Abstract
The intracellular protozoa Leishmania spp. and Trypanosoma cruzi and the causative agents of Leishmaniasis and Chagas disease, respectively, belong to the Trypanosomatidae family. Together, these two neglected tropical diseases affect approximately 25 million people worldwide. Whether the host can control the infection or develops disease depends on the complex interaction between parasite and host. Parasite surface and secreted molecules are involved in triggering specific signaling pathways essential for parasite entry and intracellular survival. The recognition of the parasite antigens by host immune cells generates a specific immune response. Leishmania spp. and T. cruzi have a multifaceted repertoire of strategies to evade or subvert the immune system by interfering with a range of signal transduction pathways in host cells, which causes the inhibition of the protective response and contributes to their persistence in the host. The current therapeutic strategies in leishmaniasis and trypanosomiasis are very limited. Efficacy is variable, toxicity is high, and the emergence of resistance is increasingly common. In this review, we discuss the molecular basis of the host-parasite interaction of Leishmania and Trypanosoma cruzi infection and their mechanisms of subverting the immune response and how this knowledge can be used as a tool for the development of new drugs.
1. Host-Parasite Interaction
Parasitic diseases are some of the greatest public health problems in developing countries. Several of these diseases are neglected, either because of their incidence in countries with little purchasing power or their low visibility. In general, the majority of these countries are located in the tropical zone. The climates of these areas contribute to the development of parasitic infections because humidity and high temperatures provide the necessary conditions for vector and protozoan growth [1].
All mammalian hosts are at risk of infection by viruses, bacteria, fungi, and parasites. The host-parasite relationship is the most important factor in determining whether an infection is successful or is resolved by the host. Several mechanisms are involved in this complex interaction, and aspects of both the host and the parasite are essential. Some parasites have evolved evasive mechanisms, such as intracellular infection, as in the case of the genus Leishmania and Trypanosoma cruzi, protozoa parasites belonging to family Trypanosomatid, order Kinetoplastida. These parasites are among the most important agents of neglected tropical diseases [2]. They are heteroxenic and infect two host types: vertebrates and invertebrates [3, 4]. Throughout their life cycle, they progress through several forms, including epimastigotes and metacyclic trypomastigotes, which are found inside the Triatominae vector of T. cruzi and procyclic and metacyclic promastigotes, which are found inside the Phlebotominae vector of Leishmania genus [3, 4]. Amastigotes are the intracellular form of the both parasites and are found inside the vertebrate host. Additionally, T. cruzi presents the blood trypomastigote forms in this host [3, 4].
Leishmania is responsible for a group of cutaneous and visceral infections known as leishmaniasis. These parasitoses are endemic in 98 countries distributed in Latin America, South and Central Asia and sub-Saharan Africa [5], where approximately 350 million people are threatened with contracting this infection. The annual incidence is estimated at 1.6 million, and the prevalence is 12 million [6].
Trypanosoma cruzi causes Chagas disease. An estimated 10 million people are infected by T. cruzi, mostly in Latin America, where Chagas disease is endemic, and more than 25 million people are danger of contracting this parasitosis [6].
The first step in the interaction between the host and these intracellular protozoa parasites is the binding of the parasite to the host cell. These protozoa have a variety of surface and secreted molecules used to attach and enter mammalian cells. Several of these molecules are involved in triggering specific signalling pathways essential for parasite entry and intracellular survival. Scientific advances in this area have identified factors critical to parasite virulence and the disease pathogenesis.
2. Molecular Basis of Trypanosomatid-Host Cell Interaction
Metacyclogenesis is an important process for parasite virulence. This mechanism allows trypanosomatids to infect their vertebrate host and thus their host cells [7]. Inside the vector gut, Leishmania parasites transform from procyclic promastigotes to metacyclic promastigotes during metacyclogenesis [7], whereas T. cruzi transitions from epimastigotes to metacyclic trypomastigotes [8].
For a long time, Leishmania spp. was believed to be obligatory intracellular pathogens of macrophages. However, recent studies have shown that these protozoa infect a large range of host cells [9–11]. Various groups have shown that these parasites can infect multiple cell types in vitro as well as in vivo, from haematopoietic cells that arise from a common myeloid precursor to nonhaematopoietic cells, such as fibroblasts [10].
Early in infection, neutrophils are recruited in response to a bite from the insect vector due to the release of the alarmins (signal for tissue damage), cytokines, and chemokines [10, 12]. These cells can act against the intracellular microorganisms through reactive oxygen species (ROS) [13, 14], neutrophil elastase (NE), and neutrophil extracellular traps (NETs) [15]. Nevertheless, if these mechanisms can be evaded, neutrophils may serve as host for Leishmania parasites. They are infected by promastigotes during the first 18 hours. These cells undergo apoptosis, and the apoptotic bodies are phagocytized by macrophages, triggering anti-inflammatory signal pathways. This results in the silent entry of the parasites inside macrophages, which promotes infection success [16]. It is interesting to note that neutrophils readily phagocytized promastigotes, but recognition or uptake of amastigotes has not been detected yet [17].
The initial binding and internalization of the Leishmania promastigotes is a classical receptor-mediated endocytic event that involves serum-derived factors as well as parasites and host cell molecules. The major macrophage plasma membrane structures involved in this interaction are (1) receptors for the complement component 3 subunits C3b and C3bi, which bind to CR1 and CR3, respectively; (2) Fc receptors; (3) lectin receptors, which mediate connections with carbohydrate molecules; and (4) the integrin family of molecules that recognize specific amino acid sequences. The major surface molecules of Leishmania that may also participate in this interaction include gp63 or promastigote surface protease (PSP), the primary parasite surface protein; lipophosphoglycan (LPG), the main promastigote glycoconjugate; and glycosyl inositol phospholipids (GPIs), which are present in large numbers in both promastigotes and amastigotes [18].
The parasite surface molecules responsible for the independent binding of serum are LPG, gp63, and glyco inositol phospholipids (GIPLs). In L. major, LPG is involved in the invasion of both promastigotes and amastigotes, although this molecule is absent in amastigotes of certain parasite species. Proteophosphoglycan (PPG) is particularly important in the invasion of macrophages by a number of Leishmania amastigotes [19, 20].
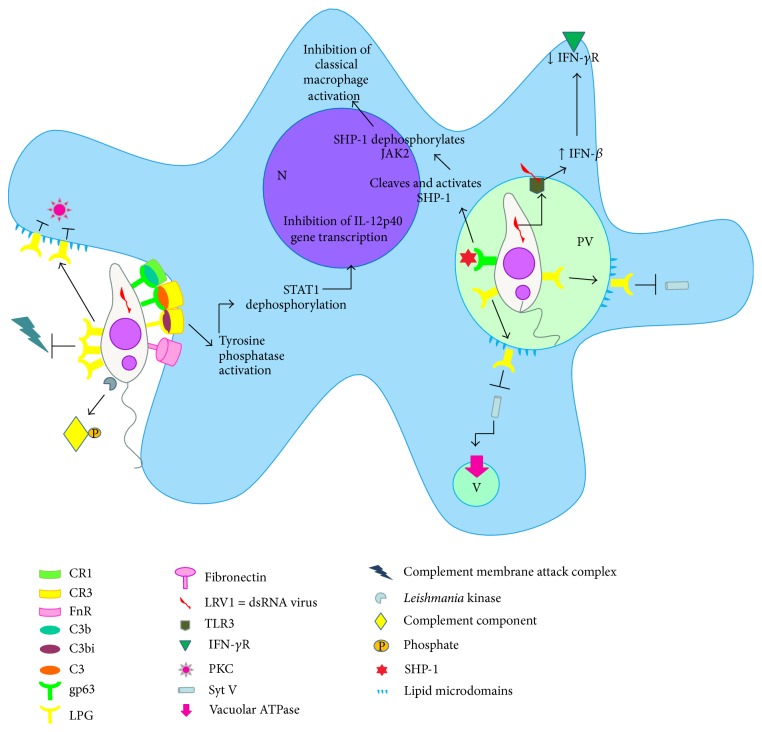
Both LPG and GIPLs are capable of binding to a mannan-binding serum protein (MBP), which is able to activate the complement system in an antibody-dependent manner. This mechanism may be particularly important in the case of amastigotes that have little or no LPG and gp63 on their surface [18]. On the other hand, gp63 and LPG act as acceptor sites for the complement component 3 (C3) and interact with CR3 and p150, 95, members of the CD18 family of integrins [21, 22]. Meantime, some studies demonstrated that internalization of promastigotes of LPG-defective Leishmania is higher than of wild-type (WT) promastigotes [23–26]. Thus, it seems unlikely that LPG plays an essential role in promastigote adhesion to macrophages, but it appears that may interfere with the process of phagocytosis. For accommodating the plasma membrane extension that occurs during the phagocytosis of large particles, as the parasites, focalized exocytosis of endomembrane occurs at the phagocytic cup [27–29]. Several intracellular compartments, including endoplasmic reticulum, late endosomes, and recycling endosomes may contribute to membrane formation of the phagosome through fusion events regulated by soluble N-ethylmaleimide sensitive factor attachment protein receptors (SNAREs), such as VAMP3, VAMP7, and syntaxin 18 [30–35]. The activity of SNARE is regulated by synaptotagmins (Syts), a family of transmembrane proteins that act as sensors of Ca2+ [36, 37]. The first Syt protein characterized in phagocytosis is the lysosomal Syt VII, which regulates Ca2+-dependent exocytosis of lysosomes [38] and directs the lysosomal membrane to the phagosome [39]. Another protein was posteriorly identified as Syt V, a recycling endosome associated protein recruited to forming phagosome and controls the phagocytic process [40]. After Leishmania-host cell contact, LPG is transferred from the parasite to the macrophage membrane during phagocytosis and seems to promote blockage of macrophage activation, protecting the parasite [41]. This insertion promotes disruption of existing lipid microdomains and alters the formation of these structures after promastigote internalization [42, 43], causing the exclusion of Syt V [44]. Consequently, LPG impairs the recruitment of Syt V to the nascent phagosome, resulting in a reduction in the phagocytic capacity of host macrophages [45]. However, the Syt V exclusion from phagosomes promoted by LPG abrogated the recruitment of the vacuolar ATPase and, consequently, their acidification [44], creating a hospitable intracellular niche for Leishmania (Figure 1). Thus, although the entry of parasites into macrophages is reduced, their higher survival is reached due to lack of the phagosome acidification and this may represent a larger gain in overall adaptation of these protozoa.
Figure 1.
Leishmania survival and host cell modulation: The LPG coating of the parasites prevents the complement membrane attack complex insertion. In addition, the promastigote kinase phosphorylates the components of the complement, inhibiting its activation. Promastigote opsonized by C3bi interacts with macrophage membrane CR3 activating tyrosine phosphatase that dephosphorylates STAT-1 leading to inhibition of transcription of the IL-12p40 gene. During the process of promastigote internalization LPG is transferred from parasite membrane to host cell membrane promoting lipid microdomain disruption inhibiting PKC activation and ROS generation (burst oxidative). Inside the parasitophorous vacuole (PV) membrane, this disruption causes the exclusion of synaptotagmins V (Syt V), abrogating the recruitment of the vacuolar ATPase and, consequently, PV acidification allowing the survival of promastigotes. The Leishmania dsRNA virus (LRV1) binds toll-like receptor 3 (TLR3) triggering strong IFN-β production and downregulation of IFNγ-R. Already gp63 cleaves SHP1 prevents classical macrophage activation by IFN-γ. N—nucleus, PV—parasitophorous vacuole and V—vacuole.
In addition to vector transmission, infection by T. cruzi can also occur through organ transplantation [46], blood transfusion [47], congenital transmission [48], oral transmission [49], or laboratory accidents [50]. The literature has suggested that host cell invasion requires the activation of signal transduction pathways that lead to an increase in cytosolic calcium concentration in both the parasite and the host cell and the recruitment and fusion of host perinuclear lysosomes to the site of invasion [51, 52]. According to Andrews [53], the trigger for host cell calcium production is the recruitment of perinuclear lysosomes to the T. cruzi invasion site. At this site, lysosomes are incorporated immediately into the parasitophorous vacuole without polymerized actin accumulation, and invasion is facilitated by disruption of microfilaments. However, the recruitment of lysosomes is not currently believed to be essential in this process but is essential for parasite persistence in the host cell. In professional phagocytes, parasite internalization occurs by conventional phagocytosis. Following the adhesion of the parasite to the host cell membrane, molecular signals are triggered, initiating this process. The invasion efficiency in nonphagocytic cells varies among the different developmental forms, that is, T. cruzi strains and phylogenetic lineages. Extracellular amastigotes, for example, are potent inducers of phagocytosis in nonprofessional phagocytes, a process that may facilitate parasite persistence in infected hosts [54].
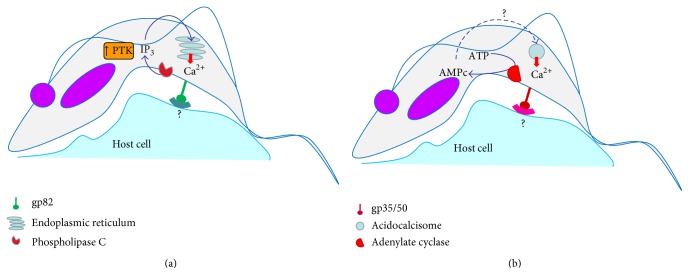
Trypomastigotes adhere to host cells using surface receptors. Surface glycoproteins such as gp82 and gp35/50, which induce calcium-mediated signaling, are utilized differently among different strains of T. cruzi. Isolates that enter the host cell in a gp82-dependent manner (T. cruzi II—endemic areas) activate a protein tyrosine kinase and a parasite phospholipase C, which releases Ca2+ from inositol-1,4,5-triphosphate (IP3) sensitive reservoirs, possibly the endoplasmic reticulum (Figure 2(a)). However, T. cruzi isolates that bind to target cells using gp35/50 (T. cruzi I—Amazon region) appear to stimulate adenylate cyclase activity that seems to participate in Ca2+ release from acidocalcisomes [55, 56] (Figure 2(b)). Metacyclic trypomastigotes trigger Ca2+ release from intracellular stores sensitive to IP3 in the host cell and induce Ca2+-dependent disorganization of actin cytoskeleton. The Ca2+ release also mobilizes perinuclear lysosomes to the site of T. cruzi invasion. Some studies report that lysosomes that fuse directly to the vacuole are already in the plasma membrane. Thus, Ca2+ would act only in the fusion and not in the recruitment in this case. Ca2+-dependent lysosomal exocytosis is regulated by cAMP and is increased by isoproterenol, a β-adrenergic agonist that activates adenylate cyclase. This mechanism appears to be used by the cell to repair cellular membrane (Figure 2) [57]. In the early 2000s, some studies suggested that Syt VII, which is located on the membrane of lysosomes and regulates exocytosis of these organelles, appears to participate in the invasion process of T. cruzi [58].
Figure 2.
