Abstract
Introduction
Phase III / IV clinical trials are expensive and time consuming and often suffer from poor enrollment and retention rates. Pediatric trials are particularly difficult because scheduling around the parent, participant and potentially other sibling schedules can be burdensome. We are evaluating using the internet and mobile devices to conduct the consent process and study visits in a streamlined pediatric asthma trial. Our hypothesis is that these study processes will be noninferior and will be less expensive compared to a traditional pediatric asthma trial.
Materials/Methods
Parents and participants, aged 12 through 17 years, complete the informed consent process by viewing a multi-media website containing a consent video and study material in the streamlined trial. Participants are provided an iPad with WiFi and EasyOne spirometer for use during FaceTime visits and online twice daily symptom reporting during an 8-week run-in followed by 12-week study period. Outcomes are compared with participants completing a similarly designed traditional trial comparing the same treatments within the same pediatric health-system. After 8 weeks of open-label Advair 250/50 twice daily, participants in both trial types are randomized to Advair 250/50, Flovent 250, or Advair 100/50 given 1 inhalation twice daily. Study staff track time spent to determine study costs.
Results
Participants have been enrolled in the streamlined and traditional trials and recuitment is ongoing.
Conclusions
This project will provide important information on both clinical and economic outcomes for a novel method of conducting clinical trials. The results will be broadly applicable to trials of other diseases.
Keywords: Clinical Trial, Informed Consent, Internet, Mobile Devices, Multimedia, Pediatric
INTRODUCTION
Clinical trials are the cornerstone of research evaluating drug efficacy and safety. Participation in most clinical research studies involves three primary components: providing informed consent; attending visits at the study center; and completing some procedures at home. However, increases in the numbers of procedures, study staff work burden, and longer trial duration coupled with reduced enrollment and retention rate of patient volunteers are increasing the cost and decreasing the value of clinical trials [1]. The cost of Phase III/IV trials was estimated at $47,000 per participant in 2011, an 83% increase from the previous 3 years [2, 3] suggesting that the current model for clinical research is fiscally unsustainable.
Current methods of obtaining informed consent using a written document are insufficient [4–11]. Data show that research participants have a poor understanding of the basic elements of informed consent whether provided in oral or written format [4, 8, 12–17]. Multimedia formats can enhance comprehension in the research informed consent process [5, 18] and participants, including children, prefer multimedia to written formats [18, 19].
The number of clinic visit procedures, including the number of extraneous procedures, and length of trials have increased while enrollment and retention rates have decreased substantially in recent years [20, 21]. Participants often perceive joining a trial as inconvenient and time-consuming [22–25]. Telemedicine has been incorporated into asthma trials since 2001 and well-designed studies indicate mostly positive effects of the intervention [26]. However, no telemedicine trials in asthma have evaluated whether these strategies reduce clinical trials costs [27].
Heath information technologies have been used since the early 2000s to collect data from participants at home and the most common uses in asthma include symptom data, spirometry or peak flow data, and monitoring medication adherence [28–41]. Patients with asthma are enthusiastic about using mobile, internet or electronic means for recording data [39, 41–44]. Several studies have evaluated the quality and reliability of the data entered electronically and suggest that information may be more complete and accurate than data entered on written questionnaires [35, 36, 39].
In 2011, the National Institutes of Health (NIH) issued a Funding Opportunity Announcement entitled “Pilot Studies to Develop and Test Novel, Low-Cost Methods for the Conduct of Clinical Trials (RFA-HL-12-019)”. The goals for the application were to test new and innovative designs that have not been previously studied but that hold potential for increased efficiency and reduced cost of conducting clinical trials. Emphasis was to be placed on exploring novel methods for obtaining consent, reducing specialized infrastructure, minimizing visits, developing low-cost methods for monitoring study conduct, and testing the feasibility in a clinical trial.
These features have been incorporated into the Use of Mobile Devices and the Internet to Streamline an Asthma Clinical Trial (MICT) grant that will compare a streamlined design with a traditional clinical trial for pediatric asthma funded by the NIH (R01HL114899) and be conducted at outpatient clinics in the Nemours Children’s Health System located in Florida and the Delaware Valley. The purpose of this manuscript is to describe the methods and rationale for the streamlined trial.
MATERIAL AND METHODS
Trial Design
The traditional trial is a multi-center, double-blinded, placebo-controlled study designed to determine the optimal way to de-escalate therapy in patients with moderate persistent asthma that is well controlled on a fixed-dose combination of inhaled corticosteroid plus a long-acting beta2-agonist (Long-acting Beta Agonist Step Down Study [LASST, NCT01437995]). The trial is being conducted at 18 academic asthma research centers that are part of the American Lung Association Asthma Clinical Research Centers (ALA-ACRC) network. GlaxoSmithKline (GSK) provided funding and blinded drug for the trial but did not have input into the scientific design. The trial was conceived and designed by academic researchers of the ALA-ACRC.
The streamlined trial [MICT, NCT02061280] is modeled after the traditional trial. While the traditional is being conducted at all of the 18 ALA-ACRC academic sites including the Nemours Children’s Health System sites in Jacksonville FL, Orlando FL, and Wilmington DE, the streamlined trial is being conducted only at Nemours Children’s Health System sites (Jacksonville FL, Orlando FL, Pensacola FL, Wilmington DE, and Philadelphia PA). GSK had no input into the concept, design, or implementation of the streamlined trial. Researchers from the Nemours Children’s Health System and the ALA-ACRC Data Coordinating Center were responsible for the design of the streamlined trial.
The relationship between the trial designs for the streamlined and traditional trials is shown in Figures 1 and 2.
Figure 1.

Trial design for streamlined and traditional trials
The relationship between the study design for the streamlined (MICT) and traditional (LASST) clinical trials. MICT, Mobile Devices and the Internet to Streamline an Asthma Clinical Trial; LASST, Long-acting Beta Agonist Step Down Study. Participants are randomized to either the streamlined or traditional trial design.
Figure 2.
Details of visit type for streamlined trial design
Sequence of onsite and FaceTime virtual study visits in the streamlined trial design. Only the first and final study visits occur at the study site.
The specific aims of MICT are: to measure and compare consent comprehension using web-based delivery of informed consent material via a dynamic interactive multimedia platform (Aim 1); to compare timeliness and completeness of study questionnaire and diary data completed electronically using an iPad with wireless internet access, and quality of spirometry performed during FaceTime visits with study staff observing participants who are using an EasyOne Plus meter from their home (Aim 2); and to compare Asthma Control Test scores between the streamlined and traditional trial design in order to test whether employing the novel internet and mobile device methods in the streamlined approach alter the clinical trial’s clinically based outcomes (Aim 3). The outcomes for each aim will be compared with a concurrently conducted traditional clinical trial (LASST) also performed within the Nemours Children’s Health System.
The primary differences between the traditional trial and the streamlined trial are listed in Table 1.
Table 1.
