Abstract
As a devastating Ebola outbreak in West Africa continues, non-pharmaceutical control measures including contact tracing, quarantine, and case isolation are being implemented. In addition, public health agencies are scaling up efforts to test and deploy candidate vaccines. Given the experimental nature and limited initial supplies of vaccines, a mass vaccination campaign might not be feasible. However, ring vaccination of likely case contacts could provide an effective alternative in distributing the vaccine. To evaluate ring vaccination as a strategy for eliminating Ebola, we developed a pair approximation model of Ebola transmission, parameterized by confirmed incidence data from June 2014 to January 2015 in Liberia and Sierra Leone. Our results suggest that if a combined intervention of case isolation and ring vaccination had been initiated in the early fall of 2014, up to an additional 126 cases in Liberia and 560 cases in Sierra Leone could have been averted beyond case isolation alone. The marginal benefit of ring vaccination is predicted to be greatest in settings where there are more contacts per individual, greater clustering among individuals, when contact tracing has low efficacy or vaccination confers post-exposure protection. In such settings, ring vaccination can avert up to an additional 8% of Ebola cases. Accordingly, ring vaccination is predicted to offer a moderately beneficial supplement to ongoing non-pharmaceutical Ebola control efforts.
Author Summary
Public health efforts for controlling the 2014–2015 Ebola outbreak in West Africa have focused on contact tracing and isolation of symptomatic individuals. In addition, substantial resources have been committed to scaling up the production of experimental vaccines. Ring vaccination—the vaccination of the contacts of an infected individual—was successfully implemented to achieve smallpox eradication. Ring vaccination is particularly feasible and effective in settings where the supply of vaccines is limited and disease incidence is low. Using a disease transmission model, we evaluated the benefit of adding ring vaccination to case isolation in Liberia and Sierra Leone. We found that ring vaccination could have averted up to 126 cases in Liberia and 560 cases in Sierra Leone, thereby saving lives and intervention resources.
Introduction
The Ebola outbreak in West Africa has resulted in unprecedented morbidity and mortality. As of March 4 2015, the World Health Organization (WHO) had reported 23,914 cases and 9,792 fatalities in countries with widespread transmission [1], with Liberia and Sierra Leone having been most profoundly impacted.
Ebola transmission occurs via direct human-to-human contact with body fluids from symptomatic patients. An elevated viral load in late-stage symptomatic or deceased victims can also put family members and funeral attendees at risk of post-mortem disease transmission [2, 3]. The health ministries in Liberia and Sierra Leone have been implementing intensive contact-tracing procedures, where patients or their relatives are interviewed to identify people with whom they came into close contact after developing symptoms. Contacts who are healthy but might have been exposed are monitored for 21 days, the maximum duration of the Ebola incubation period [4]. Contacts who present with Ebola symptoms, such as fever, are transported to isolation clinics [5]. Given that Ebola is transmitted directly between close contacts, the social clustering of individuals can be fundamental to the success of intervention strategies [6–8].
Several Ebola vaccine candidates have been developed in the past decade [9, 10], some of which have already been found to be safe and immunogenic in Phase 1 clinical trials [11]. One of these, a recombinant vesicular stomatitis viruses (rVSV) vaccine, conferred protection to non-human primates when administered immediately following exposure to an otherwise lethal dose of Ebola virus [12]. An alternate vaccine formula based on the chimpanzee adenovirus type 3 (ChAd3), developed in partnership between the National Institute of Allergy and Infectious Disease and GlaxoSmithKline, together with the rVSV vaccine are currently entering Phase 2/3 clinical trials in West Africa [13]. In addition, the WHO has deemed it ethical to use experimental vaccines in the current Ebola emergency situation [14].
Even with the scale up in production [15], the supply would be insufficient for mass vaccination of affected countries, given a combined population of over twenty million people. Consequently, the judicious prioritization of vaccine recipients is essential to maximize vaccine impact. Aside from vaccinating healthcare workers who are at high occupational risk of contracting Ebola [16, 17], a vaccination strategy to reduce community-wide transmission has yet to be evaluated. Evaluating Ebola vaccination strategies is pertinent not only to the current epidemic, but also in mitigating future outbreaks.
The targeting of the exposed contacts of infected individuals, a strategy known as ring vaccination [18, 19], is efficient for controlling rare pathogens [20]. For example, ring vaccination proved to be an effective strategy for smallpox eradication [18, 19]. Furthermore, ring vaccination could be seamlessly incorporated into the contact tracing efforts underway in the affected countries.
To evaluate the effectiveness of Ebola ring vaccination in West Africa, we developed a mathematical model that approximates disease progression in a realistic contact network. We predicted that the marginal benefit was greatest in settings where there are more contacts per individual, greater clustering, or insufficient resources for effective contact tracing. However, we found that ring vaccination provides moderate marginal benefit beyond current non-pharmaceutical interventions.
