Abstract
Evidence on best practice for optimizing communication with prelingual deaf and hard-of-hearing (DHH) children is lacking. This study examined the effect of a family-focused psychosocial video intervention program on parent–child communication in the context of childhood hearing loss. Fourteen hearing parents with a prelingual DHH child (Mage = 2 years 8 months) completed three sessions of video interaction guidance intervention. Families were assessed in spontaneous free play interactions at pre and postintervention using the Emotional Availability (EA) Scales. The Rosenberg Self-esteem Scale was also used to assess parental report of self-esteem. Compared with nontreatment baselines, increases were shown in the EA subscales: parental sensitivity, parental structuring, parental nonhostility, child responsiveness, and child involvement, and in reported self-esteem at postintervention. Video-feedback enhances communication in families with prelingual DHH children and encourages more connected parent–child interaction. The results raise implications regarding the focus of early intervention strategies for prelingual DHH children.
During the first weeks of life, parents develop intricate patterns of communication that encourage connectedness with their baby. The quality of early social experiences forms an important context for child development (Bornstein, 2002). Mothers who respond to their child with attuned affect encourage mutual engagement and offer a foundation whereby the infant begins to understand the protocols of conversation (Trevarthen, 1998). In these early interactions, the synchronicity of parental responses augment the neuroendocrine pathways affiliated with infant’s longer term emotional processing and expression (Feldman, 2012; Fleming, O’Day, & Kraemer, 1999), and shape infant hormone regulation (Feldman, Gordon, & Zagoory-Sharon, 2010). However, when an infant is born with a significant hearing loss, the nature of social exchanges between hearing parents and their deaf or hard-of-hearing (D/HH) infant is altered and hearing parents must learn to adaptively communicate with a child who cannot readily access the communicative information that parents instinctively convey with highly affective infant-directed speech (Papousek, 1992). Thus, childhood hearing loss is commonly associated with more problematic parent–child interaction (Meadow-Orlans, 1997).
Although a growing number of outcome studies show that access to early interventions and maternal sensitivity enhance language outcomes in contemporary DHH populations (Ching & Dillon, 2013; Quittner et al., 2013), a gap remains in understanding the quality of parent–child interactions in this population. Furthermore, there is a surprising lack of research into the type of interventions that facilitate the quality of interaction in the growing population of young infants identified with hearing loss. This study examines the effect of a video-feedback intervention in augmenting parent–DHH child interactions in the prelingual period, when parental scaffolding of interactions is vital.
While DHH children are likely to benefit from more synchronous interactions, much research with older cohorts has shown that hearing mothers had a tendency to supplement their child’s play with more structuring and dominate interactions with DHH children compared with hearing children (Henggeler, Watson, & Cooper, 1984; Pipp-Siegel, Blair, Deas, Pressman, & Yoshinaga-Itano, 1998; Wedell-Monnig & Lumley, 1980). In addition, compared to the interactive behaviors of hearing mothers and infants, mothers with DHH infants aged 9, 12, and 18 months were less sensitive, less responsive, and showed less affect matching (MacTurk, Meadow-Orlans, Koester, & Spencer, 1993; Meadow-Orlans, 1997).
More recent evidence also indicates a challenging nature in interactions with DHH children as they communicate less (Barker et al., 2009) and perform worse on measures of social competence than their hearing counterparts (Hoffman, Quittner, Cejas, 2014). Language delays are also evident in populations with early access to hearing prostheses (Moeller et al., 2007). Findings from a case study of twins (one DHH and one hearing infant) also highlight difficulties in the interactive synchrony between hearing mothers and DHH toddlers (Lam & Kitamura, 2010). In this study, scores on the Emotional Availability (EA) Scales (Biringen, 2008) showed that the mother provided more directives and supplementary structuring during play with her DHH son, which was not evident in her behavior towards his hearing twin. Moreover, the DHH son was less responsive and involving of his mother than his hearing twin. Such differences in child behavior have also been shown in the signaling behaviors of DHH compared with hearing infants, with more communication breakdowns (Lederberg & Mobley, 1990) and less smiling, reaching or greeting with DHH infants (Koester, 1995). Importantly, although both DHH and hearing infants show increases in communicative bids from 22 to 36 months of age, hearing children communicated twice as much as DHH infants (Lederberg & Everhart, 1998). Thus it is not surprising that the quality of mother’s speech input diminishes when communicating with DHH compared to hearing infants (Lam & Kitamura, 2010, 2012).
Though a wealth of evidence reveals differences in the way DHH and hearing infants interact with their mothers, equivocal results have been shown regarding the level of maternal sensitivity in short play sessions in a group of families with early-identified DHH children receiving the Colorado Home Intervention Research Project (Pipp-Siegel et al., 1998). Early enrolment in this intervention also predicts more positive language outcomes (Yoshinaga-Itano, 2003). However, these studies are based on relatively homogeneous populations in late toddlerhood, and typically examine the qualities of the mother and child independently of each other. With growing consensus that child development can be optimized with family-centered rehabilitation services (DesJardin, 2003; Moeller, 2000), this study assesses the potential for a video-feedback intervention to afford contemporary hearing families and their DHH child with family-centered strategies to optimize the quality of parent–child interactions in the prelingual period, a time in which important foundations for child development are laid. Considering the bidirectional influence that both members of a dyad exert in social interactions, the behaviors of both parent and child must be assessed. The EA Scales (Biringen, 2008) provide a holistic measure of the dynamic relational synchronicity between a mother and child, and have been previously used to examine differences in interactions with typically and atypically developing infants (Lam & Kitamura, 2010; Pressman, Pipp-Siegel, Yoshinaga-Itano, & Deas, 1999; Pressman, Pipp-Siegel, Yoshinaga-Itano, Kubicek, & Emde, 1998). They will be used to measure change in the interactive behaviors of mother and child in this study.
