Abstract
Purpose
Advanced lung cancer patients have high rates of multiple physical and psychological symptoms, and many of their family caregivers experience significant distress. However, little is known about strategies that these patients and their family caregivers employ to cope with physical and psychological symptoms. This study aimed to identify strategies for coping with various physical and psychological symptoms among advanced, symptomatic lung cancer patients and their primary family caregivers.
Methods
Patients identified their primary family caregiver. Individual semi-structured qualitative interviews were conducted with 21 advanced, symptomatic lung cancer patients and primary family caregivers. Thematic analysis of interview data was framed by stress and coping theory.
Results
Patients and caregivers reported maintaining a normal routine and turning to family and friends for support with symptom management, which often varied in its effectiveness. Whereas support from healthcare professionals and complementary and alternative medicine were viewed favorably, reactions to Internet and in-person support groups were mixed due to the tragic nature of participants’ stories. Several cognitive coping strategies were frequently reported (i.e., changing expectations, maintaining positivity, and avoiding illness-related thoughts) as well as religious coping strategies.
Conclusions
Results suggest that advanced lung cancer patients and caregivers may be more receptive to cognitive and religious approaches to symptom management and less receptive to peer support. Interventions should address the perceived effectiveness of support from family and friends.
Keywords: lung neoplasms, caregivers, adaptation, psychological, symptoms, complementary therapies, religion
Introduction
Lung cancer is one of the most common cancers affecting both men and women worldwide [1]. Most lung cancer patients (85%) have regional or distant stage disease at diagnosis [2], contributing to their high rate (80%) of multiple physical and psychological symptoms [3–5]. Lung cancer patients experience higher rates of anxiety and depressive symptoms and breathlessness than other cancer patients [6,7]. Research suggests that up to 52% of lung cancer patients show clinically significant anxiety and depressive symptoms [8,9] and up to 87% experience breathlessness [3,10]. Frequent and severe physical symptoms, such as pain, fatigue, and breathlessness, and psychological distress in lung cancer patients have been associated with impaired quality of life (QOL) [3,11].
Family caregivers’ QOL is also affected [9]. Studies have found that up to 50% of family caregivers of lung cancer patients report clinically elevated anxiety or depressive symptoms [9,12,13]. Greater distress among caregivers of lung cancer patients has been related to increased caregiving strain and lower self-efficacy or confidence in assisting the patient with symptom management [14,15].
Coping strategies affect patients’ and caregivers’ psychological adjustment to cancer. The theoretical framework of Lazarus and Folkman defines coping as efforts to manage adaptational demands and associated emotions [16]. Although a large literature has examined cancer patients’ coping strategies [17,18], limited research has focused on lung cancer patients. Coping strategies of lung cancer patients may differ from those of other cancer patients as they manage unique stressors, such as breathlessness [19] and the stigma associated with tobacco use [20]. Studies have found that lung cancer patients use both problem and emotion-focused coping strategies [9,21]. Several coping tendencies, including disengagement from the stressor, self-distraction, and less positive social interaction support, have been associated with poorer psychological adjustment in this population [9]. Additionally, low to moderate correlations have been found between the coping strategies of lung cancer patients and those of their caregivers [9,22]. Among lung cancer patients’ spousal caregivers, coping strategies linked to greater distress have included disengaging from the stressor, using substances, and blaming the patient for causing the cancer [9].
Although studies have provided some information regarding coping strategies used by lung cancer patients and caregivers [9,21], this research has not focused on individuals at highest risk for compromised QOL (i.e., those coping with advanced disease and moderate to severe symptoms). Furthermore, research on symptom management among lung cancer patients and caregivers has primarily examined the management of breathlessness [23] and global perceptions of physical symptoms [24], leaving gaps in our understanding of strategies employed to manage a variety of symptoms. Thus, this qualitative study aimed to identify advanced, symptomatic lung cancer patients’ and caregivers’ strategies for coping with various physical and psychological symptoms. Because little is known about this topic, qualitative methods were chosen to capture the range and complexity of coping strategies.
