Context
Anterior cruciate ligament (ACL) injury is a major concern in physically active females. Although ACL reconstruction techniques have seen significant advances in recent years, risk associated with re-injury and future osteoarthritis remains a major concern. Thus, prevention of ACL injury is a logical step to protect and preserve healthy knee joints in young athletes. The current report aims to summarize a list of evidence-based prevention strategies to reduce ACL injury in female athletes. A list of six critical principles, which come from documented, large scale clinical trial studies and further analyses, were presented with ABC format including age, biomechanics, compliance, dosage, exercise, and feedback. Also, a grade for evidence and implications of future research is noted. Finally, in the conclusion section, importance of collaborative efforts from healthcare practitioners, researchers, and personnel associated with athletics is addressed.
Key terms: Prevention, Evidence-based, ACL, Strategies, Female athletes
INTRODUCTION
Anterior cruciate ligament (ACL) ruptures are a major concern in the fields of Orthopaedics and Sports Medicine, particularly in young female athletes. ACL injury occurrence in young female athletes is two to four times higher in cutting, jumping, and pivoting sports compared with males.1–3 Because the ACL plays an integral role in knee joint mechanics, an individual with an ACL rupture often experiences functional difficulties, including inabilities to decelerate, cut, and pivot, in addition to the presence of pain and effusion in the knee joint.4 At present, a reconstructive surgery is used to replace the torn ACL. Approximately 350,000 individuals seek ACL reconstruction (ACLR) surgery in the United States annually.5 The cost associated with ACL rupture and reconstruction is estimated to be about $2 billion per year.6 Although ACLR is commonly performed to restore knee function, there are several limitations to this approach for the young athlete. The time devoted to post-ACL rehabilitation is approximately six to nine months4,7 or longer, which results in the greatest time lost from athletic participation compared to ankle and traumatic head injuries.8 Approximately 30–35% of physically active middle and high school athletes choose not to return to their original sports after their initial ACL rupture.9 In addition, about 24% of high school athletes who had ACLR surgeries sustain secondary ACL rupture within one year after return to their sports.10 Furthermore, 42% of female soccer players who had ACLR demonstrated radiographically observable knee osteoarthritis (OA) signs within 10 years, and 75% of them commented that the OA symptoms negatively affected their quality of life.11 Another study reported 71% of individuals who had an ACLR surgery developed a moderate level of knee OA within 10 to 15 years.12
Because of the unfavorable knee joint health issues associated with ACL rupture, prevention of ACL injury should be a priority. A key to the development of effective prevention strategies is to identify modifiable risk factors.13,14 While some studies report an association between ACL injury and anatomical,15,16 hormonal,17 and genetic18–20 components, they are not modifiable in current medical practices. Conversely, biomechanical and neuromuscular factors are modifiable by neuromuscular training (NMT).21–24 Control of the magnitude of external loading at the knee joint by improvement of muscular support25 and alteration of athletic techniques26 through NMT appears to be an effective intervention to reduce injury risk.27 Historically, since the 1990s, 14 large scale clinical trials have been published to test the efficacy of NMT on ACL injury reduction in female athletes.28–41 From the documented evidence based on the original studies and further analyses, this report aims to generate a list of evidence-based prevention strategies to reduce ACL injury in female athletes and to identify suggestions for future research implications to optimize implementation of NMT.
Age: Start early
Evidence shows that younger athletes have better outcomes from NMT than older athletes. In a recent study, fewer ACL injuries were documented in younger athletes who performed NMT compared to older athletes who also performed NMT.27 Compared to female athletes over age 20 years as a reference, 14–18 years old and 19–20 years old female athletes demonstrated a reduced risk of sustaining ACL injuries by 72% and 52%, respectively from NMT.27 Among the 14 reviewed studies, two studies used identical NMT programs for female soccer players.32,38 The only difference between these two studies appeared to be the age of the soccer players. A comparison of the results of these two studies shows that the 14–18 years old female soccer players demonstrated an 81% reduction (88% in 1st year and 74% in 2nd year) in ACL injury incidence;32 while the ACL injury reduction in collegiate female soccer players (mean age of 19.9 years old) was 70%.38 It is theorized that sensorimotor function is more adaptable when individuals are in the developmental stage.42,43 Thus, it is likely better to start NMT when athletes are in their early teens.44–46
Biomechanics: Change the risk movements
A prospective study that investigated modifiable risk factors in female high school soccer and basketball players reported that those who sustained noncontact ACL injury had increased knee abduction moments, limited knee flexion angles, greater ground reaction force (GRF), and asymmetrical landing pattern compared to female athletes who did not experience ACL injury.47 Among the four risk factors, increased knee abduction was the strongest indicator of increased ACL injury risk, with 73% and 78% specificity and sensitivity respectively.47 In addition, a retrospective video study that analyzed injured female athletes with ACL injury reported that those who suffered an ACL tear demonstrated increased lateral trunk flexion angles as well as knee abduction angles.48 Another prospective study also identified deficits in trunk control as a risk factor for future ACL injury in female collegiate athletes.49 The combination of this evidence indicates that decreased knee flexion and asymmetrical landing patterns do not sufficiently attenuate landing force, which results in greater GRF. The elevated GRF vectors lateral to the femoral head have been attributed to lateral trunk flexion. In order to counterbalance the force and lateral trunk flexion, hip adductor muscles need to be activated, consequently increasing hip adduction. As a result of this sequence of biomechanical events, the knee joint is placed in an abducted “valgus” position.50 Thus, it is critical to recognize that knee abduction or valgus movement is a predictor of future ACL injury.47 Additionally, the involvement of the posterior kinetic chain in this force production is important, which will be discussed in sections “E” and “F.”