Methods
Ebola transmission model
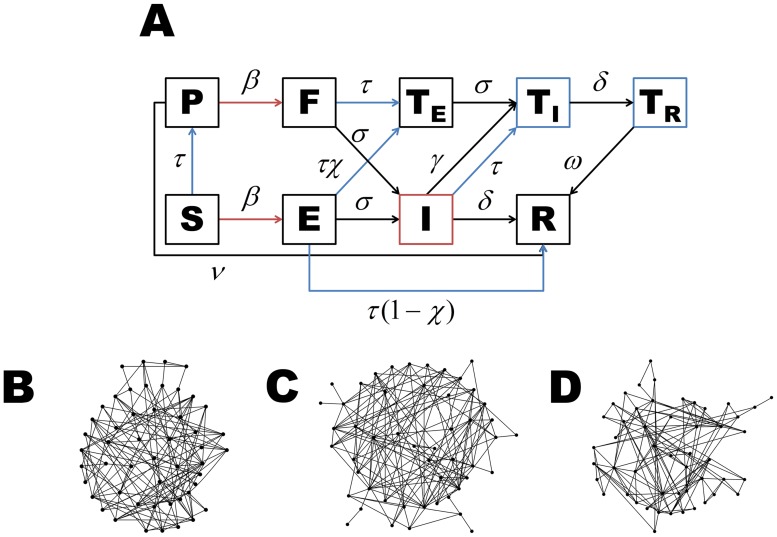
To determine the effectiveness of ring vaccination and case isolation of Ebola in West Africa, we modeled the transmission between close contacts by using the pair-approximation methodology which simulates disease propagation through a network (Fig 1, S1 Text) [6, 21]. Specifically, we tracked both the number of susceptible individuals ([S]), latently infected individuals ([E]), infectious individuals ([I]), removed individuals ([R]), as well as the number of contacts between epidemiological states. For example, [SI] denotes the number of contacts between susceptible and infectious individuals. We denoted the average number of contacts per individual in the network by k. To account for empirical mixing patterns between individuals during the Ebola outbreak in West Africa [22], we considered clustering of individuals. Clustering can be defined as the extent to which individuals who are in contact with each other share other contacts in the network and is quantified by the clustering coefficient (ϕ).
Fig 1. A) Our dynamic model is driven by the spatial correlation of individuals in the population.
New latent infections depend on the connections between susceptible and infectious individuals (red). Case isolation and ring vaccination depend on the connections between individuals in the general population (i.e. S, E, and I) and those in isolation (T I and T R) (blue). B)-D) Examples of networks with an average of 5.5 contacts per individual (approximating the 5.74 estimate from Liberia [22]) and clustering coefficients of B) 0.10, C) 0.21, and D) 0.40.
A susceptible individual becomes latently infected (E) at rate β[SI] per day, where β is the transmission rate. An individual remains in the latent period for an average duration of 1/σ days until becoming symptomatic and infectious (I). An infectious individual will transition to the removed state (R) (i.e. recovered or deceased) at rate δ, where 1/δ days is the average duration of the infectious period. In addition, we incorporated case isolation by removing a percentage of infectious individuals (ψ) from the community at rate γ per day (Table 1).
Table 1. Epidemiological parameters used in dynamic model.
| Parameter | Description (unit) | Value (SA Value) | Reference |
|---|---|---|---|
| N | Population size of Liberia | 4,092,310 | [51] |
| N | Population size of Sierra Leone | 6,348,350 | [52] |
| 1/δ | Average duration of infectious period (days) | 12 | [53–55] |
| 1/σ | Average duration of latent period (days) | 9 | [53, 56] |
| ϕ | Clustering coefficient | 0.21 (0.10 and 0.40) | [22–24] |
| k | Average number of contacts | 5.74 (10) | [22] |
| E 0 | Initial number of exposed individuals | 2 (Liberia) | |
| 14 (Sierra Leone) | [57] | ||
| 1/ω | The duration of follow up of contacts (days) | 21 | [58] |
| 1/ν | The average serial interval (days) | 15 | [53, 55] |
| 1/υ | The average time to vaccine acquired immunity (days) | 14 | [59–62] |
| 1/γ | The average number of days until infected individuals enter isolation (days) | 5 | [53, 63] |
| Ψ | The fraction of infected individuals that enter isolation | 80% | [53, 63] |
| 0.625 | [64] |
For our base case analysis, we used k = 5.74 as the mean number of contacts and ϕ = 0.21 for the clustering coefficient, derived from contact tracing data collected by the Liberian Ministry of Health and Social Welfare [22]. We also considered clustering coefficients of 0.10 and 0.40 (Table 1), consistent with previous studies on human contact networks [23–26]. In addition, we accounted for possible under-reporting of contacts by considering higher values of k (Table 1).
Contact tracing and case isolation
During contact tracing, an infected contact in the latent period moves to the observed state (T E) while a contact in the symptomatic period enters the isolated state (T I) at a daily contact tracing rate of τ per isolated case. Once an isolated individual has recovered and is no longer infectious, they transition to the T R state (S1 Text), while the individuals contacts are followed for an additional 1/ω days (Table 1). We defined the contact tracing efficacy by the probability of identifying an infected individual before transmission occurs (τ/(τ+ν)), where 1/ν is the average serial interval (Table 1). We assumed that the base case contact tracing efficacy was 40%, consistent with empirical estimates [27, 28]. We deemed the current Ebola epidemic to be eliminated at the point where incidence became lower than 0.025 cases per day, which corresponds to no new cases over a 42 day period [29].
