Abstract
Immunohistochemistry often plays an important role in the evaluation of liver tumors. Recent advances have established a classification system for hepatocellular adenomas (HCAs) based on morphology, molecular alterations, and immunohistochemistry. Specifically, loss of liver fatty acid binding protein is seen in HNF1α-inactivated HCA, staining with serum amyloid A is seen in inflammatory HCA, and diffuse staining with glutamine synthetase (GS) is seen in β-catenin activated HCA. A panel of immunohistochemical stains including glypican-3 (GPC-3), heat shock protein 70, and GS are useful in distinguishing HCC from non-malignant dysplastic nodules. Immunohistochemistry is also useful to determine whether a liver tumor is of primary hepatocellular or metastatic origin. Recently described markers useful for this purpose include arginase-1, GPC-3, and bile salt export pump. These newer markers may offer superior utility when compared to traditional markers of hepatocellular differentiation such as alpha-fetoprotein, hepatocyte paraffin-1, polyclonal carcinoembryonic antigen, and CD10. This paper will review recent advances in the immunohistochemical evaluation of liver tumors.
Keywords: Immunohistochemistry, Hepatocellular adenoma, Focal nodular hyperplasia, Hepatocellular carcinoma
Core tip: Immunohistochemical stains may be an important complement to morphology in the characterization of liver tumors. Immunohistochemical stains can now be used to subtype hepatocellular adenomas. A panel of immunohistochemical stains can help distinguish hepatocellular carcinoma from dysplastic nodules and hepatocellular adenomas. Several new markers of hepatocellular differentiation have been described. These advances are reviewed.
INTRODUCTION
Although the global incidence of hepatocellular carcinoma (HCC) varies from region to region, incidence in Europe and North America has been increasing[1]. The majority of these cancers arise in the setting of chronic liver disease, especially chronic infection by hepatitis B virus (HBV) and HCV or cirrhosis of any cause. There is a male predominance of approximately 3:1[1]. With improvements in imaging, specifically four phase multi-detector commuted tomography and dynamic, contrast-enhanced magnetic resonance imaging, there has been a concomitant increase in the detection of small liver nodules. While many of these lesions can be diagnosed on imaging, histologic diagnosis remains the gold standard, especially for small nodules (< 1-2 cm), with the goal of diagnosing cancers at an early stage where treatment may be curative. Nonetheless, it can be challenging to distinguish HCC from other hepatocellular proliferations, such as focal nodular hyperplasia (FNH), hepatocellular adenoma (HCA), and dysplastic nodules, particularly when presented with small samples (e.g., needle biopsy). Other primary tumors (e.g., cholangiocarcinoma) and metastases may also enter the differential depending on morphology and history. In recent years, there have been a number of advances reported employing immunohistochemistry to answer such questions. These advances are reviewed herein.
FNH
FNH is a benign hepatocellular lesion thought to develop in response to localized hyperperfusion relating to the presence of an anomalous artery[2,3] with a female predominance of 8:1 and a median age of 38[4]. Histologically, the classical type is a hyperplastic nodular lesion with a central scar containing the anomalous vessel, and a ductular reaction. Most cases are asymptomatic and are often incidentally discovered[4]. Frequently, this entity can be reliably diagnosed on imaging and no treatment is required; however, some cases may be difficult to confirm with imaging, and may require biopsy to rule out HCA and HCC which could require surgical excision. In challenging cases, immunohistochemistry for glutamine synthetase (GS, an enzyme that catalyzes the synthesis of glutamine from glutamate and ammonia, important in nitrogen metabolism) is useful and shows a characteristic geographic “map-like” pattern of staining[5] (Figure 1).
Figure 1.
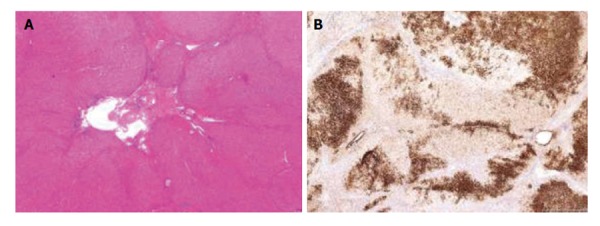
Focal nodular hyperplasia. A: On low-power, focal nodular hyperplasia (FNH) is characterized by nodular hepatocellular proliferation with central scar (hematoxilin and eosin stain, × 1); B: FNH showing typical map-like pattern on glutamine synthetase immunohistochemistry (anti-glutamine synthetase/diaminobenzidine chromogen, × 2).
HCA
In contrast to FNH, HCAs are neoplastic clonal proliferations. Resection of adenomas larger than 5 cm is recommended due to the risk of hemorrhage and potential malignant transformation in up to 7% of cases[6]. Risk factors for HCA are female gender, steroid sex hormone exposure (oral contraceptives, anabolic steroids, pregnancy), glycogen storage disease types I and III, maturity onset diabetes of the young type 3 (MODY3), and familial adenomatosis coli[7,8]. Adenomas can often be diagnosed on imaging, but if the differential diagnosis includes FNH or HCC, the lesion may be biopsied. Based on molecular and immunohistochemical studies, Bioulac-Sage et al[8] have identified 4 types of hepatocellular adenomas, now recognized by the World Health Organization. Immunohistochemical stains are therefore useful for both diagnosis and sub-classification.
HNF1α-inactivated HCA
In HNF1α-inactivated HCA (H-HCA), inactivation of both alleles of the HNF1α gene, which encodes hepatocyte nuclear factor 1 (a transcription factor related to hepatocyte differentiation), results in increased production of fatty acids, steatosis in hepatocytes, and loss of liver fatty acid binding protein expression, which can be appreciated by a negative immunohistochemical stain (Figure 2A and B). H-HCA accounts for 35%-40% of HCAs and is associated with MODY3 and adenomatosis[2,6,9], but is not thought to be associated with higher risk of transformation to HCC.