Materials and Methods
Recruitment
Following ethical review board approval, advanced lung cancer patients were recruited from the oncology clinic at the Indiana University Simon Cancer Center between May and September 2012. Purposive sampling was used to ensure diversity regarding patient gender and age. Patient eligibility criteria were: (1) at least 3 weeks post-diagnosis of advanced (stage III or IV) non-small cell lung cancer; (2) English fluency; (3) 18 years of age or older; (4) not receiving hospice care; and (5) at least one physical or psychological symptom of moderate severity. Symptoms of moderate severity were defined by validated cutpoints for depressive symptoms (Patient Health Questionnaire [PHQ-2] score ≥ 3 on this 0–6 scale) [25]; anxiety (GAD-2 score ≥ 3 on this 0–6 scale) [26]; pain (PEG score ≥ 5 on this 0–10 scale) [27]; fatigue (SF Vitality score ≤ 45 on this 0–100 scale) [28]; or breathlessness (Memorial Symptom Assessment Scale [MSAS] shortness-of-breath severity score ≥ 2 on this 1–4 scale) [29]. We excluded patients receiving hospice care because this study was conducted to inform interventions for patients who had not yet enrolled in hospice. Patients meeting criteria (1) through (4) were identified via medical record review and consultation with oncologists. A trained research assistant then screened patients for symptoms and obtained written informed consent during a clinic visit. Eligible patients identified and provided permission to contact their primary family caregiver (i.e., the person who provided the majority of their unpaid, informal care).
The research assistant evaluated family caregivers for eligibility (i.e., English fluency and age ≥ 18 years) and obtained their informed consent in clinic or via telephone. Each participant received $25 for completing the interview.
Data Collection
In-depth, semi-structured interviews were conducted by a master’s level qualitative methodologist. Interviews were conducted via telephone to maximize recruitment and retention. Patients and caregivers were interviewed separately to minimize response biases. Interviews ranged from 45 to 60 minutes and were digitally recorded. First, patients were asked to describe any physical symptoms that they had experienced and their strategies for coping with these symptoms. Caregivers were asked to describe the patient’s physical symptoms and their joint efforts to cope with these symptoms. The interviewer asked follow-up questions to patients and caregivers regarding the patient’s experience of pain, fatigue, and breathlessness and strategies for coping with these symptoms. Then patients and caregivers described their emotional reactions to the patient’s lung cancer and their strategies for coping with these emotions. Throughout the interview, follow-up questions were asked to obtain a detailed narrative. The interviewer was trained to respond to distress by making appropriate referrals. Patient medical information was collected from medical records.
Qualitative Data Analysis
Interviews were transcribed verbatim and imported into Atlas.ti software for thematic analysis [30]. Thematic analysis involves identifying, analyzing, and reporting patterns or themes across a data set [30]. For this study, a theoretical thematic analysis was conducted rather than an inductive one. Specifically, the analysis was framed by stress and coping theory such that the analytic goal was to identify patient and caregiver efforts to cope with physical and psychological symptoms [16]. A qualitative methodologist and a clinical psychologist specializing in psycho-oncology read all transcripts and generated initial codes. Examples of codes include “relaxation exercises,” “joining a support program,” and “thinking positive thoughts.” The researchers then independently coded the transcripts in Atlas.ti and met regularly (i.e., after the