Abstract
Background
North Darfur State has been affected by conflict since 2003 and the government has not been able to provide adequate curative health services to the people. The government has come to rely on Non-Governmental Organizations (NGOs) to provide curative health services. This study was conducted to examine the existing collaboration between government and NGOs in curative health service delivery in North Darfur State, and to identify the challenges that affect their collaboration.
Methods
Documentary data were collected from government offices and medical organizations. Primary data were obtained through interviews with government and NGOs representatives. The interviews were conducted with (1) expatriates working for international NGOs (N=15) and (2), health professionals and administrators working in the health sector (N= 45).
Results
The collaboration between the government and NGOs has been very weak because of security issues and lack of trust. The NGOs collaborate by providing human and financial resources, material and equipment, and communication facilities. The NGOs supply 70% of curative health services, and contribute 52.9% of the health budget in North Darfur State. The NGOs have employed 1 390 health personnel, established 44 health centres and manage and support 83 health facilities across the State.
Conclusion
The NGOs have played a positive role in collaborating with the government in North Darfur State in delivering curative health services, while government’s role has been negative. The problem that faces the government in future is how health facilities will be run should a peaceful settlement be reached and NGOs leave the region.
Keywords: Government, NGOs, Collaboration, Curative health, North Darfur State, Sudan
Introduction
North Darfur State is located in western Sudan and is divided into 15 districts and inhabited by 2 260 262 people, according to information gathered from the census of 2008 (1). North Darfur State is considered to be one of the weakest states in Sudan due to its lack of human, financial and natural resources. Since 2003 when conflict between the government and rebels groups started in the State, a shortage of both government and private sector health facilities has come about to serve the people who have been affected by conflict. The number of people thus affected is estimated to be about 1.5 million, or 75% of the total population, which includes approximately 500 000 Internally Displaced Persons (IDPs) (2). These people are living in camps in the vicinity of large towns such as El Fasher, the capital of North Darfur State. They live in poor conditions, suffer ing outbreaks of disease, with malaria and diarrhea a constant threat (3).
The federal and state governments are responsible for providing basic health services. The State Ministry of Health runs an extensive network of hospitals, rural hospitals, clinics and dispensaries, but the services suffer from shortages of human and financial resources and equipment to deliver curative health services. Furthermore, people face difficulties in accessing health services, especially in rural and conflict-affected areas. The State Ministry of Health needs assistance from NGOs and other stakeholders to become involved in financing and delivering curative health services. This situation has led international Non-Governmental Organizations (NGOs) to intervene and take responsibility for providing most of the curative health services in North Darfur State (4).
Currently, 22 international NGOs have been involved, led by WHO and UNICEF, as well as three local NGOs are collaborating with the government in providing curative health services to the poor and conflict-affected people in North Darfur State (5). These organisations concentrate their efforts on urban areas because of their lack of capacity. NGOs have provided 70% of all curative health services to the poor and conflict-affected people in North Darfur State (6).
The range of activities carried out by NGOs extends from providing hospitals, clinics and primary health care centers, to providing free consultation and drugs. NGOs contribute to curative health service delivery by providing human and financial resources, materials and equipment, sharing information, developing joint projects with government, and developing national health policy, as well as creating joint committees with government.
This article analyses all these forms of collaboration between the government and NGOs in delivering curative health services in North Darfur State and identifies the challenges that affect this collaboration. But in order to do so the way in which such collaboration is organized should first be explained.
Methods
Both quantitative and qualitative research methods were used to address the specific objectives of this study, which were to:
Examine the existing collaboration between government and NGOs in curative health service delivery;
Identify the challenges that affect their collaboration.
Documentary data were collected from a review of government and NGOs reports and other published or unpublished reports in Sudan and North Darfur State. Primary qualitative data were obtained through consultative meetings and interviews with government and NGOs representatives. The research methods included observation, recordings and open-ended interviews. To collect the experts’ opinions about the difficulties that faced the collaboration between the government and NGOs sectors and their impact on curative health service delivery, semi-structured questionnaires and guidelines were used for interviews. From November 2010 until January 2011 the author conducted numerous formal and informal interviews with (1) expatriates working for international NGOs (N=15) and (2) health professionals and administrators working in health sector in the state and district level (N=45). All the government officials’ interviews were conducted in Arabic and transcribed into English, sorted and arranged, coded into categories and analyzed using content analysis.
