Abstract
Hydrogen sulfide (H2S) is a gasotransmitter that regulates cardiovascular functions. The present study aimed to determine the protective effect of slow-releasing H2S donor GYY4137 on myocardial ischemia and reperfusion (I/R) injury and to investigate the possible signaling mechanisms involved. Male Sprague-Dawley rats were treated with GYY4137 at 12.5 mg/(kg·day), 25 mg/(kg·day) or 50 mg/(kg·day) intraperitoneally for 7 days. Then, rats were subjected to 30 minutes of left anterior descending coronary artery occlusion followed by reperfusion for 24 hours. We found that GYY4137 increased the cardiac ejection fraction and fractional shortening, reduced the ischemia area, alleviated histological injury and decreased plasma creatine kinase after myocardial I/R. Both H2S concentration in plasma and cystathionine-γ-lyase (CSE) activity in the myocardium were enhanced in the GYY4137 treated groups. GYY4137 also decreased malondialdehyde and myeloperoxidase levels in serum, attenuated superoxide anion level and suppressed phosphorylation of mitogen activated protein kinases in the myocardium after I/R. Meanwhile, GYY4137 increased the expression of Bcl-2 but decreased the expression of Bax, caspase-3 activity and apoptosis in the myocardium. The data suggest that GYY4137 protects against myocardial ischemia and reperfusion injury by attenuating oxidative stress and apoptosis.
Keywords: hydrogen sulfide, ischemia and reperfusion, myocardial infarction, oxidative stress, apoptosis
Introduction
Acute coronary artery diseases are one of the leading causes of mortality and morbidity worldwide. Clinical practice has changed rapidly over the last few years, progressing from thrombolysis to direct coronary intervention and stenting to restore myocardial blood flow. However, cardiac reperfusion after an acute myocardial infarction episode usually contributes to myocyte damage, which is named as myocardial ischemia and reperfusion (I/R) injury and is an important complication of acute arterial occlusion and subsequent recanalisation; for example, following acute myocardial infarction, coronary artery recanalisation by thrombolytic therapy or percutaneous coronary intervention to minimize the infarct area[1],[2]. Many signaling molecules are postulated to modulate I/R injury, including reactive oxygen species, calcium overload, energy metabolism dysfunction of myocardial fibers, neutrophils, vascular endothelial cells, cellular adhesion molecules, and apoptosis[3]. Previous studies have demonstrated that oxidative stress and apoptosis play a fundamental biological role in myocardial I/R injury.
Hydrogen sulfide (H2S) is the third identified gaseous transmitter after nitric oxide (NO) and carbon monoxide (CO) and it is endogenously generated in mammalians and has different effects in the cardiovascular system[4]. H2S can be produced by 3 major enzymes: cystathionine-γ-lyase (CSE), cystathionine-β-synthase (CBS) and 3-mecaptopyruvates sulfurtransferase (3-MST). CSE is the major hydrogen sulfide generating enzyme in the cardiovascular system, especially in the heart, vascular and smooth muscle cells, while CBS is expressed in the brain and nervous system, and 3-MST is present in the mitochondrials of the liver, kidney, brain and vascular cells[5]-[6]. The cardioprotective effect of H2S has been studied by several groups of scientists[7]-[8]. Johansen et al. reported that the perfusion of NaHS reduces myocardial infarction size in the Langendorff-perfused heart after 30 minutes of left main coronary artery occlusion and 120 minutes of reperfusion[9]. CSE inhibitor significantly increased the infarct size due to myocardial ischemia[10]-[11], while heart-specific overexpression of CSE significantly limited the infarct size due to left coronary artery occlusion for 45 minutes followed by reperfusion for 72 hours[12]. NaHS treatment significantly decreases the severity and duration of ischemia/reperfusion (I/R)-induced arrhythmias[13]-[14] and improves myocardial contractile function in the ISO-induced ischemic rat heart[15]. In the isolated perfused heart, H2S improves the heart mechanics after I/R injury[16].
However, pathogenesis of myocardial I/R injury is a very complex process, and the precise role of H2S remains unclear. One reason for the lack of clarity is the reliance on NaHS as an H2S donor in studies of this type. NaHS has been widely used to evaluate the biological and pharmacological effects of H2S. However, when dissolved in water, NaHS releases copious amounts of H2S over a short time frame (seconds) and as such does not effectively mimic the time course of H2S release in vivo[17]. It has been shown that high concentration of NaHS promotes lipopolysaccharides (LPS)-induced inflammation in macrophages[18]. Mice injected with NaHS also exhibits elevated MPO activity in the liver and lung[19].
Morpholin-4-ium-methoxyphenyl-morpholino-phosphinodithioate (GYY4137) slowly releases low but consistent concentrations of H2S over several hours in aqueous solution at physiological pH and temperature, and better mimics the time course of H2S release in vivo[17]. GYY4137 protects against high glucose-induced cytotoxicity in cardiomyocytes[20], relaxes phenylephrine pre-contracted arteries[21], and decreases vascular inflammation and oxidative stress[22]. However, whether GYY4137 affects myocardial I/R in vivo is unknown. In this study, we firstly used the slow-releasing H2S donor, GYY4137, to examine the effect of H2S on myocardial I/R, and to investigate the possible signaling mechanisms involved. From the present data, we raise the possibility that treatment with GYY4137 can provide a novel therapeutic approach to reduce the development and limit myocardial I/R.
Materials and Methods
Animals
Male Sprague-Dawley (SD) rats aged from 8 to 10 weeks were purchased from Vital River Laboratories, Beijing, China. The animals were fed on a laboratory diet with water and kept under constant environmental conditions (12 hour light/dark cycles). Animal experiments were performed in accordance with the guidelines for the Principles of Laboratory Animal Care and the Guide for the Care and Use of Laboratory Animals (NIH publication No. 85-23, revised 1996). This study was approved by the local institutional review board at the authors′ affiliated institutions. SD rats underwent sham operation (Sham) or coronary artery ligation followed by reperfusion (I/R); and the latter group were treated with saline (Vehicle) or GYY4137 at 3 different doses: 12.5 mg/(kg·day) (G12.5), 25 mg/(kg·day) (G25) or 50 mg/(kg·day) (G50). GYY4137 or vehicle was administered intraperitoneally in equal volume once daily for 7 continuous days.