Figure 2.
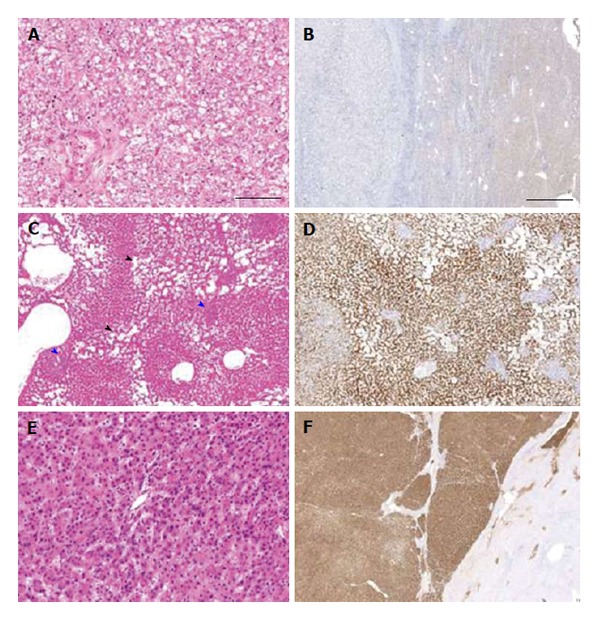
Hepatocellular adenoma. A and B: HNF1α-inactivated hepatocellular adenoma (HCA) with marked steatosis [A, hematoxylin and eosin (HE) stain, × 20] and loss of liver fatty acid binding protein (LFABP) expression by immunohistochemistry (left) in comparison to non-neoplastic liver (right) [B, anti-LFABP/3,3’-diaminobenzidine (DAB), × 1]; C and D: Inflammatory HCA with dilated sinusoids (telangiectasia, black arrowheads) and patchy inflammation (blue arrowheads) (C, HE stain, × 5) and diffuse serum amyloid A staining by immunohistochemistry (D, anti-serum amyloid A/DAB, × 5); E and F: β-catenin-activated HCA with strong diffuse staining for glutamine synthetase (upper left), in comparison to centrilobular staining of normal liver (lower right) (E, HE stain, × 20; F, anti-glutamine synthetase/DAB, × 1).
Inflammatory HCA
In inflammatory HCA (IHCA), activating mutations in genes (IL6ST, STAT3, GNAS, FRK) along the JAK-STAT pathway result in increased expression of inflammatory markers including serum amyloid A (SAA)[9,10]. Histologically, IHCA are characterized by an inflammatory infiltrate, vascular anomalies, and may exhibit a ductular reaction. In the past, this lesion was known as “telangiectatic FNH,” but has now been shown by molecular and immunohistochemical analysis to be IHCA[11]. They stain with SAA and C reactive protein by immunohistochemistry (Figure 2C and D) and account for 40%-55% of HCAs[6,9,10].
β-catenin-activated HCA
β-catenin-activated HCAs (β-HCAs) are the subtype of HCA with the highest risk (4%)[12] for transformation to HCC, and account for 10%-15% of HCAs. Histologically, β-HCAs may show cholestasis and both architectural and cytologic atypia including pseudoacinar structures. In β-HCA, activating mutations (predominantly in exons 3, 7, or 8) in the CTNNB1 gene, which encodes β-catenin, cause activation of the WNT/β-catenin pathway. This is the most commonly mutated pathway in HCC[13]. The mutations may lead to upregulation of the gene coding for GS; consequently, this subtype is expected to exhibit abnormal nuclear staining with β-catenin and diffuse GS staining by immunohistochemistry (Figure 2E and F). Staining for β-catenin is less sensitive than staining for GS, though GS is much less specific than nuclear beta-catenin. The purported sensitivity and specificity of GS in this setting is 100% and 89%[8]. However, in our experience, GS may diffusely stain many adenomas which do not exhibit atypical morphologic or clinical signs of atypia[14]. Furthermore, when our group sequenced GS overexpressing HCA, we could identify β-catenin mutations in only 1 OF 8 HCAs (unpublished data). In our opinion, GS overexpression is an imperfect surrogate for β catenin mutation, and should not be a definitional characteristic.
Unclassified HCA
Unclassified HCAs represent the remaining 10% of HCAs, and lack characteristic histology, immunohistochemistry, or molecular changes.
DYSPLASTIC NODULES
The pathogenesis of HCC is thought to be a stepwise accumulation of mutations arising in a small clonal population (dysplastic nodules and a small proportion of adenomas)[13,15]. The background liver is most often cirrhotic, with HBV as the most common underlying cause worldwide, especially in Sub-Saharan Africa and Asia where HBV is endemic, and HCV and the most common underlying cause in the United States[16]. In the cirrhotic liver, it is important to distinguish large regenerative nodules, which are benign, from low- and high-grade dysplastic nodules (H-DN), which precede HCC in a stepwise fashion, and to distinguish these from early and progressed HCC itself. Histologic criteria were established by the International Consensus Group for Hepatocellular Neoplasia in 2009, but the differences between these entities may be subtle as they lie on a continuum. The best criteria to distinguish H-DN from early HCC is the presence of invasion into portal tracts[17]. This feature may not be identifiable on biopsy material, however. Historically, thickened portal plates and subsequently a diminished reticulin framework were noted to be markers of progression from H-DN to early HCC, although an intact reticulin framework could not exclude HCC[18]. In this case, immunostains are a useful aid to histomorphology.