Ring vaccination
We assumed that a proportion of the contacts of isolated cases identified through contact tracing are vaccinated. Experimental studies indicate that several vaccine candidates facilitate recovery of latent infection in non-human primates if administered within two days post-infection [12, 30]. We used a vaccine efficacy (ɛ) of 100% as our base case scenario and consider a range of vaccine efficacies from 5% to 95% (S1 Text). We investigated two scenarios: 1) vaccination must be administered pre-exposure in order to confer protection such that only susceptible individuals (S) who are uninfected can be protectively vaccinated, and 2) vaccination is efficacious with both pre- and post-exposure administration such that vaccine protection can be conferred to individuals in both the susceptible (S) and latently infected (E) [30]. The use of a post-exposure vaccine in the equations below is represented by χ = 1, otherwise χ = 0. Susceptible and latently infected individuals are vaccinated at the same daily contact tracing rate τ per isolated individual (S1 Text). When a susceptible individual is vaccinated they remain unprotected (P) until vaccine-mediated immunity is acquired 1/υ days later.
Epidemiological data and parameter estimates
To account for the recent decline in Ebola incidence [31, 32], we used a piecewise approach to calibrate our model, fitting both the early growth phase of the epidemic and the later phase of reduced transmission (S1 Fig, S1 Table, S1 Text). We estimated the rate of transmission per infectious contact (β), the date of Ebola emergence into the population (t 0), the initiation of intervention scale up (t S), and reduced transmission mediated by factors other than intervention, such as behavior change (ξ). From the date of intervention scale up, we assumed that case isolation was implemented at our base case contact tracing efficacy. Using a least squares fitting algorithm, we estimated these four parameters from weekly confirmed incidence data in Liberia and Sierra Leone, respectively (S1 Table and S1 Text). We fit the model to confirmed incidence data from June 8, 2014 to January 4, 2015 for Liberia [31] and from May 11, 2014 to January 4, 2015 for Sierra Leone [32] (S1 Table and S1 Text). However, on December 20, 2014, the deployment of international aid began in Sierra Leone and considerably reduced transmission [33–35]. Thus, we considered a second reduction in transmission from this time point (S1 Text). To validate the calibration of Liberia and Sierra Leone, we forecasted the incidence of Ebola to March 8, 2015 and calculated the correlation fit value to the observed incidence (S1 Fig, S1 Table).
Results
Base case analysis
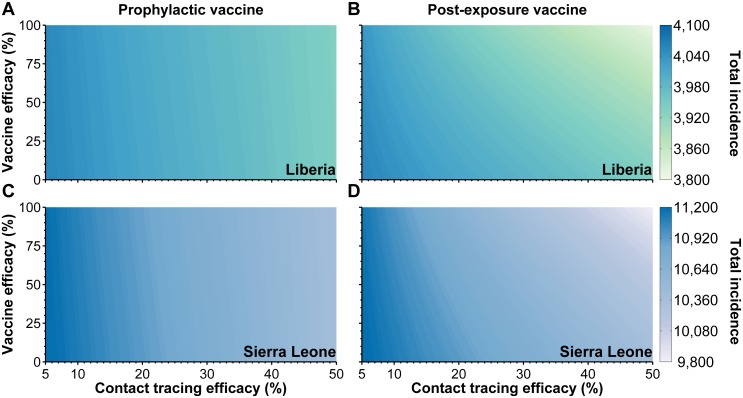
We estimated that intervention efforts were initially scaled up on September 5, 2014 in Liberia and October 8, 2014 in Sierra Leone. Our model predicts that under status quo intervention the total number of confirmed Ebola cases in Liberia will be 3,899 cases and 10,425 cases in Sierra Leone (Fig 2). If ring vaccination using a prophylactic vaccine had been combined with the initial scaling up of non-pharmaceutical interventions, four additional cases could have been averted in Liberia and 36 cases could have been averted in Sierra Leone, corresponding to relatively low marginal benefits of 0.21% and 0.48% additional cases averted, respectively (S2 Fig). By contrast, for a vaccine that can confer post-exposure protection, we estimate that 107 cases could have been averted in Liberia and 477 cases could be averted in Sierra Leone (Fig 2), corresponding to marginal benefits of 4.7% and 6.5%, respectively (S3 Fig).
Fig 2. The estimated total number of confirmed cases for various contact tracing and vaccine efficacies in (A)-B)) Liberia and (C)-D)) Sierra Leone using (A), C)) a prophylactic vaccine and (B), D)) a vaccine that confers post-exposure protection.
The model was fit using k = 5.74 with a clustering coefficient of ϕ = 0.21, as estimated for Liberia [22]. A vaccine efficacy of zero would correspond to the implementation of case isolation only.
We found that a prophylactic vaccine had minimal impact on the number of symptomatic individuals identified by contact tracing (S4 Fig). However, if the vaccine confers post-exposure protection, then ring vaccination is predicted to reduce the number of symptomatic individuals identified by contact tracing by 40 in Liberia and 137 in Sierra Leone compared to case isolation alone, thereby reducing requirements of isolation units in hospitals (S4 Fig).
Sensitivity analysis
We conducted sensitivity analysis with respect to contact tracing efficacy, average number of contacts per individuals (k), and the clustering coefficient (ϕ) (S2 Text). Varying contact tracing efficacy from 5% to 50%, the predicted epidemic size without ring vaccination ranged from 3,874 to 3,988 confirmed cases in Liberia and 10,246 to 11,048 confirmed cases in Sierra Leone (Fig 2). Implementing ring vaccination with a prophylactic vaccine is expected to achieve the greatest marginal benefit when contact tracing efficacies are between 20% and 28% in both Liberia and Sierra Leone (S2 Fig, S2 Text). Specifically, the greatest marginal benefit of ring vaccination can be up to 0.29% in Liberia and up to 0.64% in Sierra Leone, depending on the vaccine efficacy (S2 Fig). However, a vaccine with post-exposure protection is estimated to provide up to 6% marginal benefit in Liberia and 8% in Sierra Leone (S2 Text, S3 Fig). These results suggest that ring vaccination provides moderate benefit to case isolation under a range of contact tracing efficacies and vaccine efficacies.