first two interviews and then every five interviews after that) to discuss the codes and reconcile differences until complete agreement was reached. At each of these meetings, the researchers jointly determined whether saturation had been reached. Next, the researchers examined interrelationships among initial codes and sorted them into higher-order theoretical codes. Examples of theoretical codes include “maintaining normalcy,” “seeking support,” and “cognitive coping strategies.” Codes were compared between patients and caregivers and within patient-caregiver dyads. Finally, the researchers checked to ensure that data within theoretical codes were consistent, and that the codes were distinguishable from one another.
Results
Sample Characteristics
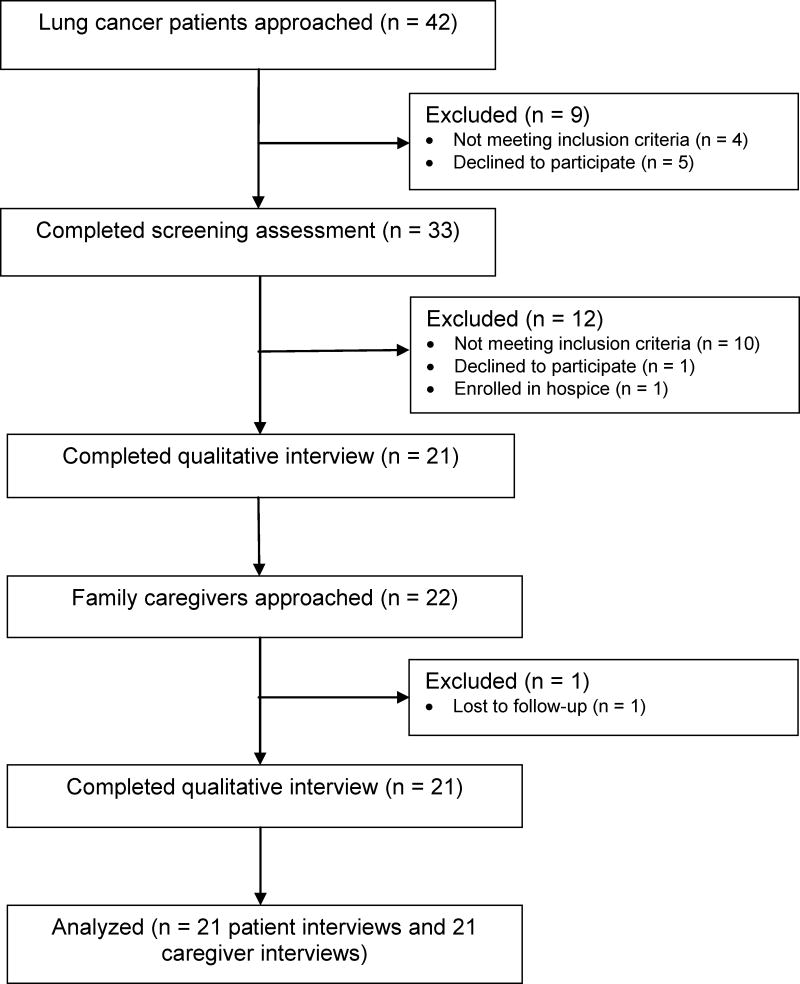
Of the 42 lung cancer patients who were approached regarding this study, four patients were found to be ineligible due to cognitive impairment, the inability to speak or read, or their disease status (see Figure 1). Of the 38 patients who were eligible to be screened for physical and psychological symptoms to determine their eligibility status, 87% (33/38) agreed to complete screening and 13% (5/38) declined to participate. Primary reasons for declining study participation were lack of interest in the study and feeling too ill to participate. Seventy percent of patients (23/33) met clinical cutoffs for significant pain, fatigue, breathlessness, anxiety, and/or depressive symptoms on standardized questionnaires. All of the symptoms were reported by a sizable percentage of the eligible sample (range = 32% for anxiety to 73% for breathlessness). Nearly all eligible patients (96%, 22/23) consented to participate in the study and permitted the research assistant to contact their primary family caregiver. One consenting patient did not complete the study interview due to hospice enrollment. Ninety-five percent of caregivers (21/22) consented to participate in this study and completed the study interview, and one caregiver could not be reached via phone. After data from 21 patients and 21 caregivers had been analyzed, the researchers determined that thematic saturation had been reached. Demographic and medical characteristics of the sample are found in Table 1.
Fig. 1.
Study schema
Table 1. Sample characteristics.
(N = 21 lung cancer patient-family caregiver dyads)
| Variable | n (%) | M (SD) | Range |
|---|---|---|---|
| Caregiver’s relationship to the patient | |||
| Spouse/partner | 12 (57%) | ||
| Adult child | 4 (19%) | ||
| Sibling | 5 (24%) | ||
| Caregiver lives with the patient | 14 (70%) | ||
| Patient sex—female | 11 (52%) | ||
| Caregiver sex—female | 15 (71%) | ||
| Patient race/ethnicity | |||
| Non-Hispanic White | 18 (86%) | ||
| African American/Black | 3 (14%) | ||
| Caregiver race/ethnicity | |||
| Non-Hispanic White | 18 (86%) | ||
| African American/Black | 3 (14%) | ||
| Patient marital status | |||
| Married or marriage equivalent | 15 (71%) | ||
| Single, divorced, or widowed | 6 (29%) | ||
| Caregiver marital status | |||
| Married or marriage equivalent | 17 (81%) | ||
| Single or divorced | 4 (19%) | ||
| Patient age (years) | 63 (12) | 39 to 80 | |
| Caregiver age (years) | 58 (12) | 38 to 78 | |
| Patient education (years) | 13 (2) | 8 to 18 | |
| Caregiver education (years) | 14 (3) | 10 to 21 | |
| Patient annual household income (median) | >$50,000 | <$21,000 to >$100,000 | |
| Caregiver annual household income (median) | >$50,000 | <$21,000 to >$100,000 | |
| Months since the patient’s lung cancer diagnosis | 15 (15) | 1 to 52 | |
| Non-small cell lung cancer stage | |||
| Stage III | 5 (24%) | ||
| Stage IV | 16 (76%) | ||
| Lung cancer treatment type | |||
| Surgery | 7 (33%) | ||
| Chemotherapy | 16 (76%) | ||
| Radiation | 6 (29%) | ||
| Chemoradiation | 4 (19%) | ||
Note. M = mean. SD = standard deviation.