Video-feedback intervention is based on the review of video clips taken during a participant’s natural social interactions, and have been shown to enhance the quality of parent–child interaction and parental well-being in populations at-risk for developmental delay. Participation in three to four sessions of video-feedback intervention, enhance parental attitudes and interactive behaviors, and improve child development in families with problematic attachment relationships (Juffer, Bakermans-Kranenburg, & van IJzendoorn, 2005). The effectiveness of the video-feedback intervention used in this study, video interaction guidance (VIG), has been established in the field of pediatrics (see Fukkink, 2008 for a review), and shown to enhance parent–child communication when a child has cerebral palsy (Wadnerkar, Pirinen, Haines-Bazrafshan, Rodgers, & James, 2012). The theoretical premise underlying VIG is strengths based and emphasises the parent’s role in identifying family-specific goals to work on, and guided shared review of only positive video examples to provide a foundation to self-model (Bandura, 1986, 1997) their own successful moments of communication. The intervention’s flexibility and focus on empowering parents in the self-reflection and microanalysis of their own successful behaviors (see James, 2011; Kennedy, 2011 for further details on the intervention) is intended to facilitate a critical element of child development, that is, sensitive parenting.
To date, there is widespread controversy surrounding the extent to which child hearing loss adversely affects mother’s psychosocial wellbeing. Psychosocial factors such as stress, depression, and anxiety are detrimental to the expression of maternal sensitivity (Shin, Park, Ryu, & Seomun, 2008), and there is evidence that these adverse factors are commonly faced by hearing families with prelingual DHH children (Topol, Girard, St Pierre, Tucker, & Vohr, 2011, but see Lederberg & Golbach, 2002 for alternate findings). Families with DHH children report increased behavior problems and more context-specific stress in relation to language delays, than parents with hearing children (Hintmair, 2006; Quittner et al., 2010). Nevertheless, there are relatively few studies that document the influence that early interventions have on a mother’s belief in her ability to parent a child that is DHH. Given that one’s belief in their ability to carry out a task is related to the level of success in task completion (Bandura, 1997), it is important to elucidate whether the self-esteem of hearing mothers with DHH infants can be enriched with early intervention. Since hearing mothers identify an increased need for social support when raising a child who is DHH (Freeman, Dietrich, & Rak, 2002; Park, Warner, Sturgill, & Alder, 2006), the identification of interventions that can reduce any negative perceptions associated with raising a DHH child are paramount.
Using a short-term longitudinal follow-up design, this pilot study tests whether participation in a video-feedback intervention facilitates (a) more optimal social engagement and sensitivity between hearing mothers and their prelingual DHH child, and (b) positively influences the psychosocial wellbeing of the mother. In an attempt to more accurately capture the heterogeneity of DHH infant populations and provide new insight to a cohort that has been largely eluded by research, this study focuses on the prelingual period to provide a common baseline and represent a trying period in which communication breakdowns are likely to occur (Lam & Kitamura, 2010; MacTurk et al., 1993). With evidence that the EA of hearing caregiver–child dyads is amenable to change following participation in an intervention program (Biringen et al., 2012), and the widespread use of the Rosenberg Self Esteem Scale to measure global self-worth (Gray-Little, Williams, & Hancock, 1997), these scales will be used to assess intervention outcomes in the present study. It was hypothesized that families would show increases in parent and child EA and maternal self-esteem from pre to postintervention.
Method
Study Design
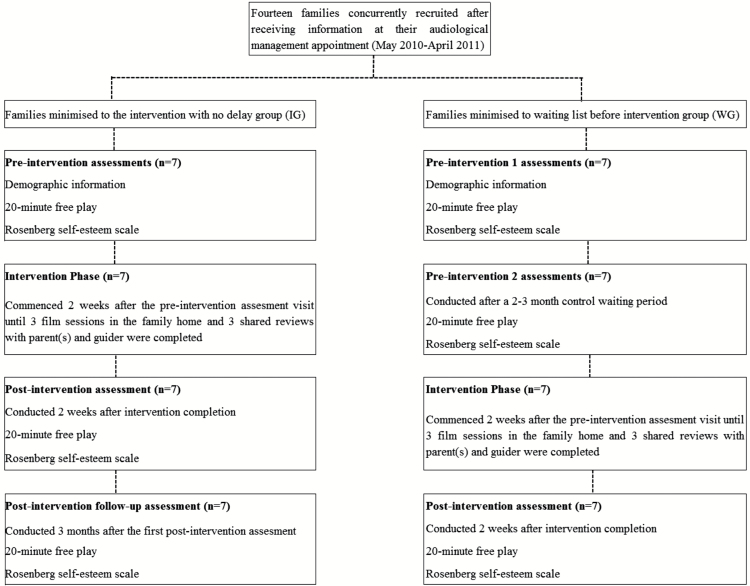
In order to examine intervention effects and longer term maintenance of intervention effects, this study employed a prospective short-term longitudinal design using pretest, posttest, and follow-up assessments with two different groups of families. Families were concurrently recruited and stratified to one of two treatment conditions, either the (a) intervention group (IG) or (b) waiting list control before intervention group (WG) to enable within family comparisons before and after intervention in addition to providing a waiting list control period. The WG schedule was designed to test for stability of the dependent variables across a waiting period approximating the duration of the intervention phase prior to testing intervention effects, and the IG schedule tested immediate and longer term retention of intervention effects. The WG completed three visits, two preintervention visits interspersed by an 8–12 week control waiting period and a postintervention visit. The IG completed three visits, one preintervention and two postintervention. Figure 1 illustrates the flow of participants through the assessment visits. The recruitment procedure and study protocol received ethics approval from Nottingham University Hospitals Trust and the Derbyshire Research Ethics Committee, UK.