Our sensitivity analysis of the social mixing patterns (k and ϕ) show that the marginal benefit of adding ring vaccination rises with more contacts per individual or increasing clustering (S2 and S5 Figs, S2 Text).
Discussion
We demonstrated that a combination of contact tracing, case isolation and ring vaccination could effectively reduce Ebola transmission. In Liberia, as well as in past Ebola outbreaks, implementing case isolation along with change in human behavior dramatically reduced transmission [36–39], which commonly occurs when people perceive infection risk associated with specific behaviors. Our results suggest that in this current context of reduced transmission, ring vaccination offers only moderate additional benefit, which is consistent with findings from a previous cholera model [40]. Although the incremental benefit of ring vaccination could be relatively moderate, the marginal benefit of ring vaccination is expected to increase with the average number of contacts per individual, the clustering coefficient or lower contact tracing efficacies. Therefore, ring vaccination is particularly useful in regions where contact tracing is logistically challenging. In addition, a vaccine that can confer post-exposure efficacy is much more effective for use in ring vaccination strategies than a vaccine that can only confer protection prophylactically. An additional benefit of ring vaccination that is more pronounced for a vaccine that confers post-exposure protection than for an exclusively prophylactic vaccine is the reduction in the number of symptomatic individuals who need hospitalization.
The 2014 Ebola outbreak in West Africa has affected both rural and urban communities [41], which differ in accessibility for contact tracing and hospital facilities for case isolation. There is also regional variation in the number and clustering of contacts [42]. Our analysis demonstrates that the benefit of adding ring vaccination to case isolation is influenced by the extent of clustering in a population. Specifically, we found ring vaccination provided the greatest marginal benefit to case isolation in highly clustered populations, such as crowded homes or schools [23–26, 43]. As social networks can be highly complex systems consisting of densely connected communities [44–46], future studies should evaluate not only transmission patterns within communities but also transmission patterns between rural and urban areas in order to tailor ring vaccination to specific locations.
Clinical trials are underway to evaluate Ebola vaccine candidates, but there is currently considerable uncertainty regarding the efficacy post-exposure and prophylactically. Our analysis of vaccine efficacy, ranging between 5–100%, demonstrates a diminishing marginal contribution with declining vaccine efficacy. For example, at a hypothetical efficacy of 50% ring vaccination could have averted up to 214 cases, whereas a vaccine with an efficacy of 75% up to 360 cases of Ebola could have been averted.
Our modeling approach is based on a deterministic approximation to a stochastic network model. Consequently, our model did not capture the stochastic effects that become pronounced in the eradication phase of an outbreak [6] and for ring vaccination strategies that include second-order ring vaccination, where contacts of exposed individuals are vaccinated in addition to the exposed contacts of the isolated case. We would expect an increase in the marginal benefit of ring vaccination if both first-order and second-order vaccination were implemented because vaccination would be administered ahead of the wave of transmission. Thus, our results are conservative with regard to second-order ring vaccination.
Ebola has similar family and household transmission as smallpox. During the final eradication phase of smallpox, public health authorities relied on case isolation and ring vaccination [18, 19, 47, 48]. Because smallpox is more infectious than Ebola [2, 49, 50], we conservatively expect that case isolation and ring vaccination would likewise be a practical approach to eliminate Ebola and contain future outbreaks, especially with limited vaccine supplies.
The combined implementation of ring vaccination and case isolation can be an effective approach in curtailing an Ebola outbreak. Our model predicts that ring vaccination offers moderate benefit to case isolation, with the greatest benefit occurring where there are more contacts per individual or greater clustering among individuals, and when contact tracing has low efficacy or vaccination can confer post-exposure protection.
Supporting Information
(PDF)
(PDF)
The model was fit to confirmed incidence data (black dots) from June 8, 2014 to January 4, 2015 for Liberia and May 11, 2014 to January 4, 2015 for Sierra Leone. We forecasted confirmed incidence until March 8, 2015 (red points). For each fit, we calculated the correlation fit value (R 2) for the fitted portion (black) and the forecasted portion (red) of the data.
(TIFF)
The model was fit using A), C) k = 5.74 and B), D) k = 10, with a clustering coefficient of ϕ = 0.21. A vaccine efficacy of zero would correspond to the implementation of case isolation only. The marginal benefit was calculated from the initiation of intervention scale up to the end of the epidemic.
(TIFF)
The model was fit using k = 5.74 with a clustering coefficient of ϕ = 0.21. A vaccine efficacy of zero would correspond to the implementation of case isolation only. The marginal benefit was calculated from the initiation of intervention scale up to the end of the epidemic.
(TIFF)
A vaccine efficacy of zero would correspond to the implementation of case isolation only. The model was fit using k = 5.74 and with a clustering coefficient of ϕ = 0.21.
(TIFF)
The model was fit using k = 5.74 with a clustering coefficient of A), D) ϕ = 0.10, B), E) ϕ = 0.21, and C), F) ϕ = 0.40. A vaccine efficacy of zero would correspond to the implementation of case isolation only. The marginal benefit was calculated from the initiation of intervention scale up to the end of the epidemic.
