Abstract
Non-alcoholic fatty liver disease (NAFLD) is one of the most common forms of chronic liver disease in the Western world. There is a close association with the metabolic syndrome and NAFLD is considered to be the hepatic manifestation of the metabolic syndrome. The components of the metabolic syndrome include hypertension, obesity and insulin resistance which are well established cardiovascular risk factors. The mortality rate of NAFLD patients from myocardial infarction is higher than that in the general United States population and there is also an increased risk of non-fatal cardiovascular events. This article reviews the cardiovascular complications associated with NAFLD. In order to provide comprehensive care of NAFLD patients, physicians need to be aware of, and search for, the cardiac morbidity associated with NAFLD.
Keywords: Cardiovascular, Diastolic dysfunction, Sleep apnea, Palatin-like phospholipase domain containing 3 gene, Non-alcoholic fatty liver disease
Core tip: Non-alcoholic fatty liver disease (NAFLD) is the hepatic manifestation of the metabolic syndrome. Due to the overlapping cardiovascular risk factors in the metabolic syndrome, there are cardiovascular consequences linked to the presence of NAFLD in a patient. We review these complications and also a less well appreciated complication of diastolic dysfunction that is intimately associated with NAFLD. Physicians looking after NAFLD patients need to be aware of these complications and actively search for and treat them.
INTRODUCTION
Non-alcoholic fatty liver disease (NAFLD) is now considered to be one of the most common forms of chronic liver disease in the Western world. NAFLD refers to a clinicopathologic spectrum of conditions ranging from simple steatosis (simple fatty liver) to non-alcoholic steatohepatitis (NASH), involving inflammation and some evidence of liver cell damage, and in some cases, cirrhosis. It occurs in an estimated 25% to 30% of the United States general population, whereas its potentially progressive form, NASH is reported in 2%-3% of the population[1].
Natural history studies of NAFLD showed that 1%-5% of patients with simple steatosis developed cirrhosis[1,2], while patients with NASH showed pathological progression of fibrosis in 15%-39% within 10 years[3,4]. NASH can potentially progress to cirrhosis and its complications including decompensated liver disease and hepatocellular carcinoma. The mortality rate of NAFLD patients in the community was higher than that in the general ultrasound (US) population[5]. Death occurred ranging from 13% to 45% with mean follow up of 8-11 years and coronary artery disease (CAD) was the leading cause of death (25%-28% of mortality)[5,6].
It is the purpose of this article to review the cardiovascular consequences of NAFLD and to suggest a diagnostic approach.
GENETICS
Advances in genome analysis, including the development of informative genetic markers, improved physical mapping methods and improvements in high throughput genotyping technologies, have contributed to the understanding of the pathogenesis of complex diseases. The Dallas Heart Study carried out a genome-wide association study of liver fat content in 2111 people from different ancestry groups[7]. They found a connection between NAFLD evaluated by proton magnetic resonance spectroscopy, with the rs738409 G allele of the palatin-like phospholipase domain containing 3 gene (PNPLA3), also known as adiponutrin. The sequence variation is a C > G single nucleotide change which encodes for the 148 isoleucine to methionine protein variant (Il48M) of PNPLA3.
The PNPLA3 GG genotype has been associated with a higher severity of carotid atherosclerosis in young patients with NAFLD[8]. However, recently a variant of the TM6SF2 gene (E167K0) has been shown to be linked to fatty liver due to reduced secretion of very low-density lipoprotein lipoproteins. This variant has also been shown to provide protection against cardiovascular disease[9].
This suggests that there is likely to be an effect of multiple genetic polymorphisms in the development of NAFLD, which require further study in diverse populations.
METABOLIC SYNDROME
The metabolic syndrome (MS) is defined by differing criteria in the United States, Europe and Asia (Table 1). The essential components of the MS include visceral obesity, insulin resistance, dyslipidemia and hypertension. Along with the epidemic of obesity, the prevalence of MS is increasing worldwide, both in the developing and developed countries. MS is associated with a risk of cardiovascular disease and is a common early abnormality in the development of type 2 diabetes.
Table 1.
Definitions of the metabolic syndrome
| NCEP ATP III | IDF | |
| Absolutely required | None | Central obesity (waist circumference) ≥ 94 cm in males or ≥ 80 cm in females European origin > 90 cm (men), ≥ 80 cm in females |
| Criteria | Any three of the five criteria below | Central obesity plus two of the four criteria below |
| Obesity | Waist circumference > 40 inches in males, or > 35 inches in females | |
| Hyperglycemia | Fasting glucose ≥ 100 mg/dL or treated for DM | Fasting glucose ≥ 100 mg/dL |
| Dyslipidemia | TG ≥ 150 mg/dL or treated for dyslipidemia | TG ≥ 150 mg/dL or treated for dyslipidemia |
| Or | Or | |
| HDL cholesterol < 40 mg/dL in males, or < 50 mg/dL in females or under treatment | HDL cholesterol < 40 mg/dL in males, or < 50 mg/dL in females or under treatment | |
| Hypertension | > 130 mmHg systolic or > 85 mmHg diastolic or treated for HTN | > 130 mmHg systolic or > 85 mmHg diastolic or treated for HTN |
NCEP ATP III: National cholesterol and education program-adult treatment panel III; IDF: International diabetes federation; TG: Triglycerides; HDL: High density lipoprotein; HTN: Hypertension.
In patients with NAFLD, metabolic abnormalities have been reported in 33% to 100% of cases, depending on study methods and selection criteria of NAFLD patients[5,10,11]. MS components including central obesity, hypertension, hypertriglyceridemia, decreased high density lipoprotein cholesterol and impaired glucose test or type 2 diabetes mellitus are commonly found in NAFLD[10,12]. Diabetes and hypertension are present up to 15-fold in patients with NASH compared to those with steatosis alone independent of age or body mass index (BMI)[13].
