Abstract
Cognitive contributions to the behaviors observed in substance and non-substance addictions have been investigated and characterized. Based on models of drug addictions and the extant literature on Internet gaming disorder (IGD), we propose a cognitive-behavioral model for conceptualizing IGD. The model focuses on three domains and their roles in addictive behaviors. The three domains include motivational drives related to reward-seeking and stress-reduction, behavioral control relating to executive inhibition, and decision-making that involves weighing the pros and cons of engaging in motivated behaviors. Based on this model, we propose how behavioral therapies might target these domains in the treatment of IGD.
Keywords: Internet gaming disorder, cognitive model, reward sensation, executive control, decision making
Background
Internet addiction disorder (IAD) or problematic Internet use has been proposed as a diagnostic entity and studied for more than a decade; however, there has been debate regarding a standardized definition for such a disorder. Although no formal diagnostic criteria for a psychiatric condition characterized by excessive and interfering patterns of Internet use were included in the fourth edition of the Diagnostic and Statistical Manual (DSM-IV) (Block, 2008, Shaw and Black, 2008, Liu et al., 2011), the DSM-5 committee considering substance-use and addictive disorders generated criteria for Internet gaming disorder (IGD), and this condition is included in the section of the DSM-5 containing disorders warranting additional study (American Psychiatric Association, 2013, Petry and O'Brien, 2013). Given this recent change in the DSM, we will refer to excessive Internet gaming, addictive Internet gaming, or pathological online gaming as IGD in the current manuscript, although we recognize that the term and diagnostic construct might differ and none have been systematically examined with respect to current criteria for IGD.
Unlike drug addiction or substance abuse, no chemical or substance intake is involved in IAD or IGD, although excessive Internet use may lead to physical dependence, similar to other addictions (Holden, 2001, Dong et al., 2013a). This observation suggests that people’s online experiences may change brain structure and function, and related cognitive processes, in manners that may perpetuate Internet use (Holden, 2001, Weinstein and Lejoyeux, 2010, Dong et al., 2011b). Although it has been proposed that excessive Internet use may involve at least three subtypes relating to gaming, sexual preoccupations, and email/text messaging (Block, 2008), other subtypes may exist (e.g. relating to other types of behaviors (social networking) or motivations that may underlie Internet use, such as those relating to positive or negative reinforcements). While additional research is needed to identify clinically meaningful subgroups, a model that describes cognitive domains, their inter-relationships and how the domains might be targeted in treatment could be helpful in the study and research of IGD.
Unanswered questions exist regarding the precise features that may lead some individuals to use the Internet excessively or compulsively. IGD behaviors may be driven by experiences involving strong emotions. The frequent and repetitive engagement in such behaviors may alter brain structure and function underlying specific cognitive processes. In this paper, we propose a cognitive-behavioral model for IGD based on the extant literatures.
Although few trials have been conducted to test the efficacies and tolerabilities of medications in the treatment of IGD (Liu and Potenza, 2007, Flisher, 2010, Huang et al., 2010, Yau et al., 2012), IGD treatments might consider psychological or cognitive processes as potential targets for pharmacological or behavioral interventions (Huang et al., 2010). Based on the proposed cognitive-behavioral model, possible approaches for the treatment of IGD are discussed, with a focus on behavioral therapies.
A cognitive-behavioral model of IGD
A central component of addictions involves reward-seeking (Potenza, 2013). Reward-centric models have focused on pleasurable aspects of drug-taking with the notion that drugs may “hijack” brain reward circuits (Volkow and Li, 2004, Nestler, 2005). The incentive salience model of drug addiction proposes that “liking” a drug may be separated from “wanting” the drug (Berridge, 2007). A “reward deficiency syndrome” model posits that addicted individuals engage in addictive behaviors to compensate for hypo-functioning reward signals in the mesolimbic dopamine pathway (Blum et al., 2006). Negative-reinforcement models suggest that relief from aversive states (e.g., relating to stress) may drive participation in addictive behaviors. Motivation-focused models have proposed that addiction might be considered a disorder of misdirected motivation in which relatively greater priority is given to drug use (as opposed to other motivational behavioral domains like occupational or familial) (Chambers et al., 2003, Kalivas and Volkow, 2005). These and other models (e.g., the impaired response inhibition salience attribution – IRISA (Goldstein and Volkow, 2011)) consider that diminished executive control over pro-motivational drives may contribute to decisions to engage in addictive behaviors.
