Abstract
Background
Visceral leishmaniasis (VL) remains an important public health problem in China. It is essential to elucidate the current epidemiological characteristics of VL for designing control policy.
Methods
The data were obtained from China Disease Prevention and Control Information System from 2004 to 2012. Characteristics by major variables, such as age, gender, season and geography were analyzed using SPSS13.0.
Results
The incidence of VL in China remained at a lower level in recent years. The outbreak appeared in xinjiang kashgar region in 2008. A total of 3337 VL cases were reported in China from 2004 to 2012, 97.03% of cases were concentrated in Xinjiang, Gansu and Sichuan provinces. The cases under 5 year-old accounted for 59.21%. concentrated in 3 ~ 5 months each year and annual December to January of next year The ratio of males to females was 1.67:1(2088:1249). The lag time between symptom onset and diagnosis of VL appeared a marked decrease after 2008, and were shorter in endemic provinces of Xinjiang, Gansu and Sichuan than non-endemic provinces. The case fatality rate was 2.99% (10/3337) during the study period.
Conclusion
The reported cases of VL were concentrated in Xinjiang, Gansu, Sichuan provinces in China, 2004-2012. The onset was given priority to children. The lag time between symptom onset and diagnosis of VL were difference among years and provinces. Therefore, prevention and control measures should be focused on improving awareness and capacities of diagnosis and treatment, targeting high-risk people in high-risk areas.
Keywords: Epidemiology, Visceral Leishmaniasis, China
Introduction
Leishmaniasis is a parasitic disease with different clinical manifestations depending on the infecting species of Leishmania and on the immune response of the host (1–3). Leishmaniasis has been considered as one of neglected tropical diseases (NTD) by WHO (4). Its transmission occurs through the bite of a sandfly infected with Leishmania parasites (3, 5–8). The disease occurs in two forms, cutaneous Leishmaniasis(CL) and visceral leishmania-sis(VL) clinical forms. CL usually occurs in the form of an ulcer or nodule on the skin, which can heal spontaneously. VL manifests with irregular bouts of fever, substantial weight loss, hepatomegaly, pancytopenia, and susceptibility to opportunistic infection (9). VL is a systemic disease that is fatal if left untreated (10, 11). More than 65 countries are currently affected by VL and approximately 500,000 new human cases occur annually. Visceral leishmaniasis accounts for 59,000 deaths per year (12–14). Desjeux indicated that in the previous decade endemic regions had spread, prevalence had increased and the number of unrecorded cases must have been substantial, because notification was compulsory in only few countries (8). Therefore, the public health impact of the disease worldwide has been grossly underestimated (1, 15).
VL has been and is still an important public health problem in China. Around 1951, VL was one of the most important parasitic diseases, 530,000 cases in >650 counties of provinces in the north area of the Yangtze River in China (16, 17). After nationwide control measures (mass registration of patients for treatment, killing of infected dogs, and use of insecticides against sandflies), VL has been under controlled and essentially eliminated in the northeastern endemic regions since 1958; however, transmission of VL has not been interrupted in western China.
In recent years, the endemic range has been expanded with a corresponding increase in the number of reported cases, resulting apparently in the recent outbreak of the disease that is due to global warming and rapid migration of large population in northwest China (17, 18). It is essential to elucidate the current epidemic situation and epidemic-ological characteristics of VL for designing control policy. In the present study, we describe the current epidemiological profile and characteristics of VL based on reported cases between 2004 and 2012.
Materials and Methods
Source of data
Data were collected from the online National Infectious Diseases Reporting System (NIDRS) from January 2004 to December 2012, which covered all notifiable diseases. All reported VL cases were diagnosed in accordance with the National Criteria for Visceral Leishmaniasis Diagnosis in China and reported via NDRIS. Criteria used for diagnosis of human cases were based in clinical, epidemiologic, and laboratory aspects. Most reported cases were clinical cases with symptoms of irregular fever, progressive splenomegaly, hepatomegaly, pancytopenia, and positive detected by rk39 immune chromatography test (ICT), very few were laboratory cases of finding Leishmania in the bone marrow, spleen aspirate smears.