Results
The structure of collaboration and co-ordination between the government and NGOs in managing and implementing health systems and policy in North Darfur State
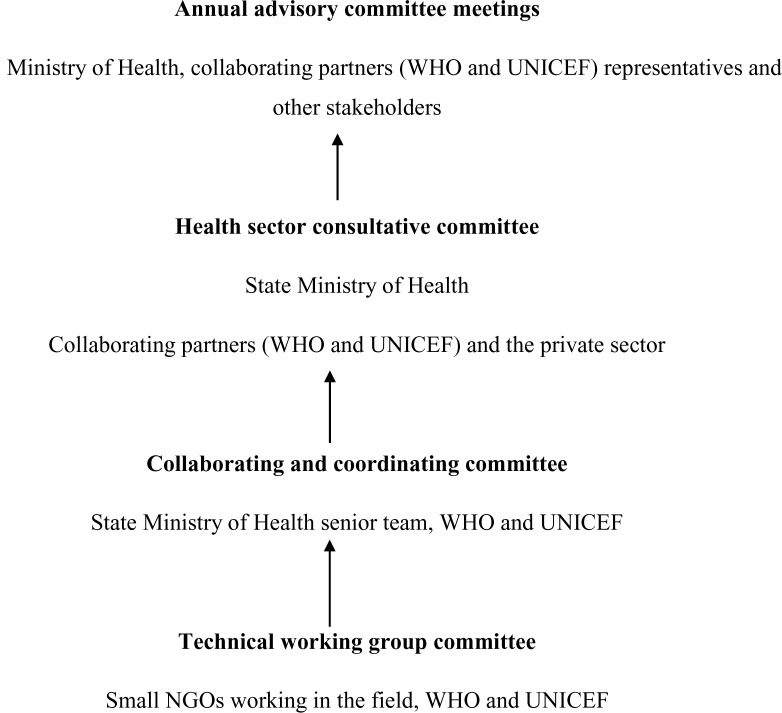
Responding to complex health problems and strengthening the health system in Sudan and in North Darfur State requires rapid and effective collaboration and co-ordination as well as communication between all actors: the Federal Ministry of Health, the State Ministry of Health, the district authorities, and NGOs. A key component of the collaborative effort is the availability of accurate and up-to-date information to plan timely and effective responses to urgent health situations. At State level, WHO and UNICEF, with the support of donors, play a leading role in collaboration between the government sector and other NGOs working in health services. They accomplish this by collecting accurate and timely information about the situation of health service delivery in the State from the smaller NGOs working in the field. Co-ordination and information sharing operate at both central and state level, as well as between the NGOs themselves, as shown in Fig. 1 below.
Fig. 1.
Overview of co-ordination structure between government and NGOs in North Darfur State. Source: Fieldwork Data, December, 2010.
As can be seen, there are three levels of committee at federal and State level to manage and implement health systems and policy in North Darfur State. At national level, health partners share progress on ongoing activities in North Darfur State so as to ensure co-ordinated donor interventions, to make strategic policy decisions, and to agree on guidelines and advocacy strategies. These issues are discussed in the annual advisory committee meetings held in Khartoum at the end of every year. The annual advisory committee meetings evaluate work processes for the previous year and review action plans and support for the following year.
At State level, the health sector consultative committee reviews the performance indicators on the ground and assesses the financial situation. This committee is directed by the General Director of the State Ministry of Health and includes private sector representatives. The State Ministry coordinates between the Health Ministry and NGOs representatives, particularly those from WHO and UNICEF. Monthly meetings discuss the major challenges that face NGO activities, such as shortages in funding, outbreaks of epidemics among IDPs and security issues. The committee attempts to resolve such issues, but if not, they are transferred to the federal level.
NGOs, the State Ministry of Health and other partners from the collaboration and coordination committee carry out regular and comprehensive assessments of health facilities, and encourage all partners to work in harmony to provide health services to the conflict-affected and poor people. There is collaboration between the State Ministry of Health and humanitarian aid commissions which are responsible for international NGOs’ movements. This responsibility is enacted in conjunction with security authorities who are mandated to make statements on behalf of NGOs working in the health field. This committee meets weekly to keep partners informed on activities and progress, to provide a forum for joint operational decision-making, and to enhance the local ownership of programmes.