CD34
Normal sinusoidal endothelium does not express CD34. However, since capillarization of sinusoidal endothelium occurs during the progression of dysplastic nodules to HCC (which corresponds to the enhancement seen in HCC on the arterial phase of dynamic imaging modalities), immunostaining for the vascular marker CD34 has been found to be a useful marker of malignant transformation (since it does mark capillarized endothelial cells) . However, while increased to diffuse vascular markings with CD34 is a suspicious finding in a liver tumor, no specific cutoff has yet been established in distinguishing between H-DN and early HCC[18-21].
In studies of biopsy and resection specimens[22,23], a panel of 3 immunostains including glypican-3 (GPC-3), heat shock protein 70 (HSP70), and GS was found to be useful in distinguishing dysplastic nodules from HCC, with a combination of at least any two positive stains shown to be 72% sensitive (resection specimens; 57% on biopsy specimens) and 100% specific in distinguishing early HCC from dysplastic nodules. Overall, it was found that positive staining in at least 2/3 markers supported a diagnosis of HCC, but lack of staining was not sufficient to rule out HCC especially on biopsy specimens.
GPC-3
GPC-3 is a heparan-sulfate cell surface oncofetal proteoglycan noted to be expressed in HCC, but generally not in benign liver (normal or cirrhotic) or in metastatic carcinomas[24,25]. Immunostaining with GPC-3 in HCC may be cytoplasmic and/or membranous. Some authors have found that the sensitivity increases as the tumor becomes less differentiated[25,26]. Other studies have not found higher GPC-3 expression in poorly differentiated tumors, however, so confirmation in additional studies would be helpful[27]. GPC-3 is also useful in distinguishing HCC from HCA[14]. Anecdotally, we have seen strong positivity in a case of scirrhous variant HCC which could easily have been mistaken for metastatic adenocarcinoma (Figure 3). On the other hand, GPC-3 may be less helpful in the fibrolamellar variant of HCC[28]. GPC-3 is known to stain a few other malignancies, such as yolk sac tumor and melanoma[29]. Another caveat is the reported expression of GPC-3 in cirrhotic nodules in cases of hepatitis C infection[30].
Figure 3.
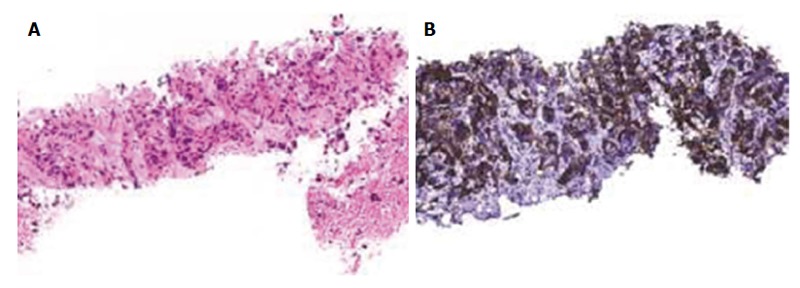
Scirrhous hepatocellular carcinoma. A: Cords and thin trabeculae of neoplastic hepatocytes are embedded in dense, abundant fibrous stroma (hematoxylin and eosin stain, × 20); B: By immunohistochemistry, strong glypican-3 positivity is present in tumor cells (anti-glypican-3/3,3’-diaminobenzidine, × 20).
HSP70
HSP70 is an anti-apoptotic regulator promoting cell survival and has been implicated in tumorigenesis. HSP70 expression increases stepwise as a lesion progresses from precancerous to advanced HCC[31]. Immunohistochemistry marks HCC, but not dysplastic nodules or HCA[14,23]. Staining is nucleocytoplasmic and may be focal or diffuse, and is 74% sensitive and 98% specific for HCC on resection specimens, and 48% and 94% on biopsy specimens, respectively when evaluating HCC vs dysplastic nodule[22,23]. However, a potential pitfall of HSP70 is that it reacts commonly with metastatic adenocarcinomas and cholangiocarcinomas[14]. Therefore, the utility is restricted to tumors which are clearly hepatocytic in differentiation.
GS
GS catalyzes the conversion of glutamate and ammonia to glutamine in the liver[32]. As noted in the discussion of b-HCA, GS is a target of β-catenin, and is upregulated when this pathway is constitutively activated. In normal liver, GS expression is restricted to perivenular hepatocytes. In neoplasms GS expression should be strong, homogenous, and diffuse (not map-like), and should stain > 50% of the cells in question. Given these conditions, on resection specimens, the sensitivity and specificity were 70% and 94%, respectively (59% and 98% on biopsy specimens) when the consideration was HCC vs dysplastic nodule[22,23]. GS is frequently positive in HCA, however, and therefore not useful in the distinction of HCA from HCC[14]. An important caveat when using these 3 markers is that GS and HSP70 are frequently positive in cholangiocarcinoma and metastases, thus highlighting that the utility of this panel is restricted to the specific contexts in which evidence supports their use. GPC-3 is the only one of the three markers above which is useful in overtly malignant tumors requiring evaluation of differentiation.
ESTABLISHING HEPATOCELLULAR ORIGIN
Since poorly differentiated HCC may have histologic overlap with poorly differentiated metastatic tumors and intra-hepatic cholangiocarcinomas, there has always been interest in reliable immunohistochemical markers of hepatocytic differentiation. At a basic level, the cytokeratin profile can be helpful but in most cases of ambiguous morphology, not definitive. Hepatocytes are generally positive for CK8 and 18 and negative for both CK7 and CK20, although HCC may acquire CK7 and or CK20 positivity in some cases[33]. One caveat is fibrolamellar carcinoma, which tends to be found in younger patients without cirrhosis, and has been found to be positive for CK7[34] (as well as CD68[35]). Some HCCs may acquire biliary features (CK19 positivity) by immunohistochemistry; in one study, these patients had a higher recurrence rate of HCC after transplantation, indicating a worse prognosis in these lesions[33]. Therefore, it is often necessary to go beyond cytokeratin analysis.
