Abstract
Background
The 3 Ayurvedic constitutional types or Doshas – vata, pitta, and kapha – are responsible for homeostasis and health. The doshas determine various functions, including sleep. According to the Ayurvedic texts, sleep is caused by increased kapha and insomnia by increased vata or pitta, which may follow physical or mental exertion, or disease. The present study was carried out to determine whether this relationship could be found using contemporary standardized questionnaires.
Material/Methods
In this cross-sectional single-group study, 995 persons participated (646 males; group average age ±S.D., 49.1±15.2 years). Participants were attending a 1-week residential yoga program in northern India. Participants were assessed for dosha scores using a Tridosha questionnaire and the quality of sleep in the preceding week was self-rated using a sleep rating questionnaire.
Results
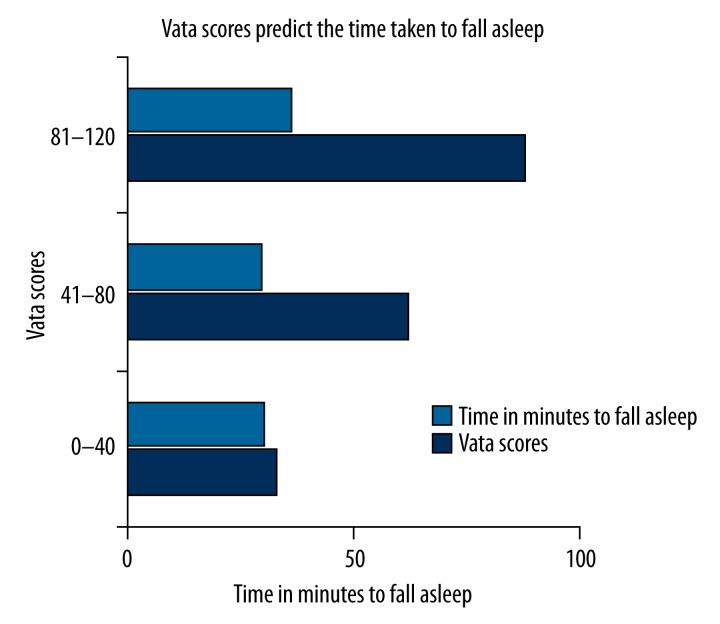
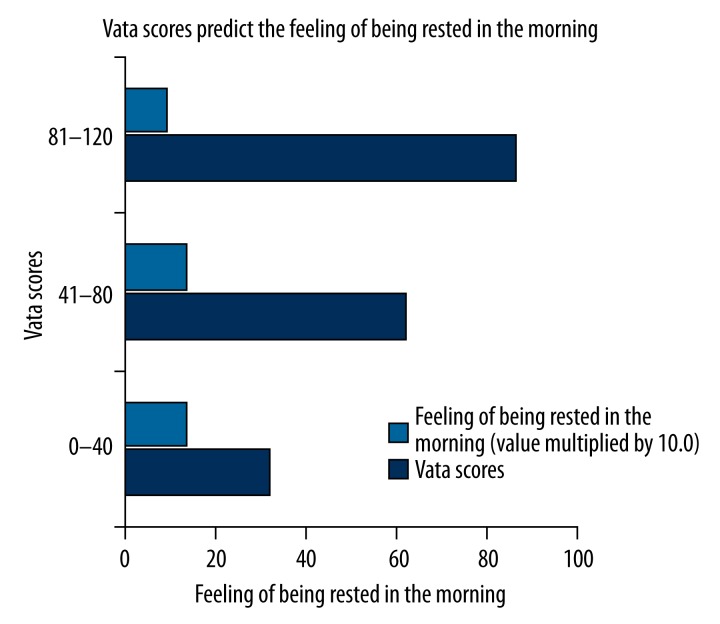
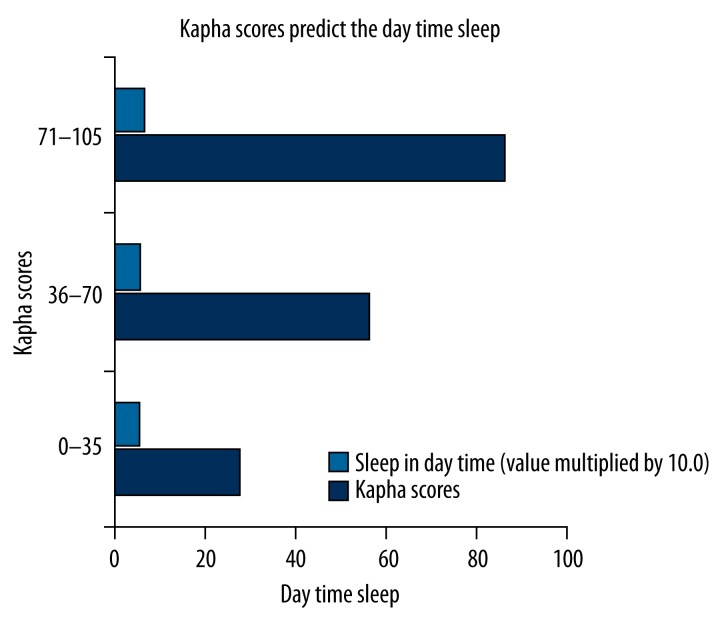
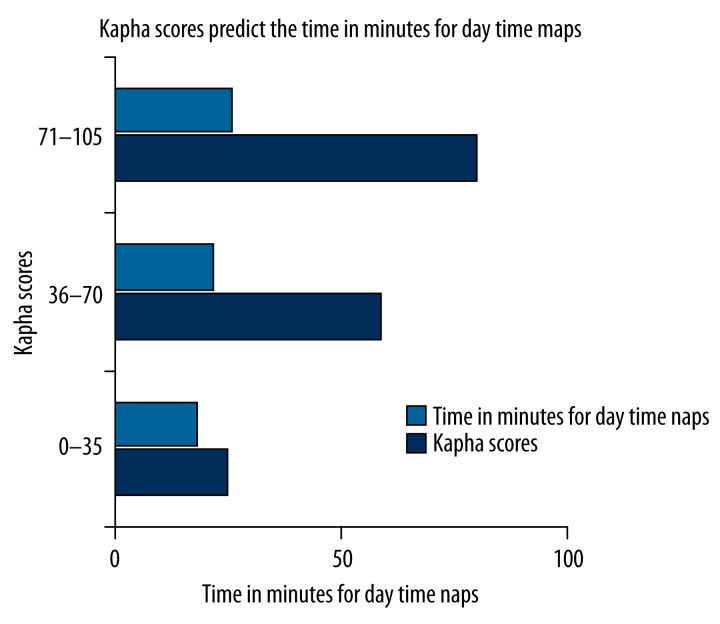
Multiple linear regression analyses were used to determine if each dosha acted as a predictor of quality and quantity of sleep. Vata scores significantly predicted the time taken to fall asleep [p<0.01], and the feeling of being rested in the morning [p<0.001]; with higher vata scores being associated with a longer time to fall asleep and a lesser feeling of being rested in the morning. Kapha scores significantly predicted day-time somnolence [p<0.05] and the duration of day-time naps in minutes [p<0.05], with higher kapha scores being associated with longer day-time naps.
