Abstract
Statement of problem
Preparation designs and ceramic thicknesses are key factors for the long-term success of minimally invasive premolar partial coverage restorations. However, only limited information is presently available on this topic.
Purpose
The aim of this in vitro study was to evaluate the fracture resistance and failure modes of ceramic premolar partial coverage restorations with different preparation designs and ceramic thicknesses.
Material and methods
Caries-free human premolars (n= 144) were divided into 9 groups. Palatal onlay preparation comprised reduction of the palatal cusp by 2 mm (Palatal-Onlay-Standard), 1 mm (Palatal-Onlay-Thin), or 0.5 mm (Palatal-Onlay-Ultra-Thin). Complete-coverage onlay preparation additionally included the buccal cusp (Occlusal-Onlay-Standard; Occlusal-Onlay-Thin; Occlusal-Onlay-Ultra-Thin). Labial surface preparations with chamfer reductions of 0.8 mm (Complete-Veneer-Standard), 0.6 mm (Complete-Veneer-Thin) and 0.4 mm (Complete-Veneer-Ultra-Thin) were implemented for complete veneer restorations. Restorations were fabricated from a pressable lithium-disilicate ceramic (IPS-e.max-Press) and cemented adhesively (Syntac-Classic/Variolink-II). All specimens were subjected to cyclic mechanical loading (F= 49 N, 1.2 million cycles) and simultaneous thermocycling (5°C to 55°C) in a mouth-motion simulator. After fatigue, restorations were exposed to single-load-to-failure. Two-way ANOVA was used to identify statistical differences. Pair-wise differences were calculated and P-values were adjusted by the Tukey–Kramer method (α= .05).
Results
All specimens survived fatigue. Mean (SD) load to failure values (N) were as follows: 837 (320/Palatal-Onlay-Standard), 1055 (369/Palatal-Onlay-Thin), 1192 (342/Palatal-Onlay-Ultra-Thin), 963 (405/Occlusal-Onlay-Standard), 1108 (340/Occlusal-Onlay-Thin), 997 (331/Occlusal-Onlay-Ultra-Thin), 1361 (333/Complete-Veneer-Standard), 1087 (251/Complete-Veneer-Thin), 883 (311/Complete-Veneer-Ultra-Thin). Palatal-onlay restorations revealed a significantly higher fracture resistance with ultra-thin thicknesses than with standard thicknesses (P=.015). Onlay restorations were not affected by thickness variations. Fracture loads of standard complete veneers were significantly higher than thin (P=.03) and ultra-thin (P<.001) restorations.
Conclusions
In this in vitro study, the reduction of preparation depth to 1.00 and 0.5 mm did not impair fracture resistance of pressable lithium-disilicate ceramic onlay restorations but resulted in lower failure loads in complete veneer restorations on premolars.
INTRODUCTION
The use of tooth colored, ceramic restorative materials has increased significantly in the last decade.1 With the development and improvement of reliable adhesive bonding techniques, minimally invasive dentistry became a field of great interest in modern restorative dentistry. Preserving tooth structure is critical for the longevity of teeth and restorations.2-4 Therefore various treatment concepts such as defect-oriented veneer restorations evolved for the anterior dentition.5,6 However, for compromised teeth in the posterior dentition, minimally invasive dentistry is most commonly associated with direct composite resin restorations.7
Reports on preparation guidelines for indirect ceramic posterior partial coverage restorations remain sparse. Minimal ceramic thicknesses ranging from 1.5 mm to 2 mm are recommended by most manufacturers.8,9 However, these thickness requirements are mostly based upon the results of laboratory tests with limited clinical evidence.8 Increased ceramic thicknesses with corresponding tooth structure removal is recommended to prevent restoration fracture failure.10 However, when extensive amounts of tooth structure have been destroyed by caries, attrition, or erosion, preservation of the remaining tooth structure is crucial.11 A direct correlation of strength degradation with increased tooth structure removal has been well documented.12 Moreover, cusp stiffness is significantly impaired by cavity preparation.13,14 As a consequence, traditional restorative treatment concepts for posterior teeth often aimed to strengthen the tooth/restoration complex by extending preparation designs from inlay and partial coverage onlay to complete-coverage onlay or crown restorations at the expense of the remaining tooth structure.15,16 Due to the weakness of extensively prepared teeth, fracture failures of these restorations involve the restoration and underlying tooth structure and are most commonly reported as catastrophic.17,18 Moreover tooth vitality is jeopardized by these extensive complete-coverage crown preparation designs.19
Quantitative analyses of various preparation designs have shown that the amount of tooth structure removal from onlay and partial crown preparation configurations in posterior teeth can be reduced by more than 40% as compared to complete coverage crown preparation.20 Therefore further preparation design modifications in the form of posterior complete veneer restorations with buccal surface coverage and chamfer margin have evolved.10
Available long-term clinical data on ceramic partial coverage restorations have revealed that ceramic bulk fracture is still the most common complication, despite ceramic thicknesses of at least 1.5 mm.10,21-23 However it should be noted that low strength ceramic materials such as feldspathic or leucite-reinforced glass ceramics have been used in most of these studies.10,22,24,25
More recently, ceramic systems such as lithium-disilicate glass ceramics have been developed for the fabrication of partial coverage restorations and have demonstrated increased fracture resistance.26 While short-term and medium-term clinical data on lithium-disilicate restorations are promising, long-term data are still sparse.27,28
Some authors have reported satisfactory clinical long-term results for ceramic restorations even with minimal ceramic thicknesses ranging from 0.3 mm to 1.0 mm.29,30 However, no definitive information on the minimum ceramic thickness for posterior ceramic onlays and complete veneer restorations and its impact on fracture behavior is available. In addition, the clinical fracture failure of ceramic restorations is affected by a complex combination of factors, including cavity and restoration geometry, mechanical properties of the restoration, cementation material, and damage caused by occlusal function.31-35 Therefore, there is a need to systematically investigate the failure mechanisms of ceramic systems in laboratory studies where target parameters such as preparation designs and restoration thicknesses can be selectively tested under highly standardized conditions.