MARKERS OF PRIMARY HCC
Traditionally, the most commonly used markers for this purpose include hepatocyte paraffin 1 (HepPar-1), alpha-fetoprotein (AFP), CD10, and polyclonal carcinoembryonic antigen (p-CEA)[36-39]. Each marker has drawbacks including limitations of sensitivity and specificity, as well as the requirement of a canalicular staining pattern for hepatocellular specificity in CD10 and p-CEA.
HepPar-1
HepPar-1 is an antibody to carbamoyl phosphate synthetase 1, a urea cycle enzyme in hepatocellular mitochondria, which is expressed predominantly in the liver, but also in other organs such as small intestine[40]. Developed in 1993 from a failed liver allograft[36], this antibody has been found to be relatively sensitive (70%, although some authors report higher sensitivity) and specific (84%) for hepatocellular differentiation[41], in both normal tissue and HCC, as well as hepatoblastoma. Caveats with this marker include the reported loss of sensitivity as tumors become less differentiated[36,42,43], and frequent negativity in the scirrhous variant[44]. Through many years of use, many of the pitfalls of HepPar-1 have been elucidated. For one, it marks hepatoid tumors of any organ[45-47]. Furthermore, because of the expression of carbamoyl phosphate synthetase in small bowel, it marks many small intestinal adenocarcinomas, as well as adenocarcinomas of the ampulla with intestinal morphology[48]. Additionally, a large study by Lugli et al[47] suggested that other tumors (notably gastric, lung, small intestinal, colonic, and pancreatic adenocarcinomas, cholangiocarcinoma, and melanoma) may have low (generally less than 15%) rates of positive staining with HepPar-1. Ovarian and neuroendocrine carcinoma have also been reported to show occasional positivity[42]. However, staining in non-hepatocellular tissues has generally been reported as weak, whereas staining in tissues of hepatocellular origin tends to be strong and cytoplasmic. Thus, despite these many well-established pitfalls, HepPar-1 remains a very useful marker.
AFP
AFP is an oncofetal glycoprotein that has been used as a tumor marker both in serum and in tissue by immunohistochemistry for some time. Although also positive in yolk sac tumors, specificity by immunohistochemistry is high (97%) with very few metastatic adenocarcinomas or cholangiocarcinomas showing positive staining. However, sensitivity is low, around 30%[17], limiting its utility.
p-CEA
In normal liver, p-CEA stains a biliary glycoprotein similar to CEA (a fetal glycoprotein), present in the bile canaliculi and ductal epithelium. The staining pattern is characteristic: a delicate branching canalicular pattern, which has been reported as 70% sensitive and 100% specific for hepatocellular differentiation[43]. However, this pattern may be lost as HCC dedifferentiates, and in general, the staining pattern may be difficult to distinguish from non-specific membranous or cytoplasmic staining, which can be seen in some HCC, bile duct epithelium, and metastatic adenocarcinoma and cholangiocarcinoma[42,43,49].
CD10
CD10 is a membrane metallo-endopeptidase which cleaves the amino group of hydrophobic residues, and is expressed in multiple tissues. Although cytoplasmic, membranous, and apical staining may be seen in adenocarcinomas from multiple other primary sites, the same canalicular pattern described above for p-CEA when seen with anti-CD10 is specific for both normal and neoplastic liver, with a reported sensitivity of 68% and specificity of 100%[39]. As above, however, canalicular staining may be difficult to establish. Recently, additional markers have been described.
GPC-3
As mentioned previously, some investigators have reported a higher GPC-3 sensitivity in poorly differentiated HCC than in well differentiated tumors[26]. This could be an important finding, as HepPar-1 expression becomes less sensitive in poorly differentiated lesions. The reported overall sensitivity of GPC-3 for HCC is 75% (39% for well-differentiated, 89% for poorly differentiated)[50] and the specificity is 86%. GPC-3 staining has been reported in extragonadal germ cell tumors, melanoma, ovarian carcinoma, and squamous cell cancer of the lung[25], and more recently, in pancreatic acinar cell carcinoma, esophageal squamous cell carcinoma and adenocarcinoma[50]. Still, most of these are rare in the liver, and so GPC-3 is now commonly used as part of the immunohistochemical panel used to establish the histogenesis of a tumor in liver.
Arginase-1
Another novel marker of hepatocellular differentiation is Arginase-1 (ARG-1). ARG-1 is a manganese urea cycle metalloenzyme isoform expressed primarily in the liver. In two series[41,51], it was been found to be more sensitive and specific (84% and 96%, respectively[41]) than HepPar-1. As with many other markers of hepatocellular differentiation, expression decreased as tumor grade increased, but ARG-1 was more sensitive grade for grade than HepPar-1 in both series. In terms of specificity, ARG-1 expression has been reported in a small subset of pancreatic, colon, gastric, and pulmonary cancers, but when HepPar-1 was also positive, specificity rose to 100%. ARG-1 does not stain non-neoplastic small intestinal and ampullary mucosa, and only rarely stains adenocarcinomas of these sites[48].
Bile salt export pump
Bile salt export pump (BSEP) is another recently described immunohistochemical marker for hepatocellular differentiation[52,53]. BSEP is a membrane-bound ATP-binding cassette transporter expressed only in hepatocytes, and functions to transport bile out of the hepatocyte. A study by Lagana et al[53] reported 90% sensitivity and 100% specificity for HCC. Furthermore, since it is expressed exclusively in hepatocytes, there is no requirement for a canalicular pattern of staining as there is with CD10 and p-CEA (though canalicular staining was present in 33 of 43 positive cases).
