Abstract
Background
Smoking cessation rates have remained stagnant globally. This study was conducted to explore the factors associated with successful smoking cessation among South Korean adult males using nationally representative data from the Korea National Health and Nutrition Examination Survey (KNHANES) from 2007 to 2012. A comparison was made between successful quitters and those who failed to quit after attempts to stop smoking.
Methods
A total of 7,839 males, aged 19–65 years, were included in this cross-sectional study. The outcome measures were the success and failure rates in smoking cessation, sociodemographic and clinical characteristics, health behaviors, perceived health status, quality of life, and mental health. Multiple logistic regression analyses were used to examine the various factors associated with smoking cessation success.
Results
The cessation success and failure rates were 45.5% and 54.5%, respectively. Smoking cessation was related to older age, marriage, higher income, smoking larger amounts of cigarettes, use of willpower, alcohol abstinence, cancer history, better mental health, and higher levels of quality of life, after controlling for multiple variables. Second-hand smoke exposure at home and using nicotine replacement therapy were associated with a lower likelihood of smoking cessation.
Conclusion
A smoke-free environment, use of willpower, alcohol abstinence, and better stress management are important for smoking cessation. Unlike previous studies, not using nicotine replacement therapy and higher levels of daily cigarette consumption were associated with successful smoking cessation, suggesting that motivation appears to be important to smoking cessation in Korean adult male population.
Keywords: Males, Smoking cessation, South Korea
Introduction
Cigarette smoking is one of the leading, but preventable, causes of premature death worldwide (1–4). Smoking harms nearly every organ of our body and increases mortality from all causes in human beings (2, 5). The worldwide economic burden related to smoking has been estimated within the billion-dollar range, which results from direct medical care, lost productivity due to premature deaths, and exposure to secondhand smoke (6). Although the prevention of smoking initiation is of paramount importance, the cessation of tobacco use is also crucial (7). Approximately two-thirds of smokers want to quit smoking, but not many people eventually succeed in smoking cessation (8–10). In addition, smoking cessation rates have been remained stagnant worldwide (11–13).
South Korea has made remarkable progress in decreasing the smoking rates of adult males from 66.3% to 45% between 1998 and 2007. However, the rates in this population ranged from 43.7% to 48.3% between 2007 and 2012, which remained nearly unchanged for the six consecutive years (14). Smoking rates among adult males in Korea are much higher compared with other developed countries (e.g., the U.S. and Canada: 16.4–17.9% and 17.4–20.4%, respectively, between 2007 and 2011) (15).
Given that smoking cessation rates have remained stagnant globally, previous researchers have examined various factors that might explain smoking cessation rates. However, the majority of the studies were conducted among smokers in smoking cessation programs who may not provide an accurate portrayal of the general population (10, 16). Further, the contributing factors of smoking cessation might vary according to ethnicity/race or geography. Few studies have explored the factors associated with successful smoking cessation using community-based Korean population, but the range factors examined in the studies were somewhat limited (9, 17–20).
Therefore, this study was conducted to explore the factors that are associated with successful smoking cessation among Korean adult males using representative data from the Korea National Health and Nutrition Examination Survey (KNHANES). A comparison was made between the successful quitters and those who failed to quit after attempts to stop smoking.
Materials and Methods
Study Design, Data Source, and Participants
The present study is a secondary data analysis of the KNHANES that was conducted over a 6-year period from 2007 to 2012 by the Korea Centers for Disease Control and Prevention (KCDC). The KNHANES is an ongoing nationwide representative cross-sectional survey intended to examine the overall physical and mental health, lifestyle behaviors, and dietary habits of the South Korean general population.
The KNHANES adopted a complex stratified multistage probability-cluster sampling design based on geographical areas, age, and gender so as to minimize sampling bias. The survey comprises a health interview (e.g., health behaviors such as smoking, physical and mental symptoms, etc.), a health examination (e.g., basic blood and urine tests, etc.), and a nutritional survey (e.g., eating amounts and habits). Further information about the study design and sampling process are provided elsewhere (21, 22). The examination data from the health interviews and examinations of the 4th (2007–2009) and 5th (2010–2012) KNHANES surveys were analyzed for the current study.
A total of 47,806 individuals took part in the survey. The inclusion criteria for the participants in this study were: 1) males, 2) adults ages 19–65 years, 3) those with a smoking history of ≥ 100 cigarettes in a lifetime, and 4) those who attempted smoking cessation. We excluded: 1) those who never smoked or with a smoking history of < 100 cigarettes in a lifetime, and 2) those who never attempted smoking cessation. Consequently, 7,839 males (16.39% of the 47,806 participants) ages 19–65 years with a history of smoking ≥ 100 cigarettes in a lifetime and prior attempts to quit smoking were included in the study. Figure 1 displays the inclusion and exclusion processes and number of the study participants in the study sample.
Fig. 1.