Like in these models of drug addiction, we propose that motivational drives linked to reward-seeking contribute importantly to IGD and that diminished executive function/cognitive control over these motivational drives contribute to decision-making that leads to persistent engagement in Internet game-playing in IGD (Figure 1). In the figure, we also indicate possible areas which may be targeted with specific therapies (which are discussed later in the manuscript), although these possible relationships remain largely untested at this point. Nonetheless, the proposed model provides a theoretical basis for hypothesis testing in mechanistic studies and treatment development.
Figure 1. A cognitive-behavioral model of IGD.
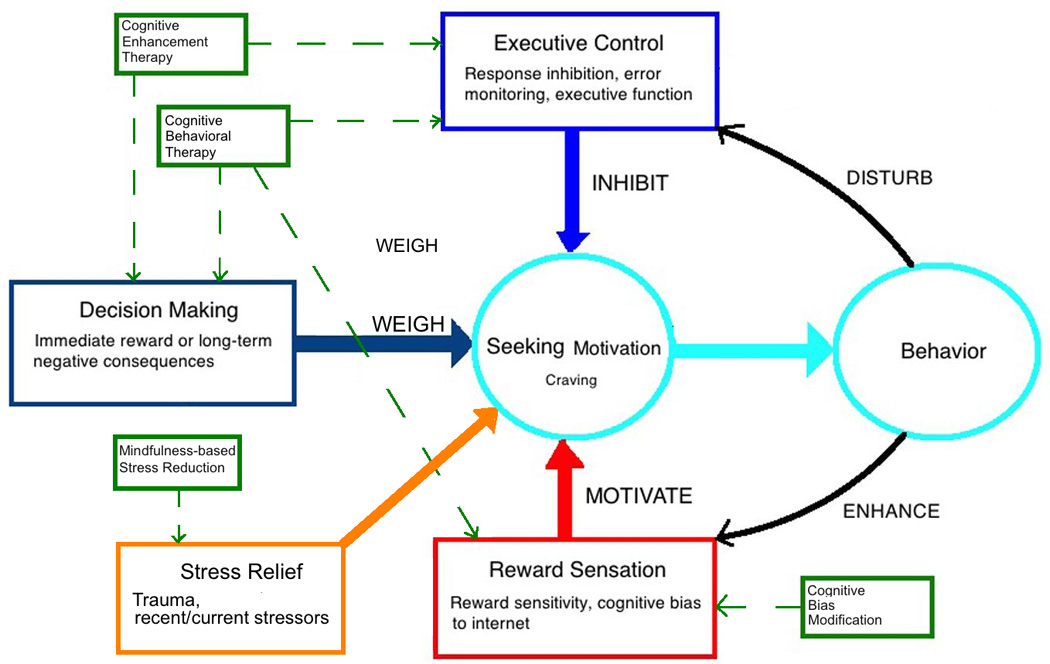
This figure shows proposed cognitive domains associated with IGD. The model focuses on three cognitive domains and their possible roles in addictive behaviors. The three domains include motivational drives related to reward-seeking and stress reduction, behavioral control relating to executive inhibition, and decision-making that weighs the consequences of engaging in motivated behaviors. Online gaming behaviors might further disturb executive control and reinforce rewarding online experiences, which may lead to a vicious cycle of addictive Internet game-playing. The contents framed in green boxes show potential psychological and cognitive treatments for IGD. Dashed lines indicate potential targets of intervention strategies, with further studies needed to investigate efficacies and possible mechanisms of actions.
Reward and motivation in IGD
Given the role of reward processing in behavioral and drug addictions, investigators have examined aspects of reward sensitivity in IGD. Studies that have used guessing tasks have found that individuals with IGD show enhanced reward sensitivity and decreased loss sensitivity in mild (Dong et al., 2011a, Dong et al., 2012) and extreme (Dong et al., 2013a) winning and losing situations. Online behaviors may be perceived as rewarding through feelings of being in control and immediate achievement (Leung, 2004). Enhanced reward sensitivity in IGD may underlie desires to use the Internet and promote online game-playing for longer periods of time. In this manner, enhanced reward sensitivity and decreased loss sensitivity might contribute to the development of IGD (Dong et al., 2013b).