Compliance: If you don’t do it, it does not work
Compliance or adherence to the NMT is critical to the success of any ACL prevention intervention and is associated with the incidence of ACL injury occurrence. Coaches and athletes who complied with prescribed NMT programs were included in the overall compliance rate and extracted from six studies.28–31,37,39 When the overall compliance rate was greater than 66%, an ACL injury reduction rate of 82% was recorded.51 However, when the overall compliance rate dropped to less than 66% or 33%, the rates of ACL injury reduction were found to be 44% and 12%, respectively.51 Several studies31,37 documented low compliance rate as a major limitation and noted that an absence of available NMT time was due to constant competitions, infrequent practice days, and occasional academic and holiday breaks possibly hindering the execution of the NMT intervention. To investigate potential barriers to NMT implementation, a set of questionnaires was delivered to high school soccer coaches through a web-based survey and phone follow-up.52 The results indicated that soccer coaches who implemented NMT regularly had more experience (greater than seven years of experience as a coach), and were further aided by the presence of healthcare practitioners including athletic trainers and strength and conditioning personnel. Therefore, having healthcare practitioners is a critical step for implementation of NMT, and athletes need to perform NMT regularly in order to attain the prophylactic effects and reduce ACL injury.
Dosage: The more you do it, the less ACL injury
The duration and frequency of NMT sessions were found to be directly associated with ACL injury reduction.53 In 14 reviewed studies, NMT duration and frequency were carefully examined and analyzed. Based on the extracted information, the volume of NMT (minutes spent per week during in-season), a combination of duration and frequency of NMT session, was developed and categorized into three different classifications: low (up to 15 minutes per week), moderate (15–30 minutes per week), and high (more than 30 minutes per week). This analysis demonstrated an inverse dose-response association between NMT volume and ACL injury: The more time the athletes spent performing NMT, the fewer ACL injuries they sustained.53 This study indicated that a prescription of at least 20 minutes per NMT session, several times per week in-season as well as in pre-season was necessary in order to attain full prophylactic effectiveness.53 Another study investigated the association between NMT program duration and movement retention ability and also reported a dosage effect: The longer athletes performed NMT, the longer athletes retained the prophylactically favorable movements.54 Hence, in order to minimize ACL injury risk, it is recommended that NMT sessions are performed longer, more frequently, and over a greater time period.
Exercise: Include a variety of exercises
NMT that consists of multiple types of exercises demonstrates greater reduction in incidence of ACL injury, compared to NMT with only a single exercise modality (e.g. plyometrics, resistance training, balance training).55 The number of ACL injuries was not reduced in two studies,29,35 in which only one type of exercise was incorporated. Conversely, NMT with multiple exercise modes demonstrated ACL injury risk reduction ranging 29%–79% relative to the control group.55 The main question remaining is “What type of NMT is most effective for prophylaxis of ACL injuries?” NMT can be mainly classified into four different modes: balance, plyometrics, strengthening, and proximal control training. One strengthening exercise commonly incorporated in NMT is the “Russian/Nordic hamstrings curl.” Using this technique, enhancement of hamstrings peak torque and to increase in knee flexion in dynamic movements were documented in these studies.21,22,56 Since decreased knee flexion is one of the risk factors for ACL injury, flexing the knee in dynamic movements may help to reduce the GRF. In terms of GRF reduction, three studies reported 17–26% of GRF reduction with landing after six to nine weeks of plyometric training.21,57,58 In addition to the GRF reduction, athletes tend to exhibit less knee abduction or lower extremity “valgus” when they perform plyometric exercises.