Figure 1.
Flow chart showing the assessment schedule for participants. As depicted half of the participants commenced the intervention without delay, and half of the participants completed an 8–12 weeks control waiting period prior to commencing the intervention phase. Both groups completed three laboratory assessments.
Participants
Fourteen families with hearing mothers 1 and congenitally deaf and prelingual children were recruited after responding to information packs provided at audiological management services (Primary Care) for children with hearing impairment between June 2010 and July 2011. Written informed consent was obtained from each parent prior to starting the study. Participants were of British origin, however one family of Latvian origin was provided with assistance from an interpreter at all assessment and intervention visits. To reflect the heterogeneity of children who are congenitally deaf and prelingual, the only exclusion criterion was children who were not at a prelinguistic stage of development and could produce more than 50 signed/spoken words as reported by the parent on the Vineland Adaptive Behavior Scales (Sparrow, Balla, & Cicchetti, 1984). Thus, participants in this study had a wider age range than may be expected for a prelingual child. Families were randomly stratified to the intervention group (IG) or waiting-list before intervention group (WG) using a minimization software program (Altman & Bland, 2005) based on child age, sex, level of hearing loss, and additional needs. Details of the intervention are provided below. The children in the IG were an average age of 3 years, 4 months (SD: 2.6; range: 6 months–6 years, 2 months), and WG were an average age of 1 year, 4 months (SD: 1.10; range: 9 months–3 years, 2 months). As is commonly found with childhood hearing loss, children in both groups were predominantly male. Children were reported to be in good health at all study visits. Further details of the sample are provided in Table 1. There was no attrition from the study. There were no statistical differences between groups in terms of sex, level of hearing loss, type of hearing prostheses, presence of complex needs, birth order, or child age at enrolment to the study. Thus, while the inclusion of children with additional needs resulted in a broader age range in participants, this did not statistically differ between groups. Participants were compensated for travel costs incurred when attending the laboratory assessments.
Table 1.
Demographic information for the DHH children at pre and postintervention
| Intervention group (IG) | Waiting list before intervention group (WG) | |
|---|---|---|
| Sex | Five male; two female | Five male; two female |
| Hearing loss | Six Profound; one moderate-severe | Seven Profound; one moderate-severe |
| Hearing prostheses | Three hearing aids, three bilateral cochlear implants, one unilateral CI | Four hearing aids, three bilateral cochlear implants |
| Cognitive status birth order | One learning difficulties, one autism, five typically developing three first born; four second born | One cytomegalovirus/developmental delay, one premature, no peripheral vision five typically developing two first born; five second born |
Outcome Measures
Emotional availability
The EA Scales, Infancy/Early Childhood version (4th edition; Biringen, 2008) were used to score the quality of interactive congruence shown by the mother and child during each 20-min free play recorded during assessment visits (the first few minutes of each tape was not used to allow families time to settle into natural play routines). The EA scales measure six dimensions: parental sensitivity, parental structuring, parental nonintrusiveness, parental nonhostility, child responsiveness, and child involvement. A direct global score is rated for each dimension using a 7-point scale with a score of 1 indicating a nonoptimal level for the dimension, and 7 demonstrating the most optimal level. All videos were coded by a single coder who was blind to the assessment session for each video. EA for the mother and child were coded separately, that is, the video was viewed on one occasion to code the maternal dimensions, and on a separate occasion to code the child dimensions. Inter-rater reliability was obtained by a second coder also blind to the assessment session on 30% of the sample tapes randomly selected from pre-, post, and follow-up postintervention visits. Both coders were certified reliable (r > .80) in using the 4th edition EA scales following distance training by the scales author. Intraclass correlations calculated for absolute agreement showed .92 agreement for parental sensitivity, .80 agreement for parental structuring, .97 agreement for parental nonintrusiveness, .99 agreement for parental nonhostility, .94 agreement for child responsiveness, and .88 agreement for child involvement. The EA scales have good test retest reliability with moderate to strong correlations (Bornstein et al., 2006), and have shown sensitivity to caregiver child dyads participating in an EA intervention program (Biringen et al., 2012).
Rosenberg Self-Esteem Scale
The Rosenberg Self-Esteem Scale (RSES) (Rosenberg, 1965) was used to assess mothers self-esteem at pre- and postintervention and follow-up. The 10-item instrument assesses an individual’s overall evaluation of their self-worth or self-acceptance on a likert scale ranging from 1 (strongly disagree) to 4 (strongly agree). The scale has demonstrated adequate validity in assessing maternal psychosocial health and is sensitive to changes in maternal psychosocial health arising from participation in parenting interventions (see Barlow, Coren, & Stewart-Brown, 2002 for a review).
Intervention
The intervention uses video feedback of spontaneous parent–child interactions to increase appropriate responsiveness to a child’s communicative cues, and promote attuned behavior between parent and child. It involved a: (a) a goal setting session; (b) three filming sessions of parent–child interaction in the family home, and (c) three shared review sessions in which three short video clips (demonstrating attuned responses linked to the family’s goal) were played so families could microanalyze and discuss the behaviors that facilitated successful communication with their child.
Parental engagement with intervention was facilitated from the outset as parents must specify their own goals for the intervention work which helps the practitioner decide how to make the films and which clips to select (Kennedy, Landor, & Todd, 2011). With the assistance of the interventionist, parents begin the intervention by participating in a goal-setting conversation (~15min) where they refine a goal based on any aspect of their family life they would like to see a change (e.g., “I want to see if I can get [child’s name] attention when I call his name”, “I want to see if she pays attention when I talk”, “When I’m following the speech and language advice…I want to use the film to find out whether it has an impact”). The interventionist then takes a brief (~15min) video recording of a typical interaction between the mother and child in the family home in a context that elicits behaviors related to their goal; for example, while building towers together with toy blocks; during unstructured play with various toys while eating morning tea; while mother and child play with dolls and style the child’s hair and a doll’s hair.