Activation of different signaling pathways for host cell invasion by T. cruzi II (a) and T. cruzi I (b). (a) The ligation gp82-receptor activates a protein tyrosine kinase and a parasite phospholipase C, which releases Ca2+ from inositol-1,4,5-triphosphate (IP3) sensitive reservoirs, possibly the endoplasmic reticulum. (b) The gp35/50-receptor binding appears to stimulate adenylate cyclase activity that seems to participate in Ca2+ release from acidocalcisomes.
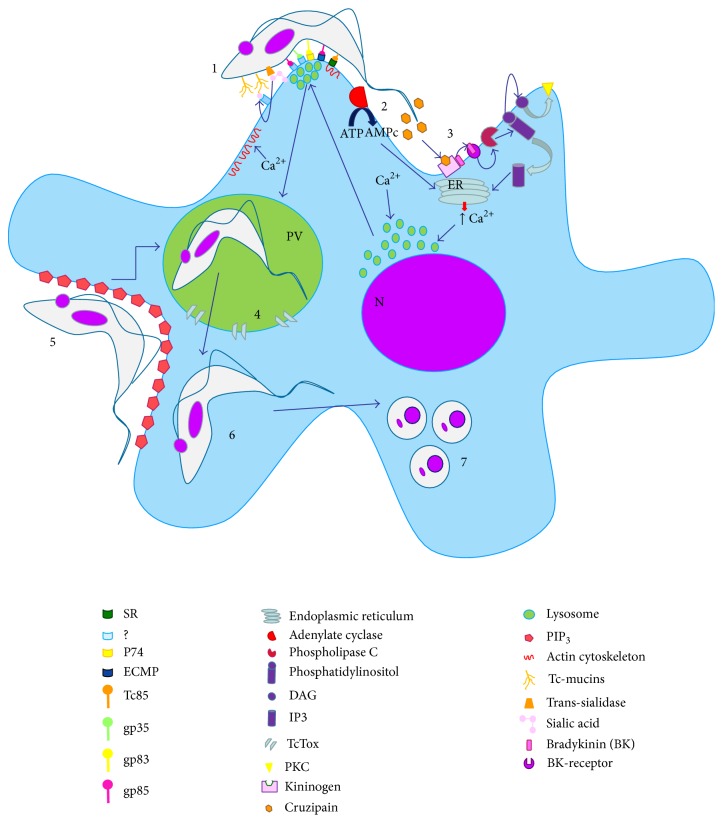
A new lysosome-independent route of host cell invasion has recently been described. In this route, the parasite enters into host cell by creating an invagination in the plasma membrane, which accumulates phosphatidylinositol-3,4,5-triphosphate (PIP3), the main product activation of phosphatidylinositol-3-kinase class I (PI3K) (Figure 2) [56]. In a quantitative analysis of the ways in which trypomastigotes of T. cruzi penetrate into the host cell, 20 to 25% of trypomastigotes were observed to enter the lysosome exocytosis- and Ca++-dependent pathway, approximately 50% invaded via the PI3K-dependent pathway and remained in a vacuole formed only by the plasma membrane for an initial period, and approximately 20% entered using the PI3K-dependent pathway and quickly associated with primary endosomes [56]. However, independently of the entry mechanism, all parasites are found in parasitophorous vacuole-associated lysosomes within 60 minutes because this fusion is essential for T. cruzi survival [59]. Unlike in many other intracellular parasites that avoid fusion with host cell lysosomes [60], this process is a prerequisite for the survival of T. cruzi [56]. If the parasite does not associate with these organelles, the persistence of parasites in the host cell is seriously compromised, and the entry process is reversed [56]. The exposure of trypomastigotes to this acidic environment is essential for the activity of the porin-like protein TcTOX; this protein is responsible for parasitophorous vacuole lysis and parasite escape into the cytoplasm, which is necessary for the differentiation of trypomastigotes into amastigotes that begins within the low vacuole pH (Figure 3) [55, 61].
Figure 3.
General molecular mechanisms for host cell invasion by Trypanosoma cruzi. (1) Several receptor-ligand complexes seem to participate in T. cruzi internalization by the host cell. The enzyme transsialidase transfers sialic acid from host cell membrane to Tc-mucins. These molecules can interact with host cell receptor. Some host cell receptors remain unknown. Glycoproteins from the parasite (gp 83 and gp 85, resp.) can bind to host cell receptors, such as P74 or EMCP. Members of Tc85 family can bind to specific receptor (SR) promoting cytoskeletal changes and facilitate parasite invasion. (2) During the process, the host cell adenylate cyclase is activated promoting an enhancement of AMPc that contributes to Ca2+ release from endoplasmic reticulum. (3) The cruzipain secreted by the parasite cleaves the host kininogen to liberate bradykinin, and the triggering of the host bradykinin receptor activates host cell PLC, contributing to Ca2+ release, via IP3. (4) Ca2+ seems to promote recruitment of perinuclear lysosomes that contributes to formation of the parasitophorous vacuole. In addition, Ca2+ promotes disorganization of actin cytoskeleton, and invasion is facilitated by disruption of microfilaments. (5) In another route, the parasite enters into host cell by creating an invagination in the plasma membrane, which accumulates PIP3. (6) After the PV formation, TcTox promotes pores in their membrane and the trypomastigotes escape for cytoplasm. (7) Trypomastigotes transform into amastigotes, multiplying inside the cytoplasm from host cell. N—nucleus, PV—parasitophorous vacuole.
Because T. cruzi is unable to synthesize sialic acid, the only mechanism for sialylation of their membrane glycoproteins is to transfer the sugar from host cell glycoconjugates through the action of enzymes. This phenomenon is important for host cell interaction and parasite internalization [62, 63]. Trypomastigotes express large amounts of a protein with transsialidase (TcTS) activity on their surface [64]. The transsialidase is bound to the parasite membrane through a glycosylphosphatidylinositol (GPI) anchor and acts to specifically catalyze the transfer of sialic acid from glycoconjugate proteins from the extracellular environment to mucin-associated surface protein (MASP) that cover the surface of the parasite (Tc-mucins) [65], which is important to promote the parasite entry and persistence in the mammalian host cells (Figure 3). These protein domains are rich in threonine residues [66, 67]. These residues can be modified by protein glycosylation, which is an important posttranslational modification for host-parasite interactions. The O-glycosylation of T. cruzi mucins (Tc-mucins) is initiated by enzymatic addition of α-O-N-acetylglucosamine (GlcNAc) to threonine (Thr) by the UDP-GlcNAc: polypeptide α-N-acetylglucosaminyltransferase (pp-α-GlcNAcT) in the Golgi [68]. These O-glycans are the acceptors of sialic acid, as already cited by the literature [69, 70]. The different evolutive forms of T. cruzi present different molecular masses of Tc-mucins. Epimastigotes and metacyclic trypomastigotes (MT) present Tc-mucins with molecular mass varying from 35 to 50 kDa, while the Tc-mucins from trypomastigotes derived from cell culture (TCT) the variation range is between 60 and 200 kDa [71, 72]. These masses are compatible with glycosylated protein containing sialic acid, which is essential for host cell binding and invasion [72]. These differences seem to contribute for differential susceptibility of MT and TCT to pepsin digestion. The mucin-like molecules that covered the MT are resistant to proteolysis and protect the parasites from lysis in the gastric milieu [73], in the meantime TCT are susceptible to peptic digestion and are mostly lysed (90%) when incubated with pepsin at pH 3.5 for 30 min [74]. In addition Tc-mucins from TCT are capable to induce NO, IL-12 and TNF-α by activated macrophages [75], modulating the immune response during T. cruzi infection.
The gene superfamily gp85/trans-sialidase (TS) encodes several glycoproteins that are present on the surface of the parasite and can participate in cell invasion. One of these glycoproteins is called gp83 and plays an important role in the interaction of T. cruzi with the host cell interacting with the p74 receptor present on the surface of the host cell and acting as a universal ligand for T. cruzi infection of both, phagocytic and non-phagocytic cells [76]. The Tc85 molecules are involved in the adhesion of parasites to the host cell by laminin and other extracellular matrix proteins (ECMP), which can be anchored to the plasma membrane (Figure 3) [77].
A synthetic peptide based on the conserved FLY domain (VTVXNVFLYNR) present in all members of the gp85/TS family promotes dephosphorylation of an intermediate filament protein (cytokeratin 18) that leads to cytoskeletal reorganization facilitating entry of the parasite [78]. This mechanism also promotes activation of the ERK1/2 signaling cascade, resulting in an increase in parasite invasion in epithelial cells [79]. However, an inactive form of TS from TCT that binds sialic acid has been shown to trigger NF-κB activation, the expression of adhesion molecules on endothelial cells and upregulation of parasite entry in an FLY-independent and carbohydrate-dependent manner [80].
The gp90 protein, an N-glycosylated protein [81] with a GPI anchor [82, 83], as well as cruzipain are also involved in host cell invasion of metacyclic trypomastigotes. Secreted cruzipain cleaves host kininogen to liberate bradykinin, and the triggering of the host bradykinin receptor activates host cell PLC, contributing to Ca2+ release (Figure 3) [81, 84]. In epimastigotes, cruzipain appears to be linked to degradation processes and localization in the endosomal-lysosomal system [85] but has been described as playing a role in adhesion [86] and cell invasion in trypomastigotes [87].
3. Immune Response against Leishmania and Trypanosoma cruzi and Their Evasion Mechanisms
The immune system recognizes and responds to a broad spectrum of pathogens, including microorganisms such as viruses, bacteria, fungi, and protozoan parasites, and multicellular parasites, such as helminthes and ectoparasites. Vertebrates possess two types of immunity: innate and adaptive. The innate immune response involves the innate lymphoid cells (ILCs), which are lymphoid cells that do not express rearranged receptors. These cells present essential effector and regulatory functions in innate immunity and tissue remodeling. Two model members of ILC family are natural killer (NK) cells and lymphoid tissue inducer (LTi) cells. The ILCs are divided into 3 groups. This classification is based on their pattern of cytokines produced and the transcription factors required for their development. Group 1 ILCs (ILC1s) produce interferon γ and depend on Tbet, group 2 ILCs (ILC2s) produce type 2 cytokines like interleukin-5 (IL-5) and IL-13 and require GATA3, and group 3 ILCs (ILC3s) include lymphoid tissue inducer (LTi) cells, produce IL-17 and/or IL-22, and are dependent on RORγt [88]. NK cells were classified into ILC1s group because they produce IFN-γ [89] and recent information about ILCs development in mouse suggests that NK cells can be considered as the innate form of TCD8 (T cytotoxic) cells as well as CD127+ILCs, the innate form of TCD4 (T helper) cells [90].
The innate response is based on the recognition of pathogen-associated molecular pattern molecules (PAMPs), which are present in diverse organisms but are absent in the host and function as an exogenous signal that alerts the host to the presence of pathogens [91]. The major PAMPs include microbial nucleic acid, lipoproteins, surface glycoproteins, and other membrane components. They are recognized by pattern recognition receptors (PPRs), such as toll-like receptors (TLRs), retinoic acid-inducible gene I- (RIG-1-) like receptors (RLRs), AIM2 like receptors (ALRs), and nucleotide-binding oligomerization domain- (NOD-) like receptors (NLRs) [92]. During infection, PAMPs are recognized by PPRs that initiate signaling cascades that lead to the activation of transcriptions factors in innate immune cells. Macrophages, dendritic cells (DCs), mast cells, and neutrophils are important cells involved in the innate immune response. Innate immune effectors mechanisms include phagocytosis, cytokine and chemokine production, and expression of costimulatory molecules on antigen present cells (APCs) and have an influence on T lymphocyte differentiation [93, 94].
The adaptive immune response involves T and B lymphocytes that recognize a large spectrum of antigens using highly specific receptors. The two major populations of T cells, TCD4 (T helper) and TCD8 (T cytotoxic) cells, have T cell receptors (TCR) that recognize antigens bound to the major histocompatibility complex (MHC) on APC (MHC class II) or target cell (MHC class I) surfaces. Antigen presenting cells such as DCs, macrophages, and B cells express MHC class II molecules and costimulatory molecules on their membranes and present antigen to naive TCD4 cells, whereas MHC class I cells can be also expressed by others cell present antigen to TCD8 cells. After an antigen is recognized, T cells proliferate and differentiate into effector T cell subsets. TCD4 cells orchestrate the immune response by the differentiation into a T helper cell population that secretes distinct sets of cytokines, providing help to B lymphocyte and TCD8 cytotoxic cells. Naive TCD4 cells differentiate into at least four T helper (Th) cell subsets: Th1, Th2, Th17, and regulatory T cells (Treg) [95]. DCs play a critical role not only in processing and presenting antigens to naive TCD4 cells but also in secreting cytokines such as IL-12 that induce Th1 effector lymphocyte differentiation. Although DCs are important in the development of Th2 response, other cells such as mast cells, basophils, natural killer cells, and monocytes, secrete cytokines like IL-4 that induce TCD4 differentiation to Th2 [96, 97]. A recent study demonstrates that lung ILC2s enhance effector functions of Th2-type CD4+ T cells when they are cultured together in vitro. The interaction between ILC2s and CD4+ T cells appears bidirectional and likely requires both OX40L and IL-4 and perhaps other molecules. These findings suggest that lung ILC2s and CD4+ T cells cooperate to mediate robust Th2-type immune responses in mice [98].
Type 1 responses are characterized by the induction of Th1 cells; these cells secrete cytokines such as interleukin-2 (IL-2) and IFN-γ, which are indispensable for host immunity to intracellular parasites (e.g., Trypanosoma cruzi). In contrast, type 2 responses are characterized by Th2 cells that secrete IL-4, IL-5, IL-9, and IL-13 and are induced by and confer immunity to extracellular parasites (e.g., helminths). IFN-γ induces cytotoxic TCD8 cell differentiation and macrophage activation, which stimulates the expression of nitric oxide (NO) synthase enzyme (iNOS or NOS2) and the production of NO, the main microbicidal agent able to destroy intracellular parasites such as Leishmania. Th2 cells promote B cell responses and immunoglobulin E (IgE) secretion through IL-4 production. In addition to antibody production, B cells have other important functions, such as presenting antigens to T cells and cytokine production. As with T cells, B cells contain functionally distinct subsets with regulatory functions, such as the production of anti-inflammatory IL-10 [99, 100]. The immune system must adjust the magnitude and duration of response because uncontrolled inflammation may lead to immune-mediated tissue injury. Treg cells are important anti-inflammatory cells that are critically involved in limiting the inflammatory response. The suppression of the immune response by Treg cells includes both cell contact- and factor-dependent mechanisms, such as cytokine production (IL-10, TGF-β, and IL-35) [101, 102].
The balance between effector and regulatory T cell responses influences the balance between infection control and pathogenesis. Comparing responses exhibited by susceptible and resistant experimental models has contributed to an understanding of protective immune responses to T. cruzi and Leishmania spp.
After transmission by sand flies, Leishmania parasites infect neutrophils, macrophages, and DCs in the vertebrate host, and the development of a protective immune response requires the coordinated action of cells of the innate and adaptive immune response. Generally, protective immunity against leishmaniasis is associated with an inflammatory Th1 response, while disease is associated with an anti-inflammatory Th2 response [103].