In vivo myocardial ischemia and reperfusion model
Rats were anesthetized with sodium pentobarbital (40 mg/kg intraperitoneally). Atropine (0.1 mg/kg) was given subcutaneously to reduce airway secretions. The rats were ventilated and adequate anaesthesia was monitored by toe pinch. Myocardial ischemia was induced by exposing the heart through a left thoracic incision and placing a 6/0 silk suture with a slipknot around the left anterior descending coronary. After 30 minutes of ischemia, the slipknot was released for reperfusion for 24 hours. The sham-treated rats underwent left thoracotomy only.
Echocardiography
After 24 hours of reperfusion, rats were anaesthetized with sodium pentobarbital (40 mg/kg intraperitoneally), and cardiac function was evaluated by echocardiography using a GE Vivid 7 (GE, Fairfield, CT, USA) equipped with a 14-MHz phase array linear transducer S12. Ejection fraction (EF) and percent of fractional shortening (FS) of the left ventricle was derived by goal-directed, diagnostically driven software installed within the echocardiograph. All measurements were averaged over 5 consecutive cardiac cycles. Cardiac tissues or blood samples were then obtained after echocardiography for further analysis.
Determination of myocardial infarct size
Myocardial infarct size was determined by Evans blue/triphenyltetrazolium chloride (TTC) staining. The heart was harvested and 1.5% Evans blue (Sigma, St Louis, MO, USA) was injected into the aorta of the heart. Then, it was removed, washed with saline and frozen at -20 °C. The heart was cut horizontally into 5 slices, which were incubated in 1.2% TTC (Amresco, Solon, OH, USA) prepared with Tris-buffered saline (TBS, pH 7.8) for 15 minutes at 37 °C. Viable non-ischemic myocardium stained blue with Evans blue, ischemic but viable myocardium stained red with TTC, while necrotic myocardium did not stain with either and appeared pale white. The infarct area (white) and the area at risk (red and white) from each section were determined using an AlphaEaseFC image analyzer (Alpha Innotech Corporation, CA, USA). The ratio of infarct size (INF) to area at risk (AAR) was calculated and expressed as a percentage.
Measurement of serum creatine kinase, myeloperoxidase and malondialdehyde
Blood samples were obtained from the right carotid artery, placed at room temperature for 2 hours and centrifuged at 1,000 g for 15 minutes at 4 °C. Supernatants were then obtained. Creatine kinase (CK), myeloperoxidase (MPO) and malondialdehyde (MDA) were determined spectrophotometrically at 340 nm, 532 nm and 460 nm, respectively, according to the manufacturer's instructions (Jianchen Bioengineering Institute, Nanjing, Jiangsu, China). Each measurement was performed in duplicate.
Measurement of H2S in plasma and myocardium
H2S was measured as described previously[22]. Briefly, the initial reaction mixture containing 50 μL plasma, 200 μL of 15:1 (V/V) of 1% zinc acetate and 12% NaOH were incubated at 37 °C for 10 minutes. Then, 1.75 mL of H2O, 200 μL of 20 mmol/L N,N,dimethyl-p-phenylenediamine sulfate dissolved in 7.2 mol/L HCl, and 200 μL of 30 mmol/L FeCl3 dissolved in 1.2 mol/L HCl were added into the reaction mixtures. H2S synthesizing activity of the myocardium was determined using tissue homogenates. The assay mixture contained 460 μL of tissue homogenate, 20 μL of 10 mol/L L-cysteine, and 20 μL of 2 mmol/L pyridoxal 5′-phosphate. After incubation at 37 °C for 30 minutes, zinc acetate (1% w/v, 250 μL) was added to trap the generated H2S for another 30 minutes followed by trichloroacetic acid (10% w/v, 25 μL) to stop the reaction. N,N-dimethyl-p-phenylenediamine sulfate (20 mmol/L, 133 μL) and FeCl3 (30 mmol/L, 133 μL) were added and the mixture centrifuged at 12,000 g for 5 minutes. Both of the above reactions were allowed to proceed for 10 minutes in a dark box, and the absorbance of aliquots (200 μL) was measured at 670 nm. The NaHS with the concentrations of 2.5, 25, 50, 100 and 200 μmol/L were used as the standard. H2S concentration for each sample was calculated against a calibration curve made using NaHS standard.
Measurement of superoxide anion generation
Cardiac tissue samples were immediately frozen after removal in OCT embedding medium (Sakura Finetek, Tokyo, Japan), and then cut into 4 μm-thick sections and placed on glass slides. Dihydroethidium (DHE, 2 μmol/L, Beyotime, Haimen, Jiangsu, China) was applied to each tissue section and the slides were incubated in a light-protected humidified chamber at 37 °C for 15 minutes. The slides were examined by fluorescence microscopy (Olympus, Tokyo, Japan).
TUNEL staining
For terminal deoxynucleotidyl-transferase mediated dUTP nick-end labeling (TUNEL) staining, the hearts were fixed in 4% V/V paraformaldehyde, embedded in paraffin, cut into 2-μm thickness sections and treated as indicated in the in situ cell death detection kit (Roche, Mannheim, Germany). Thereafter, nuclei were co-stained with hematoxylin (Beyotime, Haimen, Jiangsu, China).
Measurement of caspase-3 activity
Caspase-3 activity was measured according to the instruction of the manufacturer (BioVision, Milpitas, CA, USA) in the myocardium homogenates with excitation wavelength at 400 nm and emission wavelength at 505 nm. The cardiac tissue samples were lysed on ice and centrifuged at 10,000 g for 15 minutes and the supernatant were collected. Reactions were performed in assay buffer containing 10 mM DTT and 50 μg proteins. The assay mixtures were incubated at room temperature for 1 hour in the dark and the fluorescent intensity was monitored by wavelength scanning at a range of 400 nm to 505 nm.
Western blotting assays
Protein samples were separated on sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE), transferred onto polyvinylidene fluoride (PVDF) membrane (Millipore, Billerica, MA, USA) and then immunoblotted with primary antibodies against the following proteins: extracellular signal-regulated kinases (ERK), phospho-ERK, stress-activated/c-Jun NH2 terminal kinases (JNK), phospho-JNK, P38, phospho-P38, Bcl-2, Bax (all from Cell Signaling Technology, Danvers, MA, USA) and GAPDH (Sigma). Proteins were visualized by enhanced chemiluminescence substrate (Thermo Fisher, Waltham, MA, USA)
Quantitative real-time PCR (qRT-PCR)
Total RNA was extracted using Trizol reagent (Takara, Osaka, Japan). RNA (500 ng) was added as a template to reverse-transcriptase reactions carried out using PrimeScript™ RT Master Mix kit (Takara, Japan). qRT-PCR was carried out in triplicate with the resulting cDNAs using SYBR Green Premix (Takara) and ABI 7500 Real-time PCR System (ABI, Carlsbad, CA, USA). Experimental Ct values were normalized to 18S and relative CSE mRNA expression was calculated versus a reference sample. Primers used to amplify the fragment of CSE and 18S were listed as follows: CSE-F, 5′-TCCGGATGGAGAAACACTTC-3′; CSE-R, 5′-GCTGCCTTTAAAGCTTGACC-3′; 18S-F, 5′-TCAAGAACGAAAGTCGGAGG-3′; 18S-R, 5′- GGACATCTAAGGGCATCACA -3′.