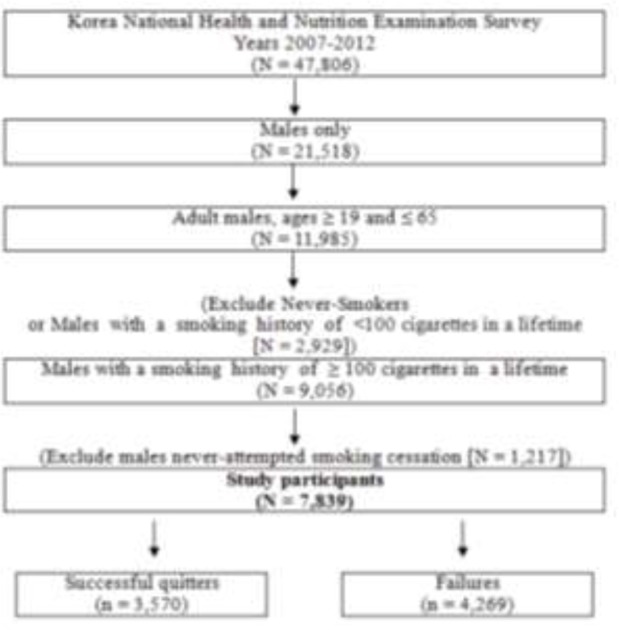
Flow diagram showing inclusion and exclusion of study participants
Ethical Considerations
The institutional review board (IRB) of the KCDC reviewed and approved the KNHANES survey annually and the IRB approval numbers were 2007-02CON-04-P, 2008-04EXP-01-C, 2009-01CON-03-2C, 2010-02CON-21-C, 2011-02CON-06-C, and 2012-01EXP-01-2C. Written informed consent was obtained from each study participant prior to the survey (21). All of the data were downloaded from the official website of the KNHANES (http://knhanes.cdc.go.kr/). These data are open to the public after completing a designated registration process for access.
Measurements and Definitions of Important General and Clinical Characteristics Smoking-related characteristics
The definitions of the participants are as follows: 1) Successful quitters in smoking cessation: those who reported a smoking history of ≥ 100 cigarettes in their lifetime, attempted smoking cessation in the past and, responded “yes” to the question, “I currently do not smoke cigarettes although I did in the past”; 2) Failed quitters (Failures) in smoking cessation: those who reported a history of ≥ 100 cigarettes in their lifetime, attempted smoking cessation in the past, and responded “yes” to the question, “I currently smoke cigarettes daily or occasionally.”
To take the history of smoking cessation, the participants were allowed to choose more than one answer to the following question, “Which of the following smoking cessation modalities did you use to quit smoking?” The possible answers included willpower (abstinence), nicotine replacement therapy (NRT) (e.g., patch or gum), prescribed oral medicines, education/counseling, and the smokers’ quit-line. Second-hand smoking exposure at the work place and home also were included as smoking-related information.
Clinical characteristics, health behaviors, perceived health status, and mental health
All of the participants’ blood samples were collected after an overnight fast (20). The medical histories (e.g., trauma history and comorbidities), health behaviors (e.g., drinking and exercise) and mental health (e.g., perceived psychological stress and depressive symptoms) were evaluated using self-report questionnaires, according to the KNHANES guidelines (21). Heavy drinkers were defined as those consuming ≥ 7 glasses of alcohol (regardless of type of the alcohol) per occasion at least ≥ 2 times per week. Moderate exercisers were defined as those exercising at a moderate level of intensity ≥ 30 minutes per session at least ≥ 5 times a week. Perceived health status was evaluated by self-reports of the level of overall health (very good/good, fair, or poor/very poor). Quality of life (QoL) was measured using the EuroQoL, which consists of both a health-status descriptive system (EQ-5D) and a visual analogue scale (EQ-VAS). The EQ-5D assesses current health status according to five dimensions (i.e., mobility, self-care, usual activities, pain/discomfort, and anxiety/depression). The final score of the EQ-5D was assessed by the EQ-5D scoring system according to three responses, including “no problems, some problems, and inability/extreme problems.” The EQ-VAS ranges from 0 to 100. Zero indicates the worst imaginable health while 100 signifies the best imaginable health (23, 24). Perceived psychological stress was defined as moderate to severe stress in daily life. Depressive symptom was defined as continuous emotional sadness and disturbance to the point of having difficulty maintaining daily activities for at least 2 weeks during the past year. Suicidal ideation was defined as thoughts of committing suicide in the past year.
Statistical Analysis
Data were analyzed using the SAS version 9.3 (SAS Institute, Inc., Cary, NC, USA). A p value < 0.05 was considered statistically significant. All of the data are presented as mean ± standard error (SE) for continuous variables or as proportions (SE) for categorical variables. T-tests and chi-square tests were performed to evaluate the differences between the groups for continuous and categorical variables, respectively. The prevalence of successful and failed quitters during the study period was presented as proportions (SE) (Table 1). Multiple logistic regression analyses were conducted to explore the associations between success of smoking cessation and various factors. The results were reported using adjusted odd ratios (ORs) and their 95% confidential interval (CI). A 95% CI that did not span 1.0 was considered statistically significant (Table 4).