Design differences between streamlined and traditional clinical trial.
| Streamlined (MICT) | Traditional (LASST) | |
|---|---|---|
| Study Duration | 20 weeks | 56 weeks |
| Sample Size | 120 | 450 |
| Ages | 12 to 17 years | 12 years and older |
| Informed Consent Process | Web-based delivery of informed consent material via a dynamic interactive multimedia platform and electronic informed consent documentation | Conventional face-to-face interaction with study staff and written documentation of informed consent |
| Study treatments | Open-label | Double-blinded |
| Primary clinical endpoints | Asthma Control Test | Episode of poor asthma control; Asthma Control Test is a secondary endpoint |
| Study site locations | Nemours Children’s Health System in Florida and the Delaware Valley | 18 academic asthma research centers located in the United States that are part of the ALA-ACRC (including Nemours Children’s Health System in Florida and the Delaware Valley) |
| Procedures being done in Traditional but not in Streamlined Trial | Exhaled nitric oxide measurement Asthma Symptom Utility Index questionnaire Asthma in Females questionnaire |
The shortened duration and smaller sample size of the streamlined study are due to the pilot nature of the grant. The streamlined trial is performed only in adolescents because the study is being conducted within a pediatric health-system that is only enrolling adolescents into the traditional trial. The consent processes differ because Aim 1 is to evaluate a novel method for obtaining informed consent (described below). Study treatments are open-label in the streamlined trial due to the unavailability of blinded drug from GSK. The Asthma Control Test (ACT) was selected as an alternative primary endpoint as the streamlined trial duration was not sufficiently long to evaluate episodes of poor asthma control in this pilot project with the NIH budget limits and proposed sample size. A one-year of follow-up period is typically required to capture episodes of poor asthma control, which is the duration of follow-up in the traditional trial. The ACT is being conducted at the same intervals in the streamlined and traditional trial. Furthermore, the Asthma Control Test is a patient reported outcome that is easier to assess than the primary outcome for the traditional trial, treatment failure. The Asthma Control Test is a 5-question Likert scale questionnaire that generates a score; a cut point has been validated to distinguish poor from well-controlled asthma [45]. The Nemours Children’s Health System locations are the only sites conducting the streamlined trial because of the need for a single electronic health record system and secure patient portal access for participants to have communication with the study coordinators. Certain procedures are conducted only in the traditional trial for practical reasons: Measurement of exhaled nitric oxide requires expensive equipment and supply costs and could not be purchased for all sites; the Asthma Symptom Utility Index questionnaire must be administered in person by a study coordinator whereas a goal of the streamlined trial is to have the questionnaires and forms self-administered and completed electronically off-site from the clinic; and the Asthma in Females questionnaire was expected to apply to only a small number of female participants.
Development of the multi-media Informed Consent Video for the Streamlined Trial
The RFA included a request to explore novel methods for obtaining consent. Therefore, we created a multi-media web-based informed consent video that provides study information including all the basic elements, as well as, additional elements of informed consent [14]. The intent was to translate complex study information into an understandable and visually appealing video format that is suitable for low health literacy participants and their family. The video is viewed online by potential study participants followed by informed consent discussion via telephone with the study coordinator; informed consent is documented electronically. The development of the video and website materials occurred with considerable input from Nemours ethics experts. Due to the non-standard nature of the proposed consent process, and the need to have ongoing IRB input into the design of the electronic consent and website content, IRB review and approval in this instance could best be described as an ongoing collaboration between the research team and Nemours IRB leadership. Co-authors Wysocki (IRB Chair) and Garfinkel (Director of Nemours Office of Human Subjects Protection) recused themselves from all official IRB deliberations about this study. The design and content of the video and supplementary materials were developed using theory and principles to facilitate electronic learning [46, 47].
The narrator script for video content was adapted from the 13-page single-spaced parental permission form used for the traditional trial. The Nemours web team and principal investigator developed a script for the proposed video images. IRB approval for the video script was sought prior to any video recording because changes to the video after shooting would have been excessively expensive. A professional video director and local actor talent was used to create the video. The video content is divided into five sections each 3- to 4-minutes in length: About this Study, Participating in the Study, Possible Benefits and Risks, Payment for Participating, and Protecting your Privacy. The 3- to 4-minute section duration was recommended by the Nemours web team as the length of time that most people are willing to watch a segment in one sitting (which is also about the average length of a YouTube video).
In addition, each video section has content-related sidebar information with a tab that changes color when the video reaches a point that is described in the sidebar. The participant can select a sidebar tab to read additional study details (Figure 3). A segment of the video may be viewed in the Supplementary Material.
Figure 3.
Screenshot of consent video navigation page
Streamlined trial consent web page demonstrating the 5 parts of the consent video. The sidebar material on the left side of the video image provides additional detail on the study and the tabs highlight as relevant parts of the video are played.
Creating the sidebar enabled us to keep the video length to about 15 minutes while providing additional information that the IRB required to be included for the informed consent process. For example, sidebar tabs “What is required for participation” and “What will the participants be asked to do” were created for the video section 2, “Participating in the Study”.
The 5 video sections must be viewed in sequence before the programming built into the video allows the viewer to progress to the next section. The participant can pause the video at anytime and resume where they left off. At the end of each video section, participants are required to answer 2 to 3 multiple-choice questions before the next video section becomes available. All responses, whether incorrect or correct, are provided with the correct answer to reinforce learning. Upon completing viewing of the final video section, participants are provided a button to select if they are ready to enroll. An automatic email is generated to viewers thanking them for their interest and an email is sent to the study staff indicating that the video has been viewed in its entirety. Data from video views are captured in one of several Research Electronic Data Capture (REDCap) [48] instruments designed for the study and include the date and time watched, who watched the video (parent, child, or other), which sections were viewed, responses to the quizzes, which sidebar tabs were selected, and the duration that the video was watched.
The Informed Consent Process
Aim 1 of the project is to measure and compare parent and adolescent comprehension of the study information provided during the informed consent process between the streamlined and traditional trials. The study team psychologists and principal investigator developed a 17-item open-ended question consent questionnaire designed to assess knowledge and comprehension of the consent material. The interview questions were derived from questionnaires previously developed by co-investigators of this grant (NCI R03CA133442, NCI R03CA133419). The study coordinators are trained by the psychology staff to ask each interview question and to use non-leading prompts to elicit further knowledge when appropriate. Each consent interview question is scored by two coders as incorrect, partially correct, or correct.
To assess health literacy, each parent and adolescent is administered the Newest Vital Sign tool and results will be used as a covariate in analyses [49–51] [52–54]. The Newest Vital Sign (based on a nutrition label from an ice cream container) was selected over other measures of health literacy because it is a valid and reliable screening tool in both parents and caregivers of adolescents, and in adolescents; requires only 3 to 4 minutes to complete; and it has no ceiling effect [50, 52–55].
Streamlined Trial Informed Consent Process
After viewing the consent video and website materials, the parent and adolescent are scheduled for a one-on-one telephone call with the study coordinator to conduct the informed consent interview and the Newest Vital Sign. The telephone interaction is audio recorded (with consent from the parent and participant) using Cisco Webex™ for later analysis by the coders. The consent interview questions are administered separately to the parent and adolescent in order to measure comprehension for each independently. The parent is instructed to have the adolescent away from the phone during the interview and to not provide cues to the adolescent during their interview. After the consent interview is complete, the coordinator reviews study understanding and answers any remaining questions.
To obtain electronic documentation of informed consent, a short single-page parental permission form was adapted from the signature page of Nemours parental permission and assent IRB template forms. The forms are sent to MyNemours accounts (MyChart®, Epic®), secure online patient portals for Nemours patients and families, that have been set up separately for the parent and adolescent [56]. The parental permission is sent to the parent’s MyNemours account and the assent is sent to the adolescent’s MyNemours account. The parental permission form has radio buttons to capture discrete responses for willingness to participate, relationship to the adolescent (parent or legal guardian), sending pulmonary function testing results to their primary care physician, and DNA storage. A short form was developed for pediatric assent. The parent and adolescent type their names onto the parental permission form and assent forms, respectively, and submit the document. The submitted document (with the date and time submitted) is stored in Epic® as part of the participant’s electronic health record.
