Abstract
Objectives:
This study aimed to describe the epidemiology of diabetes mellitus over the past two decades in Oman, particularly in terms of its prevalence and incidence. In addition, the study sought to estimate the future incidence of diabetes in Oman.
Methods:
Three national and three regional surveys conducted between 1991 and 2010 were analysed to obtain the age-adjusted prevalence and undiagnosed proportion of type 2 diabetes mellitus (T2DM) among Omani subjects aged ≥20 years. Diabetes mellitus registers and published studies were used to determine incidence rates of both type 1 diabetes mellitus (T1DM) and T2DM in Oman. Linear regression was used to determine trends and projections for diabetes in 2050.
Results:
The age-adjusted prevalence of T2DM in Oman varied from 10.4% to 21.1%, while the highest prevalence of impaired fasting glucose was found in males (35.1%). In comparison to men, higher incidence rates of T2DM were found in women (2.7 cases compared to 2.3 cases per 1,000 person-years, respectively). No significant trends were observed for the prevalence or incidence of T2DM in both genders. Undiagnosed T2DM was more common in men (range: 33–68%) than women (range: 27–53%). The results of this study show that by 2050, there will be an estimated 350,000 people with T2DM living in Oman (a 174% increase compared to estimates for 2015).
Conclusion:
Health authorities need to prioritise diabetes prevention and control in order to prevent or delay long-term complications and avert a potential epidemic of diabetes in Oman.
Keywords: Diabetes Mellitus, Epidemiology, Incidence, Prevalence, Trends, Oman
Advances in Knowledge
- The epidemiology of diabetes mellitus (DM) and related conditions in Oman over the past 20 years is described, utilising data from six surveys conducted between 1991 and 2010.
- The prevalence, incidence, proportion of undiagnosed cases and projections of the number of diabetes cases expected in Oman by the year 2050 using current trends are estimated for the first time.
Application to Patient Care
- With the recognition of the high prevalence and incidence of DM and associated risk factors in Oman, governmental and public health authorities are recommended to prioritise the control and prevention of this condition.
The global prevalence of diabetes mellitus is on the rise and is projected to increase by 55% between 2013 and 2035.1 Currently, four out of five people with diabetes live in low- or middle-income countries where resources are scarce.1 The prevalence of diabetes is projected to double in the Middle Eastern and North African (MENA) region; three countries in the MENA region are already ranked amongst the global top 10 in terms of diabetes prevalence.1 Between 1990 and 2010, diabetes mellitus was also recorded as the fifth leading cause of death among Arab states of the MENA region.2
Oman is classified as a high-income country and the total population is estimated to reach 3.6 million inhabitants, of which 58% are nationals.3,4 Nearly 14% of the population are under five years of age, 34% are under 15 years and only 6% are aged 60 years or over.5 The World Health Organization (WHO) classifies Oman as a country with low child and adult mortality rates (crude death rate: 3.2 per 1,000).6 In terms of diabetes mellitus prevalence, Oman is ranked eighth among the top 10 countries of the MENA region.7 In 2010, diabetes mellitus was the fourth leading cause of premature mortality in the country and the third leading cause of disability-adjusted life years lost.8 In the early 1990s, the Omani Ministry of Health believed that non-communicable diseases, particularly type 2 diabetes mellitus (T2DM) and cardiovascular diseases (CVD), constituted a major and increasing workload for clinicians in Omani hospitals. A WHO ad hoc consultation found that 9% of all adult hospital admissions, 12% of all hospital bed occupancy and 20–30% of all outpatient attendance in regional hospitals were associated with diabetes mellitus.9
To the best of the authors’ knowledge, although several epidemiological studies of diabetes have been published in Oman, none have collated data over the past two decades in a comprehensive single study as of yet. The aim of this study was therefore to provide a summary and up-to-date data on the epidemiology of diabetes mellitus in Oman from the early 1990s to 2010, as well as to estimate the future incidence of diabetes in Oman based on current trends.