Statistical analysis
All data are expressed as mean ± SEM. They were analyzed by one-way ANOVA followed by Student's t-test. P < 0.05 (2-tailed) was considered statistically significant.
Results
GYY4137 protects cardiac function and reduces infarct size after myocardial I/R
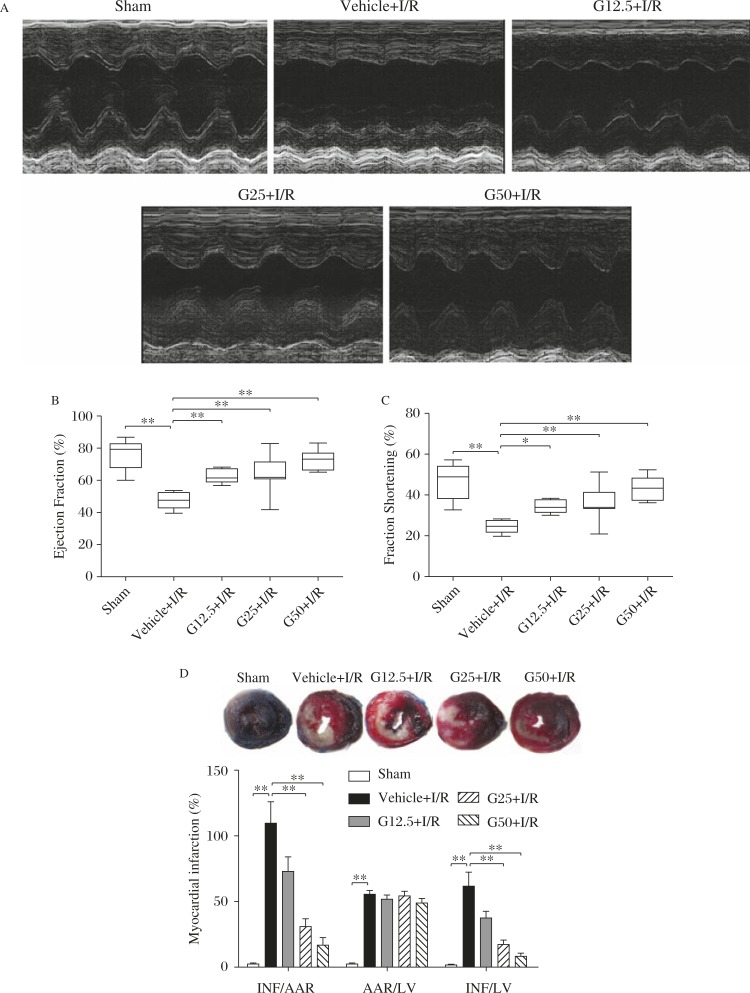
Cardiac function of rats was measured by echocardiography, and typical M-mode traces for each of the 5 groups are shown in Fig. 1A. Thirty minutes of ischemia followed by 24 hours of reperfusion decreased the EF and FS in vehicle-treated rats compared to the sham-operated rats. GYY4137 pre-treatment for 7 days improved cardiac function significantly after myocardial I/R (Fig. 1B–C). The effect of GYY4137 on infarct size after myocardial I/R was determined by the Evans-blue/TTC staining. Compared to the sham-operated group, 30 minutes of ischemia followed by 24 hours of reperfusion resulted in severe myocardial injury. Treatment with GYY4137 reduced myocardial INF/AAR and INF/LV ratio after myocardial I/R injury, respectively (Fig. 1D).
Fig. 1. GYY4137 protects cardiac function and reduces infarct size after myocardial ischemia/reperfusion (I/R).
A: Typical M-mode traces on echocardiography. B-C: Left ventricle ejection fraction and fraction shortening were measured by echocardiography in vivo after 30 minutes of myocardial ischemia and 24 hours of reperfusion (n = 9-12). D: Myocardial infarction was determined by Evans blue/TTC staining (n = 6). INF: infarct size; AAR: area at risk; LV: left ventricle; Sham: sham operation, Vehicle +I/R: saline pre-treatment for 7 days followed by 30 minutes of myocardial ischemia and 24 hours of reperfusion, G12.5+I/R, G25+I/R or G50+I/R: GYY4137 pre-treatment at 12.5 mg/(kg·day), 25 mg/(kg·day) or 50 mg/(kg·day) for 7 days followed by 30 minutes of myocardial ischemia and 24 hours of reperfusion. *P<0.05, **P<0.01.