Documentation of legal guardianship is determined prior to any MyNemours account being created within the Nemours Children’s Health System. Because Epic already meets 21 CFR [57] requirements, legal guardianship is verified through Nemours standard processes, and tracking of who sent the form and who submitted the form (an audit trail can be followed), this consent process was determined to meet the standards for electronic documentation of informed consent.
Traditional Trial Informed Consent Process
Informed consent consisting of parental permission and adolescent assent is obtained in a conventional face-to-face manner between the parent and adolescent and the study coordinator. The parent and adolescent are provided the consent documents upon arrival at their initial visit (or the documents may have been emailed/mailed to the family at their request ahead of the appointment) and allowed as much time as needed, usually about 20 to 30 minutes, to review the document (13 single-spaced pages including the signature page). The coordinator conducts the consent comprehension interview and Newest Vital Sign separately with the parent and then invites the adolescent into the room for an interview and Newest Vital Sign assessment. Because the parent is still in the room with the child, the coordinator instructs the parent not to cue the adolescent with answers to the interview questions. After the consent interview questions are completed, the coordinator reviews any incorrect responses and answers any remaining questions before obtaining parent and adolescent signatures on the parental permission form and assent documents, respectively. The entire interaction is audio recorded using the Audacity program [58] for later analysis by the coders; written informed consent from the parent and assent from the adolescent is obtained prior to audio recording.
Development of the Study Website
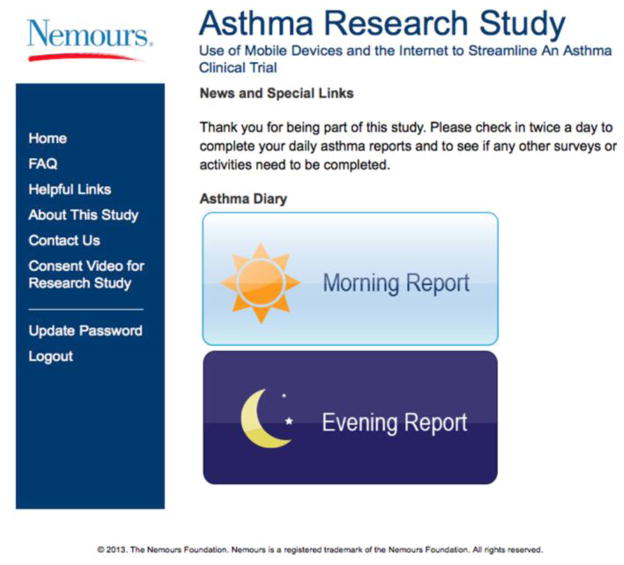
The study website is made available to streamlined trial participants who have provided consent and completed Visit 1. The study website was developed by the Nemours Bioinformatics Core Facility with the input from Nemours Web Development Team to be intuitively easy to use and visually appealing (Figure 4). The website is accessed by any device with internet connection using a unique username and password for each participant. Each participant is provided with an iPad with Wi-Fi at Visit 1. The iPad has been pre-configured with iPad passcodes and study Gmail accounts for use by each individual participant. The iPad is used to complete the Morning Report and Evening Report by simply tapping an icon (Figure 5) or can be accessed by any device with an internet connection by going to the study website and logging in.
Figure 4.
Screenshot of study webpage for morning and evening data entry
Streamlined trial study site webpage for entering symptom report data each morning and evening. Additional information can be accessed by selecting the links on the left.
Figure 5.

Screenshot of iPad dock icons
The iPad dock icons including (left to right) study Gmail account, preloaded contact information for FaceTime appointments, video for using the EasyOne and conducting FaceTime appointments, login screen for the consent and study websites, Morning Report for entering PEF and medication use, Evening Report for entering symptoms and unscheduled medication use.
PEF, peak expiratory flow.
The study website is the primary access point for entering peak expiratory flow and symptom data every morning and evening. A unique feature of the study website is that the Morning and Evening Reports section is open for data entry only during specific time intervals (morning: 3AM to 3PM and evening: 3PM to 3AM) which prevents back filling of diary data often seen with paper forms [41]. Peak expiratory flows are entered on the Morning Report and the participant’s personalized Asthma Action Plan will open up automatically if the day’s value is in the yellow or red zone. Once the user has logged into the study website for the first time on their iPad, a cookie is stored on the device and subsequent access to the Morning or Evening Report can be done by simply tapping the icon. Data from each entry is stored in the REDCap system and can be accessed by the study staff 24/7 [48]. Features in REDCap that are advantageous for this project include: (1) user authentication and role-based security, (2) intuitive case report forms, (3) real-time data validation and data integrity checks, (3) audit capabilities, (4) central data storage and backups, and (5) data export to commonly used statistical packages [48].
Because the data are captured in real-time in REDCap, several safety features are incorporated into the study for the Morning and Evening Reports. Automatic emails are sent to the study coordinator when the participant enters:
A peak expiratory flow value in the red zone for two consecutive days;
New or increased use of asthma medications;
An urgent or unscheduled visit for medical care (Figure 6 and Figure 7);
Study Diskus counter numbers that indicate adherence is below 75%, or ProAir counter numbers that indicate 10 or more puffs of albuterol (one nebulizer treatment = 2 puffs) are used two days in a row;
No morning or evening report submissions for 3 days in a row.
Figure 6.
Screenshot of evening report data entry screen
Example of drop down questions that appear if the participant selects that they required unscheduled medical care on the Evening Report.
Figure 7.

Screenshot of alert email to study coordinators
Example of an email received by the study coordinator when a participant submits an Evening Report indicating unscheduled medical care. Any text that the participant includes in the Evening Report submission is included in the email.
For each morning or evening entry submitted, the participant earns $1 ($2/day); the total potential amount that can be earned for twice daily reporting is approximately $300. The study website can be accessed 24/7and has links including their personalized asthma action plan, instructional videos on how to use the study medications, and national websites for asthma information.
Randomization and Trial Procedures
Participants undergo two randomizations, the first to trial (MICT or LASST) and the second to treatment assignment. The study staff log into a website created by the ALA-ACRC data coordinating center (Johns Hopkins University) to generate randomizations that are stratified by site to minimize biases due to site variability. The trial randomizations are stratified for the Jacksonville FL, Orlando FL, and Wilmington DE sites as these are the sites participating in both the streamlined and traditional trials. The trial randomization uses a modified Zelen design in which potential participants are randomized to be approached about enrolling in the traditional or streamlined trial prior to obtaining consent to participate in the trial [59, 60]. Random treatment assignments are assigned at Visit 3 after ensuring that participants meet all criteria for study continuation, primarily that the participant has stable asthma and is suitable for de-escalation of asthma therapy. The streamlined trial is also randomized by site for treatment assignment at the participating sites Jacksonville FL, Orlando FL, Pensacola, FL, Wilmington DE, and Philadelphia PA. The traditional trial treatment allocation is generated by the ALA-ACRC data coordinating center for the 18 academic sites participating, for which the Nemours Pediatric Health System is considered a single site. Primary inclusion and exclusion criteria are shown in Table 2. The time and events schedule for the streamlined trial are shown in Table 3.
Table 2.
