Abstract
Aim:
This paper describes how in a problem-based learning (PBL) medical curriculum, having identified the learning outcomes, problems can be developed from real-life events for teaching-learning clinical pharmacology topics for which PBL cases might be inadequate. Such problems can be very interesting and educational.
Methodology:
Using the story of the development and withdrawal of rofecoxib (Vioxx®), we developed a problem for undergraduate medical students to address important issues related to clinical pharmacology and therapeutics such as new drug development, preclinical testing, clinical trials, adverse drug reactions, professionalism, and critical appraisal of literature. These topics would otherwise be difficult to address in patient-based problems.
Results:
The evaluation of the problem based on pooled feedback from 57 tutorial groups, each comprising 8–10 students, collected over 5 years, supported the effectiveness of the problem.
Conclusion:
A systematic approach described in this paper can be used for the development and validation of educational material for introducing focal topics of pharmacology/clinical pharmacology integrated with other disciplines in innovative medical (and other health profession) curricula.
KEY WORDS: clinical pharmacology, new drug development, patient safety, problem-based learning, problem designing
Introduction
Teaching-learning is a dynamic process and depending on the subject it can be accomplished by various ways and means. Problem-based learning (PBL) is a student-centered approach in which students learn through analyzing and solving problems. The goals of PBL are to help the students develop flexible knowledge, effective problem-solving skills, self-directed learning, effective collaboration skills, and intrinsic motivation.[1] PBL is a style of active learning and represents a paradigm shift from traditional teaching and learning philosophy,[2] which is more often lecture-based.
Problem-based learning comprises problems that can be solved in many different ways.[3] Working in groups, students identify what they already know, what they need to know, and how and where to access new information that may lead to resolution of the problem. The role of the tutor is to facilitate learning by supporting, guiding, and monitoring the learning process.[4,5]
Problem-based learning addresses the need to promote lifelong learning through the process of inquiry and constructivist learning.[4] PBL can be considered a constructivist approach to instruction, emphasizing collaborative and self-directed learning and being supported by flexible teacher scaffolding.[6] Yew and Schmidt,[7] Schmidt et al.,[4] and Hung[2] elaborate on the cognitive constructivist process of PBL.
Thus problems, also referred to as tasks, are pivotal in PBL. They drive students’ learning activities. This central role places high demands on the quality of problems which in turn affects the quality of the small group process and students’ educational achievements.[8] In general, problems are composed of a relatively neutral description of phenomena or events that appear to be related in some way and require further explanation.[9] These phenomena can be physiological, biological, psychological or social. Students work on problems in small tutorial groups. They attempt to find explanations, building on previously acquired knowledge.
A problem can be of different types: explanation problem, discussion problem, strategy problem, study problem, application problem, and multi-level problem.[8] Most of these are based on clinical scenarios and are effective in triggering the generation of learning objectives covering many areas of clinical pharmacology. However, there are topics which are not addressed because they are not within the domain of a typical clinical scenario. One good example is the development of a new drug. This is an area that is often under-emphasized in most medical curricula. It is important to sensitize students to issues such as the prerequisites for clinical evaluation of new drugs in humans, phases and types of clinical trials, ethical and legal aspects of testing drugs in humans, adverse drug reactions, postmarketing surveillance, drug safety and drug-related injuries. With these learning objectives in mind, “life-cycle of a drug” was introduced in the undergraduate medical curriculum during the preclerkship phase in the last unit (unit IX): “Medicine, science and technology.” It is important for medical students to be aware of what is involved in terms of effort, time, resources, and professionalism in the development of a new drug. It helps in making rational therapeutic decisions.