Cholangiocarcinoma
Intrahepatic cholangiocarcinoma is generally unlikely to be histologically confused with HCC. The morphology can, however, be identical to metastatic carcinomas. In the rare cases where a pathologist is entertaining the diagnosis of HCC and cholangiocarcinoma, the markers listed above, along with the addition of CK7 and CK19, should suffice.
CONCLUSION
Diagnosing liver tumors can be challenging, especially on needle biopsy specimens which may only minimally sample a lesion. Proper identification and classification is essential, as some lesions require no treatment at all, whereas in others, resection, chemotherapy, and transplantation may be offered. Recent advances in immunohistochemistry have furthered our ability to accurately characterize these lesions (summarized in Table 1).
Table 1.
Immunohistochemical stains in liver tumors
| Marker | Staining pattern | Expected staining | Advantages | Disadvantages |
| LFABP | Cytoplasmic/nuclear | Normal: Diffuse | Can subclassify HCA | |
| H-HCA: Negative | ||||
| SAA | Cytoplasmic | Normal: Negative | Can subclassify HCA | |
| IHCA: Strong | ||||
| GS | Cytoplasmic | Normal: Perivenular | Can subclassify HCA | Not specific for β-HCA (other HCA sub-types can stain) |
| FNH: Map-like | HCA and HCC have similar staining patterns | |||
| β-HCA/HCC: Diffuse | Metastatic adenocarcinoma in liver usually positive | |||
| HSP70 | Cytoplasmic/nuclear | Normal, HCA, H-DN: Negative | Suggestive of malignancy | Staining may be focal |
| HCC: Positive | Metastatic adenocarcinoma frequently positive | |||
| GPC-3 | Cytoplasmic/membranous | Normal: Negative | More sensitive in poorly differentiated tumors | Low sensitivity in well-differentiated tumors |
| HCC: Positive | Marks scirrhous HCC | May not react with fibrolamellar HCC | ||
| Only single marker which supports both hepatocellular differentiation and malignancy | ||||
| CD34 | Cytoplasmic/membranous | Normal: Portal vessels, rare sinusoids | Can help demarcate extent of lesion | No specific cutoff for increased staining |
| HCC: Diffuse capillarization | ||||
| AFP | Cytoplasmic | Normal: Negative | High specificity for HCC | Low sensitivity |
| HCC: Positive | ||||
| p-CEA | Canalicular | Normal: Canalicular | High sensitivity and specificity for | May be difficult to interpret, since only |
| HCC: Canalicular | hepatocytes when definite canalicular | canalicular pattern is specific for hepatocytes | ||
| Metastatic ca: Any pattern other than canalicular | pattern present | |||
| CD10 | Canalicular | Normal: Canalicular | High sensitivity and specificity for | May be difficult to interpret, since |
| HCC: Canalicular | hepatocytes when definite canalicular | only canalicular pattern is specific for hepatocytes | ||
| Metastatic ca: Any pattern other than canalicular | pattern present | |||
| HepPar-1 | Cytoplasmic | Liver only | Marks cells of liver origin, both normal and neoplastic | Mediocre specificity, including any hepatoid lesion |
| Less sensitive in poorly differentiated tumors | ||||
| ARG-1 | Cytoplasmic/nuclear | Liver only | More sensitive and specific than HepPar-1 | Less sensitive in poorly differentiated tumors |
| BSEP | Usually, but not exclusively canalicular | Normal, HCC: Canalicular (usually) with | High sensitivity and specificity for hepatocytes | New marker, pitfalls and disadvantages |
| occasional dot-like or incomplete membranous pattern | Easier to interpret than other p-CEA and CD10 | currently unknown |
HCC: Hepatocellular carcinoma; HCA: Hepatocellular adenoma; H-DN: High-grade dysplastic nodules; p-CEA: Polyclonal carcinoembryonic antigen; H-HCA: HNF1α-inactivated HCA; LFABP: Liver fatty acid binding protein; GS: Glutamine synthetase; FNH: Focal nodular hyperplasia; SAA: Serum amyloid A; IHCA: Inflammatory HCA; GPC-3: Glypican-3; HSP70: Heat shock protein 70; HepPar-1: Hepatocyte paraffin 1; AFP: Alpha-fetoprotein; BSEP: Bile salt export pump; ARG-1: Arginase-1.