Table 1.
Prevalence of successful quitters and failures between 2007 and 2012 (n = 7,839)
| Year | Successful Quitters (n = 3,570, 45.5%; Weighted N = 4,456,114) | Failures (n = 4,269, 54.5%; Weighted N = 6,285,786) | P | ||
|---|---|---|---|---|---|
| n | % (SE) | n | % (SE) | ||
| 0.243 | |||||
| 2007 | 305 | 44.7 (2.25) | 331 | 55.3 (2.25) | |
| 2008 | 701 | 42.3 (1.33) | 839 | 57.7 (1.33) | |
| 2009 | 732 | 40.0 (1.37) | 983 | 60.0 (1.37) | |
| 2010 | 627 | 39.2 (1.61) | 809 | 60.8 (1.61) | |
| 2011 | 638 | 41.2 (1.70) | 711 | 58.8 (1.70) | |
| 2012 | 567 | 43.3 (1.62) | 596 | 56.7 (1.62) | |
| Total | 3570 | 41.5 (0.65) | 4269 | 58.5 (0.65) | |
Data are presented as % (SE): P value was by chi-square.
Table 4.
Factors associated with successful smoking cessation
| Variables | Adjusted OR (95% CI) | P |
|---|---|---|
| Age (Ref, age <30 years) | ||
| 30-39 | 1.30 (1.01 - 1.68) | 0.042 |
| 40-49 | 2.02 (1.53 - 2.67) | < 0.001 |
| 50-59 | 2.83 (2.14 - 3.75) | < 0.001 |
| 60-65 | 3.73 (2.72 - 5.13) | < 0.001 |
| Marital status (Married, %) | 1.61 (1.34 -1.94) | < 0.001 |
| Income (Quartiles) (Ref, Lowest quartile) | ||
| 2 | 1.26 (1.07 - 1.50) | 0.007 |
| 3 | 1.29 (1.09 - 1.53) | 0.003 |
| 4 (Highest) | 1.54 (1.31 - 1.82) | < 0.001 |
| Smoking amount (Ref, < 10 cigarettes/day) | ||
| 10 - 19 cigarettes/day | 1.03 (0.85 - 1.23) | 0.781 |
| ≥ 20 cigarettes/day | 1.26 (1.06 - 1.49) | 0.010 |
| Second-hand smoking | ||
| Work place (Yes) | 0.98 (0.86 - 1.11) | 0.691 |
| Home (Yes) | 0.44 (0.32 - 0.62) | < 0.001 |
| Smoking cessation modes | ||
| Willpower | 1.37 (1.09 - 1.72) | 0.007 |
| NRT | 0.29 (0.23 - 0.37) | < 0.001 |
| Education or Counseling | 0.87 (0.64 - 1.18) | 0.368 |
| SBP (each 10mmHg increase) | 1.02 (0.96 - 1.10) | 0.501 |
| DBP (each 10mmHg increase) | 1.10 (1.003 - 1.21) | 0.043 |
| BMI | 1.05 (1.01 - 1.09) | 0.028 |
| Waist Circumference | 0.99 (0.98 - 1.01) | 0.410 |
| Fasting Blood Sugar (mg/dl) (each 10mg/dL increase) | 1.01 (0.98 - 1.05) | 0.537 |
| Total Cholesterol (each 10mg/dL increase) | 1.00 (0.98 - 1.02) | 0.815 |
| Heavy Drinker (Ref, Yes) | ||
| No | 1.73 (1.50 - 1.99) | < 0.001 |
| Trauma in last year (Ref, Yes) | ||
| No | 1.02 (0.82 - 1.28) | 0.856 |
| Diabetes mellitus | 0.94 (0.71-1.24) | 0.657 |
| Hypertension | 1.17 (0.98 - 1.40) | 0.084 |
| Cardiovascular disease | 1.26 (0.85 - 1.86) | 0.250 |
| Cancer | 2.25 (1.33 - 3.79) | 0.003 |
| Perceived health status (Ref, Poor/Very poor) | ||
| Very good/Good | 1.35 (1.10 - 1.66) | 0.005 |
| Fair | 1.02 (0.85 - 1.22) | 0.866 |
| EuroQoL: VAS | 1.01 (1.004 - 1.01) | < 0.001 |
| Perceived stress (Ref, Yes) | ||
| No | 1.26 (1.09 - 1.45) | 0.001 |
| Depressive symptom (Ref, Yes) | ||
| No | 1.11 (0.87 - 1.41) | 0.403 |
| Suicidal ideation (Ref, Yes) | ||
| No | 1.08 (0.85- 1.36) | 0.541 |
Multiple logistic regression analyses; Abbreviations: OR, odds ratio; CI, confidential interval; Ref, reference; DBP, diastolic blood pressure; BMI, body mass index
Results
Prevalence of Successful vs. Failed Quitters
The prevalence rates of the successful and failed quitters are presented in Table 1. The successful and failed quitters accounted for 3,570 (45.5%) and 4,269 (54.5%), respectively, of the 7,839 males who participated in the study. There were no significant differences in the prevalence rates for the 6 years from 2007 to 2012 (39.2–44.7% for success vs. 55.3%–60.0% for failure, P = 0.243).