Following the filming session, the interventionist analyses the film using a set of VIG contact principles (including eye-gaze and attentiveness, initiative and reception of verbal and nonverbal initiatives, and turn-taking behaviors that foster attuned responses) to select three short clips of positive communication to replay for the parent in a subsequent shared review visit. During the shared review session (~45min), the parent and interventionist microanalyze and reflect on the behaviors exemplified in three short clips using the VIG contact principles to discuss the process surrounding the highly successful and attuned interactive behaviors that were filmed during a natural interaction. The intervention film and shared review sessions were conducted in two separate visits and each took place once per month for each family.
Procedure
Prior to participation in the intervention program, all families were video recorded during an unstructured 2 free play interaction in a purpose built family room at the Nottingham Hearing Research Unit. Unstructured free play recordings were taken via three wall mounted hard-drive video cameras disguised with fluffy toys (so that only the lens was showing), two of which were remote controlled by an experimenter in an adjacent room. Mothers were instructed to play and spend time with their child as they normally would at home using any of the toys available (i.e., puppets, dolls, books, tea-sets, puzzles, musical instruments, bubbles, balls, and blocks) for up to 25min. They were allowed to take a break if required. Families then participated in the video-feedback intervention (detailed above) with an accredited interventionist. Following intervention completion, families were video recorded in free play interactions at the Research Unit 2 weeks after completion of the intervention (and at 8–12 weeks postfollow up in the IG group). Self-reports of parental self-esteem were collected at all laboratory assessments.
Results
The aim of this study was to test whether the quality of parent–child communication measured by ratings of EA, and parental self-esteem would be improved after participation in a pilot video-feedback intervention program. Families were randomly allocated to one of two intervention schedules, namely, the wait-list before intervention group (WG) or the intervention group (IG) in which families completed three assessments evaluating their interactive behaviors pre- and postintervention. Data for the dependent variables parental sensitivity, parental structuring, parental nonintrusiveness, parental nonhostility, child responsiveness, child involvement, and parental self-esteem were subject to preliminary analysis to determine whether the double pre-intervention baseline in the WG and double postintervention visits in the IG showed any change. Paired t-tests showed no statistical difference from preintervention 1 to preintervention 2 in the WG, and no difference from postintervention 1 to postintervention 2 for the IG group. To test for main effects the dependent variables were analyzed in a 2 (Group: IG, WG) × (2) (Assessment visit: Pre, Post) mixed analyses of variance (ANOVAs). Descriptive statistics for EA at pre and postintervention are provided in Table 2. Examples of parent’s responses to the intervention in their final shared review are provided in Table 3.
Table 2.
Means and standard deviations for ratings of emotional availability at the three assessments for families in the wait-list control group (WG) and intervention without delay group (IG)
| WG (n = 7) | IG (n = 7) | ||||||
|---|---|---|---|---|---|---|---|
| Preintervention | Preintervention after waiting | Postintervention | Preintervention | Postintervention | Postintervention follow-up | ||
| M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | ||
| Maternal sensitivity | 5.46 (0.51) | 5.57 (0.45) | 5.79 (0.64) | 4.93 (0.84) | 5.64 (0.56) | 5.93 (0.53) | |
| Maternal structuring | 5.11 (0.45) | 5.40 (0.35) | 5.64 (0.38) | 5.07 (0.61) | 5.57 (0.45) | 5.82 (0.37) | |
| Maternal nonintrusiveness | 6.29 (0.49) | 6.07 (0.67) | 6.29 (0.57) | 5.54 (1.39) | 6.21 (0.57) | 6.15 (0.63) | |
| Maternal nonhostility | 6.07 (1.02) | 6.21 (0.39) | 5.96 (0.98) | 5.71 (0.95) | 6.57 (0.45) | 6.5 (0.41) | |
| Child responsiveness | 4.57 (0.35) | 4.86 (0.56) | 5.29 (0.70) | 4.71 (0.64) | 5.43 (0.73) | 5.57 (0.35) 5.50 (0.58) | |
| Child involvement | 4.46 (0.37) | 4.79 (0.49) | 5.43 (0.53) | 4.79 (0.76) | 5.32 (0.80) | ||
Note. Standard deviations are in parentheses.
Table 3.
Examples of participant reflections on their intervention experience during shared review sessions with the VIG guider
| Parent’s goal | Reflection of the parent |
|---|---|
| To get cooperation from the child at bed times | “It’s much better than I expected… Everything has changed” |
| To see whether she could give her child space and create opportunities that would allow her to take turns communicating | “I can stand back—I can do it” |
| See how to support wearing the cochlear implants | “It doesn’t feel like a battle getting them on now” |
| Wanted the child to learn to say “mum” | “I think he’ll be able to say a few words—more than I’d hoped for” |
| Wanted to understand how her child listened and how she could support listening behaviors | “we achieved much more than we hoped for” |
Evaluation of EA
The ANOVA comparing treatment outcomes for the parental dimensions showed: a significant difference in scores of parental sensitivity according to the assessment visit F(1,12) = 10.787, p = < .01, ηp 2 = .47, with an increase from pre (M = 5.25) to postintervention (M = 5.71). There was no effect of group, and no interaction between group and time. Parental structuring also showed a main effect for assessment visit F(1,12) = 5.40, p = < .05, ηp 2 = .31, with an increase from pre (M = 5.23) to postintervention (M = 5.61). There was no effect of group, and no interaction between group and time. Participation in the video-feedback intervention revealed no effect on ratings of parental nonintrusiveness (all p > .05). Results for parental nonhostility showed a significant interaction between group and time F(1,12) = 6.881, p = < .05, ηp 2 = .36, with ratings of parental nonhostility significantly larger from preintervention (M = 5.71) to postintervention (M = 6.57) for the IG but not WG group. Results for child responsiveness showed a main effect for assessment visit F(1,12) = 20.757, p = < .01, ηp 2 = .63 with an increase from preintervention (M = 4.79) to postintervention (M = 5.36). There was no effect of group, and no interaction between group and time. There was a main effect for child involvement F(1,12) = 41.354, p = < .01, ηp 2 = .78, with scores significantly higher from preintervention (M = 4.79) to postintervention (M = 5.38). There was no effect of group, and no interaction between group and time. Overall, the measure of assessment visit (pre vs. postintervention) showed a large effect on ratings of 5 of the 6 EA subscales.