Footnotes
P- Reviewer: Ma L S- Editor: Song XX L- Editor: A E- Editor: Liu SQ
Conflict-of-interest: The authors report no competing financial interests.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: October 28, 2014
First decision: December 17, 2014
Article in press: March 5, 2015
References
- 1.El-Serag HB. Hepatocellular carcinoma. N Engl J Med. 2011;365:1118–1127. doi: 10.1056/NEJMra1001683. [DOI] [PubMed] [Google Scholar]
- 2.Rebouissou S, Bioulac-Sage P, Zucman-Rossi J. Molecular pathogenesis of focal nodular hyperplasia and hepatocellular adenoma. J Hepatol. 2008;48:163–170. doi: 10.1016/j.jhep.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 3.Wanless IR, Mawdsley C, Adams R. On the pathogenesis of focal nodular hyperplasia of the liver. Hepatology. 1985;5:1194–1200. doi: 10.1002/hep.1840050622. [DOI] [PubMed] [Google Scholar]
- 4.Nguyen BN, Fléjou JF, Terris B, Belghiti J, Degott C. Focal nodular hyperplasia of the liver: a comprehensive pathologic study of 305 lesions and recognition of new histologic forms. Am J Surg Pathol. 1999;23:1441–1454. doi: 10.1097/00000478-199912000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Bioulac-Sage P, Laumonier H, Rullier A, Cubel G, Laurent C, Zucman-Rossi J, Balabaud C. Over-expression of glutamine synthetase in focal nodular hyperplasia: a novel easy diagnostic tool in surgical pathology. Liver Int. 2009;29:459–465. doi: 10.1111/j.1478-3231.2008.01849.x. [DOI] [PubMed] [Google Scholar]
- 6.Balabaud C, Al-Rabih WR, Chen PJ, Evason K, Ferrell L, Hernandez-Prera JC, Huang SF, Longerich T, Park YN, Quaglia A, et al. Focal Nodular Hyperplasia and Hepatocellular Adenoma around the World Viewed through the Scope of the Immunopathological Classification. Int J Hepatol. 2013;2013:268625. doi: 10.1155/2013/268625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sempoux C, Chang C, Gouw A, Chiche L, Zucman-Rossi J, Balabaud C, Bioulac-Sage P. Benign hepatocellular nodules: what have we learned using the patho-molecular classification. Clin Res Hepatol Gastroenterol. 2013;37:322–327. doi: 10.1016/j.clinre.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 8.Bioulac-Sage P, Rebouissou S, Thomas C, Blanc JF, Saric J, Sa Cunha A, Rullier A, Cubel G, Couchy G, Imbeaud S, et al. Hepatocellular adenoma subtype classification using molecular markers and immunohistochemistry. Hepatology. 2007;46:740–748. doi: 10.1002/hep.21743. [DOI] [PubMed] [Google Scholar]
- 9.Nault JC, Zucman Rossi J. Molecular classification of hepatocellular adenomas. Int J Hepatol. 2013;2013:315947. doi: 10.1155/2013/315947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pilati C, Letouzé E, Nault JC, Imbeaud S, Boulai A, Calderaro J, Poussin K, Franconi A, Couchy G, Morcrette G, et al. Genomic profiling of hepatocellular adenomas reveals recurrent FRK-activating mutations and the mechanisms of malignant transformation. Cancer Cell. 2014;25:428–441. doi: 10.1016/j.ccr.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 11.Bioulac-Sage P, Rebouissou S, Sa Cunha A, Jeannot E, Lepreux S, Blanc JF, Blanché H, Le Bail B, Saric J, Laurent-Puig P, et al. Clinical, morphologic, and molecular features defining so-called telangiectatic focal nodular hyperplasias of the liver. Gastroenterology. 2005;128:1211–1218. doi: 10.1053/j.gastro.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 12.Stoot JH, Coelen RJ, De Jong MC, Dejong CH. Malignant transformation of hepatocellular adenomas into hepatocellular carcinomas: a systematic review including more than 1600 adenoma cases. HPB (Oxford) 2010;12:509–522. doi: 10.1111/j.1477-2574.2010.00222.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nault JC, Zucman-Rossi J. Genetics of hepatobiliary carcinogenesis. Semin Liver Dis. 2011;31:173–187. doi: 10.1055/s-0031-1276646. [DOI] [PubMed] [Google Scholar]
- 14.Lagana SM, Salomao M, Bao F, Moreira RK, Lefkowitch JH, Remotti HE. Utility of an immunohistochemical panel consisting of glypican-3, heat-shock protein-70, and glutamine synthetase in the distinction of low-grade hepatocellular carcinoma from hepatocellular adenoma. Appl Immunohistochem Mol Morphol. 2013;21:170–176. doi: 10.1097/PAI.0b013e31825d527f. [DOI] [PubMed] [Google Scholar]
- 15.Roskams T, Kojiro M. Pathology of early hepatocellular carcinoma: conventional and molecular diagnosis. Semin Liver Dis. 2010;30:17–25. doi: 10.1055/s-0030-1247129. [DOI] [PubMed] [Google Scholar]
- 16.El-Serag HB, Kanwal F. Epidemiology of hepatocellular carcinoma in the United States: where are we? Where do we go? Hepatology. 2014;60:1767–1775. doi: 10.1002/hep.27222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.International Consensus Group for Hepatocellular NeoplasiaThe International Consensus Group for Hepatocellular Neoplasia. Pathologic diagnosis of early hepatocellular carcinoma: a report of the international consensus group for hepatocellular neoplasia. Hepatology. 2009;49:658–664. doi: 10.1002/hep.22709. [DOI] [PubMed] [Google Scholar]
