Abstract
Background
Prison inmates are among the high risk population for dangerous infections such HIV, HBV, HCV and other contagious diseases. In spit of many data about the prevalence and risk factors for blood born diseases among prisoners in the world, such data are spares from Iran. The aim of this study was to determine the prevalence and associated risk factors for HIV, HBV, HCV and HDV infections among a large sample of prison inmates in Iran.
Methods
In a cross-sectional study in 2009-2010, 881 inmates in three prisons of Southern Khorasan Province in Iran were selected based on a systematic, stratified random sampling method. Sera were analyzed for HBV, HDV, HCV and HIV infections by appropriate commercial ELISA kits. An anonymous questionnaire was used to collect the demographic data and information about risk factors.
Results
Overall, 881 prisoners (mean age: 34.7±11.4 years, range: 11-84 years, M/F ratio:4.5/1) were participated in this study. The prevalence of HBV and HCV infection was 6.9% and 7.7%, respectively. Among the HBsAg positive subjects, 6.6% (4/61) and 9.8% (6/61) had HDV and HCV super-infection, respectively. Only one case (0.1%) had HIV infection that was co-infection with HCV. Drug abuse and history of traditional phlebotomy were associated risk factors for HBV infection (P<0.05) and history of drug injection was associated with HCV infection (P<0.05).
Conclusions
This study show fairly higher prevalence of blood borne infections among prisoners and indicate drug abuse and phlebotomy as the associated risk factor. Implementation of appropriate screening tests and preventive programs is suggested in prisons.
Keywords: Hepatitis B, Hepatitis C, HIV, Injecting drug users, Prison
Introduction
Prison inmates are a high risk population for dangerous infections such as human immunodeficiency virus (HIV), hepatitis B and C viruses (HBV, HCV) as well as other blood born diseases (1–7). Up to 40% of all Americans with chronic viral hepatitis were in prison and the prevalence of viral hepatitis among prisoners was significantly higher than general population (8). In fact these infections have been transmitted to prisoners while they were in prison (9–11) and it could be explained by higher prevalence of risky behaviors among this population which include, but are not limited to, drug abuse, frequent injections, needle sharing, promiscuity and unprotected sex as well as tattooing. Early identification and treatment of infected prisoners can decrease the risk of infection transmission not only inside prisons but also after community re-entry.
Data about the prevalence and risk factors for blood born infections in prisoners are very scared in Iran. A few studies have reported HCV infection in 30-45% of Iranian drug abuser prisoners (12–14) and in one study, the prevalence of HBV infection was 4.7% among Iranian prisoners which is quite higher than normal population (15). This higher prevalence in inmates of different regional central prisons compared to the general population in Iran emphasizes the need for aggressive intervention for identification and treatment of patients and implementation of preventive strategies.
To our knowledge, data about the risk factors associated with higher prevalence of HIV, HBV, and HCV infections among prison inmates in Iran are scared and thus judgment about blood-borne infections within the prisons often was made based on data from other countries while socio-economical and cultural situations are somehow different in Iran and therefore study about the rate, sources and associated risk factors for blood borne diseases in prisons is a key factor for prevention and control of spreading of the infections within the prisons which leads to decrease the rate of transmission not only in prisons but also in the whole community.
The aim of this study was to determine the prevalence and associated risk factors for HIV, HBV, HDV and HCV infections among a sample of prison inmates in three central prisons in Southern Khorasan Province, Iran.
Methods
This cross-sectional study was carried out on prisoners over a period of one year (March 2009-February 2010) in three prisons (2 in Birjand City and 1 in Qaem City) in Southern Khorasan Province, Iran. The study protocol was performed in accordance with the declaration of Helsinki and subsequent revisions and approved by ethics committee of Birjand University of Medical Sciences and by Southern Khorasan Bureau of Prisons as well.