Data sorting
The inaccurate and repeated case reporting records were excluded, only the final-judgment cases were saved. Analysis is based on onset date, including both clinical and laboratory cases.
Data analysis
The data was analyzed by using statistical software SPSS13.0. The annual incidence rate was calculated using the mid-year population data. Relevant population data was collected from the national census database from the Bureau of Statistics. Geographical distribution was based on the current address of reported cases, and age distribution was based on the calculation chronological age for the onset date minus the birth date of reported cases.
Results
General status and epidemic tends
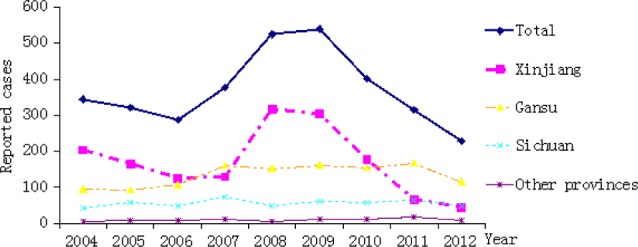
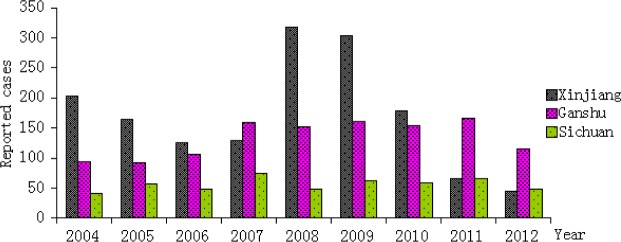
Between 2004 and 2012 a total of 3337 VL cases were notified in China through NDRIS. Overall, the incidence rate of VL maintained at a low level from 2004 to 2012, there was a sharp increase in 2008 and 2009. The incidence rate of VL was the lowest in 2012 (228 cases, incidence rate: 0.0169/100,000), and the highest in 2009 (539 cases, incidence rate: 0.0406/100,000) (Fig.1). Relatively incidence was higher in Xinjiang Autonomous Region, and peaked in 2008, 2009. Incidence in the other two northwest provinces (Gansu, Sichuan) remained relatively stable in recent years, maintaining at a lower level. Fortunately, the cases declined in all three provinces from 2011 to 2012 (Fig.2).
Fig.1.
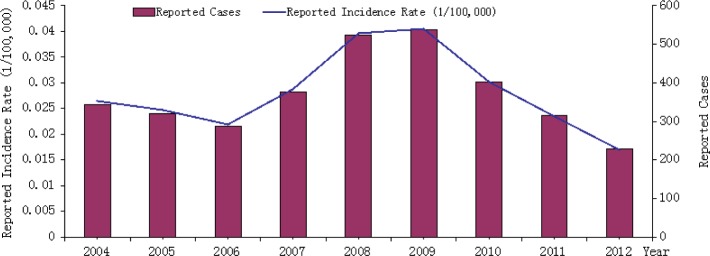
Temporal (yearly) distribution of VL cases(incidence rate) reported between 2004 and 2012
Fig. 2.
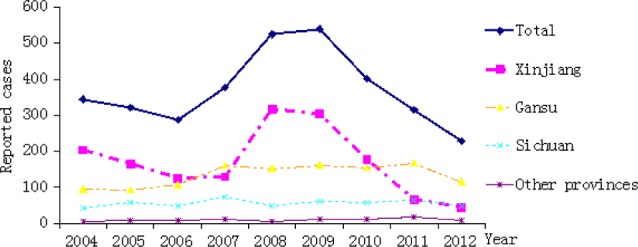
Temporal (yearly) distribution of VL cases reported in high risk provinces between 2004 and 2012
Temporal Distribution
VL Cases were reported in all months, however, monthly distribution of reported cases showed a difference. The cases increased in March and reached a peak in May. The second small peak occurred in the period of December to January of the next year, with a peak in December. The case distribution by month was similar from 2004 to 2012 (Fig.3).
Fig. 3.
The monthly number of VL cases in China from 2004 and 2012
Demographic distribution Age and gender
The age and gender distribution of cases is showed in Figure 4. During this period VL was found more in men (n=2088, 62.57%) than in women (n=1249, 37.43%). The ratio of males to females was 1.67:1(2088 : 1249). The majority of cases (1555cases, 46.60%) were in people of <5 years of age group. Secondly, 12.62% occurred in the 5-10 years of age group.