- 18.Roncalli M, Borzio M, Di Tommaso L. Hepatocellular dysplastic nodules. Hepatol Res. 2007;37 Suppl 2:S125–S134. doi: 10.1111/j.1872-034X.2007.00175.x. [DOI] [PubMed] [Google Scholar]
- 19.Park YN, Yang CP, Fernandez GJ, Cubukcu O, Thung SN, Theise ND. Neoangiogenesis and sinusoidal “capillarization” in dysplastic nodules of the liver. Am J Surg Pathol. 1998;22:656–662. doi: 10.1097/00000478-199806000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Coston WM, Loera S, Lau SK, Ishizawa S, Jiang Z, Wu CL, Yen Y, Weiss LM, Chu PG. Distinction of hepatocellular carcinoma from benign hepatic mimickers using Glypican-3 and CD34 immunohistochemistry. Am J Surg Pathol. 2008;32:433–444. doi: 10.1097/PAS.0b013e318158142f. [DOI] [PubMed] [Google Scholar]
- 21.Roncalli M, Roz E, Coggi G, Di Rocco MG, Bossi P, Minola E, Gambacorta M, Borzio M. The vascular profile of regenerative and dysplastic nodules of the cirrhotic liver: implications for diagnosis and classification. Hepatology. 1999;30:1174–1178. doi: 10.1002/hep.510300507. [DOI] [PubMed] [Google Scholar]
- 22.Di Tommaso L, Franchi G, Park YN, Fiamengo B, Destro A, Morenghi E, Montorsi M, Torzilli G, Tommasini M, Terracciano L, et al. Diagnostic value of HSP70, glypican 3, and glutamine synthetase in hepatocellular nodules in cirrhosis. Hepatology. 2007;45:725–734. doi: 10.1002/hep.21531. [DOI] [PubMed] [Google Scholar]
- 23.Di Tommaso L, Destro A, Seok JY, Balladore E, Terracciano L, Sangiovanni A, Iavarone M, Colombo M, Jang JJ, Yu E, et al. The application of markers (HSP70 GPC3 and GS) in liver biopsies is useful for detection of hepatocellular carcinoma. J Hepatol. 2009;50:746–754. doi: 10.1016/j.jhep.2008.11.014. [DOI] [PubMed] [Google Scholar]
- 24.Libbrecht L, Severi T, Cassiman D, Vander Borght S, Pirenne J, Nevens F, Verslype C, van Pelt J, Roskams T. Glypican-3 expression distinguishes small hepatocellular carcinomas from cirrhosis, dysplastic nodules, and focal nodular hyperplasia-like nodules. Am J Surg Pathol. 2006;30:1405–1411. doi: 10.1097/01.pas.0000213323.97294.9a. [DOI] [PubMed] [Google Scholar]
- 25.Chan ES, Yeh MM. The use of immunohistochemistry in liver tumors. Clin Liver Dis. 2010;14:687–703. doi: 10.1016/j.cld.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 26.Shirakawa H, Suzuki H, Shimomura M, Kojima M, Gotohda N, Takahashi S, Nakagohri T, Konishi M, Kobayashi N, Kinoshita T, et al. Glypican-3 expression is correlated with poor prognosis in hepatocellular carcinoma. Cancer Sci. 2009;100:1403–1407. doi: 10.1111/j.1349-7006.2009.01206.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yamauchi N, Watanabe A, Hishinuma M, Ohashi K, Midorikawa Y, Morishita Y, Niki T, Shibahara J, Mori M, Makuuchi M, et al. The glypican 3 oncofetal protein is a promising diagnostic marker for hepatocellular carcinoma. Mod Pathol. 2005;18:1591–1598. doi: 10.1038/modpathol.3800436. [DOI] [PubMed] [Google Scholar]
- 28.Shafizadeh N, Ferrell LD, Kakar S. Utility and limitations of glypican-3 expression for the diagnosis of hepatocellular carcinoma at both ends of the differentiation spectrum. Mod Pathol. 2008;21:1011–1018. doi: 10.1038/modpathol.2008.85. [DOI] [PubMed] [Google Scholar]
- 29.Maeda D, Ota S, Takazawa Y, Aburatani H, Nakagawa S, Yano T, Taketani Y, Kodama T, Fukayama M. Glypican-3 expression in clear cell adenocarcinoma of the ovary. Mod Pathol. 2009;22:824–832. doi: 10.1038/modpathol.2009.40. [DOI] [PubMed] [Google Scholar]
- 30.Abdul-Al HM, Makhlouf HR, Wang G, Goodman ZD. Glypican-3 expression in benign liver tissue with active hepatitis C: implications for the diagnosis of hepatocellular carcinoma. Hum Pathol. 2008;39:209–212. doi: 10.1016/j.humpath.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 31.Chuma M, Sakamoto M, Yamazaki K, Ohta T, Ohki M, Asaka M, Hirohashi S. Expression profiling in multistage hepatocarcinogenesis: identification of HSP70 as a molecular marker of early hepatocellular carcinoma. Hepatology. 2003;37:198–207. doi: 10.1053/jhep.2003.50022. [DOI] [PubMed] [Google Scholar]
- 32.Reitzer LJ, Wice BM, Kennell D. Evidence that glutamine, not sugar, is the major energy source for cultured HeLa cells. J Biol Chem. 1979;254:2669–2676. [PubMed] [Google Scholar]
- 33.Durnez A, Verslype C, Nevens F, Fevery J, Aerts R, Pirenne J, Lesaffre E, Libbrecht L, Desmet V, Roskams T. The clinicopathological and prognostic relevance of cytokeratin 7 and 19 expression in hepatocellular carcinoma. A possible progenitor cell origin. Histopathology. 2006;49:138–151. doi: 10.1111/j.1365-2559.2006.02468.x. [DOI] [PubMed] [Google Scholar]
- 34.Ward SC, Huang J, Tickoo SK, Thung SN, Ladanyi M, Klimstra DS. Fibrolamellar carcinoma of the liver exhibits immunohistochemical evidence of both hepatocyte and bile duct differentiation. Mod Pathol. 2010;23:1180–1190. doi: 10.1038/modpathol.2010.105. [DOI] [PubMed] [Google Scholar]