Participation in the study was voluntary and confidentiality of information was guaranteed. Informed consent was obtained from each prisoner who participates in this study. Sample size was calculated as 838 cases and based on a systematic, stratified random sampling, 900 prisoners were invited for this study and finally 881 prisoners enrolled in the study and demographic data as well as information about risk factors were collected by an anonymous questionnaire which completed by a trained assistant through interview with prisoners. Five ml of venous blood was drawn from all participants and sera were screened for anti-HCV antibody (Dia-pro diagnostic ® HCV ElISA, Italy), hepatitis B surface antigen (Dia lab ® HBs Ag, Austria), anti HIV antibody (Dia lab ®HIV Ab, Austria) in duplicate. All sera positive for HCV-Ab and HIV-Ab were confirmed by the second generation of recombinant immunoblot assay (RIBA) kits (Diagnostics® HCV blot; Germany) and western blot as a complementary test respectively.
Statistical analysis
The data were analyzed by SPSS software version 18 (SPSS Inc., Chicago, IL, USA) and chi-square and if necessary Fisher exact test were used to compare the variables. A P values < 0.05 was considered as statistically significant.
Results
Among the 881 participants, 723 were male (82.1%) and 158 (17.9%) were female. The mean age of study population was 34.7 ± 11.4 (range 11-84) years. Out of 881 prisoners, 61 cases (6.9%) were positive for HBsAg and 68 cases (7.7%) were positive for anti-HCV. Among subjects who were HBsAg positive, 4 cases (6.6%) were HDV positive as well. Co-infection of HBV and HCV was found in 6 (0.7%) subjects. One case was positive for HIV infection (0.1%) which also had co-infection with HCV.
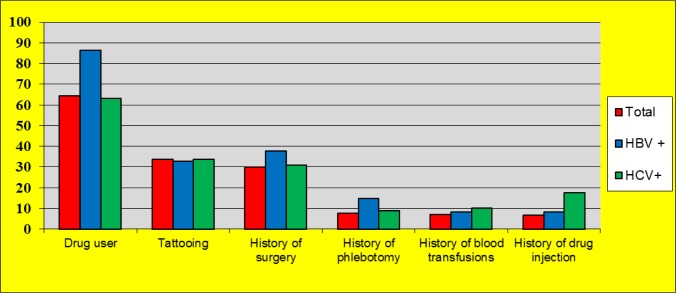
Although for both HBV and HCV, the rate of infection was higher in male than female (7.6% and 3.8%, for HBV 8% and 6.3%, for HCV respectively) but the difference was not significant. 568 cases (64.5%) had a history of drug abuse and 57% (324 cases) had history of opium consumption. Table 1 shows type of drug and route of administration among the participants. Among HBsAg and HCV positive cases, 5 (8.2%) and 12 (17.6%) cases were injecting drug users (IDUs) respectively. Figure 1 shows the occurrences of different risk factors among prisoners.
