Abstract
Stigma and stress may place HIV-positive men who have sex with men (HIV+ MSM) at risk for depression. Additionally, HIV+ MSM might utilize multiple HIV-related services as a way to gain support for, and more effectively manage, HIV-related stressors. Although prior research has demonstrated that depression severity and utilizing support services are associated with functional or dysfunctional coping strategies, researchers have not investigated the impact of different coping combinations—specifically, the concurrent use of functional and dysfunctional strategies—in this population. Thus, we explored (1) how items on one measure of coping, the Brief COPE, capture HIV-related coping of HIV+ MSM using Principal Components Analysis, (2) how HIV+ MSM’s coping groups into unique combinations, and (3) how these coping combinations relate to depression and the scope of HIV-related support service utilization. Our sample consisted of 170 HIV+ MSM engaged with medical care. Results indicated the use of both functional and dysfunctional coping strategies. Unique combinations of functional and dysfunctional strategies showed differential associations with depression and the extent of HIV-related support service utilization. Specifically, individuals who engaged in low levels of both functional and dysfunctional coping, compared to individuals who more frequently engaged in functional coping strategies, were significantly less likely to utilize a range of critical HIV-related services. Individuals who reported frequent use of dysfunctional coping strategies, regardless of functional coping strategy use, reported higher levels of depression. Therefore, providers should continue to focus more closely on identifying functional coping strategies and reducing dysfunctional coping when working with HIV+ MSM.
Keywords: coping, depression, HIV, MSM, service utilization
Individuals living with HIV often experience elevated levels of stress (e.g., Sherr et al., 2003). Identifying as a sexual minority may further exacerbate this stress, particularly among men who have sex with men (MSM), who are the demographic group with the highest incidence and prevalence of HIV in the U.S. (Centers for Disease Control and Prevention, 2011). Presently, there is considerable published literature specific to the health of HIV-positive MSM (HIV+ MSM). It is well-established that HIV+ MSM, in addition to the physical symptoms of disease progression, frequently experience stressors related to social marginalization and stigma associated with their illness, and minority stress associated with their sexual orientation (e.g., Bird & Voisin, 2013; Dowshen, Binns, & Garofalo, 2009; Kamen et al., 2012; Wohl et al., 2003). This describes a phenomenon referred to as a “dual stigma” (Radcliffe et al., 2010).
The stigma and stress experienced by HIV+ MSM has great clinical significance: it may contribute to mental health problems (e.g., Berg, Mimiaga, & Safren, 2004; O'Cleirigh, Skeer, Mayer, & Safren, 2009; Sivasubramanian et al., 2011). Clinical levels of depression, in particular, have been noted as a concern, and are commonly cited as among the most prevalent mental health issue among individuals living with HIV (e.g., Bhatia, Hartman, Kallen, Graham, & Giordano, 2011). For example, in a sample of 1,140 individuals living with HIV, Asch and colleagues (2003) found that 37% met criteria for major depression. Further evidence comes from the HIV Cost and Services Utilization Study, in which 36% of the total sample (2,864 individuals) screened positive for major depression (Bing et al., 2001). Published studies specific to HIV+ MSM show similar findings regarding prevalence estimates of depression, and in several studies, estimates are shown to be even higher (e.g., Bogart et al., 2011; Reif et al., 2012; Stoloff et al., 2013).
Given the economic and social realities for many HIV+ MSM, it is necessary for such individuals to access a range of support services to maintain a reasonable quality of life. There are many services available based on geographic region and eligibility: HIV case management, nutrition services, peer support, mental health, home-based medical care, and housing services, among many others. It is especially critical, however, to consider the impact of the range of service utilization in the context of depression, and vice-versa, given that the salience and perceived stigma of depression are often shown to be barriers to accessing service (e.g., Conner et al., 2010; Nadeem et al., 2007). Overall, the impact of service utilization, including those addressing substance abuse (e.g., Brown et al., 2006; Selwyn, 1996), mental health problems (e.g., Feldman, Weinberg, & Wu, 2012; Small, 2010), or affordable housing (e.g., Dasinger & Speiglman, 2007; Egan & Hoagland, 2006), can be quite profound for HIV+ MSM. Utilizing support services such as psychotherapy, for example, has been shown to reduce psychological distress and increase active problem-solving and illness-coping behaviors (Levine, Bystritsky, Baron, & Jones, 1991). Further, in another study, accessing housing services reduced the need for medical care and improved self-reported physical and mental health (Wolitski et al., 2010). Thus, it is important that researchers further explore factors that promote the full range of support service use among HIV+ MSM, which appear strongly associated with increases in reported health status.
In an effort to manage stress, individuals employ specific coping strategies (Lazarus & Folkman, 1984). Coping is a process that involves both cognitive and behavioral responses to perceived stressors. Results from a recent meta-analysis of 35 prospective cohort studies revealed how individuals living with HIV tend to respond to psychosocial stressors. The authors suggest that coping strategies such as avoidance, denial, and enacting hopelessness are strongly associated with faster HIV disease progression (Chida & Vedhara, 2009). Conversely, active coping strategies have been shown to be associated with positive health indicators, such as higher CD4 count and lower viral load, increased self-efficacy beliefs, and greater social support (e.g., Mosack et al., 2009; Orban et al., 2010). Given the quantity of published studies focused on HIV+ MSM, there is, accordingly, growing empirical research specific to HIV-related coping strategies used within this population. Researchers have demonstrated that HIV+ MSM might cope with HIV-related stress through the use of numerous strategies, such as avoidance (e.g., denial, disengagement, distraction, sexual activity), approach (e.g., planning, seeking support, acceptance), and substance use (Alvy et al., 2011; Kelly, Bimbi, Izienicki, & Parsons, 2009; Martin & Alessi, 2010; Penedo et al., 2003).
One of the most commonly used and psychometrically sound measures for assessing the frequency of emotion- and problem-focused coping strategies used across populations is the Brief COPE (Carver, 1997; Kapsou, Panayiotou, Kokkinos, & Demetriou, 2010; Snell, Siegert, Hay-Smith, & Surgenor, 2011). The Brief COPE's items were derived from the best performing items of the original 60-item COPE Inventory (Carver, Scheier, & Weintraub, 1989). The Brief COPE consists of 14 subscales, with two items each, and assesses how frequently (on an ordinal scale) an individual engages in a specific strategy in response to a given stressor. It is specified, however, that the application of the subscale items are “determined by the needs and imagination of the researcher” (pp. 99) and, therefore, without specific instructions (Carver, 1997). This gives support to the notion that the subscales of the Brief COPE can—and likely, should—be used in novel ways to better understand coping strategies among a given population.
Whereas the Brief COPE has been used to assess for coping strategies related to many different types of stressors (e.g., cancer, trauma, serious mental illness), there are relatively few published studies that use the measure to assess for HIV-related coping (e.g., Kotzé, Visser, Makin, Sikkema, & Forsyth, 2013; Olley, Seedat, Nei, & Stein, 2004), and even fewer inclusive of HIV+ MSM (e.g., Kamen et al., 2012; Kurtz, Buttram, Surratt, & Stall, 2012). Given the robust nature of the measure across populations, it appears well suited to be further assessed among HIV+ MSM. Typically, researchers have used the Brief COPE to link specific subscales to physical and mental health indicators among HIV-positive samples. For example, one research study, inclusive of 142 men and women living with HIV, demonstrated that more frequent coping via substance use was related to lower social functioning (i.e., engaging in limited social activities; Vosvick et al., 2003). Another study, which consisted of 640 men and women living with HIV, showed that more frequent coping via self-distraction (i.e., engaging in activities to distract from the stress of living with HIV) was negatively associated with the use of online HIV support groups (Mo & Coulson, 2010). An additional study, which included 157 individuals living with HIV, found that more frequent use of coping via self-distraction, behavioral disengagement, or self-blame was negatively associated with mental and/or physical health functioning (Armon & Lichtenstein, 2012). These are important findings that help us understand how singular coping strategies are often linked to different psychosocial health outcomes. However, this commonly used analytic approach takes the coping strategies used by the participants out of context. Specifically, this implies that the use of one coping strategy is somehow independent from the use of another coping strategy—which does not appear to match the reality of people's experiences (e.g., Hart et al., 2000).