Executive control: Inhibition of cravings and limiting excessive Internet use
Executive systems are posited to promote cognitive and behavioral control over motivational drives and may enable individuals to inhibit desires and control the extent of participation in reward-seeking behaviors (Everitt et al., 2007, Goldstein and Volkow, 2011,Sofuoglu et al., 2013). These features may contribute importantly to IGD. Reduced response-inhibition and cognitive-control tendencies or abilities have been demonstrated in subjects with IGD (as compared to those without) using go/no-go (Dong et al., 2010), Stroop (Dong et al., 2011c) and switching (Dong et al., 2014) tasks, respectively. Such response tendencies appear influenced by Internet-gaming-related stimuli, with poorer performance seen in groups with IGD relative to those without in response to online-gaming stimuli as compared to control stimuli during performance of a game-shifting task (Zhou et al., 2012). These findings suggest a cognitive bias similar to that seen in other addictions (Potenza, 2014), as well as altered set-shifting tendencies that may relate importantly to compulsive aspects of addictions. Apparent set-shifting and cognitive–control deficits in IGD may relate to inefficient processing within neural circuitry underlying these processes, a notion consistent with findings relating these neural measures to Internet addiction severity (Dong et al., 2013c). Taken together, the existing findings suggest that neural processes underlying attention, response inhibition and behavioral flexibility in individuals with IGD relate importantly to IGD severity, although the extent to which these findings reflect predisposing factors or neural functions that arise during phases of IGD development is not yet understood.
Decision-making: Weighing short-term pleasures and long-term negative consequences
Reduced cognitive capacity or willingness to avoid excessive behavioral engagement in pleasurable activities may contribute to the development of various clinical problems, including addictive disorders like gambling and substance-use disorders (Potenza et al., 2013). Studies suggest that individuals with IGD show enhanced regional brain activations when performing decision-making tasks (Dong et al., 2013b). Data also suggest that individuals with IGD show diminished consideration of experiential outcomes when making future decisions (Dong et al., 2013b). In making decisions between participating in immediately rewarding experiences (e.g., playing online) and long-term adverse consequences (e.g., using the time spent gaming instead to perform activities associated with longer term occupational success), individuals with IGD may show a “myopia for the future”, as has been described for drug addictions (Pawlikowski and Brand, 2011, Floros and Siomos, 2012, Bechara et al., 2002). As decision-making arguably acts as a final ‘check point’ before a behavior is enacted, future investigations should examine the extent to which decision-making deficits may predispose to the development of IGD or whether decision-making capacities may become impaired during the course of IGD.
Interactions among cognitive domains
Increased reward sensations during winning or pleasurable experiences may enhance desires to play online for individuals with IGD. Meanwhile, impairments in executive control capacities may lead to poor control over such desires, which may permit urges, desires or cravings to dominate and lead to excessive Internet use in IGD. Such imbalances may promote disadvantageous decision-making in IGD, leading to pursuit of short-term pleasures rather than long-term gains. Reward-seeking behaviors may be reinforced through short-term online experiences, and these may further disturb executive-control abilities, leading to a vicious cycle of addictive Internet use.
Clinical implications
Several categories of behavioral interventions have demonstrated efficacy in the treatment of gambling and/or drug addictions through randomized controlled trials (Potenza et al., 2011; Potenza et al., 2013): 1) brief and motivational interventions, which may alter decision-making processes to focus on more future-oriented goals (Burke et al., 2003); 2) contingency management, which provides immediate reinforcement to promote abstinence (Dutra et al., 2008); and, 3) cognitive behavioral therapies, which emphasize the development of cognitive strategies to countervail motivational drives for drugs and provides skills for managing situations that previously predisposed to drug use (Carroll and Onken, 2005). Additionally, other therapies that have preliminary support in targeting addictions and more established support in targeting domains that may promote engagement in addictive behaviors warrant consideration. For example, mindfulness-based therapies that have more established support in stress reduction have demonstrated support in targeting drug addictions (Brewer et al., 2009, Brewer et al., 2010, Brewer et al., 2013, Witkiewitz et al., 2013), and this approach may be particularly helpful for individuals whose behaviors are driven by negative-reinforcement motivations.
Based on the proposed cognitive-behavioral model for IGD and the evidence-based treatments for drug addictions and stress reduction, potential effective treatment methods for IGD might target one or more of the following domains: (1) inhibition of desires to play games or otherwise engage excessively in Internet use; (2) strengthening of cognitive capacities to inhibit participation in Internet use; and (3) overcoming myopic decision-making by placing emphasis on longer-term goals rather than shorter-term pleasures. Below we consider behavioral therapeutic approaches used in drug addiction, their application to IGD, and how these cognitive domains may relate to the therapies. It should be noted that limited data from randomized clinical trials exist to determine the extent to which these therapies have support in the treatment of IGD, or how their active ingredients might operate in the treatment of IGD and with respect to the proposed model.
