Abstract
Background:
In conservative breast surgery, the achievement of a satisfactory cosmetic result could be challenging; oncoplastic techniques may be helpful in many cases. A comparative analysis was performed among 3 groups of patients undergoing oncoplastic techniques plus external radiation therapy or intraoperative radiotherapy (IORT) and breast conservative surgery plus external radiation therapy; long-term oncologic results in terms of disease relapse and aesthetic outcomes were compared.
Methods:
Ninety-six patients were considered: 32 patients treated with oncoplastic surgery, 16 then subjected to radiotherapy (group 1) and another 16 treated with IORT (group 2); 64 patients treated by conservative surgery and radiotherapy formed the control group (group 3). Patients were asked to give a judgment on the cosmetic result considering the following parameters: breast symmetry, appearance of the residual scar, symmetry between the 2 nipple-areola complexes, global aesthetic judgment, and satisfaction about the result.
Results:
With respect to the oncological and aesthetic outcome, the statistical significance of the results obtained in the 3 groups was calculated using the chi-square test. The results, processed by the chi-square test, were not statistically significant; however, the overall judgments expressed by the patients of all 3 groups were more than satisfactory (scores greater than or equal to 6).
Conclusions:
In our experience, when the inclusion criteria are satisfied and the equipment is available, oncoplastic techniques associated with IORT should be considered the treatment of choice for breast cancer in early stage. The excellent cosmetic results and patient’s satisfaction encourage us to continue on this way.
In breast conserving surgery (BCS), a satisfactory cosmetic result could be difficult to obtain due to the size and ptosis of mammary gland, the tumor size and location, and the amount of excised breast tissue.1,2
The application of oncoplastic techniques allows the performance of wide excision, conserving an excellent breast shape, avoiding delayed corrections after lumpectomy when tissue scarring and fibrosis from radiotherapy are present.3
The choice between different techniques of reduction mammoplasty in our series depends on tumor location; direct approach on tumor bed is preferred so that reshaping on residual mammary gland may be minimized.4,5
In our experience, a close collaboration between surgical oncologist and plastic surgeon was carried out to integrate tumor safe excision and safe glandular reduction.5 In early breast cancer, the introduction of accelerated partial-breast irradiation (APBI),6,7 in particular intraoperative radiotherapy (IORT), has deeply modified the approach to conservative and oncoplastic treatment.
The aim of this study was to perform a comparative analysis among 3 groups of patients undergoing oncoplastic techniques plus external radiation therapy (group 1) or IORT (group 2) and BCS plus external radiation therapy (group 3). Long-term oncologic results in terms of disease relapse and aesthetic outcomes were compared.
MATERIALS AND METHODS
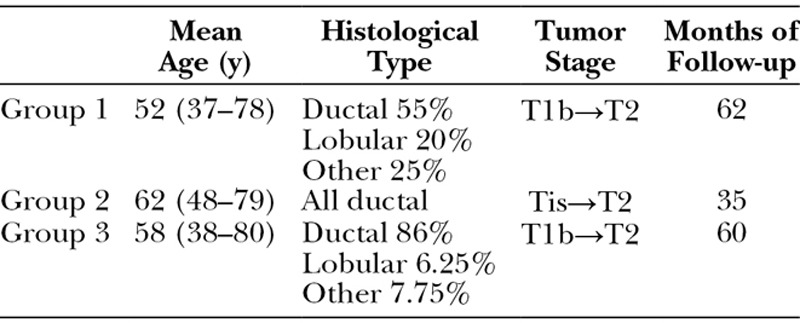
Group 1 and group 2 consisted of 16 patients each, whereas the control group was composed of 64 patients and were selected retrospectively considering similar age, histological characteristics, and tumor node mestasis (TNM) staging system.
Oncoplastic techniques were applied following the protocol approved by the Institutional Ethics Committee in 2004: to patients with particular physical features such as medium/large-sized and ptotic breast (from II–IV degree ptosis) and to those in which removed breast tissue is more than 10% of total volume for small breast and more than 20% for large breast. A specific informed consent was signed by all patients.
From the oncologic viewpoint, the admission criteria of oncoplastic techniques were the same of conserving breast surgery.8 Oncoplastic techniques were always applied, regardless of breast volume, in case of lump located behind nipple-areola complex. The choice between different techniques of reduction mammoplasty in these series depended on tumor location, so direct approach on tumor bed was achieved and reshaping on residual mammary gland was minimized.
Inclusion criteria for partial breast irradiation were respected: no lobular carcinoma, age > 45 years, single lump with diameter < 2.5 cm, pN0, intraductal component of lump < 25%, and safe resection margin < 5 mm in histological specimen.