Methods
Data from the following three national and three regional population-based surveys were analysed. The National Diabetes Survey was conducted in 1991 to ascertain and validate the findings of the previous WHO ad hoc consultation.10 Thereafter, the National Health Survey in 2000 and the Oman World Health Survey in 2008 were conducted to monitor various health indicators, including changes in the prevalence of diabetes.11,12 In addition, the city of Nizwa (located 150 km south of the capital city, Muscat) conducted two regional surveys, known as the Nizwa Healthy Lifestyle Project Surveys, in 2001 and 2010 to monitor CVD risk factors.13,14 A third regional survey, the Healthy Lifestyle Study, was conducted in 2006 in the city of Sur (located 200 km east of Muscat).15
Each national survey was designed to include a nationally representative sample and included all 11 governorates of Oman. The regional surveys also followed a similar sampling method. The response rate for these surveys ranged from 75–93%. The two national surveys (2000 and 2008) and two of the regional surveys (2006 and 2010) obtained blood samples to measure fasting plasma glucose (FPG) from subjects after they had fasted overnight for at least eight hours. In the 1991 and 2001 surveys, an oral glucose tolerance test (OGTT) was used to measure plasma glucose two hours post 75 g oral glucose load, as recommended by the WHO.16 Further methodological details of each survey are published elsewhere.10–15
Data analysis was limited to Omani nationals aged ≥20 years with complete data regarding the following variables: nationality; age; gender; fasting blood glucose levels; plasma glucose levels two hours post 75 g oral glucose load; an existing diabetes diagnosis from a physician, or a newly diagnosed case of diabetes. Patients were determined to have undiagnosed diabetes (UD) if they had stated that they were not diabetic but had a fasting blood glucose (FBG) level of ≥7 mmol/L. Proportions of UD cases were calculated by dividing the number of UD cases by the total number of subjects with a FPG level of ≥7 mmol/L. Subjects who reported a diagnosis of diabetes from a health professional or who were taking anti-diabetic medications were classified to have T2DM regardless of their measured glucose levels. Glucose metabolism abnormalities, including diabetes mellitus, impaired glucose tolerance (IGT) and/ or impaired fasting glycaemia (IFG), were classified according to diagnostic criteria from both the WHO and the American Diabetes Association (ADA).16,17
Annual incidence rates for T2DM were calculated by dividing the number of all new cases diagnosed and documented in the National Diabetes Register in a calendar year by the estimated mid-year population at risk of that year to obtain cases per person-years (P-Y). The average incidence rate for the period 2003–2013 was calculated by dividing the mean number of cases in this period by the mean P-Y at risk in the same period. As gender distribution of diabetes cases for the years 2003–2007 was not available, the mean gender distribution in subsequent years (2008–2012) was calculated and applied to that period. The mean age at diagnosis for incidence cases was calculated from aggregated age groups by multiplying the mid-interval of the age group by the frequency in that group. Population data and projections were obtained from the Annual Health Reports and the Directorate General of Planning of the Omani Ministry of Health.5
Trends over time were determined by gender for prevalence rates of T2DM and IFG using linear regression, with prevalence as a dependent variable and study year as an independent variable. A P value of <0.05 for the regression slope was considered to be significant.
Age-standardised prevalence rates of T2DM were calculated using the world standard population determined by Segi.18 Linear regression was used to evaluate the gender-specific increase in T2DM prevalence per year. Projections of expected cases of T2DM between 2015 and 2050 were calculated by multiplying the gender-specific expected prevalence by the population.
Statistical analysis was performed using Stata® data analysis and statistical software, Version 11 (StataCorp LP, College Station, Texas, USA).
Results
Among subjects aged ≥20 years, the 1991 survey, which was the first epidemiological survey to map T2DM in Oman, found the crude prevalence of T2DM to be 10.7% and the prevalence of IGT to be 10.3% [Table 1]. In the 2000 and 2008 surveys, the T2DM prevalence was 11.1% and 9.6%, respectively. A similar prevalence rate was found in the 2001 survey carried out in Nizwa (9.9%). The highest crude prevalence of T2DM was recorded in Sur in 2006 (13.9%), with 13.5% for males and 14.1% for females.