Primary Inclusion and Exclusion Criteria
| Inclusion Criteria | |
|---|---|
| Age |
|
| Diagnosis | Physician diagnosed asthma (without any other co-morbid pulmonary disease) |
| Required Daily Medication at Baseline (any combination of medium-dose inhaled corticosteroid plus long-acting beta agonist given twice daily) |
Or a combination of medium dose ICS + long-acting beta agonist:
PLUS Long-acting beta agonist
|
| Asthma Control | Asthma Control Test score ≥ 20, and the absence of unscheduled visits or use of rescue prednisone for 4 weeks prior to enrollment 45, 60 |
| FEV1 | Pre-bronchodilator FEV1 ≥ 70% predicted |
| Smoking History | < 10 pack/year history of tobacco use and abstinence for at least 1 year |
| Exclusion Criteria | |
| Chronic oral steroid therapy | |
| Hospitalization or urgent care visit within 4 weeks of the screening visit | |
| Near fatal asthma within 2 years of enrollment or high risk of near fatal or fatal asthma 61–63 | |
| Women who are pregnant or lactating | |
Table 3.
Time and Events Schedule
| Visit | V0 | V1 Part 1a | V1 Part 2b | V2 | V3 | V4 | V5 | V6 Part 1a | V6 Part 2b |
|---|---|---|---|---|---|---|---|---|---|
| Time Window (weeks) | −12 to −10 | −10 to −6 | −6 to −2 | 2–4 | 5–7 | 11–13 | |||
| Target (week) | −11 | −8 | −4 | 0 | 3 | 6 | 12 | ||
| Type of visit 1 | Pre V1 Eligibility | Phone | Clinic | iPad/ FaceTime | iPad FaceTime | iPad FaceTime | iPad FaceTime | iPad FaceTime | Clinic |
| Trial Randomization | x | ||||||||
| Consent | x | ||||||||
| Eligibility evaluation2 | x | x | x | x | |||||
| Procedures | |||||||||
| Pregnancy test | x | ||||||||
| Blood (DNA, allergy) | x | ||||||||
| Height and Weight3 | x | x | x | x | x | x | |||
| Vital Signs | x | x | |||||||
| Physical Exam | x | x | |||||||
| Treatment Randomization5 | x | ||||||||
| Consent Interview | x | x | |||||||
| Exhaled nitric oxide (selected sites) | x | x | |||||||
| Spirometry Pre and Post 6 | x | x | x | x | x | ||||
| Questionnairesc | |||||||||
| Screening Form | x | x | |||||||
| Baseline asthma and medical history | x | ||||||||
| Asthma Control Test | x | x | x | x | x | x | |||
| Children’s Health Survey for Asthma | x | x | x | x | |||||
| Clinic Visit Form | x | x | x | x | x | ||||
| EQ-5D | x | x | |||||||
| Quality of Life | x | x | x | x | |||||
| Complete Morning and Evening reports on iPad | x | x | x | x | x | ||||
| Medication and device distribution | |||||||||
| Treatment medication distribution4 | x | x | x | x | x | x | x | ||
| iPad Daily Report/PEF/AAP review | x | x | x | x | x | x | |||
| Receive/Return iPad and EasyOne8 | x | X | |||||||
Conducted during FaceTime visit
Conducted at clinic site
Questionnaires are completed online prior to each iPad/FaceTime visit
Participant identification and recruitment
Participants for the streamlined and traditional trial are identified and recruited in the same manner. Nemours implemented an electronic health record (EHR) (Epic Systems, Verona, WI) in 1998 with rollout to all Nemours campuses completed by 2005. Thus, Nemours has an extensive database of children with asthma from which to identify potentially suitable participants. An EPIC data warehouse query is generated using the inclusion criteria for age, diagnosis of asthma (ICD-9 code, 493.x), and medication prescribed on the most recent clinic visit. The recruiting staff reviews the EHR record for any information that would indicate the participant has unstable asthma or is otherwise unsuitable for participation. Any medical questions about a potential participant are resolved by discussions with the principal investigator, study physician, and study coordinator prior to initiating contact with the family. Once a suitable participant is identified, the recruiter performs the trial assignment and contacts the family by telephone and leaves a voice message if needed. Second and third attempts to reach families for unreturned calls are initiated two and three weeks later, and if still no response a flyer is sent with study information. In addition, “patient lists”, a feature of EPIC, are created for potential participants we have attempted to reach. These lists alert the study staff when the patient is coming to Nemours for a clinic appointment for any subspecialty. The staff contacts the family to let them know we will attempt to speak with them while at the clinic. In addition, we distribute flyers at health fairs, non-Nemours physician offices, and other locations; have information on Nemours Facebook page; and conduct interviews with local TV stations. Potential participants who have been randomized to the streamlined trial and who indicate preliminary interest in the study have data entered into REDCap, which will trigger an email contact with a unique link inviting the participant to view the consent video.
Study Visits for the Streamlined Trial
Only the first and last study visits are conducted onsite at the clinic in the streamlined trial; all other visits are conducted by FaceTime using the iPad. Prior to the onsite or FaceTime appointments (including Visit 1), participants are sent secure links from REDCap or via php code to their study email account to complete questionnaires including Asthma Control Test, Clinic Visit Assessment form, Quality of Life, and EuroQol-5 Dimensions (EQ-5D). These links are participant specific and once completed and submitted, the data are stored on the REDCap server in that participant’s data record. If eligibility is confirmed at Visit 1, the participant receives their iPad, which has been pre-loaded with icons for the study Gmail account; FaceTime contacts; videos for how to perform spirometry and do the FaceTime visits, and use the EasyOne handheld Spirometer; the study website; and morning and evening reports. The participant is trained on use of the EasyOne and baseline PFTs are obtained. The EasyOne device was selected because of its accurate and reliable measures of lung function in pediatric patients [65] and suitability for collection of longitudinal data [66]. Data values that indicate worsening of asthma control trigger alert emails sent to the study coordinators to prompt further review. During the FaceTime appointments, the study coordinator reviews unresolved email alerts, morning and evening report adherence, medication issues; and conducts spirometry. At the final visit, the EasyOne is returned and spirometry data is downloaded. The iPad is configured for personal use and returned to the participant to keep.
Payment for Study Participation
In the streamlined trial, participants are paid using the CT Payer system. CT Payer is an online payment operation system that allows for HIPAA safe payments using reloadable prepaid MasterCards to clinical trial participants [67]. When participants complete study responsibilities, research staff pay them immediately for onsite or FaceTime appointments and bi-weekly for Morning and Evening Report submissions, by loading payment onto their card via the CT Payer online utility. Payments to traditional trial participants are made through generating stipend requests by the coordinator that are routed through the Nemours Research Administration office, and then to Nemours Accounting Department. A paper cheque is generated which is then mailed to the participant’s home address. Participants are paid following each clinic visit.
Tracking Study Costs
Determining study costs is an essential component of the streamlined and traditional trials. Nemours has had an online effort reporting system for over 10 years in which research staff record time spent on each research project individually on a daily basis. In order to obtain more granular data for this project, the study staff keep stopwatches with them at all times to record the time for both the traditional and streamlined trial. Data collection for tracked effort is divided into discrete sections and subsections:
Preparing participant information for visit (chart reviews, paperwork preparation)
Pre-visit procedures
Onsite or FaceTime visit procedures
Post-visit procedures
Consenting procedures
Charting and interim visit procedures
We will use salary data to determine the staff costs for conducting the traditional and streamlined clinical trials. Study infrastructure (study website and consent video) start-up costs including IRB submission will be included for the streamlined trial. Because of its novel design, the streamlined trial required considerable interaction with the IRB prior to submission which differs from typical clinical trial submissions to the IRB. We will also include the costs required at our institution for processing stipend cheques to trial participants for the traditional trial and the CT Payer payments for the streamlined trial.