Thus the metabolic syndrome is strongly linked to NAFLD. Patients presenting with NAFLD need to be examined for the presence of the components of the metabolic syndrome and their complications.
NAFLD AND CARDIOVASCULAR ABNORMALITIES
Since the MS is linked to many well recognized cardiovascular risk factors, it is to be expected that there will be a high prevalence of cardiovascular morbidity in patients with NAFLD (Figure 1). Retrospective studies of cohorts of NAFLD patients have shown myocardial infarction to be the cause of death in 25% compared to 13% in patients with other liver diseases[5]. Another study with biopsy-proven NAFLD found an increased mortality in patients with NASH but not with simple steatosis and that this was primarily due to cardiovascular disease and not liver-related causes[11]. Similar results have been reported from other groups[6,11,14]. These studies had small cohort sizes. In a study with a larger cohort size, cardiovascular disease remained the number one cause of death but there was no difference detected between those patients with NASH or simple steatosis.
Figure 1.
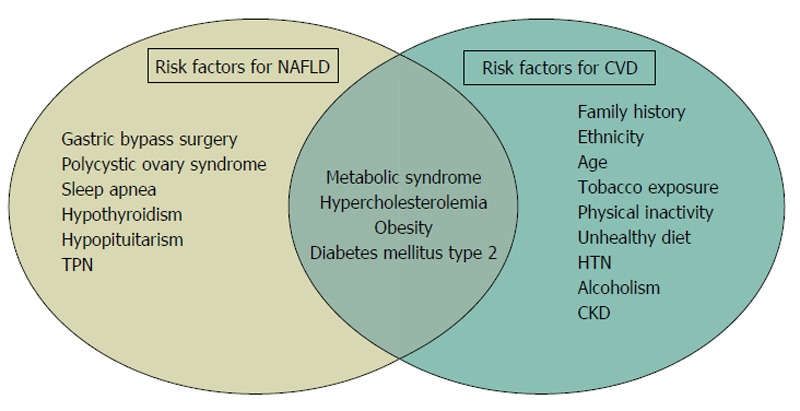
Confluence of the risk factors for both non-alcoholic fatty liver disease and cardiovascular disease. NAFLD: Non-alcoholic fatty liver disease; TPN: Total parenteral nutrition; HTN: Hypertension; CKD: Chronic kidney disease; CVD: Cardiovascular disease.
Prospective studies are usually considered as of higher quality than retrospective studies. Several prospective studies have shown an increased risk of either non-fatal cardiovascular disease events or mortality[15-22].
Coronary artery disease in asymptomatic people can be detected by computed tomography. Several studies have found a connection between coronary artery calcification and NAFLD[23-27], but 2 studies did not find a significant association[28,29].
Patients with NAFLD have a higher prevalence of CAD independent of other risk factors, including glycemic control and MS components[10,26]. The incidence of new CAD events in non-cirrhotic patients with NAFLD varied from 2% to 11% with the overall mortality of 12%- 13%[6,10,16,19,30,31]. The CAD related mortality ranged from 1% to 3% in NAFLD[19,31], and from 12% to 16% in patients with NASH[6,32].
The mechanism for the increase in atherogenesis in NAFLD is multi-factorial including genetic predisposition, insulin resistance and atherogenic dyslipidemia, oxidative stress, chronic inflammation, reduced levels of adiponectin, and altered production of pro and anticoagulant factors[33].
NAFLD AND LEFT VENTRICULAR FUNCTION
Our group was the first to report an association between NAFLD and impaired left ventricular diastolic function[34]. We examined 38 patients with NAFLD diagnosed by ultrasound less than 55 years of age, with a normal exercise test and no diabetes or hypertension. They were compared to an age and gender matched control group. The NAFLD patients had altered left ventricular (LV) geometry and early features of LV diastolic dysfunction. On multivariate analysis only early diastolic velocity, assessed on tissue Doppler imaging was found to be associated with NAFLD. This has also been found by other centers[35-41]. Furthermore this may be an early consequence of NAFLD.
Fallo et al[35] reported diastolic dysfunction in a group of 48 never-treated hypertensive patients with ultrasound diagnosed NAFLD compared to 38 with no NAFLD, who just had LV hypertrophy (LVH). This was independently linked to NAFLD and HOMA on multivariate analysis.
Fotbolcu et al[36] examined 35 NAFLD patients by tissue Doppler imaging that did not have either hypertension or diabetes mellitus. They found a lower early diastolic velocity and also a higher systolic velocity. Another group has found a higher incidence of LVH in hypertensive NAFLD patients (diagnosed by ultrasound) compared to the hypertensive patients without NAFLD[42]. The finding of early diastolic dysfunction in patients with NAFLD has also been found in a study comparing 38 diabetic patients with US diagnosed NAFLD to 18 diabetic patients without NAFLD. The patients with NAFLD had early features of diastolic dysfunction on tissue Doppler echocardiography, which was significant after adjusting for hypertension and other cardiometabolic factors[37]. Furthermore, in obese adolescents, the presence of NAFLD has been shown to be an early marker of cardiac dysfunction[43]. A larger study of 180 obese adolescents compared to 68 healthy controls employing pulsed-wave Doppler echocardiography and pulsed-wave tissue Doppler imaging showed, the NAFLD group had normal LV systolic function, impaired diastolic function, and altered global systolic and diastolic myocardial performance compared to 68 healthy controls[44].