Cognitive behavioral therapy (CBT)
CBT is one of comparatively few empirically supported therapies that has been demonstrated to be effective across a range of substance-use disorders (Carroll et al., 2011, DeVito et al., 2012). Studies suggest that the putative “active ingredients” of CBT may exert their effects to strengthen the aspects of executive control over behaviors given that acquisition of these types of skills in CBT are associated with better long-term outcomes (Kiluk et al., 2010). CBT has been used in IGD treatment because it may help individuals with IGD improve their inhibitory control ability, recognize maladaptive cognitions, and employ more adaptive decision-making ( Huang et al., 2010). However, unlike CBT for drug addictions, no studies have formally examined the efficacy of CBT for IGD, nor have manualized therapies undergone systematic assessment in randomized clinical trials. Future studies should focus on these endeavors, with initial efforts underway (Jager et al., 2012).
Cognitive enhancement therapy (CET)
As described above, IGD subjects often show cognitive disturbances relating to elevated impulsivity, impaired cognitive control and cognitive inflexibility. Thus, therapies that target these domains may be helpful in ameliorating symptoms of IGD. CET typically involves repeated practice of cognitive tasks involving problem-solving, response inhibition, visual tracking, and discrimination skills, with such practice occurring for several hours per week over a course of several months (Sofuoglu et al., 2013). Such training has resulted in significant improvement in impulsivity and delay discounting among stimulant users (Bickel et al., 2011), and similar strategies warrant consideration in targeting cognitive function in individuals with IGD.
Cognitive bias modification (CBM)
As individuals with IGD have been shown to demonstrate attentional biases towards Internet cues, therapies that target such biases might be efficacious in the treatment of IGD (Zhou et al., 2012). CBM specifically targets automatic/implicit processes, such as attention bias and approach bias (Schoenmakers et al., 2010). As CBM has shown positive effects in the treatment of alcohol-use disorders and other 11 psychopathologies ( Hakamata et al., 2010), its potential in treating IGD warrants investigation.
Mindfulness-based Stress Reduction (MBSR)
Stress has exhibited strong associations with IGD (Achab et al., 2011; Peltzer et al., 2014; Spada, 2013). As such, interventions like MBSR that target stress reduction may be helpful for IGD. As stress has been closely linked to addictions in women (Petry et al., 2005, Potenza et al., 2012), MBSR might be particularly helpful for females with IGD, although this hypothesis warrants direct examination.
Combined approaches
Preliminary treatment studies suggest that combinations of several psychotherapeutic strategies may be more effective than a single approach (Orzack et al., 2006, Shek et al., 2009). The psychotherapeutic approaches may include various methods (CBT, CBM, CET and/or MBSR) in various formats (group, individual, family therapy, and school-based intervention), with different strategies complementing aspects of the others. Additionally, combinations of behavioral and pharmacological therapies also warrant consideration and testing in randomized clinical trials.
Conclusions
Recent studies suggest neurocognitive differences in individuals with and without IGD. IGD shares multiple features with drug addictions including elevated impulsivity, cognitive inflexibility, and attentional biases. However, the extent to 12 which these may represent pre-existing factors predisposing to IGD or factors that may develop following excessive Internet gaming, or perhaps a combination of both, is not yet known. Although data from studies of substance addictions suggest the last possibility (that both options may be relevant (Fineberg et al., 2014, Mitchell and Potenza, 2014)), direct examination of these possibilities with respect to IGD is necessary and may best be accomplished though longitudinal studies. As more data become available, the model may be refined over time. Nonetheless, existing findings suggest a theoretical model for IGD and specific cognitive domains that may be targeted with specific psychotherapies. Future studies should examine the efficacies of such psychotherapies in treating IGD and investigate specific cognitive functions that may improve with effective treatment.
Acknowledgements
This research was supported by National Science Foundation of China (31371023). National Institute of Health (R01 DA035058, P50 DA09241, P20 DA027844), the Connecticut Department of Mental Health and Addictive Services, and the National Center for Responsible Gaming.
