Abstract
Background
Cesarean section (CS) is one of the most common obstetric procedures worldwide and an increased rate of cesarean section has been observed in recent studies. Maternal and fetal mortality and morbidity associated with cesarean section is an important health problem worldwide. This requires the evaluation of the effect of repeated cesarean delivery on maternal morbidity.
Material/Methods
A total of 2460 patients who underwent delivery by CS at a center in southeast Turkey between January 2012 and January 2014 (24 months) were included in the study. The patients were divided into 5 groups according to the number of CSs, and the maternal and neonatal outcomes of the groups were retrospectively evaluated.
Results
A statistically significant difference was found between the groups in terms of maternal age, education level, time of hospitalization, operating time, the presence of dense adhesions, bowel and bladder injury, the presence of placenta previa, hysterectomy, blood transfusion requirements, and need for intensive care (p<0.05). Placenta previa (OR, 11.7; 95% CI, 2.6–53.2) and placenta accreta (OR, 12.2; 95% CI, 3.9–37.8) were found to be important risk factors in terms of the need for hysterectomy. No statistically significant difference was found between the groups for gestational age at birth, birth weight, fifth-minute APGAR score, preoperative and postoperative hemoglobin levels, uterine rupture, wound infection, wound dehiscence, placenta accreta, maternal death, and endometritis (p>0.05). A total of 4 or more CSs was identified as the critical level for most of the major complications.
Conclusions
An increasing number of CSs is accompanied by serious maternal complications. Four or more CSs are of especially critical importance. Decreasing the number of cesarean sections is required to decrease relevant complications. Vaginal birth after CS is an option that should be recommended to the patient.
Keywords: Cesarean Section, Repeat; Intraoperative Complications; Morbidity; Postoperative Complications
Background
Cesarean section (CS) is a surgical procedure that may save the life of both the mother and the baby in many cases. Cesarean delivery rates have increased each year and this is now a public health problem in terms of the burden to the economy of the country as well as possible complications. While the cesarean birth rate was 4.5% in the USA in 1965, it was 31.8% according to 2007 data and is thought to be over 50% at present [1,2]. According to the 1993 Turkish Demographic and Health Survey (TDHS), the cesarean birth rate at the time was 8%, and 2008 studies [3] have reported that this has increased to 37%. There are 2 significant reasons for this increase: the increasing primary cesarean rate and the rapidly decreasing rate of normal birth after CS [1]. Although the final reason for the increase in the primary cesarean rate is not clear, medico-legal issues have probably played an important role.
CS has several inherent complications but maternal and fetal well-being, timing of the birth, the surgeon’s experience, the competence of the center, the surgical technique, and the risk of anesthesia are factors that play important roles in the emergence of complications [4]. The cesarean section rate is increasing worldwide. A lack of adequate contraceptive knowledge and the desire to have many children, especially in rural areas, is increasing cesarean section incidence. Many studies have reported the effects of multiple CSs on maternal morbidity, but most of these studies have evaluated the isolated effects of CS on placenta previa, bladder or bowel damage, and intra-abdominal adhesions [5–8]. Most of these studies also have a small percentage or unknown number of patients with 5 or 6 CSs. We planned our study to evaluate morbidity in patients with a history of 5 or more CSs using parameters that were as exact as possible and a larger number of morbidity parameters.
Material and Methods
Location and time of the study
The study was conducted by a retrospective evaluation of the files and hospital records of patients who underwent CS at the Adiyaman University Medical Faculty Training and Research Hospital’s Obstetrics and Gynecology clinic between January 2012 and January 2014 (24 months). Study approval was obtained from the Kahramanmaras Sutcu Imam University School of Medicine, Medical Ethics Committee (Reference Number: 2014/05-03).
