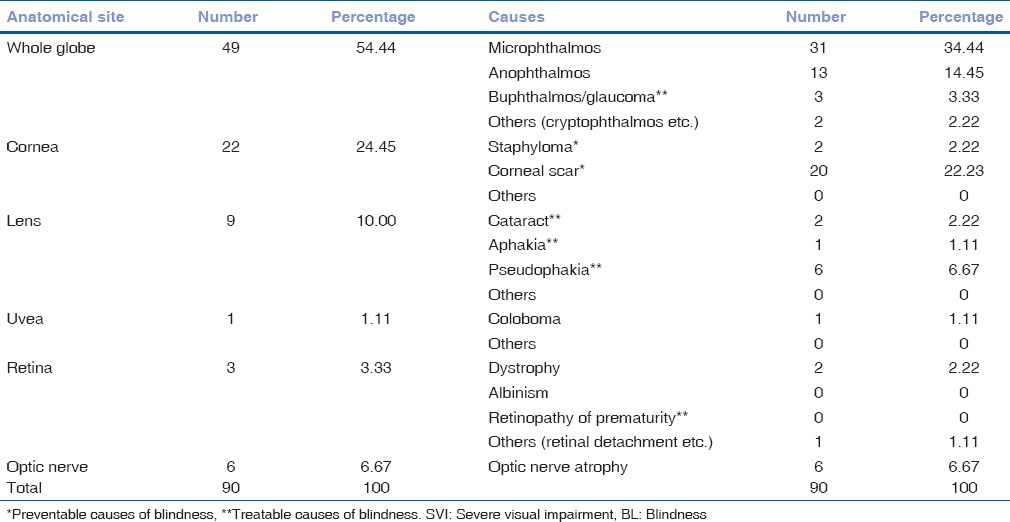
Of these, 22 (24.44%) students had preventable causes of BL (corneal scarring and staphyloma). Another 12 (13.33%) students had treatable causes of BL (buphthalmos, cataract, aphakia, and pseudophakia) [Table 4].
Discussion
At least half and possibly up to three-quarters of causes of childhood BL are avoidable. It is estimated that in developing countries, only 10% of the blind children attend blind schools.[12] Ignorance of parents and geographical inaccessibility to the schools are major factors among those residing in remote and poor areas. A culture of mistrust and scepticism exists in some tribal and village communities regarding such centers, which further hinders access. Most blind schools do not admit children below 5 years of age and hence, preschool children are excluded from these studies.[13]
There are some biases inherent in any study of children in schools for the blind; causes of BL in children with multiple disabilities, those who have died, those from lower socioeconomic groups, and those from rural communities are likely to be under-represented in schools for the blind compared with population-based studies.[4] In the present study, only 3.3% of children had an additional disability, which is very low compared to western surveys, as children with multiple disabilities are often refused entry and have difficult access to blind schools in India.
In the present study, congenital ocular anomalies (mainly microphthalmos, anophthalmos, coloboma etc.) accounted for 52.2% of SVI/BL. This has been a common finding in studies on blind children in India, including population-based studies on children in community-based rehabilitation.[14,15,16,17] but the reasons are not known as most causes of BL are sporadic.[18] These results are comparable to Maharashtra in West India (46.3%).[11] The reason for the high proportion of anomalies in our study is not clear and deservers special attention.
Corneal BL was the second most common cause of SVI/BL, and the major preventable cause identified. Although it is difficult to specifically ascertain the etiology of corneal scarring several years after the original pathology, Vitamin A deficiency appears to be the major cause as in the majority of children with corneal scarring, diarrhea, or measles (which can precipitate acute Vitamin A deficiency) preceded the onset of visual loss. Retinal causes, primarily retinal dystrophies, accounted for 3.3% of the cases, and disorders of the lens accounted for 10.0%.
The presence of a large proportion of children with visual loss of undetermined etiology is consistent with results from other studies and reflects the limited scope for investigation, and lack of examination of family members in many cases.
Overall, 37.7% of children were blind from potentially preventable or treatable conditions. Preventable causes included Vitamin A deficiency, measles, trauma, autosomal dominant conditions, and TORCH infection. These findings suggest the importance of public health strategies, primary prevention for example, high measles immunization coverage, promotion of breastfeeding, health and nutrition education, and continued programs for the control of Vitamin A deficiency through child survival programs. Reduction in BL due to genetic diseases will prove more challenging as there are few medical geneticists in India, and advice given with pediatrician collaboration will need to be sensitive to the complex social, economic, and cultural factors influencing marriage and child rearing, and the possible consequences of attributing “blame.”
Treatable causes included cataract, glaucoma, and refractive errors. There is a need to expand specialist pediatric ophthalmic services in India, and it has been recommended that there should be one well-equipped child eye care center for every 10 million total population.[19] In India, this would translate to 100 centers throughout the country. There is a need to train pediatrician in screening for early detection of cataract and glaucoma with appropriate referral to a tertiary care center.
Comparison of causes of SVI/BL in different age groups needs to be interpreted cautiously, as the data are not population-based and only a small proportion of blind children are in special education. Another factor to consider is the age at which children become blind from different disorders varies that is, keratomalacia usually occurs during preschool years, whereas BL from retinal dystrophies may not occur until later in childhood. Having said this, the data do seem to suggest that corneal BL is a less important cause in younger children than in older children. If true, this may reflect a decline in the incidence of corneal scarring in response to rapid improvements in socioeconomic development experienced by many communities in India, particularly with respect to better water supplies and sanitation, improved measles immunization coverage, and highly effective programs for child spacing with many states reaching the replacement level of fertility.