Conclusions
The results suggest that the doshas can influence the quality and quantity of sleep.
Keywords: Linear Models; Medicine, Ayurvedic; Sleep
Background
The ancient Indian science of Ayurveda describes guidelines for healthy living [1]. Ayurveda defines 3 dynamic pathophysiological constitutional types (doshas) as the basis for all body functions [2]. Tridosha is comprised of 2 words; tri and dosha. Here ‘tri’ means “a group of 3 basic elements (Vata, Pitta, and Kapha) and ‘dosha’ means “that which is capable of vitiation”. When vata, pitta, and kapha are vitiated they produce disease and when they are in equilibrium, they maintain perfect balance and harmony in the body [1].
At the cellular level, vata dosha may be associated with signaling pathways that regulate cell growth, differentiation, and cell death. The vata dosha also governs movements of cells, molecules, nutrients, and wastes [3,4]. The pitta dosha is responsible for processes bringing about change, such as digestion, metabolism, energy production, and maintenance of immunity [5–7]. At the cellular level, the pitta dosha may be associated with the activity of enzymes, growth factors, hormones, and the reactions required for homeostasis and the maintenance of basal metabolism [3,4]. The kapha dosha controls the nervous and musculoskeletal systems [5–7]. The kapha dosha acts to form and maintain body mass, shape, and flexibility [5–7]. At the cellular level, anabolic processes and the coordination of gene and protein function may be associated with the kapha dosha [3,4,8].