To better account for the combination of multiple coping strategies used by a given individual, some researchers have grouped subscale items together based on similar functions and/or valences such as, for example, “adaptive” or “maladaptive” coping (Meyer, 2001), “functional or “dysfunctional” coping (Cooper, Katona, & Livingston, 2008), and “engagement” or “disengagement” coping (Benson, 2010). Although mental health providers and researchers have used different terminology, these dichotomized coping groups represent, generally, thoughts and behaviors that either function to solve a problem (i.e., adaptive, engagement, or functional coping) or avoid, distract, or otherwise not actively solve a problem (i.e., maladaptive, disengagement, or dysfunctional coping). These coping strategy groups appear to accurately capture an individual's experience of coping. However, these are each typically used independently of the other as a grouping variable—specifically, investigators report on the impact of functional coping or dysfunctional coping on a health outcome. Prior research has shown, however, that individuals living with HIV simultaneously engage in functional and dysfunctional coping strategies (e.g., Stein & Rotheram-Borus, 2004; Varni, Miller, McCuin, & Solomon, 2012). As such, exploring different coping combinations—specifically, the impact of simultaneously engaging in functional and dysfunctional coping behaviors on a health outcome—appears to better approximate the reality of coping with HIV-related stress. Additionally, examining coping offers a strengths-based approach to HIV care and management. For example, coping responses to HIV-related stress appear amenable to coping-focused health interventions that strengthen adaptive coping strategies (e.g., Smith, Tarakeshwar, Hansen, Kochman, & Sikkema, 2009).
Thus, the purpose of this paper is threefold. First, we aim to further assess the utility of the Brief COPE as a measure of coping among a sample of HIV+ MSM. Second, we aim to identify how the individual items comprising the Brief COPE can be conceptualized and grouped into novel coping combinations more consistent with what we know of the lived experiences of HIV+ MSM. Third, based on the existing literature regarding the prevalence of depression in this population and the benefits of HIV-related support service utilization, we aim to investigate how different coping combinations may predict depression severity and the utilization of a range of clinically meaningful support services (e.g., mental health counseling, social services, housing services, and substance abuse treatment).
Method
Recruitment
Participants were recruited from two urban, outpatient, public university-affiliated HIV clinics. Clinical staff referred potential participants, who were asked about their willingness to participate in a one-time, computer-based interview study investigating “certain life experiences you may have had, and how they have affected your health and the way you feel about yourself.”
Procedures
After receiving institutional review board (IRB) approval, research study visits were conducted at the participant's usual clinic or at the investigators’ nearby research offices. Eligible participants were over 18 years old, a biological male at birth, English-speaking, identified as MSM (per self-report), and were diagnosed with HIV (per medical record). All participants consented to the study procedures through written documentation. Specifically, participants consented to take part in a one-time survey and to allow investigators to extract biomarker and utilization data from their electronic medical records. All referred participants passed the initial screening, were deemed eligible, and were enrolled.
Surveys were administered via computer-assisted self-interview (CASI), permitting the use of embedded skip patterns to eliminate redundant or irrelevant questions. CASI maximizes time efficiency, increases confidentiality, decreases socially desirable responding, and aids in subsequent data management and analysis (Jennings, Lucenko, Malow, & Dévieux, 2002). Participants were paid $20 and given a list of free/low-cost community resources related to housing, employment, and the healthcare needs of HIV+ MSM.
Measures
Demographics
An investigator-created questionnaire was used to collect demographic data. Participants were asked to specify demographic information, which included age, race, educational attainment, monthly income, employment status, time since being diagnosed with HIV, and sexual orientation. Regarding sexual orientation, participants were asked, “Considering your current behaviors and attractions, do you now consider yourself to be...” Response options included Only heterosexual/straight, Mainly heterosexual/straight, Equally heterosexual/straight and gay, Mainly gay, and Only gay.
Health-Related Variables
Health-related variables—CD4 count and viral load (HIV-1 polymerase chain reaction (PCR) RNA)—were extracted from the participants’ electronic medical records and represent results that were closest in time to participation in the research study (mean = 30.4 days). In the analyses, CD4 count and log-transformed viral load were included as continuous measures.
Depression
The Center for Epidemiological Study—Depression Scale (CES-D) measured depressive symptomatology (Radloff, 1977). Specifically, respondents rated the frequency with which they have experienced each of 20 depressive symptoms. Response choices ranged from 0 (rarely or none of the time) to 3 (most or all of the time). Example items included: “During the past week, I felt lonely” and “During the past week, I did not feel like eating; my appetite was poor.” Each participant had a total score ranging from 0 to 60, and a clinical cut-off score of 23, instead of 16, was used to indicate probable depression. In comparison to the general medical population from which this measure was standardized, individuals living with HIV are more likely to experience somatic symptoms as a result of disease progression and/or antiretroviral therapy. Therefore, given the frequency of somatic symptoms often already present in the HIV-positive population, researchers often use a higher cut-off score to indicate probable depression (Kalichman, Rompa, & Cage, 2000). All items demonstrated high internal consistency in our study (α = .92).
Coping
The Brief COPE (Carver, 1997) was used to assess the frequency with which respondents used a variety of strategies to cope with the stressor of “living with HIV.” Items inquired about the frequency of behaviors (thoughts & overt actions) the participant had employed to respond to that stressor. The measure is organized into 14 subscales, each comprising two items (total of 28 items): positive reframing, religion, substance abuse, venting, humor, instrumental support, acceptance, active coping, behavioral disengagement, self-blame, denial, self-distraction, emotional support, and planning. Example items include: “I've been using drugs or alcohol to make myself feel better” and “I've been getting emotional support from others.” Response choices ranged from 0 (I have not done this at all) to 4 (I have done this a lot). All items demonstrated high internal consistency in our study (α = .89).
Support Service Utilization
An investigator-created questionnaire was used to measure if the participants had recently utilized support services (10 types of services in total), including accessing drug or alcohol treatment, mental health counseling, assistance with rent or housing, or meeting with a case manager or social worker. Participants indicated yes/no to each. In our analysis, we used the sum of all items endorsed; therefore, each participant had a total score ranging from 0 (no services used) to 10 (many services used). As this could be considered a count variable, we examined a histogram and Q-Q plot of the utilizing support services outcome variable, to determine whether it followed a normal or Poisson distribution. Visual inspection showed the variable followed a normal distribution. One participant was identified as an outlier on this variable and was excluded from all subsequent analyses. The Kuder-Richardson test of internal consistency revealed moderate reliability (ρKR20 = .59).
Results
Participants
For the total sample, the mean age was 44 years and the majority of participants (62.94%) identified as White. Over half of the sample (58.24%) completed at least some college. Regarding health indicators, the mean score on the CES-D was 20.18 (SD = 12.90; clinical-cutoff score for depression = 23) and participants used an average of 4.34 support services (range = 0-10). Complete sociodemographic characteristics and health indicators are presented in Table 1.
TABLE 1.