Patient safety is a relatively new discipline and introducing any new material into an existing curriculum is always challenging.[10] Medicines have proved to be very beneficial for treating illness and preventing diseases. This success has resulted in a dramatic increase in medication use in recent times. Unfortunately, this increase in use has also brought with it an increase in hazards, error and adverse events associated with medication use. Several instructional strategies have been proposed to teach medical students about medication safety, and a combination of approaches is likely to be most effective. The various options include PBL, interactive lectures, small group discussions, practical workshops, tutorials, project work including tasks to be undertaken in the clinical environment and at the bedside, online learning packages, reading and case analysis.[11]
Several organizations such as World Health Organization (WHO), Association of American Medical Colleges, and General Medical Council have endorsed increased teaching of patient safety and quality improvement during medical school. Despite policy consensus, few medical schools have implemented curricula addressing these topics, and there is little evidence on the best method to teach them.[11]
Perhaps the vast majority of literature on drug safety reports investigations of postgraduate teaching of these topics. A recent systematic review of patient safety curricula in medical schools demonstrated that most teaching about patient safety occurred during the 3rd year, varied in length and was taught by clinicians, ethicists, and medical education experts.[12]
Current teaching does not meet the goals established by the WHO and includes no controlled assessment of a standardized curriculum. A recent study examined students’ preferences on timing, setting, and pedagogical methods for teaching these topics.[13]
To address all these concerns related to new drug development in a PBL setting, we thought of using a real-life event to generate relevant learning objectives. The story of rofecoxib (Vioxx®), a nonsteroidal anti-inflammatory drug with selective inhibition of cycloxygenase-2 appeared very appealing as it had all the elements and issues discussed earlier. We used it as a platform, developed it into a problem for students to trigger the necessary learning objectives and satisfy the requirements of self-directed learning in a PBL curriculum during the preclerkship phase of the medical program. In this paper, we describe our experience on these educational issues: problem development, implementation, and evaluation.
Methodology
Setting
The Arabian Gulf University (AGU) in the Kingdom of Bahrain is a regional leader in PBL. The PBL curriculum of the College of Medicine and Medical Sciences (CMMS) is a 6-year program leading to the MD degree and is divided into three phases, as shown in the curriculum map [Table 1]: Phase I (premedical), Phase II (preclerkship) and Phase III (clerkship). A comprehensive description of the medical curriculum of CMMS, AGU has been reported.[14] PBL is the main strategy for curriculum implementation during the preclerkship phase.
Table 1.
Medical curriculum map of the AGU
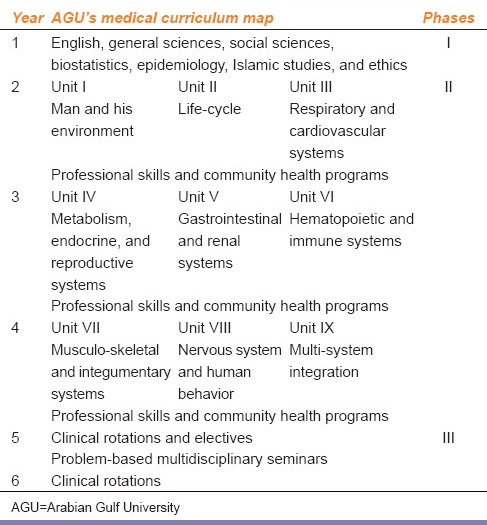
Phase II has 9 units, of which units III–VIII are system-based while units I, II, and IX are more conceptual and integrative. In each unit, problems are discussed in small tutorial groups to generate learning objectives in session 1. During the week, students undertake self-study supplemented with structured educational activities such as resource sessions, laboratory sessions, professional clinical skills training, community health activity, and interaction with faculty members. In session 2, the group assembles again, and students present and discuss what they have learned. In the beginning of the next week, students review the problem and provide feedback about the previous week's problem. At the end of each unit, there is an end-unit summative exam.
Problem Designing
Development of a problem starts with expected learning outcomes and learning objectives within the broader framework of the unit and the entire curriculum. We retrieved the literature available on the internet and gathered information about Vioxx®, its development, trials, marketing, adverse effects, withdrawal from the market, and the legal and ethical ramifications. Keeping in mind the expected learning outcomes and objectives [Table 2], the information was organized into a problem: “Life-cycle of a drug” consisting of a series of triggers to encompass the different stages and steps involved in the process of new drug development [Table 3].[15,16,17,18]
Table 2.