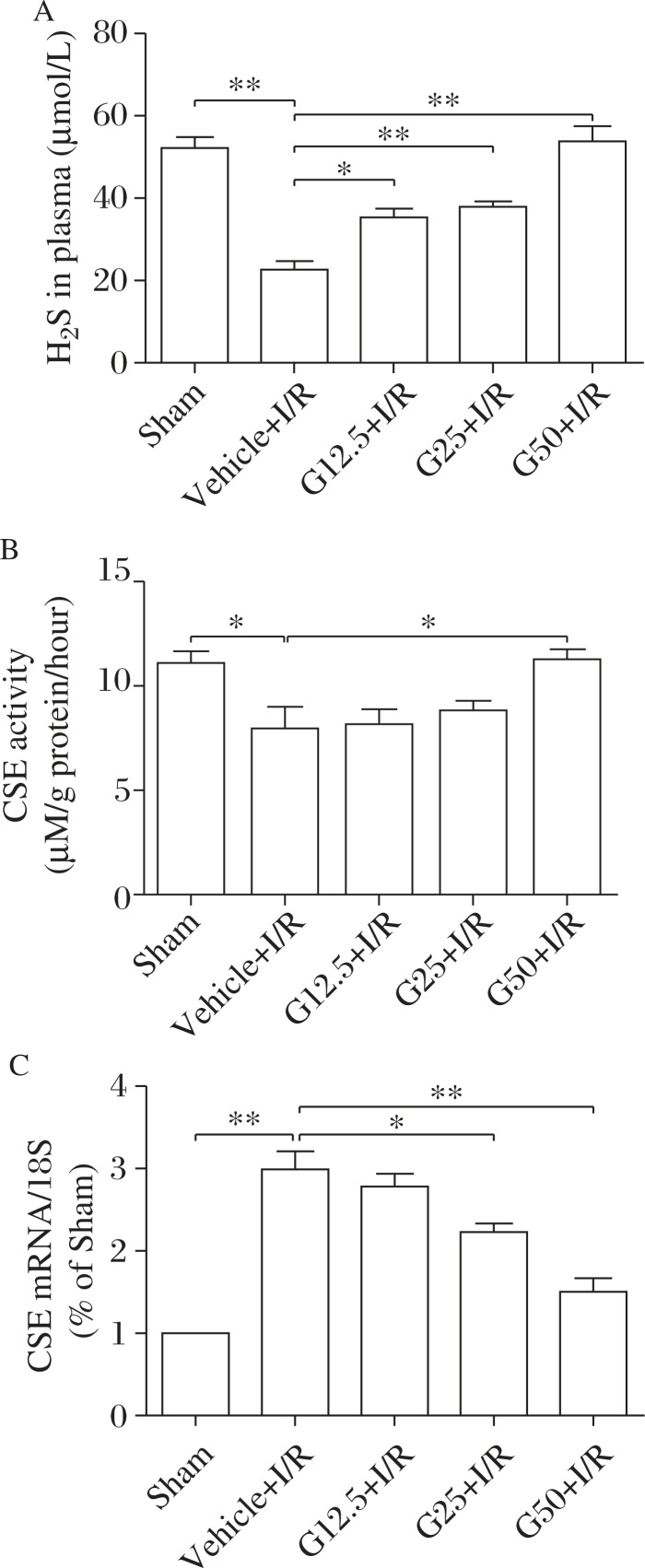
GYY4137 increases plasma H2S concentration and CSE activity in the myocardium but decreases CSE mRNA in the myocardium after myocardial I/R
H2S concentration in plasma and CSE activity in the myocardium after myocardial I/R were significantly less than those detected in the sham controls, while administration of GYY4137 for 7 days increased both plasma H2S concentration and CSE activity. However, CSE mRNA expression in the myocardium after I/R was increased and reduced by GYY4137 treatment (Fig. 2).
Fig. 2. GYY4137 increases plasma H2S and cystathionine-γ-lyase (CSE) activity but decreases CSE mRNA in the myocardium after I/R.
A: Plasma H2S concentration measured by chemical method (n = 6-9). B: Myocardial CSE activity (n = 6-10). C: CSE mRNA expression determined by quantitative real-time PCR (n = 5). Sham: sham operation; Vehicle+I/R: saline pre-treatment for 7 days followed by 30 minutes of myocardial ischemia and 24 hours of reperfusion, G12.5+I/R, G25+I/R or G50+I/R: GYY4137 pre-treatment at 12.5 mg/(kg·day), 25 mg/(kg·day) or 50 mg/(kg·day) for 7 days followed by 30 minutes of myocardial ischemia and 24 hours of reperfusion. *P<0.05, **P<0.01.
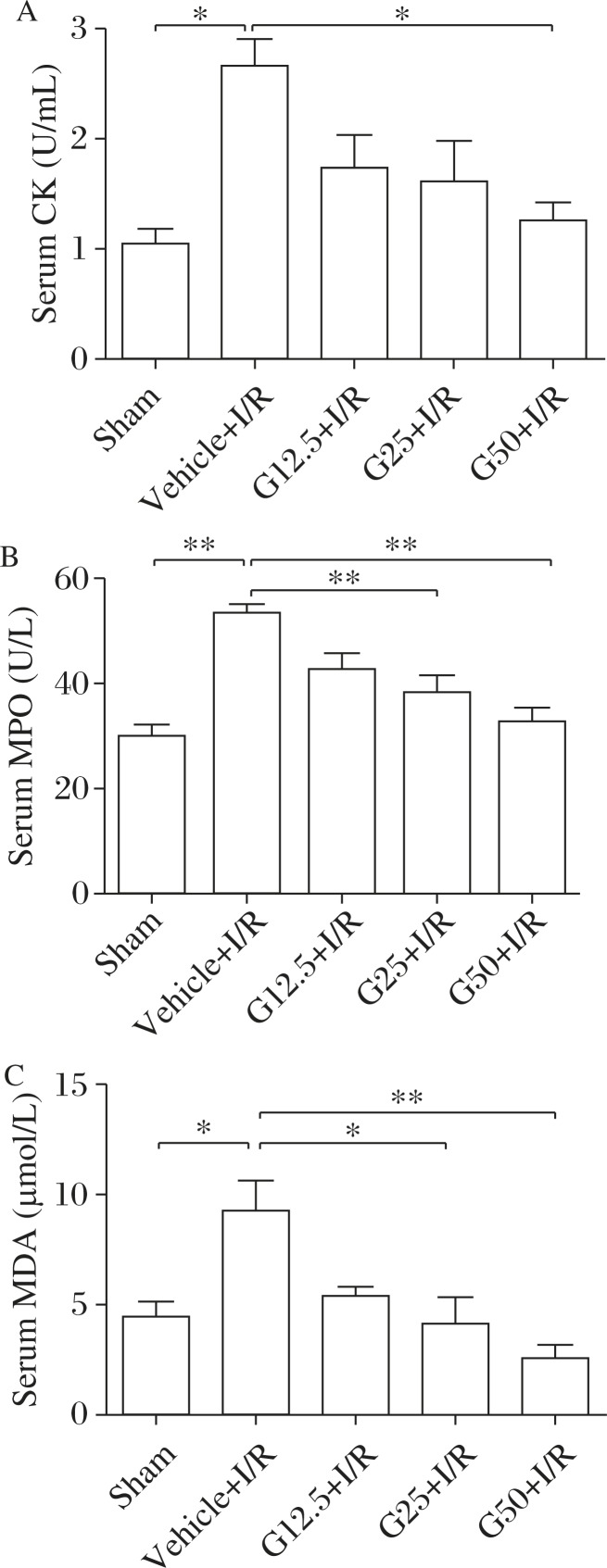
GYY4137 decreases myocardial injury and systemic oxidative stress after myocardial I/R
We measured plasma CK, which is an important indicator of the extent of myocardial injury. Thirty minutes of ischemia followed by 24 hours of reperfusion increased CK, which was prevented by 50/mg·day GYY4137 (Fig. 3A). Compared with the sham-operated group, plasma MPO activity was increased after myocardial I/R as expected. This increase was significantly prevented by GYY4137 (Fig. 3B). Plasma MDA is a sensitive indicator of oxidant stress for the whole body. There was an increase in plasma MDA in the vehicle-treated group as a result of myocardial I/R and this increase was prevented by GYY4137 (Fig. 3C).