Furthermore, dental ceramics are susceptible to progressive slow crack growth36,37 and cyclic mechanical degradation.38-44 At low continuous or cyclic loads, especially in a humid environment, gradual strength degradation of the ceramic has been reported.45,46 Therefore, fatigue is a significant factor limiting the lifespan of ceramic restorations and therefore represents a prerequisite for valid in vitro testing.47
The aim of this study was to evaluate fracture resistance and failure modes of ceramic partial coverage premolar restorations made of a lithium-disilicate ceramic (IPS e.max Press) with different preparation designs and ceramic thicknesses after simulated mouth-motion fatigue. The null hypothesis was that reduction of ceramic thickness does not affect the fracture resistance of various partial coverage restorations.
MATERIAL AND METHODS
One-hundred and forty-four extracted caries and crack free human maxillary premolars were cleaned and then stored in 0.1 % thymol solution at room temperature. The Albert-Ludwig-University of Freiburg Ethics Committee ruled that approval was not needed for the use for research purposes of unidentified and pooled extracted teeth. The teeth were divided into 9 groups of 16 specimens each. Roots were covered with an artificial periodontal membrane (Anti-Rutsch-Lack; Wenko-Wenselaar GmbH & Co. KG, Hilden, Germany) at a distance of 2 mm apically from the cementoenamel junction. Subsequently all teeth were embedded into an autopolymerizing resin (Technovit 4000; Heraeus Kulzer, GmbH & Co. KG, Wernheim, Germany). Before preparation, 2 silicone impressions were made of each tooth. One impression was used as a template for the wax pattern of the ceramic restoration. The other one was sectioned in a buccolingual direction to control tooth structure removal during preparation. Three different preparation designs with 3 different ceramic thicknesses were investigated (Fig. 1). Two faculty members of the Department of Prosthodontics at the University Freiburg performed all preparations. All teeth received a mesio-occlusal-distal inlay preparation (4573 S Expert set for ceramic inlays and partial crowns; Brasseler GmbH & Co. KG, Lemgo, Germany). The depth of the isthmus was 3 mm with a width of 2 mm. Mesial and distal rounded box forms were prepared to a depth of 1 mm above the cementoenamel junction. Preparation depths were controlled with silicone keys and measured with a periodontal probe (Probe UNC# 12 hdl#6; Hu-Friedy, Tuttlingen, Germany)
Fig. 1.
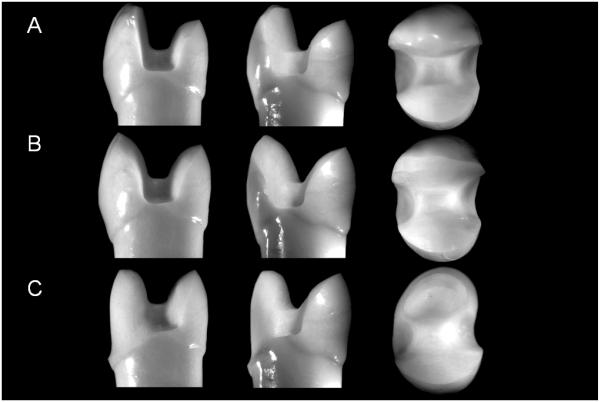
Representative photographs of preparation designs in mesial, proximal, and occlusal views. A, Palatal Onlay. B, Occlusal Onlay. C, Complete Veneer.
The palatal onlay preparation included reducing the palatal cusp by 2 mm for Palatal Onlay Standard, 1 mm for Palatal Onlay Thin, and 0.5 mm for Palatal Onlay Ultra-Thin restorations. The complete-coverage onlay preparation comprised the reduction of the palatal and buccal cusp by 2 mm (Onlay Standard), 1 mm (Onlay Thin), or 0.5 mm (Onlay Ultra-Thin). The preparation design for a complete veneer restoration was additionally extended to the labial surface with a chamfer reduction of 0.8 mm (Complete Veneer Standard), 0.6 mm (Complete Veneer Thin), and 0.4 mm (Complete Veneer Ultra-Thin). All internal cavity preparation angles were rounded, and all surfaces were smoothed with fine diamond rotary cutting instruments (25 μm diamond grit size,4573 S Expert set for ceramic inlays and partial crowns; Brasseler GmbH & Co. KG)
Fabrication of the ceramic restorations
Impressions were made with a vinyl polysiloxane material (Dimension Garant L, Permagum Putty soft; 3M Espe, Seefeld, Germany). All restorations were fabricated from a pressable lithium-disilicate glass ceramic (IPS e.max Press; Ivoclar Vivadent, Schaan, Liechtenstein) according to the manufacturer’s instruction. All restorations were manufactured in a commercial dental laboratory (Labor Woerner; Freiburg, Germany) by a master dental laboratory technician. Special attention was given to maintain the specific ceramic thicknesses described for each group. Restoration thickness was controlled with silicone impressions during waxing. Subsequently thicknesses were measured in wax and before cementation with a caliper (Iwanson caliper; Renfert, Hilzingen, Germany). Cross-sections of selected specimens depict tooth-structure (dentin/enamel) and restoration ratios (Fig. 2).