Sociodemographic Characteristics and Smoking History of the Study Participants
The sociodemographic characteristics and smoking history of the participants according to their success or failure at smoking cessation are presented in Table 2. The successful quitters were older than the failures.
Table 2.
Sociodemographic and smoking history of study participants (n = 7,839)
| Variables Si | Successful Quitter (n = 3,570) |
Failure (n = 4,269) |
P |
|---|---|---|---|
| Age (years) | 46.19 ± 0.23 | 29.23± 0.23 | < 0.001 |
| Age group (years, %) | < 0.001 | ||
| <30 | 8.9 (0.68) | 23.0 (0.94) | |
| 30-39 | 19.2 (0.87) | 30.4 (0.86) | |
| 40-49 | 30.3 (1.02) | 25.5 (0.81) | |
| 50-59 | 28.9 (0.87) | 16.3 (0.63) | |
| 60-65 | 12.7 (0.53) | 4.8 (0.33) | |
| Married (%) | 83.8 (0.81) | 66.0 (1.02) | < 0.001 |
| Education level (%) | 0.871 | ||
| ≤ High school | 62.5 (1.08) | 62.7 (0.90) | |
| University | 37.5 (1.08) | 37.3 (0.90) | |
| Currently unemployed (%) | 84.8 (0.75) | 84.2 (0.76) | 0.517 |
| Employment types (full-time, %) | 93.5 (0.84) | 90.7 (0.76) | 0.009 |
| Employment types (%) | 0.007 | ||
| Weekdays | 84.3 (0.84) | 81.4 (0.77) | |
| Others (weekend, nighttime) | 15.7 (0.84) | 18.6 (0.77) | |
| Living place (rural, %) | 17.8 (1.33) | 17.2 (1.30) | 0.579 |
| Household income (quartiles) | < 0.001 | ||
| 1 Lowest (% in quartile) | 20.5 (0.84) | 28.2 (0.93) | |
| 2 | 26.4 (0.91) | 25.4 (0.79) | |
| 3 | 26.4 (0.85) | 24.5 (0.80) | |
| 4 Highest | 26.7 (0.98) | 21.9 (0.86) | |
| Lifetime smoking amount (pack year) | 16.96 ± 0.33 | 17.20 ± 0.26 | 0.561 |
| Cigarette smoking amount (%) | < 0.001 | ||
| < 10 Cigarettes/day | 13.4 (0.66) | 14.9 (0.62) | |
| 10 - 19 Cigarettes/day | 35.5 (0.94) | 41.3 (0.89) | |
| ≥ 20 Cigarettes/day | 51.5 (0.92) | 43.7 (0.90) | |
| Second-hand smoking (%) | |||
| Work place (yes) | 57.7 (1.01) | 55.5 (0.93) | 0.003 |
| Home (yes) | 3.2 (0.37) | 9.0 (0.56) | < 0.001 |
| Smoking cessation modes (%) | |||
| Willpower | 91.8 (0.55) | 82.8 (0.64) | < 0.001 |
| NRT | 5.7 (0.46) | 19.1 (0.68) | < 0.001 |
| Prescribed oral medicines | 0.6 (0.14) | 0.8 (0.15) | 0.448 |
| Education or Counseling | 3.8 (0.38) | 6.8 (0.43) | < 0.001 |
| Smokers’ quitline. | 0.3 (0.13) | 0.5 (0.11) | 0.237 |
Data are presented as mean ± standard error (SE) or % (SE); T-test or chi-square test was adopted for continuous or categorical variables, respectively; Smoking cessation modes = Multiple selection were allowed; Abbreviation: BMI, body mass index; WC, waist circumference; NRT, nicotine replacement therapy; Income quartiles are age and gender adjusted
The successful quitters were also more likely to be married, have full-time/weekday employment, and have a higher income compared to the failures. For the smoking cessation methods, the more successful quitters chose willpower (successful quitters vs. failures: 91.8% vs. 82.8%, P < 0.001) while more failures chose NRT (successful quitters vs. failures: 5.7% vs. 19.1%, P < 0.001) and education/counseling (successful quitters vs. failures: 3.8% vs. 6.8%, P < 0.001).
Clinical Characteristics, Health Behaviors, and Perceived and Mental Health of the Study Participants
Table 3 displays the differences in clinical characteristics, health behaviors, and mental health between the successful quitters and failures. Blood pressure, BMI, waist circumference, fasting blood sugar, and total cholesterol were more likely to be higher in the successful quitters compared to the failures. In addition, comorbidities of DM, HTN, CVD, and cancer were reported to be higher in the successful quitters. However, the failures were more likely to have trauma history (P = 0.016), and be heavy drinkers (P < 0.001). Perceived health status and QoL (EQ-VAS) were higher in the successful quitters while perceived stress, depressive symptoms, and suicidal ideation were higher in the failures.
