Abstract
Neonatal septicemia is an important cause of morbidity and mortality. The present study was undertaken to determine the bacteriological profile and antimicrobial susceptibility pattern of prevalent pathogens isolated from the blood of septicemic neonates from Neonatal Intensive Care Unit (NICU). A total of 180 blood samples of septicemic neonates were studied bacteriologically. Antimicrobial susceptibility testing was done by the Kirby Bauer disc diffusion method in accordance to Clinical Laboratory Standards Institutes (CLSI) guidelines. 26.6% (48 out of 180) cases of septicemia could be confirmed by blood culture. Of these, 66.7% cases were of early onset septicemia (EOS) and 33.3% were of late onset septicemia (LOS). Klebsiella pneumoniae was the predominant pathogen (35.4%) among the Gram-negative pathogens and Staphylococcus aureus (22.9%) was the predominant Gram-positive pathogen. 28% of K. pneumoniae and E. coli isolates were extended spectrum beta-lactamase (ESBL) producers. 18.1% of the Staphylococcus isolates were methicillin-resistant S. aureus (MRSA). Multi-drug-resistance pattern was observed with all the isolates. Ciprofloxacin and aminoglycosides were the most effective drugs against Gram-positive and Gram-negative isolates. This study highlights the predominance of Gram-negative organisms in causing neonatal sepsis and emergence of multi-drug-resistant strains in our set up.
Keywords: Antibiotic policy, Multidrug resistance, Neonatal septicemia
INTRODUCTION
Septicemia is the significant cause of morbidity and mortality in the neonates and is responsible for 30-50% of total neonatal deaths each year in developing countries. It is estimated that up to 20% of neonates develop sepsis and approximately 1% die of sepsis related causes.[1] In India, according to National Perinatal Database (NNPD) 2002-03, the incidence of neonatal septicemia has been reported to be 30/1000 live births.[2] Early diagnosis and appropriate therapy of septicemia is of utmost importance to prevent morbidity and mortality.[3] The present study was undertaken to determine the bacteriological profile and their antimicrobial susceptibility pattern of prevalent pathogens isolated from the blood of septicemic neonates from Neonatal Intensive Care Unit (NICU).
DESCRIPTION
The study was carried out in the department of Microbiology. 180 neonates with clinical suspicion of septicemia admitted to NICU were studied bacteriologically. Blood samples of these neonates were collected with strict aseptic precautions.
1-2 ml venous blood was inoculated into blood culture bottle containing 10-20 ml of sterile tryptose phosphate broth. The samples were processed by standard bacteriological procedure.[4]
Antimicrobial susceptibility testing was performed by Kirby-Bauer disc diffusion susceptibility method in accordance to Clinical Laboratory Standards Institutes (CLSI) guidelines.[5]
Out of 180 blood samples, septicemia could be confirmed by culture in 26.6% (48 out of 180) cases. There has been a wide variation in the growth positivity obtained by blood culture over the years. A higher isolation rate of 52.6% was reported by Murty et al.[6] in 2007. A recent study by Rajendraprasad et al.[7] reported 47.5% isolation rate.
Out of 48 cases, 32 cases (66.7%) were of early onset septicemia (EOS — septicemia within 72 h of life) and 16 cases (33.3%) were of late onset septicemia (LOS — septicemia after 72 h of life). This clustering of 66.7% cases in first 3 days of life reflects the immaturity of immunological responses in the first few days of life. The EOS occurs due to ascending infection from infected birth canal or following rupture of membrane usually caused by Gram-negative organisms acquired after birth from human contact.[8] Movahedian et al.[9] have reported 81.5% cases of early onset neonatal septicemia.
In the present study, Gram-negative organisms predominated being responsible for 70.8% of cases of septicemia [Table 1]. A recent study conducted in Karnataka reported 70.5% neonatal septicemia cases caused by Gram-negative isolates.[7]
Table 1.