Another study on obese children and adolescents with NAFLD included 108 obese children, 54 with hepatic fat fraction over 5% on magnetic resonance imaging and 18 lean and healthy subjects. Forty one of the NAFLD patients also underwent liver biopsy and 26 were shown to have NASH. Diastolic dysfunction was again found in the patients with NAFLD and also the Tei index which reflects combined systolic and diastolic LV dysfunction was significantly higher in those children with NAFLD. Those patients with biopsy-proven NASH had a significantly lower e’ velocity and higher E-to-e’ and Tei index than those with only NAFLD[45].
The use of 2D speckle tracking echocardiography to determine left atrial deformation parameters was not found to be helpful in a recent study on 55 NAFLD patients and 21 controls from Turkey[46,47]. These studies are summarized in Table 2.
Table 2.
Non-alcoholic fatty liver disease and cardiac structure and function
| Ref. | Methods | Results |
| Goland et al[34] | 38 patients with NAFLD, < 55 years of age and normal exercise test, were compared with an age and sex-matched control group TT echo study including TDI | Patients with NAFLD have mildly altered LV geometry (Increased thickness of the intraventricular septum, posterior wall, and larger LV mass), and early features of left ventricular diastolic dysfunction. Early diastolic velocity on TDI is the only index identifying the patients with NAFLD and metabolic syndrome |
| Fallo et al[35] | Left ventricular morphology/function, metabolic parameters and NAFLD in 86 never-treated essential hypertensive patients subdivided into two subgroups according to the presence (n = 48) or absence (n = 38) of NAFLD at ultrasonography | Patients with NAFLD had similar prevalence of LVH compared to patients without NAFLD, but a higher prevalence of diastolic dysfunction |
| Fotbolcu et al[36] | 35 non-diabetic, normotensive NAFLD patients and 30 controls. TT echo and TDI performed | Patients with NAFLD have impaired LV systolic and diastolic function and lower E' (early diastolic velocity on TDI)s. TDI systolic velocity (S' on TDI) values were lower in NAFLD |
| Bonapace et al[37] | 50 patients with type 2 DM, US diagnosed NAFLD. 32 patients (64%) with NAFLD, compared to other 18 patients. TT echo and TDI performed | Early features of LV diastolic dysfunction may be detected in patients with type 2 diabetes and NAFLD |
| Kim et al[38] | 1886 participants without CVS disease. Stratified by the presence or absence of CT-diagnosed NAFLD, MetS. Assessed by TDI, carotid ultrasound and baPWV | Subjects with both NAFLD and MetS had a higher E/Ea ratio and baPWV, and lower TDI Ea velocity (P < 0.001). Subjects with either NAFLD or MetS also showed significant differences in TDI Ea velocity and baPWV (P < 0.05). No significant differences of CIMT values |
| Ozveren et al[39] | 59 patients with NAFLD and 22 healthy subjects as controls. Basal electrocardiography, echocardiography, and treadmill exercise testing were performed on all patients and controls | The heart rate recovery index is deteriorated in patients with NAFLD |
| Petta et al[41] | Anthropometric, biochemical and metabolic of 147 consecutive biopsy-proven NAFLD cases | Diastolic posterior-wall thickness, left ventricular mass, relative wall thickness, left atrial volume, as well as ejection fraction, lower lateral TDI e', E/A ratio and epicardial fat linked to severe liver fibrosis |
| Mantovani et al[42] | 116 consecutive patients with hypertension and type 2 diabetes. US diagnosed NAFLD, LVH diagnosed by TT echo | LVH higher among diabetic patients with NAFLD. NAFLD is associated with LVH independently of classical CVS risk factors |
| Singh et al[43] | IHTG content (magnetic resonance spectroscopy), insulin sensitivity and β-cell function, and left ventricular function (speckle tracking echocardiography) among 3 groups adolescents: (1) lean-BMI = 20 ± 2 kg/m2); (2) obese with normal IHTG content, BMI = 35 ± 3 kg/m2); and (3) obese with increased IHTG content, BMI = 37 ± 6 kg/m2 | The disposition index (β-cell function) and insulin sensitivity index were approximately 45% and about 70% lower, respectively, and whole body insulin resistance, was about 60% greater, in obese than in lean subjects, and about 30% and about 50% lower and about 150% greater, respectively, in obese subjects with NAFLD than those without NAFLD (P < 0.05 for all) |
| Sert et al[44] | 80 obese adolescents and 37 lean subjects. NAFLD based on elevated transaminases | LV mass and CIMT higher in both NAFLD and non-NAFLD obese patients compared to lean children |
| Pacifico et al[45] | TDI, and MRI for measurement of HFF and abdominal fat mass distribution in 108 obese children, 54 with (HFF ≥ 5%) and 54 without NAFLD, and 18 lean healthy subjects. 41 of the children with NAFLD underwent liver biopsy | Asymptomatic obese children with NAFLD exhibit features of early LV diastolic and systolic dysfunction, and are more severe in those with NASH |
| Kocabay et al[46] | 55 biopsy-proven NAFLD patients and 21 healthy controls. Categorized as simple steatosis, borderline NASH, definitive NASH | LA-Res, LA-Pump and LA-SR(A) were lower in the NAFLD vs control. LA-Res and LA-pump significantly lower in NAFLD subgroups. There were significant differences in LA-SR(A) between healthy controls compared with simple steatosis and borderline |
| Karabay et al[47] | 55 NAFLD patients and 21 healthy controls. Biopsy-proven NAFLD. Categorized as simple steatosis, borderline NASH, definitive NASH. All had echocardiography | Patients with NAFLD and its subgroups have evidence of subclinical myocardial dysfunction in relation to the presence of insulin resistance |
| Gianotti et al[48] | 171 subjects aged > than 65 yr. US diagnosed NAFLD and TT echo | NAFLD had borderline significant association with higher end-diastolic thicknesses of left-ventricle edPW and right-ventricle wall |
| Perseghin et al[49] | 21 nondiabetic men with or without fatty liver matched anthropometrically features assessed by (1) cardiac MRI; (2) cardiac P-MRS; and (3) hepatic H-MRS to assess quantitatively the IHF content | In newly diagnosed patients with fatty liver, fat accumulated in the epicardial area and despite normal LV morphological features, systolic and diastolic functions, there was abnormal LV energy metabolism |
| Hallsworth et al[50] | 19 adults with NAFLD were age-, sex-, and BMI-matched to healthy controls. Cardiac structure and function assessed by high-resolution cardiac MRI. High-energy phosphate metabolism was assessed using[31] P-MRS | Adults with NAFLD had significantly thicker left ventricular walls at systole and diastole than those without fatty liver and showed decreased longitudinal shortening. The eccentricity ratio was significantly higher in the NAFLD group indicating concentric remodelling. Peak whole wall strain was higher in the NAFLD, as was peak endocardial strain. Cardiac metabolism, measured by PCr/ATP ratio, was not altered in NAFLD |
NAFLD: Non-alcoholic fatty liver disease; TDI: Tissue Doppler imaging; DM: Diabetes mellitus; CT: Computed tomography; MetS: Metabolic syndrome; baPWV: Brachial-ankle pulse wave velocity; BMI: Body mass index; IHTG: Intrahepatic triglyceride; HFF: Hepatic fat fraction; NASH: Non-alcoholic steatohepatitis; MRI: Magnetic resonance imaging; MRS: Magnetic resonance spectroscopy; CIMT: Carotid intima-media thickness; TT: Transthoracic; US: Ultrasound; CVS: Cardiovascular; LV: Left ventricular; LVH: Left ventricular hypertrophy.