(TIFF)
The model was fit using A), C) k = 5.74 and B), D) k = 10, with a clustering coefficient of ϕ = 0.21. A vaccine efficacy of zero would correspond to the implementation of case isolation only. The marginal benefit was calculated from the initiation of intervention scale up to the end of the epidemic.
(TIFF)
The model was fit using k = 5.74 with a clustering coefficient of A), D) ϕ = 0.10, B), E) ϕ = 0.21, and C), F) ϕ = 0.40. A vaccine efficacy of zero would correspond to the implementation of case isolation only. The marginal benefit was calculated from the initiation of intervention scale up to the end of the epidemic.
(TIFF)
The model was fit using A), C) k = 5.74 and B), D) k = 10, with a clustering coefficient of ϕ = 0.21. A vaccine efficacy of zero would correspond to the implementation of case isolation only.
(TIFF)
The model was fit using A), C) k = 5.74 and B), D) k = 10, with a clustering coefficient of ϕ = 0.21. A vaccine efficacy of zero would correspond to the implementation of case isolation only.
(TIFF)
The model was fit using k = 5.74 with a clustering coefficient of A), D) ϕ = 0.10, B), E) ϕ = 0.21, and C), F) ϕ = 0.40. A vaccine efficacy of zero would correspond to the implementation of case isolation only.
(TIFF)
The model was fit using k = 5.74 with a clustering coefficient of A), D) ϕ = 0.10, B), E) ϕ = 0.21, and C), F) ϕ = 0.40. A vaccine efficacy of zero would correspond to the implementation of case isolation only.
(TIFF)
Using confirmed incidence data for Liberia and Sierra Leone, we estimated the rate of transmission per infectious contact (β), the date of Ebola emergence into the population (t 0), the initiation of intervention scale up (t S), and reduced transmission mediated by factors other than intervention (ξ) for a given average number of contacts (k) and clustering coefficient (ϕ). For each scenario we provide the basic reproductive number (R 0), the mean square error (MSE), and the correlation fit value for both the fitted portion (R 2) and the forecasted portion () of the epidemic trajectory.
(TIFF)
Data Availability
All relevant data are cited within the paper and its Supporting Information files.
Funding Statement
This work was funded by the following: APG LAM JPT: National Institutes of Health (NIH U01 GM087719, U01 GM105627). APG MLNM JPT: National Science Foundation (NSF RAPID 1514673). APG JPT: Notsew Orm Sands Foundation. FLA: National Institutes of Health (K24 DA017072). National Institutes of Health: http://grants.nih.gov/grants/guide/index.html?CFID=166949938&CFTOKEN=52322128&jsessionid=f6305bcf284b86253ec56065387171d472b7. National Science Foundation: http://www.nsf.gov/pubs/policydocs/pappguide/nsf14001/gpg_2.jsp#IID1. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.World Health Organization (2014). Ebola response roadmap situation report: October 31, 2014 URL http://apps.who.int/iris/bitstream/10665/137424/1/roadmapsitrep_31Oct2014_eng.pdf?ua=1.
- 2. Yamin D, Gertler S, Ndeffo-Mbah ML, Skrip LA, Fallah M, et al. (2015). Effect of Ebola progression on transmission and control in Liberia Ebola disease: Progression and control Annals of Internal Medicine 162:11–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ksiazek TG, Rollin PE, Williams AJ, Bressler DS, Martin ML, et al. (1999) Clinical virology of Ebola hemorrhagic fever (EHF): virus, virus antigen, and IgG and IgM antibody findings among EHF patients in Kikwit, Democratic Republic of the Congo, 1995. The Journal of infectious diseases 179 Suppl: S177–87. 10.1086/514321 [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization (2014). WHO—Case definition recommendations for Ebola or Marburg Virus Diseases. URL http://www.who.int/csr/resources/publications/ebola/ebola-case-definition-contact-en.pdf?ua=1.
- 5.Dahn B. Republic of Liberia Ministry of Health and Social Welfare Press Release June 24, 2014. http://mohsw.gov.lr/documents/press%20release%20June%2024,2014.pdf.
- 6. House T, Keeling MJ (2010) The impact of contact tracing in clustered populations. PLoS computational biology 6: e1000721 10.1371/journal.pcbi.1000721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Keeling MJ (1999) The effects of local spatial structure on epidemiological invasions. Proceedings Biological sciences / The Royal Society 266: 859–67. 10.1098/rspb.1999.0716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Smieszek T, Fiebig L, Scholz RW (2009) Models of epidemics: when contact repetition and clustering should be included. Theoretical biology & medical modelling 6: 11 10.1186/1742-4682-6-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hoenen T, Groseth A, Feldmann H (2012) Current Ebola vaccines. Expert opinion on biological therapy 12: 859–72. 10.1517/14712598.2012.685152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Galvani AP, Ndeffo-Mbah ML, Wenzel N, Childs JE (2014) Ebola Vaccination: If Not Now, When? Annals of Internal Medicine: 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Martin JE, Sullivan NJ, Enama ME, Gordon IJ, Roederer M, et al. (2006) A DNA vaccine for Ebola virus is safe and immunogenic in a phase I clinical trial. Clinical and vaccine immunology: CVI 13: 1267–77. 10.1128/CVI.00162-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Feldmann H, Jones SM, Daddario-DiCaprio KM, Geisbert JB, Ströher U, et al. (2007) Effective post-exposure treatment of Ebola infection. PLoS pathogens 3: e2 10.1371/journal.ppat.0030002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Institute of Allergy and Infectious Diseases (2015). Questions and Answers: PREVAIL Phase 2/3 Clinical Trial of Investigational Ebola Vaccines. URL http://www.niaid.nih.gov/news/QA/Pages/EbolaVaxResultsQA.aspx.