Fig.4.
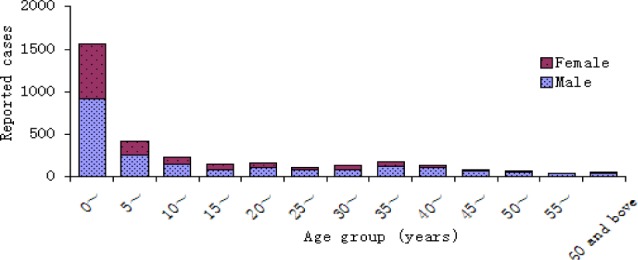
Age and gender distribution of VL cases reported between 2004 and 2012
Occupation
The majority of the cases were non-institutional children (under 5 years, 1,468 cases accounting for 43.99%). The second large group was farmers, with 739 cases (22.14%), followed by student (523 cases, 15.67%), and preschool children (272 cases, 8.15%). Migrant workers and workers were 58 and 49 cases, accounting for 1.74% and 1.47% representatively. Other occupations represented 6.83% (228 cases).
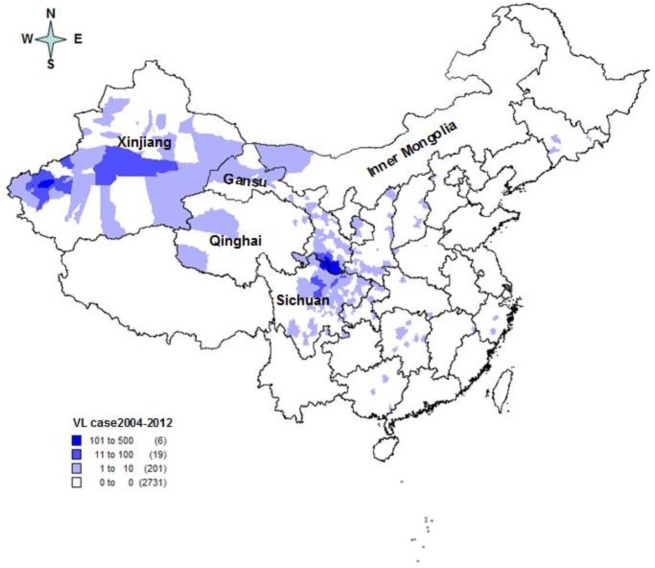
Geographic distribution
The 3337 cases were distributed in 22 provinces/municipalities/autonomous regions. 97.03% (3238/3337) of cases occurred in three provinces/autonomous regions (namely Xinjiang, Gansu and Sichuan). The highest concentration (45.91%) of reported cases was in Xinjiang (n=1532), followed by 35.96% in Gansu Province (n = 1200), 15.16% in Sichuan Province (n=506)(Table 1). The cases in these 3 provinces was also disproportionately distributed, for example, the incidence was much higher in Jiashi county and Kashgar, and Naizegemuin township in Xinjiang, in county of Wen, Zhouqu, Wudu in Gansu, and in county of Jiuzhaigou, Maoxian, and Wenchuan in Sichuan.
Table 1.
The distribution of VL case in major provinces
| Year | China No.of case |
Xinjiang NO. of case % |
Gansu NO. of case % |
Sichuan NO. of case % |
|||
|---|---|---|---|---|---|---|---|
| 2004 | 344 | 203 | 59.01 | 94 | 27.33 | 41 | 11.92 |
| 2005 | 321 | 165 | 51.40 | 92 | 28.66 | 57 | 17.76 |
| 2006 | 287 | 125 | 43.55 | 106 | 36.93 | 49 | 17.07 |
| 2007 | 377 | 129 | 34.22 | 160 | 42.44 | 75 | 19.89 |
| 2008 | 524 | 317 | 60.50 | 152 | 29.01 | 49 | 9.35 |
| 2009 | 539 | 304 | 56.40 | 161 | 29.87 | 62 | 11.50 |
| 2010 | 402 | 178 | 44.28 | 154 | 38.31 | 59 | 14.68 |
| 2011 | 315 | 66 | 20.95 | 166 | 52.70 | 65 | 20.63 |
| 2012 | 228 | 45 | 19.74 | 115 | 50.44 | 49 | 21.49 |
| Total | 3337 | 1532 | 45.91 | 1200 | 35.96 | 506 | 15.16 |
In the period 2004-2012, the number of cases in three provinces/autonomous regions showed a difference year by year. In Xinjiang, reported cases decreased year by year from 2004 to 2006, and increased from 2007, and reached the highest level in 2008 and 2009. In Gansu, The reported cases remained stable from 2004 to 2006 and then went up until 2012 when slightly went down. The number of reported cases in Sichuan showed a slight difference year by year (Fig.5, 6).