Proximal control training has also received attention for risk reduction.55 Proximal control training refers to exercises that focus on enhancing stability of segments proximal to the knee joint through strengthening and learning adequate control in dynamic movements. Recent studies have added exercises for the hip, lower trunk, and upper body such as the plank37,41 and side plank37,41 as well as sit-ups/abdominal curl,28,39 push-ups,40 and upper body weight training including bench press, pullover, pull-down and hyperextension.28 Since deficits in trunk control, especially lateral trunk flexion, has been identified as a risk factor for future ACL injury,48,49 it is logical that those exercises may contribute to enhance trunk stabilization. A study that focused on examining the effect of proximal control training reported a reduction in knee abduction angle during single leg squat.22 Lastly, balance and dynamic stabilization exercises can be useful to enhance awareness of body control. This is particularly important because deficits in trunk control were found to be a risk factor for ACL injury.49 In addition, numerous studies have demonstrated favorable kinematic and kinetic changes to the knee joint from balance exercises.23,24,59 In summary, performing only one of the exercise modes alone is probably ineffective in ACL injury prevention or may confer insufficient protection. In order to attain maximal prophylactic effects, a successful NMT program should incorporate a variety of exercises within NMT.55
Feedback: Your voice is powerful
The majority of the reviewed NMT studies incorporated a “feedback” system, which appears to be beneficial. A few studies supplied an instructional video DVD and written materials to highlight risk movements and emphasize appropriate movement patterns prior to the start of the study.37,38,40 For instance, studies instructed coaches and athletes to check knee alignment during the NMT and encouraged correction of improper knee alignment by using simple verbal cues including “knee over the toe,” and “don’t let knees cave inward.”28,33,34,40 A few studies reported biomechanically favorable alterations with verbal feedback. For example, knee flexion angle increases were reported using verbal and video feedback in female volleyball players.60 Furthermore, a group of female athletes who received NMT with verbal feedback decreased knee abduction angles significantly when compared to a group that performed NMT alone.61 Finally, video instruction given to alpine skiing instructors and patrollers resulted in a 62% reduction in ACL injury while no ACL injury reduction was observed in the control group that did not receive video instruction.62 Therefore, it is highly recommended to use a feedback system incorporating verbal cues while athletes are performing NMT.
Grade of the Evidence: Practice evidence-based medicine
Following analysis of the quality of the evidence from the reviewed studies, seven of the investigations that evaluated NMT and ACL injury risk reduction30,33,36–38,40,41 were rated as level I (high quality individual randomized control trial), while seven studies28,29,31,32,34,35,39 were rated as level II (lower quality clinical trial and cohort study). Although the number of level I and II studies are equivalent, recent meta-analysis supports consistency of evidence with 11 of the 14 reviewed studies demonstrated fewer ACL injuries in NMT intervention groups compared to control groups.27,53,55 A summary effect of the meta-analysis indicated that noncontact and overall ACL injury risk can be reduced by 73% and 44% respectively.63 No publication bias was detected (Egger’s regression, p=0.41) in these analyses.27,53,55 The level of evidence can be evaluated from A (consistent and good quality patient-oriented evidence), B (inconsistent evidence or limited quality patient oriented evidence), C (consensus, usual practice, opinion, disease-oriented evidence) scale based on Strength of Recommendation Taxonomy (SORT).64 Based on the consistency of the results from the included clinical trials, the SORT grade for the current evidence is “A” (recommendation based on consistent and good quality patient-oriented evidence).27,53,55
Sports and sex: More evidence is needed for sport and male specific prevention strategies
When the documented evidence is broken down based on sport, 10 of the 14 studies implemented NMT for soccer players,28–30,32,35,37–41 and few studies included handball,31,33,34 basketball,28,35,40 volleyball,28 and floorball athletes.36 Since epidemiological studies have demonstrated higher ACL injury risk in basketball when compared to soccer,1 more studies are necessary to determine effectiveness of NMT on ACL injury in basketball athletes as well as handball athletes. Variability of ACL injury reduction was found based on different sports (Figure 1). Wide 95% confidence intervals observed in basketball and floorball indicate the need for more evidence. Moreover, male athletes were traditionally used as a comparison group for female athletes, especially in biomechanical studies.48,65–68 Investigation of risk factors specific to males is warranted. Recent review studies concluded that existing evidence is related to environmental and anatomical risk factors69 and advocated the need to identify modifiable risk factors in the male population.70 The upshot is, more studies are essential to determine sport and sex-specific responses to NMT and ACL injury reduction. However, in the meantime, sport and sex-specific NMT programs can be empirically modeled after presently available programs for women.
Figure 1.
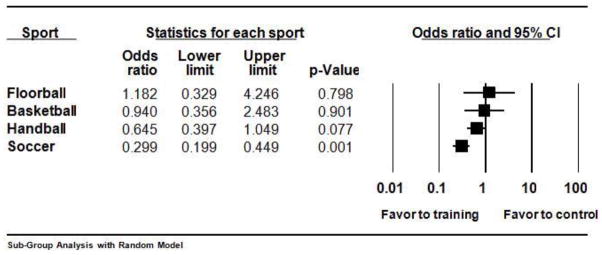
Subgroup analysis by sport with random model from 14 reviewed studies
Conclusion
Although numerous studies have been conducted and published on ACL injuries, an upward trend in incidence of ACL injury is still being reported.71 One study reported that athletes who experienced prior knee surgery including ACL-R before collegiate athletic participation were 7–20 times more likely to sustain another knee injury during their collegiate careers.72 In current medicine and science, it is difficult to treat or reverse progression of knee OA, which is a common long-term sequella of ACL injury.11,12 Therefore, it is necessary to continue to pursue preventive interventions. Many studies have now reported prophylactic effectiveness of NMT for ACL injury in female athletes. The goal of this report is to present available evidence and future research implications with a simple ABC list format. In this way, healthcare practitioners can use these recommendations in their clinical practices as ACL injury prevention strategies and help to reduce ACL injury incidence in physically active females. Evidence-based medicine should be practiced instead of only considered as “just a concept.” It is time to translate this documented evidence of ACL prevention into actual practice. With collaborative efforts from healthcare practitioners, researchers, and others associated with athletic activities, preventive medicine can move forward.