Fig. 2.
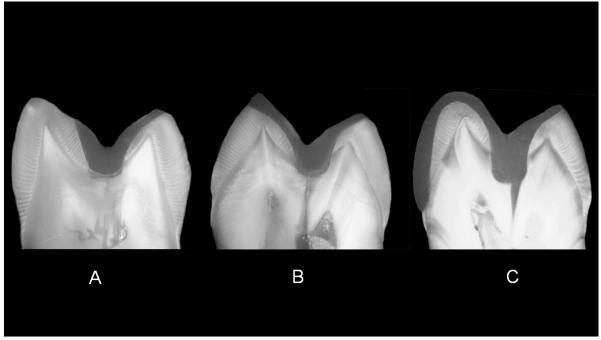
Selective cross-sections of thin restorations in various preparation designs. A, Palatal Onlay. B, Occlusal Onlay. C, Complete Veneer.
Adhesive placement of ceramic restorations
The intaglio surfaces of the restorations were etched with 4.9 % hydrofluoric acid (IPS ceramic etching gel; Ivoclar Vivadent) for 20 seconds. Etched surfaces were then thoroughly rinsed with water for 60 seconds and air dried. Subsequently a silane coupling agent (Monobond S; Ivoclar Vivadent) was applied.
Teeth were etched (30 seconds for enamel, 15 seconds for dentin) with a 37% phosphoric acid (Total Etch; Ivoclar Vivadent) and rinsed with water. Tooth surfaces were conditioned with Syntac Primer, Adhesive and Heliobond (Ivoclar Vivadent) according to the manufacturer’s instructions. All restorations were adhesively cemented with a dual-polymerizing composite resin (Variolink II; Ivoclar Vivadent). Base and catalyst paste (high viscosity) were mixed for 10 seconds and then applied to the intaglio surface of the restoration. Any excess composite resin was removed and the margins were covered with an air-inhibiting gel (Liquid Strip; Ivcolar Vivadent). The restorations were seated with finger pressure and light polymerized with a light wavelength of 480 nm and a power of 1110 mW/cm2 (Optilux 501; Kerr, Orange, Calif).
Fatigue simulation and fracture resistance test
Physiologic occlusal forces in the human mouth show a high variability among individuals and range between 10 and 120 N during mastication of food or swallowing.48-52 Therefore, a fatigue protocol with load application of 49 N was selected to represent the nominal occlusal force in the present study.
Accordingly, all specimens were exposed to dynamic loading of 1.2 million mastication cycles (Force=49 N) and 5500 thermal cycles (5°C and 55°C in water) in a computer controlled multifunctional mastication simulator (Willytec, Munich, Germany).42 A previous study showed that thermomechanical fatigue application of 1.2 million cycles was equivalent to 5 years of clinical performance.53
Cyclic fatigue testing was performed by sliding a steatite indenter (r=3 mm Steatit; Hoechst Ceram Tec AG, Wunsiedel, Germany) 0.6 mm (toward the central fissure) down the palatal cusp beginning at 0.5 mm (toward the central fissure) below the palatal cusp tip, simulating aspects of natural mastication at 1.6 Hz.42
After fatigue simulation, all specimens were loaded until fracture in a universal testing machine (Z010/TN 2S; Zwick, Ulm, Germany). The force was applied at the central fissure with a steel wedge at a cross-head speed of 0.1 mm/min until fracture. A 1-mm-thick tin foil was placed between the specimens and the steel wedge to avoid local stress concentration. The facture load values were recorded and evaluated with software (Xpert V 7.1; Zwick). For descriptive exploration of the data, boxplots were calculated and graphically displayed, stratified by group and thickness. A 2-way analysis of variance (ANOVA) was used. The continuous response variable (fracture resistance) is modeled as a function of group, thickness, and the corresponding interaction as explanatory variables. Model assumptions are graphically checked by residuals and other regression diagnostics (including Cook’s distance). Normality of error terms can be assumed. Pairwise differences of least-square means were calculated and P-values were adjusted by the Tukey-Kramer method (α=.05). All computations were performed with the statistical software (SAS system v9.1; SAS System for Unix, SAS Institute Inc, Cary, NC) by using the PROC MIXED procedure. Fractured surfaces were examined to evaluate mode of failures. Failure modes were classified as follows: (I) Extensive crack formation within the ceramic; (II) Cohesive fracture within the ceramic; (III) Fracture within the ceramic and tooth structures; (IV) Longitudinal ceramic and tooth fracture involving the root. All restorations were inspected under an optical microscope (SZH 10; Olympus Soft Imaging Solutions GmbH, Münster, Germany).
RESULTS
All specimens survived thermomechanical fatigue application. Neither cracks nor fracture failures were observed within the tooth structures or within the ceramic restorations. The results of the single load to failure test are listed in Table I.