Dr. Potenza has received financial support or compensation for the following: Dr. Potenza has consulted for and advised Lundbeck, Ironwood ad Shire; has received research support from the National Institutes of Health, Mohegan Sun Casino and the National Center for Responsible Gaming; has participated in surveys, mailings or telephone consultations related to drug addiction, impulse control disorders or other health topics; has consulted for gambling entities and law offices on issues related to impulse control disorders; provides clinical care in the Connecticut Department of Mental Health and Addiction Services Problem Gambling Services Program; has performed grant reviews for the National Institutes of Health and other agencies; has edited journals and journal sections; has given academic lectures in grand rounds, CME events and other clinical or scientific venues; and has generated books or book chapters for publishers of mental health texts.
Role of the funding Source
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Contributors
Guangheng Dong wrote the first draft of the manuscript, Marc Potenza revised and improved the manuscript. All authors contributed to and have approved the final manuscript.
Competing Interests
The authors declared that no competing interests exist.
References
- Achab S, Nicolier M, Mauny F, Monnin J, Trojak B, Vandel P, Sechter D, Gorwood P, Haffen E. Massively multiplayer online role-playing games: comparing characteristics of addict vs non-addict online recruited gamers in a French adult population. BMC Psychiatry. 2011;11:144. doi: 10.1186/1471-244X-11-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Bechara A, Dolan S, Hindes A. Decision-making and addiction (part II): myopia for the future or hypersensitivity to reward? Neuropsychologia. 2002;40:1690–1705. doi: 10.1016/s0028-3932(02)00016-7. [DOI] [PubMed] [Google Scholar]
- Berridge KC. The debate over dopamine's role in reward: the case for incentive salience. Psychopharmacology. 2007;191:391–431. doi: 10.1007/s00213-006-0578-x. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Yi R, Landes RD, Hill PF, Baxter C. Remember the Future: Working Memory Training Decreases Delay Discounting Among Stimulant Addicts. Biol Psychiat. 2011;69:260–265. doi: 10.1016/j.biopsych.2010.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Block JJ. Prevalence underestimated in problematic Internet use study. CNS Spectr. 2006;12:14–15. doi: 10.1017/s1092852900020459. [DOI] [PubMed] [Google Scholar]
- Block JJ. Issues for DSM-V: internet addiction. The American journal of psychiatry. 2008;165:306–307. doi: 10.1176/appi.ajp.2007.07101556. [DOI] [PubMed] [Google Scholar]
- Blum K, Chen TJ, Meshkin B, Downs BW, Gordon CA, Blum S, Mengucci JF, Braverman ER, Arcuri V, Varshavskiy M, Deutsch R, Martinez-Pons M. Reward deficiency syndrome in obesity: a preliminary cross-sectional trial with a Genotrim variant. Advances in therapy. 2006;23:1040–1051. doi: 10.1007/BF02850224. [DOI] [PubMed] [Google Scholar]
- Brewer JA, Bowen S, Smith JT, Marlatt GA, Potenza MN. Mindfulness-based treatments for co-occurring depression and substance use disorders: what can we learn from the brain? Addiction. 2010;105:1698–1706. doi: 10.1111/j.1360-0443.2009.02890.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer JA, Elwafi HM, Davis JH. Craving to quit: psychological models and neurobiological mechanisms of mindfulness training as treatment for addictions. Psychology of addictive behaviors : journal of the Society of Psychologists in Addictive Behaviors. 2013;27:366–379. doi: 10.1037/a0028490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer JA, Sinha R, Chen JA, Michalsen RN, Babuscio TA, Nich C, Grier A, Bergquist KL, Reis DL, Potenza MN, Carroll KM, Rounsaville BJ. Mindfulness training and stress reactivity in substance abuse: results from a randomized, controlled stage I pilot study. Substance abuse : official publication of the Association for Medical Education and Research in Substance Abuse. 2009;30:306–317. doi: 10.1080/08897070903250241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: a meta-analysis of controlled clinical trials. Journal of consulting and clinical psychology. 