Evaluation of Parental Self-Esteem
The results of the ANOVA showed a significant difference on mothers reported self-esteem from preintervention (M = 20.42) to postintervention (M = 22.71), F(1,12) = 4.815, p = < .05, ηp 2 = .29. There was no difference for group, nor any interaction between group and time. Thus, the intervention showed a significantly positive effect on reported self-esteem.
Parent’s Reflections at Postintervention
The reflection of a subset of the parents is presented below to illustrate their overall attitudes to the intervention.
Discussion
This study examined the impact of a pilot psychosocial video-feedback intervention on the quality of parent–child interaction and parental self-esteem in the context of prelingual childhood deafness. With consensus that participation in family intervention improves outcomes for DHH children (Desjardin, 2003; Yoshinaga-Itano, 2003; Moeller, 2000), this study used observational (EA Scales; Biringen, 2008) and self-report (RSES; Rosenberg, 1965) measures to provide new knowledge on the effect of a family-centered intervention that aimed to support hearing parents in providing an optimal environment for the development of their DHH child. To obtain a control waiting group and fulfil the ethical consideration of providing intervention to families that request it, all families received the video-feedback intervention, albeit following one of two different schedules (a waiting period, or no waiting period). In accordance with our hypotheses, the results showed a significant increase in scores from pre to postintervention on all but one of the EA dimensions: parental sensitivity, parental structuring, parental nonhostility, child responsiveness, and child involvement. Furthermore, positive results were shown regardless of the intervention schedule that families completed. Thus, participation in VIG enhanced the quality of social communication and sensitivity in parent–DHH child interactions.
Following the intervention, increased scores on the sensitivity and structuring dimensions of the EA scales indicated that parents were rated as showing more consistently attuned affect, more congruent and flexible responses to the child, and were more proactive in scaffolding interactions. Increased scores on the nonhostility scale indicate that parents were able to regulate overt and covert displays of negative emotions such as disapproval, impatience, and frustration. Furthermore, increased scores on the child responsiveness and child involvement dimensions showed that DHH children showed more verbal and nonverbal responsiveness and engagement with their parent, displayed more positive affect and connection throughout the interaction, and did not exclude the adult. The results provide important new evidence that three sessions of an accredited video-feedback intervention can achieve significant improvement in the dynamic interactive behaviors of parent’s and DHH children during the prelingual period. Since the behaviors that comprise each of these dimensions were not trained or specifically targeted by the intervention, the finding that parental sensitivity, structuring, and nonhostility, and child responsiveness and involvement were all enhanced postintervention highlights the strength of tailoring video-feedback sessions to address family specific goals to improve parent–child communication. Furthermore, the positive intervention effects indicate that the intervention empowered parents to increase and expand upon their use of the attuned behaviors that were identified in shared reviews to everyday interactions with their child. Certainly, parents talked about an enhanced belief in their parenting ability, a sense of empowerment and enjoyment in interacting with their child, and feeling that the intervention exceeded their expectations during their shared reviews. As shown in Table 3, these attitudes were shown whether parents were focusing on goals relating to their ability to follow the directions of the speech and language therapists, or whether they were focused on understanding child behaviors and how they could best support their child.
There was no change in parental nonintrusiveness from pre- to postintervention. These findings concur with other studies that show no effect of a psychosocial modelling intervention on parental nonintrusiveness in the context of postnatal depression, despite positive intervention effects on the remaining parental and child dimensions (van Doesum, Riksen-Walraven, Hosman, & Hoefnagels, 2008). The lack of improvement on the nonintrusiveness dimension may indicate that this characteristic is less amenable to change as a result of intervention as no EA dimension was scored in the clinical range, nor were there any reports of any major care issues in study participants, thus when scored near ceiling, the intervention is less likely to show significant changes in behavior. Overall, the preintervention EA scores concur with findings that contemporary hearing mothers with DHH children persist in trying to provide a stimulating social environment for prelingual DHH infants (Lam & Kitamura, 2010), and importantly, are not as adversely controlling, or intrusive of their child as previous studies with later-diagnosed children suggest (Henggeler, Watson, & Cooper, 1984; Wedell-Monnig & Lumley, 1980). The results are consistent with previous research (Pipp-Siegel et al., 1998; Yoshinaga-Itano, 2003) in showing that the enhancement of factors such as parental sensitivity and child responsiveness in interactions with DHH populations involves participation in early intervention.
In terms of the infant, preintervention results concur with findings that DHH infants show a more subdued level of responsiveness and are less engaged in social interaction than hearing infants (Koester, 1995; Lam & Kitamura, 2010; Lederberg & Mobley, 1990). Critically, increased child responsiveness and involvement at postintervention demonstrate the effectiveness of the intervention in facilitating an increase in parental behaviors that stimulate child responsiveness and involvement because children were not involved in setting the goals of the intervention, nor did they receive any guidance on interactive behaviors. The enhancement of the child’s interactive behaviors concur with other intervention studies showing improvements in the behaviors of children with attachment difficulties following participation in video-feedback intervention (Fukkink, 2008; Juffer et al., 2005). More importantly, the results provide support to the argument that access to family-centered early intervention is a critical component in improving the outcomes of young DHH children (DesJardin, 2003; Moeller, 2000; Yoshinaga-Itano, 2003).