Sociodemographic Characteristics and Health Indicators
| Characteristic | n | % of sample |
|---|---|---|
| Age M (SD), Range | 170 | 44.08 (8.40), 25-66 |
| Race | ||
| White | 107 | 62.94 |
| Black/African American | 30 | 17.65 |
| More than one race | 13 | 7.65 |
| American Indian/Alaskan Native | 10 | 5.88 |
| Unknown | 7 | 4.12 |
| Sexual Orientation | ||
| Only heterosexual/straight | 5 | 2.94 |
| Mainly heterosexual/straight | 6 | 3.53 |
| Equally heterosexual/straight and gay | 10 | 5.88 |
| Mainly gay | 49 | 28.82 |
| Only gay | 100 | 58.82 |
| Income | ||
| ≤$738 per month | 78 | 45.88 |
| >$738 per month | 88 | 51.76 |
| Employment Status | ||
| Employed (full-time or part-time) | 31 | 18.24 |
| Unemployed | 71.12 | |
| Educational attainment | ||
| High school graduate/GED/fewer years of schooling | 71 | 42.01 |
| Some college/AA degree/tech school/Bachelor's/graduate degree | 98 | 57.99 |
| Health indicator | Mean (SD) | Range |
|---|---|---|
| Depression score (CES-D) | 20.18 (12.90) | 0.00-57.00 |
| # of support services used | 4.34 (2.13) | 0.00-10.00 |
| CD4 count | 413.66 (232.31) | 8.00-1329.00 |
| Viral load (log of copies/mL) | 2.37 (1.38) | 1.48-6.00 |
| Time since HIV diagnosis (in years) | 12.28 (7.27) | 1.00-27.00 |
Principal Components Analysis
To better understand how HIV+ MSM may engage in different coping strategies, we conducted a Principal Components Analysis (PCA) on the Brief COPE. PCA identifies the best grouping for the different items. The original PCA revealed an underlying factor structure of eight components, each with eigenvalues >1, and explaining 69.10% of the total variance. However, the first two components alone explained 39.42% of the total variance, and the accompanying scree plot suggested the emergence of two distinct components. Therefore, we then performed a PCA with two extracted components and with direct oblimin rotation to aid interpretation of the two components. Items typically considered “functional coping” (17 items) loaded onto Component 1, and items typically considered “dysfunctional coping” (10 items) loaded on Component 2. Seven items had a loading of <0.5 or cross-loadings >0.3 and thus were excluded from subsequent analyses. One item (“Making fun of the situation”) did not load on either component and was also dropped. The final functional coping component consisted of 12 items, and the final dysfunctional coping component consisted of eight items (see Table 2).
TABLE 2.
Principal Components Analysis with Direct Oblimin Rotation 2-Factor Structure of the Brief COPE
| Subscale item | 1 | 2 |
|---|---|---|
| Looking for something good in what's happening | .760 | |
| Concentrating my efforts on doing something about the situation | .737 | |
| Taking action to make the situation better | .713 | |
| Thinking hard about what steps to take | .696 | |
| Trying to get advice or help from others | .673 | |
| Trying to see it in a different light, more positive | .673 | |
| Trying to come up with a strategy about what to do | .626 | |
| Getting help/advice from other people | .629 | |
| Getting emotional support from others | .579 | |
| Getting comfort and understanding from someone | .580 | |
| Trying to find comfort in my religion/spiritual beliefs | .583 | |
| Learning to live with it* | .589 | −.392 |
| Accepting the reality of the fact that it has happened* | .573 | −.315 |
| Doing something to think about it less | .520 | |
| Praying or meditating* | .469 | |
| Turning to work or other activities to take my mind off things* | .456 | |
| Making jokes about it* | .315 | |
| Giving up on attempts to cope | .775 | |
| Refusing to believe that is has happened | .709 | |
| Giving up | .706 | |
| Criticizing myself | .642 | |
| Using alcohol or drugs to help me get through it | .643 | |
| Blaming myself | .645 | |
| Saying things to let my unpleasant feelings escape* | .348 | .531 |
| Using alcohol or drugs to feel better | .552 | |
| Saying to myself, “This isn't real” | .561 | |
| Expressing my negative feelings* | .326 | .357 |
| Making fun of the situation* |
Item excluded from the components used in future analyses.
Cluster Analysis
To determine patterns of functional and dysfunctional coping in our sample, we followed a two-step procedure to examine cluster types (Gordon, 1999). First, hierarchical cluster analysis was conducted using Ward's method (Ward, 1963) in SAS 9.4. In this step, we examined patterns of explained variance to determine the cluster solution that best fit the data. Results suggested a four-cluster solution maximized between-groups variability while minimizing within-groups variability. Second, we used nonhierarchical k-means clustering with PROC FASTCLUS in SAS 9.4, specifying two, three, four, and five cluster solutions. Simulation studies indicate that k-means clustering performs as well as latent clustering methods under most conditions (Steinley & Brusco, 2011). In this step, we specified the number of clusters and evaluated their respective solutions to decide on a final cluster solution. We found the four-cluster solution to be the most interpretable and to result in the largest increase in variance explained by cluster type. In order to describe the configuration of sources of coping within each cluster, we described mean cluster scores on a component as “low” if they were below the total sample mean and as “high” if they were above the total sample mean. This resulted in four groups, each representing a unique combination of an individual's coping pattern: “High Functional/Low Dysfunctional,” “High Functional/High Dysfunctional,” “Low Functional/High Dysfunctional,” and “Low Functional/Low Dysfunctional.”
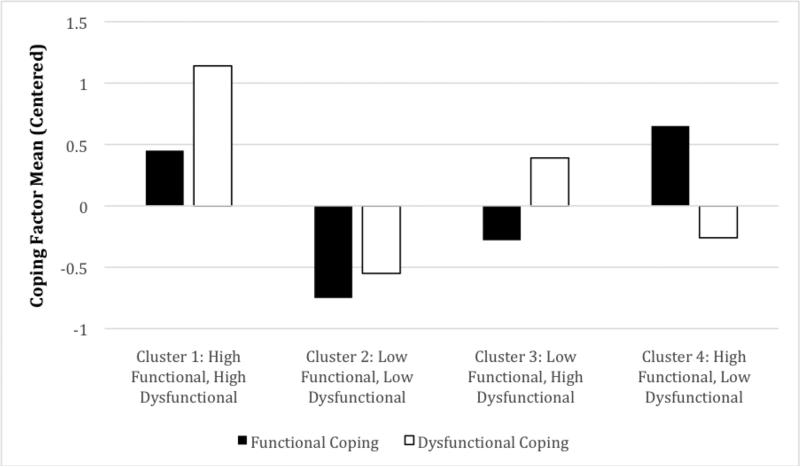
Cluster 1 (n = 22, 12.9% of participants) was characterized by high levels of both functional (M = 2.12, SD = 0.50) and dysfunctional (M = 1.92, SD = 0.52) coping. Cluster 2 (n = 46, 27.1% of participants) was characterized by low levels of both functional (M = 0.92, SD = 0.50) and dysfunctional (M = 0.24, SD = 0.24) coping. Cluster 3 (n = 42, 24.7% of participants) was characterized by low levels of functional (M = 1.40, SD = 0.42) and high levels of dysfunctional (M = 1.17, SD = 0.30) coping. Cluster 4 (n = 59, 34.7% of participants) was characterized by high levels of functional (M = 2.32, SD = 0.35) and low levels of dysfunctional (M = 0.52, SD = 0.33) coping. The visual depiction of cluster types is presented in Figure 1 and shows mean scores for each cluster type centered around the sample mean, which illustrates the patterns of coping on the two components across the four cluster groups.
Figure 1.
Cluster group means on centered coping factors.