Six major Leishmania species (L. tropica, L. major, and L. donovani, in the Old World and L. infantum, L. braziliensis, and L. mexicana, in the New World) cause the three main forms of the disease in humans, dermal cutaneous leishmaniasis (CL), visceral leishmaniasis (VL), and muco-cutaneous leishmaniasis or mucosal leishmaniasis (MCL or ML). The form and severity of the disease depend on the Leishmania species causing the infection and the immune status of the host [104]. Some of these species have metastatic characteristics and up to 10% of CL cases progress to MCL forming destructive secondary lesions in the mucosa of nose and mouth, in South America. This clinical complication is associated with Leishmania (Viannia) subgenus, since it is promoted by species inside of this group, predominantly L. (Viannia) braziliensis but also L. (Viannia) guyanensis and L. (Viannia) panamensis [105]. A common characteristic in the cases of metastatic infection of Leishmania is the destructive hyper-inflammatory immune response, caused by numerous activated immune cells, promoting swelling and destroying local tissue [106, 107]. Thus, in ML/MCL exacerbated inflammatory immune response induces tissue injury, and patients present higher levels of proinflammatory cytokines, such as IFN-γ, and low levels of anti-inflammatory cytokines, such as IL-10, even after cure compared to the benign cutaneous clinical form of disease [108]. This exacerbated reaction generally is associated to a parasite factor. Although endosymbiont dsRNA virus already have been described on the subgenus Leishmania (Viannia) a long time ago [109–111], just recently the presence of this endosymbiont was associated with leishmanial virulence and metastasis [112, 113]. The nucleic acid of Leishmania dsRNA virus (LRV1) behaves as a strong innate immunogen, inducing a hyper-inflammatory immune response by pathway of toll-like receptor 3 (TLR3). This pathway induces production of a type 1 IFN response: IFN-β-mediated antiviral response. Type I IFNs promote downregulation of IFNγ-R on the surface of macrophages. Consequently, the macrophages become insensitive to classical activation, which promotes the reactive nitrogen species (NO) production responsible to kill intracellular pathogens (Figure 1) [114]. In this way, this mechanism is proposed as promoter of the exacerbated MCL phenotype, triggering an increase in the disease severity and parasite persistence [115].
The dsRNA virus seems to interfere with NO production for another via: metastatic L. braziliensis species induce higher levels of insulin-like growth factor (IGF) which is able to promote upregulation on the arginase activity [116]. However, this kind of report does not have to investigate the possible influence of LRV infection on oxidative resistance [115].
VL exhibits a mixed type 1 and type 2 cytokine profiles. Studies in experimental models show that neither IL-4 nor IL-13 (typically Th2 cytokines) is able to induce disease exacerbation. However, a consensus exists in relation to the suppressive effect of IL-10 on the immune response in VL and its correlation with disease severity, as this cytokine is an important immunosuppressant and inhibitor of macrophage microbicidal activity in both mice and humans with VL [103, 117]. The control of VL is also dependent on the development of type 1 cytokines and effector antileishmanial molecules such as reactive nitrogen and oxygen intermediates for parasite control in the spleen [118].
In the case of Chagas disease, the existence of a large spectrum of clinical manifestations is associated with parasite heterogeneity and the host immune response. The acute phase is followed by the development of effective acquired immunity, leading to the control of parasitaemia and parasitism levels in tissues. Some authors have shown that in experimental models of acute T. cruzi infection, the T helper type 1 response (Th1) appears to have a critical role in infection control. This response can occur through toll-like receptor- (TLR-) mediated and TLR-independent cytokine production [119–121]. Early studies indicated that this infection promotes a certain degree of immunosuppression; however, subsequent data using new approaches demonstrate a substantial antiparasite response during acute experimental infection [122]. Peripheral blood mononuclear cells (PBMCs) from children with acute phase infections present mRNA profiles of interferon (IFN)-γ, interleukin (IL)-2, and IL-10, with low levels of IL-4 [123]. Interestingly, children with asymptomatic chronic Chagas disease present upregulated IL-4 mRNA, suggesting that following Th1-mediated parasite clearance, a balance of both Th1 and Th2 immune responses occurs to suppress parasite load and protect against immunopathology [122, 123]. Another study showed that children with acute infection present higher serum levels of tumor necrosis factor (TNF)-α, sIL2R, sCD8, sCD4, and IL-6, but no change in IL-2, IL-12, and IL-8 is observed compared to healthy controls or children with asymptomatic Chagas disease in the chronic phase [124].
The lifelong chronic phase is maintained with low parasitaemia and tissue parasitism. The first source of IFN-γ seems to be natural killer (NK) cells. This cytokine augments IL-12, TNF-α and other cytokines synthesized by classically activated macrophages [125–127]. IFN-γ produced by NK cells and IL-12 produced by macrophages have been suggested to induce the differentiation of T-helper cells to a predominant protective Th1 phenotype [128, 129]. IFN-γ produced by Th1 cells activates effector mechanisms in macrophages. These effector mechanisms destroy both amastigotes and phagocytized trypomastigotes, whereas cytotoxic activity displayed by CD8+ T cells destroys cells containing intracellular amastigotes [130–137]. T. cruzi antigen-specific CD8 T cells are frequently present in infected mice and humans [137]. Antibodies produced by B cells lyse the extracellular trypomastigote form, facilitate the phagocytosis of parasites opsonized with IgG [138], and promote the complement-dependent killing of the parasites [139]. During severe cardiomyopathy of the chronic phase of Chagas disease, the occurrence of intense inflammatory response is correlated with the production of type 1 cytokines, such as TNF-α and IFN-γ. In this disease phase, the level of these cytokines is higher than during indeterminate phase of Chagas disease [140]. Indeterminate patients seem to have a more regulated response by Treg cells, limiting tissue damage with the maintenance of improved cardiac function, but apparently the mechanism is not IL-10- or CTLA-4-dependent [141]. These essential responses to Chagas disease have been clearly shown using experimental models or natural human infections in that the absence or the reduction in any of these immune responses (via targeted depletion, immunosuppressive treatments, or infection-induced immunosuppression) can exacerbate parasitaemia [142–144]. In summary, the literature indicates that the persistence of protozoans is related to the delayed kinetics of CD8+ T cell development and the balance between Th1 and Th2 responses. An efficient protective response against T. cruzi requires the Th1 response, activation of phagocytes, T-helper cells and cytotoxic T lymphocytes, and lytic antibodies.
The ability of parasitic protozoa to interfere with effector mechanisms of the immune response has been studied over decades. The complex life cycle of Leishmania sp. and T. cruzi involves the emergence of a number of characteristics that allow its survival in different microenvironments in the insect vector and the vertebrate host. Polyclonal lymphocyte activation is an example of an immune evasion mechanism found in some pathogens. In a mouse model of T. cruzi infection, reduced levels of polyclonal lymphocyte responses correlate with infection and control of cardiomyopathy. The enzyme proline racemase was described in T. cruzi (TcPRAC) and is expressed either as a cytoplasmic, membrane-associated protein [145] or as a secreted isoform, which can be detected at all stages of the parasite life cycle. The secreted form is shown to be a B cell mitogen, which contributes to parasite evasion of the host immune system and its persistence in the vertebrate host [146].
The vertebrate infective forms have developed several strategies to survive in the hostile host environment. For example, bloodstream T. cruzi trypomastigotes express molecules on their surface that are capable of interfering with the activation of the classical and alternative complement pathways [147]. Several membrane glycoprotein-specific trypomastigotes participate efficiently and prevent complement activation on the surface of the parasite. Some of these molecules, such as gp160, gp58/68, and T-DAF, regulate complement by inhibiting the development and/or accelerating the decay of C3 convertase, a central enzyme in the complement cascade [148]. Recent studies [149] provide evidence that metacyclic trypomastigotes induce the formation of vesicles derived from the host cell, which form a complex released from the parasite surface, leading to stabilization and inhibition of C3 convertase resulting in increased survival of the parasite.
Another mechanism for the attachment-independent invasion of trypomastigotes involves the activation of the TGF-β signaling pathway [150]. A protease secreted by the parasite is likely to activate latent TGF-β associated with extracellular matrix (ECM) components, allowing activation of Smad 2/3 pathway through the TGF-β receptors (I and II) present on the surface of host cells. The pivotal role of this pathway in infections of heart tissues and, consequently, in the chagasic cardiomyopathy has previously been described [150].
T. cruzi has a gene, FL-160, encoding the C-terminus of flagellar protein. This protein has a twelve amino acid epitope similar to nervous tissue proteins present in the sciatic nerve plexus and mesenteric SNC. This gene belongs to a family of highly related genes that are encoded in more than 750 copies in the parasite genome; sequential analyses reveal that all copies of this gene have the 12 amino acids that mimic the human sequence, which may be a prevalence and immunosuppression factor in Chagas disease [151].
In the T. cruzi experimental murine acute infection model, several changes are observed in lymphoid organs, including the thymus, where intense and severe thymic atrophy due to depletion of CD4+8+ double-positive cells (DP) thymocytes by apoptosis in the cortical area of the thymus occurs [152]. A recent study shows that T. cruzi trans-sialidase (TcTS) induces thymic atrophy that affects the dynamics of intrathymic thymocytes, resulting in an increase in the number of CD4+8+ DP recent thymic emigrants in the spleen. TcTS is also capable of activating MAPK JNK signaling in thymocytes, modulating their adhesion to thymic epithelial cells and their migration toward the extracellular matrix. These data suggest the possible involvement of this enzyme in abnormal thymocyte trafficking inside the thymus of animals acutely infected by T. cruzi, which could influence the escape of immature thymocytes to peripheral blood in Chagas disease. The authors report that the frequency of DP T cells in chronic patients presenting high antibody titles against TcTS with the cardiac form of Chagas disease is increased. Thus, the presence of peripheral activated DP cells with potentially autoreactive TCRs may contribute to the immunopathological events found in this disease [153].
T. cruzi can also interfere with signaling via new members of the B7 family, such as the programmed death ligand 1 (PD-L1). This ligand binds to the programmed death 1 (PD-1) receptor, which is expressed on activated T cells, B cells, and myeloid cells. Their interactions result in downmodulation of the T-cell response [154, 155]. T. cruzi infection promotes an increase in expression of PD-1 and its ligands on peritoneal macrophages as well as during in vitro infection. Macrophages from mice infected by this protozoan are able to promote suppression of T cell proliferation. This suppression is restored when anti-PD-1 and anti-PD-L1 antibodies are added. Additionally, the blockage of PD-1 and PD-L1 increases iNOS expression and NO production on peritoneal macrophages from T. cruzi-infected mice [156].
T. cruzi infection promotes the formation of lipid bodies in macrophages through TLR2 signaling, which is amplified by the uptake of apoptotic cells in a mechanism dependent on integrins and TGF-β synthesis and results in an increased parasite survival and proliferation [157].
For leishmanial infection to be successful, the parasite must resist the hostile environment inside the host and survive to its innate and acquired immune response. Initially these include complement system, followed by phagocytosis, acidification of the phagolysosome, ROS release and, finally, NO production. Leishmania promastigotes abundantly express LPG (lipophosphoglycan), which forms a great glycocalyx surround the parasite and interferes with the insertion of membrane attack complex [158]. Promastigotes also present specific kinases able to deactivate the classical and alternative complement pathway by phosphorylating of complement components [159]. In addition gp63 can convert C3b (complement subunit 3), attached to parasite surface, into its inactive form, iC3b, which prevents parasite lysis via the complement system [160]. Furthermore, iC3b can opsonize Leishmania and allow entry in the host cell by binding the receptors CR1 and CR3 (complement receptors) (Figure 1) [161, 162].
Inside the neutrophils, the first cell to phagocyte the promastigotes, LPG and an acid phosphatase resistant to tartrate, present on the parasite cell surface, inhibit lysosome fusion and the respiratory burst [163–165]. Promastigotes release a chemotactic substance, lipid Leishmania chemotactic factor (LCF) to attract more neutrophils [166]. The LCF can interact with lipoxin A4 receptors (ALX), resulting in the deactivation of oxidative burst of neutrophils [167]. Furthermore, Leishmania presents an inhibitor of serine peptidase capable to inhibit the serine peptidase released by neutrophils, the neutrophil elastase. This is crucial for intracellular parasite survival [168].
The Trojan horse theory supports the idea that apoptotic neutrophils infected by Leishmania, when taken up by macrophages, allow a silent entrance of the parasite, contributing to the success of infection [169]. Peters et al. [16] showed robust neutrophil infiltration after the bite of the sand fly (vector insect of leishmaniasis) infected with L. major. These parasites survive and appear to be better adapted to resist macrophages that were committed during the clearance of apoptotic neutrophils and thus with impaired inflammatory functions when released by neutrophils. Apoptotic Leishmania parasites seem to be essential for disease development, because when these cells were depleted from a population of virulent L. major, experimental infection was controlled both in vitro and in vivo. This is due to the increased production of TGF-β induced by apoptotic promastigotes [170].
After neutrophils, Leishmania promastigotes can enter into dermal macrophages, which lack the respiratory burst machinery. Thus, promastigotes have opportunity to ameliorate their ability to transform into amastigotes and grow inside the host cell [171]. In the same way, promastigotes and amastigotes can be actively ingested by the skin fibroblasts [172], where they find a safe environment for up to 7 days after infection, since these cells produce low levels of NO even in the presence of interferon-γ, compared to macrophages [172].
Inside the macrophage, LPG can inhibit the oxidative burst initiated by NADPH oxidase at the time of their entry into the host cell. This phenomenon seems to be another strategy used by Leishmania to buy time to transform into the resistant amastigote form. LPG can inhibit PKC (protein kinase C), a key enzyme for initiation of the oxidative burst. LPG is known to inhibit the translocation of this enzyme to the cell membrane due to its transference from parasites membrane to the macrophage membrane during phagocytosis and binds to the regulatory domain of PKC, inactivating the production of reactive oxygen species (ROS) (Figure 1) [173–175]. Furthermore, LPG can inhibit the production of IL-12 by macrophages, thus impairing Th1 differentiation, though the mechanism has not been elucidated [175].
The metalloprotease gp63 is also involved in parasite protection within the phagolysosome. This protease activity appears to protect against host proteolytic enzymes [176]. This important protease is also involved in processes of immune evasion. Gp63 cleaves and activates the protein tyrosine phosphatase SHP-1, interfering with the IFN-γ signaling pathway by dephosphorylating Janus kinase 2 (JAK2) (Figure 1) [177]. This JAK2 dephosphorylating negatively interferes with ERK1/2 (extracellular signal-regulated kinase 1/2), MAPK (mitogen-activated protein kinase), nuclear factor-κB (NFκB), IRF-1 (interferon regulatory factor-1), and AP-1 (activator protein 1), inhibiting classical macrophage activation and impairing the production of IL-12, NO, and immunoproteasome formation [178, 179]. NFκB is a key transcription factor that mediates innate and adaptive immunity and is involved in the transcription of adhesion molecules and chemokines that leads to the recruitment and activation of effector cells. GP63 in Leishmania promastigotes can cleave the p65RelA subunit of this transcription factor, resulting in the p35RelA fragment that is associated with promotion of certain chemokines (MIP-1β and MIP-2—macrophage inflammatory protein) and favors the recruitment of phagocytic cells but does not induce other macrophage products such as iNOS and IL-12, essential for a protective response [180, 181]. Leishmania may also stimulate the degradation of STAT-1 (signal transducer and activator of transcription) in host cells by modulating signaling pathways through receptors CR3 and FcуR, which inhibits iNOS expression and NO production, leading to parasite survival [182, 183].