Increases in reports of parental self-esteem at postintervention are promising as parental self-esteem was not directly targeted by the intervention. However, it must be acknowledged that the positive effect on self-esteem was conservative and may be better assessed with a measure that directly assesses parental self-efficacy. It may be the case that greater changes in self-esteem develop over a longer period of time which was not captured in the short-term follow-up of this study. Given the video-feedback intervention is based on the premise of empowering parents to perpetuate more successful communicative behaviors (James, 2011; Kennedy et al., 2011), the question remains as to whether the intervention effects could be strengthened with a greater frequency of sessions. Overall, the results concur with the conclusions of a meta-analysis—that shorter interventions lead to more positive outcomes for interventions that target sensitivity and attachment behaviors (Bakermans-Kranenburg, van Ijzendoorn, & Juffer, 2003). They also replicate the findings of other video-feedback intervention studies that show enhancement in both parental attitudes and interactive behaviors after participation in only three to four sessions (Fukkink, 2008; Juffer et al., 2005), and extend these findings to the context of prelingual childhood hearing loss.
These results provide critical knowledge to a field that currently lacks an evidence base beyond early access to amplification and intervention services, on best practice in optimizing child outcomes in the growing population of very young DHH infants. The positive intervention effect on parent and child EA, and parental self-esteem underlines the plausibility of clinical application of video-feedback intervention to enhance the attitudes and communicative behaviors of hearing families with DHH children. With evidence that maternal sensitivity and infant responsiveness at 2 years of age predict gains in the expressive language of DHH children at 3 years (Pressman, Pipp-Siegel, Yoshinaga-Itano, & Deas, 1999), quantifying the effect of the intervention on child language outcomes is an important next step, and is currently under further investigation.
Although the presence of medical conditions such as developmental delay and autism are commonly found in addition to a child’s hearing loss, children who have additional medical conditions are frequently excluded from larger scale studies on deafness. While it may be the case that the increased complexity of ~40% of the children in study sample limited the degree of change following intervention, the results of this study showed large effect sizes, indicating the practicality of using a video-feedback intervention with DHH populations. Nonetheless, the limited statistical power because of the small number of participants in this pilot study cannot be overlooked. A power analysis indicated that a full scale study using ANOVA, with alpha set at .05, power > .80 and a large effect size, requires a total sample size of 42 (n = 21), thus further work needs to be conducted to consolidate the findings.
With empirical evidence that children with less responsive mothers show impaired social emotional and cognitive development (Murray, Fiori-Cowley, Hooper, & Cooper, 1996) future studies should place greater focus on assessing additional theoretically relevant outcome variables relating to social outcomes such as maternal stress, parenting self-efficacy, and social competence in the child. The inclusion of such outcome measures is an important step in identifying behaviors that should be targeted and strengthened by early intervention services in DHH populations.
In summary, this study contributes an important new evidence base to support a family-centered intervention for DHH children during the prelingual period when parental scaffolding provides a critical support to child development. The results showed that a psychosocial video-feedback intervention enhanced the dynamic interactive behaviors shown by parent and child during social interactions, particularly in terms of parental: sensitivity, structuring, and nonhostility, and child: responsiveness and involvement. Parental reports of self-esteem also increased following intervention completion. The results have important implications regarding the type of early intervention available for families that are adversely affected by prelingual deafness as we show that participation in three sessions of video-feedback paired with attendance at typical audiological services significantly enhanced the quality of parent–child interactions. Overall, the results underscore that more positive outcomes can be achieved for prelingual DHH children (with and without additional needs) by providing access to evidence based video-feedback interventions. It is hoped that this study will encourage further systematic and widespread research into the effectiveness of early intervention with contemporary DHH cohorts.
Funding
National Institute for Health Research, United Kingdom.
Conflicts of Interest
No conflicts of interest were reported.
Acknowledgments
The authors thank the families who took part in the study and the colleagues in specialist and community National Health Services for their support with the study.
Footnotes
Notes
In one family, the father attended all study visits as the primary caregiver, however, family characteristics and scores on the outcome measures did not differ from the group mean at pre or postintervention baselines thus the term mother will be used to represent all adult caregivers henceforth.
Unlike a face-to-face interaction or structured play, the mother–child pair is free to choose their play activity and move about in the room.