Regression Models
For the regression models, we entered age, educational attainment, race/ethnicity, CD4 count, viral load, and time since HIV diagnosis as control variables. These have been previously identified as factors associated with depression and service utilization (e.g., Gonzalez, Alegría, Prihoda, Copeland, & Zeber, 2011; Horvitz-Lennon et al., 2009; Turan & Yargic, 2012). We controlled for depression in the model predicting the range of support services, and for the range of support services in the model predicting depression. Because depression is continuous, it was mean-centered before we entered it into the model, to aid interpretation and avoid multicollinearity (Frazier, Tix, & Barron, 2004). As a secondary measure, to test whether an alternative distribution was more appropriate for the range of support service utilization outcome, we ran this regression specifying normal, Poisson, and negative binomial distributions. The likelihood ratio chi-square statistic, AIC, and log likelihood statistics indicated the regression using the normal distribution was the best fit to the data and results for predictors of interest were consistent between the models; thus, we continued to use the normal approach to linear regression for both outcome variables.
For the regression model predicting the range of support service utilization, dummy coded coping cluster types were entered as a predictor variable (using the High Functional/Low Dysfunctional cluster as the reference group). After adjusting for demographic and health indicator variables, and in comparison to individuals who engage in High Functional/Low Dysfunctional coping strategies (Cluster 4), individuals who engage in Low Functional/Low Dysfunctional coping strategies (Cluster 2) were significantly less likely to utilize a range of HIV-related support services (β = −0.25, t = −2.67, p < .01). The other two clusters were not significantly associated with the range of support service utilization (see Table 3). The overall model was significant (F(13, 128) = 1.99, p < .05) and accounted for 17% of the variance in support service utilization.
TABLE 3.
Linear Regression Analysis Predicting Support Service Utilization
| Predictor | B | 95% CI | β | SE | t | F | R2 |
|---|---|---|---|---|---|---|---|
| 2.35* | 0.17 | ||||||
| Age | 0.05 | [0.00,0.09] | 0.20 | 0.02 | 2.20* | ||
| African American | 0.41 | [−0.51,1.32] | 0.08 | 0.46 | 0.88 | ||
| American Indian | 1.27 | [−0.31,2.84] | 0.13 | 0.80 | 1.59 | ||
| Multiracial | 0.02 | [−1.16,1.21] | 0.00 | 0.60 | 0.04 | ||
| Other/Unknown | −0.02 | [−1.74,1.69] | −0.00 | 0.87 | −0.03 | ||
| At least some college | 0.01 | [−0.68,0.70] | 0.00 | 0.35 | 0.02 | ||
| CD4 count | 0.00 | [−0.00,0.00] | 0.06 | 0.00 | 0.68 | ||
| Viral Load (log) | 0.14 | [−0.13,0.40] | 0.09 | 0.13 | 1.02 | ||
| Time since diagnosis | 0.00 | [−0.05,0.05] | 0.01 | 0.03 | 0.16 | ||
| CESD | 0.04 | [0.01,0.07] | 0.24 | 0.02 | 2.35* | ||
| Hi/Hi Cluster | −0.88 | [−2.13,0.36] | −0.14 | 0.63 | −1.41 | ||
| Lo/Hi Cluster | −0.10 | [−1.10,0.89] | −0.02 | 0.50 | −0.21 | ||
| Lo/Lo Cluster | −1.19 | [−2.06,−0.31] | −0.25 | 0.44 | −2.67** |
Note.
White participants, participants who had completed high school or less, and members of the Hi/Lo Cluster were used as reference groups.
p < .05
p < .01
For the regression model predicting depression, dummy coded coping cluster types were entered as a predictor variable (using the High Functional/Low Dysfunctional cluster as the reference group). After adjusting for demographic and health indicator variables, and in comparison to individuals who engage in High Functional/Low Dysfunctional coping strategies (Cluster 4), individuals who engage in High Functional/High Dysfunctional coping strategies (Cluster 1) or Low Functional/High Dysfunctional coping strategies (Cluster 3) were significantly more likely to report symptoms of depression (β = 0.36, t = 4.47, p < .01 and β = 0.50, t = 6.34, p < .01, respectively). The other cluster was not significantly associated with support service utilization (see Table 4). The overall model was significant (F(13, 128) = 6.88, p < .001) and accounted for 41% of the variance in depression.
TABLE 4 Linear Regression Analysis Predicting Depression
| Predictor | B | 95% CI | β | SE | t | F | R2 |
|---|---|---|---|---|---|---|---|
| 6.88** | 0.41 | ||||||
| Age | −0.15 | [−0.39,0.09] | −0.09 | 0.12 | −1.23 | ||
| African American | −0.68 | [−5.63,4.27] | −0.02 | 2.50 | −0.27 | ||
| American Indian | −9.72 | [−18.10,−1.34] | −0.16 | 4.24 | −2.30* | ||
| Multiracial | −6.44 | [−12.74,−0.15] | −0.14 | 3.18 | −2.02* | ||
| Other/Unknown | −0.64 | [−9.86,8.57] | −0.01 | 4.66 | −0.14 | ||
| At least some college | 0.96 | [−2.74,4.65] | 0.04 | 0.96 | 0.51 | ||
| CD4 count | −0.00 | [−0.01,0.00] | −0.08 | 0.00 | −1.08 | ||
| Viral Load (log) | −0.39 | [−1.82,1.03] | −0.04 | 0.72 | −0.55 | ||
| Time since diagnosis | −-0.10 | [−0.37,0.16] | −0.06 | 0.13 | −0.77 | ||
| Used support services | 1.10 | [0.17,2.02] | 0.17 | 0.47 | 2.35* | ||
| Hi/Hi Cluster | 14.14 | [7.88,20.41] | 0.36 | 3.17 | 4.47** | ||
| Lo/Hi Cluster | 14.99 | [10.31,19.67] | 0.50 | 2.36 | 6.34** | ||
| Lo/Lo Cluster | 0.32 | [−4.53,5.17] | 0.01 | 2.45 | 0.13 |
Note.
White participants, participants who had completed high school or less, and members of the Hi/Lo Cluster were used as reference groups.
p < .05
p < .01
Discussion
The present study examined how to conceptualize different combinations of functional and dysfunctional coping, and the extent to which these coping combinations impacted the range of support service utilization and depression in HIV+ MSM. Regarding the study's first aim, we found that the Brief COPE demonstrated high internal consistency and captured the range of individual coping strategies used by HIV+ MSM. Specifically, participants endorsed that they responded frequently to HIV-related stress through a variety of cognitive and behavioral coping strategies; some of which were in line with their values and overarching goals, and some of which were not. Regarding the second aim, we found that the individual items comprising the Brief COPE could be conceptualized into two components (i.e., functional and dysfunctional coping) that were used to group participants into different clusters consistent with their unique experiences. The results suggest that coping is a multidimensional process, rather than a single trait-like quality. That is to say: our participants simultaneously engaged in different frequencies of different types of coping strategies, both functional and dysfunctional. The use of k-means cluster analysis allowed us to identify existing patterns of coping in the population. Thus, our results emphasize the need for mental health providers to assess for the frequency of both functional and dysfunctional coping strategies in an effort to more accurately capture the totality of an individual's coping pattern, and to better understand how the pattern may be related to health-promoting (or inhibiting) behaviors. Additionally, mental health providers should consider the connotations that may accompany specific coping labels. Functional and dysfunctional coping, by definition, reference the function of the coping strategy, as opposed to a judgment levied at the individual (e.g., “positive” or “negative” coping). Therefore, mental health providers should consider how they label coping strategies and the manner in which they convey these thoughts to patients/clients.