Acknowledgments
The authors would like to acknowledge funding support from National Institutes of Health/NIAMS grants R01-AR049735, R01-AR05563, and R01- AR056259. The authors acknowledge members and supporting personnel of the Micheli Center for Sports Injury Prevention, the Human Performance Laboratory of the Cincinnati Children’s Hospital Sports Medicine, and Sports Health & Performance Institute and Sports Medicine Biodynamics Laboratories of the Ohio State University. All authors are independent of any commercial funder, had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analyses.
Footnotes
Conflict of Interest
D Sugimoto, GD Myer, LJ Micheli, and TE Hewett all declare no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Papers of particular interest, published recently, have been highlighted as:
•• Of major importance
• Of importance
- 1.Arendt EA, Agel J, Dick R. Anterior cruciate ligament injury patterns among collegiate men and women. J Athl Train. 1999 Apr;34(2):86–92. [PMC free article] [PubMed] [Google Scholar]
- 2.Walden M, Hagglund M, Werner J, Ekstrand J. The epidemiology of anterior cruciate ligament injury in football (soccer): a review of the literature from a gender-related perspective. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2011 Jan;19(1):3–10. doi: 10.1007/s00167-010-1172-7. [DOI] [PubMed] [Google Scholar]
- 3.Walden M, Hagglund M, Werner J, Ekstrand J. The epidemiology of anterior cruciate ligament injury in football (soccer): a review of the literature from a gender-related perspective. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2010 Jun 9; doi: 10.1007/s00167-010-1172-7. [DOI] [PubMed] [Google Scholar]
- 4.Cimino F, Volk BS, Setter D. Anterior cruciate ligament injury: diagnosis, management, and prevention. American family physician. 2010 Oct 15;82(8):917–922. [PubMed] [Google Scholar]
- 5.Wojtys EM, Brower AM. Anterior cruciate ligament injuries in the prepubescent and adolescent athlete: clinical and research considerations. J Athl Train. 2010 Sep-Oct;45(5):509–512. doi: 10.4085/1062-6050-45.5.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Silvers HJ, Mandelbaum BR. Prevention of anterior cruciate ligament injury in the female athlete. British journal of sports medicine. 2007 Aug;41( Suppl 1):i52–59. doi: 10.1136/bjsm.2007.037200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dugan SA. Sports-related knee injuries in female athletes: what gives? Am J Phys Med Rehabil. 2005 Feb;84(2):122–130. doi: 10.1097/01.phm.0000154183.40640.93. [DOI] [PubMed] [Google Scholar]
- 8.Hootman JM, Albohm MJ. Anterior cruciate ligament injury prevention and primary prevention of knee osteoarthritis. J Athl Train. 2012;47(5):589–590. doi: 10.4085/1062-6050-47.5.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McCullough KA, Phelps KD, Spindler KP, et al. Return to high school- and college-level football after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) cohort study. The American journal of sports medicine. 2012 Nov;40(11):2523–2529. doi: 10.1177/0363546512456836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. The American journal of sports medicine. 2010 Oct;38(10):1968–1978. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lohmander LS, Ostenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004 Oct;50(10):3145–3152. doi: 10.1002/art.20589. [DOI] [PubMed] [Google Scholar]
- 12.Oiestad BE, Holm I, Engebretsen L, Risberg MA. The association between radiographic knee osteoarthritis and knee symptoms, function and quality of life 10–15 years after anterior cruciate ligament reconstruction. British journal of sports medicine. 2011 Jun;45(7):583–588. doi: 10.1136/bjsm.2010.073130. [DOI] [PubMed] [Google Scholar]
- 13.Hewett TE, Myer GD, Ford KR, Slauterbeck JR. Dynamic neuromuscular analysis training for preventing anterior cruciate ligament injury in female athletes. Instr Course Lect. 2007;56:397–406. [PubMed] [Google Scholar]
- 14.Hewett TE, SS, Griffin LY. In: Understanding and preventing noncontact ACL injuries. 1. Kinetics H, editor. 2007. [Google Scholar]
- 15.Beynnon BD, Hall JS, Sturnick DR, et al. Increased Slope of the Lateral Tibial Plateau Subchondral Bone Is Associated With Greater Risk of Noncontact ACL Injury in Females but Not in Males: A Prospective Cohort Study With a Nested, Matched Case-Control Analysis. The American journal of sports medicine. 2014 Mar 3; doi: 10.1177/0363546514523721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Webb JM, Salmon LJ, Leclerc E, Pinczewski LA, Roe JP. Posterior tibial slope and further anterior cruciate ligament injuries in the anterior cruciate ligament-reconstructed patient. The American journal of sports medicine. 2013 Dec;41(12):2800–2804. doi: 10.1177/0363546513503288. [DOI] [PubMed] [Google Scholar]