In Ayurveda, one’s basic “body constitution” is described as “prakriti”, which arises due to a unique combination of varying amounts of the 3 doshas. Thus, prakriti determines individuality and is akin to one’s genotype. Ayurveda recognizes 7 main types of prakritis, based on the different combinations of the 3 doshas. One’s doshas are in dynamic equilibrium, and the optimal function of each dosha and normal interactions between doshas are essential for good health. Accordingly, individuals with “balanced” doshas are less susceptible to disease than individuals with abnormal doshas. In fact, imbalances or disturbed interactions between doshas are considered a major cause of disease. An abnormal dosha can be inhibited, excessive, or vitiated [9]. The type and nature of disease are primarily determined by which dosha is affected.
In Ayurveda sleep is considered a basic instinct of life, which is essential for all living beings [10]. There are descriptions of sleep and its disorders in ancient Ayurveda texts, such as Sushruta Samhita, circa 100 B.C.–900 A.D. [11], Charaka Samhita, circa 300–500 A.D. [12], and Vagbhatta, circa 700 A.D. [13]. In Ayurveda a unique feature is that the dosha of each individual is determined based on the psychosomatic attributes of an individual’s personality [14]. The doshas determine various basic functions, including sleep.
Traditionally keeping the balance between these 3 constitutional types is considered to be essential for health (Charaka Samhita Sutrasthana, Chapter 20, Verse 9) [5]. Disturbance in the balance between the doshas results in changes in various functions, including sleep, and can lead to sleep disorders. In a specific study, dominance of the vata dosha was reported to be associated with increased arousals at night, and daytime naps in persons over the age of 60 years who fulfilled the criteria for senile dementia based on Ayurveda and conventional medicine [15]. This description is considered to apply to people of all ages whose vata dosha is dominant (Charaka Samhita Sutrasthana, Chapter 20, Verse 12) [5]. Such persons are described as having poor-quality sleep and they often complain of insomnia [16]. In contrast, the pitta dosha is associated with heat (Charaka Samhita Sutrasthana, Chapter 20, Verse 15) [5]. Persons with the pitta dosha dominant have moderate sleep often disturbed by dreams [16]. Persons with the kapha dosha dominant also differ and have been described as being able to fall asleep easily and finding it difficult to keep awake [16]. This dosha is associated with heaviness, moisture, and lubrication (Charaka Samhita Sutrasthana, Chapter 20, Verse 18) [5].
Finally, those with a calm and lethargic temperament are more likely to have no difficulty in falling asleep or maintaining sleep [17]. These individuals can be considered to be kapha dosha-dominant, as calmness and lethargy are associated with the kapha dosha, which is also associated with daytime somnolence (Charaka Samhita Vimanasthanam, Chapter 8, Verse 96) [5].
Despite descriptions of variations of the quality and quantity of sleep with the Ayurvedic doshas, there has been no attempt to study the quality and quantity of sleep in relation to Ayurvedic doshas or constitutional type using contemporary research methods. Hence, the present study was carried out to determine whether the Ayurvedic doshas can predict the quality and quantity of sleep.
Material and Methods
Participants
A total of 995 persons participated in the study, of whom 646 were males; 71.8% of them were 20–60 years of age, and the age range was 12–86 years. The group average age ±SD was 49.1±15.2 years. Statistical calculation of the sample size was not done prior to the experiment. However, post hoc analyses were carried out for the present study. With the sample size as 995; the power was calculated using a post hoc statistical power calculator for multiple regression [18], separately for the sleep rating questionnaire. This is provided for Question 1 (a) Number of predictors=3; (b) Observed R2=.009; (c) Probability level=0.05 [19]; (d) Sample size=995; (e) Observed statistical power=0.718. Participants were attending a 1-week, residential program on yoga for the promotion of health. The program was held in a yoga center in northern India. To be included in the trial, participants had to meet the following criteria: (i) a history of a chronic illness, which was under control based on recent reports; (ii) all participants over 20 years of age had to have at least 10 years of education. Participants were excluded from the trial if they submitted incomplete or incorrectly filled in questionnaires. No participants had to be excluded for this reason. Participants were told that the questionnaires given to them were for a research study, but the purpose of the study was not explained to them. All participants provided signed consent to participate in the study. The project had the approval of the institution’s ethics committee. The baseline characteristics of the participants are given in Table 1.
Table 1.