In summary, Leishmania parasites have a very complex repertoire of strategies to escape the immune system by interfering in a range of signal transduction pathways in host cells (mainly macrophages), inhibiting the protective response and continuing the life cycle.
4. Therapeutic Targets
There are large differences between the trypanosomatids and mammalian cells, so different biochemical pathways of parasites from the hosts would be excellent targets for the new drugs design [184]. With the post genomic era, the discovery of new targets can be amplified and supporting the development of drugs more specific for the parasite and less toxic for the host. Among these possible targets include (a) mitochondrial markers; (b) fatty acids, sterols, carbohydrates, and folate biosynthesis [185, 186]; (c) recovery and metabolism of purines, pyrimidines [187], and aminoacids (as proline) [145]; (d) biosynthesis, transport, and metabolism of polyamines [188]; (e) the cell cycle [189, 190]; (f) proteases [191] and (g) proteasomes [192, 193].
Current therapeutic strategies in leishmaniasis and trypanosomiasis are far from satisfactory. The efficacy is variable, toxicity is high, and the emergence of resistance is increasingly common.
The trypanosomiasis treatment dates back over 50 years and is based on nifurtimox and benznidazole, which belong to the class of nitroaromatic compounds. These agents function as pro-drugs and must depend of enzyme-mediated activation inside parasites. The nitroreductases mediate reduction of the nitro-group generating an unstable nitroradical that, in presence of oxygen, generate superoxide. The T. cruzi sensibility depends on its capacity detoxification of free radicals as well as associated to downregulation of type I nitroreductases of the parasites [194]. Although benznidazole is considered to be better tolerated than nifurtimox, various adverse effects are attributed to their use, such as neuropathy and agranulocytosis. These drugs are active against blood forms of T. cruzi and effective in treating the acute phase of infection; however their efficiency in chronic phase is controversial. Actually, studies are being done to make nitro drugs selectively toxic to the parasite and more effective in chronic phase [195]. Fexinidazole is a nitroheterocyclic effective oral treatment of acute and chronic experimental T. cruzi infection [196]. Recently a study showed the efficacy of the metabolites fexinidazole in a mouse model of acute infection, leading to reduced inflammation in heart tissue associated with the chronic phase of Chagas disease [197].
In general, the first line leishmaniasis treatments are pentavalent antimonial that have been developed over 50 years ago. To exert its antileishmanial activity, the pentavalent antimony needs to be reduced to its trivalent form inside macrophages. The mechanism of action of antimonials is not completely clarified, but is known to involve inhibition of glycolitic pathway, fatty acids and trypanotione reductase [198, 199]. Pentamidine, amphotericin B, miltefosine, and paramomycin are used as second-line drugs [200–203]. The action mechanism of pentamidine is not well characterized, although there is evidence that involves mitochondrial functions interference [204]. The paromomycin mechanism is based on inhibition of protein synthesis of the parasite [203], covalently bound to protein and effects translation and vesicle-mediated trafficking [205]. The miltefosine acts on the cell signal transduction pathway by inhibiting protein kinase B, which makes an important role in the biosynthesis of sterols and phospholipids [206]. Already amphotericin B binds to ergosterol, a major component of the cellular membrane of Leishmania, forming transmembrane channels that release monovalent ions (K+, Na+, H+ and Cl−) leading to cell death [207]. To minimize the adverse events of amphotericin B, various lipid formulations have been introduced leading rapidly concentrated into organs such as liver, spleen and increase the antileishmanial activity with selectivity to macrophage reticular-endothelial system [208]. Sitamaquine (8-aminoquinoline) is oral drug for the treatment of visceral leishmaniasis which has completed Phase II trials in India and Kenya [208, 209]. The molecular targets of sitamaquine are still unknown, however it was shown that upon binding to transiently membrane sterols is found in the cytoplasm and induces changes mitochondrial membrane potential [210].
The sterol biosynthesis is a potential drugs target in trypanosomatids since there are some differences between parasite and host. Parasite is entirely dependent of endogenously sterols for survival and growth and cannot use the supply of the host cholesterol. The major product sterol biosynthesis of trypanosomatids is ergosterol and other 24-methyl sterols and the 14α-demethylase (CYP51) is key of pathway inhibited by azoles. These azoles have antiparasite action same the antifungal because block the biosynthesis accumulating toxic methylated precursors [211, 212]. Besides the main targets are membranes of mitochondria, the protozoan cell body and flagellum, other important changes take place in the organization of the kinetoplast DNA network and on the protozoan cell cycle leading to cell death [213]. Azoles as ketoconazole and fluconazole demonstrate the efficacy to treat some clinical forms of leishmaniasis [214–216], while posaconazole and ravuconazole have been reported on clinical trials (phase I or II) on T. cruzi infection [217–219].
The TcPRAC is a promising target for the development of a new therapy against Chagas disease since parasites are no longer viable when PRAC genes are knocked down or more virulent if PRAC genes are over expressed [220]. Two compounds, which are irreversible competitive inhibitors of TcPRAC, were able to inhibit the mammalian host cell infection [221].
Recently, protease inhibitors used in antiretroviral therapy regimen of high efficiency (HAART) to treat HIV-infected patients have been used to treat trypanosomiasis and leishmaniasis. Studies show that the strategy had good results against T. cruzi and different species of Leishmania genus [222]. It is believed that these inhibitors affect the proteasomes of parasites responsible for the proliferation, differentiation and intracellular survival of microorganisms [223].
Aspartic peptidase inhibitors used in the current chemotherapy against HIV were able to inhibit the aspartic peptidase activity produced by different species of Leishmania spp and induced an increase in the level of reactive oxygen species, triggering parasite death pathways such as programed cell death (apoptosis) and uncontrolled autophagy [224, 225].
Finally, the possibility of different therapies combination against trypanosomatids can be result ameliorates to the low efficiency, high toxicity and especially reduce possibility of parasite resistance [226]. Thus emerged over the last decade this strategy has been tested successfully against others parasites included malaria and tuberculosis agents [227]. The multitarget compounds use against trypanosomatids is another way to reduce resistance to treatment, since drugs with a single target are susceptible to high level of resistance, a result of the mutation of the target protein [197, 228, 229]. Besides the combination chemotherapy, another important therapeutic approach is immunotherapy. The immunotherapy includes the use of biological substances or molecules to modulate the immune responses for the purpose of achieving a prophylactic and/or therapeutic success. The immunotherapeutic agents can exert their effect by directly or indirectly augmenting the host natural defenses, restoring the impaired effectors functions or decreasing host excessive response. The combination of immunotherapy with chemotherapeutic drugs (immunochemotherapy) is showing promise in the treatment of visceral and mucosal leishmaniasis [230–233].
5. Concluding Remarks
The complexity of the relationship between intracellular Leishmania spp. and T. cruzi and their human hosts is a limitation to vaccine and drug design. Heterogeneity within the same parasite species and our limited experimental models make it even more challenging to understand this complex association. However, knowledge is accumulating regarding the molecular machinery of these parasites and the host immune response can be used to change our paradigms and develop new strategies for the treatment and control of these diseases. Treatments that target different points in parasite metabolism are an important strategy to improve efficacy and prevent resistance. In this sense, a combination of drugs for treatment should be encouraged. The use of immunomodulators may also be relevant to restore homeostasis of the host and attenuate tissue damage contributing to the therapeutic success.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
Authors' Contribution
Silvia Amaral Gonçalves Da Silva and Patrícia Maria Lourenço Dutra share equal contribution in authorship.
References
- 1.Patz J. A., Graczyk T. K., Geller N., Vittor A. Y. Effects of environmental change on emerging parasitic diseases. International Journal for Parasitology. 2000;30(12-13):1395–1405. doi: 10.1016/S0020-7519(00)00141-7. [DOI] [PubMed] [Google Scholar]
- 2.Butler D. Lost in translation. Nature. 2007;449(7159):158–159. doi: 10.1038/449158a. [DOI] [PubMed] [Google Scholar]
- 3.Lainson R., Ward R. D., Shaw J. J. Leishmania in phlebotomid sandflies: VI. Importance of hindgut development in distinguishing between parasites of the Leishmania mexicana and L. braziliensis complexes. Proceedings of the Royal Society of London: Biological Sciences. 1977;199(1135):309–320. doi: 10.1098/rspb.1977.0141. [DOI] [PubMed] [Google Scholar]
- 4.Killick-Kendrick R. The biology and control of phlebotomine sand flies. Clinics in Dermatology. 1999;17(3):279–289. doi: 10.1016/S0738-081X(99)00046-2. [DOI] [PubMed] [Google Scholar]
- 5.Alvar J., Vélez I. D., Bern C., et al. Leishmaniasis worldwide and global estimates of its incidence. PLoS ONE. 2012;7(5) doi: 10.1371/journal.pone.0035671.e35671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO. TDR Disease Reference Group on Chagas Disease; 2012. Research priorities for chagas disease, human African trypanosomiasis and leishmaniasis. [PubMed] [Google Scholar]
- 7.da Silva R., Sacks D. L. Metacyclogenesis is a major determinant of Leishmania promastigote virulence and attenuation. Infection and Immunity. 1987;55(11):2802–2806. doi: 10.1128/iai.55.11.2802-2806.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zeledon R., Bolanos R., Rojas M. Scanning electron microscopy of the final phase of the life cycle of Trypanosoma cruzi in the insect vector. Acta Tropica. 1984;41(1):39–43. [PubMed] [Google Scholar]
- 9.de Trez C., Magez S., Akira S., Ryffel B., Carlier Y., Muraille E. iNOS-producing inflammatory dendritic cells constitute the major infected cell type during the chronic Leishmania major infection phase of C57BL/6 resistant mice. PLoS Pathogens. 2009;5(6) doi: 10.1371/journal.ppat.1000494.e1000494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaye P., Scott P. Leishmaniasis: complexity at the host-pathogen interface. Nature Reviews Microbiology. 2011;9(8):604–615. doi: 10.1038/nrmicro2608. [DOI] [PubMed] [Google Scholar]
- 11.Beattie L., Peltan A., Maroof A., et al. Dynamic imaging of experimental Leishmania donovani-induced hepatic granulomas detects kupffer cell-restricted antigen presentation to antigen-specific CD8+ T cells. PLoS Pathogens. 2010;6(3) doi: 10.1371/journal.ppat.1000805.e1000805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bianchi M. E. DAMPs, PAMPs and alarmins: all we need to know about danger. Journal of Leukocyte Biology. 2007;81(1):1–5. doi: 10.1189/jlb.0306164. [DOI] [PubMed] [Google Scholar]
- 13.Pearson R. D., Steigbigel R. T. Phagocytosis and killing of the protozoan Leishmania donovani by human polymorphonuclear leukocytes. Journal of Immunology. 1981;127(4):1438–1443. [PubMed] [Google Scholar]
- 14.Chang K. P. Leishmanicidal mechanisms of human polymorphonuclear phagocytes. The American Journal of Tropical Medicine and Hygiene. 1981;30(2):322–333. doi: 10.4269/ajtmh.1981.30.322. [DOI] [PubMed] [Google Scholar]
- 15.Guimarães-Costa A. B., Nascimento M. T. C., Froment G. S., et al. Leishmania amazonensis promastigotes induce and are killed by neutrophil extracellular traps. Proceedings of the National Academy of Sciences of the United States of America. 2009;106(16):6748–6753. doi: 10.1073/pnas.0900226106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peters N. C., Egen J. G., Secundino N., et al. In vivo imaging reveals an essential role for neutrophils in leishmaniasis transmitted by sand flies. Science. 2008;321(5891):970–974. doi: 10.1126/science.1159194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wenzel U. A., Bank E., Florian C., et al. Leishmania major parasite stage-dependent host cell invasion and immune evasion. FASEB Journal. 2012;26(1):29–39. doi: 10.1096/fj.11-184895. [DOI] [PubMed] [Google Scholar]
- 18.Vannier-Santos M. A., Martiny A., de Souza W. Cell biology of Leishmania spp.: invading and evading. Current Pharmaceutical Design. 2002;8(4):297–318. doi: 10.2174/1381612023396230. [DOI] [PubMed] [Google Scholar]
- 19.Desjardins M., Descoteaux A. Inhibition of phagolysosomal biogenesis by the Leishmania lipophosphoglycan. Journal of Experimental Medicine. 1997;185(12):2061–2068. doi: 10.1084/jem.185.12.2061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Descoteaux A., Turco S. J. Functional aspects of the Leishmania donovani lipophosphoglycan during macrophage infection. Microbes and Infection. 2002;4(9):975–981. doi: 10.1016/S1286-4579(02)01624-6. [DOI] [PubMed] [Google Scholar]