Table 1:
Type and route of drug administration among prisoners
| Number | Percent | |
|---|---|---|
| Total substance users | 568 | 64.5 |
| Type of substance | ||
| Opium | 324 | 57 |
| Heroin | 27 | 4.7 |
| Crystal methamphetamine | 40 | 7 |
| Multi-drug use | 177 | 31.3 |
| Route of administration | ||
| Smoking | 435 | 76.6 |
| Injection | 25 | 4.4 |
| Oral | 21 | 3.7 |
| Combine injection and other ways | 34 | 6.1 |
| Combine smoking and other ways | 53 | 9.2 |
Fig. 1:
Prevalence of different risk factors among HBV and HCV positive subjects
Statistical analysis showed that the prevalence of HBsAg was significantly higher among drug users (9.3 vs. 2.6%, P<0.001) or those who had a history of traditional phlebotomy (cupping) (13.2 vs. 6.4%, P=0.03) (Table 2) but there was no significant difference in the rate of HBV infection regarding history of drug injection (8.5% vs. 9.4%, P=0.81). The rate of HCV was significantly higher among prisoners with a history of drug injection (20.3 vs. 6.1%, P<0.001) (Table 3). There was no significant correlation between HBsAg or HCV infection and history of surgery, tattooing or receiving blood transfusions
Table 2:
Analysis of potential risk factors for HBV infection among prisoners
| Risk factor | HBsAg + | HBsAg- | P-value |
|---|---|---|---|
| Drug user | 53 (9.3) | 8 (2.6) | <0.001 |
| Tattooing | 20 (6.7) | 41 (7) | 0.86 |
| History of surgery | 23 (8.7) | 38 (6.2) | 0.17 |
| History of traditional phlebotomy | 9 (13.2) | 52 (6.4) | 0.03 |
| History of blood transfusions | 5 (8.1) | 56 (6.8) | 0.6 |
| History of drug injection | 5 (8.5) | 48 (9.4) | 0.81 |
Table 3:
Analysis of potential risk factors for HCV infection among prisoners
| Risk factor | Anti-HCV + | Anti-HCV - | P-value |
|---|---|---|---|
| Drug user | 43 (7.6) | 25 (8) | 0.82 |
| Tattooing | 23 (7.7) | 45 (7.7) | 1 |
| History of surgery | 21 (8) | 47 (7.6) | 0.86 |
| History of traditional phlebotomy | 6 (8.8) | 62 (7.6) | 0.72 |
| History of blood transfusions | 7 (11.3) | 61 (7.4) | 0.27 |
| History of drug injection | 12 (20.3) | 31 (6.1) | <0.001 |
Discussion
Prisoners are a high risk population for blood born diseases and regular assessment of prisoner’s health and identification of infected cases and related risk factors has a very important role in prevention and reducing the risk of transmission inside and outside prisons. In the present study the rate of HCV, HBV, HDV and HIV infections in three central prisons of Southern Khorasan was quite higher than general population. In another study on prisoners in our region (Birjand) also report similar results in which the HBV and HCV prevalence was 6.1% and 8.1%, respectively with no HIV positive case (16).
In comparison to other parts of Iran, the rate of HCV infection in our study (8% in all, 9.3% in drug users, and 8.5% in IDUs) was lower. A study in west of Iran (Hamedan) indicated that 30% of all drug using prisoners and 31.5% of IDUs had HCV infection (12). Rate of HCV infection in drug using prisoners was reported around 30.8 and 45.4 in Gilan and Mazandaran provinces respectively (13, 14) and HCV was high as 88.9% in IDUs prisoners in Gilan study. The rates of all blood-borne infections were dramatically high among prisoners in south of Iran. HIV, HCV and HBV infection rate among IDU inmates in Hormozgan Province (in Northern margin of Persian Gulf) was found to be 15.1%, 64.8%, and 4.7%, respectively (15). In other countries, studies on prisoners reported a variety of results. In Pakistan, which is relatively near to our study location, the rate of HCV among prisoners was 12.8% (17). A study in Europe (Croatia), had similar rates to our result for overall infections (HBV 11.3%, HCV 8.3%, HBV/HCV 6.3%), but higher rates among IDUs (52% HCV and 26.2% HBV) (18). Another study in prison of Australia showed that the incidence rate for HCV infection among IDUs was 34.2% per 100 person years (19). Although the results are different and it could be explained by differences in the prevalence of infection in communities and some socio-economical and cultural factors but all studies indicated that the rate of HCV infection in IDUs is higher than non-IDUs prisoners. Our study showed that HBV infection was significantly associated with drug abuse and traditional phlebotomy which is a therapeutic method used in traditional medicine and still is popular in many societies including Iran. It can be a risky behavior especially considering that mostly the hygienic criteria is not met during phlebotomy. The association of HBV seroposit-ivity with phlebotomy was reported in other parts of Iran as well (20).