In the NGO sector, WHO and UNICEF hold a weekly technical working group committee, meeting every Wednesday with all the other NGOs working in the health field in order to discuss obstacles that they encounter in delivering quality health services. Collaboration among NGOs to address all determinants of poor health is an increasingly important role for WHO and UNICEF since they co-ordinate the activities of all the other NGOs. In these meetings, mortality and morbidity reports, fact sheets, guidelines for best practice and technical documents are discussed in order to ensure their dissemination to stakeholders. The issues addressed in these documents are discussed with the State Ministry of Health in an effort to bring about harmony between the government, international agencies like the United Nations and NGOs in developing strategies and work-plans for the health sector. In addition, these meetings address particular problems that arise in assisting the poor in remote areas, especially those affected by conflict. A central concern is to avoid any needless duplication of effort.
Forms of collaboration between the State Ministry of Health and NGOs in providing curative health services in North Darfur State
How effective has collaboration been in North Darfur State between government and the NGOs? The interviewees were asked about human and financial resources, material and equipment, communication and exchange information, as well as experiences in developing joint projects and policy.
Providing human resources
The health personnel include those working in the health facilities as well as community staff working in the same catchment area as the health facilities (rural areas and camps). According to a World Health Organization Report (5), in North Darfur State the number of health workers managed by NGOs is 1 390, which outnumbers those employed by State Ministry of Health (1 164). NGOs also provide training courses for health staff in the public sector, especially for doctors, nurses and midwifes. According to the State Ministry of Health Survey Report (6), since 2003 NGOs have provided technical assistance to hospitals, rural hospitals and health clinics in the State. As a result, more than 50 nurses have been trained to provide care and treatment; more than 23 doctors have been trained to operate laboratory equipment; and approximately six senior doctors and hospital directors have received management training.
In this regard, 43 out of 49 (94%) interviewees stated that international NGOs provide qualified health staff for curative health services delivery in North Darfur State. According to an interviewee (1-1, 18 January 2011, El Fasher1) working in Kutum rural hospital:
Without the NGO health staff who are well qualified and trained, the government cannot deliver curative health services to the poor and conflict affected- people in the State. The government health institutions, whether rural hospitals, health centres or basic health units in Kutum district are facing a lack of human resources. NGO health staff helps us to train local health staff to deliver curative health services to the district populations.
Providing financial resources
International NGOs have been supporting the State Ministry of Health with financial resources for delivering curative health service to the poor and conflict-affected people in North Darfur State. External financial support from NGOs for health care in North Darfur State is substantial, and it has become increased from 30.6% of total spending on health in 2003 to 31.3% in 2006, and increased even more to 52.9% in 2009 (7, 8). The State is therefore greatly depends on the NGOs support.
This statistical portrait of sources of financing on health was confirmed by 47 out of 49 (96%) interviewees. One interviewee (2-1, 15 January 2011, El Fasher) in the finance division in the State Ministry of Health commented that:
The State Ministry of Health faces big challenges to finance health services in the State. Most people are not able to access private health services by paying. The public sector does not able to provide free health services because of financial problems. Therefore, the State Ministry of Health is depending completely on donors and international NGOs to support.
Providing materials and equipment
Interviewees pointed out that the materials and equipment provided by NGOs include generators, some kinds of laboratory equipment, some medical machines, beds for patients, and contributions towards maintenance of health institutions. In addition, all health centres which have been established and managed by NGOs are provided with substantial materials and equipment, whether in rural areas or in IDP camps. Overall, 63% of all the interviewees and 92% of those in NGOs indicated that NGOs provide materials and equipment to government health institutions to assist with curative health services. This is confirmed indirectly by the State Ministry of Health Survey Report (6), which noted that the capacity of the State Ministry of Health to provide health materials and equipment is limited.