- 21.Handman E., Goding J. W. The Leishmania receptor for macrophages is a lipid-containing glycoconjugate. EMBO Journal. 1985;4(2):329–336. doi: 10.1002/j.1460-2075.1985.tb03633.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Talamás-Rohana P., Wright S. D., Lennartz M. R., Russell D. G. Lipophosphoglycan from Leishmania mexicana promastigotes binds to members of the CR3, p150,95 and LFA-1 family of leukocyte integrins. Journal of Immunology. 1990;144(12):4817–4824. [PubMed] [Google Scholar]
- 23.Descoteaux A., Matlashewski G., Turco S. J. Inhibition of macrophage protein kinase C-mediated protein phosphorylation by Leishmania donovani lipophosphoglycan. The Journal of Immunology. 1992;149(9):3008–3015. [PubMed] [Google Scholar]
- 24.Holm Å., Tejle K., Gunnarsson T., Magnusson K.-E., Descoteaux A., Rasmusson B. Role of protein kinase C α for uptake of unopsonized prey and phagosomal maturation in macrophages. Biochemical and Biophysical Research Communications. 2003;302(4):653–658. doi: 10.1016/S0006-291X(03)00231-6. [DOI] [PubMed] [Google Scholar]
- 25.McNeely T. B., Turco S. J. Requirement of lipophosphoglycan for intracellular survival of Leishmania donovani within human monocytes. Journal of Immunology. 1990;144(7):2745–2750. [PubMed] [Google Scholar]
- 26.Späth G. F., Garraway L. A., Turco S. J., Beverley S. M. The role(s) of lipophosphoglycan (LPG) in the establishment of Leishmania major infections in mammalian hosts. Proceedings of the National Academy of Sciences of the United States of America. 2003;100(16):9536–9541. doi: 10.1073/pnas.1530604100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Booth J. W., Trimble W. S., Grinstein S. Membrane dynamics in phagocytosis. Seminars in Immunology. 2001;13(6):357–364. doi: 10.1006/smim.2001.0332. [DOI] [PubMed] [Google Scholar]
- 28.Hackam D. J., Rotstein O. D., Sjolin C., Schreiber A. D., Trimble W. S., Grinstein S. v-SNARE-dependent secretion is required for phagocytosis. Proceedings of the National Academy of Sciences of the United States of America. 1998;95(20):11691–11696. doi: 10.1073/pnas.95.20.11691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huynh K. K., Kay J. G., Stow J. L., Grinstein S. Fusion, fission, and secretion during phagocytosis. Physiology. 2007;22(6):366–372. doi: 10.1152/physiol.00028.2007. [DOI] [PubMed] [Google Scholar]
- 30.Bajno L., Peng X.-R., Schreiber A. D., Moore H. P., Trimble W. S., Grinstein S. Focal exocytosis of VAMP3-containing vesicles at sites of phagosome formation. Journal of Cell Biology. 2000;149(3):697–706. doi: 10.1083/jcb.149.3.697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Braun V., Niedergang F. Linking exocytosis and endocytosis during phagocytosis. Biology of the Cell. 2006;98(3):195–201. doi: 10.1002/humu.20247. [DOI] [PubMed] [Google Scholar]
- 32.Cox D., Lee D. J., Dale B. M., Calafat J., Greenberg S. A Rab11-containing rapidly recycling compartment in macrophages that promotes phagocytosis. Proceedings of the National Academy of Sciences of the United States of America. 2000;97(2):680–685. doi: 10.1073/pnas.97.2.680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Desjardins M. ER-mediated phagocytosis: a new membrane for new functions. Nature Reviews Immunology. 2003;3(4):280–291. doi: 10.1038/nri1053. [DOI] [PubMed] [Google Scholar]
- 34.Hatsuzawa K., Tamura T., Hashimoto H., et al. Involvement of syntaxin 18, an endoplasmic reticulum (ER)-localized SNARE protein, in ER-mediated phagocytosis. Molecular Biology of the Cell. 2006;17(9):3964–3977. doi: 10.1091/mbc.E05-12-1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Niedergang F., Colucci-Guyon E., Dubois T., Raposo G., Chavrier P. ADP ribosylation factor 6 is activated and controls membrane delivery during phagocytosis in macrophages. The Journal of Cell Biology. 2003;161(6):1143–1150. doi: 10.1083/jcb.200210069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chapman E. R. How does synaptotagmin trigger neurotransmitter release? Annual Review of Biochemistry. 2008;77:615–641. doi: 10.1146/annurev.biochem.77.062005.101135. [DOI] [PubMed] [Google Scholar]
- 37.Jahn R., Lang T., Südhof T. C. Membrane fusion. Cell. 2003;112(4):519–533. doi: 10.1016/S0092-8674(03)00112-0. [DOI] [PubMed] [Google Scholar]
- 38.Martinez I., Chakrabarti S., Hellevik T., Morehead J., Fowler K., Andrews N. W. Synaptotagmin VII regulates Ca2+-dependent exocytosis of lysosomes in fibroblasts. Journal of Cell Biology. 2000;148(6):1141–1149. doi: 10.1083/jcb.148.6.1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Czibener C., Sherer N. M., Becker S. M., et al. Ca2+ and synaptotagmin VII-dependent delivery of lysosomal membrane to nascent phagosomes. Journal of Cell Biology. 2006;174(7):997–1007. doi: 10.1083/jcb.200605004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vinet A. F., Fukuda M., Descoteaux A. The exocytosis regulator synaptotagmin V controls phagocytosis in macrophages. Journal of Immunology. 2008;181(8):5289–5295. doi: 10.4049/jimmunol.181.8.5289. [DOI] [PubMed] [Google Scholar]
- 41.Vieira L. L., Sacerdoti-Sierra N., Jaffe C. L. Effect of pH and temperature on protein kinase release by Leishmania donovani . International Journal for Parasitology. 2002;32(9):1085–1093. doi: 10.1016/S0020-7519(02)00067-X. [DOI] [PubMed] [Google Scholar]
- 42.Dermine J.-F., Goyette G., Houde M., Turco S. J., Desjardins M. Leishmania donovani lipophosphoglycan disrupts phagosome microdomains in J774 macrophages. Cellular Microbiology. 2005;7(9):1263–1270. doi: 10.1111/j.1462-5822.2005.00550.x. [DOI] [PubMed] [Google Scholar]
- 43.Winberg M. E., Holm Å., Särndahl E., et al. Leishmania donovani lipophosphoglycan inhibits phagosomal maturation via action on membrane rafts. Microbes and Infection. 2009;11(2):215–222. doi: 10.1016/j.micinf.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 44.Vinet A. F., Fukuda M., Turco S. J., Descoteaux A. The Leishmania donovani lipophosphoglycan excludes the vesicular proton-ATPase from phagosomes by impairing the recruitment of Synaptotagmin V. PLoS Pathogens. 2009;5(10) doi: 10.1371/journal.ppat.1000628.e1000628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vinet A. F., Jananji S., Turco S. J., Fukuda M., Descoteaux A. Exclusion of synaptotagmin V at the phagocytic cup by Leishmania donovani lipophosphoglycan results in decreased promastigote internalization. Microbiology. 2011;157(9):2619–2628. doi: 10.1099/mic.0.050252-0. [DOI] [PubMed] [Google Scholar]
- 46.Phan B. A. P., Laflamme M. A., Stempien-Otero A., Limaye A. P., Buckner F. S., Levy W. C. Confirmation of Chagas’ cardiomyopathy following heart transplantation. Heart and Vessels. 2006;21(5):325–327. doi: 10.1007/s00380-005-0899-4. [DOI] [PubMed] [Google Scholar]
- 47.Dodd R. Y., Notari E. P., Stramer S. L. Current prevalence and incidence of infectious disease markers and estimated. Transfusion. 2002;42(8):975–979. doi: 10.1046/j.1537-2995.2002.00174.x. [DOI] [PubMed] [Google Scholar]
- 48.Punukollu G., Gowda R. M., Khan I. A., Navarro V. S., Vasavada B. C. Clinical aspects of the Chagas’ heart disease. International Journal of Cardiology. 2007;115(3):279–283. doi: 10.1016/j.ijcard.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 49.Yoshida N. Trypanosoma cruzi infection by oral route: how the interplay between parasite and host components modulates infectivity. Parasitology International. 2008;57(2):105–109. doi: 10.1016/j.parint.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 50.Teixeira A. R. L., Nitz N., Guimaro M. C., Gomes C., Santos-Buch C. A. Chagas disease. Postgraduate Medical Journal. 2006;82(974):788–798. doi: 10.1136/pgmj.2006.047357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yoshida N., Favoreto S., Jr., Ferreira A. T., Manque P. M. Signal transduction induced in Trypanosoma cruzi metacyclic trypomastigotes during the invasion of mammalian cells. Brazilian Journal of Medical and Biological Research. 2000;33(3):269–278. doi: 10.1590/S0100-879X2000000300003. [DOI] [PubMed] [Google Scholar]
- 52.Moreno S. N. J., Docampo R. Calcium regulation in protozoan parasites. Current Opinion in Microbiology. 2003;6(4):359–364. doi: 10.1016/S1369-5274(03)00091-2. [DOI] [PubMed] [Google Scholar]
- 53.Andrews N. W. Lysosomes and the plasma membrane: trypanosomes reveal a secret relationship. Journal of Cell Biology. 2002;158(3):389–394. doi: 10.1083/jcb.200205110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fernandes M. C., Flannery A. R., Andrews N., Mortara R. A. Extracellular amastigotes of Trypanosoma cruzi are potent inducers of phagocytosis in mammalian cells. Cellular Microbiology. 2013;15(6):977–991. doi: 10.1111/cmi.12090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Burleigh B. A., Woolsey A. M. Cell signalling and Trypanosoma cruzi invasion. Cellular Microbiology. 2002;4(11):701–711. doi: 10.1046/j.1462-5822.2002.00226.x. [DOI] [PubMed] [Google Scholar]
- 56.Burleigh B. A. Host cell signaling and Trypanosoma cruzi invasion: do all roads lead to lysosomes? Science’s STKE. 2005;2005, article pe36 doi: 10.1126/stke.2932005pe36. [DOI] [PubMed] [Google Scholar]
- 57.Yoshida N. Molecular basis of mammalian cell invasion by Trypanosoma cruzi . Anais da Academia Brasileira de Ciencias. 2006;78(1):87–111. doi: 10.1590/s0001-37652006000100010. [DOI] [PubMed] [Google Scholar]
- 58.Caler E. V., Chakrabarti S., Fowler K. T., Rao S., Andrews N. W. The exocytosis-regulatory protein synaptotagmin VII mediates cell invasion by Trypanosoma cruzi . Journal of Experimental Medicine. 2001;193(9):1097–1104. doi: 10.1084/jem.193.9.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Caradonna K. L., Burleigh B. A. Mechanisms of host cell invasion by Trypanosoma cruzi . Advances in Parasitology. 2011;76:33–61. doi: 10.1016/B978-0-12-385895-5.00002-5. [DOI] [PubMed] [Google Scholar]
- 60.Amer A. O., Swanson M. S. A phagosome of one’s own: a microbial guide to life in the macrophage. Current Opinion in Microbiology. 2002;5(1):56–61. doi: 10.1016/S1369-5274(02)00286-2. [DOI] [PubMed] [Google Scholar]
- 61.Rubin-de-Celis S. S. C., Uemura H., Yoshida N., Schenkman S. Expression of trypomastigote trans-sialidase in metacyclic forms of Trypanosoma cruzi increases parasite escape from its parasitophorous vacuole. Cellular Microbiology. 2006;8(12):1888–1898. doi: 10.1111/j.1462-5822.2006.00755.x. [DOI] [PubMed] [Google Scholar]
- 62.Neres J., Bryce R. A., Douglas K. T. Rational drug design in parasitology: trans-sialidase as a case study for Chagas disease. Drug Discovery Today. 2008;13(3-4):110–117. doi: 10.1016/j.drudis.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 63.Neres J., Brewer M. L., Ratier L., et al. Discovery of novel inhibitors of Trypanosoma cruzi trans-sialidase from in silico screening. Bioorganic & Medicinal Chemistry Letters. 2009;19(3):589–596. doi: 10.1016/j.bmcl.2008.12.065. [DOI] [PubMed] [Google Scholar]
- 64.Barros H. C., Silva S. D. A., et al. Release of membrane-bound trails by Trypanosoma cruzi amastigotes onto modified surfaces and mammalian cells. Journal of Eukaryotic Microbiology. 1996;43(4):275–285. doi: 10.1111/j.1550-7408.1996.tb03990.x. [DOI] [PubMed] [Google Scholar]
- 65.Acosta-Serrano A., Almeida I. C., Freitas-Junior L. H., Yoshida N., Schenkman S. The mucin-like glycoprotein super-family of Trypanosoma cruzi: structure and biological roles. Molecular and Biochemical Parasitology. 2001;114(2):143–150. doi: 10.1016/S0166-6851(01)00245-6. [DOI] [PubMed] [Google Scholar]
- 66.Previato J. O., Jones C., Gonçalves L. P. B., Wait R., Travassos L. R., Mendonça-Previato L. O-glycosidically linked N-acetylglucosamine-bound oligosaccharides from glycoproteins of Trypanosoma cruzi . Biochemical Journal. 1994;301, part 1:151–159. doi: 10.1042/bj3010151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Di Noia J. M., Pollevick G. D., Xavier M. T., et al. High diversity in mucin genes and mucin molecules in Trypanosoma cruzi . The Journal of Biological Chemistry. 1996;271(50):32078–32083. doi: 10.1074/jbc.271.50.32078. [DOI] [PubMed] [Google Scholar]
- 68.Mendonça-Previato L., Todeschini A. R., Heise N., Agrellos O. A., Dias W. B., Previato J. O. Chemical structure of major glycoconjugates from parasites. Current Organic Chemistry. 2008;12(11):926–939. doi: 10.2174/138527208784892187. [DOI] [Google Scholar]
- 69.Previato J. O., Andrade A. F. B., Pessolani M. C. V., Mendonca-Previato L. Incorporation of sialic acid into Trypanosoma cruzi macromolecules: a proposal for a new metabolic route. Molecular and Biochemical Parasitology. 1985;16(1):85–96. doi: 10.1016/0166-6851(85)90051-9. [DOI] [PubMed] [Google Scholar]
- 70.Mendonça-Previato L., Todeschini A. R., Freire de Lima L., Previato J. O. The trans-sialidase from Trypanosoma cruzi a putative target for Trypanocidal agents. Open Parasitology Journal. 2010;4(1):111–115. doi: 10.2174/1874421401004010111. [DOI] [Google Scholar]
- 71.Almeida I. C., Ferguson M. A. J., Schenkman S., Travassos L. R. Lytic anti-α-galactosyl antibodies from patients with chronic Chagas’ disease recognize novel O-linked oligosaccharides on mucin-like glycosyl-phosphatidylinositol-anchored glycoproteins of Trypanosoma cruzi . Biochemical Journal. 1994;304(3):793–802. doi: 10.1042/bj3040793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Schenkman S., Jiang M.-S., Hart G. W., Nussenzweig V. A novel cell surface trans-sialidase of Trypanosoma cruzi generates a stage-specific epitope required for invasion of mammalian cells. Cell. 1991;65(7):1117–1125. doi: 10.1016/0092-8674(91)90008-M. [DOI] [PubMed] [Google Scholar]
- 73.Mortara R. A., da Silva S., Araguth M. F., Blanco S. A., Yoshida N. Polymorphism of the 35- and 50-kilodalton surface glycoconjugates of Trypanosoma cruzi metacyclic trypomastigotes. Infection and Immunity. 1992;60(11):4673–4678. doi: 10.1128/iai.60.11.4673-4678.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Cortez C., Yoshida N., Bahia D., Sobreira T. J. P. Structural basis of the interaction of a Trypanosoma cruzi surface molecule implicated in oral infection with host cells and gastric mucin. PLoS ONE. 2012;7(7) doi: 10.1371/journal.pone.0042153.e42153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Camargo M. M., Almeida I. C., Pereira M. E. S., Ferguson M. A. J., Travassos L. R., Gazzinelli R. T. Glycosylphosphatidylinositol-anchored mucin-like glycoproteins isolated from Trypanosoma cruzi trypomastigotes initiate the synthesis of proinflammatory cytokines by macrophages. The Journal of Immunology. 1997;158(12):5890–5901. [PubMed] [Google Scholar]