Bacteriological profile of EOS and LOS cases and antimicrobial resistance pattern for Gram-negative and Gram-positive isolates
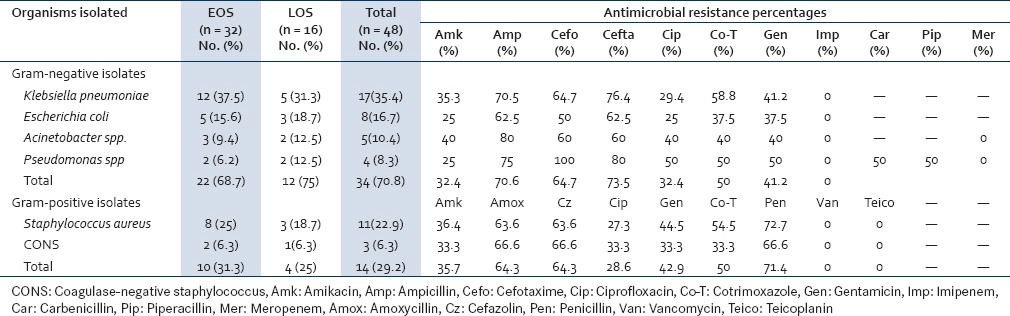
Klebsiella pneumoniae was found to be the predominant pathogen followed by Staphylococcus aureus accounting for 35.4% and 22.9% cases respectively. K. pneumoniae was reported as a predominant pathogen in NNPD Report 2002-2003[2] and by Mane et al.[10] Roy et al.[11] and Mustafa et al.[12] from India and by Iregbu et al.[13] from Nigeria.
Other Gram-negative organisms isolated were Escherichia coli, Acinetobacter spp. and Pseudomonas spp. Acinetobacter spp. causing septicemia in neonates were reported by Arora et al.[14] and Vinodkumar et al.[15] Acinetobacter poses a major problem in NICU.
S. aureus was isolated from 22.9% cases and was the next common pathogen following K. pneumoniae. S. aureus as a major pathogen of neonatal septicemia has been reported by Karthikeyan et al.[16] These findings have implications for therapy and infection control. K. pneumoniae and S. aureus can survive in the environment for a relatively long time and fairly widely distributed in the hospital environment and therefore have the potential for being transmitted from the environment to the patients through practices that breach infection control measures.[13]
An alarming finding of this study is the high proportion of organisms resistant to commonly used antibiotics [Table 1]. Resistance ranging from 50% to 73% was observed in Gram-negative isolates for co-trimoxazole, cefotaxime, ampicillin and ceftazidime.
Gram-positive isolates had shown the resistance ranging from 42% to 71% against co-trimoxazole, cefazolin, amoxycillin and penicillin.
Predominance of K. pneumoniae as the causative agent of neonatal sepsis may be due to the selective pressure of antimicrobial agents so that resistant organisms tend to colonize and proliferate in the neonates.[8] This is true with septicemia caused by K. pneumoniae and S. aureus. In the present study, K. pneumoniae and S. aureus had exhibited multi-drug-resistance pattern. 18.1% S. aureus isolates were found to be methicillin resistant. 29.4% of the K. pneumoniae isolates and 25% E. coli isolates were ESBL producers. It would therefore appear that the choice of drug for empiric treatment of suspected neonatal septicemia is likely to be difficult in the presence of MRSA and ESBL producers which often fail to achieve therapeutic goals even after showing in vitro susceptibility.
Maximum sensitivity for ciprofloxacin and amikacin was exhibited not only by K. pneumoniae but even by rest of the Gram-negative isolates and Gram-positive isolates. This implicates that these two antibiotics can be included as empirical therapy for neonatal septicemia. This has been corroborated by many other workers.[7,10,12,16,17,18]
Vancomycin remains the drug of choice for MRSA strains in our set up.
Not a single Gram-negative isolate was resistant to imipenem. This indicates the absence of selective pressure since the drug is rarely prescribed.
CONCLUSION
This study concludes that empiric therapy for suspected neonatal septicemia should cover both Gram-negative bacilli and Gram-positive cocci particularly Klebsiella pneumoniae and Staphylococcus aureus. Ciprofloxacin and Amikacin, these two antibiotics can be included as empirical therapy for neonatal septicemia. An effective infection-control programme, regular antibiotic susceptibility surveillance and evaluation, and the enforcement and periodic review of the antibiotic policy of the hospital as well as the encouragement of rational antibiotic use will reduce the rates of acquiring nosocomial infections and development of bacterial resistance.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Tripathi S, Malik GK. Neonatal sepsis: Past, present and future; a review article. Internet J Med Update. 2010;5:45–54. [Google Scholar]
- 2.Report of the National Neonatal Perinatal Database. Report 2002-2003. NNPD Network. [Last accessed on 2010 July 17]. Available from: http://www.newbornwhocc.org/pdf/nnpd_report_2002-03.PDF .