- 14.World Health Organization (2014). Statement on the WHO consultation on potential Ebola therapies and vaccines. URL http://www.who.int/mediacentre/news/statements/2014/ebola-therapies-consultation/en/.
- 15. Cohen J, Kupferschmidt K (2014) Infectious Diseases. Ebola vaccine trials raise ethical issues. Science (New York, NY) 346: 289–90. 10.1126/science.346.6207.289 [DOI] [PubMed] [Google Scholar]
- 16. Fischer Wa, Hynes Na, Perl TM (2014) Protecting Health Care Workers From Ebola: Personal Protective Equipment Is Critical but Is Not Enough. Annals of Internal Medicine 161: 753 10.7326/M14-1953 [DOI] [PubMed] [Google Scholar]
- 17. Matanock A, Arwady A, Ayscue P, Forrester J, Gaddis B, et al. (2014) Ebola Virus Disease Cases Among Health Care Workers Not Working in Ebola Treatment Units Liberia, JuneAugust, 2014. CDC Morbidity and Mortality Weekly Report 63: 1077–1081. [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control (2004). What CDC is doing to protect the public from smallpox. URL http://www.bt.cdc.gov/agent/smallpox/prep/cdc-prep.asp.
- 19. Geddes AM (2006) The history of smallpox. Clinics in dermatology 24: 152–7. 10.1016/j.clindermatol.2005.11.009 [DOI] [PubMed] [Google Scholar]
- 20. Foege WH, Millar JD, Lane JM (1971) Selective epidemiologic control in smallpox eradication. American journal of epidemiology 94: 311–5. [DOI] [PubMed] [Google Scholar]
- 21. Rand D (1999) Correlation equations and pair approximations for spatial ecologies. Advanced ecological theory: principles and applications 100 10.1002/9781444311501.ch4 [DOI] [Google Scholar]
- 22.Scarpino SV, Iamarino A, Wells C, Yamin D, Ndeffo-Mbah M, et al. (2014) Epidemiological and Viral Genomic Sequence Analysis of the 2014 Ebola Outbreak Reveals Clustered Transmission. Clinical Infectious Diseases. [DOI] [PMC free article] [PubMed]
- 23. Barclay VC, Smieszek T, He J, Cao G, Rainey JJ, et al. (2014) Positive network assortativity of influenza vaccination at a high school: Implications for outbreak risk and herd immunity. PLoS ONE 9 10.1371/journal.pone.0087042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Salathé M, Kazandjieva M, Lee JW, Levis P, Feldman MW, et al. (2010) A high-resolution human contact network for infectious disease transmission. Proceedings of the National Academy of Sciences of the United States of America 107: 22020–22025. [DOI] [PMC free article] [PubMed]
- 25. Leventhal GE, Hill AL, Nowak Ma, Bonhoeffer S (2015) Evolution and emergence of infectious diseases in theoretical and real-world networks. Nature Communications 2: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Curtis DE, Hlady CS, Kanade G, Pemmaraju SV, Polgreen PM, et al. (2013) Healthcare worker contact networks and the prevention of hospital-acquired infections. PLoS ONE 8(12): e79906 10.1371/journal.pone.0079906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Meltzer M, Atkins C, Santibanez S, Knust B, Peterson B, et al. (2014) Estimating the Future Number of Cases in the Ebola Epidemic Liberia and Sierra Leone, 2014–2015. Technical Report 3, Centers for Disease Control and Prevention. URL http://www.cdc.gov/mmwr/preview/mmwrhtml/su6303a1.htm.
- 28. Dhillon RS, Srikrishna D, Sachs J (2014) Controlling Ebola: next steps. Lancet 384: 1409–1411. 10.1016/S0140-6736(14)61696-2 [DOI] [PubMed] [Google Scholar]
- 29.World Health Organization (2014). Are the Ebola outbreaks in Nigeria and Senegal over? URL http://www.who.int/mediacentre/news/ebola/14-october-2014/en/.
- 30. Qiu X, Wong G, Fernando L, Audet J, Bello A, et al. (2013) mAbs and ad-vectored IFN-α therapy rescue Ebola-infected nonhuman primates when administered after the detection of viremia and symptoms. Science translational medicine 5: 207ra143–207ra143. 10.1126/scitranslmed.3006605 [DOI] [PubMed] [Google Scholar]
- 31.World Health Organization (2014). Ebola data and statistics: Liberia. URL http://apps.who.int/gho/data/node.ebola-sitrep.ebola-country-LBR?lang=en.
- 32.World Health Organization (2014). Ebola data and statistics: Sierra Leone. URL http://apps.who.int/gho/data/node.ebola-sitrep.ebola-country-SLE?lang=en.
- 33.Emma Farge UF (2014). Ebola end game in sight as new cases fall sharply in Sierra Leone. URL http://www.reuters.com/article/2015/01/21/health-ebola-leone-idUSL6N0UT2Z120150121.
- 34.Government of Canada (2014). Operation SIRONA Task Force commences operations in fighting Ebola outbreak—Canadian Armed Forces personnel working with British forces in Sierra Leone. URL http://news.gc.ca/web/article-en.do?nid=917269.