Findings
Drawing upon stress and coping theory, our thematic analysis identified six types of coping strategies that patients and caregivers used to manage physical and psychological symptoms: maintaining “normalcy” (i.e., engaging in routine activities), seeking support, medication use, complementary and alternative medicine (CAM) use, cognitive coping strategies (i.e., changing expectations, maintaining a positive outlook, and avoiding thoughts about the illness), and religious coping (i.e., engaging in beliefs and practices of a specific faith) [31]. Approximately equal numbers of patients and caregivers reported using each set of coping strategies, with the exception of greater use of medication and CAM among patients (see Table 2). In addition, patient-caregiver dyads often reported similar coping strategies, except for the types of cognitive strategies employed. Each of these sets of coping strategies is described below.
Table 2.
Comparison of patient and caregiver coping strategies
| Maintaining Normalcy | Seeking Support | Medication Use | CAM Use | Cognitive Coping | Religious Coping | |
|---|---|---|---|---|---|---|
| Description | Engaging in routine activities. | Seeking instrumental and emotional support from formal and informal sources. | Taking medication for physical and psychological symptoms; using oxygen. | Engaging in breathing or other relaxation exercises; practicing yoga or Tai Chi; using herbs or homeopathic creams. | Changing expectations; maintaining a positive outlook; avoiding thoughts about the illness. | Engaging in church activities, prayer, and other religious practices. |
| Similar prevalence of coping strategy among patients and caregivers | Yes | Yes | No. Greater use among patients. | No. Greater use among patients. | Yes | Yes |
| Comparison of coping strategy within patient-caregiver dyads | Similar | Similar | Similar | Similar | Different | Similar |
Note. CAM = complementary and alternative medicine.
Maintaining “normalcy”
Maintaining a normal routine, including work, meal preparations, naps, time with family, and other enjoyable activities, was often described as the primary method of coping with emotional reactions to the illness. As one patient said,
I certainly don’t lie in the chair or on the couch all day. I … do the dishes and sweep the floors and do some of the washing, enough to keep me where I don’t feel worthless (62-year-old male patient).
Caregivers often described routine activities, such as chores and trips to visit family, as interconnected efforts to cope with their own emotions and those of the patient. As one caregiver said,
usually on the weekends he [the patient] is ready to go, go, go. I would like to stay home, but I figure if he wants to go we’re going to go. If that makes him feel better, we just get out and take a ride … that seems to help us … to keep busy (60-year-old wife of the patient).
Seeking support
Patients and caregivers also coped with various physical and psychological symptoms by seeking instrumental and emotional support from family and friends. The effectiveness of this support often varied within and across support providers. As one caregiver said,
with each person … you have to tailor what you can and can’t say to them because some can handle more and some are better at dealing with different aspects. So it is nice for me that I have such a wide range of people that I can go to and ask questions or vent to (45-year-old daughter of the patient).
Another caregiver noted the strengths and weaknesses of her husband’s support in caring for her sister:
he’s a wonderful listener and cares very much, but I don’t know that he necessarily would have the best advice about how I’m supposed to deal with this (47-year-old sister of the patient).
Patients and caregivers also described receiving formal support. Whereas support from doctors and nurses was uniformly described in a positive manner, feedback regarding Internet and in-person support groups was mixed. Some participants described harmful psychological effects of reading or listening to “extremely depressing” or “tragic” stories of other families coping with lung cancer. For example, one caregiver noted her mother’s reaction to attending an in-person support group:
we are going to forbid her from going back, because when you go to a place for support, and you come back and you’re more depressed than when you went, I … do not take that brand of support (48-year-old daughter of the patient).
Medication use
Participants reported using medication and oxygen to lessen physical and psychological symptoms. With regard to medication, patients and caregivers described efforts to monitor and adjust psychiatric and pain medication intake around the clock and ensure that prescriptions were refilled in a timely manner. In addition, oxygen was often used at night and transported to various locations with the patient to reduce not only feelings of breathlessness and fatigue, but also anxiety. As one patient stated,
I started getting an anxiety attack and reached a point where I felt like I couldn’t breathe anymore … I was breathing but I was having a hard time catching my breath. I knew a lot of it was psychological … so my doctor prescribed oxygen (63-year-old male patient).
CAM use
CAM also was used by one-third of patients and two caregivers. The most common forms of CAM were breathing and other relaxation exercises. Participants uniformly characterized these exercises as helpful for reducing anxiety or breathlessness. Other forms of CAM included yoga, Tai Chi, herbs, and homeopathic creams.
Cognitive coping strategies
Patients and caregivers reported several cognitive coping strategies, including changing their expectations, maintaining a positive outlook, and avoiding thoughts about the illness. Changes in expectations included patients’ acknowledgement of limitations in their ability to perform activities and need for accommodations. One patient described these accommodations:
I know what my limits are … I bought enough clothes to last four weeks. So I do laundry once a month … I use a lot of paper plates and things like that so I don’t have to do dishes … I used to do them every day but now, once the sink gets full, I do it and that’s just the way I’m coping with a lot of it (65-year-old male patient).