Satisfaction Survey for the Consent Process
A satisfaction survey was developed specifically to evaluate the parent’s satisfaction with the consent process for both the streamlined and traditional trials. The electronic survey is sent to parents of participants through REDCap after Visit 1 in the streamlined and traditional trials. On each survey, parents are asked about their satisfaction on the amount of and the way information was provided as well as key questions to determine if the consent process provided them with the necessary information to make a well-informed decision about participation. In addition, a slider scale is provided to determine their preference for the video website and phone call at one extreme and written consent with in-person meeting with the study staff at the other extreme.
Data Analysis
The sample size was determined for Specific Aim 1 (comprehension and retention following the consent interview between participants enrolled in the streamlined and traditional trial), with subsequent assessment of detectable differences for Specific Aims 2 and 3 using that sample size. Because our hypothesis is that our novel web-based consent process will be at least as good as the traditional process, we have elected to use a non-inferiority design. We used the preliminary data from two R03 grants on consent comprehension, assumed normalcy of the data, and defined the non-inferiority margin as 2.4, which corresponds to 0.5 standard deviation units to calculate the power for a range of sample sizes.
Based on these calculations and other considerations discussed below, we propose to randomize 120 participants: 60 participants into the streamlined trial and 60 participants into the traditional trial. This will give us greater than 80% power to reject the hypothesis that the web-based consent process yields significantly lower scores than the traditional process at a threshold of 2.4 units on the consent interview scale, after allowing for approximately 10% loss to follow-up.
For Aim 2, because we are unaware of meaningful measures to establish non-inferiority margins for completeness and quality of data collection, we will use 0.5 SD as a qualitative measure of non-inferiority. We anticipate this sample size will allow us to estimate the proportion of study days with diary data with a 95% confidence interval width of 15%. For example, in a recently completed ALA-ACRC pediatric trial, the proportion of days with a diary card entry was 90%, the corresponding 95% confidence interval would be 82.5% to 97.5%. The second objective of Aim 2 is to evaluate the comparability of the quality of spirometry from the streamlined and traditional trials. We will employ the spirometry review system currently used in an ALA-ACRC trial, which grades each spirometry session with a letter grade (A to F). For initial spirometry sessions, the current overall Grade Point Average (GPA) is 3.68, with a standard deviation of 0.67. Using these values, with a sample size of 60 in each of the traditional and streamlined trials, we expect to be able to estimate spirometry quality using a similar review system with a 95% confidence interval ranging from approximately 3.51 to 3.85, which should be adequate to allow us to compare spirometry quality in the two groups.
For Aim 3, we will have greater than 90% power to detect a clinically meaningful difference of 3 in the ACT score [61, 68] between one of the treatment arms in the traditional trial and the corresponding treatment arm in the streamlined trial, assuming a mean score of 19 with a standard deviation of 4 (data from a ALA-ACRC trial).
We will compare the consent interview scores of those participating in the streamlined trial with those participating in the traditional trial (Specific Aim 1) and data completeness and quality GPA (Specific Aim 2) using t-tests without adjustment to estimate the differences in scores. We will consider the novel interactive consent process to be non-inferior to the traditional process if the upper bound of the 95% confidence interval for the difference (traditional minus streamlined) is less than 2.4, our a priori margin of non-inferiority as determined from pilot data using the assessment. We will use a similar approach for the evaluating non-inferiority of data quality.
For Aim 3, we will compare ACT scores within each treatment group between the traditional and streamlined groups, using a multivariate regression model that incorporates both trial and treatment group. We will evaluate the contrast for each treatment group and determine if there is evidence to support an interaction between treatment group and trial. If there is not sufficient evidence to support an interaction, we will perform the test of the trial effect on the change in ACT score without including an interaction term. In all cases, primary analyses will use crude (unadjusted) comparisons, although we will also report analyses that include adjustments for possible differences between the streamlined and traditional groups in important demographic characteristics.
Progress and Challenges
The primary challenge for the project has been participant recruitment. Identification of suitable participants is predicated on the traditional trial inclusion and exclusion criteria, which are used for the streamlined trial. Because Nemours is a pediatric institution, we are limited to enrollment of adolescents 12 through 17 years old whereas other sites within the ALA-ACRC are able to enroll adults. However, Nemours has recruited very successfully for ALA-ACRC trials for the past 15 years by enrolling participants from the organization’s subspecialty pulmonary and allergy clinics. To bolster recruitment, we have added sites within the Nemours primary care network to refer patients to the trial. Nemours has over 30 primary care sites in the Delaware Valley and 12 surrounding the Nemours Children’s Hospital in Orlando. Adding the primary care sites will also increase the robustness of the data.
Because enrollment for the traditional trial was competitive across the 18 ALA-ACRC sites, the streamlined trial was faced with matching the traditional trial enrollment deadline which ended in July 2014. Enrollment for the traditional trial began in the summer of 2012 and the streamlined study website was ready in June 2013. Therefore, we began collecting data in January 2013 for the consent comprehension portion of the project in traditional trial participants before the trial randomization process began to ensure adequate data were collected for Aim 1. To date, we have enrolled 31 participants in the streamlined trial and 37 in the traditional trial.
In addition, early in the trial we found that sending emails with the study questionnaire links far in advance of the clinic or FaceTime appointment resulted in participants not completing the questionnaires in a timely manner. Thus, we changed our process such that the questionnaires are sent 4 days and 3 nights before the scheduled appointment. The study staff monitor for questionnaire completion in REDCap as the visit approaches but at times follow-up text messages and phone calls are required.
DISCUSSION
This grant was funded through NHLBI in response to RFA-HL-12-019 “Pilot Studies to Develop and Test Novel, Low-Cost Methods for the Conduct of Clinical Trials” for 4-years starting in August 2012. The project received IRB approval in June 2012 to develop the study processes including the novel consenting component. The consent video script and the electronic consenting process were approved by the IRB in May 2013. The study website was completed in June 2013.
Phase III/IV trials are often complex and involve considerable staff time and numerous study procedures. Over the 1999 to 2005 period, Phase III staff work burden increased by nearly 70% and median number of study procedures by 65% according to one report [21]. Thus, the typical Phase III/IV trial design provided an opportunity to create a study which could focus on reducing the number of procedures performed by study staff and reduce the amount of time the study staff spend at clinic visit appointments with study participants. To optimally compare two study designs, it is important that the trials run concurrently by the same study staff that have all received the same training for each of the projects. At the time the RFA was posted, we were fortunate that the ALA-ACRC network was finalizing LASST, a large Phase IV comparative effectiveness trial, of traditional proportions in both sample size and number of procedures. Our streamlined trial was designed to shorten the consent process from the study staff perspective, and eliminate as much of the pre-study visit, onsite study visit, and immediate post-study visit procedures for the study staff. One other area we chose to focus on was eliminating the tedious process for requisitioning paper cheques for participant stipends that involves multiple steps, individuals, and departments before they are mailed to participants. Each step in the stipend process is another opportunity for problems and delays so we chose to work with CT Payer for online payments. CT Payer had reasonable start-up fees and easy setup process.
There are few recently published data on costs for conducting clinical trials [69–71]. Therefore, we developed a process for capturing granular data on the time taken to conduct each study step by the study staff for both the traditional and streamlined trial. Having the same staff conduct both the traditional and streamlined trials will allow for accurate comparison of study expenses. Data are recorded in real-time by having all study staff use stopwatches to record the time spent.