A finding of NAFLD on ultrasound in the population aged more than 65 years of age may be valuable to alert for the coexistence of multiple cardiovascular risk factors and changes in cardiac morphology and diastolic dysfunction[48].
In newly diagnosed individuals with fatty liver, both systolic and diastolic LV functions were normal but there was abnormal LV energy metabolism[49]. A cohort of 19 NAFLD adults compared to age, gender and BMI-matched controls were shown to have a thicker left ventricular wall in both systole and diastole as well as decreased longitudinal shortening than those without fatty liver[50].
One of the consequences of diastolic dysfunction is atrial fibrillation and NAFLD has been shown to have an increased risk (OR = 4.49) of atrial fibrillation which was independent of age, gender, hypertension, and left ventricular hypertrophy and pr interval[51].
Thus adults with NAFLD have changes in cardiac structure and function that may predate overt cardiac artery disease. We suggest that NAFLD patients undergo a routine transthoracic echocardiogram examination as part of their assessment.
NAFLD AND OBSTRUCTIVE SLEEP APNEA SYNDROME
Obstructive sleep apnea (OSAS) syndrome is a common condition with prevalence estimates of 2% to 4% in the general population. Amongst obese patients the prevalence is as high as 35%[52]. OSAS is accompanied by proinflammatory cytokine production, platelet aggregation, endothelial dysfunction and metabolic dysregulation which can increase the risk of cardiovascular disease[53].
OSA has been shown to be a risk factor for insulin resistance[54-60] and carotid intima media thickening[61], and in addition there are reports of ischemic hepatitis accompanying severe OSAS[62,63].
A study of 163 non-drinking OSAS patients found that the more severe the OSAS, sufferers had more insulin resistance and more steatosis and fibrosis[64]. This was independent of weight, It has also been shown that continuous positive airway pressure (CPAP) therapy for OSAS improves cardiac function, decreases cardiovascular risk and improves insulin resistance[7].
Furthermore, OSAS is linked to NAFLD. This association is more than just a convergence of risk factors. There is evidence for a derangement of the immune system in such patients resulting in a low-grade chronic inflammation[65]. Uncontrolled treatment studies of adults and children with OSAS receiving CPAP treatment and tonsillectomy have shown a decrease in liver enzymes[66]. In addition a proportion of NAFLD patients without severe obesity are at risk for OSAS and this is associated with the severity of the liver damage independently of BMI and other co-factors[67].
Thus the finding of NFALD should prompt physicians to inquire regarding symptoms of OSAS. In addition patients with OSAS need to be assessed for the presence of NAFLD.
CONCLUSION
NAFLD is considered to be the hepatic manifestation of the metabolic syndrome, although there are cases that do not fulfill the metabolic syndrome criteria. Patients with NAFLD have an increased risk for cardiovascular disease, which is in part due to the overlapping of the risk factors of the metabolic syndrome with the risk factors for cardiovascular disease. In addition, however, there are changes in left ventricular function both systolic and diastolic, endothelial function, arterial stiffness and a link with sleep apnea syndrome.
Physicians treating NAFLD patients need to be aware of these cardiovascular complications and actively search for them in order to provide the comprehensive care that patients deserve. We suggest that all patients with NAFLD have an echocardiogram performed in order to detect LVH, systolic and diastolic dysfunction which may increase the risk for cardiac mortality. The benefit of treatment of the metabolic syndrome and associated NAFLD likely extends to many aspects of the cardiovascular system as well. Thus an integrative approach considering all the possible organ complications of the metabolic syndrome is necessary for NAFLD patients.