Patients and caregivers also altered their expectations regarding the future, as reflected in statements regarding the inevitability of the disease process and death:
at a certain age your life changes with each phase of getting older. It’s a matter of realizing that you’ll be spending time alone … at my age right now, I’ve seen that happen frequently. So you know what to expect (74-year-old wife of the patient).
Other patients and caregivers described their efforts to replace negative thoughts and emotions with a positive outlook. As one caregiver stated,
I’ll be thinking of something negative and I’ll just say, ‘Oh, well, it’s only temporary. Someday we’ll be back to normal again’ (59-year-old wife of the patient).
One younger patient noted the importance of gratitude:
I just tell myself that I’m lucky to be here and I’m thankful for what I have … Sometimes I feel … that I shouldn’t feel so bad because things could be worse (39-year-old female patient).
Another patient expressed the belief that positive thinking would help reduce the likelihood of illness:
I’ve heard from people that you can worry yourself sick, and I just don’t want to do that. I try to keep positive and stay around positive people that help me through this (52-year-old male patient).
Whereas some participants maintained a positive perspective, others attempted to avoid thinking about the illness. As one patient said,
I try not to think about it quite honestly. I don’t want to get into how long I have to live or anything like that (68-year-old male patient).
Religious coping
Many patients and caregivers mentioned turning to church community, prayer, and other religious activities to cope with physical symptoms and emotional reactions to the illness. The emotional comfort derived from the belief that God is in control of the future was expressed by many participants. As one patient stated,
God is going to do what’s best for me. If He thinks it’s best that I leave and go with Him, that’s His choice for me. Or if He thinks I can stay around for a while, that’s His choice for me. I’m comfortable with that. I am at peace (64-year-old female patient).
Discussion
This study provides initial information regarding strategies for coping with physical and psychological symptoms among advanced, symptomatic lung cancer patients and their primary family caregivers. Many patients described maintaining a “normal” routine to manage their emotional reactions to the illness. Patients also described cognitive coping efforts, including changing their expectations, maintaining positivity, and avoiding illness-related thoughts. Thus, symptomatic patients tended to report avoiding negative emotions rather than processing and expressing them, a finding that warrants additional study. Furthermore, the types of coping strategies employed, with the exception of cognitive coping strategies, were often comparable within patient-caregiver dyads. These findings parallel the positive correlations between lung cancer patient and caregiver coping strategies found in quantitative research [9,22]. In this study, many caregivers reported efforts to avoid negative emotions, such as distracting themselves and the patient through continual preoccupation with activities. Results converge with prior theory and research that has conceptualized “emotion work” as a key aspect of family caregiving [32]. In this study, emotion work involved efforts to simultaneously manage their own emotions and those of the patient.
Patients and caregivers often relied on family and friends for support in managing emotions and physical symptoms. Great variation in the effectiveness of this support within and across support providers was noted. Whereas most studies of cancer patients and caregivers have examined the perceived availability of social support, the perceived effectiveness of this support has rarely been documented and was negatively correlated with cancer survivors’ distress in one study [33]. The present findings suggest that a number of patients and caregivers coping with advanced lung cancer turn to a social network that collectively provides effective emotional and practical assistance. Thus, future research with this population may benefit from taking into account both the quantity and quality of support from different sources when predicting distress.
Regarding the receipt of formal support, patients and caregivers uniformly described interactions with healthcare professionals as helpful, whereas some individuals viewed Internet and in-person support groups as unhelpful due to the tragic nature of participants’ stories. To date, evidence for the psychosocial benefits of peer support in cancer populations has been mixed [34], and the uptake of support services has been low among lung and other cancer patients [35–37] and caregivers [12,38]. Given the increasing availability of peer support, its potentially helpful and harmful effects in the context of advanced lung cancer warrant further investigation.
In contrast to peer support, patients characterized CAM use, especially breathing exercises, as an effective treatment for anxiety, breathlessness, and other symptoms. CAM use was more prevalent among patients than caregivers. Given positive perceptions of CAM in the current sample and the widespread use of CAM among cancer patients [39], further research is needed to determine the prevalence and efficacy of CAM use among advanced lung cancer patients.
Many patients and caregivers, all of whom lived in a predominantly Christian area of the U.S., drew upon their religious resources to cope with physical and psychological symptoms. Participants derived emotional comfort from the belief that God was in control of their circumstances. In another qualitative study in the U.S., primarily Christian patients with advanced cancer expressed similar perceptions of God’s sovereignty [40]. However, among early-stage breast cancer survivors in the U.S., the belief that God controls one’s health was associated with greater depressive symptoms [41]. Early-stage patients might be less likely to employ religious beliefs as a coping mechanism than later stage patients. Indeed, among American lung cancer patients, having advanced disease predicted the receipt of support from clergy [36]. Future research may assess changes in religious coping efforts following an advanced lung cancer diagnosis and their association with distress across cultures.