Table 3.
Comparison of health behaviors, mental health, and medical conditions between successful quitters and failures (n = 7,839)
| Variables | Successful Quitter (n = 3,570) | Failure (n = 4,269) | P |
|---|---|---|---|
| SBP (mmHg) | 120.13 ± 0.32 | 116.40 ± 0.27 | < 0.001 |
| DBP (mmHg) | 80.09 ± 0.22 | 77.78 ± 0.22 | < 0.001 |
| BMI (kg/m2) | 24.49 ± 0.06 | 24.12 ± 0.06 | < 0.001 |
| Waist circumference (cm) | 85.42 ± 0.17 | 84.02 ± 0.18 | < 0.001 |
| Fasting blood sugar (mg/dL) | 100.75 ± 0.45 | 96.85 ± 0.40 | < 0.001 |
| Total cholesterol (mg/dL) | 190.84 ± 0.71 | 187.75 ± 0.70 | 0.002 |
| Diabetes mellitus (%) | 10.9 (0.62) | 7.4 (0.47) | < 0.001 |
| Hypertension (%) | 31.5 (0.89) | 19.8 (0.75) | < 0.001 |
| CVD (%) | 3.7 (0.37) | 1.8 (0.22) | < 0.001 |
| Cancer (%) | 2.1 (0.25) | 0.6 (0.14) | < 0.001 |
| Trauma history (%) | 7.6 (0.56) | 9.3 (0.53) | 0.016 |
| Heavy drinker (%) | 21.6 (0.84) | 31.1 (0.84) | < 0.001 |
| Moderate physical exerciser (%) | 11.9 (0.64) | 11.9 (0.59) | 0.932 |
| Perceived health status (%) | < 0.001 | ||
| Very good/Good | 43.6 (0.98) | 36.7 (0.90) | |
| Fair | 42.7 (1.01) | 48.8 (0.94) | |
| Poor/Very poor | 13.7 (0.67) | 14.5 (0.63) | |
| EQ-5D | 0.97 ± 0.001 | 0.97 ± 0.002 | 0.351 |
| EuroQoL: VAS | 77.22 ± 0.31 | 74.70 ± 0.28 | < 0.001 |
| Perceived psychological stress (%) | 23.3 (0.80) | 31.6 (0.86) | < 0.001 |
| Depressive symptom (%) | 8.3 (0.54) | 10.5 (0.55) | 0.006 |
| Suicidal ideation (%) | 8.5 (0.54) | 10.7 (0.54) | 0.006 |
Data presented as mean ± standard error (SE) or % (SE). Abbreviations: SBP, systolic blood pressure; DBP, diastolic blood pressure; BMI, body mass index; CVD, cardiovascular disease; VAS, visual analogue scale. Diabetes mellitus (DM): a fasting blood sugar ≥ 126 mg/dL, currently on oral hypoglycemic agents or insulin injection; Hypertension (HTN): a systolic blood pressure (SBP) ≥ 140 mmHg, a diastolic blood pressure (DBP) ≥ 90 mmHg, or taking antihypertensive medications; Cardiovascular disease (CVD): having a medical history of angina pectoris, myocardial infarction or stroke; Cancer: having a medical history of any type of cancer; Trauma history: having a medical history of at least ≥ 1 accident or intoxication requiring hospitalization and/or emergency room treatment during the past year
Factors Associated with Smoking Cessation Success
Table 4 presents the various factors associated with success in smoking cessation. The factors that were significantly associated with the rate of success were age, income, second-hand smoke, smoking cessation methods (i.e., willpower and use of NRT), DBP, BMI, perceived health status, heavy drinker, EQ-VAS, perceived stress, and cancer diagnosis, after controlling for the significant variables reported in Tables 2 and 3. In particular, the likelihood of success in smoking cessation was higher in people who were older (i.e., 60 to 65 years compared with those younger than 30 years of age; OR = 3.73; 95% CI 2.72–5.13), had a higher income (OR = 1.54, 95% CI 1.31–1.82), smoked a larger amount of cigarettes daily (≥ 20 cigarettes/day compared with < 10 cigarettes/day; OR = 1.26; 95% CI 1.06–1.49), used willpower for smoking cessation (OR = 1.37; 95% CI 1.09– 1.72), had a cancer history (OR = 2.25; 95% CI 1.33–3.79), and had low perceptions of stress (OR = 1.26; 95% CI 1.09–1.45) (See Table 4). On the other hand, the likelihood of succeeding in smoking cessation was lower in people who were exposed to second-hand smoke at home (OR = 0.44; 95% CI 0.32–0.62) and used NRT for smoking cessation (OR = 0.29; 95% CI 0.29–0.37).