Regarding the study's third aim, results show that, among HIV+ MSM, distinct coping combinations are associated with depressive symptoms and the utilization of a range of HIV-related support services. Examining combinations of functional and dysfunctional coping allowed us to examine the role of these coping styles concurrently. Specific to service utilization, individuals who engage in a low frequency of coping strategies, in general, compared to individuals who more frequently engage in specific functional coping strategies, are significantly less likely to utilize the breadth of critical HIV-related services. From a translational perspective, this supports the notion that individuals living with HIV might ultimately engage in a broader range of support services if they are actively using functional coping strategies. This idea is demonstrated in our results, in which the High Functional/Low Dysfunctional cluster tended to use the most support services overall. Thus, mental health providers should focus on assisting patients/clients in identifying functional coping strategies (e.g., items such as looking for something good in what is happening or trying to come up with a strategy about what to do). Engaging in available support services might be a form of coping itself. Fostering functional coping strategies, then, could have a profound influence on the health and well-being of HIV+ MSM. Beyond HIV-focused care alone, the development and utilization of functional coping skills likely would promote short- and long-term life goals, increase behaviors that strengthen social networks, and further develop perspective-taking skills when faced with general life difficulties.
Based on the trends shown in the regression analysis predicting the range of support service utilization, there are no significant differences between the High Functional/High Dysfunctional coping cluster and the Low Functional/High Dysfunctional coping cluster. It appears that the common factor for both clusters is the presence of a high frequency of dysfunctional coping. One possibility, which warrants further investigation, is that in the presence of more frequent dysfunctional coping (e.g., items such as refusing to believe that it has happened or blaming myself), concurrent functional coping, then, may not have a profound impact on the use of different support services and other possible forms of HIV-related care. This is an important consideration, given that HIV+ MSM will employ both functional and dysfunctional coping strategies to manage daily stressors. Therefore, it may be necessary for mental health providers to reduce dysfunctional coping skills by selectively promoting and strengthening only functional coping skills. By shifting the focus to the functional coping skills, individuals might be more likely to seek out continued support and care. This speaks to the benefit of using a strengths-based approach when working with HIV+ MSM.
Regarding psychological health, individuals who reported a high frequency of dysfunctional coping, regardless of the frequency of functional coping, were significantly more likely to report depressive symptoms. Notably, these results align with what was reported regarding the range of support services used—that functional coping strategies may not have as profound of an effect in the presence of frequent dysfunctional coping. Given the prevalence of dysfunctional coping skills, which appear to be either punctuated by or leading to significant levels of depression, there appears to be a need for interventions that address both. A recently published randomized controlled trial (RCT) demonstrated the utility of a culturally tailored, cognitive-behavioral therapy intervention that targeted depression and medication adherence among individuals living with HIV (Safren et. al, 2012). Through the intervention, participants developed and strengthened skills specific to behavioral change motivation, problem-solving, and restructuring negative thought patterns—all of which relate to the items that comprise the functional coping factor in our analysis.
Although there appears to be a benefit to selectively targeting and reinforcing functional coping skills, mental health providers also should consider that dysfunctional coping strategies may underlie and promote the presence of depressive symptoms. Our regression model accounted for 41% of the variance in depression, which is a sizable amount. As an example of how this information might translate into health intervention development, Smith et al. (2009) published findings from an RCT that utilized a coping-focused group intervention for individuals living with HIV. The researchers found that participants reported a decrease in depressive symptoms after decreasing their use of avoidant (i.e., dysfunctional) coping strategies. Beyond the focus of coping strategies alone, mental health providers might also consider the additional impact of different support services already in place. Services that include psychotherapy, case management, and housing assistance are known correlates of mental health (e.g., Levine et al., 1991; Wolitski et al., 2010). Thus, a more effective clinical approach to reducing depressive symptoms might include targeting specific coping skills while concurrently promoting peripheral support services—all of which would likely impact the presence and severity of depression in HIV+ MSM.
Given the prevalence of depression among HIV+ MSM, and the frequent need for a range of support services, it is important to understand how these factors are impacted by distinct coping strategies; which would likely aid mental health providers in better facilitating health-promoting services (e.g., Levine et al., 1991; Wolitski et al., 2010). Thus, future work should replicate and extend these findings into other samples of HIV+ MSM. Mental health providers working directly with this population should assess the need for additional support and care, and refer and connect clients/patients with services that extend beyond primary care alone. Another clinical strategy in working with HIV+ MSM is to further assess how coping strategies specific to HIV are impacting the relation between mental health symptoms and the range of possible health indicators. Based on the results of this study, and consistent with other previously cited studies on HIV+ MSM, it should be assumed that clients/patients simultaneously engage in functional and dysfunctional coping—and that it would be a meaningful oversight to not assess for the full range of possible coping strategies.
As with any individual study, there are several limitations to consider. First, the study would have benefited from a larger sample size. Although our regression models are conceptualized based on theoretical findings from previous studies, the use of cross-sectional data make it difficult to determine the accurate temporal sequencing and direction among variables. For example, we cannot fully determine that specific coping styles impact the breadth service utilization. Similarly, we cannot say with certainty that specific coping styles impact depression. Additionally, stress and stigma are frequently shown to be strongly associated with different health outcomes in HIV + MSM (e.g., Berg et al., 2004; O'Cleirigh et al., 2009). Although our analyses focused on the novelty of different coping combinations and how these relate to health indicators, not including measures of stress and stigma in the regression models further limits our ability to draw firm conclusions about the relation between the study variables.
Notably, our sample was recruited from HIV clinics in the Pacific Northwest section of the U.S. Although our sample accurately represents the HIV+ MSM of this region, there is a lack of racial/ethnic diversity when compared to the demographics of HIV+ MSM nationally (Public Health Seattle and King County, 2009). Further, participants were already accessing HIV primary care, which may have impacted their knowledge and accessibility of different support services. This limited variability in our sampling strategy because every participant, in effect, was accessing at least one support service (i.e., medical care). Thus, we recommend that future studies assess across different levels of engagement with care, different geographic locations, and with other HIV populations that are more demographically diverse. It is possible that coping styles are culturally embedded; therefore, the results may not accurately reflect other HIV+ MSM populations. From a measurement perspective, we treated the use of support services as a unidimensional construct. However, because the items in this measure were yes/no questions asking about use of different types of services, we were not able to capture the degree to which participants engaged in different services. Thus, participants may have heavily engaged in some services but cursorily engaged in others. Future research may wish to examine associations between depression, coping, and specific types of service utilization. This goal was beyond the scope of this paper, but is an important direction for future research.
Finally, there are specific sample characteristics that likely impact our results and clinical implications. Although the participants in our sample are labeled as MSM, approximately 88% of the sample identified as “only” or “mainly” gay (based on sexual behaviors and attraction). Published research has shown that a gay identity, as opposed to behavioral markers for sexual activity, is associated with various forms of stigma and minority stressors (e.g., Meyer, 2003). Gay identity related stigma has been linked to a number of negative health indicators, such as psychological distress, depression, and social isolation, and problematic behaviors, such as substance use and sexual risk behaviors (e.g., Bruce, Ramirez-Valles, & Campbell, 2008; Russell & Joyner, 2001). Similarly, HIV/AIDS-related stigma—which likely is of salience to this group of men, given the average number of years since their diagnosis—has been linked to less social support, higher levels of depression, and lower self-esteem (e.g., Dowshen, Binns, & Garofalo, 2009; Soto, Komaie, Neilands, & Johnson, 2013; Wohl et al., 2013). Further, our sample consisted of individuals with a mean age in the mid 40s who were of low socioeconomic status (e.g., the majority were unemployed and many were living below the poverty line). Both aging with HIV/AIDS and financial strain are associated with a number of negative health indicators (e.g., Illangasekare, Burke, Chander, & Gielen, 2013; Vance, 2013). Published studies have shown that HIV+ MSM ages 50 and over—an age group that many in our sample are quickly approaching—report a number of psychosocial burdens, such as substance use and psychiatric disorders (e.g., Halkitis et al., 2012). Thus, the frequency and types of coping that individuals in our sample utilized, and the extent to which they experienced depression and sought support services, may be linked to unaccounted factors related to their sexual orientation, and the cumulative impact of aging with a stigmatized illness and socioeconomic disadvantage.