Footnotes
P- Reviewer: Dirchwolf M, Garcia-Martinez R, Maroni L, Peltec A, Souza-Mello V
S- Editor: Qi Y L- Editor: A E- Editor: Liu SQ
Conflict-of-interest: The authors have no conflicts of interest to declare.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: December 21, 2014
First decision: January 20, 2015
Article in press: April 2, 2015
References
- 1.Adams LA, Lindor KD. Nonalcoholic fatty liver disease. Ann Epidemiol. 2007;17:863–869. doi: 10.1016/j.annepidem.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 2.Fan JG, Farrell GC. Epidemiology of non-alcoholic fatty liver disease in China. J Hepatol. 2009;50:204–210. doi: 10.1016/j.jhep.2008.10.010. [DOI] [PubMed] [Google Scholar]
- 3.Bacon BR, Farahvash MJ, Janney CG, Neuschwander-Tetri BA. Nonalcoholic steatohepatitis: an expanded clinical entity. Gastroenterology. 1994;107:1103–1109. doi: 10.1016/0016-5085(94)90235-6. [DOI] [PubMed] [Google Scholar]
- 4.Matteoni CA, Younossi ZM, Gramlich T, Boparai N, Liu YC, McCullough AJ. Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology. 1999;116:1413–1419. doi: 10.1016/s0016-5085(99)70506-8. [DOI] [PubMed] [Google Scholar]
- 5.Adams LA, Lymp JF, St Sauver J, Sanderson SO, Lindor KD, Feldstein A, Angulo P. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology. 2005;129:113–121. doi: 10.1053/j.gastro.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 6.Rafiq N, Bai C, Fang Y, Srishord M, McCullough A, Gramlich T, Younossi ZM. Long-term follow-up of patients with nonalcoholic fatty liver. Clin Gastroenterol Hepatol. 2009;7:234–238. doi: 10.1016/j.cgh.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 7.Zamarrón C, Valdés Cuadrado L, Alvarez-Sala R. Pathophysiologic mechanisms of cardiovascular disease in obstructive sleep apnea syndrome. Pulm Med. 2013;2013:521087. doi: 10.1155/2013/521087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Petta S, Valenti L, Marchesini G, Di Marco V, Licata A, Cammà C, Barcellona MR, Cabibi D, Donati B, Fracanzani A, et al. PNPLA3 GG genotype and carotid atherosclerosis in patients with non-alcoholic fatty liver disease. PLoS One. 2013;8:e74089. doi: 10.1371/journal.pone.0074089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dongiovanni P, Petta S, Maglio C, Fracanzani AL, Pipitone R, Mozzi E, Motta BM, Kaminska D, Rametta R, Grimaudo S, et al. Transmembrane 6 superfamily member 2 gene variant disentangles nonalcoholic steatohepatitis from cardiovascular disease. Hepatology. 2015;61:506–514. doi: 10.1002/hep.27490. [DOI] [PubMed] [Google Scholar]
- 10.Targher G, Bertolini L, Padovani R, Rodella S, Tessari R, Zenari L, Day C, Arcaro G. Prevalence of nonalcoholic fatty liver disease and its association with cardiovascular disease among type 2 diabetic patients. Diabetes Care. 2007;30:1212–1218. doi: 10.2337/dc06-2247. [DOI] [PubMed] [Google Scholar]
- 11.Ong JP, Pitts A, Younossi ZM. Increased overall mortality and liver-related mortality in non-alcoholic fatty liver disease. J Hepatol. 2008;49:608–612. doi: 10.1016/j.jhep.2008.06.018. [DOI] [PubMed] [Google Scholar]
- 12.Khashab MA, Liangpunsakul S, Chalasani N. Nonalcoholic fatty liver disease as a component of the metabolic syndrome. Curr Gastroenterol Rep. 2008;10:73–80. doi: 10.1007/s11894-008-0012-0. [DOI] [PubMed] [Google Scholar]
- 13.Sung KC, Ryan MC, Wilson AM. The severity of nonalcoholic fatty liver disease is associated with increased cardiovascular risk in a large cohort of non-obese Asian subjects. Atherosclerosis. 2009;203:581–586. doi: 10.1016/j.atherosclerosis.2008.07.024. [DOI] [PubMed] [Google Scholar]
- 14.Söderberg C, Stål P, Askling J, Glaumann H, Lindberg G, Marmur J, Hultcrantz R. Decreased survival of subjects with elevated liver function tests during a 28-year follow-up. Hepatology. 2010;51:595–602. doi: 10.1002/hep.23314. [DOI] [PubMed] [Google Scholar]
- 15.Targher G, Bertolini L, Poli F, Rodella S, Scala L, Tessari R, Zenari L, Falezza G. Nonalcoholic fatty liver disease and risk of future cardiovascular events among type 2 diabetic patients. Diabetes. 2005;54:3541–3546. doi: 10.2337/diabetes.54.12.3541. [DOI] [PubMed] [Google Scholar]
- 16.Hamaguchi M, Kojima T, Takeda N, Nagata C, Takeda J, Sarui H, Kawahito Y, Yoshida N, Suetsugu A, Kato T, et al. Nonalcoholic fatty liver disease is a novel predictor of cardiovascular disease. World J Gastroenterol. 2007;13:1579–1584. doi: 10.3748/wjg.v13.i10.1579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haring R, Wallaschofski H, Nauck M, Dörr M, Baumeister SE, Völzke H. Ultrasonographic hepatic steatosis increases prediction of mortality risk from elevated serum gamma-glutamyl transpeptidase levels. Hepatol Baltim Md. 2009;50:1403–1411. doi: 10.1002/hep.23135. [DOI] [PubMed] [Google Scholar]