Number of patients and study inclusion criteria
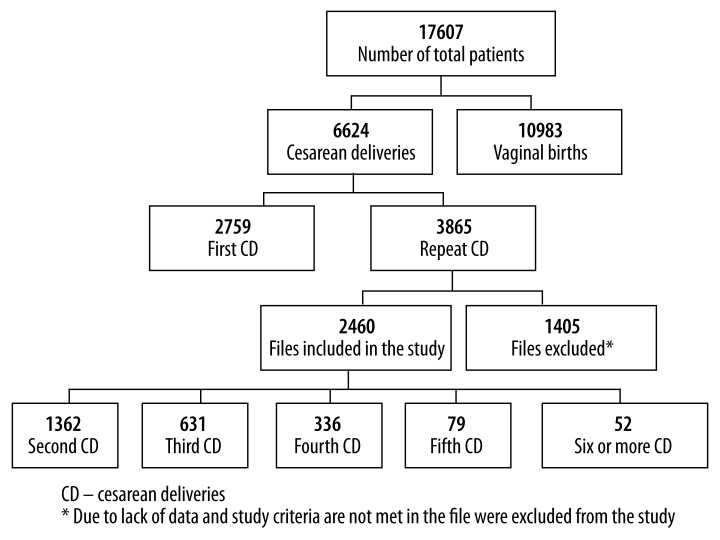
The inclusion criteria were patients who were 20–45 years old, had undergone at least 1 CS, had not undergone non-cesarean abdominal surgery, and the presence of complete patient data. We made sure at least 6 weeks had passed after delivery. A total of 2460 patients who met the required criteria were included in the study (Figure 1).
Figure 1.
Search and selection of patients
Patient exclusion criteria
The patients who were not included in the study were Syrian refugees who had come to Turkey because of civil war and whose pregnancy records could not be accessed (190 patients). Additional exclusions were 674 patients who were living in our region but had irregular pregnancy follow-up and 389 patients who did not come for postnatal follow-up. The 48 patients who underwent other abdominal surgery were also excluded, as were 104 patients who had inadequate data in their hospital records.
Groups and investigated parameters
A total of 5 patient groups were created according to the number of CSs. We recorded each patient’s demographic data and information related to the surgery, such as preoperative and postoperative hemoglobin levels, presence of dense adhesions, presence of wound dehiscence, placenta previa, placenta accreta, bladder and bowel injury, need for hysterectomy, time of hospitalization, uterine rupture, wound infection, operation time, need for blood transfusion, need for intensive care, maternal mortality, and the presence of endometritis. The fetal data recorded were birth weight, fifth-minute APGAR value, and gestational week at birth. Feto-maternal results and surgical complications were evaluated regarding the presence of any difference between the groups.
Descriptions
Dense adhesion was defined as the presence of adhesions detected intraoperatively, extending from the abdominal wall to the bladder or to the front wall of the uterus, not separating easily, and left alone during surgery as much as possible due to the concern that it could cause serious morbidity. A clinical description of endometritis was used, where puerperal fever, foul-smelling vaginal discharge, and pelvic tenderness were present in the post-natal period and no other focus was found. Placenta previa was the placenta closing the cervical internal os completely or partially as found on an ultrasonographic evaluation performed in the third trimester. For patients who did not undergo ultrasonography in the third trimester, complete placenta previa covered the lower segment of the uterus and cervix completely and partial placenta previa covered it partially during intraoperative observation. Placental adhesion abnormalities were diagnosed with histopathological verification if the patient had undergone a hysterectomy, and based on intraoperative findings otherwise. These were described as the presence of intensive bleeding from the adhesion site after the separation attempts in cases where the placenta could not be separated from the adhesion site or where it was difficult to separate them with gentle intraoperative traction. Bladder injury was described as unintentional damage directly related to the incision or during intraoperative tissue dissection. Intestinal damage was described as intestinal entry during intraoperative tissue dissection or seromuscular damage requiring repair. Blood transfusion was required in cases with an Hb value lower than 10 g/dl, when intraoperative estimated blood loss was more than 20% of the total blood volume, or when the Hb level was lower than 8.5 g/dl postoperatively. The operation time was calculated as the time between anesthesia induction and skin closure. Wound infection was defined as discharge from the incision site after the third postoperative day and growth in wound site cultures.