Fig. 5.
Temporal (yearly) distribution of VL cases in major provinces reported between 2004 and 2012
Fig. 6.
Geographic distribution of VL cases reported in China from 2004 to 2012
Lag time between onset of symptoms and diagnosis
The lag time between symptom onset and diagnosis of VL was the shortest in 2011 with a median of 9 days (range 0-214), and the longest in 2005 with a median of 18 days (range 0-398). Overall, the lag-time after 2008 appeared a marked decrease (Fig. 7).
Fig.7.
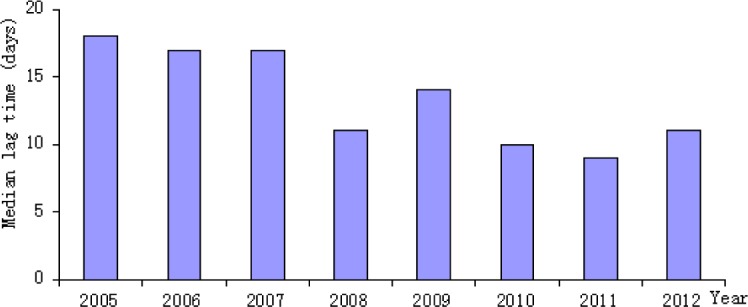
Median lag-time between onset of symptoms and diagnosis of VL in China from 2004 to 2012
Lag time between onset of symptoms and diagnosis in different Provinces
The median lag time between onset of symptoms and diagnosis in Xinjiang was the shortest (11 days). The longest median lag time between onset of symptoms and diagnosis in other provinces was 45 days. The lag time was similar in the 3 high risk provinces of Xinjiang, Gansu, and Sichuan (P>0.05), while the lag time in other provinces was significantly longer than that of the high risk provinces (P<0.01) (Fig. 8).
Fig.8.
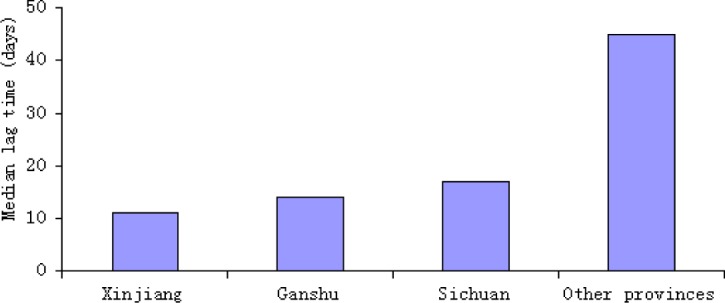
Median lag-time between onset of symptoms and diagnosis of VL in different Provinces in china from 2004 to 2012
Deaths
Of these 3337 VL cases, ten fatalities were reported in the 9 years, the case fatality rate was 2.99% (Table 2).
Table 2.