Table I.
Load to fracture test results, in newton (N)
| Group | Minimum | Lower Quartile |
Median | Mean | Upper Quartile |
Maximum | Standard deviation |
|---|---|---|---|---|---|---|---|
| Palatal Onlay Standard |
346 | 573 | 776 | 837 | 1041 | 1472 | 320 |
| Palatal Onlay Thin |
596 | 779 | 1001 | 1055 | 1192 | 1946 | 369 |
| Palatal- onlay ultra-thin |
757 | 985 | 1108 | 1192 | 1402 | 2091 | 342 |
| Occlusal onlay standard |
481 | 672 | 814 | 963 | 1183 | 1691 | 405 |
| Occlusal Onlay Thin |
378 | 905 | 1055 | 1108 | 1343 | 1777 | 340 |
| Occlusal Onlay Ultra-Thin |
523 | 801 | 979 | 997 | 1089 | 1969 | 331 |
| Complete veneer standard |
900 | 1130 | 1300 | 1361 | 1532 | 2211 | 333 |
| Complete veneer thin |
675 | 898 | 1039 | 1087 | 1255 | 1510 | 251 |
| Complete- veneer ultra-thin |
415 | 651 | 729 | 833 | 963 | 1627 | 311 |
The overall P-values of the analysis of variance were as follows: group (P=.52), thickness (P=.54), and interaction of group and thickness (P<.001). Since the interaction was significant, a stratified analysis was performed.
Restorations with identical ceramic thickness but different preparation designs were compared and graphically displayed in box plots (Fig. 3). With standard ceramic thicknesses, complete veneer restorations showed significantly higher mean fracture loads than palatal onlays (P<.001) or occlusal onlays (P=.008). No significant differences among all preparation designs could be observed with thin ceramic thicknesses. Ultra-thin ceramic thickness palatal onlays revealed significantly higher fracture loads than complete veneers (P=.001).
Fig. 3.
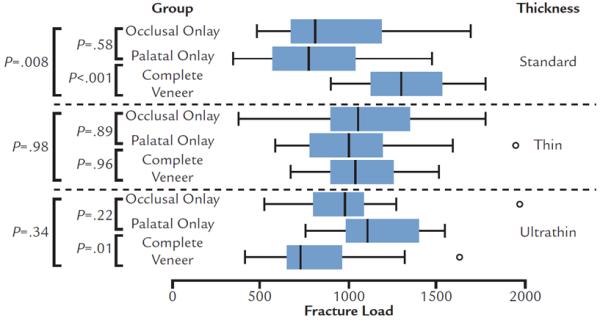
Box plots of single load to failure test results in newtons (N). Comparison of groups with identical ceramic thickness and different preparation designs.
Restorations with identical preparation design but different ceramic thicknesses were compared (Fig. 4). Palatal onlays with ultra-thin ceramic showed significantly higher mean fracture loads compared to their standard thicknesses counterparts (P=.015). Ceramic thickness had no influence on the fracture resistance of occlusal onlay restorations (P>.05). Ceramic thickness had a significant influence on the fracture resistance of the complete veneer groups. Significantly higher fracture load values were observed with standard thickness as compared to thin (P=.035) and ultra-thin restorations (P<.001).
Fig. 4.

Box plots of single load to failure test results in newtons (N). Comparison of groups with identical preparation design and different ceramic thicknesses.
Failure mode analysis after the single load to failure test are shown in Table II and depicted in Figure 5. Thin and ultra-thin palatal and occlusal onlay as well as complete veneer restorations failed predominately because of extensive crack formation within the ceramic or cohesive fractures limited to the ceramic material. Standard thickness restorations exhibited fracture failures that involved the ceramic material and the underlying tooth structure, irrespective of the preparation design. Longitudinal fractures which extended into the root were most commonly observed with the standard thickness of 2 mm.
Table II.
Failure mode description after single load to failure testing. Percent failure for each preparation design and ceramic thickness. I: Extensive crack formation within ceramic. II: Cohesive fracture within ceramic. III: Fracture within ceramic and tooth structures. IV: Longitudinal ceramic and tooth fracture involving root
| Group | Mode of failure (%) | |||
|---|---|---|---|---|
| I | II | III | IV | |
| Palatal onlay standard | 6.25 | 25.00 | 31.25 | 37.50 |
| Palatal onlay thin | 6.25 | 56.25 | 18.75 | 18.75 |
| Palatal onlay ultra-thin | 6.25 | 50.00 | 25.00 | 18,75 |
| Onlay standard | 0.00 | 12.50 | 18.75 | 68.75 |
| Onlay thin | 25.00 | 37.50 | 25.00 | 12.50 |
| Onlay ultra-thin | 43.75 | 31.25 | 18.75 | 6.25 |
| Complete veneer standard | 0.00 | 37.50 | 6.25 | 56.25 |
| Complete veneer thin | 50.00 | 31.25 | 12.50 | 6.25 |
| Complete veneer ultra-thin | 75.00 | 12.50 | 0.00 | 12.50 |
Fig. 5.