The intended learning needs of “life-cycle of a drug” problem
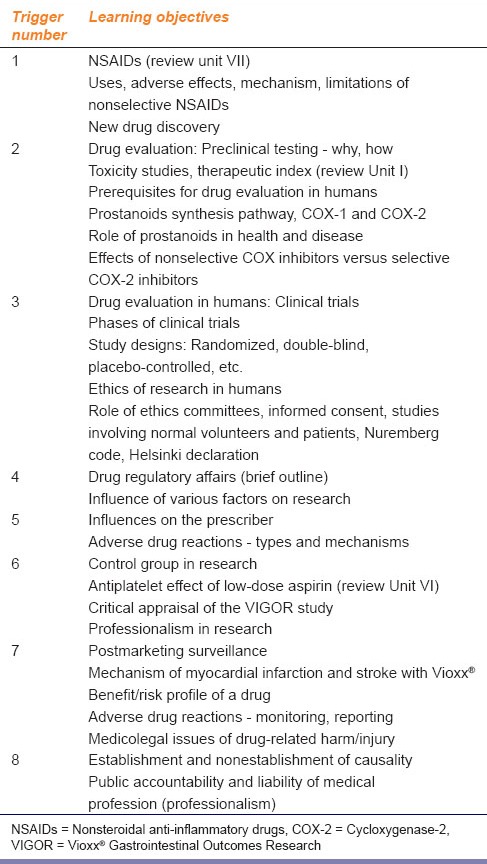
Table 3.
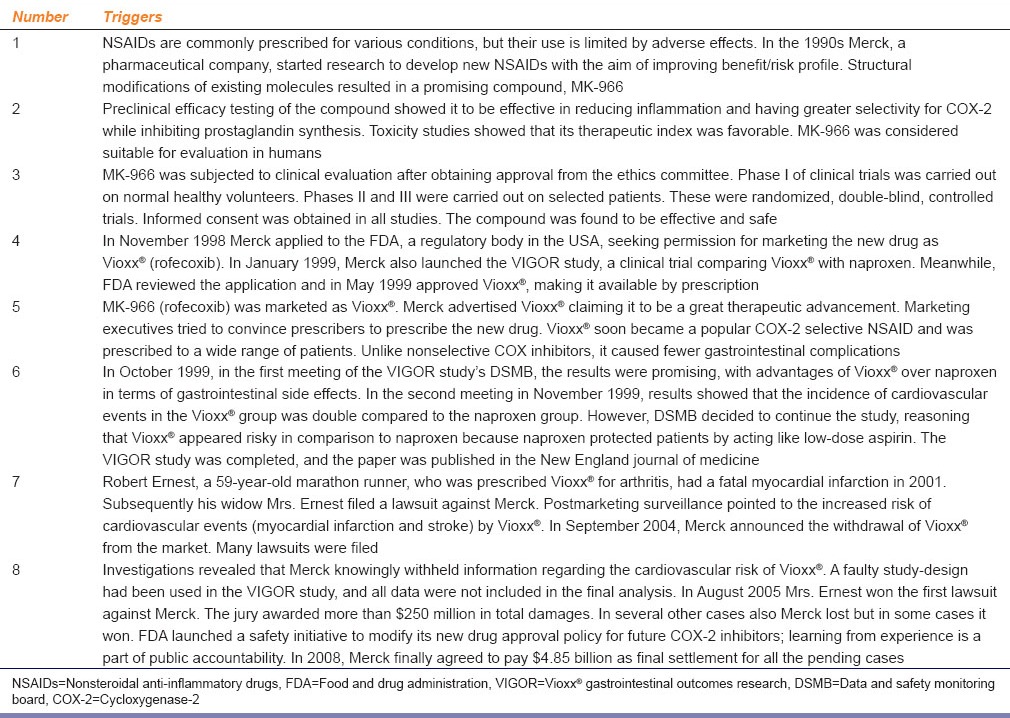
Problem Implementation
In session 1, students discussed the problem in small groups facilitated by a faculty tutor. Students took turns in reading the triggers. Any difficult terms were clarified, and discussion focused on the events in the triggers, revisiting previously acquired knowledge, and more importantly, what new knowledge was required to fully understand the contents of a trigger. They came up with learning objectives as generated by each trigger [Table 2].
After completing the discussion in session 1, students devoted themselves to self-study about the learning objectives, acquiring new knowledge. This was supplemented with a mini problem on Fen-Phen® (an appetite suppressant withdrawn from the market in the 90s due to concerns about its safety), MCQs, interaction with resource people and attending structured resource sessions, and a workshop on medication errors and patient safety.