Therefore, patients must meet both selection criteria of conservative surgery and IORT.
A comprehensive preoperative consultation with plastic and oncologic surgeon, including a discussion with the patient about her physical peculiarity, psychological status, expectations, and choice between unilateral or bilateral procedure, preceded the operation. The markings on the breast were made with the patient in standing position, considering the lump position, the extension of undermining tissue, and the amount of breast reduction. In patients undergoing oncoplastic techniques and IORT, after reduction mammoplasty and lump resection, a total dose of 18 Gy or 21 Gy was delivered directly to the mammary gland depending on tumor volume. After tumor resection, a mobilization of the mammary gland, from the pectoralis muscle and the skin, is carried out to obtain a good exposure to radiation beam. A shielding disk, available in various diameters from 4 to 10 cm, is positioned between gland and pectoralis muscle to protect thoracic wall, heart, and lung. The lead disk is chosen keeping in consideration the ratio of tumor size and breast volume.
The standard schedules for external breast irradiation were 1.8- to 2-Gy daily fractions given 5 times a week to a total dose of 45–50 Gy with optional addition of a boost to the primary site of 10–16 Gy in 5–8 daily fractions over 1–1.5 weeks.
All patients were followed prospectively. The aesthetic outcomes of all groups were evaluated using a scale from 0 to 10,9 where 0 means the worst aesthetic outcome and 10 the best possible one. The aesthetic global result, breast symmetry, areola-nipple symmetry, and scarring were considered.
The results were further divided into 4 categories: low (score 1–5), sufficient (score 6), good (score 7–9), and very good (score 10).
The variables were compared using Fisher’s exact test; regression analysis was used to analyze correlation between 2 different variables (global cosmetic outcome/specimen weight) in the oncoplastic groups.
RESULTS
Mean age, histological type, tumor stage, and duration of follow-up of the 3 groups are shown in Table 1.
Table 1.
Characteristics of the 3 Groups
As regards recurrence and metastasis/second tumor, in group 1, 2 metastasis/second tumor appeared, whereas in group 3, 1 recurrence and 1 metastasis appeared; no metastasis or recurrence appeared in group 2. No statistically significant differences concerning oncologic parameters were observed in 3 groups (recurrence P = 0.505; metastasis/second tumor P = 0.506).
One patient of the control group was not interviewed because of serious mental illness.
Concerning the aesthetic parameters, all patients of 3 groups expressed favorable judgment (scores ≥6) (Table 2). To evaluate the statistical significance among the 3 groups, we have further distinguished sufficient (score >6)/insufficient (score <6) judgment: the difference between the 3 groups was not statistically significant (chi-square test, 4 in the symmetry analysis; chi-square test, 1.014 for the scar evaluation; chi-square test, 2.277 for nipple-areola complex analysis; chi-square test, 0 for the global judgment); however, group 2 expressed higher scores in all parameters (Fig. 1).
Table 2.
Results Regarding Patient Behavior When a Consult with the Plastic Surgeon Was Offered in Cases of Sufficient or Insufficient Judgment
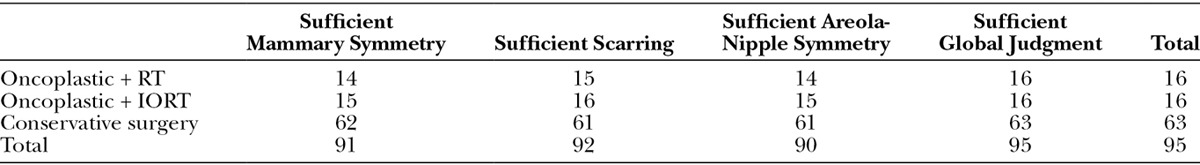
Fig. 1.
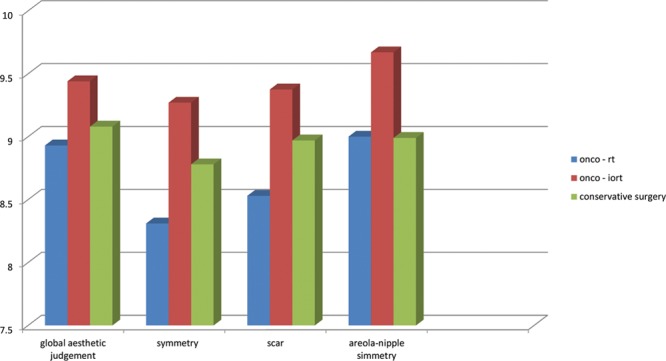
Scores given by the patients of each group on the aesthetic parameters (global aesthetic judgment, breast symmetry, scar, and symmetry between the 2 nipple-areola complex).