Fig. 3. GYY4137 decreases serum CK, MPO and MDA level after myocardium I/R.
Serum CK (A), MPO (B) and MDA (C) in serum were measured (n = 5-10). CK: creatine kinase, MPO: myeloperoxidase; MDA: malondialdehyde; Sham: sham operation; Vehicle +I/R: saline pre-treatment for 7 days followed by 30 minutes of myocardial ischemia and 24 hours of reperfusion, G12.5+I/R, G25+I/R or G50+I/R: GYY4137 pre-treatment at 12.5 mg/(kg·day), 25 mg/(kg·day) or 50 mg/(kg·day) for 7 days followed by 30 minutes of myocardial ischemia and 24 hours of reperfusion. *P<0.05, **P<0.01.
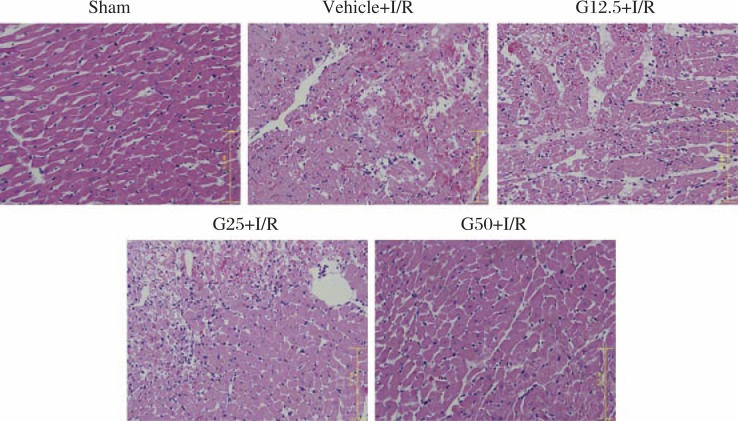
GYY4137 alleviates histological injury after myocardial I/R
Myocardial fibers were arranged irregularly with hematoma emerged in the myocardium under the ligature with H&E staining in the vehicle group after 30 minutes of myocardial ischemia and 24 hours of reperfusion, which was alleviated by 7-day treatment of GYY4137 (Fig. 4).
Fig. 4. GYY4137 alleviates histological injury after myocardial I/R.
Histological examination of the myocardium under the ligature with H&E staining (n = 5). Sham: sham operation; Vehicle +I/R: saline pre-treatment for 7 days followed by 30 minutes of myocardial ischemia and 24 hours of reperfusion, G12.5+I/R, G25+I/R or G50+I/R: GYY4137 pre-treatment at 12.5 mg/(kg·day), 25 mg/(kg·day) or 50 mg/(kg·day) for 7 days followed by 30 minutes of myocardial ischemia and 24 hours of reperfusion.
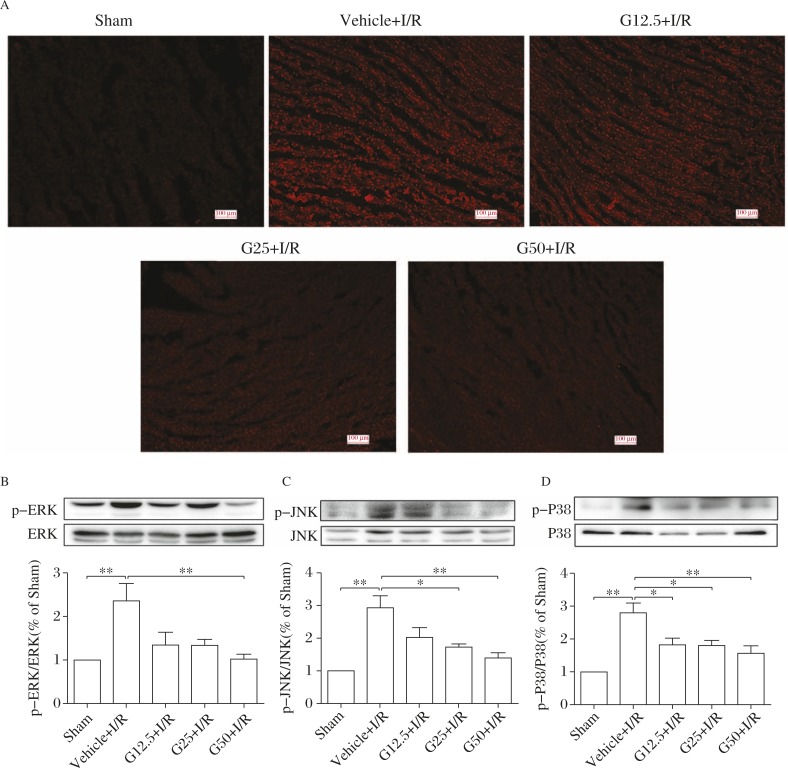
GYY4137 attenuates oxidative stress and inhibits the MAPK signal pathway in the myocardium after myocardial I/R
Compared with the sham control, myocardial DHE fluorescence was elevated in the vehicle group after 30 minutes of ischemia followed by 24 hours of reperfusion, suggesting severe oxidative stress in the myocardium. After GYY4137 pre-administration for 7 days, oxidative stress in the myocardium was reduced significantly (Fig. 5A). Western blotting assay showed that phosphorylation of mitogen activated protein kinases (MAPK) was enhanced after myocardial I/R, while GYY4137 inhibited myocardial MAPK phosphorylation significantly after 7-day treatment (Fig. 5B–D).
Fig. 5. GYY4137 attenuates oxidative stress in the myocardium after I/R.
A: Representative photomicrographs of dihydroethidium (DHE) stained cardiac sections. B–D: Representative Western blots of MAPK (ERK, JNK and P38) and quantification of phosphorylation was evaluated by ratio of phospho-ERK/ERK phospho-JNK/JNK and phospho-P38/P38 (n = 4-8). Sham: sham operation, Vehicle +I/R: saline pre-treatment for 7 days followed by 30 minutes of myocardial ischemia and 24 hours of reperfusion, G12.5+I/R, G25+I/R or G50+I/R: GYY4137 pre-treatment at 12.5 mg/(kg·day), 25 mg/(kg·day) or 50 mg/(kg·day) for 7 days followed by 30 minutes of myocardial ischemia and 24 hours of reperfusion. *P<0.05, **P<0.01.