- 17.Bell DR, Blackburn JT, Norcorss MF, et al. Estrogen and muscle stiffness have a negative relationship in females. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2012 Feb;20(2):361–367. doi: 10.1007/s00167-011-1577-y. [DOI] [PubMed] [Google Scholar]
- 18.Lo IK, Marchuk LL, Hart DA, Frank CB. Comparison of mRNA levels for matrix molecules in normal and disrupted human anterior cruciate ligaments using reverse transcription-polymerase chain reaction. Journal of orthopaedic research : official publication of the Orthopaedic Research Society. 1998 Jul;16(4):421–428. doi: 10.1002/jor.1100160405. [DOI] [PubMed] [Google Scholar]
- 19.Nakase J, Tsuchiya H, Kitaoka K. Contralateral anterior cruciate ligament injury after anterior cruciate ligament reconstruction: a case controlled study. Sports medicine, arthroscopy, rehabilitation, therapy & technology : SMARTT. 2012;4(1):46. doi: 10.1186/1758-2555-4-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Posthumus M, September AV, Keegan M, et al. Genetic risk factors for anterior cruciate ligament ruptures: COL1A1 gene variant. British journal of sports medicine. 2009 May;43(5):352–356. doi: 10.1136/bjsm.2008.056150. [DOI] [PubMed] [Google Scholar]
- 21.Hewett TE, Stroupe AL, Nance TA, Noyes FR. Plyometric training in female athletes. Decreased impact forces and increased hamstring torques. The American journal of sports medicine. 1996 Nov-Dec;24(6):765–773. doi: 10.1177/036354659602400611. [DOI] [PubMed] [Google Scholar]
- 22.de Marche Baldon R, Lobato DF, Carvalho LP, Lam Wun PY, Santiago PR, Serrao FV. Effect of Functional Stabilization Training on Lower Limb Biomechanics in Women. Med Sci Sports Exerc. 2011 Jun 22; doi: 10.1249/MSS.0b013e31822a51bb. [DOI] [PubMed] [Google Scholar]
- 23.Myer GD, Ford KR, Palumbo JP, Hewett TE. Neuromuscular training improves performance and lower-extremity biomechanics in female athletes. Journal of strength and conditioning research/National Strength & Conditioning Association. 2005 Feb;19(1):51–60. doi: 10.1519/13643.1. [DOI] [PubMed] [Google Scholar]
- 24.Myer GD, Ford KR, Brent JL, Hewett TE. The effects of plyometric vs. dynamic stabilization and balance training on power, balance, and landing force in female athletes. Journal of strength and conditioning research/National Strength & Conditioning Association. 2006 May;20(2):345–353. doi: 10.1519/R-17955.1. [DOI] [PubMed] [Google Scholar]
- 25.Markolf KL, Burchfield DM, Shapiro MM, Shepard MF, Finerman GA, Slauterbeck JL. Combined knee loading states that generate high anterior cruciate ligament forces. Journal of orthopaedic research : official publication of the Orthopaedic Research Society. 1995 Nov;13(6):930–935. doi: 10.1002/jor.1100130618. [DOI] [PubMed] [Google Scholar]
- 26.Donnelly CJ, Elliott BC, Ackland TR, et al. An anterior cruciate ligament injury prevention framework: incorporating the recent evidence. Research in sports medicine (Print) 2012 Jul;20(3–4):239–262. doi: 10.1080/15438627.2012.680989. [DOI] [PubMed] [Google Scholar]
- 27**.Myer GD, Sugimoto D, Thomas S, Hewett TE. The Influence of Age on the Effectiveness of Neuromuscular Training to Reduce Anterior Cruciate Ligament Injury in Female Athletes: A Meta-Analysis. The American journal of sports medicine. 2012 Oct 9; doi: 10.1177/0363546512460637. This study displayed age influence on ACL injury reduction, which was a core component of section A: Age: Start early. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hewett TE, Lindenfeld TN, Riccobene JV, Noyes FR. The effect of neuromuscular training on the incidence of knee injury in female athletes. A prospective study. The American journal of sports medicine. 1999 Nov-Dec;27(6):699–706. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- 29.Soderman K, Werner S, Pietila T, Engstrom B, Alfredson H. Balance board training: prevention of traumatic injuries of the lower extremities in female soccer players? A prospective randomized intervention study. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2000;8(6):356–363. doi: 10.1007/s001670000147. [DOI] [PubMed] [Google Scholar]