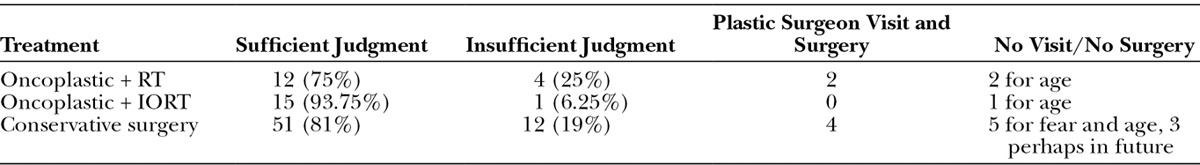
Among patients who expressed judgment around sufficient or insufficient (score ≤6), a consult with a plastic surgeon was offered with different results in the 3 groups (Table 3).
Table 3.
Aesthetic Parameters Were Evaluated in the 3 Groups
When regression test was used to analyze the correlation between aesthetic global judgment and specimen weight in oncoplastic groups, the aesthetic judgments were more favorable when more glandular tissues were removed in groups 1 and 2 (Fig. 2).
Fig. 2.
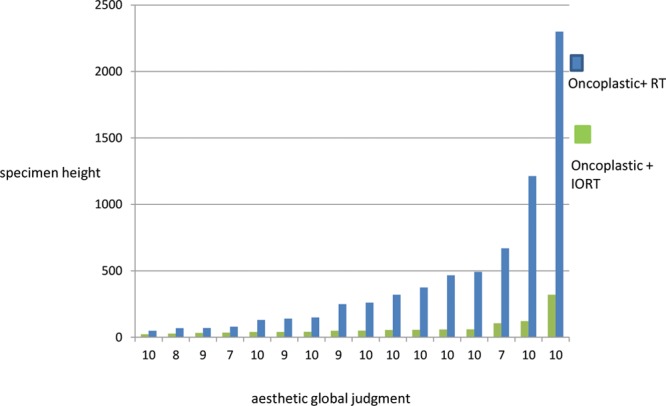
Analysis of the correlation between aesthetic global judgment and specimen weight in oncoplastic groups (P value in group 1 = 0.000395; P value in group 2 = 0.0028).
DISCUSSION
Oncoplastic surgery combines the principles of surgical oncology with those of plastic surgery so that satisfactory cosmetic results can be achieved respecting the oncologic safety. The low rate of recurrence/metastasis observed in the groups confirms the oncologic safety of both conservative and oncoplastic surgery. Moreover, the absence of recurrence in group 2 proves that IORT is a safe technique when criteria of inclusion/exclusion are respected and radiotherapy technique is carefully performed. The extension of cutaneous access in oncoplasty plus IORT is wider in comparison with classic lumpectomy plus IORT so that larger disks may be used and radiation therapy may be applied on wider extension of residual glandular flaps optimizing the procedure.
The aesthetic parameters evaluated in the 3 groups have not shown statistically significant differences. In particular, the results obtained by groups 1 and 3 are substantially equivalent. This could be due to different reasons. In group 1, 6 of 16 patients (37.5%) chose unilateral oncoplastic surgery without immediate contralateral mammoplasty, causing the presumption of an unsatisfactory result. The medium volume removed in group 1 was 434 g, whereas in the control group, it was 43. In BCS, almost all authors agree that a satisfactory cosmetic result depends on percentage of excised breast tissues.6,7 Oncoplastic techniques give more satisfactory results when more conspicuous glandular tissue is removed, appearing an overtreatment for breast with small volume/ptosis due to wider extension of scars; good aesthetic results can be achieved also without reduction mammoplasty techniques as supported by other authors.7
The external radiation therapy produces an increase of density in breast tissues so that the postoperative cosmetic result can be maintained in the irradiated breast more than in the healthy breast; the aesthetic results became unsatisfactory after 5 years, and a further mammoplasty procedure should be recommended to restore breast symmetry (Fig. 3).
Fig. 3.

A, Preoperative view of a 53-year-old woman. B, Postoperative view after 6 months. C, Postoperative view after 5 years..
The scars that follow reduction mammoplasty are wider than those following conservative breast surgery and can become even more evident after radiotherapy, causing an impairment of cosmetic results (Fig. 4).
Fig. 4.

Postoperative view of a 50-year-old patient who underwent left oncoplastic surgery and external radiotherapy plus contralateral reduction mammoplasty, giving a low score concerning the scar appearance.