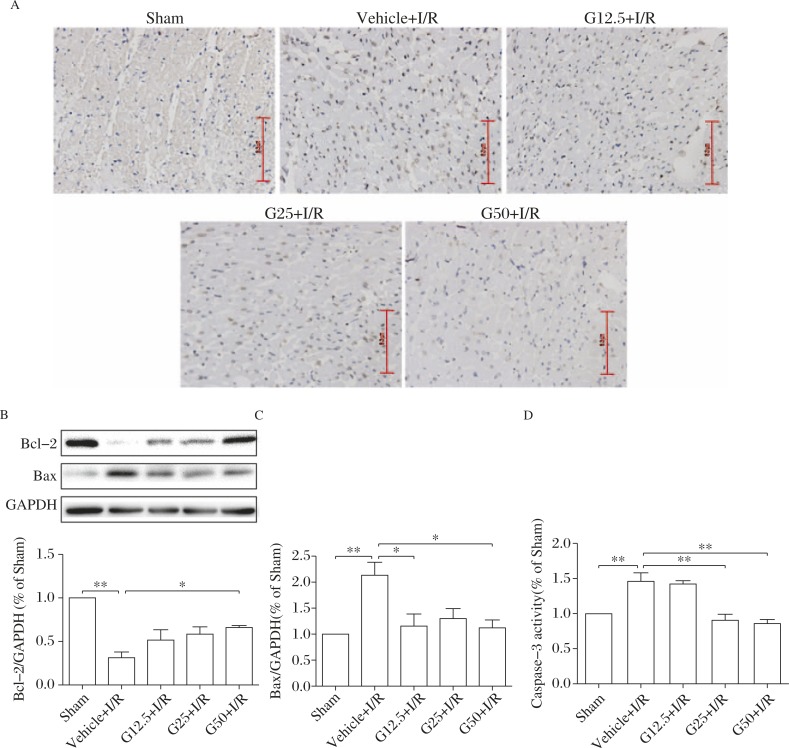
GYY4137 ameliorates apoptosis of cardiomyocytes after myocardial I/R
As apoptosis is a major outcome of I/R injury, we additionally evaluated the effect of GYY4137 on apoptosis in this study. There were large numbers of TUNEL-positive cells in the ischemic border zone in the vehicle group, which decreased significantly in GYY4137 pre-treated rats (Fig. 6A). We also found that 30 minutes of ischemia followed by 24 hours of reperfusion decreased the expression of Bcl-2 while increasing the expression of Bax and activity of caspase-3 in the myocardium as compared to the sham-operated rats. GYY4137 restored all of these changes significantly (Fig. 6B–D).
Fig. 6. GYY4137 ameliorates cardiomyocytes apoptosis after myocardial I/R.
A: Apoptosis was determined by TUNEL staining of cardiac sections. B–C: Representative examples and quantification of Bcl-2 and Bax expression in the myocardium with Western blotting assay. GAPDH was used as a loading control (n = 6-7). D: Caspase-3 activity in the myocardium (n = 7-8). Sham: sham operation, Vehicle +I/R: saline pre-treatment for 7 days followed by 30 minutes of myocardial ischemia and 24 h of reperfusion, G12.5+I/R, G25+I/R or G50+I/R: GYY4137 pre-treatment at 12.5 mg/(kg·day), 25 mg/(kg·day) or 50 mg/(kg·day) for 7 days followed by 30 minutes of myocardial ischemia and 24 hours of reperfusion. *P<0.05, **P<0.01.
Discussion
In our study, after 24 hours of reperfusion followed by 30 minutes of myocardial ischemia, echocardiography was performed to evaluate the cardiac functional. It was found that compared with the vehicle control, GYY4137-treated rats had higher EF and FS, indicating that GYY4137 can significantly improve the systolic function. GYY4137 also markedly reduced the ischemic area and alleviated the degree of histological injury after myocardial I/R. Creatine kinase (CK) is a classical indicator of myocardial injury[23]. GYY4137 (50/mg·day) significantly inhibited the release of CK after myocardial I/R. In conclusion, all these results confirmed that GYY4137 protected against myocardial ischemic reperfusion injury.
We found the reduced H2S content in plasma as well as decreased activity of CSE in the myocardium. The reduced endogenous H2S production in the ischemic heart implies that ischemic heart injury may, at least in part, result from impaired endogenous production of H2S. Surprisingly, we noted high CSE mRNA expression but reduced H2S synthesis after myocardial I/R. It is similar to our previous finding in high fat fed apolipoprotein E-/- mice[22]. This apparent discrepancy might be attributed to the presence of a positive compensatory feedback mechanism, through low concentrations of H2S, to promote CSE expression. Understandably, in our experiments, exogenous administration of GYY4137 (which elevated H2S concentration) reversed the rise in CSE expression. Further experiments are required to examine the possible feedback loop in more details.
There is accumulating evidence that oxidative stress induces I/R injury, and reactive oxygen species have long been recognized as major mediators of I/R injury[24]. Therefore, we examined the potential contribution of oxidative stress to the protective effect of GYY4137 against I/R injury. Previous studies have demonstrated that activated neutrophils are major sources of oxygen-derived free radicals during reperfusion after prolonged myocardial ischemia in vivo[25]. Many studies have indicated that MPO is specific for leukocytes, especially polymorphonuclear neutrophils. Therefore, MPO has been used as a marker of activated neutrophils released into the bloodstream[26]. We confirmed that, indeed, MPO levels were higher after I/R; however, GYY4137 treatment restored MPO levels to normal. Lipids can be oxidized by free radicals and changed into MDA finally. MDA is cytotoxic and can crosslink proteins or nucleic acids into polymers, damaging the mitochondrial respiratory chain complexes and key mitochondrial enzymes. As one of the end-products in the lipid peroxidation process, MDA has also been used to assess oxygen-derived free radical-mediated injury[27]. In our study, plasma MDA level in the GYY4137-treated groups was lower than that in the vehicle-treated group. Moreover, myocardial superoxide anion generation in response to I/R was attenuated by GYY4137 treatment. Therefore, GYY4137 may protect against myocardial I/R at least in part through attenuating oxidative stress.