- 3.Levy I, Leibovici L, Ducker M, Samra Z, Konisberger H, Ashkenazi S. A prospective study of Gram-negative bacteraemia in children. Pediatr Infect Dis J. 1996;15:117–22. doi: 10.1097/00006454-199602000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Koneman EW, Allen SD, Janda WM, Schreckenberger PC, Winn WC., Jr . 6th ed. Philadelphia: Lippincott Williams & Wilkins; 2006. Koneman's Color Atlas and Textbook of Diagnostic Microbiology. [Google Scholar]
- 5.Pennsylvania, USA: Clinical Laboratory and Standards Institutes; 2011. Performance Standards for Antimicrobial Susceptibility Testing; Twenty first informational supplement. M100-S21. [Google Scholar]
- 6.Murty DS, Gyaneshwari M. Blood cultures in pediatric patients: A study of clinical impact. Indian J Med Microbiol. 2007;25:220–4. doi: 10.4103/0255-0857.34762. [DOI] [PubMed] [Google Scholar]
- 7.Rajendraprasad BP, Basavaraj KN, Antony B. Bacterial spectrum of neonatal septicemia with their antibiogram with reference to various predisposing factors in a tertiary care hospital in Southern India. Ann Trop Med Public Health. 2013;6:96–9. [Google Scholar]
- 8.Klein JO, Marchy SM. Bacterial sepsis and meningitis. In: Remington JS, Klein JO, editors. Infectious Diseases of the Fetus and Newborn Infants. 4th ed. Philadephia: W.B. Saunders; 1995. pp. 36–90. [Google Scholar]
- 9.Movahedian AH, Moniri R, Mosayebi Z. Bacterial culture of neonatal sepsis. Iranian J Pub Health. 2006;33:84–9. [Google Scholar]
- 10.Mane AK, Nagdeo NV, Thombare VR. Study of neonatal septicemia in a tertiary care hospital in rural Nagpur. Journal of Recent Advances In Applied Sciences J Recent Adv Appl Sci. 2010;25:19–24. [Google Scholar]
- 11.Roy I, Jain A, Kumar M, Agarwal SK. Bacteriology of neonatal septicemia in a tertiary care hospital of northern India. Indian J Med Microbiol. 2002;20:156–9. [PubMed] [Google Scholar]
- 12.Mustafa M, Ahmed SL. Bacteriological profile and antibiotic susceptibility patterns in neonatal septicemia in view of emerging drug resistance. J Med Allied Sci. 2014;4:2–8. [Google Scholar]
- 13.Iregbu KC, Elegba OY, Babaniyi IB. Bacteriological profile of neonatal septicemia in a tertiary hospital in Nigeria. Afr Health Sci. 2006;6:151–4. doi: 10.5555/afhs.2006.6.3.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arora U, Jaitwani J. Acinetobacter spp.- an emerging pathogen in neonatal septicemia in Amritsar. Indian J Med Microbiol. 2006;24:81. doi: 10.4103/0255-0857.19911. [DOI] [PubMed] [Google Scholar]
- 15.Vinodkumar CS, Neelagund YF. Acinetobacter septicemia in neonates. Indian J Med Microbiol. 2004;22:71. [PubMed] [Google Scholar]
- 16.Karthikeyan G, Premkumar K. Neonatal sepsis: Staphylococcus aureus as the predominant Pathogen. Indian J Pediatr. 2001;68:715–7. doi: 10.1007/BF02752407. [DOI] [PubMed] [Google Scholar]
- 17.Joshi SJ, Ghole VS, Niphadkar KB. Neonatal gram negative bacteremia. Indian J Pediatr. 2000;67:27–32. doi: 10.1007/BF02802632. [DOI] [PubMed] [Google Scholar]
- 18.Prabhu K, Bhat S, Rao S. Bacteriological profile and antibiogram of blood culture isolates in a pediatric care unit. J Lab Physicians. 2010;2:85–8. doi: 10.4103/0974-2727.72156. [DOI] [PMC free article] [PubMed] [Google Scholar]