References
- Altman D. G., Bland J. M. (2005). Treatment allocation by minimisation. BMJ, 330, 843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakermans-Kranenburg M. J. van Ijzendoorn M. H., & Juffer F (2003). Less is more: Meta-analyses of sensitivity and attachment interventions in early childhood. Psychological Bulletin, 129, 195–215. doi:10.1037/0033-2909.129.2.195 [DOI] [PubMed] [Google Scholar]
- Bandura A. (1986). Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall. [Google Scholar]
- Bandura A. (1997). Self-efficacy: The exercise of control. New York, NY: W.H. Freeman. [Google Scholar]
- Barker D. H., Quittner A. L., Fink N. E., Eisenberg L. S., Tobey E. A., Niparko J. K. (2009). Predicting behavior problems in deaf and hearing children: The influences of language, attention, and parent-child communication. Development and Psychopathology, 21, 373–392. doi:10.1017/S0954579409000212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow J., Coren E., Stewart-Brown S. (2002). Meta-analysis of the effectiveness of parenting programmes in improving maternal psychosocial health. The British Journal of General Practice, 52, 223–233. [PMC free article] [PubMed] [Google Scholar]
- Biringen Z. (2008). The Emotional Availability (EA) Scales (4th Ed). Retrieved from www.emotionalavailability.com. [Google Scholar]
- Biringen Z. Altenhofen S. Aberle J. Baker M. Brosal A. Bennett S. Coker E. Lee C. Meyer B. Moorlag A., & Swaim R (2012). Emotional availability, attachment, and intervention in center-based child care for infants and toddlers. Development and Psychopathology, 24, 23–34. doi:10.1017/S0954579411000630 [DOI] [PubMed] [Google Scholar]
- Bornstein M. H. (2002). Parenting infants. In M. H., Bornstein (Ed.), Handbook of parenting, children and parenting (Vol. 1, 2nd Ed, pp. 3–43). Mahwah, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Bornstein M. Gini M. Suwalsky J. Putnick D., & Haynes O (2006). Emotional availability in mother-child Dyads: Short-term stability and continuity from variable-centered and person-centered perspectives. Merrill-Palmer Quarterly, 52, 547–571. [Google Scholar]
- Ching T. Y., Dillon H. (2013). Major findings of the LOCHI study on children at 3 years of age and implications for audiological management. International Journal of Audiology, 52 (Suppl 2), S65–S68. doi:10.3109/14992027.2013.866339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DesJardin J. L. (2003). Assessing parental perceptions of self-efficacy and involvement in families of young children with hearing loss. Volta Review, 103, 391–409. [Google Scholar]
- Feldman R, (2012). Parent-infant synchrony: A bio-behavioral model of mutual influences in the formation of affiliative bonds. Monographs of the Society for Research in Child Development, 77, 42–51. doi:10.1111/j.1540-5834.2011.00660.x [Google Scholar]
- Feldman R., Gordon I., Zagoory-Sharon O. (2010). The cross-generation transmission of oxytocin in humans. Hormones and Behavior, 58, 669–676. doi:10.1016/j.yhbeh.2010.06.005 [DOI] [PubMed] [Google Scholar]
- Fleming A. S., O’Day D. H., Kraemer G. W. (1999). Neurobiology of mother-infant interactions: Experience and central nervous system plasticity across development and generations. Neuroscience and Biobehavioral Reviews, 23, 673–685. [DOI] [PubMed] [Google Scholar]
- Freeman B., Dieterich C. A., Rak C. (2002). The struggle for language: Perspectives and practices of urban parents with children who are deaf or hard of hearing. American Annals of the Deaf, 147, 37–44. [DOI] [PubMed] [Google Scholar]
- Fukkink R. G. (2008). Video feedback in widescreen: A meta-analysis of family programs. Clinical Psychology Review, 28, 904–916. [DOI] [PubMed] [Google Scholar]
- Gray-Little B. Williams V. S. L., & Hancock T. D (1997). An item response theory analysis of the Rosenberg Self-Esteem Scale. Personality and Social Psychology Bulletin, 23, 443–451. [Google Scholar]
- Henggeler S. W. Watson S. M., & Cooper P. F (1984). Verbal and nonverbal maternal controls in hearing mother-deaf child interaction. Journal of Applied Developmental Psychology, 5, 319–329. [Google Scholar]
- Hintmair M. (2006). Parental resources, parental stress, and socioemotional development of deaf and hard of hearing children. Journal of Deaf Studies and Deaf Education, 11, 493–513. [DOI] [PubMed] [Google Scholar]
- Hoffman M. F. Quittner A. L., & Cejas I (2014). Comparisons of social competence in young children with and without hearing loss: A dynamic systems framework. Journal of Deaf Studies and Deaf Education. doi:10.1093/deafed/enu040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James D. (2011). Video interaction guidance in the context of childhood hearing impairment: A tool for family centred practice. In H., Kennedy M., Landor, L., Todd (Eds.), Video interaction guidance. A relationship-based intervention to promote attunement, empathy and wellbeing. London, UK: Jessica Kingsley. [Google Scholar]
- Juffer F., Bakermans-Kranenburg M. J., van IJzendoorn M. H. (2005). The importance of parenting in the development of disorganized attachment: Evidence from a preventive intervention study in adoptive families. Journal of child Psychology and Psychiatry, and Allied Disciplines, 46, 263–274. [DOI] [PubMed] [Google Scholar]
- Kennedy H. Landor M., & Todd L (2011). Video interaction guidance: A relationship-based intervention to promote attunement, empathy and wellbeing. London, UK: Jessica Kingsley Publishers. [Google Scholar]
- Koester L. S. (1995). Face-to-face interactions between hearing mothers and their deaf or hearing infants. Infant Behavior and Development, 18, 145–153. [Google Scholar]
- Lam C., Kitamura C. (2010). Maternal interactions with a hearing and hearing-impaired twin: Similarities and differences in speech input, interaction quality, and word production. Journal of Speech, Language, and Hearing Research, 53, 543–555. doi:10.1044/1092-4388(2010/09-0126) [DOI] [PubMed] [Google Scholar]