Statistics
The Statistical Package for the Social Sciences software version 13.0 (SPSS Inc., Chicago, IL, USA) was used for the statistical evaluations. The continuous variables were presented as mean ± standard deviation. Comparisons between 2 groups with normally distributed variables were performed with the dependent samples t test. Comparison of more than 2 groups was done with the single-factor analysis of variance (ANOVA) test. The differences between 2 and more than 2 groups without normal distribution were checked with the Mann-Whitney U and Kruskal-Wallis tests, respectively. Groups with categorical variables were compared with the Pearson chi-square test. The level of statistical significance was defined as p<0.05.
Results
There were 17 607 births at our clinic within the specified period. Our total cesarean rate was 37.62%, primary cesarean rate was 15.67%, and the repeated cesarean rate was 21.95%. The demographic data of the patient groups are presented in Table 1.
Table 1.
Demographic features of patients.
| Characteristic | Second CD n=1362 | Third CD n=631 | Fourth CD n=336 | Fifth CD n=79 | ≥6 CD n=52 | p* |
|---|---|---|---|---|---|---|
| Maternal age at delivery (y, mean ±SD) | 28.6±5.3 | 30.1±4.6 | 33.4±2.3 | 35.3±3.7 | 37.1±3.3 | <0.001 |
| Smoker during pregnancy (%) (n) | 1.2 (16) | 1.0 (6) | 2.4 (8) | 1.3 (1) | 1.9 (1) | 0.409 |
| Educational level (years) (mean ±SD) | 8.4±5.3 | 9.0±4.9 | 4.7±5.0 | 2.4±2.9 | 2.6±3.6 | <0.001 |
CD – cesarean delivery; SD – standard deviation; n – number of patients.
There was no statistically significant difference in terms of demographic characteristics between the groups except for maternal age and education status. Maternal age was the lowest in the second CS group (28.6±5.3 years) and the highest in the group with 6 or more CSs (37.1±3.3 years) (p<0.001) (Table 1). A statistically significant difference was present between the groups in terms of educational level (p<0.001). The lowest educational level was found in the group with 5 CSs (2.4±2.9 years). When the fetal values were evaluated, no statistically significant difference was found between the groups for gestational age at birth, birth weight, and fifth-minute APGAR values (p=0.151).
The maternal and fetal complications are presented in Table 2. A statistically significant difference was found between the groups regarding the presence of dense adhesions (p<0.001). The rate of adhesion presence was similar between the second CS (8.4%) and third CS (7.6%) groups (p>0.05), but significantly higher in the fourth CS group (16.1%) and the sixth or more CS (17.3%) groups compared to the other groups (p<0.001).
Table 2.
Maternal and fetal complications in different cesarean section groups.
| Characteristic | Second CD n=1362 | Third CD n=631 | Fourth CD n=336 | Fifth CD n=79 | ≥6 CD n=52 | p |
|---|---|---|---|---|---|---|
| Preop Hb (gr/dL, mean ±SD) | 10.1±1.2 | 10.2±1.2 | 10.2±1.4 | 10.3±1.4 | 10±1.2 | 0.297 |
| Postop Hb (gr/dL) | 10.2±1.2 | 9.4±1.2 | 9.4±1.2 | 9.5±1 | 9.4±0.9 | 0.116 |
| Hospital stay (day) | 2.1±0.4 | 2.1±0.4 | 2.1±0.3 | 2.4±0.8 | 2.9±0.9 | <0.001 |
| Operation time (min) | 38.7±13.6 | 38.9±13.7 | 47.9±14.3 | 45.2±12.2 | 50.3±13.4 | <0.001 |
| Dens adezyon (%)(n) | 8.4 (115) | 7.6 (48) | 16.1 (54) | 5.1 (4) | 17.3 (9) | <0.001 |
| Blader injury (%)(n) | 0.50 (7) | 0.80 (5) | 4.20 (14) | 0.00 (0) | 3.80 (2) | <0.001 |
| Bowel injury (%)(n) | 0.40 (5) | 0.30 (2) | 0.60 (2) | 0.00 (0) | 3.80 (2) | 0.006 |
| Uterine rupture (%)(n) | 0.40 (6) | 1.10 (7) | 1.20 (4) | 1.30 (1) | 0.00 (0) | 0.343 |
| Wound infection (%)(n) | 4.90 (67) | 5.50 (35) | 5.40 (18) | 0.00 (0) | 11.50 (6) | 0.060 |