- 35.National Defence and the Canadian Armed Forces (2014). Operation SIRONA. URL http://www.forces.gc.ca/en/operations-abroad/op-sirona.page.
- 36. Chowell G, Hengartner N, Castillo-Chavez C, Fenimore P, Hyman J (2004) The basic reproductive number of Ebola and the effects of public health measures: the cases of Congo and Uganda. Journal of Theoretical Biology 229: 119–126. 10.1016/j.jtbi.2004.03.006 [DOI] [PubMed] [Google Scholar]
- 37.Freeman C (2014). Ebola outbreak: fight against disease hampered by belief in witchcraft, warns British doctor. The Telegraph. URL http://www.telegraph.co.uk/news/worldnews/africaandindianocean/sierraleone/11001610/Ebola-outbreak-fight-against-disease-hampered-by-belief-in-witchcraft-warns-British-doctor.html.
- 38.Unicef (2014). Liberia Ebola Situation Report. URL http://www.unicef.org/appeals/files/UNICEF-Liberia_Sitrep_51_Ebola_Outbreak_12_September_2014.pdf.
- 39. Funk S, Salathé M, Jansen VAA (2010) Modelling the influence of human behaviour on the spread of infectious diseases: a review. Journal of the Royal Society, Interface / the Royal Society 7: 1247–56. 10.1098/rsif.2010.0142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chao DL, Halloran ME, Longini IM (2011) Vaccination strategies for epidemic cholera in Haiti with implications for the developing world. Proceedings of the National Academy of Sciences 108: 7081–7085. [DOI] [PMC free article] [PubMed]
- 41.World Health Organization:Regional office for Africa. Ebola virus disease, West Africa update 3 July 2014.
- 42. Kerry SM, Emmett L, Micah FB, Martin-Peprah R, Antwi S, et al. (2005) Rural and semi-urban differences in salt intake, and its dietary sources, in Ashanti, West Africa. Ethnicity & disease 15: 33–9. [PubMed] [Google Scholar]
- 43. Volz EM, Miller JC, Galvani A, Meyers L (2011) Effects of heterogeneous and clustered contact patterns on infectious disease dynamics. PLoS Computational Biology 7 10.1371/journal.pcbi.1002042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Newman M, Park J (2003) Why social networks are different from other types of networks. Physical Review E 68: 036122 10.1103/PhysRevE.68.036122 [DOI] [PubMed] [Google Scholar]
- 45. Gfeller D, Chappelier JC, De Los Rios P (2005) Finding instabilities in the community structure of complex networks. Physical Review E 72: 056135 10.1103/PhysRevE.72.056135 [DOI] [PubMed] [Google Scholar]
- 46.Girvan M, Newman MEJ (2002) Community structure in social and biological networks. Proceedings of the National Academy of Sciences of the United States of America 99: 7821–6. [DOI] [PMC free article] [PubMed]
- 47. Fraser SM (1980) Leicester and smallpox: the Leicester method. Medical history 24: 315–332. 10.1017/S0025727300040345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Strassburg MA (1982) The global eradication of smallpox. American journal of infection control 10: 53–59. 10.1016/0196-6553(82)90003-7 [DOI] [PubMed] [Google Scholar]
- 49. Eichner M (2003) Transmission Potential of Smallpox: Estimates Based on Detailed Data from an Outbreak. American Journal of Epidemiology 158: 110–117. 10.1093/aje/kwg103 [DOI] [PubMed] [Google Scholar]
- 50. Pandey A, Atkins KE, Medlock J, Wenzel N, Townsend JP, et al. (2014) Strategies for containing Ebola in West Africa. Science: 1260612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Central Intelligence Agency (2014). The World fact book: Liberia. URL https://www.cia.gov/library/publications/the-world-factbook/geos/li.html.
- 52.The Republic of Sierra Leone Ministry of Health and Sanitation (2014). Ebola Situation Report. URL http://health.gov.sl/?page_id=583.
- 53. Team WER (2014) Ebola virus disease in West Africa-the first 9 months of the epidemic and forward projections. N Engl J Med 371: 1481–95. 10.1056/NEJMoa1411100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Chertow DS, Kleine C, Edwards JK, Scaini R, Giuliani R, et al. (2014) Ebola virus disease in West Africa-clinical manifestations and management. The New England journal of medicine 371: 2054–7. 10.1056/NEJMp1413084 [DOI] [PubMed] [Google Scholar]
- 55. Chowell G, Nishiura H (2014) Transmission dynamics and control of Ebola virus disease (EVD): a review. BMC Medicine 12: 1–16. 10.1186/s12916-014-0196-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Baize S, Leroy EM, Georges AJ, Georges-Courbot MC, Capron M, et al. (2002) Inflammatory responses in Ebola virus-infected patients. Clinical & Experimental Immunology 128: 163–168. 10.1046/j.1365-2249.2002.01800.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Gire SK, Goba A, Andersen KG, Sealfon RSG, Park DJ, et al. (2014) Genomic surveillance elucidates Ebola virus origin and transmission during the 2014 outbreak. Science 1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Centers for Disease Control (2004). Contact Tracing: Contact tracing can stop Ebola in its tracks. URL http://www.cdc.gov/vhf/ebola/outbreaks/what-is-contact-tracing.html.