Finally, patients of the control group are older than those of the group 1, and they may be more inclined to be satisfied with cosmetic global results.
The best judgment about breast symmetry and scar was formulated by group 2; perhaps intraoperative radiation therapy may be considered the key to obtain a satisfactory aesthetic result. It spares breast tissue and skin because it is applied only on tumor bed during surgery so that less fibrosis develops on glandular tissue and consequently breast ptosis can be equivalent as years go on (Fig. 5).
Fig. 5.

Postoperative view of a 50-year-old patient who underwent oncoplastic techniques and IORT. After 5 years, the satisfactory result is maintained.
Moreover, the global judgment may also be affected by psychological factors: the patients of group 2 have an early-stage breast cancer, only 18 (75%) underwent chemotherapy and they have had no experience of external radiotherapy with repeated sessions.
CONCLUSIONS
We can conclude that on oncologic viewpoint, if guidelines are met, all 3 techniques gave satisfactory results, leading to adequate tumor resection. On aesthetic viewpoint, both oncoplastic and BCS determine satisfactory aesthetic results, if different body structure of patients has to be evaluated. However, the association between oncoplasty and IORT gives very acceptable outcomes as long as strict criteria of inclusion are applied. Encouraging results may be obtained with a close collaboration among surgical oncologist, plastic surgeon, and radiotherapist during preoperative planning and surgery.
Footnotes
Presented at the 63rd SICPRE National Meeting (Società Italiana di Chirurgia Plastica Ricostruttiva ed Estetica, Italian Society of Plastic, Reconstructive and Aesthetic Surgery), October 12–15, 2014, Bergamo, Italy.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the Società Italiana di Chirurgia Plastica Ricostruttiva ed Estetica.
REFERENCES
- 1.Haloua MH, Krekel NM, Winters HA, et al. A systematic review of oncoplastic breast-conserving surgery: current weaknesses and future prospects. Ann Surg. 2013;257:609–620. doi: 10.1097/SLA.0b013e3182888782. [DOI] [PubMed] [Google Scholar]
- 2.Ozmen T, Polat AV, Polat AK, et al. Factors affecting cosmesis after breast conserving surgery without oncoplastic techniques in an experienced comprehensive breast center. Surgeon. 2014 doi: 10.1016/j.surge.2013.12.005. Feb 12 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 3.Munhoz AM, Aldrighi CM, Montag E, et al. Outcome analysis of immediate and delayed conservative breast surgery reconstruction with mastopexy and reduction mammaplasty techniques. Ann Plast Surg. 2011;67:220–225. doi: 10.1097/SAP.0b013e3181f77bba. [DOI] [PubMed] [Google Scholar]
- 4.Clough KB, Kaufman GJ, Nos C, et al. Improving breast cancer surgery: a classification and quadrant per quadrant atlas for oncoplastic surgery. Ann Surg Oncol. 2010;17:1375–1391. doi: 10.1245/s10434-009-0792-y. [DOI] [PubMed] [Google Scholar]
- 5.Franchelli S, Meszaros P, Guenzi M, et al. Preliminary experience using oncoplastic techniques of reduction mammaplasty and intraoperative radiotherapy: report of 2 cases. Aesthetic Plast Surg. 2011;35:1180–1183. doi: 10.1007/s00266-011-9735-7. [DOI] [PubMed] [Google Scholar]
- 6.Smith BD, Arthur DW, Buchholz TA, et al. Accelerated partial breast irradiation consensus statement from the American Society for Radiation Oncology (ASTRO). Int J Radiat Oncol Biol Phys. 2009;74:987–1001. doi: 10.1016/j.ijrobp.2009.02.031. [DOI] [PubMed] [Google Scholar]
- 7.Hannoun-Levi JM, Resch A, Gal J, et al. GEC-ESTRO Breast Cancer Working Group. Accelerated partial breast irradiation with interstitial brachytherapy as second conservative treatment for ipsilateral breast tumour recurrence: multicentric study of the GEC-ESTRO Breast Cancer Working Group. Radiother Oncol. 2013;108:226–231. doi: 10.1016/j.radonc.2013.03.026. [DOI] [PubMed] [Google Scholar]
- 8.NICE. National Institute for Health and Clinical Excellence (NICE) Guidelines. Available at: http://www.guideline.gov. Accessed February 2009.
- 9.Garbay JR, Rietjens M, Petit JY. [Esthetic results of breast reconstruction after amputation for cancer. 323 cases]. J Gynecol Obstet Biol Reprod (Paris) 1992;21:405–412. [PubMed] [Google Scholar]