Some limitations were encountered in this study including poor history by some students and parents/guardians of the precise period of onset, cause, and process of BL; this made correlation of findings and determining the exact diagnosis difficult. Furthermore, further evaluation was hampered by the unavailability of electrophysiological devices and a portable ocular ultrasound device.
Conclusion
In this study, it was found that hereditary diseases, corneal scar, and cataract were the prominent causes of BL in childhood. Most cases of corneal scars are most likely attributed to infections and nutritional deficiencies in infancy and are preventable conditions. Almost 38% of the students in schools for the blind had preventable or treatable causes, indicating the need of specific public health strategies.
More studies and visual assessment need to be carried out on students in blind schools to determine which students can benefit from a distance and near visual aids. By decreasing the rate of consanguineous marriage and performing a regular genetic consultation before marriage, we can prevent the genetic/hereditary eye diseases.
As this study provides information on the causes in a selected population, the findings as to absolute numbers have to be interpreted with caution. Population-based studies are, therefore, necessary in order to obtain more appropriate epidemiological information on childhood BL and provide relevant information for national or regional BL prevention policy-making.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Gilbert CE, Anderton L, Dandona L, Foster A. Prevalence of visual impairment in children: A review of available data. Ophthalmic Epidemiol. 1999;6:73–82. doi: 10.1076/opep.6.1.73.1571. [DOI] [PubMed] [Google Scholar]
- 2.Danish Assistance to the National Program for control of Blindness. New Delhi: India; 1996. Vision screening in school children. Training module 1. [Google Scholar]
- 3.Rahi JS, Gilbert CE, Foster A, Minassian D. Measuring the burden of childhood blindness. Br J Ophthalmol. 1999;83:387–8. doi: 10.1136/bjo.83.4.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhattacharjee H, Das K, Borah RR, Guha K, Gogate P, Purukayastha S, et al. Causes of childhood blindness in the northeastern states of India. Indian J Ophthalmol. 2008;56:495–9. [PMC free article] [PubMed] [Google Scholar]
- 5.Gilbert C, Rahi J, Quinn G. Visual impairment and blindness in children. In: Johnson G, Minassian D, Weale W, West S, editors. Epidemiology of Eye Disease. 2nd ed. UK: Arnold Publishers; 2003. [Google Scholar]
- 6.World Health Organization. WHO/PBL/97.61. Geneva: WHO; 1997. Global Initiative for the Elimination of Avoidable Blindness. [Google Scholar]
- 7.Rao GN. VISION 2020: The right to sight. Indian J Ophthalmol. 2000;48:3. [PubMed] [Google Scholar]
- 8.Dandona L, Gilbert CE, Rahi JS, Rao GN. Planning to reduce childhood blindness in India. Indian J Ophthalmol. 1998;46:117–22. [PubMed] [Google Scholar]
- 9.Gilbert C, Foster A, Négrel AD, Thylefors B. Childhood blindness: A new form for recording causes of visual loss in children. Bull World Health Organ. 1993;71:485–9. [PMC free article] [PubMed] [Google Scholar]
- 10.Rahi JS, Sripathi S, Gilbert CE, Foster A. Childhood blindness due to vitamin A deficiency in India: Regional variations. Arch Dis Child. 1995;72:330–3. doi: 10.1136/adc.72.4.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gogate P, Deshpande M, Sudrik S, Taras S, Kishore H, Gilbert C. Changing pattern of childhood blindness in Maharashtra, India. Br J Ophthalmol. 2007;91:8–12. doi: 10.1136/bjo.2006.094433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gilbert C, Foster A. Childhood blindness in the context of VISION 2020 - The right to sight. Bull World Health Organ. 2001;79:227–32. [PMC free article] [PubMed] [Google Scholar]
- 13.Madgula I. Childhood blindness in India - Regional variations. J Clin Diagn Res. 2009 Feb;:1255–60. [Google Scholar]
- 14.Titiyal JS, Pal N, Murthy GV, Gupta SK, Tandon R, Vajpayee RB, et al. Causes and temporal trends of blindness and severe visual impairment in children in schools for the blind in North India. Br J Ophthalmol. 2003;87:941–5. doi: 10.1136/bjo.87.8.941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hornby SJ, Adolph S, Gothwal VK, Gilbert CE, Dandona L, Foster A. Evaluation of children in six blind schools of Andhra Pradesh. Indian J Ophthalmol. 2000;48:195–200. [PubMed] [Google Scholar]
- 16.Sil AK, Gilbert C. Childhood blindness in India. J Indian Med Assoc. 2001;99:557–60. [PubMed] [Google Scholar]
- 17.Rahi JS, Sripathi S, Gilbert CE, Foster A. Childhood blindness in India: Causes in 1318 blind school students in nine states. Eye (Lond) 1995;9(Pt 5):545–50. doi: 10.1038/eye.1995.137. [DOI] [PubMed] [Google Scholar]
- 18.Hornby SJ, Gilbert CE, Rahi JK, Sil AK, Xiao Y, Dandona L, et al. Regional variation in blindness in children due to microphthalmos, anophthalmos and coloboma. Ophthalmic Epidemiol. 2000;7:127–38. [PubMed] [Google Scholar]
- 19.World Health Organization. WHO/PBL/00.71. Geneva: WHO; 2000. Preventing Blindness in Children. Report of a WHO/IAPB Scientific Meeting. [Google Scholar]


