Abstract
Neoplasms of the lacrimal drainage system are uncommon, but potentially life-threatening and are often difficult to diagnose. Among primary lacrimal sac tumors, benign mixed tumors are extremely rare. Histologically, benign mixed tumors have been classified as a type of benign epithelial tumor. Here we report a case of benign mixed tumor of the lacrimal sac.
Keywords: Benign mixed tumor, primary lacrimal sac tumor, external dacryocystorhinostomy
Neoplasms of the lacrimal drainage system are uncommon, but potentially life-threatening conditions and are often difficult to diagnose.[1,2] Early diagnosis and treatment are thus particularly important. The most common signs and symptoms associated with lacrimal sac neoplasms include epiphora, recurrent dacryocystitis, and lacrimal sac mass.[3]
Among primary lacrimal sac tumors, benign mixed tumors are histologically classified as a benign epithelial tumor.[4] These tumors are believed to be originated from epithelial cells of ductal origin.[5]
Benign epithelial lacrimal sac tumors are often managed by dacryocystorhinostomy (DCR) and excision of the mass.[2,6] Recurrence after excision occurs in an average of 10–40% of all cases.[2,7] Most recurrences are of the inverted papilloma type and may also show foci of carcinomatous change.[7,8]
Ophthalmologically, the benign mixed tumor is an extremely rare form of a primary lacrimal sac tumor that usually arises from the lacrimal gland. Here, we report a case of benign mixed tumor of the lacrimal sac.
Case Report
A 60-year-old male presented to the ophthalmology clinic with a 5-year history of epiphora and a 1-month history of bloody discharge from the right lower punctum. The patient did not complain of marked medial canthal swelling or tenderness. On examination, best corrected visual acuity was 20/20 bilaterally. There was mucoid discharge with a blood clot found in the right lower punctum [Fig. 1a]. Pressure over the lacrimal sacs produced bloody discharge, suggesting a primary lacrimal sac tumor [Fig. 1b]. Syringing and dacryocystography demonstrated a complete obstruction at the level of the lacrimal sac [Fig. 2]. Endoscopic endonasal examination was normal as were anterior segment and fundoscopic examinations.
Figure 1.
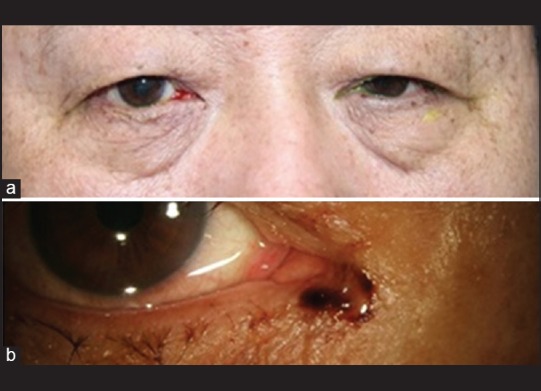
(a) Mucoid discharge with blood clot of the right lower punctum was observed. (b) Pressure over the lacrimal sacs resulted in expression of bloody discharge
Figure 2.

Complete obstruction of lacrimal drainage at the level of lacrimal sac shown on dacryocystography. Dacryocystography revealed a complete obstruction of lacrimal drainage at the level of the common canaliculus
The patient then underwent a computed tomography (CT) scan which demonstrated a solid mass, measuring 1.2 cm × 1.2 cm × 1.6 cm, centered on the enlarged right lacrimal sac fossa [Fig. 3a]. With high clinical suspicion of a tumor, the patient was advised to undergo an open DCR with excisional biopsy of the mass, lacrimal sac and the proximal portion of the nasolacrimal duct.
Figure 3.