- Lam C., Kitamura C. (2012). Mommy, speak clearly: Induced hearing loss shapes vowel hyperarticulation. Developmental Science, 15, 212–221. doi:10.1111/j.1467-7687.2011.01118.x [DOI] [PubMed] [Google Scholar]
- Lederberg A. R., Golbach T. (2002). Parenting stress and social support in hearing mothers of deaf and hearing children: A longitudinal study. Journal of Deaf Studies and Deaf Education, 7, 330–345. [DOI] [PubMed] [Google Scholar]
- Lederberg A. R., Everhart V. S. (1998). Communication between deaf children and their hearing mothers: The role of language, gesture, and vocalizations. Journal of Speech, Language, and Hearing Research, 41, 887–899. [DOI] [PubMed] [Google Scholar]
- Lederberg A. R., Mobley C. E. (1990). The effect of hearing impairment on the quality of attachment and mother-toddler interaction. Child Development, 61, 1596–1604. [DOI] [PubMed] [Google Scholar]
- Meadow-Orlans K. P. (1997). Effects of mother and infant hearing status on interactions at twelve and eighteen months. Journal of Deaf Studies and Deaf Education, 2, 26–36. [DOI] [PubMed] [Google Scholar]
- MacTurk R. H., Meadow-Orlans K. P., Koester L. S., Spencer P. E. (1993). Social support, motivation, language, and interaction. A longitudinal study of mothers and deaf infants. American Annals of the Deaf, 138, 19–25. [DOI] [PubMed] [Google Scholar]
- Moeller M. P. (2000). Early intervention and language development in children who are deaf and hard of hearing. Pediatrics, 106, E43. [DOI] [PubMed] [Google Scholar]
- Moeller M. P., Hoover B., Putman C., Arbataitis K., Bohnenkamp G., Peterson B.,…, Stelmachowicz P. (2007). Vocalizations of infants with hearing loss compared with infants with normal hearing: Part I–phonetic development. Ear and Hearing, 28, 605–627. [DOI] [PubMed] [Google Scholar]
- Murray L., Fiori-Cowley A., Hooper R., Cooper P. (1996). The impact of postnatal depression and associated adversity on early mother-infant interactions and later infant outcome. Child Development, 67, 2512–2526. [PubMed] [Google Scholar]
- Papousek, (1992). Early ontogeny of vocal communication in parent-infant interactions. In J., Papousek U, Jurgens, M, Papousek (Eds.), Nonverbal vocal communication: comparative and developmental approaches. New York, NY: Cambridge University Press. [Google Scholar]
- Park A. H., Warner J., Sturgill N., Alder S. C. (2006). A survey of parental views regarding their child’s hearing loss: A pilot study. Otolaryngology–head and neck surgery, 134, 794–800. [DOI] [PubMed] [Google Scholar]
- Pipp-Siegel S. Blair N. L. Deas A. M. Pressman L. J., & Yoshinaga-Itano C (1998). Touch and emotional availability in hearing and deaf or hard of hearing toddlers and their hearing mothers. The Volta Review, 100, 279–298. [Google Scholar]
- Pressman L., Pipp-Siegel S., Yoshinaga-Itano C., Deas A. (1999). Maternal sensitivity predicts language gain in preschool children who are deaf and hard of hearing. Journal of Deaf Studies and Deaf Education, 4, 294–304 [DOI] [PubMed] [Google Scholar]
- Pressman L. J. Pipp-Siegel S. Yoshinaga-Itano C. Kubicek L., & Emde R. N (1998). A comparison of the links between emotional availability and language gain in young children with and without hearing loss. The Volta Review, 100, 251–278. [Google Scholar]
- Quittner A. L., Barker D. H., Cruz I., Snell C., Grimley M. E., Botteri M. (2010). Parenting stress among parents of deaf and hearing children: Associations with language delays and behavior problems. Parenting, Science and Practice, 10, 136–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quittner A. L., Cruz I., Barker D. H., Tobey E., Eisenberg L. S., Niparko J. K. (2013). Effects of maternal sensitivity and cognitive and linguistic stimulation on cochlear implant users’ language development over four years. The Journal of Pediatrics, 162, 343–8.e3. doi:10.1016/j.jpeds.2012.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg M. (1965). Society and the adolescent self-image. Princeton, NJ: Princeton University Press. [Google Scholar]
- Shin H., Park Y. J., Ryu H., Seomun G. A. (2008). Maternal sensitivity: A concept analysis. Journal of Advanced Nursing, 64, 304–314. [DOI] [PubMed] [Google Scholar]
- Sparrow S., Balla D., Cicchetti D. (1984) The vineland adaptive behavior scales: Interview edition, Survey form American Guidance Service. Circle Pines MN: Pearson Clinical. [Google Scholar]
- Topol D., Girard N., St Pierre L., Tucker R., Vohr B. (2011). The effects of maternal stress and child language ability on behavioral outcomes of children with congenital hearing loss at 18-24 months. Early Human Development, 87, 807–811. doi:10.1016/j.earlhumdev.2011.06.006 [DOI] [PubMed] [Google Scholar]
- Trevarthen C. (1998). The concept and foundations of infant intersubjectivity. In S., Braten (Ed.), Intersubjective communication and emotion in early ontogeny (pp. 15–46). Cambridge, UK: Cambridge University Press. [Google Scholar]
- van Doesum K. T., Riksen-Walraven J. M., Hosman C. M., Hoefnagels C. (2008). A randomized controlled trial of a home-visiting intervention aimed at preventing relationship problems in depressed mothers and their infants. Child Development, 79, 547–561. [DOI] [PubMed] [Google Scholar]
- Wadnerkar M. B., Pirinen T., Haines-Bazrafshan R., Rodgers J., James D. (2012). A single case study of a family-centred intervention with a young girl with cerebral palsy who is a multimodal communicator. Child: Care, Health and Development, 38, 87–97. doi:10.1111/j.1365-2214.2011.01214.x [DOI] [PubMed] [Google Scholar]
- Wedell-Monnig J., Lumley J. M. (1980). Child deafnes and mother-child interaction. Child Development, 51, 766–774. [PubMed] [Google Scholar]
- Yoshinaga-Itano C. (2003). From screening to early identification and intervention: Discovering predictors to successful outcomes for children with significant hearing loss. Journal of Deaf Studies and Deaf Education, 8, 11–30. [DOI] [PubMed] [Google Scholar]