At the time the study was developed, there were fewer tablet devices on the market than are available currently. The intent was to have a device the participants could use to complete study questionnaires from home with an integrated email program for sending/receiving the questionnaires. In addition, in order to assess participant effort when performing spirometry for scheduled appointments, we needed a device that would allow us to view their spirometry technique in real time. While we could have used a video conferencing program such as Skype for most any device, it would have meant setting up additional accounts and passwords whereas the Apple iPad had FaceTime integrated into the system. We also debated about including a security program, Mobile Iron Sentry, on the iPad to allow study staff to track the device should it be lost or stolen. However, the iPad 2 iOS (the device we purchased for the project) would not prevent the device from being wiped even with Mobile Iron and could be set up for a new user should it be stolen. With each iPad we provided the participants with a Defender case to minimize the chance for damage should the iPad be dropped. So far no iPads have been lost or stolen and only one iPad developed a crack on the screen but was not replaced.
We also debated whether to use iPads with Wi-Fi only or cellular service. The intent was to allow participants to have 24/7 internet access for the purpose of completing questionnaires and morning and evening reports without service interruption. However, there was concern that the cellular data plan could be easily used up by adolescents before the service month ended and then there might be difficulty completing the study procedures. Therefore, we decided to purchase iPads with Wi-Fi capability. We purchased a limited number of Sprint hotspots for families without Wi-Fi to borrow for the study period or if they were travelling and would not have Wi-Fi at their destination. Thus far, only 20% of participants have required hotspot use.
REDCap has been very functional for the study purpose. We selected using REDCap to house the data because we had a bioinformatics team that is highly experienced in its use and it is available to institutions worldwide. In addition, our intent is to have our data system be freely available to other investigators after the trial is complete. Currently, REDCap is used in over 1300 institutions in 86 countries by 134,000 projects [48, 72].
Conclusion
We have developed a multi-media informed consent process that allows for electronic documentation of consent that families can complete from home. The process meets both federal and ethical requirements for electronic signature and engaging in a consent process with families, respectively. In addition, we used REDCap, a database system widely available at academic centers around the world, to send participant specific questionnaires by email and receive completed responses without the need for external data entry. This approach was developed to improve the efficiency of and reduce the costs of conducting large clinical trials. These processes will be applicable to clinical trials in most therapeutic areas.
Supplementary Material
Section 1, “About this Study” of the informed consent video that is viewed by potential participants in the streamlined trial prior to the informed consent discussion with the study staff. There are 5 sections to the video, “About this Study”, “Participating in the Study”, “Possible Benefits and Risks”, “Payment for Participating”, and “Protecting your Privacy”. The website programming requires participants to view the video sections in sequence. At the end of each section are 2 to 3 multiple-choice questions to reinforce learning. The entire video is about 15 minutes in length. In addition, the consent video website contains supplementary information related to the video content in the sidebar.
Acknowledgments
Supported by NIH grant 101HL114899 (to K. Blake); ClinicalTrials.gov Identifier: NCT02061280
The authors gratefully acknowledge the efforts of Yang Li, Kate Norton, and Ferdie Martinez on the webpage design and REDCap infrastructure. In addition, the critical evaluation of study logistics provided by Stacey Gray and Nancy Archer, RN were invaluable during study start-up.
Footnotes
All work is being performed through the Center for Pharmacogenomics and Translational Research, Nemours Children’s Clinic, Jacksonville, FL, Nemours Children’s Hospital, Orlando FL, Nemours Children’s Clinic, Pensacola, and Nemours/Alfred I. duPont Hospital and Nemours duPont Pediatrics in the Delaware Valley, USA.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Kathryn Blake, Email: kathryn.blake@nemours.org.
Janet T. Holbrook, Email: janet.holbrook@jhu.edu.
Holly Antal, Email: holly.antal@nemours.org.
David Shade, Email: dshade1@jhu.edu.
H. Timothy Bunnell, Email: tim.bunnell@nemours.org.
Suzanne M. McCahan, Email: Suzanne.mccahan@nemours.org.
Robert A. Wise, Email: rwise@jhmi.edu.
Chris Pennington, Email: chris.pennington@nemours.org.
Paul Garfinkel, Email: paul.garfinkel@nemours.org.
Tim Wysocki, Email: tim.wysocki@nemours.org.
References
- 1.Roy ASA. STIFLING NEW CURES: The True Cost of Lengthy Clinical Drug Trials. Manhattan Institute for Policy Research; 2012. [Accessed October 10, 2014]. at http://www.manhattan-institute.org/html/fda_05.htm. [Google Scholar]
- 2.Silverman E. Clinical Trial Costs Are Rising Rapidly. Pharmalot: Wall Street Journal. 2011 [Google Scholar]
- 3.Phase 3 Clinical Trial Costs Exceed $26,000 per Patient. [Accessed 09/30/2011];PR Newswire. 2006 at http://www.lifesciencesworld.com/news/view/11080.
- 4.Tamariz L, Palacio A, Robert M, Marcus EN. Improving the informed consent process for research subjects with low literacy: a systematic review. J Gen Intern Med. 2013;28:121–6. doi: 10.1007/s11606-012-2133-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Palmer BW, Lanouette NM, Jeste DV. Effectiveness of multimedia aids to enhance comprehension of research consent information: a systematic review. IRB. 2012;34:1–15. [PMC free article] [PubMed] [Google Scholar]
- 6.Cico SJ, Vogeley E, Doyle WJ. Informed consent language and parents’ willingness to enroll their children in research. IRB. 2011;33:6–13. [PubMed] [Google Scholar]
- 7.Stunkel L, Benson M, McLellan L, Sinaii N, Bedarida G, Emanuel E, et al. Comprehension and informed consent: assessing the effect of a short consent form. IRB. 2010;32:1–9. [PMC free article] [PubMed] [Google Scholar]
- 8.Tait AR, Voepel-Lewis T, Zikmund-Fisher BJ, Fagerlin A. Presenting research risks and benefits to parents: does format matter? Anesth Analg. 2010;111:718–23. doi: 10.1213/ANE.0b013e3181e8570a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tait AR, Voepel-Lewis T, Malviya S. Do they understand? (part I): parental consent for children participating in clinical anesthesia and surgery research. Anesthesiology. 2003;98:603–8. doi: 10.1097/00000542-200303000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Stryker JE, Wray RJ, Emmons KM, Winer E, Demetri G. Understanding the decisions of cancer clinical trial participants to enter research studies: factors associated with informed consent, patient satisfaction, and decisional regret. Patient Educ Couns. 2006;63:104–9. doi: 10.1016/j.pec.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 11.Barrett R. Quality of informed consent: measuring understanding among participants in oncology clinical trials. Oncol Nurs Forum. 2005;32:751–5. doi: 10.1188/05.ONF.751-755. [DOI] [PubMed] [Google Scholar]
- 12.Sanchini V, Reni M, Calori G, Riva E, Reichlin M. Informed consent as an ethical requirement in clinical trials: an old, but still unresolved issue. An observational study to evaluate patient’s informed consent comprehension. J Med Ethics. 2014;40:269–75. doi: 10.1136/medethics-2012-101115. [DOI] [PubMed] [Google Scholar]
- 13.Kripalani S, Bengtzen R, Henderson LE, Jacobson TA. Clinical research in low-literacy populations: using teach-back to assess comprehension of informed consent and privacy information. IRB. 2008;30:13–9. [PubMed] [Google Scholar]
- 14.Adminstration FaD, editor. Code of Federal Regulations Title 21 Part 50 Subpart B Section 50.25: Elements of Informed Consent. Bethesda: 2011. [Google Scholar]
- 15.Flory J, Emanuel E. Interventions to improve research participants’ understanding in informed consent for research: a systematic review. JAMA. 2004;292:1593–601. doi: 10.1001/jama.292.13.1593. [DOI] [PubMed] [Google Scholar]
- 16.Kodish ED, Pentz RD, Noll RB, Ruccione K, Buckley J, Lange BJ. Informed consent in the Childrens Cancer Group: results of preliminary research. Cancer. 1998;82:2467–81. doi: 10.1002/(sici)1097-0142(19980615)82:12<2467::aid-cncr22>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 17.Sachs GA, Hougham GW, Sugarman J, Agre P, Broome ME, Geller G, et al. Conducting empirical research on informed consent: challenges and questions. IRB. 2003;(Suppl 25):S4–S10. [PubMed] [Google Scholar]
- 18.Nishimura A, Carey J, Erwin PJ, Tilburt JC, Murad MH, McCormick JB. Improving understanding in the research informed consent process: a systematic review of 54 interventions tested in randomized control trials. BMC medical ethics. 2013;14:28. doi: 10.1186/1472-6939-14-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O’Lonergan TA, Forster-Harwood JE. Novel approach to parental permission and child assent for research: improving comprehension. Pediatrics. 2011;127:917–24. doi: 10.1542/peds.2010-3283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Development TCftSoD. [Accessed October 10, 2014];Outlook 2013. 2013 at http://csdd.tufts.edu/reports/outlook_reports.)