Table 1:
Crude and age-adjusted prevalence of diabetes mellitus, impaired glucose tolerance and fasting glycaemia among Omani adults aged ≥20 years between 1991–2010 according to diagnostic criteria
| Survey type, location and year | Test | Sample size | Crude prevalence in % | Age-adjusted prevalence in % | |||||
|---|---|---|---|---|---|---|---|---|---|
| M | F | M | F | Total | M | F | Total | ||
| DM by WHO criteria16 | |||||||||
| Ptrend | - | - | 0.53 | 0.81 | 0.69 | 0.32 | 0.62 | 0.51 | |
| National (1991)10 | Two hour post-OGTT | 2,097 | 2,938 | 10.7 | 10.8 | 10.7 | 12.5 | 14.4 | 13.5 |
| National (1991)10 | FPG | 2,097 | 2,938 | 10.2 | 8.8 | 9.4 | 11.6 | 11.5 | 11.5 |
| National (2000)11 | FPG | 2,887 | 2,922 | 11.3 | 11.0 | 11.1 | 13.2 | 13.3 | 13.2 |
| National (2008)12 | FPG | 1,259 | 1,479 | 10.6 | 8.8 | 9.6 | 13.0 | 11.5 | 12.2 |
| Regional (Nizwa, 2001)13 | Two hour post-OGTT | 694 | 790 | 10.4 | 9.5 | 9.9 | 12.3 | 14.2 | 13.0 |
| Regional (Nizwa, 2001)13 | FPG | 694 | 790 | 8.7 | 7.1 | 7.8 | 10.6 | 10.8 | 10.4 |
| Regional (Nizwa, 2010)14 | FPG | 827 | 1,024 | 10.9 | 8.3 | 9.5 | 13.9 | 12.3 | 12.9 |
| Regional (Sur, 2006)15 | FPG | 599 | 772 | 13.5 | 14.1 | 13.9 | 17.9 | 21.1 | 19.5 |
| Impaired glucose tolerance and impaired fasting glycaemia by WHO criteria16 | |||||||||
| Ptrend | - | - | 0.87 | 0.53 | 0.68 | 0.79 | 0.71 | 0.73 | |
| National (1991)10 | Two hour post-OGTT | 2,097 | 2,938 | 7.3* | 12.5* | 10.3* | 8.2* | 14.3* | 11.6* |
| National (1991)10 | FPG | 2,097 | 2,938 | 5.3 | 5.1 | 5.2 | 5.9 | 6.4 | 6.2 |
| National (2000)11 | FPG | 2,887 | 2,922 | 7.2 | 5.2 | 6.2 | 7.9 | 5.8 | 6.8 |
| National (2008)12 | FPG | 1,259 | 1,479 | 4.8 | 4.4 | 4.6 | 5.5 | 4.8 | 5.1 |
| Regional (Nizwa, 2001)13 | Two hour post-OGTT | 694 | 790 | 14.7* | 16.0* | 15.4* | 15.4* | 18.1* | 16.7* |
| Regional (Nizwa, 2001)13 | FPG | 694 | 790 | 10.1 | 5.8 | 7.8 | 10.9 | 7.4 | 9.0 |
| Regional (Nizwa, 2010)14 | FPG | 827 | 1,024 | 6.4 | 6.5 | 6.5 | 7.5 | 7.4 | 7.5 |
| Regional (Sur, 2006)15 | FPG | 599 | 772 | 9.5 | 8.6 | 9.1 | 10.4 | 11.7 | 10.8 |
| Impaired fasting glycaemia by ADA criteria17 | |||||||||
| Ptrend | - | - | 0.68 | 0.52 | 0.58 | 0.66 | 0.59 | 0.61 | |
| National (1991)10 | FPG | 2,097 | 2,938 | 15.9 | 14.2 | 14.9 | 16.8 | 16.5 | 16.6 |
| National (2000)11 | FPG | 2,887 | 2,922 | 18.3 | 14.0 | 16.1 | 19.5 | 15.0 | 17.3 |
| National (2008)12 | FPG | 1,259 | 1,479 | 16.2 | 11.6 | 13.7 | 16.8 | 13.1 | 14.7 |
| Regional (Nizwa, 2001)13 | FPG | 694 | 790 | 34.0 | 20.5 | 26.8 | 35.1 | 23.6 | 29.1 |
| Regional (Nizwa, 2010)14 | FPG | 827 | 1,024 | 21.6 | 20.7 | 21.1 | 23.4 | 22.2 | 22.9 |
| Regional (Sur, 2006)15 | FPG | 599 | 772 | 31.8 | 29.3 | 30.3 | 33.1 | 32.4 | 32.5 |
M = males; F = females; T = total; DM = diabetes mellitus; WHO = World Health Organization; OGTT = oral glucose tolerance test; FPG = fasting plasma glucose; ADA = American Diabetes Association.