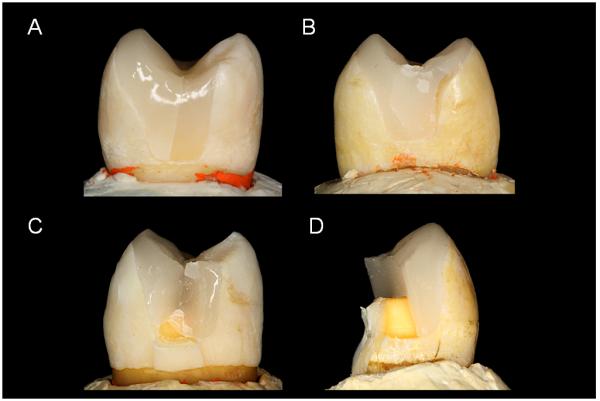
Representative photographs of failed specimens in proximal view. A, I : Extensive crack formation within the ceramic. B, II: Cohesive fracture within the ceramic. C, III: Fracture within the ceramic and tooth structures. D, IV: Longitudinal ceramic and tooth fracture involving the root.
DISCUSSION
The null hypothesis that a reduction in ceramic thickness does not affect the fracture resistance of various partial coverage restorations was partially rejected. Reduced ceramic thicknesses of 1.0 and 0.5 mm did not impair the fracture resistance of pressable lithium-disilicate ceramic onlay restorations but resulted in lower failure loads in complete veneer restorations.
Controlled indentation fatigue studies have been used to simulate basic elements of mastication and identify damage modes in monolithic ceramic systems.38 Failures in ceramic restorations can initiate from a number of different sites. Near-contact occlusal surface fracture modes, including outer and inner Hertzian cone cracks or partial cone cracks (when sliding contact occurs) (brittle mode) and micro deformation yield median radial cracks (quasiplastic mode) have been described.38-42 Far-field flexural radial fractures, initiating from the cementation surface with subsequent upward propagation and finally leading to bulk fracture of the restoration, are the prevalent failure mode of monolithic ceramics,43 especially for thin restorations (thickness < 1 mm).40 The critical load for radial crack initiation is determined by the difference in the elastic modulus between the restorative material and the cement/tooth supporting structure.44 These observations are confirmed by the present study. Palatal onlays with reduced ceramic thicknesses of 1 mm and 0.5 mm exhibited significantly higher failure loads as the supporting tooth structure was predominately enamel (Fig. 2), revealing a high modulus of elasticity relative to dentin.54 In contrast, the palatal onlay preparation with standard thickness exposed predominately dentin, providing a support of lower modulus of elasticity. This allows increased flexural tensile stresses to develop at the cementation intaglio surface during loading, putting the ceramic at higher risk of fracture.55 Minimally invasive occlusal onlay restorations showed a similar trend, which is in agreement with other studies reporting that the fracture resistance of ceramic restorations bonded with resin to enamel was higher than those bonded to dentin.25,26 Moreover, thinner, conservative occlusal veneers provide the advantage of bonding to enamel with superior bond strength than to dentin.25
Cusp coverage with partial or complete-crown preparation is commonly recommended in order to protect the weakened tooth structure.16 However, in the present study extending the preparation from a palatal onlay to a complete coverage occlusal onlay on premolars did not reveal increased failure loads. Similar results were observed in other in vitro studies32-35 and were also confirmed by clinical investigations.4,30 The benefit of the onlay preparation design can be explained by the amount of the remaining tooth structure,20 resulting in favorable distribution of stresses in teeth and reduced risk of fracture.56
Ceramic complete veneer restorations are well known as an esthetic and minimally invasive alternative for conventional complete-coverage crowns.2 In the present study the highest failure load values were observed for the complete veneer preparation design with standard ceramic thickness. However, reduction of the ceramic complete veneer thickness significantly decreased fracture resistance in premolars. This could be explained by the relatively complex restoration geometry of the complete veneer preparation design, which might have led to stress peaks at regions of geometrical changes.57 Upon occlusal loading, the bonded ceramic along the buccal veneer part is supported by both the underlying tooth structure and axial walls of the ceramic veneer. Therefore reductions in ceramic veneer thickness at the occlusal surface and axial walls result in a higher susceptibility to flexural fracture. As a consequence, thin and ultra-thin complete veneer restorations failed predominately from extensive crack or fracture failures that were limited to the ceramic restoration. Due to the limited reduction during preparation, the underlying tooth structure was only rarely involved in fracture. From a clinical perspective, these ceramic restoration failures could be readily treated by renewing the restoration.4 In contrast, catastrophic failures involving the underlying tooth structure and root, as generally observed with standard thickness restorations, would require further treatment, including endodontic treatment.58 This highlights the advantage of minimally invasive strategies, preserving the structural integrity of teeth.4
There are several limitations to this study. The results are applicable only to the ceramic and luting system and preparation designs evaluated in premolars. Moreover, the single load to failure method resulted in a distributed load and did not replicate aspects of parafunctional occlusal habits that might involve individual cusp loading.
CONCLUSIONS
Within the limitation of this in vitro fatigue study, it was concluded that:
All premolar pressed lithium-disilicate glass ceramic partial coverage restorations revealed failure loads exceeding physiologic mastication forces.
Minimal invasive ceramic thicknesses can be successful as onlay restorations in premolars.
A beneficial effect of occlusal complete-coverage compared to partial-coverage onlay restorations could not be observed with any of the investigated ceramic thicknesses.
Complex complete veneer preparation designs revealed impaired fracture resistance with thin and ultra-thin ceramic thicknesses.
Irrespective of preparation designs, reduced ceramic thickness resulted in fewer catastrophic failure modes.