Baseline characteristics of the 995 participants.
| Characteristics | Details |
|---|---|
| (i) Age, gender | |
| Group mean age ±S.D. (years) | 49.1 ± 15.2 |
| Age range | 12–86 |
| Gender M: F as actual values, % | 646: 349, 64.9: 35.1 |
| (ii) Years of education | |
| 10 years of education (%) | 239 (24.02) |
| 12 years of education (%) | 109 (10.95) |
| 15 years of education (%) | 349 (35.08) |
| ≥17 years of education (%) | 259 (26.03) |
| No details (%) | 39 (3.92) |
| (iii) Diseases (Blocks [36], number)% | |
| Certain infectious and parasitic diseases | A00–B99, 2, (.20) |
| Neoplasms | C00–D48, 14, (1.41) |
| Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism | D50–D89, 8, (.80) |
| Endocrine, nutritional and metabolic diseases | E00–E90, 252, (25.33) |
| Diseases of the nervous system | G00–G99, 25, (2.51) |
| Diseases of the eye and adnexa | H00–H59, 7, (.70) |
| Diseases of the ear and mastoid process | H60–H95, 2, (.20) |
| Diseases of the circulatory system | I00–I99, 104, (10.45) |
| Diseases of the respiratory system | J00–J99, 66, (6.63) |
| Diseases of the digestive system | K00–K93, 65, (6.53) |
| Diseases of the skin and subcutaneous tissue | L00–L99, 29, (2.91) |
| Diseases of the musculoskeletal system and connective tissue | M00–M99, 169, (16.98) |
| Diseases of the genitourinary system | N00–N99, 26, (2.61) |
| Chronic pain | 226, (22.71) |
Values are Group Mean (S.D.); M – male; F – female (S.D.).
Design of the study
The study used a single-group, cross-sectional design. Participants were assessed once, in the middle of the yoga program. The participants completed 2 questionnaires – the Tridosha questionnaire [20] and the sleep rating questionnaire [21]. The questionnaires were administered to participants as a group. These 2 questionnaires were distributed among participants sequentially, such that in 50% of participants the Tridosha questionnaire was administered first and the sleep-rating questionnaire was administered second, then this order was reversed for the other 50% of participants. All participants were told not to begin filling in the questionnaires until instructions were complete. Questions were read aloud. If participants had any queries, these were responded to by trained volunteers. The administration of questionnaires and blind scoring were done by a person who was unaware of the details of the participants and the experiment. After completion of the first questionnaire, participants were asked to put their pens down and the questionnaires were collected. The second questionnaire was then administered and after completion the questionnaires were collected. As mentioned above, both questionnaires were scored blindly.
Assessments
There were 2 questionnaires. The administration and scoring were done by a person who was unaware of any other details of the participants.
Tridosha questionnaire
As already described, dosha is a Sanskrit word to describe the psychosomatic attributes of a person. The questionnaire has 60 questions or statements, which can be considered as 3 sections, each corresponding to the different doshas (vata / pitta / kapha). The questionnaire is an abbreviated version of the Mysore Tridosha Questionnaire [20], which has 157 questions. This version was selected because it was shorter and hence easier to administer to the large sample studied (n=995). The validity and reliability of the scale has been established [22]. Each of the 3 sections has 20 questions or statements. There are 3 possible responses: (i) does not apply, scored as ‘0’, (ii) applies sometimes, scored as ‘3’, and (iii) applies the most/best, scored as ‘6’. Hence, scores for each section were between 0 and 120. A higher score indicates the greater prevalence of a particular dosha in an individual’s constitution. Different aspects of reliability and of validity of the questionnaire were determined for use in an adult Indian population [20, 22]. The questionnaire includes questions related to sleep. There are 5 statements: (i) I often have difficulty in falling asleep or having a sound night’s sleep; (ii) I tend to be irregular in my eating and sleeping habits; (iii) I must get at least 8 hours of sleep in order to be comfortable; (iv) I sleep very deeply; and (v) I have a tendency towards oversleeping, grogginess upon awakening, and am generally slow to get going in the morning. Although these statements were intended to assess the quality and quantity of sleep, none of them were the same as the questions in the sleep rating questionnaire. To selectively remove these questions would give an incomplete idea about the participant’s dosha, so they were retained in the questionnaire.