| Wound dehicsence (%)(n) | 1.00 (13) | 0.50 (3) | 0.90 (3) | 0.00 (0) | 0.00 (0) | 0.663 |
| Placenta accreta (%)(n) | 0.80 (11) | 1.00 (6) | 2.10 (7) | 1.30 (1) | 0.00 (0) | 0.287 |
| Placenta previa (%)(n) | 1.50 (20) | 2.10 (13) | 4.50 (15) | 3.80 (3) | 3.80 (2) | 0.010 |
| Hysterectomy (%)(n) | 0.40 (6) | 0.60 (4) | 1.80 (6) | 2.50 (2) | 3.80 (2) | 0.004 |
| Blood transfusion (%)(n) | 2.10 (28) | 2.10 (13) | 4.80 (16) | 8.90 (7) | 3.80 (2) | <0.001 |
| Intensive care unit (%) | 0.70 (9) | 0.30 (2) | 1.20 (4) | 0.00 (0) | 3.80 (2) | 0.031 |
| Maternal death | 0.10 (1) | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.938 |
| Endometritis | 1.80 (24) | 1.00 (6) | 1.50 (5) | 3.80 (3) | 1.90 (1) | 0.350 |
| Gestational age at delivery (wk, mean ±SD) | 37.6±1.6 | 37.5±1.7 | 37.5±1.4 | 37.7±1.9 | 37.5±1.6 | 0.629 |
| Gestational diabetes mellitus | 2.6 (36) | 4.6 (29) | 3 (10) | 5.1 (4) | 3.8 (2) | 0.192 |
| Preeclampsia | 3.4 (46) | 3.6 (23) | 1.8 (6) | 3.8 (3) | 1.9 (1) | 0.547 |
| Birth weight (gr, mean ±SD) | 3166.1±515.9 | 3137.3±485.7 | 3222.2±664.2 | 3190.8±622.7 | 3268.3±638.6 | 0.116 |
| 5. min APGAR score | 7.4±1.5 | 7.5±1.5 | 7.3±1.5 | 7.8±1.6 | 7.4 ±.7 | 0.151 |
wk – week; CD – cesarean delivery; SD – standart deviation; n – number of patients.
A statistically significant difference was found between the groups in terms of hospitalization time (p<0.001). The rates were similar between the second CS (2.1±0.4 days), third CS (2.1±0.4 days), and fourth CS (2.1±0.3 days) (p>0.05) groups, but the fifth CS (2.4±0.8 days) and the sixth or more CS (2.9±0.9 days) groups had statistically significantly higher rates (p<0.001). The longest hospitalization time was found in the 6 or more CS patient group. A statistically significant difference was also present between the groups in terms of bladder injury rate (p<0.001), with a higher rate in the fourth CS group (4.2%) and sixth or more CS (3.8%) group than the other groups (p<0.001), but with no significant difference between these 2 groups. When evaluated in terms of bowel injury, a statistically significant difference was again found between these 2 groups (p=0.006), with the sixth or more CS group suffering a critical level of intestinal injury (3.8%). No statistically significant difference was found among the other groups.
A significant difference was present between the groups in terms of placenta previa (p=0.010), hysterectomy after CS (p=0.004), and need for blood transfusion (p<0.001). The incidence of these conditions was found to increase in correlation with the increasing number of CSs, but remained stable after the fourth CS. When the relationships between the need for hysterectomy and the placenta accreta and placenta previa rates were evaluated separately, both disorders showed a close relationship with hysterectomy following CS, with placenta accreta increasing the risk of hysterectomy by 11.7-fold (OR, 11.7; 95% CI, 2.6–53.2) and placenta previa increasing this risk 12.2-fold (OR, 12.2; 95% CI, 3.9–37.8).
No statistically significant difference was found between the groups in terms of the need for intensive care (p=0.031) or length of operation time (p<0.001). The need for intensive care (3.8%) and the operation time (50.3±13.4 min) in the group with 6 or more CSs were both significantly higher than in the other groups. When other maternal data were evaluated, there was no statistically significant difference between the groups in terms of uterine rupture, wound infection, placenta accreta, wound dehiscence, endometritis, the incidence of gestational diabetes mellitus and preeclampsia, or maternal mortality rates (p>0.05).