The MAPK signal pathways, including ERK, JNK and P38, play key roles in various intercellular pathological processes, such as cellular growth, development, division, and apoptosis. Exogenous NaHS protects H9c2 cardiac cells against high glucose-induced injury by inhibiting the activities of the p38 MAPK and ERK1/2 pathways[28]. Na2S administration attenuated myocardial ischemia-reperfusion injury in db/db mice in an ERK-dependent manner[29]. However, Hu et al. observed that NaHS protected the heart against I/R injury by reducing myocardial injury. The blockade of ERK1/2 with PD98059 during either preconditioning or ischemia periods reversed these cardioprotective effects, suggesting that action of ERK1/2 may at least partly mediate the cardioprotection afforded by H2S[30]. NaHS also prevented I/R-induced P38 and JNK phosphorylation on gastric epithelial cells[31]. Our study discovered that exogenous GYY4137 administration could significantly decrease the phosphorylation of MAPK in myocardial I/R, which is at least partially involved in the attenuating effect of myocardial I/R by GYY4137.
Apoptosis also plays a significant role in myocardial ischemia reperfusion injury[32]. It has been reported that inhibition of caspase during reperfusion resulted in less cell apoptosis. While in patients who died from acute cardiac infarction, the balance between Bcl-2 and Bax was disturbed. Previous study found that H2S inhibits apoptosis of cardiomyocytes induced by myocardial I/R injury via enhancing phosphorylation of apoptosis repressor with caspase recruitment domain[33]. We found reduced Bcl-2 but up-regulated Bax expression after reperfusion, as well as increased activity of caspase-3 and severe apoptosis in the vehicle group. The GYY4137 treated group showed significant enhanced expression of Bcl-2 but decreased levels of apoptosis, Bax expression and caspase-3 activity. In conclusion, the results proven that the myocardial protection against ischemia reperfusion of GYY4137 was realized partially through releasing apoptosis by regulation of Bcl-2, Bax and caspase-3.
In summary, our study confirmed that H2S slow-releasing agent GYY4137 protected against I/R injury of SD rats evidenced as improvement of cardiac function and ischemia area. Enhancement of oxidative stress and activation of the MAPK signaling pathway were suppressed by GYY4137 after I/R. GYY4137 also down-regulated the activity and expression of pro-apoptosis proteins but up-regulated anti-apoptosis proteins to inhibit apoptosis. Thus, the present data provided novel evidence that treatment with H2S can provide a novel therapeutic approach to limit myocardial I/R injury.
Acknowledgements
This work was supported by grants from the National Natural Science Foundation of China (Grant No. 81170083, 81400203), Universities Natural Science Research Project of Jiangsu Province (No. 10KJA310033), Major Science and Technology Development Fund Project of Nanjing Medical University (2011NJMU264) and the Priority Academic Program Development (PAPD) of Jiangsu Higher Education Institutions.
References
- 1.Jennings RB. Historical perspective on the pathology of myocardial ischemia/reperfusion injury[J] Circ Res. 2013;113(4):428–438. doi: 10.1161/CIRCRESAHA.113.300987. [DOI] [PubMed] [Google Scholar]
- 2.Vander Heide RS, Steenbergen C. Cardioprotection and myocardial reperfusion: Pitfalls to clinical application[J] Circ Res. 2013;113(4):464–477. doi: 10.1161/CIRCRESAHA.113.300765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mozaffari MS, Liu JY, Abebe W, et al. Mechanisms of load dependency of myocardial ischemia reperfusion injury[J] Am J Cardiovasc Dis. 2013;3(4):180–196. [PMC free article] [PubMed] [Google Scholar]
- 4.Wang R. Physiological implications of hydrogen sulfide: A whiff exploration that blossomed[J] Physiol Rev. 2012;92(2):791–896. doi: 10.1152/physrev.00017.2011. [DOI] [PubMed] [Google Scholar]
- 5.Liu YH, Lu M, Hu LF, et al. Hydrogen sulfide in the mammalian cardiovascular system[J] Antioxid Redox Signal. 2012;17(1):141–185. doi: 10.1089/ars.2011.4005. [DOI] [PubMed] [Google Scholar]
- 6.Tan BH, Wong PT, Bian JS. Hydrogen sulfide: A novel signaling molecule in the central nervous system[J] Neurochem Int. 2010;56(1):3–10. doi: 10.1016/j.neuint.2009.08.008. [DOI] [PubMed] [Google Scholar]
- 7.Wang R. The gasotransmitter role of hydrogen sulfide[J] Antioxid Redox Signal. 2003;5(4):493–501. doi: 10.1089/152308603768295249. [DOI] [PubMed] [Google Scholar]
- 8.Pearson RJ, Wilson T, Wang R. Endogenous hydrogen sulfide and the cardiovascular system-what's the smell all about? Clin Invest Med. 2006;29(3):146–150. [PubMed] [Google Scholar]
- 9.Johansen D, Ytrehus K, Baxter GF. Exogenous hydrogen sulfide (h2s) protects against regional myocardial ischemia-reperfusion injury–evidence for a role of k atp channels[J] Basic Res Cardiol. 2006;101(1):53–60. doi: 10.1007/s00395-005-0569-9. [DOI] [PubMed] [Google Scholar]
- 10.Bliksoen M, Kaljusto ML, Vaage J, et al. Effects of hydrogen sulphide on ischaemia-reperfusion injury and ischaemic preconditioning in the isolated, perfused rat heart[J] Eur J Cardiothorac Surg. 2008;34(2):344–349. doi: 10.1016/j.ejcts.2008.03.017. [DOI] [PubMed] [Google Scholar]
- 11.Sivarajah A, McDonald MC, Thiemermann C. The production of hydrogen sulfide limits myocardial ischemia and reperfusion injury and contributes to the cardioprotective effects of preconditioning with endotoxin, but not ischemia in the rat[J] Shock. 2006;26(2):154–161. doi: 10.1097/01.shk.0000225722.56681.64. [DOI] [PubMed] [Google Scholar]