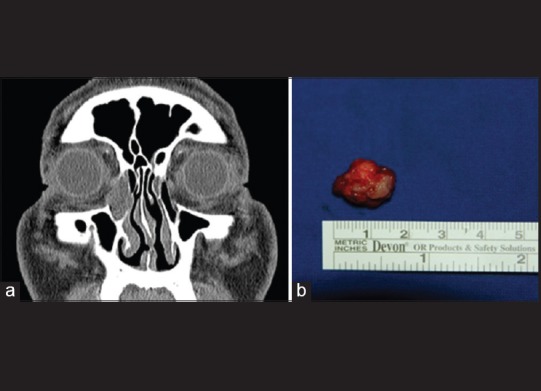
A solid, well-circumscribed, 1.2 cm × 1.2 cm × 1.6 cm mass centered on the enlarged right lacrimal sac fossa. (a) Computed tomography revealed a solid, well-circumscribed mass centered on the enlarged right lacrimal sac fossa. (b) The excised mass was oval-shaped and measured 1.2 cm × 1.2 cm × 1.6 cm
A relatively well-circumscribed 1.2 cm × 1.2 cm × 1.6 cm solid mass [Fig. 3b] was excised and sent for histological examination. The cutting plane was grossly white in color and had a negative resection margin. The specimen was subsequently evaluated for SMA, S-100, p63, CK5, CK6, and Alcian blue. The specimen was made up of variable patterns of epithelial and spindle cells in a hyalinized stroma with apocrine differentiation, similar to the histologic features of a pleomorphic adenoma of the lacrimal gland [Fig. 4]. These histologic findings favored the diagnosis of a benign mixed tumor.
Figure 4.
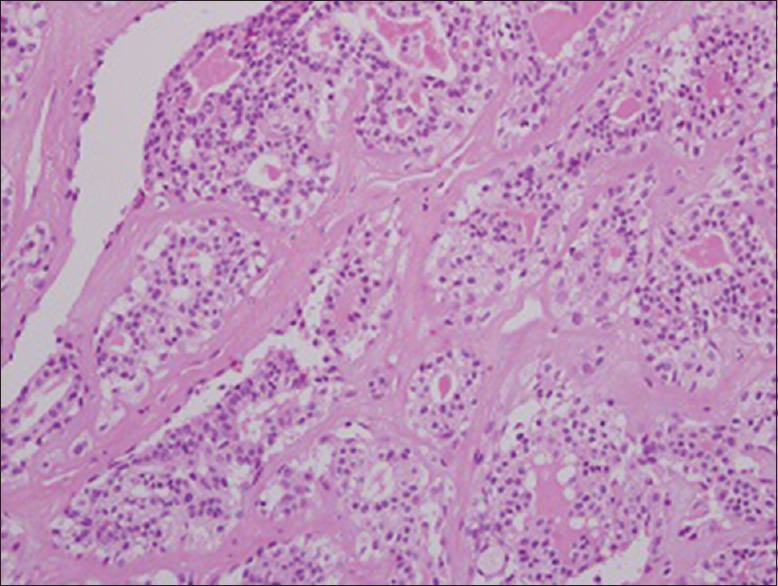
Histology of the tissue showed variable patterns of epithelial cells and spindle cells in a hyalinized stroma with apocrine differentiation (H&E, ×40)
One month after excision of the mass, the patient underwent a repeat CT, and no evidence of recurrence was found. The patient complained of epiphora in the right eye after surgery and underwent canaliculo-rhinostomy with silicone tube intubation.