Discussion
The purpose of this study was to explore the potential factors that are associated with success in smoking cessation by comparing the successful quitters to the failures among adult males using South Korea’s nationally representative database. Self-reports of tobacco smoking by Korean females are not reliable as there is social prejudice against Korean women who smoke (25). Therefore, we decided to focus on male smokers in this study.
Our study’s findings can be summarized as follows: 1) smoking cessation rates have not improved significantly during the 6-year study period; 2) factors significantly associated with success in smoking cessation were older age, marriage, higher income, larger amount of cigarettes smoked prior to the cessation attempt, use of willpower for smoking cessation, non-heavy drinking, cancer diagnosis and other comorbidities, perception of good health status, higher levels of QoL, and not being under psychological stress. However, second-hand smoke exposure at home and using NRT among various smoking cessation modalities were significantly associated with a lower likelihood of smoking cessation.
Previous researchers have examined various factors that might predict smoking cessation rates. A few studies have reported a significant relationship between lower socioeconomic statuses, higher rates of tobacco use, and unsuccessful quit attempts (16, 26–30). Our study also confirmed that those with higher income were more likely to succeed in smoking cessation. We also observed a significant association between successful smoking cessation and older age (16, 18, 27), and marital status (18), which was consistent with the findings of other studies.
Our study reported higher prevalence of having comorbidities, in particular cancers, among successful quitters. Having cancer increased the likelihood of success in smoking cessation to 2.25 times (95% CI = 1.33–3.79). It has been previously reported that cancer survivors are more likely to have healthier behaviors leading to smoking cessation (31–33). Therefore, we can only speculate that the comorbidities might have provided our study population with a stronger motivation to quit.
Previous studies have reported that lower levels of cigarette consumption (16, 27) were associated with higher success rates of smoking cessation. However, our report found that those who successfully quit reported higher levels of daily cigarette consumption (≥ 20 cigarettes/day) in the past. As stated above, we observed that comorbidities such as cancer could have contributed to smoking cessation in our study population. Thus, it is possible that a higher prevalence of major comorbidities in heavier smokers will have conferred to a stronger motivation to quit. Indeed, we observed significantly higher prevalence of DM, hypertension, cardiovascular disease and cancer among heavier smokers in this study population (Data not shown).
In the present study, successful quitters reported having used willpower (successful quitters, 91.8% vs. failures, 82.8%, P < 0.001) more often to quit smoking compared to failures who used NRT (failures, 19.1% vs. successful quitters, 5.7%, P < 0.001) and education/counseling (failures, 6.8% vs. successful quitters, 3.8%, P < 0.001). It was found that NRT, such as the patch or gum, was the major smoking cessation mode chosen among the various pharmaceutical modes by Koreans between 2005 and 2011 according to a study using national data (34). The use of NRT has increased the likelihood of tobacco cessation by 50–70% in other studies (35, 36). However, our study found that the participants who used NRT were less likely to succeed in smoking cessation (OR = 0.29, CI = 0.23–0.37), which is somewhat contradictory to previous reports. The smoking relapse of NRT users is frequently compared to that of those who tried to quit by using the cold-turkey method (37). At this time, we do not have historical information on whether the successful quitters tried NRT or were aware of the advantages of using NRT before using the cold turkey method as a final attempt to quit. It will be beneficial to know whether this pattern of smoking cessation seen in our participants may be attributed to their Korean ethnicity with its unique cultural characteristics.
Our study also found that people exposed to secondhand smoke at home were less likely to quit smoking compared to those without exposure to secondhand smoke. This finding is similar to a recent study (10) who reported that smoking cessation was less likely to occur among workers frequently exposed to smokers at work or home.
Kahler et al. (38) found that males who were heavy drinkers (at least 5 drinks for more than once a week) had lower rates of smoking cessation. Our finding that people who are not heavy drinkers were 1.73 times (95% CI = 1.50-1.99) more likely to succeed in smoking cessation is consistent with previous studies.
Perceived stress and continuous smoking cessation were negatively associated (39–41). Our study results also indicated that less stress was associated with successful smoking cessation, but we are not able to confirm whether better mental health was the consequence of smoking cessation or a contributor to it.
In sum, the findings of our study are in agreement with others in that we found multiple factors were involved in successful smoking cessation, such as older age, higher income, being married, having a smoke-free environment, abstinence from alcohol, and better stress management. In contrast to previous studies, using will power to quit smoking, and higher levels of cigarette consumption were associated with successful smoking cessation in the adult males in our study.
The strength of our study is that we examined a broader spectrum of potential contributors to successful smoking cessation than most of the previous studies among a homogenous population in terms of its race/ethnicity and geography. However, this study also has several limitations. First, a cause-effect relationship cannot be inferred from our study results due to the nature of cross-sectional studies; therefore, determining cause-effect relationships would require future studies. Second, the data on the duration of smoking abstinence was not available. Given the high relapse rate of cigarette smoking, future studies using follow-up or longitudinal approaches may be needed for further verification of our study’s results. Finally, the generalization of our study’s findings may be somewhat limited, given the homogeneity of our study participants in terms of geography, gender, and ethnicity/race. This limitation can be addressed in future studies using more diverse populations.