- 30.Heidt RS, Jr, Sweeterman LM, Carlonas RL, Traub JA, Tekulve FX. Avoidance of soccer injuries with preseason conditioning. The American journal of sports medicine. 2000 Sep-Oct;28(5):659–662. doi: 10.1177/03635465000280050601. [DOI] [PubMed] [Google Scholar]
- 31.Myklebust G, Engebretsen L, Braekken IH, Skjolberg A, Olsen OE, Bahr R. Prevention of anterior cruciate ligament injuries in female team handball players: a prospective intervention study over three seasons. Clin J Sport Med. 2003 Mar;13(2):71–78. doi: 10.1097/00042752-200303000-00002. [DOI] [PubMed] [Google Scholar]
- 32.Mandelbaum BR, Silvers HJ, Watanabe DS, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. The American journal of sports medicine. 2005 Jul;33(7):1003–1010. doi: 10.1177/0363546504272261. [DOI] [PubMed] [Google Scholar]
- 33.Olsen OE, Myklebust G, Engebretsen L, Holme I, Bahr R. Exercises to prevent lower limb injuries in youth sports: cluster randomised controlled trial. BMJ (Clinical research ed) 2005 Feb 26;330(7489):449. doi: 10.1136/bmj.38330.632801.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Petersen W, Braun C, Bock W, et al. A controlled prospective case control study of a prevention training program in female team handball players: the German experience. Arch Orthop Trauma Surg. 2005 Nov;125(9):614–621. doi: 10.1007/s00402-005-0793-7. [DOI] [PubMed] [Google Scholar]
- 35.Pfeiffer RP, Shea KG, Roberts D, Grandstrand S, Bond L. Lack of effect of a knee ligament injury prevention program on the incidence of noncontact anterior cruciate ligament injury. J Bone Joint Surg Am. 2006 Aug;88(8):1769–1774. doi: 10.2106/JBJS.E.00616. [DOI] [PubMed] [Google Scholar]
- 36.Pasanen K, Parkkari J, Pasanen M, Kannus P. Effect of a neuromuscular warm-up programme on muscle power, balance, speed and agility: a randomised controlled study. British journal of sports medicine. 2009 Dec;43(13):1073–1078. doi: 10.1136/bjsm.2009.061747. [DOI] [PubMed] [Google Scholar]
- 37.Steffen K, Myklebust G, Olsen OE, Holme I, Bahr R. Preventing injuries in female youth football--a cluster-randomized controlled trial. Scandinavian journal of medicine & science in sports. 2008 Oct;18(5):605–614. doi: 10.1111/j.1600-0838.2007.00703.x. [DOI] [PubMed] [Google Scholar]
- 38.Gilchrist J, Mandelbaum BR, Melancon H, et al. A randomized controlled trial to prevent noncontact anterior cruciate ligament injury in female collegiate soccer players. The American journal of sports medicine. 2008 Aug;36(8):1476–1483. doi: 10.1177/0363546508318188. [DOI] [PubMed] [Google Scholar]
- 39.Kiani A, Hellquist E, Ahlqvist K, Gedeborg R, Michaelsson K, Byberg L. Prevention of soccer-related knee injuries in teenaged girls. Arch Intern Med. 2010 Jan 11;170(1):43–49. doi: 10.1001/archinternmed.2009.289. [DOI] [PubMed] [Google Scholar]
- 40.LaBella CR, Huxford MR, Grissom J, Kim KY, Peng J, Christoffel KK. Effect of neuromuscular warm-up on injuries in female soccer and basketball athletes in urban public high schools: cluster randomized controlled trial. Arch Pediatr Adolesc Med. 2011 Nov;165(11):1033–1040. doi: 10.1001/archpediatrics.2011.168. [DOI] [PubMed] [Google Scholar]
- 41.Walden M, Atroshi I, Magnusson H, Wagner P, Hagglund M. Prevention of acute knee injuries in adolescent female football players: cluster randomised controlled trial. BMJ (Clinical research ed) 2012;344:e3042. doi: 10.1136/bmj.e3042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Morrison S, Sosnoff JJ. Age-related changes in the adaptability of neuromuscular output. Journal of motor behavior. 2009 May;41(3):274–283. doi: 10.3200/JMBR.41.3.274-288. [DOI] [PubMed] [Google Scholar]
- 43.Sosnoff JJ, Voudrie SJ. Practice and age-related loss of adaptability in sensorimotor performance. Journal of motor behavior. 2009 Mar;41(2):137–146. doi: 10.3200/JMBR.41.2.137-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Myer GD, Faigenbaum AD, Chu DA, et al. Integrative training for children and adolescents: techniques and practices for reducing sports-related injuries and enhancing athletic performance. Phys Sportsmed. 2011 Feb;39(1):74–84. doi: 10.3810/psm.2011.02.1854. [DOI] [PubMed] [Google Scholar]
- 45.Myer GD, Faigenbaum AD, Ford KR, Best TM, Bergeron MF, Hewett TE. When to initiate integrative neuromuscular training to reduce sports-related injuries and enhance health in youth? Current sports medicine reports. 2011 May-Jun;10(3):155–166. doi: 10.1249/JSR.0b013e31821b1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Myer GD, Kushner AM, Faigenbaum AD, Kiefer A, Kashikar-Zuck S, Clark JF. Training the developing brain, part I: cognitive developmental considerations for training youth. Current sports medicine reports. 2013 Sep-Oct;12(5):304–310. doi: 10.1097/01.CSMR.0000434106.12813.69. [DOI] [PubMed] [Google Scholar]