- 76.Villalta F., Smith C. M., Ruiz-Ruano A., Lima M. F. A ligand that Trypanosoma cruzi uses to bind to mammalian cells to initiate infection. FEBS Letters. 2001;505(3):383–388. doi: 10.1016/S0014-5793(01)02853-8. [DOI] [PubMed] [Google Scholar]
- 77.Giordano R., Chammas R., Veiga S. S., Colli W., Alves M. J. M. An acidic component of the heterogeneous Tc-85 protein family from the surface of Trypanosoma cruzi is a laminin binding glycoprotein. Molecular and Biochemical Parasitology. 1994;65(1):85–94. doi: 10.1016/0166-6851(94)90117-1. [DOI] [PubMed] [Google Scholar]
- 78.Magdesian M. H., Tonelli R. R., Fessel M. R., et al. A conserved domain of the gp85/trans-sialidase family activates host cell extracellular signal-regulated kinase and facilitates Trypanosoma cruzi infection. Experimental Cell Research. 2007;313(1):210–218. doi: 10.1016/j.yexcr.2006.10.008. [DOI] [PubMed] [Google Scholar]
- 79.Dias W. B., Fajardo F. D., Graça-Souza A. V., et al. Endothelial cell signalling induced by trans-sialidase from Trypanosoma cruzi . Cellular Microbiology. 2008;10(1):88–99. doi: 10.1111/j.1462-5822.2007.01017.x. [DOI] [PubMed] [Google Scholar]
- 80.Magdesian M. H., Giordano R., Ulrich H., et al. Infection by Trypanosoma cruzi: identification of a parasite ligand and its host cell receptor. The Journal of Biological Chemistry. 2001;276(22):19382–19389. doi: 10.1074/jbc.M011474200. [DOI] [PubMed] [Google Scholar]
- 81.Yoshida N., Blanco S. A., Araguth M. F., González J. The stage-specific 90-kilodalton surface antigen of metacyclic trypomastigotes of Trypanosoma cruzi . Molecular and Biochemical Parasitology. 1990;39(1):39–46. doi: 10.1016/0166-6851(90)90006-8. [DOI] [PubMed] [Google Scholar]
- 82.Schenkman S., Andrews N. W., Nussenzweig V., Robbins E. S. Trypanosoma cruzi invade a mammalian epithelial cell in a polarized manner. Cell. 1988;55(1):157–165. doi: 10.1016/0092-8674(88)90018-9. [DOI] [PubMed] [Google Scholar]
- 83.Guther M. L. S., De Almeida M. L. C., Yoshida N., Ferguson M. A. J. Structural studies on the glycosylphosphatidylinositol membrane anchor of Trypanosoma cruzi 1G7-antigen. The structure of the glycan core. Journal of Biological Chemistry. 1992;267(10):6820–6828. [PubMed] [Google Scholar]
- 84.Scharfstein J., Schmitz V., Morandi V., et al. Host cell invasion by Trypanosoma cruzi is potentiated by activation of bradykinin B2 receptors. Journal of Experimental Medicine. 2000;192(9):1289–1300. doi: 10.1084/jem.192.9.1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Murta A. C. M., Persechini P. M., De Souto Padron T., De Souza W., Guimaraes J. A., Scharfstein J. Structural and functional identification of GP57/51 antigen of Trypanosoma cruzi as a cysteine proteinase. Molecular and Biochemical Parasitology. 1990;43(1):27–38. doi: 10.1016/0166-6851(90)90127-8. [DOI] [PubMed] [Google Scholar]
- 86.Souto-Padron T., Campetella O. E., Cazzulo J. J., de Souza W. Cysteine proteinase in Trypanosoma cruzi: immunocytochemical localization and involvement in parasite-host cell interaction. Journal of Cell Science. 1990;96, part 3:485–490. doi: 10.1242/jcs.96.3.485. [DOI] [PubMed] [Google Scholar]
- 87.Meirelles M. N. L., Juliano L., Carmona E., et al. Inhibitors of the major cysteinyl proteinase (GP57/51) impair host cell invasion and arrest the intracellular development of Trypanosoma cruzi in vitro. Molecular and Biochemical Parasitology. 1992;52(2):175–184. doi: 10.1016/0166-6851(92)90050-T. [DOI] [PubMed] [Google Scholar]
- 88.Hazenberg M. D., Spits H. Human innate lymphoid cells. Blood. 2014;124(5):700–709. doi: 10.1182/blood-2013-11-427781. [DOI] [PubMed] [Google Scholar]
- 89.Spits H., Artis D., Colonna M., et al. Innate lymphoid cells-a proposal for uniform nomenclature. Nature Reviews Immunology. 2013;13(2):145–149. doi: 10.1038/nri3365. [DOI] [PubMed] [Google Scholar]
- 90.Klose C. S. N., Flach M., Möhle L., et al. Differentiation of type 1 ILCs from a common progenitor to all helper-like innate lymphoid cell lineages. Cell. 2014;157(2):340–356. doi: 10.1016/j.cell.2014.03.030. [DOI] [PubMed] [Google Scholar]
- 91.Schenten D., Medzhitov R. The control of adaptive immune responses by the innate immune system. Advances in Immunology. 2011;109:87–124. doi: 10.1016/B978-0-12-387664-5.00003-0. [DOI] [PubMed] [Google Scholar]
- 92.Olive C. Pattern recognition receptors: sentinels in innate immunity and targets of new vaccine adjuvants. Expert Review of Vaccines. 2012;11(2):237–256. doi: 10.1586/erv.11.189. [DOI] [PubMed] [Google Scholar]
- 93.Medzhitov R., Janeway C. A., Jr. Innate immune recognition and control of adaptive immune responses. Seminars in Immunology. 1998;10(5):351–353. doi: 10.1006/smim.1998.0136. [DOI] [PubMed] [Google Scholar]
- 94.Iwasaki A., Medzhitov R. Regulation of adaptive immunity by the innate immune system. Science. 2010;327(5963):291–295. doi: 10.1126/science.1183021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.O’Shea J. J., Paul W. E. Mechanisms underlying lineage commitment and plasticity of helper CD4+ T cells. Science. 2010;327(5969):1098–1102. doi: 10.1126/science.1178334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Allen J. E., Maizels R. M. Diversity and dialogue in immunity to helminths. Nature Reviews Immunology. 2011;11(6):375–388. doi: 10.1038/nri2992. [DOI] [PubMed] [Google Scholar]
- 97.Pulendran B., Artis D. New paradigms in type 2 immunity. Science. 2012;337(6093):431–435. doi: 10.1126/science.1221064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Drake L. Y., Iijima K., Kita H. Group 2 innate lymphoid cells and CD4+ T cells cooperate to mediate type 2 immune response in mice. Allergy. 2014 doi: 10.1111/all.12446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Mizoguchi A., Bhan A. K. A case for regulatory B cells. Journal of Immunology. 2006;176(2):705–710. doi: 10.4049/jimmunol.176.2.705. [DOI] [PubMed] [Google Scholar]
- 100.Dilillo D. J., Matsushita T., Tedder T. F. B10 cells and regulatory B cells balance immune responses during inflammation, autoimmunity, and cancer. Annals of the New York Academy of Sciences. 2010;1183:38–57. doi: 10.1111/j.1749-6632.2009.05137.x. [DOI] [PubMed] [Google Scholar]
- 101.Vignali D. A. A., Collison L. W., Workman C. J. How regulatory T cells work. Nature Reviews Immunology. 2008;8(7):523–532. doi: 10.1038/nri2343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Banchereau J., Pascual V., O’Garra A. From IL-2 to IL-37: the expanding spectrum of anti-inflammatory cytokines. Nature Immunology. 2012;13(10):925–931. doi: 10.1038/ni.2406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.McMahon-Pratt D., Alexander J. Does the Leishmania major paradigm of pathogenesis and protection hold for New World cutaneous leishmaniases or the visceral disease? Immunological Reviews. 2004;201:206–224. doi: 10.1111/j.0105-2896.2004.00190.x. [DOI] [PubMed] [Google Scholar]
- 104.Kane M. M., Mosser D. M. Leishmania parasites and their ploys to disrupt macrophage activation. Current Opinion in Hematology. 2000;7(1):26–31. doi: 10.1097/00062752-200001000-00006. [DOI] [PubMed] [Google Scholar]
- 105.Guerra J. A. D. O., Prestes S. R., Silveira H., et al. Mucosal Leishmaniasis caused by Leishmania (Viannia) braziliensis and Leishmania (Viannia) guyanensis in the Brazilian Amazon. PLoS Neglected Tropical Diseases. 2011;5(3):p. e980. doi: 10.1371/journal.pntd.0000980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Marsden P. D. Mucosal leishmaniasis (“spundia” Escomel, 1911) Transactions of the Royal Society of Tropical Medicine and Hygiene. 1986;80(6):859–876. doi: 10.1016/0035-9203(86)90243-9. [DOI] [PubMed] [Google Scholar]
- 107.Ronet C., Hauyon-La Torre Y., Revaz-Breton M., et al. Regulatory B cells shape the development of Th2 immune responses in BALB/c mice infected with Leishmania major through IL-10 production. Journal of Immunology. 2010;184(2):886–894. doi: 10.4049/jimmunol.0901114. [DOI] [PubMed] [Google Scholar]
- 108.Gomes-Silva A., de Cássia Bittar R., dos Santos Nogueira R., et al. Can interferon-γ and interleukin-10 balance be associated with severity of human Leishmania (Viannia) braziliensis infection? Clinical & Experimental Immunology. 2007;149(3):440–444. doi: 10.1111/j.1365-2249.2007.03436.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Tarr P. I., Aline R. F., Jr., Smiley B. L., Scholler J., Keithly J., Stuart K. LR1: a candidate RNA virus of Leishmania . Proceedings of the National Academy of Sciences of the United States of America. 1988;85(24):9572–9275. doi: 10.1073/pnas.85.24.9572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Widmer G., Comeau A. M., Furlong D. B., Wirth D. F., Patterson J. L. Characterization of a RNA virus from the parasite Leishmania . Proceedings of the National Academy of Sciences of the United States of America. 1989;86(15):5979–5982. doi: 10.1073/pnas.86.15.5979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Salinas G., Zamora M., Stuart K., Saravia N. Leishmania RNA viruses in Leishmania of the Viannia subgenus. The American Journal of Tropical Medicine and Hygiene. 1996;54(4):425–429. doi: 10.4269/ajtmh.1996.54.425. [DOI] [PubMed] [Google Scholar]
- 112.Ives A., Ronet C., Prevel F., et al. Leishmania RNA virus controls the severity of mucocutaneous leishmaniasis. Science. 2011;331(6018):775–778. doi: 10.1126/science.1199326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Ronet C., Beverley S. M., Fasel N. Muco-cutaneous leishmaniasis in the New World: the ultimate subversion. Virulence. 2011;2(6):547–552. doi: 10.4161/viru.2.6.17839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Rayamajhi M., Humann J., Kearney S., Hill K. K., Lenz L. L. Antagonistic crosstalk between type I and II interferons and increased host susceptibility to bacterial infections. Virulence. 2010;1(5):418–422. doi: 10.4161/viru.1.5.12787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Hartley M.-A., Ronet C., Zangger H., Beverley S. M., Fasel N. Leishmania RNA virus: when the host pays the toll. Frontiers in Cellular and Infection Microbiology. 2012;2:p. 99. doi: 10.3389/fcimb.2012.00099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Vendrame C. M. V., Souza L. D., Carvalho M. D. T., Salgado K., Carvalho E. M., Goto H. Insulin-like growth factor-I induced and constitutive arginase activity differs among isolates of Leishmania derived from patients with diverse clinical forms of Leishmania braziliensis infection. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2010;104(8):566–568. doi: 10.1016/j.trstmh.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 117.Cummings H. E., Tuladhar R., Satoskar A. R. Cytokines and their STATs in cutaneous and visceral leishmaniasis. Journal of Biomedicine and Biotechnology. 2010;2010:6. doi: 10.1155/2010/294389.294389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Liese J., Schleicher U., Bogdan C. The innate immune response against Leishmania parasites. Immunobiology. 2008;213(3-4):377–387. doi: 10.1016/j.imbio.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 119.Bafica A., Santiago H. C., Goldszmid R., Ropert C., Gazzinelli R. T., Sher A. Cutting edge: TLR9 and TLR2 signaling together account for MyD88-dependent control of parasitemia in Trypanosoma cruzi infection. Journal of Immunology. 2006;177(6):3515–3519. doi: 10.4049/jimmunol.177.6.3515. [DOI] [PubMed] [Google Scholar]
- 120.Koga R., Hamano S., Kuwata H., et al. TLR-dependent induction of IFN-β mediates host defense against Trypanosoma cruzi . Journal of Immunology. 2006;177(10):7059–7066. doi: 10.4049/jimmunol.177.10.7059. [DOI] [PubMed] [Google Scholar]
- 121.Monteiro A. C., Schmitz V., Svensjo E., et al. Cooperative activation of TLR2 and bradykinin B2 receptor is required for induction of type 1 immunity in a mouse model of subcutaneous infection by Trypanosoma cruzi . Journal of Immunology. 2006;177(9):6325–6335. doi: 10.4049/jimmunol.177.9.6325. [DOI] [PubMed] [Google Scholar]
- 122.Bern C., Martin D. L., Gilman R. H. Acute and congenital Chagas disease. Advances in Parasitology. 2011;75:19–47. doi: 10.1016/B978-0-12-385863-4.00002-2. [DOI] [PubMed] [Google Scholar]
- 123.Samudio M., Montenegro-James S., Cabral M., Martinez J., De Arias A. R., James M. A. Cytokine responses in Trypanosoma cruzi-infected children in Paraguay. The American Journal of Tropical Medicine and Hygiene. 1998;58(1):119–121. doi: 10.4269/ajtmh.1998.58.119. [DOI] [PubMed] [Google Scholar]
- 124.Moretti E., Basso B., Cervetta L., Brigada A., Barbieri G. Patterns of cytokines and soluble cellular receptors in the sera of children with acute Chagas’ disease. Clinical and Diagnostic Laboratory Immunology. 2002;9(6):1324–1327. doi: 10.1128/CDLI.9.6.1324-1327.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Almeida I. C., Camargo M. M., Procópio D. O., et al. Highly purified glycosylphosphatidylinositols from Trypanosoma cruzi are potent proinflammatory agents. EMBO Journal. 2000;19(7):1476–1485. doi: 10.1093/emboj/19.7.1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Aliberti J. C. S., Souto J. T., Marino A. P. M. P., et al. Modulation of chemokine production and inflammatory responses in interferon-γ- and tumor necrosis factor-R1-deficient mice during Trypanosoma cruzi infection. The American Journal of Pathology. 2001;158(4):1433–1440. doi: 10.1016/S0002-9440(10)64094-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Almeida I. C., Gazzinelli R. T. Proinflammatory activity of glycosylphosphatidylinositol anchors derived from Trypanosoma cruzi: structural and functional analyses. Journal of Leukocyte Biology. 2001;70(4):467–477. [PubMed] [Google Scholar]
- 128.Abrahamsohn I. A., Coffman R. L. Trypanosoma cruzi: IL-10, TNF, IFN-γ and IL-12 regulate innate and acquired immunity to infection. Experimental Parasitology. 1996;84(2):231–244. doi: 10.1006/expr.1996.0109. [DOI] [PubMed] [Google Scholar]