Sleep-rating questionnaire
The questionnaire has 7 questions (Q) that require the participant to rate their sleep during the preceding week. Questions 1, 2, 3, 4, and 7 are open-ended. Questions 5 and 6 are close-ended and dichotomous, requiring responses such as ‘yes’ or ‘no’. The 7 questions were: (Q1) Approximately how long (in minutes) does it take you to fall asleep? (Q2) How many hours do you sleep each night? (Q3) How many times (if any) do you wake up during the night? (Q4) What are the usual reasons for waking up if you do so? (Q5) Do you feel rested in the morning? (‘yes’ or ‘no’) (Q6) Do you sleep in the daytime? (‘yes’ or ‘no’) and (Q7) If your answer to question 6 was ‘yes’, for how long do your daytime naps last? (in minutes). The reliability and validity of this questionnaire has been determined for use in an Indian population [21].
Results
Linear multiple regression analysis using PASW (SPSS Version 18.0) was performed with scores of the sleep-rating questionnaire as the dependent variables and with the vata, pitta, and kapha scores of the Tridosha questionnaire as independent variables. Regression analyses showed that vata scores predicted the time taken to fall asleep and the feeling of being rested in the morning, whereas kapha scores predicted daytime somnolence and long daytime naps (average time around 25 minutes). The resulting model had an adjusted R2 of.009 (standard error of the estimate=27.753), df (3, 991), F=3.945 for vata scores as a predictor for the time taken to fall asleep at p<0.01 with 95% C.I. of [.305,.065]. Vata scores as a predictor for the feeling of being rested in the morning had adjusted R2 of.020 (standard error of the estimate=.416), df (3, 991), F=7.929 and this was significant at p<0.001 with 95% C.I. of [−.002, −.005]. Kapha scores as a predictor for daytime somnolence had adjusted R2 of.005 (standard error of the estimate=.499), df (3, 991), F=2.592, and this was significant at p<0.05 with 95% C.I. of [.004,.000],and long daytime naps, adjusted R2 of.003 (standard error of the estimate=33.931), df (3, 991), F=2.056 and this was significant at p<0.05 with 95% C.I. of [.312,.032].
Group mean values ±S.D. for scores of Questions 1, 2, 3, 5, 6, and 7 of the sleep-rating questionnaire are given in Table 2 and details of the multiple linear regression analysis are given in Table 3.
Table 2.
Group mean values ±S.D. for scores of questions 1, 2, 3, 5, 6 and 7 of the sleep rating questionnaire.
| Questions | ||||||
|---|---|---|---|---|---|---|
| Q1 (minutes) | Q2 (hours) | Q3 (number) | Q5 | Q6 | Q7 (minutes) | |
| Mean ±S.D. | 31.12±27.88 | 6.81±1.36 | 1.85±1.49 | .77±.42 | .49±.50 | 24.08±33.99 |
Q1 – time in minutes to fall asleep; Q2 – hours of sleep each night; Q3 – number of awakenings during the night; Q5 – feeling being rested in the morning (Yes=1/No=0); Q6 – sleep in day time (Yes=1/No=0); Q7 – time in minutes for day time naps.
Table 3.
Ayurvedic doshas and response to the sleep rating questionnaire.
| Ayurvedic doshas | Measures | Q1 (minutes) | Q2 (hours) | Q3 (number) | Q5 | Q6 | Q7 (minutes) |
|---|---|---|---|---|---|---|---|
| Vata | F | 3.945** | 1.777 | 3.173 | 7.929*** | 2.592 | 2.056 |
| df | 3,991 | 3,991 | 3,991 | 3,991 | 3,991 | 3,991 | |
| Adjusted R2 | .009 | .002 | .007 | .020 | .005 | .003 | |
| β | .108 | −.064 | .067 | −.134 | −.047 | −.023 | |
| Tolerance values | .777 | .777 | .777 | .777 | .777 | .777 | |
| Pitta | F | 3.945 | 1.777 | 3.173 | 7.929 | 2.592 | 2.056 |
| df | 3,991 | 3,991 | 3,991 | 3,991 | 3,991 | 3,991 | |
| Adjusted R2 | .009 | .002 | .007 | .020 | .005 | .003 | |
| β | .002 | −.016 | .038 | −.023 | −.037 | −.017 | |
| Tolerance values | .748 | .748 | .748 | .748 | .748 | .748 | |
| Kapha | F | 3.945 | 1.777 | 3.173 | 7.929 | 2.592* | 2.056* |
| df | 3,991 | 3,991 | 3,991 | 3,991 | 3,991 | 3,991 | |
| Adjusted R2 | .009 | .002 | .007 | .020 | .005 | .003 | |
| β | −.007 | .025 | .020 | −.026 | .068 | .078 | |
| Tolerance values | .942 | .942 | .942 | .942 | .942 | .942 |
p<0.01 (vata scores versus Q1 scores),
p<0.001 (vata scores versus Q5 scores),
p<0.05 (kapha scores versus Q6 scores and Q7 scores), multiple linear regression.