In session 2, each tutorial group gathered again and students shared the knowledge acquired about various learning objectives with each other.
Problem Evaluation
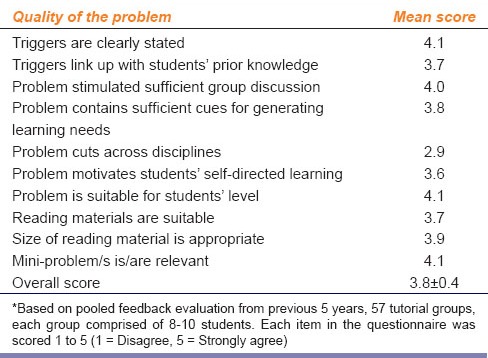
In the following week, the problem was reviewed, and queries were addressed. Each tutorial group of students, along with respective tutors, provided feedback about different aspects of the problem and the educational activities of the week as a whole. Problem evaluation feedback was provided by each group of students in discussion with the tutor by completing a questionnaire with close-ended and open-ended items [Table 4]. The close-ended items were scored from 1 to 5 (1 = disagree, 5 = strongly agree). Each year, based on the previous year's feedback, the problem is modified.
Table 4.
Problem evaluation*
Results
The intended learning needs are presented in Table 2. The problem triggers that were created[15,16,17,18] to bring out these learning needs are presented in Table 3. Feedback pertaining to various aspects of the problem was collected over a period of 5 years; provided by 57 tutorial groups, each comprising 8–10 students. The pooled results of problem evaluation are presented in Table 4. As can be seen, overall the problem has been perceived positively.
Discussion
There are concerns that graduating doctors are not competent in prescribing skills. Several approaches have been used in addressing this issue both from curriculum design and implementation perspectives, in traditional as well as innovative medical curricula. The speed with which new technology, including drugs, is introduced into health care treatments demonstrates the constant change in health care which, in turn, is changing the nature of the work or tasks undertaken by different health professionals. Taking into account the workplace context, it is necessary to bring authenticity to the learning experience and prepare the students for the work environment they will be entering.
It is important to delineate the distinction between PBL and case-based learning (CBL). There are fundamental differences in terms of educational philosophy, curriculum design, and implementation between PBL and CBL.[19,20] Hence, the approach to designing problems versus cases differs.
There are two guiding principles in developing problems. First, the problems must raise the concepts and principles relevant to the content domain. Second, the problem must be real. Because the students are open to explore all discussions of the problem, there is real difficulty in creating a rich problem with a consistent set of information. Furthermore, real problems tend to engage learners more. It is also essential to know the outcome of the problem.[21] The problem on “life-cycle of a drug” met these criteria.
The process of problem development, implementation, and evaluation is quite elaborate. Several elements need to be considered in problem design: the learning outcomes (educational objectives), the type of problem and its format. A written problem is the most common format for trigger material; the triggers should be relevant, interesting and provoke discussion in small groups.
The curriculum committee, in consultation with different departments, identified the core learning objectives in each discipline. Because of the integrated and spiral nature of PBL curriculum different departments (Epidemiology, Biochemistry, Family Medicine, Professionalism, Pharmacology, and Therapeutics) worked together in contributing to the problem. Resource people from different disciplines met and contributed to problem development.
Core learning objectives of basic and clinical pharmacology for undergraduate medical students have been identified and listed. Most of these relate to different organ systems and important disease conditions. We noticed a gap: new drug development was not being addressed, and there was no way to introduce it through the existing problems. A new problem was developed in which students could understand the different stages and issues involved in the process of drug development.
The story of Vioxx® appeared very appealing as it had all the elements of new drug development. It went even further: it brought out several other important issues, such as ethics of clinical research, particularly of clinical trials, patient safety, and legal implications of drug-induced harm. The problem was placed in unit IX towards the end of the preclerkship phase.
The process of developing new drugs generally starts with the identification or development of a new lead chemical molecule. This is brought out in trigger 1 against a backdrop of nonsteroidal anti-inflammatory drugs (NSAIDs), their widespread use, their limitations, and the need for better drugs. Students reviewed NSAIDs, which they had studied in previous problems, for example, in unit I (inflammation), unit III (pulmonary embolism), unit V (peptic ulcer disease), unit VI (immunothrombocytopenic purpura) and unit VII (arthritis). They discussed their mechanism of action and adverse effects. This raised the topic of the need for new NSAIDs and how new drugs are discovered and developed.