Limitations of this study should be noted. The sample primarily consisted of Caucasian participants from the Midwestern U.S. Whether the findings are transferable to other cultural groups requires study. In addition, this study was intended as an overview of coping strategies for symptom management among advanced, symptomatic lung cancer patients and their family caregivers. Coping strategies identified in our analysis should be examined in greater depth by both qualitative and quantitative research. Conducting interviews over time would allow us to gain an understanding of changes in coping efforts as symptoms worsen.
Conclusion
The present results have important implications for future research and clinical practice. First, assessment of patients’ and caregivers’ informal support system should take into account the quantity and quality of this support, as variation in its effectiveness was noted in the current sample. Clinicians may assist those with inadequate support by connecting them to supportive resources available in their medical facility and community. Given that coping strategies were often similar within patient-caregiver dyads, holding a joint conversation with the patient and caregiver about resources may be beneficial. In addition, a recent Cochrane review found limited empirical support for non-pharmacologic interventions in lung cancer [42]. Furthermore, few studies have included both lung cancer patients and their family caregivers in the intervention [43–45]. Our results inform future intervention development by suggesting that advanced lung cancer patients and caregivers may be receptive to cognitive approaches and those that build upon their religious resources. Interventions also may aim to increase the perceived effectiveness of existing support by altering maladaptive cognitions regarding this support and enhancing communication skills. Given the high symptom burden and unique psychosocial challenges associated with lung cancer, efforts to improve lung cancer symptom management should be a high priority for future research and clinical care.
Acknowledgments
This work was supported by grant RR025761 from the National Center for Research Resources and grant K07CA168883 from the National Cancer Institute. The authors would like to thank the study participants and Heather A. Jaynes and Joseph G. Winger for their assistance.
Footnotes
Conflict of Interest: Remuneration and stock ownership in Eli Lilly, Inc. (M. Ott). The authors have full control of all primary data and agree to allow the journal to review their data if requested.
References
- 1.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.American Cancer Society. Cancer facts and figures 2014. American Cancer Society; Atlanta, GA: 2014. [Google Scholar]
- 3.Hopwood P, Stephens RJ. Symptoms at presentation for treatment in patients with lung cancer: implications for the evaluation of palliative treatment. The Medical Research Council (MRC) Lung Cancer Working Party. Br J Cancer. 1995;71:633–636. doi: 10.1038/bjc.1995.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kurtz ME, Kurtz JC, Stommel M, Given CW, Given B. Predictors of depressive symptomatology of geriatric patients with lung cancer-a longitudinal analysis. Psychooncology. 2002;11:12–22. doi: 10.1002/pon.545. [DOI] [PubMed] [Google Scholar]
- 5.Rolke HB, Bakke PS, Gallefoss F. Health related quality of life, mood disorders and coping abilities in an unselected sample of patients with primary lung cancer. Respir Med. 2008;102:1460–1467. doi: 10.1016/j.rmed.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 6.Dudgeon DJ, Kristjanson L, Sloan JA, Lertzman M, Clement K. Dyspnea in cancer patients: Prevalence and associated factors. J Pain Symptom Manage. 2001;21(2):95–102. doi: 10.1016/s0885-3924(00)00258-x. [DOI] [PubMed] [Google Scholar]
- 7.Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psychooncology. 2001;10:19–28. doi: 10.1002/1099-1611(200101/02)10:1<19::aid-pon501>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 8.Gore JM, Brophy CJ, Greenstone MA. How well do we care for patients with end stage chronic obstructive pulmonary disease (COPD)? A comparison of palliative care and quality of life in COPD and lung cancer. Thorax. 2000;55:1000–1006. doi: 10.1136/thorax.55.12.1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carmack Taylor CL, Badr H, Lee JH, Fossella F, Pisters K, Gritz ER, Schover L. Lung cancer patients and their spouses: psychological and relationship functioning within 1 month of treatment initiation. Ann Behav Med. 2008;36:129–140. doi: 10.1007/s12160-008-9062-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith EL, Hann DM, Ahles TA, Furstenberg CT, Mitchell TA, Meyer L, Maurer LH, Rigas J, Hammond S. Dyspnea, anxiety, body consciousness, and quality of life in patients with lung cancer. J Pain Symptom Manage. 2001;21(4):323–329. [Google Scholar]