- 129.Duthie M. S., Kahn S. J. During acute Trypanosoma cruzi infection highly susceptible mice deficient in natural killer cells are protected by a single α-galactosylceramide treatment. Immunology. 2006;119(3):355–361. doi: 10.1111/j.1365-2567.2006.02439.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Muñoz-Fernández M. A., Fresno M. Activation of human macrophages for the killing of intracellular Trypanosoma cruzi by TNF-α and IFN-γ through a nitric oxide-dependent mechanism. Immunology Letters. 1992;33(1):35–40. doi: 10.1016/0165-2478(92)90090-B. [DOI] [PubMed] [Google Scholar]
- 131.Muñoz-Fernández M. A., Fresno M. Synergism between tumor necrosis factor-α and interferon-γ on macrophage activation for the killing of intracellular Trypanosoma cruzi through a nitric oxide-dependent mechanism. European Journal of Immunology. 1992;22(2):301–307. doi: 10.1002/eji.1830220203. [DOI] [PubMed] [Google Scholar]
- 132.Cardoni R. L. La respuesta inflamatoria en la infección aguda con Trypanosoma cruzi . Medicina. 1997;57(2):227–234. [PubMed] [Google Scholar]
- 133.DosReis G. A. Cell-mediated immunity in experimental Trypanosoma cruzi infection. Parasitology Today. 1997;13(9):335–342. doi: 10.1016/S0169-4758(97)01073-9. [DOI] [PubMed] [Google Scholar]
- 134.Martins G. A., Cardoso M. A. G., Aliberti J. C. S., Silva J. S. Nitric oxide-induced apoptotic cell death in the acute phase of Trypanosoma cruzi infection in mice. Immunology Letters. 1998;63(2):113–120. doi: 10.1016/S0165-2478(98)00066-2. [DOI] [PubMed] [Google Scholar]
- 135.Melo R. C. N., Fabrino D. L., D’Ávila H., Teixeira H. C., Ferreira A. P. Production of hydrogen peroxide by peripheral blood monocytes and specific macrophages during experimental infection with Trypanosoma cruzi in vivo . Cell Biology International. 2003;27(10):853–861. doi: 10.1016/S1065-6995(03)00173-2. [DOI] [PubMed] [Google Scholar]
- 136.Miyahira Y. Trypanosoma cruzi infection from the view of CD8+ T cell immunity—an infection model for developing T cell vaccine. Parasitology International. 2008;57(1):38–48. doi: 10.1016/j.parint.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 137.Padilla A. M., Bustamante J. M., Tarleton R. L. CD8+ T cells in Trypanosoma cruzi infection. Current Opinion in Immunology. 2009;21(4):385–390. doi: 10.1016/j.coi.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Junqueira C., Caetano B., Bartholomeu D. C., et al. The endless race between Trypanosoma cruzi and host immunity: lessons for and beyond Chagas disease. Expert Reviews in Molecular Medicine. 2010;12, article e29 doi: 10.1017/S1462399410001560. [DOI] [PubMed] [Google Scholar]
- 139.Krautz G. M., Kissinger J. C., Krettli A. U. The targets of the lytic antibody response against Trypanosoma cruzi . Parasitology Today. 2000;16(1):31–34. doi: 10.1016/S0169-4758(99)01581-1. [DOI] [PubMed] [Google Scholar]
- 140.Dutra W. O., Rocha M. O. C., Teixeira M. M. The clinical immunology of human Chagas disease. Trends in Parasitology. 2005;21(12):581–587. doi: 10.1016/j.pt.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 141.de Araújo F. F., Corrêa-Oliveira R., Rocha M. O. C., et al. Foxp3+ CD25high CD4+ regulatory T cells from indeterminate patients with Chagas disease can suppress the effector cells and cytokines and reveal altered correlations with disease severity. Immunobiology. 2012;217(8):768–777. doi: 10.1016/j.imbio.2012.04.008. [DOI] [PubMed] [Google Scholar]
- 142.Sartori A. M. C., Lopes M. H., Caramelli B., et al. Simultaneous occurrence of acute myocarditis and reactivated Chagas’ disease in a patient with AIDS. Clinical Infectious Diseases. 1995;21(5):1297–1299. doi: 10.1093/clinids/21.5.1297. [DOI] [PubMed] [Google Scholar]
- 143.Almeida D. R., Carvalho A. C., Branco J. N., et al. Chagas’ disease reactivation after heart transplantation: efficacy of allopurinol treatment. The Journal of Heart and Lung Transplantation. 1996;15(10):988–992. [PubMed] [Google Scholar]
- 144.Tarleton R. L., Grusby M. J., Postan M., Glimcher L. H. Trypanosoma cruzi infection in MHC-deficient mice: Further evidence for the role of both class I- and class II-restricted T cells in immune resistance and disease. International Immunology. 1996;8(1):13–22. doi: 10.1093/intimm/8.1.13. [DOI] [PubMed] [Google Scholar]
- 145.Reina-San-Martín B., Cosson A., Minoprio P. Lymphocyte polyclonal activation: a pitfall for vaccine design against infectious agents. Parasitology Today. 2000;16(2):62–67. doi: 10.1016/S0169-4758(99)01591-4. [DOI] [PubMed] [Google Scholar]
- 146.Reina-San-Martín B., Degrave W., Rougeot C., et al. A B-cell mitogen from a pathogenic trypanosome is a eukaryotic proline racemase. Nature Medicine. 2000;6(8):890–897. doi: 10.1038/78651. [DOI] [PubMed] [Google Scholar]
- 147.Ansa-Addo E., Inal J. T. cruzi interference with host cell membrane integrity triggers the release of Plasma Membrane-derived Vesicles: a mechanism for entry into mammalian cells. The Journal of Immunology. 2010;148:p. 5. [Google Scholar]
- 148.Zambrano-Villa S., Rosales-Borjas D., Carrero J. C., Ortiz-Ortiz L. How protozoan parasites evade the immune response. Trends in Parasitology. 2002;18(6):272–278. doi: 10.1016/S1471-4922(02)02289-4. [DOI] [PubMed] [Google Scholar]
- 149.Cestari I., Ansa-Addo E., Deolindo P., Inal J. M., Ramirez M. I. Trypanosoma cruzi immune evasion mediated by host cell-derived microvesicles. Journal of Immunology. 2012;188(4):1942–1952. doi: 10.4049/jimmunol.1102053. [DOI] [PubMed] [Google Scholar]
- 150.Araújo-Jorge T. C., Waghabi M. C., Soeiro M. D. N. C., Keramidas M., Bailly S., Feige J.-J. Pivotal role for TGF-β in infectious heart disease: the case of Trypanosoma cruzi infection and consequent Chagasic myocardiopathy. Cytokine and Growth Factor Reviews. 2008;19(5-6):405–413. doi: 10.1016/j.cytogfr.2008.08.002. [DOI] [PubMed] [Google Scholar]
- 151.Abu-Shakra M., Buskila D., Shoenfeld Y. Molecular mimicry between host and pathogen: examples from parasites and implication. Immunology Letters. 1999;67(2):147–152. doi: 10.1016/S0165-2478(99)00004-8. [DOI] [PubMed] [Google Scholar]
- 152.Savino W., Do Carmo Leite-de-Moraes M., Hontebeyrie-Joskowicz M., Dardenne M. Studies on the thymus in Chagas’ disease. I. Changes in the thymic microenvironment in mice acutely infected with Trypanosoma cruzi . European Journal of Immunology. 1989;19(9):1727–1733. doi: 10.1002/eji.1830190930. [DOI] [PubMed] [Google Scholar]
- 153.Nardy A. F. F. R., Luiz da Silva Filho J., Pérez A. R., et al. Trans-sialidase from Trypanosoma cruzi enhances the adhesion properties and fibronectin-driven migration of thymocytes. Microbes and Infection. 2013;15(5):365–374. doi: 10.1016/j.micinf.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 154.Latchman Y. E., Liang S. C., Wu Y., et al. PD-L1-deficient mice show that PD-L1 on T cells, antigen-presenting cells, and host tissues negatively regulates T cells. Proceedings of the National Academy of Sciences of the United States of America. 2004;101(29):10691–10696. doi: 10.1073/pnas.0307252101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Terrazas L. I., Montero D., Terrazas C. A., Reyes J. L., Rodríguez-Sosa M. Role of the programmed Death-1 pathway in the suppressive activity of alternatively activated macrophages in experimental cysticercosis. International Journal for Parasitology. 2005;35(13):1349–1358. doi: 10.1016/j.ijpara.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 156.Dulgerian L. R., Garrido V. V., Stempin C. C., Cerbán F. M. Programmed death ligand 2 regulates arginase induction and modifies Trypanosoma cruzi survival in macrophages during murine experimental infection. Immunology. 2011;133(1):29–40. doi: 10.1111/j.1365-2567.2011.03406.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.D’Avila H., Freire-de-Lima C. G., Roque N. R., et al. Host cell lipid bodies triggered by Trypanosoma cruzi infection and enhanced by the uptake of apoptotic cells are associated with prostaglandin E2 generation and increased parasite growth. Journal of Infectious Diseases. 2011;204(6):951–961. doi: 10.1093/infdis/jir432. [DOI] [PubMed] [Google Scholar]
- 158.Puentes S. M., Da Silva R. P., Sacks D. L., Hammer C. H., Joiner K. A. Serum resistance of metacyclic stage Leishmania major promastigotes is due to release of C5b-9. The Journal of Immunology. 1990;145(12):4311–4316. [PubMed] [Google Scholar]
- 159.Hermoso T., Fishelson Z., Becker S. I., Hirschberg K., Jaffe C. L. Leishmanial protein kinases phosphorylate components of the complement system. The EMBO Journal. 1991;10(13):4061–4067. doi: 10.1002/j.1460-2075.1991.tb04982.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Brittingham A., Morrison C. J., McMaster W. R., McGwire B. S., Chang K.-P., Mosser D. M. Role of the Leishmania surface protease gp63 in complement fixation, cell adhesion, and resistance to complement-mediated lysis. Journal of Immunology. 1995;155(6):3102–3111. [PubMed] [Google Scholar]
- 161.Sacks D., Sher A. Evasion of innate immunity by parasitic protozoa. Nature Immunology. 2002;3(11):1041–1047. doi: 10.1038/ni1102-1041. [DOI] [PubMed] [Google Scholar]
- 162.Kulkarni M. M., McMaster W. R., Kamysz E., Kamysz W., Engman D. M., McGwire B. S. The major surface-metalloprotease of the parasitic protozoan, Leishmania, protects against antimicrobial peptide-induced apoptotic killing. Molecular Microbiology. 2006;62(5):1484–1497. doi: 10.1111/j.1365-2958.2006.05459.x. [DOI] [PubMed] [Google Scholar]
- 163.Remaley A. T., Kuhns D. B., Basford R. E., Glew R. H., Kaplan S. S. Leishmanial phosphatase blocks neutrophil O2-production. The Journal of Biological Chemistry. 1984;259(18):11173–11175. [PubMed] [Google Scholar]
- 164.Gueirard P., Laplante A., Rondeau C., Milon G., Desjardins M. Trafficking of Leishmania donovani promastigotes in non-lytic compartments in neutrophils enables the subsequent transfer of parasites to macrophages. Cellular Microbiology. 2008;10(1):100–111. doi: 10.1111/j.1462-5822.2007.01018.x. [DOI] [PubMed] [Google Scholar]
- 165.Tuwaijri A. S. A., Mofleh I. A. A., Mahmoud A. A. Effect of Leishmania major on human polymorphonuclear leucocyte function in vitro . Journal of Medical Microbiology. 1990;32(3):189–193. doi: 10.1099/00222615-32-3-189. [DOI] [PubMed] [Google Scholar]
- 166.Van Zandbergen G., Hermann N., Laufs H., Solbach W., Laskay T. Leishmania promastigotes release a granulocyte chemotactic factor and induce interleukin-8 release but inhibit gamma interferon-inducible protein 10 production by neutrophil granulocytes. Infection and Immunity. 2002;70(8):4177–4184. doi: 10.1128/IAI.70.8.4177-4184.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Wenzel A., Van Zandbergen G. Lipoxin A4 receptor dependent leishmania infection. Autoimmunity. 2009;42(4):331–333. doi: 10.1080/08916930902828239. [DOI] [PubMed] [Google Scholar]
- 168.Faria M. S., Reis F. C. G., Azevedo-Pereira R. L., Morrison L. S., Mottram J. C., Lima A. P. C. A. Leishmania inhibitor of serine peptidase 2 prevents TLR4 activation by neutrophil elastase promoting parasite survival in murine macrophages. The Journal of Immunology. 2011;186(1):411–422. doi: 10.4049/jimmunol.1002175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.John B., Hunter C. A. Immunology: neutrophil soldiers or Trojan horses? Science. 2008;321(5891):917–918. doi: 10.1126/science.1162914. [DOI] [PubMed] [Google Scholar]
- 170.Van Zandbergen G., Bollinger A., Wenzel A., et al. Leishmania disease development depends on the presence of apoptotic promastigotes in the virulent inoculum. Proceedings of the National Academy of Sciences of the United States of America. 2006;103(37):13837–13842. doi: 10.1073/pnas.0600843103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Locksley R. M., Heinzel F. P., Fankhauser J. E., Nelson C. S., Sadick M. D. Cutaneous host defense in leishmaniasis: Interaction of isolated dermal macrophages and epidermal Langerhans cells with the insect-stage promastigote. Infection and Immunity. 1988;56(2):336–342. doi: 10.1128/iai.56.2.336-342.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Bogdan C., Donhauser N., Döring R., Röllinghoff M., Diefenbach A., Rittig M. G. Fibroblasts as host cells in latent leishmaniosis. Journal of Experimental Medicine. 2000;191(12):2121–2129. doi: 10.1084/jem.191.12.2121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Bogdan C., Röllinghoff M. The immune response to Leishmania: mechanisms of parasite control and evasion. International Journal for Parasitology. 1998;28(1):121–134. doi: 10.1016/S0020-7519(97)00169-0. [DOI] [PubMed] [Google Scholar]
- 174.Descoteaux A., Turco S. J. Glycoconjugates in Leishmania infectivity. Biochimica et Biophysica Acta. 1999;1455(2-3):341–352. doi: 10.1016/S0925-4439(99)00065-4. [DOI] [PubMed] [Google Scholar]
- 175.Shio M. T., Hassani K., Isnard A., et al. Host cell signalling and leishmania mechanisms of evasion. Journal of Tropical Medicine. 2012;2012:14. doi: 10.1155/2012/819512.819512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Bogdan C., Rollinghoff M., Solbach W. Evasion strategies of Leishmania parasites. Parasitology Today. 1990;6(6):183–187. doi: 10.1016/0169-4758(90)90350-D. [DOI] [PubMed] [Google Scholar]
- 177.Gomez M. A., Contreras I., Hallé M., Tremblay M. L., McMaster R. W., Olivier M. Leishmania GP63 alters host signaling through cleavage-activated protein tyrosine phosphatases. Science Signaling. 2009;2(90):p. ra58. doi: 10.1126/scisignal.2000213. [DOI] [PubMed] [Google Scholar]
- 178.Ghosh S., Bhattacharyya S., Das S., et al. Generation of ceramide in murine macrophages infected with Leishmania donovani alters macrophage signaling events and aids intracellular parasitic survival. Molecular and Cellular Biochemistry. 2001;223(1-2):47–60. doi: 10.1023/A:1017996609928. [DOI] [PubMed] [Google Scholar]