Discussion
There has been a significant increase in the CS rate worldwide, despite variations according to a patient age, place of residence, and cultural conditions. This increase is especially evident for women in cities and those over the age of 35 [9,10]. Repeated cesarean birth is related to serious maternal and fetal complications when compared to normal birth and the first cesarean [9,11]. However, medico-legal factors, increased reliability of cesarean birth, and decreased rates of vaginal birth after CS play important roles in the current increased CS rates. Another serious problem is the higher cost of CS, especially in developed countries [12].
Adhesions are a cause of acute morbidity with bleeding and increased surgery duration and of chronic morbidity with chronic pelvic pain and intestinal problems. An increasing number of CSs increases the adhesion rate as well as intensity [13,14]. In addition, the adhesions can cause additional increased morbidity directly or with peripheral organ injury [14]. Adhesions concurrent with cesarean birth are also influenced by the surgical technique. The adhesion incidence in our study was similar to many other studies and increased in correlation with the number of CSs. The fourth CS seems to be the critical level. The general opinion is that adhesion incidence is within the 46–65% range, depending on the number of cesarean sections [15]. However, our rates are lower than those previously reported in the literature. This may be because we only evaluated adhesions that could cause significant morbidity.
Abnormal placenta development following repeated cesarean birth is concurrent with an increased risk of placenta previa and abruptio placenta in addition to placenta accreta. The risk of placenta previa has been reported to increase by 0.28–2% in patients who have undergone at least 1 CS in a metaanalysis including 36 studies [16]. The incidence of placenta previa was found to be 5.2 per 1,000 births in a cohort study that included an extensive 9-year follow-up period where primiparas were included. Placenta previa (OR, 1.4; 95% CI, 1.1–1.6) and placental abruption (OR, 1.3; 95% CI, 1.1–1.5) were found to increase, favoring cesarean birth for second births, again in the same study [17]. However, there are also studies that do not support this finding, especially for placenta previa [18]. We found that the placenta previa rate increased with the number of CSs in our study. However, the risk remained proportionately stable after the fourth CS. This result correlates with the literature data [19]. Similarly, an increase in the need for blood transfusion was found, along with an increasing number of cesarean sections, increasing in association with placenta previa.
Placenta accreta is one of the most important morbidities in repeating cesarean births. The risk is reported to be associated with the increasing number of CSs, and especially with placenta previa located on the uterine anterior wall. The concurrence of placenta previa and placenta accreta was less than 24% in the second CS group, 40% in the third CS group, and over 60% with the fourth and more CS [14,20]. However, the critical number is generally accepted as having undergone at least two CSs [8,19]. However, some publications report no association between placenta accreta and the number of CSs [21]. We also found no placenta accreta risk increase with the number of CSs, and no relationship was found between placenta previa and placenta accreta rates. This contrast to the common literature may be due to the surgical techniques, suture materials, placental localization differences, or racial characteristics.
Hysterectomy is another significant morbidity. It is mostly associated with placenta accreta, placenta previa, uterine atony, and uterine rupture. Each uterine scar is accompanied with an increasing risk of hysterectomy, independent of the presence of placenta previa. This is usually the result of increased placenta accreta frequency, together with inadequate decidualization [14,22]. We observed that an increased number of hysterectomies correlated with an increasing number of CSs, usually due to placenta previa, and this was consistent with the literature.
Peripheral organ damage (such as to the intestines and bladder), inpatient duration, need for intensive care, and surgery duration are affected by the presence of placenta accreta, dense adhesions, and hysterectomy. All these outcomes are correlated with an increasing number of cesarean births, and the fourth CS is notable as the critical level. However, 6 or more CSs is an important level regarding intestinal damage and the need for intensive care.
Of the parameters evaluated, no significant difference was found between the groups for uterine rupture, incision site infection and dehiscence, and endometritis (p>0.05). Follow-up is more frequent in patients who have undergone many CSs and the 39th gestational week is not waited for; therefore, the patients avoid staying in labor long enough to create the risk of uterine rupture. The low ratio of maternal mortality related to the surgical technique and improvements in surgical techniques and operating room equipment as noted in many studies were also observed in our study, and there was only 1 maternal mortality secondary to disseminated intravascular coagulation (DIC), which developed due to postpartum hemorrhage.