CLINICAL IMPLICATIONS.
Minimally invasive onlay preparation designs on premolars appeared to be fracture resistant. However, for complete veneer restorations, reduced ceramic thicknesses can only be recommended with caution.
ACKNOWLEDGEMENT
This project was supported by Ivoclar Vivadent, and the United States National Institute of Dental and Craniofacial Research (Grant 2R01 DE017925) and the National Science Foundation (Grant CMMI-0758530) for financial support.
Footnotes
Presented at the Academy of Prosthodontics Meeting, May 12, 2012.
REFERENCES
- 1.Christensen GJ. Porcelain-fused-to-metal versus zirconia-based ceramic restorations, 2009. J Am Dent Assoc. 2009;140:1036–9. doi: 10.14219/jada.archive.2009.0316. [DOI] [PubMed] [Google Scholar]
- 2.Christensen GJ. Considering tooth-colored inlays and onlays versus crowns. J Am Dent Assoc. 2008;139:617–20. doi: 10.14219/jada.archive.2008.0224. [DOI] [PubMed] [Google Scholar]
- 3.Zitzmann NU, Krastl G, Hecker H, Walter C, Weiger R. Endodontics or implants? A review of decisive criteria and guidelines for single tooth restorations and full arch reconstructions. Int Endod J. 2009;42:757–74. doi: 10.1111/j.1365-2591.2009.01561.x. [DOI] [PubMed] [Google Scholar]
- 4.van Dijken JW, Hasselrot L. A prospective 15-year evaluation of extensive dentin-enamel-bonded pressed ceramic coverages. Dent Mater. 2010;26:929–39. doi: 10.1016/j.dental.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 5.Fradeani M, Redemagni M, Corrado M. Porcelain laminate veneers: 6- to 12-year clinical evaluation--a retrospective study. Int J Periodontics Restorative Dent. 2005;25:9–17. [PubMed] [Google Scholar]
- 6.Guess PC, Stappert CF. Midterm results of a 5-year prospective clinical investigation of extended ceramic veneers. Dent Mater. 2008;24:804–13. doi: 10.1016/j.dental.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 7.Staehle HJ. Minimally invasive restorative treatment. J Adhes Dent. 1999;1:267–84. [PubMed] [Google Scholar]
- 8.Ahlers MO, Morig G, Blunck U, Hajto J, Probster L, Frankenberger R. Guidelines for the preparation of CAD/CAM ceramic inlays and partial crowns. Int J Comput Dent. 2009;12:309–25. [PubMed] [Google Scholar]
- 9.Tsitrou EA, van Noort R. Minimal preparation designs for single posterior indirect prostheses with the use of the Cerec system. Int J Comput Dent. 2008;11:227–40. [PubMed] [Google Scholar]
- 10.Murgueitio R, Bernal G. Three-Year Clinical Follow-Up of Posterior Teeth Restored with Leucite-Reinforced IPS Empress Onlays and Partial Veneer Crowns. J Prosthodont. 2012;21:340–5. doi: 10.1111/j.1532-849X.2011.00837.x. [DOI] [PubMed] [Google Scholar]
- 11.Jaeggi T, Gruninger A, Lussi A. Restorative therapy of erosion. Monogr Oral Sci. 2006;20:200–14. doi: 10.1159/000093364. [DOI] [PubMed] [Google Scholar]
- 12.St-Georges AJ, Sturdevant JR, Swift EJ, Jr., Thompson JY. Fracture resistance of prepared teeth restored with bonded inlay restorations. J Prosthet Dent. 2003;89:551–7. doi: 10.1016/s0022-3913(03)00173-2. [DOI] [PubMed] [Google Scholar]
- 13.Magne P, Belser UC. Porcelain versus composite inlays/onlays: effects of mechanical loads on stress distribution, adhesion, and crown flexure. Int J Periodontics Restorative Dent. 2003;23:543–55. [PubMed] [Google Scholar]
- 14.Magne P, Knezevic A. Influence of overlay restorative materials and load cusps on the fatigue resistance of endodontically treated molars. Quintessence Int. 2009;40:729–37. [PubMed] [Google Scholar]
- 15.Dejak B, Mlotkowski A, Romanowicz M. Strength estimation of different designs of ceramic inlays and onlays in molars based on the Tsai-Wu failure criterion. J Prosthet Dent. 2007;98:89–100. doi: 10.1016/S0022-3913(07)60042-0. [DOI] [PubMed] [Google Scholar]
- 16.Kuijs RH, Fennis WM, Kreulen CM, Roeters FJ, Verdonschot N, Creugers NH. A comparison of fatigue resistance of three materials for cusp-replacing adhesive restorations. J Dent. 2006;34:19–25. doi: 10.1016/j.jdent.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 17.Beier US, Kapferer I, Dumfahrt H. Clinical long-term evaluation and failure characteristics of 1,335 all-ceramic restorations. Int J Prosthodont. 2012;25:70–8. [PubMed] [Google Scholar]
- 18.Stokes AN, Hood JA. Impact fracture characteristics of intact and crowned human central incisors. J Oral Rehabil. 1993;20:89–95. doi: 10.1111/j.1365-2842.1993.tb01518.x. [DOI] [PubMed] [Google Scholar]