The next step in new drug development is testing the new compound. Trigger 2 is about preclinical testing of the new compound MK-966. It raised discussion about the preclinical testing of new drugs in animals as a prerequisite for testing them in humans. Students discussed the ethics of testing in animals and prevention of cruelty to animals. The concept of the therapeutic index also emerged. Success in animal testing leads to the emergence of an investigational new drug (IND).
Trigger 3 is about testing the IND in humans. Students are introduced to clinical trial Phases I, II and III. Consent for participation in trials, ethics, and strategies to minimize bias are also discussed. Students who were better informed also raised topics from history, e.g., unethical testing on prisoners of war or on vulnerable people.
Once a drug has been successfully tested in humans, it is time for new drug application (NDA). In trigger 4 discussion is about the prerequisites for NDA, drug regulatory affairs in general, generic name and brand name, evidence-based medicine and critical appraisal of the literature.
The stage is now set for marketing the new drug. In trigger 5, MK-966 (Rofecoxib) was marketed as Vioxx® and Merck actively advertised their new pharmaceutical product. Unlike nonselective COX inhibitors, it caused fewer gastrointestinal adverse effects. Students discussed the necessity for new drugs, various influences on the prescriber, and drug nomenclature. Advantages and disadvantages of prescribing by generic versus brand names were also discussed. The topic of adverse drug reactions was revisited.
Trigger 6 elicited extensive discussion among students. Results from the Vioxx® Gastrointestinal Outcomes Research (VIGOR) study were promising, with advantages of Vioxx® over naproxen, a nonselective NSAID, in terms of gastrointestinal adverse effects. But later results showed that the incidence of cardiovascular events in the Vioxx® group was double compared to the naproxen group. However, reasoning that Vioxx® appeared risky in comparison to naproxen because naproxen protected patients by acting like low-dose aspirin, the company decided to continue the study. It is a turning point, and Merck could have avoided litigations associated with Vioxx® if only it had taken the alternative decision to discontinue the study. The VIGOR study was completed, and the paper was published in the New England Journal of Medicine.[22] This trigger raised important issues of ethics and professionalism in research. No doubt developing new drugs is an expensive affair, but efficacy and safety are of utmost importance. Other topics raised in this trigger were the use of controls in study design, type of controls, conflict of interests, and bias in data interpretation and nondisclosure.
Trigger 7 is about one of the first reported deaths associated with the use of Vioxx® and the subsequent lawsuit against Merck. Postmarketing surveillance and reporting (Phase IV) is the last (but not the least) step in new drug development. Students compared it to the previous phases and noted important differences. In this story, there was an increased risk of cardiovascular events (myocardial infarction and stroke) associated with Vioxx®. In September 2004, Merck announced the withdrawal of Vioxx® from the market. Several lawsuits followed. Revisiting adverse drug reactions, there was a discussion about the possible reasons for myocardial infarction and stroke associated with Vioxx®. The role of evidence-based medicine, medicolegal and ethical issues also emerged.
Finally, we have the results of legal investigations into the Vioxx® story. Trigger 8 is about professionalism in research and drug development. It triggered interesting discussions: publication bias, critical appraisal of the scientific literature, and public accountability and liability of the medical profession. It was also pointed out that the company did win some legal cases, because in other cases with multiple diseases and multi-drug therapy, it can be impossible to link an adverse event to one particular cause with certainty due to nonestablishment of causality.[23]
Along with the main problem, mini-problems and MCQs are also given to the students for elaboration and self-assessment. Mini-problems are used for elaboration or for presentation in different clinical settings or contexts.