Our center often accepts risky patients from neighboring districts who have not had follow-ups. This increases our multiple repeat CS number and enables us to see the related morbidity data more clearly. An interesting point of our study is the many patients with 5 or more CSs. As shown in many studies, this increases the complications rate, especially those related to the surgery. We found that the rates of injuries of adjacent organs (such as the bladder and intestines), placenta previa, blood transfusion requirement, and infectious complications were significantly higher in the groups with 5 or 6 CSs. It is possible that the complications rate would be even higher if the procedures for these patients were performed in centers without adequate experience or capacity. Important strengths of our study are similar patient care and follow-up conditions, patient populations with similar demographic data, and the large number of patients. The records were carefully evaluated and charts with incomplete or inadequate data would not be included in the evaluation. Our study’s retrospective design is its most important weakness.
The number of births is quite high in our region. Women become pregnant again within a short time after CS due to a lack of education and information, as well related social reasons, and they do not have adequate knowledge about the potential complications. This is a common problem in many regions of the world. Providing adequate contraception training can prevent an increased number of pregnancies. On the other hand, reducing the number of primary CSs and encouraging patients and physicians to consider vaginal birth after CS is of critical importance in reducing maternal-fetal mortality and morbidity related to repeat CSs.
Conclusions
The evaluation of our study data shows a significant increase in maternal morbidity with an increasing number of CSs. However, the fourth CS operation emerges as the critical level for most of the morbidity. Placenta previa and adhesions seem to play a central role in all the risks. Peripheral organ damage, bleeding, need for intensive care, long surgery time, and an increased incidence of hysterectomy are all correlated. The occurrence of placental development abnormalities, especially in patients taken to surgery under emergency conditions, is a significant issue. This problem can be overcome by identifying patients at risk during pregnancy in peripheral centers and directing these patients to referral centers, especially during the third trimester. Our study, in light of this background, will help us provide information on the probable complications of placenta previa and adhesions in particular, guiding patients away from elective CS and directing them towards vaginal delivery after CS.
Footnotes
Source of support: Departmental sources
Conflict of interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- 1.MacDorman MF, Menacker F, Declercq E. Cesarean birth in the United States: epidemiology, trends, and outcomes. Clin Perinatol. 2008;35(2):293–307. doi: 10.1016/j.clp.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 2.Hamilton BE, Martin JA, Ventura SJ. Births: preliminary data for 2007. Natl Vital Stat Rep. 2009;57:1–23. [PubMed] [Google Scholar]
- 3.Turkey Demographic and Health Survey (TDHS) Hacettepe Institute of Population Studies Ministry of Health. 2008. 2008 ( http://www.hips.hacettepe.edu.tr/turkiyede_dogurganlik_ureme_sagligi_yaslilik_160910.pdf.