Conclusion
Our study demonstrates that different combinations of functional and dysfunctional coping strategies are relevant to the health of HIV+ MSM. Through continued research, a better understanding of the differences between patterns of coping can inform mental health providers about which responses can lead to an increase in quality of life (e.g., through mental health or substance abuse treatment), and a decrease in psychological distress and need for tertiary care (e.g., through stable and affordable housing, and effective depressive symptom management). Additionally, future research should explore the function of coping within the context of resilience processes, which would help to elucidate personal strengths and areas of growth in response to HIV/AIDS-related stigma and stress. Ultimately, efforts to further explore coping using a fine-grained analytic approach with HIV+ MSM should be continued.
Acknowledgments
This research was supported by a National Institute of Mental Health award (F31 MH71179, mentored by Dr. Jane Simoni) and a small grant from the Robert C. Bolles Research Fund of the University of Washington, both awarded to David Pantalone.
Contributor Information
Brian A. Rood, Suffolk University
Elizabeth A. McConnell, DePaul University
David W. Pantalone, University of Massachusetts—Boston and The Fenway Institute at Fenway Health
References
- Alvy L, McKirnan D, Mansergh G, Koblin B, Colfax G, Flores S, Hudson S. Depression is associated with sexual risk among men who have sex with men, but is mediated by cognitive escape and self-efficacy. AIDS and Behavior. 2011;15(6):1171–1179. doi: 10.1007/s10461-010-9678-z. doi:10.1007/s10461-010-9678-z. [DOI] [PubMed] [Google Scholar]
- Armon C, Lichtenstein K. The associations among coping, nadir CD4+ T-cell count, and non-HIV-related variables with health-related quality of life among an ambulatory HIV-positive patient population. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation. 2012;21(6):993–1003. doi: 10.1007/s11136-011-0017-2. doi:10.1007/s11136-011-0017. [DOI] [PubMed] [Google Scholar]
- Asch S, Kilbourne A, Gifford A, Burnam M, Turner B, Shapiro M, Bozzette S. Underdiagnosis of depression in HIV: Who are we missing?. Journal of General Internal Medicine. 2003;18(6):450–460. doi: 10.1046/j.1525-1497.2003.20938.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benson PR. Coping, distress, and well-being in mothers of children with autism. Research in Autism Spectrum Disorders. 2010;4(2):217–228. doi:10.1016/j.rasd.2009.09.008. [Google Scholar]
- Berg MB, Mimiaga MJ, Safren SA. Mental health concerns of HIV-infected gay and bisexual men seeking mental health services: An observational study. AIDS Patient Care and STDs. 2004;18(11):635–643. doi: 10.1089/apc.2004.18.635. doi:10.1089/1087291042531070. [DOI] [PubMed] [Google Scholar]
- Bhatia R, Hartman C, Kallen M, Graham J, Giordano T. Persons newly diagnosed with HIV infection are at high risk for depression and poor linkage to care: Results from the Steps Study. AIDS and Behavior. 2011;15(6):1161–1170. doi: 10.1007/s10461-010-9778-9. doi:10.1007/s10461-010-9778-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bing E, Burnam M, Longshore D, Fleishman J, Sherbourne C, London A, Shapiro M. Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Archives of General Psychiatry. 2001;58(8):721–728. doi: 10.1001/archpsyc.58.8.721. [DOI] [PubMed] [Google Scholar]
- Bird JP, Voisin DR. “You're an open target to be abused”: A qualitative study of stigma and HIV self-disclosure among black men who have sex with men. American Journal of Public Health. 2013;103(12):2193–2199. doi: 10.2105/AJPH.2013.301437. doi:10.2105/AJPH.2013.301390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogart LM, Wagner GJ, Galvan FH, Landrine H, Klein DJ, Sticklor LA. Perceived discrimination and mental health symptoms among black men with HIV. Cultural Diversity and Ethnic Minority Psychology. 2011;17(3):295–302. doi: 10.1037/a0024056. doi:10.1037/a0024056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown LR, Kritz S, Goldsmith R, Bini EJ, Rotrosen J, Baker S, McAuliffe P. Characteristics of substance abuse treatment programs providing services for HIV/AIDS, hepatitis C virus infection, and sexually transmitted infections: The National Drug Abuse Treatment Clinical Trials Network. Journal of Substance Abuse Treatment. 2006;30(4):315–321. doi: 10.1016/j.jsat.2006.02.006. doi:10.1016/j.jsat.2006.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce D, Ramirez-Valles J, Campbell R. Stigmatization, substance use, and sexual risk behavior among Latino gay and bisexual men and transgender persons. Journal of Drug Issues. 2008;38(1):235–260. [Google Scholar]
- Carver CS. You want to measure coping but your protocol's too long: Consider the Brief COPE. International Journal of Behavioral Medicine. 1997;4(1):92–100. doi: 10.1207/s15327558ijbm0401_6. doi:10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Carver CS, Scheier MF, Weintraub J. Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology. 1989;56(2):267–283. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention [June 15, 2014];HIV/AIDS surveillance among men who have sex with men (MSM) 2011 from http://www.cdc.gov/hiv/topics/surveillance/resources/slides/msm/index.htm.