- 179.Ghosh S., Bhattacharyya S., Sirkar M., et al. Leishmania donovani suppresses activated protein 1 and NF-κB activation in host macrophages via ceramide generation: involvement of extracellular signal-regulated kinase. Infection and Immunity. 2002;70(12):6828–6838. doi: 10.1128/IAI.70.12.6828-6838.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Gregory D. J., Godbout M., Contreras I., Forget G., Olivier M. A novel form of NF-κB is induced by Leishmania infection: involvement in macrophage gene expression. European Journal of Immunology. 2008;38(4):1071–1081. doi: 10.1002/eji.200737586. [DOI] [PubMed] [Google Scholar]
- 181.Neves B. M., Silvestre R., Resende M., et al. Activation of phosphatidylinositol 3-kinase/akt and impairment of nuclear factor-κB: Molecular mechanisms behind the arrested maturation/activation state of leishmania infantum-infected dendritic cells. The American Journal of Pathology. 2010;177(6):2898–2911. doi: 10.2353/ajpath.2010.100367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Forget G., Gregory D. J., Olivier M. Proteasome-mediated degradation of STAT1α following infection of macrophages with Leishmania donovani . The Journal of Biological Chemistry. 2005;280(34):30542–30549. doi: 10.1074/jbc.M414126200. [DOI] [PubMed] [Google Scholar]
- 183.Olivier M., Gregory D. J., Forget G. Subversion mechanisms by which Leishmania parasites can escape the host immune response: a signaling point of view. Clinical Microbiology Reviews. 2005;18(2):293–305. doi: 10.1128/CMR.18.2.293-305.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Barrett M. P., Mottram J. C., Coombs G. H. Recent advances in identifying and validating drug targets in trypanosomes and leishmanias. Trends in Microbiology. 1999;7(2):82–88. doi: 10.1016/S0966-842X(98)01433-4. [DOI] [PubMed] [Google Scholar]
- 185.Lee S. H., Stephens J. L., Paul K. S., Englund P. T. Fatty acid synthesis by elongases in trypanosomes. Cell. 2006;126(4):691–699. doi: 10.1016/j.cell.2006.06.045. [DOI] [PubMed] [Google Scholar]
- 186.Michels P. A. M., Bringaud F., Herman M., Hannaert V. Metabolic functions of glycosomes in trypanosomatids. Biochimica et Biophysica Acta. 2006;1763(12):1463–1477. doi: 10.1016/j.bbamcr.2006.08.019. [DOI] [PubMed] [Google Scholar]
- 187.El Kouni M. H. Potential chemotherapeutic targets in the purine metabolism of parasites. Pharmacology and Therapeutics. 2003;99(3):283–309. doi: 10.1016/S0163-7258(03)00071-8. [DOI] [PubMed] [Google Scholar]
- 188.Müller S., Liebau E., Walter R. D., Krauth-Siegel R. L. Thiol-based redox metabolism of protozoan parasites. Trends in Parasitology. 2003;19(7):320–328. doi: 10.1016/S1471-4922(03)00141-7. [DOI] [PubMed] [Google Scholar]
- 189.Hammarton T. C., Clark J., Douglas F., Boshart M., Mottram J. C. Stage-specific differences in cell cycle control in Trypanosoma brucei revealed by RNA interference of a mitotic cyclin. The Journal of Biological Chemistry. 2003;278(25):22877–22886. doi: 10.1074/jbc.M300813200. [DOI] [PubMed] [Google Scholar]
- 190.Werbovetz K. A., Morgan R. E. Selective lead compounds against kinetoplastid tubulin. Advances in Experimental Medicine and Biology. 2008;625:33–47. doi: 10.1007/978-0-387-77570-8-4. [DOI] [PubMed] [Google Scholar]
- 191.Savoia D., Allice T., Tovo P.-A. Antileishmanial activity of HIV protease inhibitors. International Journal of Antimicrobial Agents. 2005;26(1):92–94. doi: 10.1016/j.ijantimicag.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 192.Nkemgu-Njinkeng J., Rosenkranz V., Wink M., Steverding D. Antitrypanosomal activities of proteasome inhibitors. Antimicrobial Agents and Chemotherapy. 2002;46(6):2038–2040. doi: 10.1128/AAC.46.6.2038-2040.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Glenn R. J., Pemberton A. J., Royle H. J., et al. Trypanocidal effect of alpha′,beta′-epoxyketones indicates that trypanosomes are particularly sensitive to inhibitors of proteasome trypsin-like activity. International Journal of Antimicrobial Agents. 2004;24(3):286–289. doi: 10.1016/j.ijantimicag.2004.02.023. [DOI] [PubMed] [Google Scholar]
- 194.Wilkinson S. R., Taylor M. C., Horn D., Kelly J. M., Cheeseman I. A mechanism for cross-resistance to nifurtimox and benznidazole in trypanosomes. Proceedings of the National Academy of Sciences of the United States of America. 2008;105(13):5022–5027. doi: 10.1073/pnas.0711014105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Patterson S., Wyllie S. Nitro drugs for the treatment of trypanosomatid diseases: past, present, and future prospects. Trends in Parasitology. 2014;30(6):289–298. doi: 10.1016/j.pt.2014.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Bahia M. T., de Andrade I. M., Martins T. A. F., et al. Fexinidazole: a potential new drug candidate for chagas disease. PLoS Neglected Tropical Diseases. 2012;6(11) doi: 10.1371/journal.pntd.0001870.e1870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Bahia M. T., Nascimento A. F., Mazzeti A. L., et al. Antitrypanosomal activity of fexinidazole metabolites, potential new drug candidates for chagas disease. Antimicrobial Agents and Chemotherapy. 2014;58:4362–4370. doi: 10.1128/AAC.02754-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Zhou Y., Messier N., Ouellette M., Rosen B. P., Mukhopadhyay R. Leishmania major LmACR2 is a pentavalent antimony reductase that confers sensitivity to the drug Pentostam. The Journal of Biological Chemistry. 2004;279(36):37445–37451. doi: 10.1074/jbc.M404383200. [DOI] [PubMed] [Google Scholar]
- 199.Amato V. S., Tuon F. F., Bacha H. A., Neto V. A., Nicodemo A. C. Mucosal leishmaniasis. Current scenario and prospects for treatment. Acta Tropica. 2008;105(1):1–9. doi: 10.1016/j.actatropica.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 200.Golenser J., Domb A. New formulations and derivatives of amphotericin B for treatment of leishmaniasis. Mini-Reviews in Medicinal Chemistry. 2006;6(2):153–162. doi: 10.2174/138955706775476037. [DOI] [PubMed] [Google Scholar]
- 201.Chappuis F., Sundar S., Hailu A., et al. Visceral leishmaniasis: what are the needs for diagnosis, treatment and control? Nature Reviews Microbiology. 2007;5(11):873–882. doi: 10.1038/nrmicro1748. [DOI] [PubMed] [Google Scholar]
- 202.Chugh P., Bradel-Tretheway B., Monteiro-Filho C. M. R., et al. Akt inhibitors as an HIV-1 infected macrophage-specific anti-viral therapy. Retrovirology. 2008;5, article 11 doi: 10.1186/1742-4690-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Berman J. J. Treatment of leishmaniasis with miltefosine: 2008 status. Expert Opinion on Drug Metabolism and Toxicology. 2008;4(9):1209–1216. doi: 10.1517/17425255.4.9.1209. [DOI] [PubMed] [Google Scholar]
- 204.Sun T., Zhang Y. Pentamidine binds to tRNA through non-specific hydrophobic interactions and inhibits aminoacylation and translation. Nucleic Acids Research. 2008;36(5):1654–1664. doi: 10.1093/nar/gkm1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Chawla B., Jhingran A., Panigrahi A., Stuart K. D., Madhubala R. Paromomycin affects translation and vesicle-mediated trafficking as revealed by proteomics of paromomycin -susceptible -resistant leishmania donovani . PLoS ONE. 2011;6(10) doi: 10.1371/journal.pone.0026660.e26660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Soto J., Tolado J., Valda L., et al. Treatment of bolivian mucosal leishmaniasis with miltefosine. Clinical Infectious Diseases. 2007;44(3):350–356. doi: 10.1086/510588. [DOI] [PubMed] [Google Scholar]
- 207.Baginski M., Czub J. Amphotericin B and its new derivatives—mode of action. Current Drug Metabolism. 2009;10(5):459–469. doi: 10.2174/138920009788898019. [DOI] [PubMed] [Google Scholar]
- 208.Sundar S., Chakravarty J. Leishmaniasis: an update of current pharmacotherapy. Expert Opinion on Pharmacotherapy. 2013;14(1):53–63. doi: 10.1517/14656566.2013.755515. [DOI] [PubMed] [Google Scholar]
- 209.Sundar S., Sinha P. K., Dixon S. A., et al. Pharmacokinetics of oral sitamaquine taken with or without food and safety and efficacy for treatment of visceral leishmaniais: a randomized study in Bihar, India. The American Journal of Tropical Medicine and Hygiene. 2011;84(6):892–900. doi: 10.4269/ajtmh.2011.10-0409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Loiseau P. M., Cojean S., Schrével J. Sitamaquine as a putative antileishmanial drug candidate: from the mechanism of action to the risk of drug resistance. Parasite. 2011;18(2):115–119. doi: 10.1051/parasite/2011182115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Urbina J. A. Lipid biosynthesis pathways as chemotherapeutic targets in kinetoplastid parasites. Parasitology. 1997;114:S91–S99. [PubMed] [Google Scholar]
- 212.Lepesheva G. I., Villalta F., Waterman M. R. Targeting Trypanosoma cruzi Sterol 14α-demethylase (CYP51) Advances in Parasitology. 2011;75:65–87. doi: 10.1016/B978-0-12-385863-4.00004-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.de Souza W., Rodrigues J. C. Sterol biosynthesis pathway as target for anti-trypanosomatid drugs. Interdisciplinary Perspectives on Infectious Diseases. 2009;2009:19. doi: 10.1155/2009/642502.642502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Khatami A., Firooz A., Gorouhi F., Dowlati Y. Treatment of acute Old World cutaneous leishmaniasis: a systematic review of the randomized controlled trials. Journal of the American Academy of Dermatology. 2007;57(2):335.e1–335.e29. doi: 10.1016/j.jaad.2007.01.016. [DOI] [PubMed] [Google Scholar]
- 215.Ramanathan R., Talaat K. R., Fedorko D. P., Mahanty S., Nash T. E. A species-specific approach to the use of non-antimony treatments for cutaneous leishmaniasis. The American Journal of Tropical Medicine and Hygiene. 2011;84(1):109–117. doi: 10.4269/ajtmh.2011.10-0437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Sousa A. Q., Frutuoso M. S., Moraes E. A., Pearson R. D., Pompeu M. M. L. High-dose oral fluconazole therapy effective for cutaneous leishmaniasis due to leishmania (vianna) Braziliensis . Clinical Infectious Diseases. 2011;53(7):693–695. doi: 10.1093/cid/cir496. [DOI] [PubMed] [Google Scholar]
- 217.Duschak V. G. A decade of targets and patented drugs for chemotherapy of chagas disease. Recent Patents on Anti-Infective Drug Discovery. 2011;6(3):216–259. doi: 10.2174/157489111796887864. [DOI] [PubMed] [Google Scholar]
- 218.Buckner F. S., Urbina J. A. Recent developments in sterol 14-demethylase inhibitors for Chagas disease. International Journal for Parasitology: Drugs and Drug Resistance. 2012;2:236–242. doi: 10.1016/j.ijpddr.2011.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Molina I., Gómez I Prat J., Salvador F., et al. Randomized trial of posaconazole and benznidazole for chronic Chagas’ disease. The New England Journal of Medicine. 2014;370(20):1899–1908. doi: 10.1056/NEJMoa1313122. [DOI] [PubMed] [Google Scholar]
- 220.Chamond N., Goytia M., Coatnoan N., et al. Trypanosoma cruzi proline racemases are involved in parasite differentiation and infectivity. Molecular Microbiology. 2005;58(1):46–60. doi: 10.1111/j.1365-2958.2005.04808.x. [DOI] [PubMed] [Google Scholar]
- 221.Berneman A., Montout L., Goyard S., et al. Combined approaches for drug design points the way to novel proline racemase inhibitor candidates to fight chagas’ disease. PLoS ONE. 2013;8(4) doi: 10.1371/journal.pone.0060955.e60955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Pozio E. Hiqhly active anti-retroviral therapy and opportunistic protozoan infections. Parassitologia. 2004;46(1-2):89–93. [PubMed] [Google Scholar]
- 223.Abbenante G., Fairlie D. P. Protease inhibitors in the clinic. Medicinal Chemistry. 2005;1(1):71–104. doi: 10.2174/1573406053402569. [DOI] [PubMed] [Google Scholar]
- 224.Santos L. O., Vitório B. S., Branquinha M. H., Pedroso e silva C. M., Santos A. L. S., D’avila-Levy C. M. Nelfinavir is effective in inhibiting the multiplication and aspartic peptidase activity of Leishmania species, including strains obtained from HIV-positive patients. Journal of Antimicrobial Chemotherapy. 2013;68(2):348–353. doi: 10.1093/jac/dks410.dks410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Santos L. O., Garcia-Gomes A. S., Catanho M., et al. Aspartic peptidases of human pathogenic trypanosomatids: perspectives and trends for chemotherapy. Current Medicinal Chemistry. 2013;20(25):3116–3133. doi: 10.2174/0929867311320250007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Croft S. L., Sundar S., Fairlamb A. H. Drug resistance in leishmaniasis. Clinical Microbiology Reviews. 2006;19(1):111–126. doi: 10.1128/CMR.19.1.111-126.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Martinelli A., Moreira R., Cravo P. V. L. Malaria combination therapies: advantages and shortcomings. Mini-Reviews in Medicinal Chemistry. 2008;8(3):201–212. doi: 10.2174/138955708783744092. [DOI] [PubMed] [Google Scholar]
- 228.Silver L. L. Multi-targeting by monotherapeutic antibacterials. Nature Reviews Drug Discovery. 2007;6(1):41–55. doi: 10.1038/nrd2202. [DOI] [PubMed] [Google Scholar]
- 229.Petrelli A., Giordano S. From single- to multi-target drugs in cancer therapy: when aspecificity becomes an advantage. Current Medicinal Chemistry. 2008;15(5):422–432. doi: 10.2174/092986708783503212. [DOI] [PubMed] [Google Scholar]
- 230.Roatt B. M., Aguiar-Soares R. D., Coura-Vital W., et al. Immunotherapy and immunochemotherapy in visceral leishmaniasis: promising treatments for this neglected disease. Frontiers in Immunology. 2014;5:p. 272. doi: 10.3389/fimmu.2014.00272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Joshi J., Malla N., Kaur S. A comparative evaluation of efficacy of chemotherapy, immunotherapy and immunochemotherapy in visceral leishmaniasis-an experimental study. Parasitology International. 2014;63(4):612–620. doi: 10.1016/j.parint.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 232.Monge-Maillo B., López-Vélez R. Therapeutic options for old world cutaneous leishmaniasis and new world cutaneous and mucocutaneous leishmaniasis. Drugs. 2013;73(17):1889–1920. doi: 10.1007/s40265-013-0132-1. [DOI] [PubMed] [Google Scholar]
- 233.Khamesipour A. Therapeutic vaccines for leishmaniasis. Expert Opinion on Biological Therapy. 2014;31:1–9. doi: 10.1517/14712598.2014.945415. [DOI] [PubMed] [Google Scholar]