- 4.Voigt M, Fröhlich CW, Hüttelet C, et al. Prophylaxis of intra- and postoperative nausea and vomiting in patients during cesarean section in spinal anesthesia. Med Sci Monit. 2013;19:993–1000. doi: 10.12659/MSM.889597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bates GW, Jr, Shomento S. Adhesion prevention in patients with multiple cesarean deliveries. Am J Obstet Gynecol. 2011;205(6 Suppl):S19–24. doi: 10.1016/j.ajog.2011.09.030. [DOI] [PubMed] [Google Scholar]
- 6.Qublan HS, Tahat Y. Multiple cesarean section. The impact on maternal and fetal outcome. Saudi Med J. 2006;27(2):210–14. [PubMed] [Google Scholar]
- 7.Ben-Ami I, Schneider D, Svirsky R, et al. Safety of late second-trimester pregnancy termination by laminaria dilatation and evacuation in patients with previous multiple cesarean sections. Am J Obstet Gynecol. 2009;201(2):154.e1–5. doi: 10.1016/j.ajog.2009.04.029. [DOI] [PubMed] [Google Scholar]
- 8.Marshall NE, Fu R, Guise JM. Impact of multiple cesarean deliveries on maternal morbidity: a systematic review. Am J Obstet Gynecol. 2011;205(3):262.e1–8. doi: 10.1016/j.ajog.2011.06.035. [DOI] [PubMed] [Google Scholar]
- 9.Tampakoudis P. Caesarean section rates and indications in Greece: data from a 24-year period in a teaching hospital. Clin Exp Obstet Gynecol. 2004;31(4):289–92. [PubMed] [Google Scholar]
- 10.Chigbu CO, Ezeome IV, Iloabachie GC. Cesareansection on request in a developing country. Int J Gynaecol Obstet. 2007;96(1):54–56. doi: 10.1016/j.ijgo.2006.09.032. [DOI] [PubMed] [Google Scholar]
- 11.O’Dwyer V, Hogan JL, Farah N, et al. Maternal mortality and the rising cesarean rate. Int J Gynaecol Obstet. 2012;116(2):162–64. doi: 10.1016/j.ijgo.2011.09.024. [DOI] [PubMed] [Google Scholar]
- 12.Fawsitt CG, Bourke J, Greene RA, et al. At What Price? A Cost-Effectiveness Analysis Comparing Trial of Labour after Previous Caesarean versus Elective Repeat Caesarean Delivery. PLoS ONE. 2013;8:e58577. doi: 10.1371/journal.pone.0058577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tulandi T, Agdi M, Zarei A, et al. Adhesion development and morbidity after repeat cesarean delivery. Am J Obstet Gynecol. 2009;201(1):e1–6. doi: 10.1016/j.ajog.2009.04.039. [DOI] [PubMed] [Google Scholar]
- 14.Silver RM, Landon MB, Rouse DJ, et al. Maternal morbidity associated with multiple cesarean deliveries. Obstet Gynecol. 2006;107(6):1226–32. doi: 10.1097/01.AOG.0000219750.79480.84. [DOI] [PubMed] [Google Scholar]
- 15.Lyell DJ. Adhesions and perioperative complications of repeat cesarean delivery. Am J Obstet Gynecol. 2011;205(6):11–18. doi: 10.1016/j.ajog.2011.09.029. [DOI] [PubMed] [Google Scholar]
- 16.Ananth CV, Smulian JC, Vintzileos AM. The association of placenta previa with history of cesarean delivery and abortion: a metaanalysis. Am J Obstet Gynecol. 1997;177(5):1071–78. doi: 10.1016/s0002-9378(97)70017-6. [DOI] [PubMed] [Google Scholar]
- 17.Lydon-Rochelle M, Holt VL, Easterling TR, et al. First-birth cesarean and placental abruption or previa at second birth(1) Obstet Gynecol. 2001;97(5 Pt 1):765–69. [PubMed] [Google Scholar]
- 18.Hershkowitz R, Fraser D, Mazor M, et al. One or multiple previous cesarean sections are associated with similar increased frequency of placenta previa. Eur J Obstet Gynecol Reprod Biol. 1995;62(2):185–88. doi: 10.1016/0301-2115(95)02194-c. [DOI] [PubMed] [Google Scholar]
- 19.Clark EA, Silver RM. Long-term maternal morbidity associated with repeat cesarean delivery. Am J Obstet Gynecol. 2011;205(6):2–10. doi: 10.1016/j.ajog.2011.09.028. [DOI] [PubMed] [Google Scholar]
- 20.Makoha FW, Felimban HM, Fathuddien MA, et al. Multiple cesarean section morbidity. Int J Gynaecol Obstet. 2004;87(3):227–32. doi: 10.1016/j.ijgo.2004.08.016. [DOI] [PubMed] [Google Scholar]
- 21.Gasim T, Al Jama FE, Rahman MS, et al. Multiple repeat cesarean sections: operative difficulties, maternal complications and outcome. J Reprod Med. 2013;58(7–8):312–18. [PubMed] [Google Scholar]
- 22.Khong TY. The pathology of placenta accreta, a worldwide epidemic. J Clin Pathol. 2008;61(12):1243–46. doi: 10.1136/jcp.2008.055202. [DOI] [PubMed] [Google Scholar]