- 18.Zhou YJ, Li YY, Nie YQ, Huang CM, Cao CY. Natural course of nonalcoholic fatty liver disease in southern China: a prospective cohort study. J Dig Dis. 2012;13:153–160. doi: 10.1111/j.1751-2980.2011.00571.x. [DOI] [PubMed] [Google Scholar]
- 19.Treeprasertsuk S, Leverage S, Adams LA, Lindor KD, St Sauver J, Angulo P. The Framingham risk score and heart disease in nonalcoholic fatty liver disease. Liver Int. 2012;32:945–950. doi: 10.1111/j.1478-3231.2011.02753.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lazo M, Hernaez R, Bonekamp S, Kamel IR, Brancati FL, Guallar E, Clark JM. Non-alcoholic fatty liver disease and mortality among US adults: prospective cohort study. BMJ. 2011;343:d6891. doi: 10.1136/bmj.d6891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stepanova M, Younossi ZM. Independent association between nonalcoholic fatty liver disease and cardiovascular disease in the US population. Clin Gastroenterol Hepatol. 2012;10:646–650. doi: 10.1016/j.cgh.2011.12.039. [DOI] [PubMed] [Google Scholar]
- 22.Kim D, Kim WR, Kim HJ, Therneau TM. Association between noninvasive fibrosis markers and mortality among adults with nonalcoholic fatty liver disease in the United States. Hepatology. 2013;57:1357–1365. doi: 10.1002/hep.26156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tanaka M, Tomiyasu K, Fukui M, Akabame S, Kobayashi-Takenaka Y, Nakano K, Kadono M, Hasegawa G, Oda Y, Nakamura N. Evaluation of characteristics and degree of remodeling in coronary atherosclerotic lesions by 64-detector multislice computed tomography (MSCT) Atherosclerosis. 2009;203:436–441. doi: 10.1016/j.atherosclerosis.2008.07.013. [DOI] [PubMed] [Google Scholar]
- 24.Santos RD, Nasir K, Orakzai R, Meneghelo RS, Carvalho JA, Blumenthal RS. Relation of uric acid levels to presence of coronary artery calcium detected by electron beam tomography in men free of symptomatic myocardial ischemia with versus without the metabolic syndrome. Am J Cardiol. 2007;99:42–45. doi: 10.1016/j.amjcard.2006.07.057. [DOI] [PubMed] [Google Scholar]
- 25.Assy N, Djibre A, Farah R, Grosovski M, Marmor A. Presence of coronary plaques in patients with nonalcoholic fatty liver disease. Radiology. 2010;254:393–400. doi: 10.1148/radiol.09090769. [DOI] [PubMed] [Google Scholar]
- 26.Chen CH, Nien CK, Yang CC, Yeh YH. Association between nonalcoholic fatty liver disease and coronary artery calcification. Dig Dis Sci. 2010;55:1752–1760. doi: 10.1007/s10620-009-0935-9. [DOI] [PubMed] [Google Scholar]
- 27.Jung CH, Lee WY, Kim SY, Jung JH, Rhee EJ, Park CY, Mok JO, Oh KW, Kim CH, Park SW, et al. The relationship between coronary artery calcification score, plasma osteoprotegerin level and arterial stiffness in asymptomatic type 2 DM. Acta Diabetol. 2010;47 Suppl 1:145–152. doi: 10.1007/s00592-009-0154-z. [DOI] [PubMed] [Google Scholar]
- 28.Ballestri S, Meschiari E, Baldelli E, Musumeci FE, Romagnoli D, Trenti T, Zennaro RG, Lonardo A, Loria P. Relationship of serum fetuin-A levels with coronary atherosclerotic burden and NAFLD in patients undergoing elective coronary angiography. Metab Syndr Relat Disord. 2013;11:289–295. doi: 10.1089/met.2012.0149. [DOI] [PubMed] [Google Scholar]
- 29.McKimmie RL, Daniel KR, Carr JJ, Bowden DW, Freedman BI, Register TC, Hsu FC, Lohman KK, Weinberg RB, Wagenknecht LE. Hepatic steatosis and subclinical cardiovascular disease in a cohort enriched for type 2 diabetes: the Diabetes Heart Study. Am J Gastroenterol. 2008;103:3029–3035. doi: 10.1111/j.1572-0241.2008.02188.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kadayifci A, Tan V, Ursell PC, Merriman RB, Bass NM. Clinical and pathologic risk factors for atherosclerosis in cirrhosis: a comparison between NASH-related cirrhosis and cirrhosis due to other aetiologies. J Hepatol. 2008;49:595–599. doi: 10.1016/j.jhep.2008.05.024. [DOI] [PubMed] [Google Scholar]
- 31.Schindhelm RK, Dekker JM, Nijpels G, Bouter LM, Stehouwer CD, Heine RJ, Diamant M. Alanine aminotransferase predicts coronary heart disease events: a 10-year follow-up of the Hoorn Study. Atherosclerosis. 2007;191:391–396. doi: 10.1016/j.atherosclerosis.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 32.Ekstedt M, Franzén LE, Mathiesen UL, Thorelius L, Holmqvist M, Bodemar G, Kechagias S. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology. 2006;44:865–873. doi: 10.1002/hep.21327. [DOI] [PubMed] [Google Scholar]
- 33.Fargion S, Porzio M, Fracanzani AL. Nonalcoholic fatty liver disease and vascular disease: state-of-the-art. World J Gastroenterol. 2014;20:13306–13324. doi: 10.3748/wjg.v20.i37.13306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Goland S, Shimoni S, Zornitzki T, Knobler H, Azoulai O, Lutaty G, Melzer E, Orr A, Caspi A, Malnick S. Cardiac abnormalities as a new manifestation of nonalcoholic fatty liver disease: echocardiographic and tissue Doppler imaging assessment. J Clin Gastroenterol. 2006;40:949–955. doi: 10.1097/01.mcg.0000225668.53673.e6. [DOI] [PubMed] [Google Scholar]