2003;71:843–861. doi: 10.1037/0022-006X.71.5.843. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Kiluk BD, Nich C, Babuscio TA, Brewer JA, Potenza MN, Ball SA, Martino S, Rounsaville BJ, Lejuez CW. Cognitive function and treatment response in a randomized clinical trial of computer-based training in cognitive-behavioral therapy. Substance use & misuse. 2011;46:23–34. doi: 10.3109/10826084.2011.521069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Onken LS. Behavioral therapies for drug abuse. The American journal of psychiatry. 2005;162:1452–1460. doi: 10.1176/appi.ajp.162.8.1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambers RA, Taylor JR, Potenza MN. Developmental neurocircuitry of motivation in adolescence: a critical period of addiction vulnerability. The American journal of psychiatry. 2003;160:1041–1052. doi: 10.1176/appi.ajp.160.6.1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeVito EE, Worhunsky PD, Carroll KM, Rounsaville BJ, Kober H, Potenza MN. A preliminary study of the neural effects of behavioral therapy for substance use disorders. Drug and alcohol dependence. 2012;122:228–235. doi: 10.1016/j.drugalcdep.2011.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong G, DeVito E, Huang J, Du X. Diffusion tensor imaging reveals thalamus and posterior cingulate cortex abnormalities in internet gaming addicts. Journal of psychiatric research. 2012;46:1212–1216. doi: 10.1016/j.jpsychires.2012.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong G, Hu Y, Lin X. Reward/punishment sensitivities among internet addicts: Implications for their addictive behaviors. Progress in neuro-psychopharmacology & biological psychiatry. 2013a;46:139–145. doi: 10.1016/j.pnpbp.2013.07.007. [DOI] [PubMed] [Google Scholar]
- Dong G, Hu Y, Lin X, Lu Q. What makes Internet addicts continue playing online even when faced by severe negative consequences? Possible explanations from an fMRI study. Biological psychology. 2013b;94:282–289. doi: 10.1016/j.biopsycho.2013.07.009. [DOI] [PubMed] [Google Scholar]
- Dong G, Huang J, Du X. Enhanced reward sensitivity and decreased loss sensitivity in Internet addicts: an fMRI study during a guessing task. Journal of psychiatric research. 2011a;45:1525–1529. doi: 10.1016/j.jpsychires.2011.06.017. [DOI] [PubMed] [Google Scholar]
- Dong G, Lin X, Zhou H, Lu Q. Cognitive flexibility in internet addicts: fMRI evidence from difficult-to-easy and easy-to-difficult switching situations. Addict Behav. 2014;39:677–683. doi: 10.1016/j.addbeh.2013.11.028. [DOI] [PubMed] [Google Scholar]
- Dong G, Lu Q, Zhou H, Zhao X. Precursor or sequela: pathological disorders in people with Internet addiction disorder. PloS one. 2011b;6:e14703. doi: 10.1371/journal.pone.0014703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong G, Shen Y, Huang J, Du X. Impaired error-monitoring function in people with internet addiction disorder: an event-related fMRI study. European addiction research. 2013c;19:269–275. doi: 10.1159/000346783. [DOI] [PubMed] [Google Scholar]
- Dong G, Zhou H, Zhao X. Impulse inhibition in people with Internet addiction disorder: electrophysiological evidence from a Go/NoGo study. Neuroscience letters. 2010;485:138–142. doi: 10.1016/j.neulet.2010.09.002. [DOI] [PubMed] [Google Scholar]
- Dong G, Zhou H, Zhao X. Male Internet addicts show impaired executive control ability: evidence from a color-word Stroop task. Neuroscience letters. 2011c;499:114–118. doi: 10.1016/j.neulet.2011.05.047. [DOI] [PubMed] [Google Scholar]
- Dutra L, Stathopoulou G, Basden SL, Leyro TM, Powers MB, Otto MW. A meta-analytic review of psychosocial interventions for substance use disorders. Am J Psychiat. 2008;165:179–187. doi: 10.1176/appi.ajp.2007.06111851. [DOI] [PubMed] [Google Scholar]
- Everitt BJ, Hutcheson DM, Ersche KD, Pelloux Y, Dalley JW, Robbins TW. The orbital prefrontal cortex and drug addiction in laboratory animals and humans. Annals of the New York Academy of Sciences. 2007;1121:576–597. doi: 10.1196/annals.1401.022. [DOI] [PubMed] [Google Scholar]