- 21.Roy ASA. Stifling New Cures: The True Cost of Lengthy Clinical Drug Trials. Manhattan Institute for Policy Research; 2012. [Accessed October 10, 2014]. at http://www.manhattan-institute.org/html/fda_05.htm. [Google Scholar]
- 22.Zook PM, Jordan C, Adams B, Visness CM, Walter M, Pollenz K, et al. Retention strategies and predictors of attrition in an urban pediatric asthma study. Clin Trials. 2010;7:400–10. doi: 10.1177/1740774510373798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sen Biswas M, Newby LK, Bastian LA, Peterson ED, Sugarman J. Who refuses enrollment in cardiac clinical trials? Clin Trials. 2007;4:258–63. doi: 10.1177/1740774507079434. [DOI] [PubMed] [Google Scholar]
- 24.Ellis PM, Butow PN, Tattersall MH, Dunn SM, Houssami N. Randomized clinical trials in oncology: understanding and attitudes predict willingness to participate. J Clin Oncol. 2001;19:3554–61. doi: 10.1200/JCO.2001.19.15.3554. [DOI] [PubMed] [Google Scholar]
- 25.Grunfeld E, Zitzelsberger L, Coristine M, Aspelund F. Barriers and facilitators to enrollment in cancer clinical trials: qualitative study of the perspectives of clinical research associates. Cancer. 2002;95:1577–83. doi: 10.1002/cncr.10862. [DOI] [PubMed] [Google Scholar]
- 26.Wootton R. Twenty years of telemedicine in chronic disease management--an evidence synthesis. Journal of telemedicine and telecare. 2012;18:211–20. doi: 10.1258/jtt.2012.120219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morrison D, Wyke S, Agur K, Cameron EJ, Docking RI, Mackenzie AM, et al. Digital asthma self-management interventions: a systematic review. J Med Internet Res. 2014;16:e51. doi: 10.2196/jmir.2814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Runge C, Lecheler J, Horn M, Tews JT, Schaefer M. Outcomes of a Web-based patient education program for asthmatic children and adolescents. Chest. 2006;129:581–93. doi: 10.1378/chest.129.3.581. [DOI] [PubMed] [Google Scholar]
- 29.Carter ER, Ananthakrishnan M. Adherence to montelukast versus inhaled corticosteroids in children with asthma. Pediatr Pulmonol. 2003;36:301–4. doi: 10.1002/ppul.10318. [DOI] [PubMed] [Google Scholar]
- 30.van der Meer V, van Stel HF, Detmar SB, Otten W, Sterk PJ, Sont JK. Internet-based self-management offers an opportunity to achieve better asthma control in adolescents. Chest. 2007;132:112–9. doi: 10.1378/chest.06-2787. [DOI] [PubMed] [Google Scholar]
- 31.Joseph CL, Peterson E, Havstad S, Johnson CC, Hoerauf S, Stringer S, et al. A web-based, tailored asthma management program for urban African-American high school students. Am J Respir Crit Care Med. 2007;175:888–95. doi: 10.1164/rccm.200608-1244OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Grad R, McClure L, Zhang S, Mangan J, Gibson L, Gerald L. Peak flow measurements in children with asthma: what happens at school? J Asthma. 2009;46:535–40. doi: 10.1080/02770900802468509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wise M, Pulvermacher A, Shanovich KK, Gustafson DH, Sorkness C, Bhattacharya A. Using action research to implement an integrated pediatric asthma case management and eHealth intervention for low-income families. Health Promot Pract. 2010;11:798–806. doi: 10.1177/1524839909334621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barbot O, Platt R, Marchese C. Using preprinted rescue medication order forms and health information technology to monitor and improve the quality of care for students with asthma in New York City public schools. J Sch Health. 2006;76:329–32. doi: 10.1111/j.1746-1561.2006.00122.x. [DOI] [PubMed] [Google Scholar]
- 35.Raat H, Mangunkusumo RT, Mohangoo AD, Juniper EF, Van Der Lei J. Internet and written respiratory questionnaires yield equivalent results for adolescents. Pediatr Pulmonol. 2007;42:357–61. doi: 10.1002/ppul.20576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vargas PA, Robles E, Harris J, Radford P. Using information technology to reduce asthma disparities in underserved populations: a pilot study. J Asthma. 2010;47:889–94. doi: 10.3109/02770903.2010.497887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Burkhart PV, Rayens MK, Oakley MG, Abshire DA, Zhang M. Testing an intervention to promote children’s adherence to asthma self-management. J Nurs Scholarsh. 2007;39:133–40. doi: 10.1111/j.1547-5069.2007.00158.x. [DOI] [PubMed] [Google Scholar]
- 38.Wise M, Gustafson DH, Sorkness CA, Molfenter T, Staresinic A, Meis T, et al. Internet telehealth for pediatric asthma case management: integrating computerized and case manager features for tailoring a Web-based asthma education program. Health Promot Pract. 2007;8:282–91. doi: 10.1177/1524839906289983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mangunkusumo RT, Duisterhout JS, de Graaff N, Maarsingh EJ, de Koning HJ, Raat H. Internet versus paper mode of health and health behavior questionnaires in elementary schools: asthma and fruit as examples. J Sch Health. 2006;76:80–6. doi: 10.1111/j.1746-1561.2006.00072.x. [DOI] [PubMed] [Google Scholar]
- 40.Gentles SJ, Lokker C, McKibbon KA. Health information technology to facilitate communication involving health care providers, caregivers, and pediatric patients: a scoping review. J Med Internet Res. 2010;12:e22. doi: 10.2196/jmir.1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cruz-Correia R, Fonseca J, Lima L, Araujo L, Delgado L, Castel-Branco MG, et al. Web-based or paper-based self-management tools for asthma--patients’ opinions and quality of data in a randomized crossover study. Stud Health Technol Inform. 2007;127:178–89. [PubMed] [Google Scholar]
- 42.Fonseca JA, Costa-Pereira A, Delgado L, Fernandes L, Castel-Branco MG. Asthma patients are willing to use mobile and web technologies to support self-management. Allergy. 2006;61:389–90. doi: 10.1111/j.1398-9995.2006.01016.x. [DOI] [PubMed] [Google Scholar]
- 43.Anhoj J, Moldrup C. Feasibility of collecting diary data from asthma patients through mobile phones and SMS (short message service): response rate analysis and focus group evaluation from a pilot study. J Med Internet Res. 2004;6:e42. doi: 10.2196/jmir.6.4.e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mosnaim GS, Powell LH, Rathkopf M. A Review of Published Studies Using Interactive Internet Tools or Mobile Devices to Improve Asthma Knowledge or Health Outcomes. Pediatric Allergy, Immunology, and Pulmonology. 2012;25:55–63. [Google Scholar]
- 45.Schatz M, Sorkness CA, Li JT, Marcus P, Murray JJ, Nathan RA, et al. Asthma Control Test: reliability, validity, and responsiveness in patients not previously followed by asthma specialists. J Allergy Clin Immunol. 2006;117:549–56. doi: 10.1016/j.jaci.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 46.Macy ML, Davis MM, Clark SJ, Stanley RM. Parental health literacy and asthma education delivery during a visit to a community-based pediatric emergency department: a pilot study. Pediatr Emerg Care. 2011;27:469–74. doi: 10.1097/PEC.0b013e31821c98a8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Baddeley A. Working memory, thought, and action. Oxford University Press; 2007. [Google Scholar]
- 48.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. [Accessed 09/30/2011];The Newest Vital Sign: A New Health Literacy Assessment Tool for Health Care Providers. 2011 at http://www.pfizerhealthliteracy.com/physicians-providers/NewestVitalSign.aspx.