- 19.Valderhaug J, Jokstad A, Ambjornsen E, Norheim PW. Assessment of the periapical and clinical status of crowned teeth over 25 years. J Dent. 1997;25:97–105. doi: 10.1016/s0300-5712(96)00008-5. [DOI] [PubMed] [Google Scholar]
- 20.Edelhoff D, Sorensen JA. Tooth structure removal associated with various preparation designs for posterior teeth. Int J Periodontics Restorative Dent. 2002;22:241–9. [PubMed] [Google Scholar]
- 21.Naeselius K, Arnelund CF, Molin MK. Clinical evaluation of all-ceramic onlays: a 4-year retrospective study. Int J Prosthodont. 2008;21:40–4. [PubMed] [Google Scholar]
- 22.Felden A, Schmalz G, Federlin M, Hiller KA. Retrospective clinical investigation and survival analysis on ceramic inlays and partial ceramic crowns: results up to 7 years. Clin Oral Investig. 1998;2:161–7. doi: 10.1007/s007840050064. [DOI] [PubMed] [Google Scholar]
- 23.Arnelund CF, Johansson A, Ericson M, Hager P, Fyrberg KA. Five-year evaluation of two resin-retained ceramic systems: a retrospective study in a general practice setting. Int J Prosthodont. 2004;17:302–6. [PubMed] [Google Scholar]
- 24.Smales RJ, Etemadi S. Survival of ceramic onlays placed with and without metal reinforcement. J Prosthet Dent. 2004;91:548–53. doi: 10.1016/j.prosdent.2004.03.011. [DOI] [PubMed] [Google Scholar]
- 25.Piemjai M, Arksornnukit M. Compressive fracture resistance of porcelain laminates bonded to enamel or dentin with four adhesive systems. J Prosthodont. 2007;16:457–64. doi: 10.1111/j.1532-849X.2007.00227.x. [DOI] [PubMed] [Google Scholar]
- 26.Clausen JO, Abou Tara M, Kern M. Dynamic fatigue and fracture resistance of non-retentive all-ceramic full-coverage molar restorations. Influence of ceramic material and preparation design. Dent Mater. 2010;26:533–8. doi: 10.1016/j.dental.2010.01.011. [DOI] [PubMed] [Google Scholar]
- 27.Guess PC, Strub JR, Steinhart N, Wolkewitz M, Stappert CF. All-ceramic partial coverage restorations--midterm results of a 5-year prospective clinical splitmouth study. J Dent. 2009;37:627–37. doi: 10.1016/j.jdent.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 28.Tagtekin DA, Ozyoney G, Yanikoglu F. Two-year clinical evaluation of IPS Empress II ceramic onlays/inlays. Oper Dent. 2009;34:369–78. doi: 10.2341/08-97. [DOI] [PubMed] [Google Scholar]
- 29.Malament KA, Socransky SS. Survival of Dicor glass-ceramic dental restorations over 14 years. Part II: effect of thickness of Dicor material and design of tooth preparation. J Prosthet Dent. 1999;81:662–7. doi: 10.1016/s0022-3913(99)70104-6. [DOI] [PubMed] [Google Scholar]
- 30.Frankenberger R, Taschner M, Garcia-Godoy F, Petschelt A, Kramer N. Leucite-reinforced glass ceramic inlays and onlays after 12 years. J Adhes Dent. 2008;10:393–8. [PubMed] [Google Scholar]
- 31.Rekow ED, Silva NR, Coelho PG, Zhang Y, Guess P, Thompson VP. Performance of Dental Ceramics: Challenges for Improvement. J Dent Res. 2011;90:937–52. doi: 10.1177/0022034510391795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Habekost Lde V, Camacho GB, Pinto MB, Demarco FF. Fracture resistance of premolars restored with partial ceramic restorations and submitted to two different loading stresses. Oper Dent. 2006;31:204–11. doi: 10.2341/05-11. [DOI] [PubMed] [Google Scholar]
- 33.Soares CJ, Martins LR, Fonseca RB, Correr-Sobrinho L, Fernandes Neto AJ. Influence of cavity preparation design on fracture resistance of posterior Leucite-reinforced ceramic restorations. J Prosthet Dent. 2006;95:421–9. doi: 10.1016/j.prosdent.2006.03.022. [DOI] [PubMed] [Google Scholar]
- 34.Morimoto S, Vieira GF, Agra CM, Sesma N, Gil C. Fracture strength of teeth restored with ceramic inlays and overlays. Braz Dent J. 2009;20:143–8. doi: 10.1590/s0103-64402009000200010. [DOI] [PubMed] [Google Scholar]
- 35.Cubas GB, Habekost L, Camacho GB, Pereira-Cenci T. Fracture resistance of premolars restored with inlay and onlay ceramic restorations and luted with two different agents. J Prosthodont Res. 2011;55:53–9. doi: 10.1016/j.jpor.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 36.Wiederhorn S. Influence of water vapor on crack propagation in soda-lime glass. J Am Ceram Soc. 1967;50:407–444. [Google Scholar]
- 37.Gonzaga CC, Yoshimura HN, Cesar PF, Miranda WG., Jr. Subcritical crack growth in porcelains, glass-ceramics, and glass-infiltrated alumina composite for dental restorations. J Mater Sci Mater Med. 2009;20:1017–24. doi: 10.1007/s10856-008-3667-z. [DOI] [PubMed] [Google Scholar]