- 12.Elrod JW, Calvert JW, Morrison J, et al. Hydrogen sulfide attenuates myocardial ischemia-reperfusion injury by preservation of mitochondrial function[J] Proc Natl Acad Sci U S A. 2007;104(39):15560–15565. doi: 10.1073/pnas.0705891104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bian JS, Yong QC, Pan TT, et al. Role of hydrogen sulfide in the cardioprotection caused by ischemic preconditioning in the rat heart and cardiac myocytes[J] J Pharmacol Exp Ther. 2006;316(2):670–678. doi: 10.1124/jpet.105.092023. [DOI] [PubMed] [Google Scholar]
- 14.Zhang Z, Huang H, Liu P, et al. Hydrogen sulfide contributes to cardioprotection during ischemia-reperfusion injury by opening k atp channels[J] Can J Physiol Pharmacol. 2007;85(12):1248–1253. doi: 10.1139/Y07-120. [DOI] [PubMed] [Google Scholar]
- 15.Geng B, Chang L, Pan C, et al. Endogenous hydrogen sulfide regulation of myocardial injury induced by isoproterenol[J] Biochem Biophys Res Commun. 2004;318(3):756–763. doi: 10.1016/j.bbrc.2004.04.094. [DOI] [PubMed] [Google Scholar]
- 16.Rossoni G, Manfredi B, Tazzari V, et al. Activity of a new hydrogen sulfide-releasing aspirin (acs14) on pathological cardiovascular alterations induced by glutathione depletion in rats[J] Eur J Pharmacol. 2010;648(1-3):139–145. doi: 10.1016/j.ejphar.2010.08.039. [DOI] [PubMed] [Google Scholar]
- 17.Li L, Whiteman M, Guan YY, et al. Characterization of a novel, water-soluble hydrogen sulfide-releasing molecule (gyy4137): New insights into the biology of hydrogen sulfide[J] Circulation. 2008;117(18):2351–2360. doi: 10.1161/CIRCULATIONAHA.107.753467. [DOI] [PubMed] [Google Scholar]
- 18.Whiteman M, Li L, Rose P, et al. The effect of hydrogen sulfide donors on lipopolysaccharide-induced formation of inflammatory mediators in macrophages[J] Antioxid Redox Signal. 2010;12(10):1147–1154. doi: 10.1089/ars.2009.2899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li L, Bhatia M, Zhu YZ, et al. Hydrogen sulfide is a novel mediator of lipopolysaccharide-induced inflammation in the mouse[J] FASEB J. 2005;19(9):1196–1198. doi: 10.1096/fj.04-3583fje. [DOI] [PubMed] [Google Scholar]
- 20.Wei WB, Hu X, Zhuang XD, et al. Gyy4137, a novel hydrogen sulfide-releasing molecule, likely protects against high glucose-induced cytotoxicity by activation of the ampk/mtor signal pathway in h9c2 cells[J] Mol Cell Biochem. 2013;389(1-2):249–256. doi: 10.1007/s11010-013-1946-6. [DOI] [PubMed] [Google Scholar]
- 21.Chitnis MK, Njie-Mbye YF, Opere CA, et al. Pharmacological actions of the slow release hydrogen sulfide donor gyy4137 on phenylephrine-induced tone in isolated bovine ciliary artery[J] Exp Eye Res. 2013;116(1):350–354. doi: 10.1016/j.exer.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 22.Liu Z, Han Y, Li L, et al. The hydrogen sulfide donor, gyy4137, exhibits anti-atherosclerotic activity in high fat fed apolipoprotein e(-/-) mice[J] Br J Pharmacol. 2013;169(8):1795–1809. doi: 10.1111/bph.12246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li ZL, Hu J, Li YL, et al. The effect of hyperoside on the functional recovery of the ischemic/reperfused isolated rat heart: Potential involvement of the extracellular signal-regulated kinase 1/2 signaling pathway[J] Free Radic Biol Med. 2013;57(1):132–140. doi: 10.1016/j.freeradbiomed.2012.12.023. [DOI] [PubMed] [Google Scholar]
- 24.Kleikers PW, Wingler K, Hermans JJ, et al. Nadph oxidases as a source of oxidative stress and molecular target in ischemia/reperfusion injury[J] J Mol Med (Berl) 2012;90(12):1391–1406. doi: 10.1007/s00109-012-0963-3. [DOI] [PubMed] [Google Scholar]
- 25.Schofield ZV, Woodruff TM, Halai R, et al. Neutrophils-a key component of ischemia-reperfusion injury[J] Shock. 2013;40(6):463–470. doi: 10.1097/SHK.0000000000000044. [DOI] [PubMed] [Google Scholar]
- 26.Wang XL, Liu HR, Tao L, et al. Role of inos-derived reactive nitrogen species and resultant nitrative stress in leukocytes-induced cardiomyocyte apoptosis after myocardial ischemia/reperfusion[J] Apoptosis. 2007;12(7):1209–1217. doi: 10.1007/s10495-007-0055-y. [DOI] [PubMed] [Google Scholar]
- 27.de Vries DK, Kortekaas KA, Tsikas D, et al. Oxidative damage in clinical ischemia/reperfusion injury: A reappraisal[J] Antioxid Redox Signal. 2013;19(6):535–545. doi: 10.1089/ars.2012.4580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Xu W, Wu W, Chen J, et al. Exogenous hydrogen sulfide protects h9c2 cardiac cells against high glucose-induced injury by inhibiting the activities of the p38 mapk and erk1/2 pathways[J] Int J Mol Med. 2013;32(4):917–925. doi: 10.3892/ijmm.2013.1462. [DOI] [PubMed] [Google Scholar]
- 29.Peake BF, Nicholson CK, Lambert JP, et al. Hydrogen sulfide preconditions the db/db diabetic mouse heart against ischemia-reperfusion injury by activating nrf2 signaling in an erk-dependent manner[J] Am J Physiol Heart Circ Physiol. 2013;304(9):H1215–1224. doi: 10.1152/ajpheart.00796.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hu Y, Chen X, Pan TT, et al. Cardioprotection induced by hydrogen sulfide preconditioning involves activation of erk and pi3k/akt pathways[J] Pflugers Arch. 2008;455(4):607–616. doi: 10.1007/s00424-007-0321-4. [DOI] [PubMed] [Google Scholar]
- 31.Guo C, Liang F, Shah Masood W, et al. Hydrogen sulfide protected gastric epithelial cell from ischemia/reperfusion injury by keap1 s-sulfhydration, mapk dependent anti-apoptosis and nf-kappab dependent anti-inflammation pathway[J] Eur J Pharmacol. 2014;725(1):70–78. doi: 10.1016/j.ejphar.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 32.Xu T, Li D, Jiang D. Targeting cell signaling and apoptotic pathways by luteolin: Cardioprotective role in rat cardiomyocytes following ischemia/reperfusion[J] Nutrients. 2012;4(12):2008–2019. doi: 10.3390/nu4122008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yao X, Tan G, He C, et al. Hydrogen sulfide protects cardiomyocytes from myocardial ischemia-reperfusion injury by enhancing phosphorylation of apoptosis repressor with caspase recruitment domain[J] Tohoku J Exp Med. 2012;226(4):275–285. doi: 10.1620/tjem.226.275. [DOI] [PubMed] [Google Scholar]