- 50.Weiss BD, Mays MZ, Martz W, Castro KM, DeWalt DA, Pignone MP, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005;3:514–22. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shah LC, West P, Bremmeyr K, Savoy-Moore RT. Health literacy instrument in family medicine: the “newest vital sign” ease of use and correlates. J Am Board Fam Med. 2010;23:195–203. doi: 10.3122/jabfm.2010.02.070278. [DOI] [PubMed] [Google Scholar]
- 52.Driessnack M, Chung S, Perkhounkova E, Hein M. Using the “Newest Vital Sign” to assess health literacy in children. J Pediatr Health Care. 2014;28:165–71. doi: 10.1016/j.pedhc.2013.05.005. [DOI] [PubMed] [Google Scholar]
- 53.Warsh J, Chari R, Badaczewski A, Hossain J, Sharif I. Can the Newest Vital Sign be used to assess health literacy in children and adolescents? Clin Pediatr (Phila) 2014;53:141–4. doi: 10.1177/0009922813504025. [DOI] [PubMed] [Google Scholar]
- 54.Morrison AK, Schapira MM, Hoffmann RG, Brousseau DC. Measuring health literacy in caregivers of children: a comparison of the newest vital sign and S-TOFHLA. Clin Pediatr (Phila) 2014;53:1264–70. doi: 10.1177/0009922814541674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chisolm DJ, Buchanan L. Measuring adolescent functional health literacy: a pilot validation of the Test of Functional Health Literacy in Adults. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2007;41:312–4. doi: 10.1016/j.jadohealth.2007.04.015. [DOI] [PubMed] [Google Scholar]
- 56.MyNemours. [Accessed 11/15/2014]; at ( http://www.nemours.org/patientfamily/mynemours.html.
- 57.Administration FaD, editor. Code of Federal Regulations Title 21 Part 11 Electronic Records; Electronic Signatures. Bethesda: 1997. [Google Scholar]
- 58.Audacity. [Accessed 3/15/2012]; at http://audacity.sourceforge.net.)
- 59.Zelen M. Randomized consent designs for clinical trials: an update. Statistics in medicine. 1990;9:645–56. doi: 10.1002/sim.4780090611. [DOI] [PubMed] [Google Scholar]
- 60.Homer CS. Using the Zelen design in randomized controlled trials: debates and controversies. Journal of advanced nursing. 2002;38:200–7. doi: 10.1046/j.1365-2648.2002.02164.x. [DOI] [PubMed] [Google Scholar]
- 61.Liu AH, Zeiger R, Sorkness C, Mahr T, Ostrom N, Burgess S, et al. Development and cross-sectional validation of the Childhood Asthma Control Test. J Allergy Clin Immunol. 2007;119:817–25. doi: 10.1016/j.jaci.2006.12.662. [DOI] [PubMed] [Google Scholar]
- 62.Suissa S, Ernst P, Boivin JF, Horwitz RI, Habbick B, Cockroft D, et al. A cohort analysis of excess mortality in asthma and the use of inhaled beta-agonists. AmJ RespirCrit Care Med. 1994;149:604–10. doi: 10.1164/ajrccm.149.3.8118625. [DOI] [PubMed] [Google Scholar]
- 63.Kallenbach JM, Frankel AH, Lapinsky SE, Thornton AS, Blott JA, Smith C, et al. Determinants of near fatality in acute severe asthma. Am J Med. 1993;95:265–72. doi: 10.1016/0002-9343(93)90278-w. [DOI] [PubMed] [Google Scholar]
- 64.Greenberger PA, Miller TP, Lifschultz B. Circumstances surrounding deaths from asthma in Cook County (Chicago) Illinois. Allergy Proc. 1993;14:321–6. doi: 10.2500/108854193778773994. [DOI] [PubMed] [Google Scholar]
- 65.Mortimer KM, Fallot A, Balmes JR, Tager IB. Evaluating the use of a portable spirometer in a study of pediatric asthma. Chest. 2003;123:1899–907. doi: 10.1378/chest.123.6.1899. [DOI] [PubMed] [Google Scholar]
- 66.Thompson R, Delfino RJ, Tjoa T, Nussbaum E, Cooper D. Evaluation of daily home spirometry for school children with asthma: new insights. Pediatr Pulmonol. 2006;41:819–28. doi: 10.1002/ppul.20449. [DOI] [PubMed] [Google Scholar]
- 67.CT Payer. [Accessed 11/15/2014]; at www.ctpayer.com.)
- 68.Schatz M, Kosinski M, Yarlas AS, Hanlon J, Watson ME, Jhingran P. The minimally important difference of the Asthma Control Test. J Allergy Clin Immunol. 2009;124:719–23. doi: 10.1016/j.jaci.2009.06.053. e1. [DOI] [PubMed] [Google Scholar]
- 69.Arenz D, Hero B, Eichhorst BF, Langer M, Pester L, von Tresckow J, et al. Estimating site costs prior to conducting clinical trials. Clinical Investigation. 2014;4:227–34. [Google Scholar]
- 70.Emanuel EJ, Schnipper LE, Kamin DY, Levinson J, Lichter AS. The costs of conducting clinical research. J Clin Oncol. 2003;21:4145–50. doi: 10.1200/JCO.2003.08.156. [DOI] [PubMed] [Google Scholar]
- 71.Eisenstein EL, Collins R, Cracknell BS, Podesta O, Reid ED, Sandercock P, et al. Sensible approaches for reducing clinical trial costs. Clin Trials. 2008;5:75–84. doi: 10.1177/1740774507087551. [DOI] [PubMed] [Google Scholar]
- 72. [Accessed January 15, 2015];Research Electronic Data Capture. at http://project-redcap.org.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Section 1, “About this Study” of the informed consent video that is viewed by potential participants in the streamlined trial prior to the informed consent discussion with the study staff. There are 5 sections to the video, “About this Study”, “Participating in the Study”, “Possible Benefits and Risks”, “Payment for Participating”, and “Protecting your Privacy”. The website programming requires participants to view the video sections in sequence. At the end of each section are 2 to 3 multiple-choice questions to reinforce learning. The entire video is about 15 minutes in length. In addition, the consent video website contains supplementary information related to the video content in the sidebar.