- 38.Lawn BR, Deng Y, Thompson VP. Use of contact testing in the characterization and design of all-ceramic crownlike layer structures: a review. J Prosthet Dent. 2001;86:495–510. doi: 10.1067/mpr.2001.119581. [DOI] [PubMed] [Google Scholar]
- 39.Lawn B, Padture N, Cai H, Guiberteau F. Making ceramics ductile. Science. 1994;263:1114–16. doi: 10.1126/science.263.5150.1114. [DOI] [PubMed] [Google Scholar]
- 40.Bhowmick S, Zhang Y, Lawn BR. Competing fracture modes in brittle materials subject to concentrated cyclic loading in liquid environments:bilayer structures. J Mater Res. 2005;20:2792–800. [Google Scholar]
- 41.Jung YG, Wuttiphan S, Peterson IM, Lawn BR. Damage modes in dental layer structures. J Dent Res. 1999;78:887–97. doi: 10.1177/00220345990780040901. [DOI] [PubMed] [Google Scholar]
- 42.Delong R, Douglas W. Development of an artificial oral environment for the testing of dental restoratives: bi-axial force and movement control. J Dent Res. 1983;62:32–6. doi: 10.1177/00220345830620010801. [DOI] [PubMed] [Google Scholar]
- 43.Zhang Y, Kim JW, Bhowmick S, Thompson VP, Rekow ED. Competition of fracture mechanisms in monolithic dental ceramics: flat model systems. J Biomed Mater Res B Appl Biomater. 2009;88:402–11. doi: 10.1002/jbm.b.31100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lawn BR, Deng Y, Miranda P, Pajares A, Chai H, Kim D. Overview: Damage in brittle layer structures from concentrated loads. J Mater Res. 2002;17:3019–36. [Google Scholar]
- 45.Lawn B. Fracture of brittle solids. Vol. 2. Cambridge University Press; Cambride: 1993. pp. 106–12. [Google Scholar]
- 46.Zhang Y, Lawn B. Long-term strength of ceramics for biomedical applications. J Biomed Mater Res B Appl Biomater. 2004;69:166–72. doi: 10.1002/jbm.b.20039. [DOI] [PubMed] [Google Scholar]
- 47.Suttor D, Bunke K, Hoescheler S, Hauptmann H, Hertlein G. LAVA--the system for all-ceramic ZrO2 crown and bridge frameworks. Int J Comput Dent. 2001;4:195–206. [PubMed] [Google Scholar]
- 48.De Boever JA, McCall WD, Jr., Holden S, Ash MM., Jr. Functional occlusal forces: an investigation by telemetry. J Prosthet Dent. 1978;40:326–33. doi: 10.1016/0022-3913(78)90042-2. [DOI] [PubMed] [Google Scholar]
- 49.Eichner K. Evaluation of Chewing forces during mastication. Dtsch Zahnärztl Z. 1963;18:915–24. [Google Scholar]
- 50.Bates JF, Stafford GD, Harrison A. Masticatory function - a review of the literature. III. Masticatory performance and efficiency. J Oral Rehabil. 1976;3:57–67. doi: 10.1111/j.1365-2842.1976.tb00929.x. [DOI] [PubMed] [Google Scholar]
- 51.Kohyama K, Hatakeyama E, Sasaki T, Dan H, Azuma T, Karita K. Effects of sample hardness on human cheweing force: a model study using silicone rubber. Arch Oral Biol. 2004;49:805–16. doi: 10.1016/j.archoralbio.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 52.Schindler HJ, Stengel E, Spiess WE. Feedback control during mastication of solid food textures--a clinical-experimental study. J Prosthet Dent. 1998;80:330–6. doi: 10.1016/s0022-3913(98)70134-9. [DOI] [PubMed] [Google Scholar]
- 53.Kern M, Strub JR, Lu XY. Wear of composite resin veneering materials in a dual-axis chewing simulator. J Oral Rehabil. 1999;26:372–8. doi: 10.1046/j.1365-2842.1999.00416.x. [DOI] [PubMed] [Google Scholar]
- 54.Habelitz S, Marshall SJ, Marshall GW, Jr., Balooch M. Mechanical properties of human dental enamel on the nanometre scale. Arch Oral Biol. 2001;46:173–83. doi: 10.1016/s0003-9969(00)00089-3. [DOI] [PubMed] [Google Scholar]
- 55.Craig RG, Peyton FA. Elastic and mechanical properties of human dentin. J Dent Res. 1958;37:710–8. doi: 10.1177/00220345580370041801. [DOI] [PubMed] [Google Scholar]
- 56.Mondelli J, Steagall L, Ishikiriama A, de Lima Navarro MF, Soares FB. Fracture strength of human teeth with cavity preparations. J Prosthet Dent. 1980;43:419–22. doi: 10.1016/0022-3913(80)90213-9. [DOI] [PubMed] [Google Scholar]
- 57.Quinn JB, Quinn GD. A practical and systematic review of Weibull statistics for reporting strengths of dental materials. Dent Mater. 2010;26:135–47. doi: 10.1016/j.dental.2009.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Dijken JW. Resin-modified glass ionomer cement and self-cured resin composite luted ceramic inlays. A 5-year clinical evaluation. Dent Mater. 2003;19:670–4. doi: 10.1016/s0109-5641(03)00011-3. [DOI] [PubMed] [Google Scholar]