- 11.Cooley ME, Short TH, Moriarty HJ. Symptom prevalence, distress, and change over time in adults receiving treatment for lung cancer. Psychooncology. 2003;12:694–708. doi: 10.1002/pon.694. [DOI] [PubMed] [Google Scholar]
- 12.Mosher CE, Champion VL, Hanna N, Jalal SI, Fakiris AJ, Birdas TJ, Okereke IC, Kesler KA, Einhorn LH, Given BA, Monahan PO, Ostroff JS. Support service use and interest in support services among distressed family caregivers of lung cancer patients. Psychooncology. 2013;22:1549–1556. doi: 10.1002/pon.3168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim Y, Duberstein PR, Sörensen S, Larson MR. Levels of depressive symptoms in spouses of people with lung cancer: Effects of personality, social support, and caregiving burden. Psychosomatics. 2005;46:123–130. doi: 10.1176/appi.psy.46.2.123. [DOI] [PubMed] [Google Scholar]
- 14.Braun M, Mikulincer M, Rydall A, Walsh A, Rodin G. Hidden morbidity in cancer: Spouse caregivers. J Clin Oncol. 2007;25(30):4829–4834. doi: 10.1200/JCO.2006.10.0909. [DOI] [PubMed] [Google Scholar]
- 15.Porter LS, Keefe FJ, Garst J, McBride CM, Baucom D. Self-efficacy for managing pain, symptoms, and function in patients with lung cancer and their informal caregivers: associations with symptoms and distress. Pain. 2008;137(2):306–315. doi: 10.1016/j.pain.2007.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lazarus RS, Folkman S. Stress, appraisal, and coping. Springer; New York: 1984. [Google Scholar]
- 17.Stanton AL, Ganz PA, Rowland JH, Meyerowitz BE, Krupnick JL, Sears SR. Promoting adjustment after treatment for cancer. Cancer. 2005;104(11 Suppl):2608–2613. doi: 10.1002/cncr.21246. [DOI] [PubMed] [Google Scholar]
- 18.Carver CS. Enhancing adaptation during treatment and the role of individual differences. Cancer. 2005;104(11 Suppl):2602–2607. doi: 10.1002/cncr.21247. [DOI] [PubMed] [Google Scholar]
- 19.Beckles MA, Spiro SG, Colice GL, Rudd RM. Initial evaluation of the patient with lung cancer: symptoms, signs, laboratory tests, and paraneoplastic syndromes. Chest. 2003;123(1 Suppl):97S–104S. doi: 10.1378/chest.123.1_suppl.97s. [DOI] [PubMed] [Google Scholar]
- 20.Gonzalez BD, Jacobsen PB. Depression in lung cancer patients: the role of perceived stigma. Psychooncology. 2012;21(3):239–246. doi: 10.1002/pon.1882. [DOI] [PubMed] [Google Scholar]
- 21.Ellis J, Lloyd Williams M, Wagland R, Bailey C, Molassiotis A. Coping with and factors impacting upon the experience of lung cancer in patients and primary carers. Eur J Cancer Care (Engl) 2013;22(1):97–106. doi: 10.1111/ecc.12003. [DOI] [PubMed] [Google Scholar]
- 22.Badr H, Carmack Taylor CL. Effects of relationship maintenance on psychological distress and dyadic adjustment among couples coping with lung cancer. Health Psychol. 2008;27(5):616–627. doi: 10.1037/0278-6133.27.5.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Henoch I, Bergman B, Danielson E. Dyspnea experience and management strategies in patients with lung cancer. Psychooncology. 2008;17(7):709–715. doi: 10.1002/pon.1304. [DOI] [PubMed] [Google Scholar]
- 24.Lowe M, Molassiotis A. A longitudinal qualitative analysis of the factors that influence patient distress within the lung cancer population. Lung Cancer. 2011;74(2):344–348. doi: 10.1016/j.lungcan.2011.03.011. [DOI] [PubMed] [Google Scholar]
- 25.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41:1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 26.Kroenke K, Spitzer RL, Williams JB, Monahan PO, Lowe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146:317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- 27.Krebs EE, Lorenz KA, Bair MJ, Damush TM, Wu J, Sutherland JM, Asch SM, Kroenke K. Development and initial validation of the PEG, a three-item scale assessing pain intensity and interference. J Gen Intern Med. 2009;24:733–738. doi: 10.1007/s11606-009-0981-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McHorney CA, Ware JE, Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247–263. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 29.Portenoy RK, Thaler HT, Kornblith AB, Lepore JM, Friedlander-Klar H, Kiyasu E, Sobel K, Coyle N, Kemeny N, Norton L, Scher H. The Memorial Symptom Assessment Scale: an instrument for the evaluation of symptom prevalence, characteristics and distress. Eur J Cancer. 1994;30A:1326–1336. doi: 10.1016/0959-8049(94)90182-1. [DOI] [PubMed] [Google Scholar]