Discussion
Neoplasms of the lacrimal drainage system are uncommon, but are potentially life-threatening and are often difficult to diagnose.[1,2] Among primary lacrimal sac tumors, the benign mixed tumor, also known as a pleomorphic adenoma, is histologically classified as a benign epithelial tumor.[4]
Pleomorphic adenomas are common benign salivary gland tumors and are the most common tumors of the parotid gland.[8] These tumors are believed to be originated from epithelial cells of ductal origin.[5] Histologically, they are characterized by an admixture of polygonal epithelial elements with ductal or acinar arrangement and spindle-shaped myoepithelial elements in a variable background stroma that may be mucoid, myxoid, cartilaginous or hyaline.[5,8]
Ophthalmologically, benign mixed tumors usually arise from the lacrimal gland, but are an extremely rare form of a primary lacrimal sac tumor. Furthermore, the origin of these glandular structures in the walls of the lacrimal sac and nasolacrimal duct is not completely understood, because the embryology of the human lacrimal system is not clearly defined in the literature.[5]
Benign epithelial lacrimal sac tumors are often managed by external DCR and simple excision of the mass.[1] The most common symptoms indicating dysfunction of the lacrimal drainage system include punctual discharge and epiphora. Bloody discharge and mass above the medial canthal ligament imply tumorous condition of lacrimal sac. In addition to a full ophthalmic examination (ocular surface, eyelid, assessment of the lacrimal drainage system, syringing and probing and digital expression of lacrimal sac contents), imaging studies including dacryocyctography and CT should reserve for selected patients with tumorous condition. In the case of suspicious of lacrimal sac tumor, external DCR is regarded as the gold standard in terms of surgical success.[9,10] The external approach allows an excellent possibility for inspection of the lacrimal sac and for biopsy of abnormal appearing findings.[3]
Our patient had a benign mixed tumor with no evidence of the other tumor foci or systemic spread. The patient underwent open DCR with excisional biopsy of the mass, lacrimal sac, and the proximal portion of the nasolacrimal duct and after 1-month, canaliculo-rhinostomy with silicone tube intubation for the treatment of epiphora. A repeat CT scan showed no evidence of tumor recurrence. Although benign mixed tumors of the lacrimal sac are very uncommon, this case provides a rationale for including this condition in the differential diagnosis of lacrimal sac masses.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Parmar DN, Rose GE. Management of lacrimal sac tumours. Eye (Lond) 2003;17:599–606. doi: 10.1038/sj.eye.6700516. [DOI] [PubMed] [Google Scholar]
- 2.Ryan SJ, Font RL. Primary epithelial neoplasms of the lacrimal sac. Am J Ophthalmol. 1973;76:73–88. doi: 10.1016/0002-9394(73)90014-7. [DOI] [PubMed] [Google Scholar]
- 3.Stefanyszyn MA, Hidayat AA, Pe’er JJ, Flanagan JC. Lacrimal sac tumors. Ophthal Plast Reconstr Surg. 1994;10:169–84. doi: 10.1097/00002341-199409000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Heindl LM, Jünemann AG, Kruse FE, Holbach LM. Tumors of the lacrimal drainage system. Orbit. 2010;29:298–306. doi: 10.3109/01676830.2010.492887. [DOI] [PubMed] [Google Scholar]
- 5.Pe’er J, Hidayat AA, Ilsar M, Landau L, Stefanyszyn MA. Glandular tumors of the lacrimal sac. Their histopathologic patterns and possible origins. Ophthalmology. 1996;103:1601–5. doi: 10.1016/s0161-6420(96)30457-0. [DOI] [PubMed] [Google Scholar]
- 6.Font RL. Eyelids and lacrimal drainage system. In: Spencer WH, editor. Ophthalmic Pathology. Vol. 4. Philadelphia: Saunders; 1996. pp. 2412–27. [Google Scholar]
- 7.Duke-Elder S. System of Ophthalmology. 5th ed. St. Louis: CV Mosby; 1952. Tumors of the lacrimal passages; pp. 5346–58. [Google Scholar]
- 8.Baron S, Koka V, El Chater P, Cucherousset J, Paoli C. Pleomorphic adenoma of the nasal septum. Eur Ann Otorhinolaryngol Head Neck Dis. 2014;131:139–41. doi: 10.1016/j.anorl.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 9.Boboridis KG, Bunce C, Rose GE. Outcome of external dacryocystorhinostomy combined with membranectomy of a distal canalicular obstruction. Am J Ophthalmol. 2005;139:1051–5. doi: 10.1016/j.ajo.2005.01.009. [DOI] [PubMed] [Google Scholar]
- 10.Emmerich KH, Busse H, Meyer-Rüsenberg HW. Dacryocystorhinostomia externa. Technique, indications and results. Ophthalmologe. 1994;91:395–8. [PubMed] [Google Scholar]