- Chida Y, Vedhara K. Adverse psychosocial factors predict poorer prognosis in HIV disease: A meta-analytic review of prospective investigations. Brain, Behavior, and Immunity. 2009;23(4):434–445. doi: 10.1016/j.bbi.2009.01.013. doi:10.1016/j.bbi.2009.01.013. [DOI] [PubMed] [Google Scholar]
- Conner KO, Copeland VC, Grote NK, Rosen D, Albert S, McMurray ML, Koeske G. Barriers to treatment and culturally endorsed coping strategies among depressed African-American older adults. Aging and Mental Health. 2010;14(8):971–983. doi: 10.1080/13607863.2010.501061. doi:10.1080/13607863.2010.501061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper C, Katona C, Livingston G. Validity and reliability of the Brief COPE in carers of people with dementia: The LASER-AD study. Journal of Nervous and Mental Disease. 2008;196(11):838–843. doi: 10.1097/NMD.0b013e31818b504c. doi:10.1097/NMD.0b013e31818b504c. [DOI] [PubMed] [Google Scholar]
- Dasinger L, Speiglman R. Homelessness prevention: The effect of a shallow rent subsidy program on housing outcomes among people with HIV or AIDS. AIDS and Behavior. 2007;11(6 Suppl):128–139. doi: 10.1007/s10461-007-9250-7. [DOI] [PubMed] [Google Scholar]
- Dowshen N, Binns H, Garofalo R. Experiences of HIV-related stigma among young men who have sex with men. AIDS Patient Care and STDs. 2009;23(5):371–376. doi: 10.1089/apc.2008.0256. doi:10.1089/apc.2008.0256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egan B, Hoagland J. In-house work opportunities: Implications for housing organizations serving persons living With HIV/AIDS. Work. 2006;27(3):247–253. [PubMed] [Google Scholar]
- Feldman MB, Weinberg GS, Wu E. Evaluation of a system designed to link people living with HIV/AIDS with mental health services at an AIDS-service organization. Evaluation and Program Planning. 2012;35(1):133–138. doi: 10.1016/j.evalprogplan.2011.08.005. doi:10.1016/j.evalprogplan.2011.08.005. [DOI] [PubMed] [Google Scholar]
- Frazier PA, Tix AP, Barron KE. ‘Testing moderator and mediator effects in counseling psychology research’: Correction to Frazier et al. (2004). Journal of Counseling Psychology. 2004;51(2):157. doi:10.1037/0022-0167.51.2.157. [Google Scholar]
- Gonzalez J, Alegría M, Prihoda T, Copeland L, Zeber J. How the relationship of attitudes toward mental health treatment and service use differs by age, gender, ethnicity/race and education. Social Psychiatry and Psychiatric Epidemiology. 2011;46(1):45–57. doi: 10.1007/s00127-009-0168-4. doi:10.1007/s00127-009-0168-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon AD. Classification. Chapman & Hall; Boca Raton, FL: 1999. [Google Scholar]
- Halkitis PN, Kupprat SA, Hampton MB, Perez-Figueroa R, Kingdon M, Eddy JA, Ompad DC. Evidence for a syndemic in aging HIV-positive gay, bisexual, and other MSM: Implications for a holistic approach to prevention and healthcare. Natural Resource Modeling. 2012;36(2):365–386. doi: 10.1111/napa.12009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart S, Gore-Felton C, Maldonado J, Lagana L, Blake-Mortimer J, Israelski D, Spiegel D. The relationship between pain and coping styles among HIV-positive men and women. Psychology and Health. 2000;15(6):869–879. doi:10.1080/08870440008405588. [Google Scholar]
- Horvitz-Lennon M, Frank RG, Thompson W, Baik S, Alegría M, Rosenheck RA, Normand ST. Investigation of racial and ethnic disparities in service utilization among homeless adults with severe mental illnesses. Psychiatric Services. 2009;60(8):1032–1038. doi: 10.1176/appi.ps.60.8.1032. doi:10.1176/appi.ps.60.8.1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Illangasekare S, Burke J, Chander G, Gielen A. The syndemic effects of intimate partner violence, HIV/AIDS, and substance abuse on depression among low-income urban women. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2013;90(5):934–947. doi: 10.1007/s11524-013-9797-8. doi:10.1007/s11524-013-9797-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jennings TE, Lucenko BA, Malow RM, Dévieux JG. Audio-CASI vs interview method of administration of an HIV/STD risk of exposure screening instrument for teenagers. International Journal of STD and AIDS. 2002;13(11):781–784. doi: 10.1258/095646202320753754. doi:10.1258/095646202320753754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman S, Rompa D, Cage M. Distinguishing between overlapping somatic symptoms of depression and HIV disease in people living with HIV-AIDS. The Journal of Nervous and Mental Disease. 2000;188(10):662–670. doi: 10.1097/00005053-200010000-00004. [DOI] [PubMed] [Google Scholar]
- Kamen C, Flores S, Taniguchi S, Khaylis A, Lee S, Koopman C, Gore-Felton C. Sexual minority status and trauma symptom severity in men living with HIV/AIDS. Journal of Behavioral Medicine. 2012;35(1):38–46. doi: 10.1007/s10865-011-9329-5. doi:10.1007/s10865-011-9329-5. [DOI] [PubMed] [Google Scholar]
- Kapsou M, Panayiotou G, Kokkinos CM, Demetriou AG. Dimensionality of coping: An empirical contribution to the construct validation of the Brief-COPE with a Greek-speaking sample. Journal of Health Psychology. 2010;15(2):215–229. doi: 10.1177/1359105309346516. doi:10.1177/1359105309346516. [DOI] [PubMed] [Google Scholar]
- Kelly B, Bimbi D, Izienicki H, Parsons J. Stress and coping among HIV-positive barebackers. AIDS and Behavior. 2009;13(4):792–797. doi: 10.1007/s10461-009-9586-2. doi:10.1007/s10461-009-9586-2. [DOI] [PubMed] [Google Scholar]
- Kotzé M, Visser M, Makin J, Sikkema K, Forsyth B. Psychosocial variables associated with coping of HIV-positive women diagnosed during pregnancy. AIDS and Behavior. 2013;17(2):498–507. doi: 10.1007/s10461-012-0379-7. doi:10.1007/s10461-012-0379-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurtz SP, Buttram ME, Surratt HL, Stall RD. Resilience, syndemic factors, and serosorting behaviors among HIV-positive and HIV-negative substance-using MSM. AIDS Education and Prevention. 2012;24(3):193–205. doi: 10.1521/aeap.2012.24.3.193. doi:10.1521/aeap.2012.24.3.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. Springer; New York: 1984. [Google Scholar]
- Levine SH, Bystritsky A, Baron D, Jones LD. Group psychotherapy for HIV-seropositive patients with major depression. American Journal of Psychotherapy. 1991;45(3):413–424. doi: 10.1176/appi.psychotherapy.1991.45.3.413. [DOI] [PubMed] [Google Scholar]
- Martin J, Alessi E. Stressful events, avoidance coping, and unprotected anal sex among gay and bisexual men. The American Journal of Orthopsychiatry. 2010;80(3):293–301. doi: 10.1111/j.1939-0025.2010.01032.x. doi:10.1111/j.1939-0025.2010.01032.x. [DOI] [PubMed] [Google Scholar]
- Meyer B. Coping with severe mental illness: Relations of the Brief COPE with symptoms, functioning, and well-being. Journal of Psychopathology and Behavioral Assessment. 2001;23(4):265–277. doi: 10.1023/A:1010929402770. doi:10.1023/A:1012731520781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH. Prejudice, social stress, and mental health in lesbian, gay and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mo PH, Coulson NS. Living with HIV/AIDS and use of online support groups. Journal of Health Psychology. 2010;15(3):339–350. doi: 10.1177/1359105309348808. doi:10.1177/1359105309348808. [DOI] [PubMed] [Google Scholar]
- Mosack K, Weinhardt L, Kelly J, Gore-Felton C, McAuliffe T, Johnson M, Morin S. Influence of coping, social support, and depression on subjective health status among HIV-positive adults with different sexual identities. Behavioral Medicine. 2009;34(4):133–144. doi: 10.3200/BMED.34.4.133-144. doi:10.3200/BMED.34.4.133-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadeem E, Lange JM, Edge D, Fongwa M, Belin T, Miranda J. Does stigma keep poor young immigrant and U.S.-born Black and Latina women from seeking mental health care?. Psychiatric Services. 2007;58(12):1547–1554. doi: 10.1176/ps.2007.58.12.1547. doi:10.1176/appi.ps.58.12.1547. [DOI] [PubMed] [Google Scholar]
- O'Cleirigh C, Skeer M, Mayer KH, Safren SA. Functional impairment and health care utilization among HIV-infected men who have sex with men: The relationship with depression and post-traumatic stress. Journal of Behavioral Medicine. 2009;32(5):466–477. doi: 10.1007/s10865-009-9217-4. doi:10.1007/s10865-009-9217-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olley BO, Seedat SS, Nei DG, Stein DJ. Predictors of major depression in recently diagnosed patients with HIV/AIDS in South Africa. AIDS Patient Care and STDs. 2004;18(8):481–487. doi: 10.1089/1087291041703700. doi:10.1089/1087291041703700. [DOI] [PubMed] [Google Scholar]
- Orban LA, Stein R, Koenig LJ, Conner LC, Rexhouse EL, Lewis JV, LaGrange R. Coping strategies of adolescents living with HIV: Disease-specific stressors and responses. AIDS Care. 2010;22(4):420–430. doi: 10.1080/09540120903193724. doi:10.1080/09540120903193724. [DOI] [PubMed] [Google Scholar]
- Penedo F, Gonzalez J, Davis C, Dahn J, Antoni M, Ironson G, Schneiderman N. Coping and psychological distress among symptomatic HIV+ men who have sex with men. Annals of Behavioral Medicine. 2003;25(3):203–213. doi: 10.1207/S15324796ABM2503_06. [DOI] [PubMed] [Google Scholar]
- Public Health Seattle and King County [June 15, 2014];Facts about HIV infection in King County. 2009 Jun; from http://www.kingcounty.gov/healthservices/health/communicable/hiv/epi/facts.aspx.