According to an interviewee (1-2, 28 January 2011, El Fasher) in a teaching hospital in El Fasher:
The hospital, which serves all people in the State, faces an extreme lack of modern health service appliances and equipment. 90% of health appliances and equipment in the hospital are old and some are not available. The other 10% of modern equipment is provided by NGOs. Therefore patients have their tests done outside the hospital in private laboratories. NGOs make a good effort in providing materials and equipment to health facilities in the public sector but what they provide is still little and does not cover all health facilities in the public sector. Due to the lack of modern materials and equipment in public health facilities and the expensive treatment in the private sector, the majority of patients seek health care from traditional healers.
Communication and information exchange
In terms of communication and information exchange between government and NGOs, there is a noticeably mixed response to this issue. Those in government, especially at district level (85%), believe that government does not have the capacity to communicate, whereas 80% of those in higher levels of government sector and 87% of those in the NGOs express confidence in the ability of NGOs to exchange information, and to communicate more generally. According to an interviewee (1-3, 11 January 2011, El Fasher) working in the State Ministry of Health as a coordinator with NGOs:
NGOs have shown a good capacity in providing health information, in communicating with IDPs, the poor and conflict-affected people in the State. They are also very responsible in attending the collaboration meetings between the small NGOs as well as the collaboration meetings between the representatives of NGOs, such as WHO and UNCIEF and the State Ministry of Health. In their meetings they discuss issues regarding controlling the spread of diseases and the funding-gap situation and how they can collaborate to co-manage. However, the State Ministry of Health faces a lack of capacity in terms of human and financial resources on one side and insecurity issues on the other. Therefore it depends completely on information provided by NGOs which focus on controlling the spread of diseases.
According to an interviewee (1- 4, 21 January 2011, El Fasher) who is with Medicines Sans Frontiers — Spain:
NGOs have a great ability to establish reports with target populations because many of them have years of experience in working with people in their communities. They are trusted by those populations and people listen to them and accept their offers. NGOs are very co-operative and helpful. The State Ministry of Health is ineffectual in reaching some rural areas, in particular, areas which have been controlled by rebel groups. They are also not trusted by the people living there. Therefore the collaboration between the State Ministry of Health and NGOs is still weak.
Developing joint projects
In terms of developing joint projects and policy between two partners, 88% of the interviewees at all levels, 90% of the interviewees at district level and all of the interviewees in the NGO sector, indicated that there is collaboration between the government and NGOs in establishing and developing joint health projects, especially relating to rural hospitals and health centers. NGOs have established 24 health centres in IDP camps, and 20 health centres across all the districts in North Darfur State; this has happened in co-operation with the community and the Ministry of Health (6) where 89 health facilities across the State have been supported and managed (5). In joint projects such as establishing health centers, the State Ministry of Health contributes by consulting on and determining the location of a health center. The community contributes by providing a monitoring function and safeguards the funds for the health center, both during implementation and after completion. In this regard, NGOs considered the involvement of the State Ministry of Health and the community to be important indicators of the likelihood of a project being completed successfully because consultants from the State are able to affect the implementation process and the involvement of the community is considered some guarantee of the sustainability of a health project.
In situations of collaboration between the State Ministry of Health and NGOs an interviewee (2-2, 15 January 2011, El Fasher) with the Medicine Sans Frontieres- Belgium said:
The structure of organizations in the government negatively impacts collaboration projects in the implementation of health projects; bureaucracy on the side of the State Ministry of Health hinders successful collaboration with NGOs. The State Ministry of Health has to receive orders from higher levels such as the Federal Ministry of Health and security authorities to allow them to undertake health projects. This takes a long time, while the NGOs are more flexible in taking their decisions. Therefore NGOs feel that collaborating with the State Ministry of Health is an obstacle rather than a help to them in implementing health projects.
According to an interviewee (1- 5, 12 January 2011, El Fasher) working in the World Health Organization sub-office in El Fasher:
The donors do not trust the government to implement health projects. Donors are more likely to give money to the NGOs rather than government, but government requires donors to support them directly to implement health projects. Therefore, the State authorities see that the NGOs take over their area of influence in the health sector. NGOs are more likely to approach the State Ministry of Health with partnerships in health projects rather than to fund the State Ministry of Health to do so. This reality negatively affects the collaboration between them. Involving the State at the stage of discussion makes the State more willing to participate in the implementation of the project. This means that the proposal for the project will include State Ministry of Health views and receive their immediate acceptance for future collaboration.