- 35.Fallo F, Dalla Pozza A, Sonino N, Lupia M, Tona F, Federspil G, Ermani M, Catena C, Soardo G, Di Piazza L, et al. Non-alcoholic fatty liver disease is associated with left ventricular diastolic dysfunction in essential hypertension. Nutr Metab Cardiovasc Dis. 2009;19:646–653. doi: 10.1016/j.numecd.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 36.Fotbolcu H, Yakar T, Duman D, Karaahmet T, Tigen K, Cevik C, Kurtoglu U, Dindar I. Impairment of the left ventricular systolic and diastolic function in patients with non-alcoholic fatty liver disease. Cardiol J. 2010;17:457–463. [PubMed] [Google Scholar]
- 37.Bonapace S, Perseghin G, Molon G, Canali G, Bertolini L, Zoppini G, Barbieri E, Targher G. Nonalcoholic fatty liver disease is associated with left ventricular diastolic dysfunction in patients with type 2 diabetes. Diabetes Care. 2012;35:389–395. doi: 10.2337/dc11-1820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim NH, Park J, Kim SH, Kim YH, Kim DH, Cho GY, Baik I, Lim HE, Kim EJ, Na JO, et al. Non-alcoholic fatty liver disease, metabolic syndrome and subclinical cardiovascular changes in the general population. Heart. 2014;100:938–943. doi: 10.1136/heartjnl-2013-305099. [DOI] [PubMed] [Google Scholar]
- 39.Ozveren O, Dogdu O, Sengul C, Cinar V, Eroglu E, Kucukdurmaz Z, Degertekin M. Deterioration of heart rate recovery index in patients with non-alcoholic fatty liver disease (NAFLD) Med Sci Monit. 2014;20:1539–1543. doi: 10.12659/MSM.890741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Baktır AO, Şarlı B, Altekin RE, Karaman A, Arınç H, Sağlam H, Doğan Y, Erden A, Karaman H. Non alcoholic steatohepatitis is associated with subclinical impairment in left ventricular function measured by speckle tracking echocardiography. Anatol J Cardiol. 2015;15:137–142. doi: 10.5152/akd.2014.5212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Petta S, Argano C, Colomba D, Cammà C, Di Marco V, Cabibi D, Tuttolomondo A, Marchesini G, Pinto A, Licata G, et al. Epicardial fat, cardiac geometry and cardiac function in patients with non-alcoholic fatty liver disease: association with the severity of liver disease. J Hepatol. 2015;62:928–933. doi: 10.1016/j.jhep.2014.11.030. [DOI] [PubMed] [Google Scholar]
- 42.Mantovani A, Zoppini G, Targher G, Golia G, Bonora E. Non-alcoholic fatty liver disease is independently associated with left ventricular hypertrophy in hypertensive Type 2 diabetic individuals. J Endocrinol Invest. 2012;35:215–218. doi: 10.1007/BF03345421. [DOI] [PubMed] [Google Scholar]
- 43.Singh GK, Vitola BE, Holland MR, Sekarski T, Patterson BW, Magkos F, Klein S. Alterations in ventricular structure and function in obese adolescents with nonalcoholic fatty liver disease. J Pediatr. 2013;162:1160–1168, 1168.e1. doi: 10.1016/j.jpeds.2012.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sert A, Pirgon O, Aypar E, Yilmaz H, Odabas D. Relationship between left ventricular mass and carotid intima media thickness in obese adolescents with non-alcoholic fatty liver disease. J Pediatr Endocrinol Metab. 2012;25:927–934. doi: 10.1515/jpem-2012-0187. [DOI] [PubMed] [Google Scholar]
- 45.Pacifico L, Di Martino M, De Merulis A, Bezzi M, Osborn JF, Catalano C, Chiesa C. Left ventricular dysfunction in obese children and adolescents with nonalcoholic fatty liver disease. Hepatology. 2014;59:461–470. doi: 10.1002/hep.26610. [DOI] [PubMed] [Google Scholar]
- 46.Kocabay G, Karabay CY, Colak Y, Oduncu V, Kalayci A, Akgun T, Guler A, Kirma C. Left atrial deformation parameters in patients with non-alcoholic fatty liver disease: a 2D speckle tracking imaging study. Clin Sci (Lond) 2014;126:297–304. doi: 10.1042/CS20130298. [DOI] [PubMed] [Google Scholar]
- 47.Karabay CY, Kocabay G, Kalayci A, Colak Y, Oduncu V, Akgun T, Kalkan S, Guler A, Kirma C. Impaired left ventricular mechanics in nonalcoholic fatty liver disease: a speckle-tracking echocardiography study. Eur J Gastroenterol Hepatol. 2014;26:325–331. doi: 10.1097/MEG.0000000000000008. [DOI] [PubMed] [Google Scholar]
- 48.Gianotti G, Cenni A, Bianchi G, Masetti M, Zappoli P, Muscari A, Zoli M. Diastolic dysfunction and cardiovascular risk in old subjects: possible association with NAFLD? Arch Gerontol Geriatr. 2014;58:188–195. doi: 10.1016/j.archger.2013.10.012. [DOI] [PubMed] [Google Scholar]
- 49.Perseghin G, Lattuada G, De Cobelli F, Esposito A, Belloni E, Ntali G, Ragogna F, Canu T, Scifo P, Del Maschio A, et al. Increased mediastinal fat and impaired left ventricular energy metabolism in young men with newly found fatty liver. Hepatology. 2008;47:51–58. doi: 10.1002/hep.21983. [DOI] [PubMed] [Google Scholar]