- 47**.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. The American journal of sports medicine. 2005 Apr;33(4):492–501. doi: 10.1177/0363546504269591. This study explained critical components of section B: Biomechanics: Change the risk movements. [DOI] [PubMed] [Google Scholar]
- 48.Hewett TE, Torg JS, Boden BP. Video analysis of trunk and knee motion during non-contact anterior cruciate ligament injury in female athletes: lateral trunk and knee abduction motion are combined components of the injury mechanism. British journal of sports medicine. 2009 Jun;43(6):417–422. doi: 10.1136/bjsm.2009.059162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zazulak BT, Hewett TE, Reeves NP, Goldberg B, Cholewicki J. Deficits in neuromuscular control of the trunk predict knee injury risk: a prospective biomechanical-epidemiologic study. The American journal of sports medicine. 2007 Jul;35(7):1123–1130. doi: 10.1177/0363546507301585. [DOI] [PubMed] [Google Scholar]
- 50.Hewett TE, Myer GD. The Mechanistic Connection between the Trunk, Knee, and ACL Injury. Exerc Sport Sci Rev. 2011 Jul 21; doi: 10.1097/JES.0b013e3182297439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51**.Sugimoto D, Myer GD, Bush HM, Klugman MF, Medina McKeon JM, Hewett TE. Compliance with neuromuscular training and anterior cruciate ligament injury risk reduction in female athletes: a meta-analysis. J Athl Train. 2012;47(6):714–723. doi: 10.4085/1062-6050-47.6.10. This study encompassed importance of adherence and compliance of NMT, which was addressed in section C: Compliance: If you don’t do it, it does not work. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Joy E, Taylor JR, Novak M, Chen M, Fink B, Porucznik C. Factors Influencing the Implementation of ACL Injury Prevention Strategies by Girls Soccer Coaches. Journal of strength and conditioning research/National Strength & Conditioning Association. 2013 Jan 2; doi: 10.1519/JSC.0b013e31827ef12e. [DOI] [PubMed] [Google Scholar]
- 53**.Sugimoto D, Myer GD, Foss KD, Hewett TE. Dosage effects of neuromuscular training intervention to reduce anterior cruciate ligament injuries in female athletes: meta- and sub-group analyses. Sports Med. 2014 Apr;44(4):551–562. doi: 10.1007/s40279-013-0135-9. This study generated evidence of inverse dose-response relationship, which was a crucial point described in section D: Dosage: The more you do it, less ACL injury. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Padua DA, DiStefano LJ, Marshall SW, Beutler AI, de la Motte SJ, DiStefano MJ. Retention of movement pattern changes after a lower extremity injury prevention program is affected by program duration. The American journal of sports medicine. 2012 Feb;40(2):300–306. doi: 10.1177/0363546511425474. [DOI] [PubMed] [Google Scholar]
- 55**.Sugimoto D, Myer GD, Barber Foss KD, Hewett TE. Specific exercise effects of preventive neuromuscular training intervention on anterior cruciate ligament injury risk reduction in young females: meta-analysis and subgroup analysis. British journal of sports medicine. 2014 Dec 1; doi: 10.1136/bjsports-2014-093461. This study demonstrated specific exercise effects of NMT and pointed out importance of exercise variations within NMT, which was synthesized in section E: Exercise: Include a variety of exercises. [DOI] [PubMed] [Google Scholar]
- 56.Lim BO, Lee YS, Kim JG, An KO, Yoo J, Kwon YH. Effects of sports injury prevention training on the biomechanical risk factors of anterior cruciate ligament injury in high school female basketball players. The American journal of sports medicine. 2009 Sep;37(9):1728–1734. doi: 10.1177/0363546509334220. [DOI] [PubMed] [Google Scholar]
- 57.Irmischer BS, Harris C, Pfeiffer RP, DeBeliso MA, Adams KJ, Shea KG. Effects of a knee ligament injury prevention exercise program on impact forces in women. Journal of strength and conditioning research/National Strength & Conditioning Association. 2004 Nov;18(4):703–707. doi: 10.1519/R-13473.1. [DOI] [PubMed] [Google Scholar]