The rate of blood born diseases was lower in female and it could be explained by lower rate of crimes, drug abuse and other risky behaviors among female which is related to cultural and religious believes. As far as we know, there is no data about the rate of HDV among prisoners but in several studies on general population in Shiraz, Golestan and Tabriz the rate of HDV infection among Hepatitis B patients was 13.9%, 5.8% and 6.15% respectively (21–23) with is close to our result.
In spit of higher prevalence of blood born diseases among prisoners than general population, still the prevalence of HBV, HCV and especially HIV was lower than other reports from Iran and other countries as well. Iran is a large country and people in different parts have different ethnicities, culture and lifestyles. South Khorasan is located in Mid-East of Iran with a fairly high level of education and general health and low rate of crimes for example there are just two known cases of HIV infection in the whole province (unpublished date). In the same context, prevalence of hepatitis B among blood donors was reported around 0.8% (24) while the prevalence in our province is around 0.47%, therefore the lower rate of infections among prisoners can be a result of some factors including low prevalence of these diseases among general population, good level of education, traditional lifestyle and low density of prisoners in prison.
Conclusions
With consideration of higher prevalence of blood born infection among prisoners, it is necessary to effectively apply practical approaches to reduce risk of transmission for these infections in prisons such as vaccination, education of prisoners and prison staffs about blood-borne infections and transmission risk factors especially sharing needles and syringes and phlebotomy.
Ethical considerations
Ethical issues (Including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgments
This study was made possible by a grant from the Health Department of Birjand University of Medical Sciences, Birjand, Iran. We would like to thank our colleagues in Health Department of Birjand University of Medical Sciences, responsible people in prisons and Dr M. Shayesteh, Mr H. Zangooee and Mr MA. Miraki. The authors declare that there is no conflict of interests.
References
- Dolan K, Kite B, Black E, Aceijas C, Stimson GV (2007). HIV in prison in low-income and middle-income countries. Lancet Infect Dis, 7: 32–41. [DOI] [PubMed] [Google Scholar]
- Singh S, Prasad R, Mohanty A (1999). High prevalence of sexually transmitted and blood-borne infections amongst the inmates of a district jail in Northern India. Int J STD AIDS, 10: 475–478. [DOI] [PubMed] [Google Scholar]
- Long J, Allwright S, Barry J, et al. (2001). Prevalence of antibodies to hepatitis B, hepatitis C, and HIV and risk factors in entrants to Irish prisons: a national cross sectional survey. BMJ, 323: 1209–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinbaum CM, Sabin KM, Santibanez SS (2005). Hepatitis B, hepatitis C, and HIV in correctional populations: a review of epidemiology and prevention. AIDS, 19 Suppl 3:S41–46. [DOI] [PubMed] [Google Scholar]
- Stark K, Herrmann U, Ehrhardt S, Bienzle U (2006). A syringe exchange programme in prison as prevention strategy against HIV infection and hepatitis B and C in Berlin, Germany. Epidemiol Infect, 134: 814–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poulin C, Alary M, Lambert G, et al. (2007). Prevalence of HIV and hepatitis C virus infections among inmates of Quebec provincial prisons. CMAJ, 177: 252–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adjei AA, Armah HB, Gbagbo F, et al. (2008). Correlates of HIV, HBV, HCV and syphilis infections among prison inmates and officers in Ghana: A national multicenter study. BMC Infect Dis, 8: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammett TM, Harmon MP, Rhodes W (2002). The burden of infectious disease among inmates of and releasees from US correctional facilities, 1997. Am J Public Health 92: 1789–1794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutter RC, Grimes RM, Labarthe D (1994). Evidence of intraprison spread of HIV infection. Arch Intern Med, 154: 793–795. [PubMed] [Google Scholar]