- Fineberg NA, Chamberlain SR, Goudriaan AE, Stein DJ, Vanderschuren LJ, Gillan CM, Shekar S, Gorwood PA, Voon V, Morein-Zamir S, Denys D, Sahakian BJ, Moeller FG, Robbins TW, Potenza MN. New developments in human neurocognition: clinical, genetic, and brain imaging correlates of impulsivity and compulsivity. CNS spectrums. 2014;19:69–89. doi: 10.1017/S1092852913000801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flisher C. Getting plugged in: an overview of internet addiction. Journal of paediatrics and child health. 2010;46:557–559. doi: 10.1111/j.1440-1754.2010.01879.x. [DOI] [PubMed] [Google Scholar]
- Floros G, Siomos K. Patterns of choices on video game genres and Internet addiction. Cyberpsychology, behavior and social networking. 2012;15:417–424. doi: 10.1089/cyber.2012.0064. [DOI] [PubMed] [Google Scholar]
- Goldstein RZ, Volkow ND. Dysfunction of the prefrontal cortex in addiction: neuroimaging findings and clinical implications. Nature reviews Neuroscience. 2011;12:652–669. doi: 10.1038/nrn3119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hakamata Y, Lissek S, Bar-Haim Y, Britton JC, Fox NA, Leibenluft E, Ernst M, Pine DS. Attention bias modification treatment: a meta-analysis toward the establishment of novel treatment for anxiety. Biol Psychiatry. 2010;68:982–990. doi: 10.1016/j.biopsych.2010.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holden C. 'Behavioral' Addictions: Do They Exist? Science. 2001;294:980–982. doi: 10.1126/science.294.5544.980. [DOI] [PubMed] [Google Scholar]
- Huang XQ, Li MC, Tao R. Treatment of Internet Addiction. Curr Psychiat Rep. 2010;12:462–470. doi: 10.1007/s11920-010-0147-1. [DOI] [PubMed] [Google Scholar]
- Jager S, Muller KW, Ruckes C, Wittig T, Batra A, Musalek M, Mann K, Wolfling K, Beutel ME. Effects of a manualized short-term treatment of internet and computer game addiction (STICA): study protocol for a randomized controlled trial. Trials. 2012;13:43. doi: 10.1186/1745-6215-13-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalivas PW, Volkow ND. The neural basis of addiction: a pathology of motivation and choice. The American journal of psychiatry. 2005;162:1403–1413. doi: 10.1176/appi.ajp.162.8.1403. [DOI] [PubMed] [Google Scholar]
- Kiluk BD, Nich C, Babuscio T, Carroll KM. Quality versus quantity: acquisition of coping skills following computerized cognitive-behavioral therapy for substance use disorders. Addiction. 2010;105:2120–2127. doi: 10.1111/j.1360-0443.2010.03076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung L. Net-generation attributes and seductive properties of the internet as predictors of online activities and internet addiction. Cyberpsychology & behavior : the impact of the Internet, multimedia and virtual reality on behavior and society. 2004;7:333–348. doi: 10.1089/1094931041291303. [DOI] [PubMed] [Google Scholar]
- Liu T, Potenza MN. Problematic Internet use: clinical implications. CNS spectrums. 2007;12:453–466. doi: 10.1017/s1092852900015339. [DOI] [PubMed] [Google Scholar]
- Liu TC, Desai RA, Krishnan-Sarin S, Cavallo DA, Potenza MN. Problematic Internet use and health in adolescents: data from a high school survey in Connecticut. The Journal of clinical psychiatry. 2011;72:836–845. doi: 10.4088/JCP.10m06057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell M, Potenza M. Addictions and Personality Traits: Impulsivity and Related Constructs. Curr Behav Neurosci Rep. 2014;1:1–12. doi: 10.1007/s40473-013-0001-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nestler EJ. Is there a common molecular pathway for addiction? Nature neuroscience. 2005;8:1445–1449. doi: 10.1038/nn1578. [DOI] [PubMed] [Google Scholar]
- Orzack MH, Voluse AC, Wolf D, Hennen J. An ongoing study of group treatment for men involved in problematic Internet-enabled sexual behavior. Cyberpsychology & behavior : the impact of the Internet, multimedia and virtual reality on behavior and society. 2006;9:348–360. doi: 10.1089/cpb.2006.9.348. [DOI] [PubMed] [Google Scholar]
- Pawlikowski M, Brand M. Excessive Internet gaming and decision making: do excessive World of Warcraft players have problems in decision making under risky conditions? Psychiatry research. 2011;188:428–433. doi: 10.1016/j.psychres.2011.05.017. [DOI] [PubMed] [Google Scholar]
- Peltzer K, Pengpid S, Apidechkul T. Heavy Internet use and its associations with health risk and health-promoting behaviours among Thai university students. Int J Adolesc Med Health. 2014;26:187–194. doi: 10.1515/ijamh-2013-0508. [DOI] [PubMed] [Google Scholar]