Q1 – time in minutes to fall asleep; Q2 – hours of sleep each night; Q3 – number of awakenings during the night; Q5 – feeling being rested in the morning (Yes =1/No=0); Q6 – sleep in day time (Yes=1/No=0); Q7 – time in minutes for day time naps.
The relationship between (i) vata scores and the time taken to fall asleep is given in Figure 1; (ii) vata scores and the feeling of being rested in the morning is given in Figure 2; (iii) kapha scores and daytime sleep is given in Figure 3; and (iv) kapha scores and the time in minutes for daytime naps is given in Figure 4.
Figure 1.
The relationship between vata scores and the time taken to fall asleep.
Figure 2.
The relationship between vata scores and the feeling of being rested in the morning.
Figure 3.
The relationship between kapha scores and the day time sleep.
Figure 4.
The relationship between kapha scores and the time in minutes for day time naps.
Discussion
We assessed 995 persons participating in a week-long yoga residential camp for general well-being to determine whether their Ayurvedic constitution or dosha could predict their quantity and quality of sleep. A regression analysis showed that higher scores for the vata dosha significantly predicted the time taken to fall asleep (longer with higher scores) and the feeling of being rested in the morning (less when vata scores were high). There was also a positive prediction between kapha scores and the likelihood of daytime naps as well as the duration. The descriptions in ancient Ayurveda texts did mention that vata dosha is associated with less restful sleep, while kapha dosha is associated with daytime somnolence (Charaka Samhita Sutrasthana, Chapter 21, Verse 58) [5].
Sleep onset latency can vary with physical factors such as physical discomfort due to hunger [23], ambient temperature [24], and presence of sensory disturbances such as bright light [25] or loud sounds [26] as well as pathological causes or disease [27]. Among the latter, apart from pain [28], most of the causes are psychological, such as anxiety [29], depression [29], and psychological arousal associated with extreme joy [30], sorrow [31], or anger [12]. Similarly, frequent arousals during the night are also indicators of poor-quality sleep. If physical discomfort is ruled out, frequent arousals usually can be attributed to psychological and emotional causes [32]. With frequent arousals, the chances of persons having sustained periods of deep or slow-wave sleep are reduced [33]. This would appear to be the reason why people who scored high for a vata constitution and had greater number of arousals felt less refreshed in the morning. It was found that 88.34 of participants woke in the night. The 5 most common reasons were: (i) to urinate (49.1%), (ii) pain (7.2%), (iii) dreams (6.7%), (iv) mental tension (6.3%), and (v) external disturbances (2.9%). The psychological mechanisms underlying the amount of time spent in different stages of sleep depends on several physical, emotional, and cognitive factors [34].
The present study examined whether the dosha was a predictor for different aspects of self-rated sleep. However, it is essential to mention that the scores an individual obtained for the 3 doshas were considered separately. In actual fact, an individual’s constitution (prakriti in Sanskrit) could consist of combinations of the different doshas, with 1 dosha being predominant in certain cases. Previous studies have proposed genetic, biochemical, hematological, and physiological differences in persons with different prakritis [35]. To the best of our knowledge, the present study is the first attempt to examine the descriptions related to sleep and the Ayurvedic constitution in the ancient texts using contemporary research methods. The present results are in agreement with descriptions of how the vata and kapha doshas influence sleep (Susruta-Samhita Sarirasthana, Chapter 4, Verse 64) [6]. Since Ayurveda is an ancient science that looks at diverse aspects of a person’s lifestyle [1], sleep is also considered to be influenced by dietary and psychological factors [10]. Accordingly, sleep disorders are corrected by altering these factors and by specific remedies to balance whichever dosha is in a state of imbalance [10].
The main limitations of the study are the following: (i) The results were based on the self-reported quality of sleep of the participants. (ii) The dosha of the individuals was also assessed using questionnaires, thus no objective measure was used. To some extent this is countered by the fact that the sleep-rating questionnaire had quantifiable questions (for example, ‘what is the approximate time taken to fall asleep in the week prior to assessment?’) and the dosha questionnaire also had quantifiable and specific, rather than non-specific or difficult to answer, questions. (iii) The study included adolescents 10–18 years, (1.61%), young adults 19–34 years, (19.10%), middle-aged adults 35–59 years, (48.74%), and adults over 60 years of age (30.55%). No attempt was made to separate participants based on age. This study needs to be supported by whole-night polysomnography studies and month-long sleep diaries.