- 59. Jones SM, Feldmann H, Ströher U, Geisbert JB, Fernando L, et al. (2005) Live attenuated recombinant vaccine protects nonhuman primates against Ebola and Marburg viruses. Nature medicine 11: 786–790. 10.1038/nm1258 [DOI] [PubMed] [Google Scholar]
- 60. Qiu X, Fernando L, Alimonti JB, Melito PL, Feldmann F, et al. (2009) Mucosal immunization of cynomolgus macaques with the vsvδzebovgp vaccine stimulates strong Ebola gp-specific immune responses. PloS one 4: e5547 10.1371/journal.pone.0005547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Geisbert TW, Daddario-DiCaprio KM, Geisbert JB, Reed DS, Feldmann F, et al. (2008) Vesicular stomatitis virus-based vaccines protect nonhuman primates against aerosol challenge with Ebola and Marburg viruses. Vaccine 26: 6894–6900. 10.1016/j.vaccine.2008.09.082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Geisbert TW, Geisbert JB, Leung A, Daddario-DiCaprio KM, Hensley LE, et al. (2009) Single-injection vaccine protects nonhuman primates against infection with Marburg virus and three species of Ebola virus. Journal of virology 83: 7296–7304. 10.1128/JVI.00561-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Khan AS, Tshioko FK, Heymann DL, Le Guenno B, Nabeth P, et al. (1999) The reemergence of Ebola hemorrhagic fever, Democratic Republic of the Congo, 1995. Commission de Lutte contre les Epidémies 00E0 Kikwit. The Journal of infectious diseases 179 Suppl 1: S76–S86. 10.1086/514306 [DOI] [PubMed] [Google Scholar]
- 64. Legrand J, Grais RF, Boelle PY, Valleron AJ, Flahault A (2007) Understanding the dynamics of Ebola epidemics. Epidemiology and infection 135: 610–21. 10.1017/S0950268806007217 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
The model was fit to confirmed incidence data (black dots) from June 8, 2014 to January 4, 2015 for Liberia and May 11, 2014 to January 4, 2015 for Sierra Leone. We forecasted confirmed incidence until March 8, 2015 (red points). For each fit, we calculated the correlation fit value (R 2) for the fitted portion (black) and the forecasted portion (red) of the data.
(TIFF)
The model was fit using A), C) k = 5.74 and B), D) k = 10, with a clustering coefficient of ϕ = 0.21. A vaccine efficacy of zero would correspond to the implementation of case isolation only. The marginal benefit was calculated from the initiation of intervention scale up to the end of the epidemic.
(TIFF)
The model was fit using k = 5.74 with a clustering coefficient of ϕ = 0.21. A vaccine efficacy of zero would correspond to the implementation of case isolation only. The marginal benefit was calculated from the initiation of intervention scale up to the end of the epidemic.
(TIFF)
A vaccine efficacy of zero would correspond to the implementation of case isolation only. The model was fit using k = 5.74 and with a clustering coefficient of ϕ = 0.21.
(TIFF)
The model was fit using k = 5.74 with a clustering coefficient of A), D) ϕ = 0.10, B), E) ϕ = 0.21, and C), F) ϕ = 0.40. A vaccine efficacy of zero would correspond to the implementation of case isolation only. The marginal benefit was calculated from the initiation of intervention scale up to the end of the epidemic.
(TIFF)
The model was fit using A), C) k = 5.74 and B), D) k = 10, with a clustering coefficient of ϕ = 0.21. A vaccine efficacy of zero would correspond to the implementation of case isolation only. The marginal benefit was calculated from the initiation of intervention scale up to the end of the epidemic.
(TIFF)
The model was fit using k = 5.74 with a clustering coefficient of A), D) ϕ = 0.10, B), E) ϕ = 0.21, and C), F) ϕ = 0.40. A vaccine efficacy of zero would correspond to the implementation of case isolation only. The marginal benefit was calculated from the initiation of intervention scale up to the end of the epidemic.
(TIFF)
The model was fit using A), C) k = 5.74 and B), D) k = 10, with a clustering coefficient of ϕ = 0.21. A vaccine efficacy of zero would correspond to the implementation of case isolation only.
(TIFF)
The model was fit using A), C) k = 5.74 and B), D) k = 10, with a clustering coefficient of ϕ = 0.21. A vaccine efficacy of zero would correspond to the implementation of case isolation only.
(TIFF)
The model was fit using k = 5.74 with a clustering coefficient of A), D) ϕ = 0.10, B), E) ϕ = 0.21, and C), F) ϕ = 0.40. A vaccine efficacy of zero would correspond to the implementation of case isolation only.
(TIFF)
The model was fit using k = 5.74 with a clustering coefficient of A), D) ϕ = 0.10, B), E) ϕ = 0.21, and C), F) ϕ = 0.40. A vaccine efficacy of zero would correspond to the implementation of case isolation only.
(TIFF)
Using confirmed incidence data for Liberia and Sierra Leone, we estimated the rate of transmission per infectious contact (β), the date of Ebola emergence into the population (t 0), the initiation of intervention scale up (t S), and reduced transmission mediated by factors other than intervention (ξ) for a given average number of contacts (k) and clustering coefficient (ϕ). For each scenario we provide the basic reproductive number (R 0), the mean square error (MSE), and the correlation fit value for both the fitted portion (R 2) and the forecasted portion () of the epidemic trajectory.
(TIFF)
Data Availability Statement
All relevant data are cited within the paper and its Supporting Information files.