- Petry NM, O'Brien CP. Internet gaming disorder and the DSM-5. Addiction. 2013;108:1186–1187. doi: 10.1111/add.12162. [DOI] [PubMed] [Google Scholar]
- Petry NM, Steinberg KL, Women's Problem Gambling Research C. Childhood maltreatment in male and female treatment-seeking pathological gamblers. Psychology of addictive behaviors : journal of the Society of Psychologists in Addictive Behaviors. 2005;19:226–229. doi: 10.1037/0893-164X.19.2.226. [DOI] [PubMed] [Google Scholar]
- Potenza MN. Biological Contributions to Addictions in Adolescents and Adults: Prevention, Treatment, and Policy Implications. Journal of Adolescent Health. 2013;52:S22–S32. doi: 10.1016/j.jadohealth.2012.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potenza MN. Biased behaviors: towards understanding vulnerability and resilience factors in addictions. Biol Psychiatry. 2014;75:94–95. doi: 10.1016/j.biopsych.2013.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potenza MN, Balodis IM, Franco CA, Bullock S, Xu J, Chung T, Grant JE. Neurobiological considerations in understanding behavioral treatments for pathological gambling. Psychology of addictive behaviors : journal of the Society of Psychologists in Addictive Behaviors. 2013;27:380–392. doi: 10.1037/a0032389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potenza MN, Hong KI, Lacadie CM, Fulbright RK, Tuit KL, Sinha R. Neural correlates of stress-induced and cue-induced drug craving: influences of sex and cocaine dependence. The American journal of psychiatry. 2012;169:406–414. doi: 10.1176/appi.ajp.2011.11020289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potenza MN, Sofuoglu M, Carroll KM, Rounsaville BJ. Neuroscience of Behavioral and Pharmacological Treatments for Addictions. Neuron. 2011;69:695–712. doi: 10.1016/j.neuron.2011.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoenmakers TM, de Bruin M, Lux IF, Goertz AG, Van Kerkhof DH, Wiers RW. Clinical effectiveness of attentional bias modification training in abstinent alcoholic patients. Drug and alcohol dependence. 2010;109:30–36. doi: 10.1016/j.drugalcdep.2009.11.022. [DOI] [PubMed] [Google Scholar]
- Shaw M, Black DW. Internet addiction: definition, assessment, epidemiology and clinical management. CNS drugs. 2008;22:353–365. doi: 10.2165/00023210-200822050-00001. [DOI] [PubMed] [Google Scholar]
- Shek DT, Tang VM, Lo CY. Evaluation of an Internet addiction treatment program for Chinese adolescents in Hong Kong. Adolescence. 2009;44:359–373. [PubMed] [Google Scholar]
- Sofuoglu M, DeVito EE, Waters AJ, Carroll KM. Cognitive enhancement as a treatment for drug addictions. Neuropharmacology. 2013;64:452–463. doi: 10.1016/j.neuropharm.2012.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spada MM. An overview of problematic Internet use. Addict Behav. 2014;39:3–6. doi: 10.1016/j.addbeh.2013.09.007. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Li TK. Drug addiction: the neurobiology of behaviour gone awry. Nature reviews Neuroscience. 2004;5:963–970. doi: 10.1038/nrn1539. [DOI] [PubMed] [Google Scholar]
- Weinstein A, Lejoyeux M. Internet Addiction or Excessive Internet Use. Am J Drug Alcohol Ab. 2010;36:277–283. doi: 10.3109/00952990.2010.491880. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Lustyk MK, Bowen S. Retraining the addicted brain: a review of hypothesized neurobiological mechanisms of mindfulness-based relapse prevention. Psychology of addictive behaviors : journal of the Society of Psychologists in Addictive Behaviors. 2013;27:351–365. doi: 10.1037/a0029258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yau YH, Crowley MJ, Mayes LC, Potenza MN. Are Internet use and video-game-playing addictive behaviors? Biological, clinical and public health implications for youths and adults. Minerva psichiatrica. 2012;53:153–170. [PMC free article] [PubMed] [Google Scholar]
- Zhou Z, Yuan G, Yao J. Cognitive biases toward Internet game-related pictures and executive deficits in individuals with an Internet game addiction. PloS one. 2012;7:e48961. doi: 10.1371/journal.pone.0048961. [DOI] [PMC free article] [PubMed] [Google Scholar]