Conclusions
This survey-based cross-sectional study carried out on 995 persons of both sexes (average age 49.1 years) suggests that higher vata scores are associated with a longer time to fall asleep and a lesser feeling of being rested in the morning. Higher kapha scores, in contrast, are associated with longer daytime naps. These results suggest that the connection between the Ayurveda tridoshas and sleep described in ancient texts are supported by present-day investigations.
Footnotes
Source of support: Departmental sources
References
- 1.Balkrishna A. A practical approach to the science of ayurveda: a comprehensive guide for healthy living. Haridwar, India: Divya Prakashan, Divya Yoga Mandir Trust; 2013. [Google Scholar]
- 2.Sumantran VN, Tillu G. Cancer, inflammation, and insights from ayurveda. Evid Based Complement Alternat Med. 2012;2012:306346. doi: 10.1155/2012/306346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prasher B, Negi S, Aggarwal S. Whole genome expression and biochemical correlates of extreme constitutional types defined in Ayurveda. J Transl Med. 2008;6:48. doi: 10.1186/1479-5876-6-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharma HM. “Contemporary ayurveda,” in Fundamentals of Complementary and Alternative Medicine. 4th Edition. USA: Saunders Elsevier; 2011. pp. 495–508. [Google Scholar]
- 5.Sharma PV. Caraka Samhita. Varanasi: Chaukhambha Orientalia; 2011. Reprint Edition. [Google Scholar]
- 6.Murthy KRS. Susruta Samhita. Varanasi: Chaukhambha Orientalia; 2010. Reprint Edition. [Google Scholar]
- 7.Valiathan MS. The Legacy of Charaka. Orient: Longman; 2003. [Google Scholar]
- 8.Sharma H, Chandola HM. Ayurvedic concept of obesity, metabolic syndrome, and diabetes mellitus. J Altern Complement Med. 2011;17:549–52. doi: 10.1089/acm.2010.0690. [DOI] [PubMed] [Google Scholar]
- 9.Svoboda RE. Ayurveda Life Health and Longevity. Penguin: Books India; 1992. [Google Scholar]
- 10.Toolika E, Narayan PB, Kumar SS. A review on ayurvedic management of primary insomnia. IAMJ. 2013:1. [Google Scholar]
- 11.Trikamji J. Sushrutha Samhita with Ni-bandha Sangraha commentary of Sri Dalhanacharya. 6th ed. Varanasi: Chaukhamba Orientalia; 1997. pp. 358–59. [Google Scholar]
- 12.Acharya YT. Charaka Samhita with Ayurveda Deepika Teekha of Chakrapani Dutta. Varanasi: Choukhambha Sanskrit Sansthan; 2011. Edition Reprint. [Google Scholar]
- 13.Padakara HSS. Ashtanga Hridaya with Sarvanga Sundari Commentry by Aruna-datta and Ayurveda Rasayana of Hemadri. 9th ed. Varanasi: Krishnadas Academy; 2005. pp. 40–143. [Google Scholar]
- 14.Bhushan P, Kalpana J, Arvind C. Classification of human population based on HLA gene polymorphism and the concept of Prakriti in Ayurveda. J Altern Complement Med. 2005;11:349–53. doi: 10.1089/acm.2005.11.349. [DOI] [PubMed] [Google Scholar]
- 15.Chaudhuri K, Samarakoon SM, Chandola HM, et al. Evaluation of diet and life style in etiopathogenesis of senile dementia: A survey study. Ayu. 2011;32:171–76. doi: 10.4103/0974-8520.92554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rao AV. Mind in ayurveda. Indian J Psychiatry. 2002;44:201–11. [PMC free article] [PubMed] [Google Scholar]
- 17.Yang CM, Lin FW, Spielman AJ. A standard procedure enhances the correlation between subjective and objective measures of sleepiness. Sleep. 2004;27:329–32. doi: 10.1093/sleep/27.2.329. [DOI] [PubMed] [Google Scholar]
- 18.Soper DS. Post-hoc Statistical Power Calculator for Multiple Regression Software. 2014. Available from: URL: http://www.danielsoper.com.