Conclusion
A smoke-free environment, use of willpower and abstinence from alcohol are crucial to the success of smoking cessation, but different strategies to help in this effort may need to be tailored to an individual’s geography, gender, and ethnicity/race. Our study findings will be helpful in developing effective strategies and/or intervention programs for smoking cessation.
Acknowledgements
The authors declare that there is no conflict of interests.
References
- Kulik MC, Menvielle G, Eikemo TA et al. (2013). Educational Inequalities in Three Smoking-Related Causes of Death in 18 European Populations. Nicotine Tob Res, [Epub ahead of print]. doi: 10.1093/ntr/ntt175. [DOI] [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL (2004). Actual causes of death in the United States, 2000. JAMA, 291: 1238–1245. [DOI] [PubMed] [Google Scholar]
- Mishra GA, Pimple SA, Shastri SS (2012). An overview of the tobacco problem in India. Indian J Med Paediatr Oncol, 33(3): 139–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He Y, Jiang B, Li LS, Li LS, Sun DL, Wu L, Liu M, He SF, Liang BQ, Hu FB, Lam TH (2014). Changes in Smoking Behavior and Subsequent Mortality Risk During a 35-Year Follow-up of a Cohort in Xi’an, China. Am J Epidemiol, 179: 1060–1070. [DOI] [PubMed] [Google Scholar]
- Ezzati M, Lopez AD (2003). Estimates of global mortality attributable to smoking in 2000. Lancet, 362: 847–852. [DOI] [PubMed] [Google Scholar]
- Barnum H (1994). The economic burden of the global trade in tobacco. Tobacco Control, 3(4): 358–361. [Google Scholar]
- Gellert C. Schottker B, Brenner H (2012). Smoking and all-cause mortality in older people: systematic review and meta-analysis. Arch Intern Med, 172: 837–844. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) (2011). Quitting Smoking among Adults--United States, 2001. –2010. MMWR (Morbidity and Mortality Weekly Reports), 60(44): 1513–1519. [PubMed] [Google Scholar]
- Liu F (2010). Quit attempts and intention to quit cigarette smoking among medicalrecipients in the USA. Public Health, 124: 553–558. [DOI] [PubMed] [Google Scholar]
- Yong LC, Luckhaupt SE, Calvert GM (2014). Quit interest, quit attempt and recentcigarette smoking cessation in the US working population. Occup Environ Med, doi: 10.1136/oemed-2013-101852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter MJ, Alberg AJ, Gray KM, Saladin ME (2010). Motivating the unmotivated for health behavior change: a randomized trial of cessation induction for smokers. Clin Trials, 7: 157–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter MJ, Hughes JR, Gray KM, Wahlquist AE, Saladin ME, Alberg AJ (2011). Nicotine therapy sampling to induce quit attempts among smokers unmotivated to quit: a randomized clinical trial. Arch Intern Med, 171: 1901–1907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jardin BF, Carpenter MJ (2012). Predictors of quit attempts and abstinence among smokers not currently interested in quitting. Nicotine Tob Res, 14(10): 1197–1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korea Centers for Disease Control and Prevention (KCDC) (2013). The statistical report on health behaviors and chronic illnesses 2012. Available:: https://knhanes.cdc.go.kr/knhanes/index.do [Accessed 6April2014].
- Korean Statistical Information Service (2013). International smoking rates 1990-2012. Available: http://kosis.kr/statHtml/statHtml.do?orgId=101&blId=DT_2IK\AC04&conn_path=I3 [Accessed 6April2014].
- Monsó E, Campbell J, Tønnesen P, Gustavsson G, Morera J. (2001). Sociodemographic predictors of success in smoking intervention. Tobacco Control, 10(2): 165–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corsi DJ, Subramanian S, Lear SA, Teo KK, Boyle MH, Raju PK, Joshi R, Neal B, Chow CK (2013). Tobacco use, smoking quit rates, and socioeconomic patterning among men and women: a cross-sectional survey in rural Andhra Pradesh, India. Eur J Prev Cardiol, [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- Lee CW, Kahende J (2007). Factors associated with successful smoking cessation in the United States, 2000. Am J Public Health, 97(8): 1503–1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid JL, Hammond D, Boudreau C, Fong GT, Siahpush M; ITC Collaboration (2010). Socioeconomic disparities in quit intentions, quit attempts, and smoking abstinence among smokers in four western countries: findings from the International Tobacco Control Four Country Survey. Nicotine Tob Res, 12 Suppl: S20–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West R, McEwen A, Bolling K, Owen L (2001). Smoking cessation and smoking patterns in the general population: a 1-year follow-up. Addiction, 96(6): 891–902. [DOI] [PubMed] [Google Scholar]
- Korea Centers for Disease Control and Prevention (KCDC) (2014). The work-shop report and guide to the utilization of the data from the Korea National Health and Nutrition Examination Survey. Available from: https://knhanes.cdc.go.kr/knhanes/index.do [Accessed 1April2014].