Deaths of VL in China from 2004-2012
| Province (Autonomous Region) |
County(district) | Gender | Year of death | Age at death |
|---|---|---|---|---|
| Sichuan | Qingyang | Female | 2005 | 28 years old |
| Maoxian | Male | 2005 | 13months | |
| Maoxian | Male | 2005 | 53 years old | |
| Jiuzhaigou | Male | 2006 | 9 years old | |
| Xingjiang | Wudou | Male | 2007 | 2 years old |
| Wudou | Male | 2007 | 12months | |
| Wudou | Female | 2007 | 3 years old | |
| Wudou | Male | 2007 | 12months | |
| Ganshu | Kashgar | Female | 2010 | 31years old |
| Bachu County | Male | 2012 | 7 years old |
Discussion
Leishmaniases are endemic diseases in 88 countries in the world (19). Leishmaniasis was endemic in north areas of the Yangtze River in the 1950s, especially in the East China. There were about 530,000 cases nationwide annually in early liberation period, with high fatality rate. A large-scale campaign of killing sandflies and dogs, and widespread treatment of patients since 1950 controlled the disease, and even eliminated in East China and North China in late 1950s. However, there are still epidemics and sporadic cases in Northwest China, such as Gansu, Xinjiang, and Sichuan (16–17).
In this study, data were based on passive case finding (Suspected patients referred to Health centers or hospitals) and then reported to online National Infectious Diseases Reporting System (NI-DRS), it is an limitation, but NIDRS established in 2004 has covered about 96.99% of county hospitals and 82.21% of township hospitals of China, According to a sampling study, the overall underreporting rate of communicable diseases in 459 health institutions was 5. 47%. Therefore, the data derived from NIDRS could reflect the epidemic situation of VL in China (20).
This study shows that the leishmaniasis is maintained at a low-level overall in recent years. However, there were outbreaks in some areas. The outbreak in Jiashi County, Xinjiang Province in 2008, and 2009 led to the national peak incidence. The outbreak in Jiashi County (January 1 2008 to March 12, 2009) resulted in 245 cases in total among whom 232 were infants and toddlers. The outbreak mainly concentrated in three rural eastern desert townships. The outbreak was caused by natural source (desert type), with possible reasons of changes in infectious source, medium density, living environment, personal behaviors (21).
Male cases are much more than female cases, which may related to more naked body leading to more exposure to bites of sandfly, and more moving out for work in men. The patients were mainly children of 0-4 and 5-9 year-old, with total cases of 1,976 (representing for 59.21%). This result is similar to that of Iran (22–26). The non-institutional children under 5 years old are the main infected population. More cases in young children are related to low or no immunity in children (27). The disease was controlled and even was eliminated in late 1950s in major endemic areas in China, such as the east, north China. This paper shows the disease is mainly distributed in Xinjiang, Gansu, and Sichuan provinces in recent years, which may be related to natural factors and social factors (28). Three epidemiological types of VL are distinguished in China based on infected Leishmania species and source of infection (29, 30): The human source type of VL, caused by L. donovani, transmitted by Phlebotomus chinensis and Phlebotomus longiductus inhabiting in house, human being the infectious source (31, 32); The canine source type, transmitted by wild Phlebotomus chinensis from dog to human. (30, 33); The desert type, caused by L. infantum, mainly transmitted by wild Phlebotomus Wui and Phlebotomus alexandri from undefined wild animal to human (34). In Xinjiang province, VL is mainly classified as a desert type, meanwhile, there is human source type also, with undefined infectious source, multiple media, leading to more complex influence factors, and more difficulties in prevention and control. In Gansu, Sichuan Province, VL is classified as a canine source type, with high dog density (30). The endemic areas in these 2 provinces are most mountainous with relatively poor economic conditions. The infectious source is difficult to manage, without highly specific measures to eliminate sandfly. These factors may result in the local endemic.
Median time from onset to diagnosis varies with years and provinces. The median time shortened after 2008, and it is shorter in endemic provinces of Xinjiang, Gansu, and Sichuan than other provinces, which may be related to the outbreak in Xinjiang in 2008. Because of the outbreak, Xinjiang, Gansu and Sichuan provinces vigorously carried out widespread spraying of lacewing drug, case screening, training, public education, leading to high awareness and improved diagnostic skills.
In summary, the effective prevention and control of leishmaniasis in the future should be more focused on high-risk areas and groups. Training of health care workers, and disease prevention & control staff, and improving the capacities of health care workers, should be strengthened to achieve “early detection, early diagnosis and early treatment.” Considering that there are multiple sandfly media in Xinjiang where there are desert source type and human source type, an in-depth research of sandfly species and their ecological habits, defining infectious source, should be conducted to guide the control. In the endemic mountainous areas of Sichuan and Gansu, where dogs are the main source of infection, measures to break the route of dog-sandfly should be continued to prevent infection of domestic dogs. In addition, public education targeting high-risk groups should be carried out to improve their awareness.