- 19.Zar JH. Biostatistical analysis. UK: Pearson education Publishers; 1999. [Google Scholar]
- 20.Shilpa S, Murthy CG. Development and standardization of Mysore Tridosha scale. Ayu. 2011;32:308–14. doi: 10.4103/0974-8520.93905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Manjunath NK, Telles S. Influence of Yoga and Ayurveda on self-rated sleep in a geriatric population. Indian J Med Res. 2005;121:683–90. [PubMed] [Google Scholar]
- 22.Hankey A. Establishing the Scientific Validity of Tridosha part 1: Doshas, Subdoshas and Dosha Prakritis. Anc Sci Life. 2010;29:6–18. [PMC free article] [PubMed] [Google Scholar]
- 23.Weller M. Nutrition and sleep. Br Med J. 1972;2:593. doi: 10.1136/bmj.2.5813.593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Anders D, Gompper B, Kräuchi K. A two-night comparison in the sleep laboratory as a tool to challenge the relationship between sleep initiation, cardiophysiological and thermoregulatory changes in women with difficulties initiating sleep and thermal discomfort. Physiol Behav. 2013;114–15:77–82. doi: 10.1016/j.physbeh.2013.02.020. [DOI] [PubMed] [Google Scholar]
- 25.Ortiz-Tudela E, Bonmatí-Carrión Mde L, De la Fuente M, Mendiola P. Chronodisruption and ageing. Rev Esp Geriatr Gerontol. 2012;47:168–73. doi: 10.1016/j.regg.2011.09.013. [in Spanish] [DOI] [PubMed] [Google Scholar]
- 26.Tarnopolsky A, Watkins G, Hand DJ. Aircraft noise and mental health: I. Prevalence of individual symptoms. Psychol Med. 1980;10:683–98. doi: 10.1017/s0033291700054982. [DOI] [PubMed] [Google Scholar]
- 27.Menet JS, Rosbash M. When brain clocks lose track of time: cause or consequence of neuropsychiatric disorders. Curr Opin Neurobiol. 2011;21:849–57. doi: 10.1016/j.conb.2011.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Palermo TM, Law E, Churchill SS, Walker A. Longitudinal course and impact of insomnia symptoms in adolescents with and without chronic pain. J Pain. 2012;13:1099–106. doi: 10.1016/j.jpain.2012.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berg SK, Higgins M, Reilly CM, et al. Sleep quality and sleepiness in persons with implantable cardioverter defibrillators: outcome from a clinical randomized longitudinal trial. Pacing Clin Electrophysiol. 2012;35:431–43. doi: 10.1111/j.1540-8159.2011.03328.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brand S, Luethi M, von Planta A. Romantic love, hypomania, and sleep pattern in adolescents. J Adolesc Health. 2007;41:69–76. doi: 10.1016/j.jadohealth.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 31.Krishnamurthy KH. Bhela Samhitha. Varanasi: Chaukhambha Visvabharati; 2008. p. 448. [Google Scholar]
- 32.Boudebesse C, Henry C. Emotional hyper-reactivity and sleep disturbances in remitted patients with bipolar disorders. Encephale. 2012;38(Suppl 4):S173–78. doi: 10.1016/S0013-7006(12)70096-9. [in French] [DOI] [PubMed] [Google Scholar]
- 33.Simor P, Horváth K, Gombos F. Disturbed dreaming and sleep quality: altered sleep architecture in subjects with frequent nightmares. Eur Arch Psychiatry Clin Neurosci. 2012;262:687–96. doi: 10.1007/s00406-012-0318-7. [DOI] [PubMed] [Google Scholar]
- 34.King DL, Gradisar M, Drummond A, et al. The impact of prolonged violent video-gaming on adolescent sleep: an experimental study. J Sleep Res. 2013;22:137–43. doi: 10.1111/j.1365-2869.2012.01060.x. [DOI] [PubMed] [Google Scholar]
- 35.Tripathi PK, Patwardhan K, Singh G. The basic cardiovascular responses to postural changes, exercise, and cold pressor test: do they vary in accordance with the dual constitutional types of ayurveda? Evid Based Complement Alternat Med. 2011;2011 doi: 10.1155/2011/251850. pii: 251850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.ICD-10. International Statistical Classification of Diseases and Related Health Problems 10th Revision. Available from: URL: http://en.wikipedia.org/wiki/ICD-10. [PubMed]