The success of joint projects seems to depend on building trust. Where local communities are able to participate in making decisions, or at least are consulted. NGOs have succeeded with health projects. But where collaboration with government is made difficult, for example, by a turnover in staffing, NGOs have to be sensitive to protocol and to maintain relations with government institutions.
Developing national health policy
The issues raised here reveal that government health authorities and the NGOs experience some difficulties in working together, partly due to problems of communication and trust. Do NGOs play a role in developing national health policy in collaboration with the Ministry of Health in North Darfur State? Those in NGOs largely thought (69%) that they did not contribute to national health policy, as did 70% of interviewees in government at district level. Those in State government had mixed views, 44% indicated yes, and 56% no. The issues raised here reveal that government health authorities and the NGOs experience some difficulties in collaborating, partly due to problems of communication and trust.
Interviewees noted that NGOs deliver curative health services in accordance with their own policies, not in terms of government policy. This is confirmed by an interviewee (2-3, 17 January 2011, El Fasher) in the State Ministry of Health:
When the national health policy was adopted in 2007, there were many NGOs working in the State but they were not given the opportunity to participate in health policy formulation nor to develop legal frameworks. Therefore, NGOs are now implementing their own policies, due to restrictions by donors who support them financially. Thus the State Ministry of Health and NGOs’ collaboration in terms of health policy implementation has not yet been developed.
NGOs view their involvement in health systems and policy from a socioeconomic development perspective. Therefore NGOs want to be part of the health system and to participate in policy design, not only as implementers. However, the government regards NGOs as global players and any criticism of health systems and policy by them is treated as a move to destabilize the government. NGOs wish to contribute to formulating health policy, so as to avoid government regulation of NGOs which would curtail their freedom and prevent them from carrying out their activities as they prefer.
From these comments it is apparent that NGOs see themselves mainly concerned with practical programs and projects in the health sector, whereas policy matters are viewed as government’s responsibility even if it calls on the assistance of international agencies from time to time.
Discussion
Challenges affecting collaboration between government and NGOs to deliver curative health services in North Darfur State
According to the Health and Fragile States Network Report (9), the provision of health services in areas best by conflict requires good relations and co-ordination between health stakeholders in order to overcome significant infrastructural and human resources constraints. Moreover, to have the opportunity to start a new health system based experience from similar contexts. According to interviewees in government and in the NGO sector, several challenges have affected their efforts to deliver curative health services and to manage the health system successfully. There were two particular challenges: the ability of NGOs to gain access to the conflict- affected areas; and challenges relating to experience and capacity.
The challenges of NGOs gaining access to the conflict- affected areas
The NGOs have faced difficulties to access conflict affected areas in order to deliver curative health services to the poor and conflict-affected people. This is not only because of security issues due to the control of areas by rebel groups, but also because of the complicated process of obtaining government permission to travel to such areas and to offer health services. The activities of NGOs are concentrated in remote areas and in IDP camps, which the government has not served for political reasons, thus potentially bringing NGOs into conflict with the government. 88% of the interviewees at all levels, and noticeably 100% at the local level in district government and in the NGO sector maintained that NGOs have encountered many difficulties in accessing conflict-affected areas. According to an interviewee (2- 4, 10 January 2011, El Fasher) in the State Ministry of Health:
Good collaboration between the government and NGOs eases the possibility of accessing areas seriously affected by conflict and the people in need of health services. However, in North Darfur State, the security authorities remain the gatekeepers to the populations in conflict-affected areas. NGOs face difficulties in accessing these areas. The government does not believe that NGOs provide health services to the people in these areas. However, besides that, NGOs have a political agenda that serves their countries of origin, especially most international NGOs from Western countries with which the government differs politically and ideologically.
The government is skeptical of international NGOs’ intentions; therefore government expelled 13 of them from Darfur in early March 2009 (10). Most of them had worked in the health field in North Darfur State which left a huge gap in health service delivery for conflict-affected people. The government compels NGOs to undergo a regulative process to gain access to IDP camps and remote rural areas in order to ensure that the NGOs do not have any political or intelligence agenda and that their purpose really is to deliver health services. According to an interviewee (1-6, 15 December 2010, El Fasher) with Medicines Sans Frontiers — Spain:
All NGOs working in the curative health service delivery field complained that the government did not provide the time and flexibility of access to the remote areas where people affected by conflict are badly in need of health services. The process of getting permission to access the conflict- affected areas took four to six days, especially in those areas controlled by rebel groups. The delay of getting permission to access the conflict-affected areas influenced the collaboration between the NGOs and government.