- Stark K, Bienzle U, Vonk R, Guggenmoos-Holzmann I (1997). History of syringe sharing in prison and risk of hepatitis B virus, hepatitis C virus, and human immunodeficiency virus infection among injecting drug users in Berlin. Int J Epidemiol, 26: 1359–1366. [DOI] [PubMed] [Google Scholar]
- Haber PS, Parsons SJ, Harper SE, et al. (1999). Transmission of hepatitis C within Australian prisons. Med J Aust, 171: 31–33. [DOI] [PubMed] [Google Scholar]
- Alizadeh AH, Alavian SM, Jafari K, Yazdi N (2005). Prevalence of hepatitis C virus infection and its related risk factors in drug abuser prisoners in Hamedan--Iran. World J Gastroenterol, 11: 4085–4089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohtasham Amiri Z, Rezvani M, Jafari Shakib R, Jafari Shakib A (2007). Prevalence of hepatitis C virus infection and risk factors of drug using prisoners in Guilan province. East Mediterr HealthJ, 13: 250–256. [PubMed] [Google Scholar]
- Zakizad M, Salmeh F, Yaghoobi T, et al. (2009). Seroprevalence of hepatitis C infection and associated risk factors among addicted prisoners in Sari-Iran. Pak J Biol Sci, 12: 1012–1018. [DOI] [PubMed] [Google Scholar]
- Davoodian P, Dadvand H, Mahoori K, Amoozandeh A, Salavati A (2009). Prevalence of selected sexually and blood-borne infections in Injecting drug abuser inmates of Bandar Abbas and Roodan correction facilities, Iran, 2002. Braz J Infect Dis, 13: 356–358. [DOI] [PubMed] [Google Scholar]
- Azarkar Z, Sharifzadeh G (2010). Evaluation of the Prevalence of Hepatitis B, Hepatitis C, and HIV in Inmates with Drug-Related Convictions in Birjand, Iran in 2008. Hepatitis Monthly, 10: 26–30. [PMC free article] [PubMed] [Google Scholar]
- Gorar ZA, Zulfikar I (2010). Seropositivity of hepatitis C in prison inmates of Pakistan--a cross sectional study in prisons of Sindh. J Pak Med Assoc, 60: 476–479. [PubMed] [Google Scholar]
- Burek V, Horvat J, Butorac K, Mikulic R (2010). Viral hepatitis B, C and HIV infection in Croatian prisons. Epidemiol Infect, 138: 1610–1620. [DOI] [PubMed] [Google Scholar]
- Dolan K, Teutsch S, Scheuer N, et al. (2010). Incidence and risk for acute hepatitis C infection during imprisonment in Australia. Eur J Epidemiol, 25: 143–148. [DOI] [PubMed] [Google Scholar]
- Abedi F, Madani H, Asadi A, Nejatizadeh A (2011). Significance of blood-related high-risk behaviors and horizontal transmission of hepatitis B Virus in Iran. Arch Virol 156(4): 629–635. [DOI] [PubMed] [Google Scholar]
- Malekzadeh R, Borhanmanesh F (1989). Prevalence of HDV in asymptomatic healthy carrier of HBV in Iran. Iran J Med Sci 14(2): 33–38. [Google Scholar]
- Taghavi S, Sedighi S, Mehrabani D, Khademolhosseini F (2008). Hepatitis D in chronic active hepatitis B: prevalence, liver enzymes and histopathology-an epidemiological study in Shiraz, southern Iran, 2003. –2004. Hepatitis Monthly 4(8): 248–251. [Google Scholar]
- Roshandel G, Semnani S, Abdolahi N, et al. (2007). Prevalence of hepatitis D virus infection in HBsAg positive subjects in Iran. Pak J Biol Sci 10(10): 1751–1754. [DOI] [PubMed] [Google Scholar]
- Poorolajal J, Majdzadeha R (2009). Prevalence of chronic hepatitis B infection in Iran: a review article. J Res Med Sci 14(4): 249–258. [PMC free article] [PubMed] [Google Scholar]