Conclusion
This study highlights the epidemiological feature of visceral leishmaniasis in China. This disease, which has been eliminated in most areas, continues to be popular in the western region of China. Most of cases of three types of VL were under 5 years old and the infectious resource of the desert type of VL is undefined in China.
Ethical considerations
Ethical issues (Including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgments
This study was financially supported by Key Laboratory of Surveillance and Early-warning on Infectious Disease, Division of Infectious Disease, Chinese Center for Disease Control and Prevention. The authors declare that they have no conflicts of interest.
References
- World Health Organization (2009). Leishmaniasis: background information. A brief history of the disease. Available from: www.who.int/leishmaniasis/en.
- Alvar J, Yactayo S, Bern C (2006). Leishmaniasis and poverty. Trends Parasitol, 22(12): 552–7. [DOI] [PubMed] [Google Scholar]
- Ready PD (2008). Leishmaniasis emergence and climate change. Rev Sci Tech, 27(2): 399–412. [PubMed] [Google Scholar]
- Zhang Yaobi, Chad MacArthur, Likezo Mubila (2010). Control of neglected tropical diseases needs a long-term commitment. BMC Medicine, 29(8): 67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killick-Kendrick R (1990). Phlebotomine vectors of the leishmaniases: a review. Med Vet Entomol, 4(1): 1–24. [DOI] [PubMed] [Google Scholar]
- Guerin PJ, Olliaro P, Sundar S (2002). Visceral leishmaniasis: current status of control, diagnosis, and treatment, and a proposed research and development agenda. Lancet Infect Dis, 2(8): 494–501. [DOI] [PubMed] [Google Scholar]
- Reithinger R, Davies CR (2002). Canine leishmaniasis: novel strategies for control. Trends Parasitol, 18(7): 289–90. [DOI] [PubMed] [Google Scholar]
- Desjeux P (1996). Leishmaniasis: Public health aspects and control. Clin Dermatol, 14: 417–23. [DOI] [PubMed] [Google Scholar]
- Zijlstra EE, El-Hassan AM (2001). Leishmaniasis in Sudan. T Roy Soc Trop Med H, 95(1): S27–S58. [DOI] [PubMed] [Google Scholar]
- Stanislaw Gorski, Collin Simon M., Koert Ritmeijer, et al. (2010). Visceral Leishmaniasis Relapse in Southern Sudan (1999–2007): A Retrospective Study of Risk Factors and Trends. PLOS Neg Trop Dis, 6(4): 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rançois Chappuis, Shyam Sundar, Asrat Hailu, et al. (2007). Visceral leishmaniasis: what are the needs for diagnosis, treatment and control? Nature Review, 5(11): 872–3. [DOI] [PubMed] [Google Scholar]
- Desjeux P (2004). Leishmaniasis: current situation and new perspectives. Comp Immunol Microb, 27(5): 305–18. [DOI] [PubMed] [Google Scholar]
- Fu Q, Li SZ, Wu WP, et al. (2013). Endemic characteristics of infantile visceral leishmaniasis in the People’s Republic. Parasite Vector, 6(1): 143–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahmoudvand H, Mohebali1 M, Sharifi I, et al. (2011). Epidemiological Aspects of Visceral Leishmaniasis in Baft District, Kerman Province, Southeast of Iran. Iran J Parasitol, 6(1): 1–11. [PMC free article] [PubMed] [Google Scholar]
- Ready, PD (2010). Leishmaniasis emergence in Europe. Euro Surveill, 15(10): 36. [PubMed] [Google Scholar]
- Xu LQ, Yu SH, Xu SH (2000). Chinese human parasite: distribution and hazards. 1st ed. People’s Health Publishing House, Chnia, pp.: 230–50. [Google Scholar]