- Kim Y, Cho W, Evangelista, LS (2013). Effect of Second-Hand Smoke Exposure on Lung Function among Non-Smoking Korean Women. Iran J Public Health, 42(12): 1363–1373. [PMC free article] [PubMed] [Google Scholar]
- Rabin R, de Charro F (2001). EQ-5D: a measure of health status from the EuroQol Group. Ann Med, 33: 337–343. [DOI] [PubMed] [Google Scholar]
- The EuroQoL Group. (1990). EuroQoL--a new facility for the measurement of health-related quality of life. Health Policy, 16(3): 199–208. [DOI] [PubMed] [Google Scholar]
- Kang HG, Kwon KH, Lee IW, Jung B, Park EC, Jang SI (2013). Biochemically-verified smoking rate trends and factors associated with inaccurate self-reporting of smoking habits in Korean women. Asian Pac J Cancer Prev, 14(11): 6807–6812. [DOI] [PubMed] [Google Scholar]
- Hiscock R, Bauld L, Amos A, Fidler JA, Munafo M (2012). Socioeconomic status and smoking: a review Ann N Y Acad Sci, 1248: 107–123. [DOI] [PubMed] [Google Scholar]
- Hymowitz N, Cummings KM, Hyland A, Lynn WR, Pechacek TF, Hartwell TD (1997). Predictors of smoking cessation in a cohort of adult smokers followed for five years. Tob Contro, 6(Suppl 2): S57–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagelhout GE, de Korte-de D. Boer D, Kunst AE, van der Meer RM, de Vries H, van Gelder BM, Willemsen MC (2012). Trends in socioeconomic inequalities in smoking prevalence, consumption, initiation, and cessation between 2001 and 2008 in the Netherlands. Findings from a national population survey. BMC Public Health, 12: 303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siahpush M, Borland R (2001). Sociodemographic variations in smoking status among Australians aged ≥ or = 18: multivariate results from the 1995 National Health Survey. Aust N Z J Public Health, 25: 438–442. [PubMed] [Google Scholar]
- Thakur JS, Prinja S, Bhatnagar N, Rana S, Sinha DN (2013). Socioeconomic inequality in the prevalence of smoking and smokeless tobacco use in India. Asian Pac J Cancer Prev, 14: 6965–6969. [DOI] [PubMed] [Google Scholar]
- Burke L, Miller LA, Saad A, Abraham J (2009). Smoking behaviors among cancer survivors: an observational clinical study. J Oncol Pract, 5(1): 6–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh MG, Han MA, Park J, Ryu SY, Park CY, Choi SW (2013). Health behaviors of cancer survivors: the Fourth Korea National Health and Nutrition Examination Survey (KNHANES IV 2007-09). Jpn J Clin Onco, 43: 981–987. [DOI] [PubMed] [Google Scholar]
- Yang HK, Shin DW, Park JH, Kim SY, Eom CS, Kam S, Choi JH, Cho BL, Seo HG (2013). The association between perceived social support and continued smoking in cancer survivors. Jpn J Clin Onco, 43: 45–54. [DOI] [PubMed] [Google Scholar]
- Shin DW Suh B, Chun S, Cho J, Yoo SH, Kim SJ, Oh B, Cho B (2013). The prevalence of and factors associated with the use of smoking cessation medication in Korea: trend between 2005-2011. PloS one, 8: e74904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stead LF, Perera R, Bullen C, Mant D, Hartmann-Boyce J, Cahill K, Lancaster T (2012). Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev, 11: CD000146. [DOI] [PubMed] [Google Scholar]
- Zhu S, Melcer T, Sun J, Rosbrook B, Pierce JP (2000). Smoking cessation with and without assistance: a population-based analysis. Am J Prev Med, 18: 305–311. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Shiftman S, Callas P, Zhang J (2003). A meta-analysis of the efficacy of over-the-counter nicotine replacement. Tob Control, 12: 21–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler CW, Borland R, Hyland A, McKee SA, O’Connor RJ, Fong GT, Cummings KM (2010). Quitting smoking and change in alcohol consumption in the International Tobacco Control (ITC) Four Country Survey. Drug Alcohol Depend, 110: 101–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- al’Absi M (2006). Hypothalamic-pituitary-adrenocortical responses to psychological stress and risk for smoking relapse. Int J Psychophysiol, 59: 218–227. [DOI] [PubMed] [Google Scholar]
- Carey MP, Kalra DL, Carey KB, Halperin S, Richards CS (1993). Stress and unaided smoking cessation: a prospective investigation. J Consult Clin Psychol, 61: 831–838. [DOI] [PubMed] [Google Scholar]
- Piper ME, Kenford S, Fiore MC, Baker TB (2012). Smoking cessation and quality of life: changes in life satisfaction over 3 years following a quit attempt. Ann Behav Med, 43: 262–270. [DOI] [PMC free article] [PubMed] [Google Scholar]