Most interviewees indicated that in districts such as Kepkabiya and Dar El Salam, where health services were delivered by means of collaboration between the government and NGOs, the service provided had been more efficient and equitable than in those areas which remained under government control, such as El Towasha and El Malha districts. For example, according to an interviewee (1-7, 12 January 2011, El Fasher) in Kepkabiya district hospital:
The NGOs are very active and have been providing quality health services to the people of the district, whether in their health centres or in government facilities, which are co-ordinated by the health sector in the district. Therefore, people get curative health services easily because the health network in the district consists of 13 health facilities, out of which 8 are run by NGOs.
This confirms Keen’s (11) study which stated that the NGOs are important in identifying needs, providing services, assisting with policy implementation, linking the government and the community, and sharing their expertise.
The challenges of experience and capacity
Both those in NGOs and government believe that there is no balance between NGOs and government in terms of experience and capacity and that this constitutes the biggest challenge affecting collaboration between them. Government officials, whether doctors or managers, lack experience, in dealing with employees in NGOs who are far better equipped to deliver curative health services in North Darfur State. For example, according to an interviewee (2- 5, 28 January 2011, El Fasher) in the State Ministry of Health: ‘Without NGO financial resources and health staff, the government sector does not have the capacity and capability to deliver curative health services alone to all people in the district’. This confirms Wamai’s (12) research which indicated that the NGOs have numerous comparative advantages in health services provision, such as serving the community in remote places and within close proximity to the community.
A lack of knowledge, skills and capacity of government personnel prevents successful engagement between government and NGOs in collaborative initiatives. Although continuous interaction with NGOs needs a high level of skill and capacity among government health staff, without concrete steps to prepare an adequate database of the human resources, skills and capacities of the government sector. Hence, it is not possible for the government to benefit from the NGOs large human and financial capacities so as to strengthen the health system and enhance policy implementation.
General challenges to collaboration between government and NGOs
Several broad challenges affect the level of collaboration between the government and NGOs to deliver curative health services to poor and vulnerable people in North Darfur State. According to an interviewee (1-8, 15 December 2010, El Fasher) with Medicines Sans Frontiers — Spain:
Most NGOs prefer to work in isolation, as they feel that the government does not have the capacity and capability in terms of qualified health staff and communication facilities to collaborate effectively with them. Government, on the other hand, feels that they have capacity and capability to collaborate with NGOs, but the NGOs have hidden political agendas which are the main purpose of their work, rather than providing health services, and so they do not wish to collaborate closely with government to deliver curative health services to the conflict-affected people in North Darfur State.
In terms of organizational roles, the following three factors arose. Firstly, NGOs see government as putting many obstacles in front of them which limit their freedom by attempting to control them in an authoritarian manner, which in turn prevents the NGOs from doing their work properly. Government, on the other hand, regard NGOs as: more verbal and less active; opposed to any move to ensure transparency, especially in financial matters, which are driven by donors; obsessed with sectoral issues; over-critical of government policies; and blind to macro-challenges of development. In this respect the government prefers donors to support it directly to deliver health services to its citizens, not through NGOs.
Secondly, NGOs focus mostly on delivering health services as humanitarian aid, while the government wants NGOs to build health institutions and to deliver health services as a form of social development in the State. This is especially so in rural areas, which are crowded by people as a consequence of the persistent conflict and which require rehabilitation. However, there is no plan for future co-operative work between government and NGOs, as most NGOs are restricted to annual contracts, and concentrate on health delivery and not on reconstruction.
Thirdly, NGOs make a considerable effort to involve the community in health service delivery issues, by consulting them and representing them in their teams to manage health institutions which are established as joint health projects. However, the government wants to manage such health institutions, and therefore they see the NGOs as undermining their authority and thus presenting themselves as an alternative to government.