- 50.Hallsworth K, Hollingsworth KG, Thoma C, Jakovljevic D, MacGowan GA, Anstee QM, Taylor R, Day CP, Trenell MI. Cardiac structure and function are altered in adults with non-alcoholic fatty liver disease. J Hepatol. 2013;58:757–762. doi: 10.1016/j.jhep.2012.11.015. [DOI] [PubMed] [Google Scholar]
- 51.Targher G, Valbusa F, Bonapace S, Bertolini L, Zenari L, Rodella S, Zoppini G, Mantovani W, Barbieri E, Byrne CD. Non-alcoholic fatty liver disease is associated with an increased incidence of atrial fibrillation in patients with type 2 diabetes. PLoS One. 2013;8:e57183. doi: 10.1371/journal.pone.0057183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mirrakhimov AE, Polotsky VY. Obstructive sleep apnea and non-alcoholic Fatty liver disease: is the liver another target? Front Neurol. 2012;3:149. doi: 10.3389/fneur.2012.00149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Musso G, Cassader M, Olivetti C, Rosina F, Carbone G, Gambino R. Association of obstructive sleep apnoea with the presence and severity of non-alcoholic fatty liver disease. A systematic review and meta-analysis. Obes Rev. 2013;14:417–431. doi: 10.1111/obr.12020. [DOI] [PubMed] [Google Scholar]
- 54.Stoohs RA, Facchini F, Guilleminault C. Insulin resistance and sleep-disordered breathing in healthy humans. Am J Respir Crit Care Med. 1996;154:170–174. doi: 10.1164/ajrccm.154.1.8680675. [DOI] [PubMed] [Google Scholar]
- 55.Ip MS, Lam B, Ng MM, Lam WK, Tsang KW, Lam KS. Obstructive sleep apnea is independently associated with insulin resistance. Am J Respir Crit Care Med. 2002;165:670–676. doi: 10.1164/ajrccm.165.5.2103001. [DOI] [PubMed] [Google Scholar]
- 56.Wilcox I, McNamara SG, Collins FL, Grunstein RR, Sullivan CE. “Syndrome Z”: the interaction of sleep apnoea, vascular risk factors and heart disease. Thorax. 1998;53 Suppl 3:S25–S28. [PMC free article] [PubMed] [Google Scholar]
- 57.Brooks B, Cistulli PA, Borkman M, Ross G, McGhee S, Grunstein RR, Sullivan CE, Yue DK. Obstructive sleep apnea in obese noninsulin-dependent diabetic patients: effect of continuous positive airway pressure treatment on insulin responsiveness. J Clin Endocrinol Metab. 1994;79:1681–1685. doi: 10.1210/jcem.79.6.7989475. [DOI] [PubMed] [Google Scholar]
- 58.Vgontzas AN, Papanicolaou DA, Bixler EO, Hopper K, Lotsikas A, Lin HM, Kales A, Chrousos GP. Sleep apnea and daytime sleepiness and fatigue: relation to visceral obesity, insulin resistance, and hypercytokinemia. J Clin Endocrinol Metab. 2000;85:1151–1158. doi: 10.1210/jcem.85.3.6484. [DOI] [PubMed] [Google Scholar]
- 59.Punjabi NM, Ahmed MM, Polotsky VY, Beamer BA, O’Donnell CP. Sleep-disordered breathing, glucose intolerance, and insulin resistance. Respir Physiol Neurobiol. 2003;136:167–178. doi: 10.1016/s1569-9048(03)00079-x. [DOI] [PubMed] [Google Scholar]
- 60.Punjabi NM, Sorkin JD, Katzel LI, Goldberg AP, Schwartz AR, Smith PL. Sleep-disordered breathing and insulin resistance in middle-aged and overweight men. Am J Respir Crit Care Med. 2002;165:677–682. doi: 10.1164/ajrccm.165.5.2104087. [DOI] [PubMed] [Google Scholar]
- 61.Drager LF, Togeiro SM, Polotsky VY, Lorenzi-Filho G. Obstructive sleep apnea: a cardiometabolic risk in obesity and the metabolic syndrome. J Am Coll Cardiol. 2013;62:569–576. doi: 10.1016/j.jacc.2013.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Henrion J, Colin L, Schapira M, Heller FR. Hypoxic hepatitis caused by severe hypoxemia from obstructive sleep apnea. J Clin Gastroenterol. 1997;24:245–249. doi: 10.1097/00004836-199706000-00013. [DOI] [PubMed] [Google Scholar]
- 63.Mathurin P, Durand F, Ganne N, Mollo JL, Lebrec D, Degott C, Erlinger S, Benhamou JP, Bernuau J. Ischemic hepatitis due to obstructive sleep apnea. Gastroenterology. 1995;109:1682–1684. doi: 10.1016/0016-5085(95)90659-2. [DOI] [PubMed] [Google Scholar]
- 64.Tanné F, Gagnadoux F, Chazouillères O, Fleury B, Wendum D, Lasnier E, Lebeau B, Poupon R, Serfaty L. Chronic liver injury during obstructive sleep apnea. Hepatology. 2005;41:1290–1296. doi: 10.1002/hep.20725. [DOI] [PubMed] [Google Scholar]
- 65.Tarantino G, Citro V, Finelli C. What non-alcoholic fatty liver disease has got to do with obstructive sleep apnoea syndrome and viceversa? J Gastrointestin Liver Dis. 2014;23:291–299. doi: 10.15403/jgld.2014.1121.233.gvt. [DOI] [PubMed] [Google Scholar]
- 66.Garcia JM, Sharafkhaneh H, Hirshkowitz M, Elkhatib R, Sharafkhaneh A. Weight and metabolic effects of CPAP in obstructive sleep apnea patients with obesity. Respir Res. 2011;12:80. doi: 10.1186/1465-9921-12-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pulixi EA, Tobaldini E, Battezzati PM, D’Ingianna P, Borroni V, Fracanzani AL, Maggioni M, Pelusi S, Bulgheroni M, Zuin M, et al. Risk of obstructive sleep apnea with daytime sleepiness is associated with liver damage in non-morbidly obese patients with nonalcoholic fatty liver disease. PLoS One. 2014;9:e96349. doi: 10.1371/journal.pone.0096349. [DOI] [PMC free article] [PubMed] [Google Scholar]