- 35.Ross HM, Daniel HD, Vivekanandan P, Kannangai R, Yeh MM, Wu TT, Makhlouf HR, Torbenson M. Fibrolamellar carcinomas are positive for CD68. Mod Pathol. 2011;24:390–395. doi: 10.1038/modpathol.2010.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wennerberg AE, Nalesnik MA, Coleman WB. Hepatocyte paraffin 1: a monoclonal antibody that reacts with hepatocytes and can be used for differential diagnosis of hepatic tumors. Am J Pathol. 1993;143:1050–1054. [PMC free article] [PubMed] [Google Scholar]
- 37.Carrozza MJ, Calafati SA, Edmonds PR. Immunocytochemical localization of polyclonal carcinoembryonic antigen in hepatocellular carcinomas. Acta Cytol. 1991;35:221–224. [PubMed] [Google Scholar]
- 38.Tsuji M, Kashihara T, Terada N, Mori H. An immunohistochemical study of hepatic atypical adenomatous hyperplasia, hepatocellular carcinoma, and cholangiocarcinoma with alpha-fetoprotein, carcinoembryonic antigen, CA19-9, epithelial membrane antigen, and cytokeratins 18 and 19. Pathol Int. 1999;49:310–317. doi: 10.1046/j.1440-1827.1999.00865.x. [DOI] [PubMed] [Google Scholar]
- 39.Borscheri N, Roessner A, Röcken C. Canalicular immunostaining of neprilysin (CD10) as a diagnostic marker for hepatocellular carcinomas. Am J Surg Pathol. 2001;25:1297–1303. doi: 10.1097/00000478-200110000-00011. [DOI] [PubMed] [Google Scholar]
- 40.Butler SL, Dong H, Cardona D, Jia M, Zheng R, Zhu H, Crawford JM, Liu C. The antigen for Hep Par 1 antibody is the urea cycle enzyme carbamoyl phosphate synthetase 1. Lab Invest. 2008;88:78–88. doi: 10.1038/labinvest.3700699. [DOI] [PubMed] [Google Scholar]
- 41.Radwan NA, Ahmed NS. The diagnostic value of arginase-1 immunostaining in differentiating hepatocellular carcinoma from metastatic carcinoma and cholangiocarcinoma as compared to HepPar-1. Diagn Pathol. 2012;7:149. doi: 10.1186/1746-1596-7-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chu PG, Ishizawa S, Wu E, Weiss LM. Hepatocyte antigen as a marker of hepatocellular carcinoma: an immunohistochemical comparison to carcinoembryonic antigen, CD10, and alpha-fetoprotein. Am J Surg Pathol. 2002;26:978–988. doi: 10.1097/00000478-200208000-00002. [DOI] [PubMed] [Google Scholar]
- 43.Lau SK, Prakash S, Geller SA, Alsabeh R. Comparative immunohistochemical profile of hepatocellular carcinoma, cholangiocarcinoma, and metastatic adenocarcinoma. Hum Pathol. 2002;33:1175–1181. doi: 10.1053/hupa.2002.130104. [DOI] [PubMed] [Google Scholar]
- 44.Krings G, Ramachandran R, Jain D, Wu TT, Yeh MM, Torbenson M, Kakar S. Immunohistochemical pitfalls and the importance of glypican 3 and arginase in the diagnosis of scirrhous hepatocellular carcinoma. Mod Pathol. 2013;26:782–791. doi: 10.1038/modpathol.2012.243. [DOI] [PubMed] [Google Scholar]
- 45.Maitra A, Murakata LA, Albores-Saavedra J. Immunoreactivity for hepatocyte paraffin 1 antibody in hepatoid adenocarcinomas of the gastrointestinal tract. Am J Clin Pathol. 2001;115:689–694. doi: 10.1309/5C2C-FP3H-GE7Q-2XJ5. [DOI] [PubMed] [Google Scholar]
- 46.Fan Z, van de Rijn M, Montgomery K, Rouse RV. Hep par 1 antibody stain for the differential diagnosis of hepatocellular carcinoma: 676 tumors tested using tissue microarrays and conventional tissue sections. Mod Pathol. 2003;16:137–144. doi: 10.1097/01.MP.0000052103.13730.20. [DOI] [PubMed] [Google Scholar]
- 47.Lugli A, Tornillo L, Mirlacher M, Bundi M, Sauter G, Terracciano LM. Hepatocyte paraffin 1 expression in human normal and neoplastic tissues: tissue microarray analysis on 3,940 tissue samples. Am J Clin Pathol. 2004;122:721–727. doi: 10.1309/KC09-YTF2-M4DL-UYQ6. [DOI] [PubMed] [Google Scholar]
- 48.ESP Abstracts 2013. Virchows Arch. 2013;463:101–352. doi: 10.1007/s00428-013-1444-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wee A. Diagnostic utility of immunohistochemistry in hepatocellular carcinoma, its variants and their mimics. Appl Immunohistochem Mol Morphol. 2006;14:266–272. doi: 10.1097/00129039-200609000-00003. [DOI] [PubMed] [Google Scholar]
- 50.Mounajjed T, Zhang L, Wu TT. Glypican-3 expression in gastrointestinal and pancreatic epithelial neoplasms. Hum Pathol. 2013;44:542–550. doi: 10.1016/j.humpath.2012.06.016. [DOI] [PubMed] [Google Scholar]
- 51.Yan BC, Gong C, Song J, Krausz T, Tretiakova M, Hyjek E, Al-Ahmadie H, Alves V, Xiao SY, Anders RA, et al. Arginase-1: a new immunohistochemical marker of hepatocytes and hepatocellular neoplasms. Am J Surg Pathol. 2010;34:1147–1154. doi: 10.1097/PAS.0b013e3181e5dffa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Knisely A. Hepatocellular carcinoma, renal cell carcinoma metastatic to liver, and adrenal carcinoma metastatic to liver: immunostaining for bile salt export pump as a marker of hepatocellular differentiation. United States and Canadian Academy of Pathology 98th Annual Meeting Abstracts; March 7-13, 2009; Boston, Masachusetts. Laboratory Investigation. 2009;89 Supp 1s:312A–313A. [Google Scholar]
- 53.Lagana SM, Salomao M, Remotti HE, Knisely AS, Moreira RK. Bile salt export pump: a sensitive and specific immunohistochemical marker of hepatocellular carcinoma. Histopathology. 2015;66:598–602. doi: 10.1111/his.12601. [DOI] [PubMed] [Google Scholar]