In general, there are two approaches to measuring the quality of problems. One approach is to evaluate whether students are able to generate the same learning goals as intended by the curriculum. The degree of congruence between the two is considered to be reflective of problem effectiveness.[24,25,26] An alternative approach is the administration of self-report rating scale.[19,27,28] The problem “life-cycle of a drug” is a dynamic one. Each year, based on the previous year's feedback, it is modified. The feedback received from students over the years has been very positive and encouraging. The problem was perceived positively with a mean overall score of 3.8 ± 0.4 out of 5. All close-ended items scored 3 and above except item no. 5: “Problem cuts across disciplines” which scored 2.9. It seems most groups perceived the problem as mainly pharmacology/clinical pharmacology discipline-oriented. It is quite understandable because the nature of the problem is such. Nevertheless, the problem does integrate with some other discipline, e.g., biochemistry, evidence-based medicine, epidemiology, and professionalism. According to the open-ended comments by various groups, the problem was perceived as very interesting, informative, and an eye-opener. The triggers generated interesting discussions which were much enjoyed by the learners. It indicates the effectiveness and success of this innovative approach in teaching-learning such important topics of clinical pharmacology.
Conclusion
In a PBL curriculum, having identified the learning outcomes, problems can be developed from real-life events for teaching-learning clinical pharmacology topics for which patient-based scenarios might be inadequate. Such problems can be very interesting and educational, as described in this paper. A systematic approach described in this paper can be used for the development and validation of educational material for introducing focal topics of pharmacology/clinical pharmacology integrated with other disciplines in innovative medical (and other health profession) curricula.
Note:
The World Federation of Medical Education and the Medical Council of India have recommended the introduction of innovative medical curricula. PBL has gained rapid acceptance, mostly in North America. Other variants like Case-Based Learning and Team-Based Learning are also used in some schools across the world. These being relatively novel concepts in India, we chose to publish this article to create awareness among the readers about the trends in health professions education (including pharmacology education). A note of caution, however, against adopting these methods without evaluating its feasibility and validity in the Indian context.
Chief Editor
Footnotes
Source of Support: Nill.
Conflict of Interest: No.
References
- 1.Silver CE. Problem-based learning: What and how do students learn? Educ Psychol Rev. 2004;16:235–66. [Google Scholar]
- 2.Hung W. Theory to reality: A few issues in implementing problem-based learning. Educ Technol Res Dev. 2011;59:529–52. [Google Scholar]
- 3.Mara C, Milena VZ. Problem-based instruction in mathematics and its impact on the cognitive results of the students and on affective-motivational aspects. Educ Stud. 2009;35:297–310. [Google Scholar]
- 4.Schmidt HG, Rotgans JI, Yew EH. The process of problem-based learning: What works and why. Med Educ. 2011;45:792–806. doi: 10.1111/j.1365-2923.2011.04035.x. [DOI] [PubMed] [Google Scholar]
- 5.Barrows HS. Problem-based learning in medicine and beyond: A brief overview. New Dir Teach Learn. 1996;68:3–12. [Google Scholar]
- 6.Schmidt HG, Loyens SM, van Gog T, Paas F. Problem-based learning is compatible with human cognitive architecture: Commentary on Kirschner, Sweller, and Clark (2006) Educ Psychol. 2007;42:91–7. [Google Scholar]
- 7.Yew EH, Schmidt HG. What students learn in problem-based learning: A process analysis. Instr Sci. 2011;40:371–95. [Google Scholar]
- 8.Dolmans DH, Snellen-Balendong H. Maastricht, The Netherlands: Department of Educational Development and Research, Maastricht University; 1999. Problem Construction. [Google Scholar]
- 9.Schmidt HG. Problem-based learning: Rationale and description. Med Educ. 1983;17:11–6. doi: 10.1111/j.1365-2923.1983.tb01086.x. [DOI] [PubMed] [Google Scholar]
- 10.WHO Patient Safety Curriculum Guide, Topic 11: Improving Medication Safety. [Last accessed on 28 Apr 2015]. Available from: http://www.who.int/patientsafety/education/curriculum/PSP_mpc_topic-11.pdf .