Conclusions
The conflict in Sudan, especially in North Darfur State, has led to a collapse in the health system, especially its infrastructure and supplies. This has limited the effectiveness of collaboration and coordination as well as communication between all actors: the Federal Ministry of Health, the State Ministry of Health, the district authorities, and the NGOs. Because the government has focused more attention and devoted more resources to addressing the continuing conflict in North Darfur State, less revenue has become available for health service delivery. Therefore, NGOs have come to play an increasing role in: providing human and financial resources; materials and equipment; changing health information; and in developing joint projects with government. However, the NGOs face many challenges and obstacles from the government in attempting to deliver curative health services to the people, especially those in rural and remote areas. The misunderstanding between the government and NGOs has had a negative impact on the level of collaboration between them.
Finally, a lack of trust has undermined collaboration between government and the NGOs, largely because they have different interests. The government does not wish to lose control to the NGOs, but public officials are at a disadvantage in having less capacity and experience in delivering and managing curative health services than the international agencies. NGOs wish to pursue humanitarian programmes and projects, and in doing so often have difficulty in arriving at effective working relationships with government. Although the collaboration between the NGOs and government is weak, especially because government lacks capacity in essential respects, the biggest challenge is how the government would be able to deliver curative health services to those affected by the conflict and to the poor more generally, should a peaceful settlement be reached and NGOs leave the region.
Ethical considerations
Ethical issues (Including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc) have been completely observed by the author.
Acknowledgements
I wish to thank all those who agreed to be interviewed. Without their patience and cooperation, I could not have completed this study. The author declares that there is no conflict of interests.
Footnotes
1 The interviewees and interviews are coded as follows: 1 = professional (doctor), 2= administrator. Thus 1-1 indicates an interview with the first professional, 1-2 with the second professional, and so on.
References
- Central Bureau of Statistics, Fifth Sudan Population and Housing Census (2008). Khartoum, Sudan: Available from: http://www.cbs.gov.sd/Tiedadat/Tiedadat%205th%20E.htm. [Google Scholar]
- United Nations (2008). Darfur Humanitarian Profile No 33, Office of UN Deputy Special Representative of the UN Secretary-General for Sudan UN Resident and Humanitarian coordinator. Available from: http://www.unsudanig.org/docs/DHP33_narrative_1%20October%202008.pdf.
- World Bank (2003). Sudan Health Status Report, World Bank/AFTH3. Draft Version 1. Available from: http://www.emro.who.int/sudan/pdf/Sudan%20Health%20Status%20Report%20August%202003.pdf.
- State Ministry of Health Survey Report (2009). The Final Survey Report about Spreads of Diseases in the State, December 2009, El Fasher, North Darfur State. [Google Scholar]
- World Health Organization (2010). Health Resources Availability Mapping System, Greater Darfur Report 2nd Quarter 2010. Available from: http://www.emro.who.int/sudan/pdf/HeRAMS_2Q_2010.pdf.
- State Ministry of Health Survey Report (2010). The Final Health Facilities and Human Resources Survey Report in the State and Distracts, December 2010, El Fasher, North Darfur State. [Google Scholar]
- State Ministry of Health Financial Report (2006). The Final Financial Report of Ministry of Health, El Fasher, North Darfur State. [Google Scholar]
- State Ministry of Health Financial Report (2009). The Final Financial Report of Ministry of Health, November 2009, El Fasher, North Darfur State [Google Scholar]
- Health and Fragile States Network Report (2009). Health Systems Strengthening in Fragile Contexts: A Report on Good Practices and New Approaches. Available from: www.healthandfragilestates.org.
- Wasabi W (2009). Aid Expulsions Leave Huge Gap in Darfur's Health Service, World Report, Vol 373 Available from: www.thelancet.com. [DOI] [PubMed] [Google Scholar]
- Keen S (2006). Non-Government Organizations in Policy. In: Beyond the Policy Cycle: The policy process in Australia. Eds, Colebatch HK. Allen and Unwin Pty LTD; Sydney, pp. 27–41. [Google Scholar]
- Wamai RG. Recent International Trends in NGO Health System Organization, Development and Collaborations with Government in Transforming Health Care Systems, the Case of Finland and Kenya [PhD thesis]. Institute of Development Studies, University of Helsinki, Finland; 2004. Available from: http://ethesis.helsinki.fi/julkaisut/val/sospo/vk/wamai/recentin.pdf. [Google Scholar]