- 30.Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3:77–101. [Google Scholar]
- 31.Zinnbauer BJ, Pargament KI, Scott AB. The emerging meanings of religiousness and spirituality: Problems and prospects. J Pers. 1999;67(6):889–919. [Google Scholar]
- 32.Thomas C, Morris SM, Harman JC. Companions through cancer: the care given by informal carers in cancer contexts. Soc Sci Med. 2002;54(4):529–544. doi: 10.1016/s0277-9536(01)00048-x. [DOI] [PubMed] [Google Scholar]
- 33.Rini C, Redd WH, Austin J, Mosher CE, Meschian YM, Isola L, Scigliano E, Moskowitz CH, Papadopoulos E, Labay LE, Rowley S, Burkhalter JE, Schetter CD, Duhamel KN. Effectiveness of partner social support predicts enduring psychological distress after hematopoietic stem cell transplantation. J Consult Clin Psychol. 2011;79(1):64–74. doi: 10.1037/a0022199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hoey LM, Ieropoli SC, White VM, Jefford M. Systematic review of peer-support programs for people with cancer. Patient Educ Couns. 2008;70(3):315–337. doi: 10.1016/j.pec.2007.11.016. [DOI] [PubMed] [Google Scholar]
- 35.Kadan-Lottick NS, Vanderwerker LC, Block SD, Zhang B, Prigerson HG. Psychiatric disorders and mental health service use in patients with advanced cancer. Cancer. 2005;104(12):2872–2881. doi: 10.1002/cncr.21532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mosher CE, Hanna N, Jalal SI, Fakiris AJ, Einhorn LH, Birdas TJ, Kesler KA, Champion VL. Support service use and interest in support services among lung cancer patients. Lung Cancer. 2013;82(1):162–167. doi: 10.1016/j.lungcan.2013.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Waller A, Williams A, Groff SL, Bultz BD, Carlson LE. Screening for distress, the sixth vital sign: examining self-referral in people with cancer over a one-year period. Psychooncology. 2013;22(2):388–395. doi: 10.1002/pon.2102. [DOI] [PubMed] [Google Scholar]
- 38.Vanderwerker LC, Laff RE, Kadan-Lottick NS, McColl S, Prigerson HG. Psychiatric disorders and mental health service use among caregivers of advanced cancer patients. J Clin Oncol. 2005;23(28):6899–6907. doi: 10.1200/JCO.2005.01.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Horneber M, Bueschel G, Dennert G, Less D, Ritter E, Zwahlen M. How many cancer patients use complementary and alternative medicine: a systematic review and metaanalysis. Integr Cancer Ther. 2012;11(3):187–203. doi: 10.1177/1534735411423920. [DOI] [PubMed] [Google Scholar]
- 40.Volker DL, Wu HL. Cancer patients’ preferences for control at the end of life. Qual Health Res. 2011;21(12):1618–1631. doi: 10.1177/1049732311415287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Naus MJ, Price EC, Peter MP. The moderating effects of anxiety and breast cancer locus of control on depression. J Health Psychol. 2005;10(5):687–694. doi: 10.1177/1359105305055324. [DOI] [PubMed] [Google Scholar]
- 42.Rueda JR, Solà I, Pascual A, Subirana Casacuberta M. Non-invasive interventions for improving well-being and quality of life in patients with lung cancer. Cochrane Database Syst Rev. 2011;9:CD004282. doi: 10.1002/14651858.CD004282.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Porter LS, Keefe FJ, Garst J, Baucom DH, McBride CM, McKee DC, Sutton L, Carson K, Knowles V, Rumble M, Scipio C. Caregiver-assisted coping skills training for lung cancer: Results of a randomized clinical trial. J Pain Symptom Manage. 2011;41:1–13. doi: 10.1016/j.jpainsymman.2010.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Northouse LL, Mood DW, Schafenacker A, Kalemkerian G, Zalupski M, Lorusso P, Hayes DF, Hussain M, Ruckdeschel J, Fendrick AM, Trask PC, Ronis DL, Kershaw T. Randomized clinical trial of a brief and extensive dyadic intervention for advanced cancer patients and their family caregivers. Psychooncology. 2013;22(3):555–563. doi: 10.1002/pon.3036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Given B, Given CW, Sikorskii A, Jeon S, Sherwood P, Rahbar M. The impact of providing symptom management assistance on caregiver reaction: results of a randomized trial. J Pain Symptom Manage. 2006;32(5):433–443. doi: 10.1016/j.jpainsymman.2006.05.019. [DOI] [PubMed] [Google Scholar]