Values for impaired glucose tolerance.
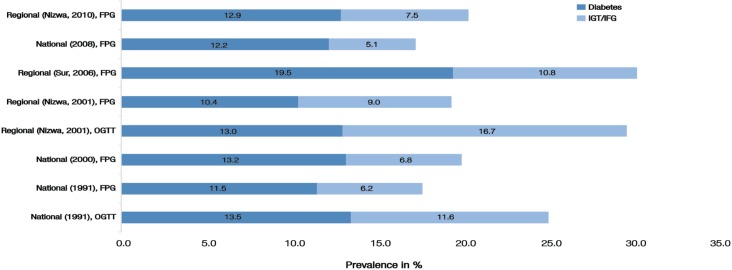
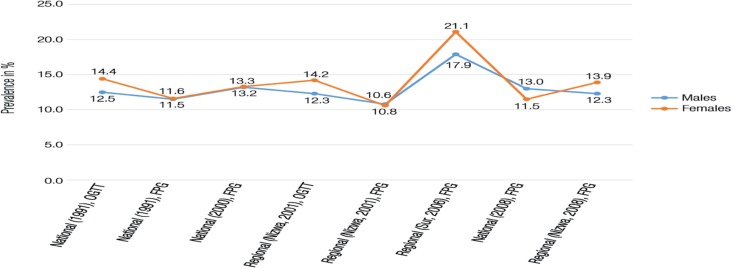
Age-adjustment inflated all prevalence rates, particularly in the 2006 survey in Sur, where the highest T2DM rates were observed in females (21.1%). The prevalence of IFG varied drastically depending on the diagnostic criteria used. With WHO criteria, most IFG prevalence rates were between 5–7%, while age-adjusted rates were between 7–10% [Table 1]. On the other hand, using ADA criteria led to much higher prevalence rates of IFG (three to four times higher than the crude rates). The combined proportion of Omanis affected by either diabetes or IFG/IGT exceeded 30% in two of the regional studies in Nizwa and Sur (2001 and 2006) [Figure 1]. Neither of the diagnostic criteria showed a statistically significant trend in crude or age-adjusted prevalence rates of T2DM and IFG for both genders [Figure 2]. The mean age of subjects with prevalent diabetes during successive surveys increased from 47.4 years in 1991 to 51.4 years in 2008 and 52.5 years in 2010.
Figure 1:
Total age-adjusted prevalence of diabetes mellitus and impaired glucose tolerance/impaired fasting glucose among Omanis aged ≥20 years between 1991–2010 using data from six population-based national and regional surveys.10–15 The World Health Organization diagnostic criteria for diabetes was used.16
IGT = impaired glucose tolerance; IFG = impaired fasting glycaemia; OGTT = oral glucose tolerance test; FPG = fasting plasma glucose.