- 58.Vescovi JD, Canavan PK, Hasson S. Effects of a plyometric program on vertical landing force and jumping performance in college women. Physical therapy in sport : official journal of the Association of Chartered Physiotherapists in Sports Medicine. 2008 Nov;9(4):185–192. doi: 10.1016/j.ptsp.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 59.Myer GD, Ford KR, McLean SG, Hewett TE. The effects of plyometric versus dynamic stabilization and balance training on lower extremity biomechanics. The American journal of sports medicine. 2006 Mar;34(3):445–455. doi: 10.1177/0363546505281241. [DOI] [PubMed] [Google Scholar]
- 60.Parsons JL, Alexander MJ. Modifying spike jump landing biomechanics in female adolescent volleyball athletes using video and verbal feedback. Journal of strength and conditioning research/National Strength & Conditioning Association. 2012 Apr;26(4):1076–1084. doi: 10.1519/JSC.0b013e31822e5876. [DOI] [PubMed] [Google Scholar]
- 61**.Myer GD, Stroube BW, DiCesare CA, et al. Augmented feedback supports skill transfer and reduces high-risk injury landing mechanics: a double-blind, randomized controlled laboratory study. The American journal of sports medicine. 2013 Mar;41(3):669–677. doi: 10.1177/0363546512472977. This study was the highest evidence to support importance of biofeedback system, which was discussed in section F: Feedback: Your voice is powerful. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ettlinger CF, Johnson RJ, Shealy JE. A method to help reduce the risk of serious knee sprains incurred in alpine skiing. The American journal of sports medicine. 1995 Sep-Oct;23(5):531–537. doi: 10.1177/036354659502300503. [DOI] [PubMed] [Google Scholar]
- 63**.Sugimoto D, Myer GD, McKeon JM, Hewett TE. Evaluation of the effectiveness of neuromuscular training to reduce anterior cruciate ligament injury in female athletes: a critical review of relative risk reduction and numbers-needed-to-treat analyses. British journal of sports medicine. 2012 Nov;46(14):979–988. doi: 10.1136/bjsports-2011-090895. This study focused on identifying specific percent (%) of risk reduction of ACL injury performing NMT intervention, which emphasized section G: Grade of the Evidence: Practice evidence-based medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ebell MH, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. The Journal of the American Board of Family Practice/American Board of Family Practice. 2004 Jan-Feb;17(1):59–67. doi: 10.3122/jabfm.17.1.59. [DOI] [PubMed] [Google Scholar]
- 65.Chappell JD, Creighton RA, Giuliani C, Yu B, Garrett WE. Kinematics and electromyography of landing preparation in vertical stop-jump: risks for noncontact anterior cruciate ligament injury. The American journal of sports medicine. 2007 Feb;35(2):235–241. doi: 10.1177/0363546506294077. [DOI] [PubMed] [Google Scholar]
- 66.Ford KR, Myer GD, Smith RL, Vianello RM, Seiwert SL, Hewett TE. A comparison of dynamic coronal plane excursion between matched male and female athletes when performing single leg landings. Clin Biomech (Bristol, Avon) 2006 Jan;21(1):33–40. doi: 10.1016/j.clinbiomech.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 67.Ford KR, Myer GD, Hewett TE. Valgus knee motion during landing in high school female and male basketball players. Med Sci Sports Exerc. 2003 Oct;35(10):1745–1750. doi: 10.1249/01.MSS.0000089346.85744.D9. [DOI] [PubMed] [Google Scholar]
- 68.Jacobs CA, Uhl TL, Mattacola CG, Shapiro R, Rayens WS. Hip abductor function and lower extremity landing kinematics: sex differences. J Athl Train. 2007 Jan-Mar;42(1):76–83. [PMC free article] [PubMed] [Google Scholar]
- 69.Alentorn-Geli E, Mendiguchia J, Samuelsson K, et al. Prevention of anterior cruciate ligament injuries in sports. Part I: systematic review of risk factors in male athletes. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2014 Jan;22(1):3–15. doi: 10.1007/s00167-013-2725-3. [DOI] [PubMed] [Google Scholar]
- 70.Alentorn-Geli E, Mendiguchia J, Samuelsson K, et al. Prevention of non-contact anterior cruciate ligament injuries in sports. Part II: systematic review of the effectiveness of prevention programmes in male athletes. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2014 Jan;22(1):16–25. doi: 10.1007/s00167-013-2739-x. [DOI] [PubMed] [Google Scholar]
- 71.Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007 Apr-Jun;42(2):311–319. [PMC free article] [PubMed] [Google Scholar]
- 72.Rugg CM, Wang D, Sulzicki P, Hame SL. Effects of Prior Knee Surgery on Subsequent Injury, Imaging, and Surgery in NCAA Collegiate Athletes. The American journal of sports medicine. 2014 Feb 11; doi: 10.1177/0363546513519951. [DOI] [PubMed] [Google Scholar]