- Radcliffe J, Doty N, Hawkins LA, Gaskins CS, Beidas R, Rudy BJ. Stigma and sexual health risk in HIV-positive African American young men who have sex with men. AIDS Patient Care and STDs. 2010;24(8):493–499. doi: 10.1089/apc.2010.0020. doi:10.1089/apc.2010.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. doi:10.1177/014662167700100306. [Google Scholar]
- Reif SS, Pence BW, Legrand S, Wilson ES, Swartz M, Ellington T, Whetten K. In-home mental health treatment for individuals with HIV. AIDS Patient Care and STDs. 2012;26(11):655–661. doi: 10.1089/apc.2012.0242. doi:10.1089/apc.2012.0242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell ST, Joyner K. Adolescent sexual orientation and suicide risk: Evidence from a national study. American Journal of Public Health. 2001;91:1276–1281. doi: 10.2105/ajph.91.8.1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safren SA, O'Cleirigh CM, Bullis JR, Otto MW, Stein MD, Pollack MH. Cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected injection drug users: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2012;80(3):404–415. doi: 10.1037/a0028208. doi:10.1037/a0028208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selwyn P. The impact of HIV infection on medical services in drug abuse treatment programs. Journal of Substance Abuse Treatment. 1996;13(5):397–410. doi: 10.1016/s0740-5472(96)00114-6. [DOI] [PubMed] [Google Scholar]
- Sherr L, Nagra N, Kulubya G, Catalan J, Clucas C, Harding R. HIV infection associated post-traumatic stress disorder and post-traumatic growth—a systematic review. Psychology, Health, and Medicine. 2011;16(5):612–629. doi: 10.1080/13548506.2011.579991. doi:10.1080/13548506.2011.579991. [DOI] [PubMed] [Google Scholar]
- Sivasubramanian M, Mimiaga MJ, Mayer KH, Anand VR, Johnson CV, Prabhugate P, Safren SA. Suicidality, clinical depression, and anxiety disorders are highly prevalent in men who have sex with men in Mumbai, India: Findings from a community-recruited sample. Psychology, Health, and Medicine. 2011;16(4):450–462. doi: 10.1080/13548506.2011.554645. doi:10.1080/13548506.2011.554645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Small LF. Use of mental health services among people with co-occurring disorders and other mental health co-morbidities: Employing the behavioral model of vulnerable populations. Mental Health and Substance Use: Dual Diagnosis. 2010;3(2):81–93. doi: 10.1080/17523281003717871. doi:10.1080/17523281003717871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith NG, Tarakeshwar N, Hansen NB, Kochman A, Sikkema KJ. Coping mediates outcome following a randomized group intervention for HIV-positive bereaved individuals. Journal of Clinical Psychology. 2009;65(3):319–335. doi: 10.1002/jclp.20547. doi:10.1002/jclp.20547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snell DL, Siegert RJ, Hay-Smith EC, Surgenor LJ. Factor structure of the Brief COPE in people with mild traumatic brain injury. The Journal of Head Trauma Rehabilitation. 2011;26(6):468–477. doi: 10.1097/HTR.0b013e3181fc5e1e. doi:10.1097/HTR.0b013e3181fc5e1e. [DOI] [PubMed] [Google Scholar]
- Soto T, Komaie G, Neilands TB, Johnson MO. Exposure to crime and trauma among HIV-infected men who have sex with men: Associations with HIV stigma and treatment engagement. Journal of the Association of Nurses in AIDS Care. 2013;24(4):299–307. doi: 10.1016/j.jana.2012.11.008. doi:10.1016/j.jana.2012.11.008. [DOI] [PubMed] [Google Scholar]
- Stein JA, Rotheram-Borus M. Cross-sectional and longitudinal associations in coping strategies and physical health outcomes among HIV-positive youth. Psychology and Health. 2004;19(3):321–336. doi:10.1080/0887044042000193479. [Google Scholar]
- Steinley D, Brusco MJ. K-means clustering and mixture model clustering: Reply to McLachlan (2011) and Vermunt (2011). Psychological Methods. 2011;16(1):89–92. [Google Scholar]
- Stoloff K, Joska J, Feast D, De Swardt G, Hugo J, Struthers H, Rebe K. A description of common mental disorders in men who have sex with men (MSM) referred for assessment and intervention at an MSM clinic in Cape Town, South Africa. AIDS and Behavior. 2013;17(Suppl 1):S77–S81. doi: 10.1007/s10461-013-0430-3. doi:10.1007/s10461-013-0430-3. [DOI] [PubMed] [Google Scholar]
- Turan R, Yargic I. The relationship between substance abuse treatment completion, sociodemographics, substance use characteristics, and criminal history. Substance Abuse. 2012;33(2):92–98. doi: 10.1080/08897077.2011.630948. doi:10.1080/08897077.2011.630948. [DOI] [PubMed] [Google Scholar]
- Vance D. The cognitive consequences of stigma, social withdrawal, and depression in adults aging with HIV. Journal of Psychosocial Nursing and Mental Health Services. 2013;51(5):18–20. doi: 10.3928/02793695-20130315-01. doi:10.3928/02793695-20130315-01. [DOI] [PubMed] [Google Scholar]
- Varni SE, Miller CT, McCuin T, Solomon S. Disengagement and engagement coping with HIV/AIDS stigma and psychological well-being of people with HIV/AIDS. Journal of Social and Clinical Psychology. 2012;31(2):123–150. doi: 10.1521/jscp.2012.31.2.123. doi:10.1521/jscp.2012.31.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vosvick M, Koopman C, Gore-Felton C, Thoresen C, Krumboltz J, Spiegel D. Relationship of functional quality of life to strategies for coping with the stress of living with HIV/AIDS. Psychosomatics. 2003;44(1):51–58. doi: 10.1176/appi.psy.44.1.51. doi:10.1176/appi.psy.44.1.51. [DOI] [PubMed] [Google Scholar]
- Ward JH. Hierarchical grouping to optimize an objective function. Journal of the American Statistical Association. 1963;58:236–244. [Google Scholar]
- Wohl A, Galvan FH, Carlos J, Myers HF, Garland W, Witt MD, George S. A comparison of MSM stigma, HIV stigma and depression in HIV-positive Latino and African American men who have sex with men (MSM). AIDS and Behavior. 2013;17(4):1454–1464. doi: 10.1007/s10461-012-0385-9. doi:10.1007/s10461-012-0385-9. [DOI] [PubMed] [Google Scholar]
- Wolitski R, Kidder D, Pals S, Royal S, Aidala A, Stall R, Courtenay-Quirk C. Randomized trial of the effects of housing assistance on the health and risk behaviors of homeless and unstably housed people living with HIV. AIDS and Behavior. 2010;14(3):493–503. doi: 10.1007/s10461-009-9643-x. doi:10.1007/s10461-009-9643-x. [DOI] [PubMed] [Google Scholar]