- 11.Windish DM, Reed DA, Boonyasai RT, Chakraborti C, Bass EB. Methodological rigor of quality improvement curricula for physician trainees: A systematic review and recommendations for change. Acad Med. 2009;84:1677–92. doi: 10.1097/ACM.0b013e3181bfa080. [DOI] [PubMed] [Google Scholar]
- 12.Nie Y, Li L, Duan Y, Chen P, Barraclough BH, Zhang M, et al. Patient safety education for undergraduate medical students: A systematic review. BMC Med Educ. 2011;11:33. doi: 10.1186/1472-6920-11-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Teigland CL, Blasiak RC, Wilson LA, Hines RE, Meyerhoff KL, Viera AJ. Patient safety and quality improvement education: A cross-sectional study of medical students’ preferences and attitudes. BMC Med Educ. 2013;13:16. doi: 10.1186/1472-6920-13-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Al Khaja KA, James H, Sequeira RP. Effectiveness of an educational intervention on prescription writing skill of preclerkship medical students in a problem-based learning curriculum. J Clin Pharmacol. 2013;53:483–90. doi: 10.1002/jcph.68. [DOI] [PubMed] [Google Scholar]
- 15.Prakash S, Valentine V. Timeline: The Rise and Fall of Vioxx®. National Public Radio. [Last accessed on 28 Apr 2015]. Available from: http://www.npr.org/templates/story/story.php?storyId = 5470430 .
- 16.Karha J, Topol EJ. The sad story of Vioxx, and what we should learn from it. Cleve Clin J Med. 2004;71:933–4. doi: 10.3949/ccjm.71.12.933. 936, 938-9. [DOI] [PubMed] [Google Scholar]
- 17.Krumholz HM, Ross JS, Presler AH, Egilman DS. What have we learnt from Vioxx? BMJ. 2007;20(334):120–3. doi: 10.1136/bmj.39024.487720.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rofecoxib. [Last accessed on 28 Apr 2015]. Available from: http://www.en.wikipedia.org/wiki/Rofecoxib .
- 19.Sockalingam N, Rotgans J, Schmidt HG. Assessing the quality of problems in problem-based learning. Int J Teach Learn High Educ. 2012;24:43–51. [Google Scholar]
- 20.Hay PJ, Katsikitis M. The ‘expert’ in problem-based and case-based learning: Necessary or not? Med Educ. 2001;35:22–6. doi: 10.1046/j.1365-2923.2001.00679.x. [DOI] [PubMed] [Google Scholar]
- 21.Savery JR, Duffy TM. Problem based learning: An instructional model and its constructivist framework. Educ Technol. 1995;35:31–8. [Google Scholar]
- 22.Claire B, Loren L, Alise R, Deborah S, Vargas RB, Barry D, et al. Comparison of upper gastrointestinal toxicity of rofecoxib and naproxen in patients with rheumatoid arthritis. N Engl J Med. 2000;343:1520–8. doi: 10.1056/NEJM200011233432103. [DOI] [PubMed] [Google Scholar]
- 23.Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, Roberts EA, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30:239–45. doi: 10.1038/clpt.1981.154. [DOI] [PubMed] [Google Scholar]
- 24.Dolmans DH, Gijselaers WH, Schmidt HG, van der Meer SB. Problem effectiveness in a course using problem-based learning. Acad Med. 1993;68:207–13. doi: 10.1097/00001888-199303000-00013. [DOI] [PubMed] [Google Scholar]
- 25.Dolmans DH, Gijselaers WH, Moust JH, de Grave WS, Wolfhagen IH, van der Vleuten CP. Trends in research on the tutor in problem-based learning: Conclusions and implications for educational practice and research. Med Teach. 2002;24:173–80. doi: 10.1080/01421590220125277. [DOI] [PubMed] [Google Scholar]
- 26.Abdul Ghaffar Al-Shaibani TA, Sachs-Robertson A, Al Shazali HO, Sequeira RP, Hamdy H, Al-Roomi K. Student generated learning objectives: Extent of congruence with faculty set objectives and factors influencing their generation. Educ Health (Abingdon) 2003;16:189–97. doi: 10.1080/1357628031000116916. [DOI] [PubMed] [Google Scholar]
- 27.Schmidt HG, Dolmans DH, Gijselaers WH, Marchais JE. Theory-guided design of a rating scale for course evaluation in problem-based curriculum. Teach Learn Med. 1995;7:82–91. [Google Scholar]
- 28.Jacobs AE, Dolmans DH, Wolfhagen IH, Scherpbier AJ. Validation of a short questionnaire to assess the degree of complexity and structuredness of PBL problems. Med Educ. 2003;37:1001–7. doi: 10.1046/j.1365-2923.2003.01630.x. [DOI] [PubMed] [Google Scholar]