- Zeng LR, Qu JQ, Chai JJ (2000). Current status of leishmaniasis in China and suggestions on prevention. End Dis brief, 15(3): 49–52. [Google Scholar]
- Yisilagin O, Tong SX, Zuo XP, et al. (2008). Endemic situation of visceral Leishmaniasis at Baishikeranmu Township, Kashi City in Xinjiang Uygur Autonomous Region during 1996-2006. Int J Med Parasitic Dis, 35(2): 75–7. [Google Scholar]
- Desjeux P (2004). Leishmaniasis: current situation and new perspectives. Comp Immunol Microb, 27(5): 305–18. [DOI] [PubMed] [Google Scholar]
- Liu Sw, Wang Lp, Zhang CX, et al. (2011). Evaluation on quality of notifiable communicable diseases network direct reporting and discussion about evaluation indicators in China, 2009. Dis Surveillance, 26(6): 499–503. [Google Scholar]
- Yang SJ, Wu WP, Tong SX (2009). Risk factors in the desert type Leishmaniasis disease outbreak in Jiashi County in Xinjiang. Int J Med Parasitic Dis, 36(3): 140–3. [Google Scholar]
- Mohebali M (2013). Visceral leishmaniasis in Iran: Review of the Epidemiological and Clinical Features. Ira J Parasitol, 8(3): 348–58. [PMC free article] [PubMed] [Google Scholar]
- Badirzadeh A, Mohebali M, Ghasemian M, et al. (2013). Cutaneous and post kala-azar dermal leishmaniasis caused by Leishmania infantum in endemic areas of visceral leishmaniasis, northwestern Iran 2002-2011: a case series. Pathog Glob Health, 107(4): 194–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shafiei R, Mohebali M, Akhoundi B, et al. (2014). Mehrdad Ghasemian Emergence of co-infection of visceral leishmaniasis in HIV-positive patients in northeast Iran: A preliminary study. Travel Med Infect Di, 12(2): 173–8. [DOI] [PubMed] [Google Scholar]
- Mohebali M, Hajjaran H, Hamzavi Y, et al. (2005). Epidemiological aspects of canine visceral leishmaniosis in the Islamic Republic of Iran. Vet Parasitol, 129(3-4): 243–251. [DOI] [PubMed] [Google Scholar]
- World Health Organization (1990). Control of the leishmaniases. Report of a WHO expert committee. Available from: www.who.int/iris/bitstream. [PubMed]
- Wu YX, Zhang AZ, Li G, et al. (1992). Leishmaniasis disease in Sichuan in 1991. Sichuan Pro Res Con Parasitic Dis, 20(2): 9–12. [Google Scholar]
- Wang Zhaojun (2000). Epidemiology and achievements in prevention ofLeishmaniasis disease in new China. Chin J Epidemiol, 21(1): 51–54. [Google Scholar]
- Guan LR, Qu JQ, Chai JJ (2000). Leishmaniasis in China–present status of prevalence and some suggestions on its control. End Dis Bull, 15(3): 49–52. [Google Scholar]
- Wang JY, Gao CH, Yang YT, Chen HT, et al. (2010). An outbreak of the desertsub-typeof zoonotic visceral leishmaniasis in Jiashi, Xinjiang Uygur AutonomousRegion, People’s Re-public of China. Parasitol Int, 59(3): 331–7. [DOI] [PubMed] [Google Scholar]
- Guan LR, Shen WX (1991). Recent advances in visceral leishmaniasis in China. Se Asian J Trop Med, 22(3): 291–8. [PubMed] [Google Scholar]
- Wang J, Peng XD, Guo YK, Yang GY (1966). A preliminary survey of epidemicity of ala-azar in Xinjiang Urghur Autonomous Region. J Epidemiol, 4(4): 30–2. [Google Scholar]
- Lu HG, Zhong L, Guan LR, Qu JQ, et al. (1994). Separation of Chinese Leishmania isolates into five genotypes by kinetoplast and chromosomal DNA heterogeneity. Am J Trop Med Hyg, 50(6): 763–70. [DOI] [PubMed] [Google Scholar]
- Wang JY, Ha Y, Gao CH, et al. (2011). The prevalence of canine Leishmania infantum infection in western China detected by PCR and sero-logical tests. Parasit Vectors, 9(4): 69. [DOI] [PMC free article] [PubMed] [Google Scholar]