Figure 2:
Trend in age-adjusted prevalence of diabetes mellitus among Omani adults aged ≥20 years between 1991–2010 using data from six population-based national and regional surveys.10–15 Trends are presented according to gender, survey and method of test used.
OGTT = oral glucose tolerance test; FPG = fasting plasma glucose.
It was found that there were approximately 4,900 new cases of T2DM diagnosed in Oman each year among patients aged ≥20 years. The mean age of incident cases was 48 years, with males at 48.1 years and females at 47.8 years (P = 0.001; male to female ratio = 100:113). The incidence rate of T2DM in females was higher than males (2.7 compared to 2.3 cases per 1,000 P-Y, respectively; P = 0.789). The age-specific incidence rate increased in both genders from 0.7 cases per 1,000 P-Y in the second decade, peaking in the fifth decade for both men and women (14 and 16 cases per 1,000 P-Y, respectively) and declining thereafter. No significant temporal trend in incidence rate over two decades was observed for men or women (Ptrend = 0.42 and 0.43, respectively).
Table 2 shows that the proportion of subjects with UD decreased in Nizwa from 60.3% in 2001 to 30.7% in 2010. Overall, men had a significantly higher proportion of UD (51.5%) compared to women (42.8%; P = 0.009).
Table 2:
Prevalence of undiagnosed diabetes mellitus among Omani adults aged ≥20 years between 1991–2010*
| Survey type, location and year | Prevalence of UD in % | ||
|---|---|---|---|
| M | F | T | |
| National (1991)10 | 47.4 | 45.9 | 46.6 |
| National (2000)11 | 64.0 | 53.4 | 58.7 |
| National (2008)12 | 46.3 | 35.4 | 40.9 |
| Regional (Nizwa, 2001)13 | 68.3 | 51.8 | 60.3 |
| Regional (Nizwa, 2010)14 | 33.3 | 27.1 | 30.7 |
| Regional (Sur, 2006)15 | 49.4 | 43.1 | 45.8 |
UD = undiagnosed diabetes mellitus; M = males; F = females; T = total.
Table 3 forecasts the total number of T2DM cases expected in Oman between 2015 and 2050 by gender, using mean prevalence rates of the national surveys and the predicted increase rate using linear regression models. On average, more than 350,000 people with T2DM are estimated to be living in Oman in 2050. This is an increase of approximately 174% compared to 2015.
Table 3:
Projected number of cases of diabetes among Omanis aged ≥20 years between 2015–2050*
| Year | Diabetes cases | ||
|---|---|---|---|
| M | F | T | |
| 2015 | 69,323 | 60,548 | 128,769 |
| 2020 | 80,490 | 69,779 | 149,195 |
| 2030 | 108,339 | 92,522 | 199,918 |
| 2040 | 149,571 | 125,425 | 274,265 |
| 2050 | 192,790 | 159,603 | 352,156 |
| Total increase in % | 178.1 | 163.6 | 173.5 |
M = males; F = females; T = total.
Projections of expected cases were calculated by multiplying the gender-specific expected prevalence by the estimated population of that particular year .
Discussion
A persistently high prevalence of T2DM among subjects aged ≥20 years in Oman over the past two decades was found after analysing data from six surveys, reaching as high as 21% in the region of Sur. Similar rates have been reported in Egypt (15.2%), Saudi Arabia (16.2%), Qatar (16.7%) and Iran (9.3%).19 A similar proportion of the Omani population suffer from IGT and/or IFG. Despite the statistically non-significant increase in the trend of T2DM prevalence and incidence over the past two decades, the absolute number of people living with T2DM in Oman is expected to increase by 174% by the year 2050, when compared to current estimates.
There are several indications of an impending epidemic of T2DM and CVD in Oman. First, high prevalences of obesity, physical inactivity and sedentary lifestyles have been reported in Oman.20 Data regarding obesity from the three national surveys used in this study show an increasing proportion of males with a body mass index (BMI) of ≥30 kg/m2 (10.5%, 16.7% and 22.0% in 1991, 2000, and 2008 surveys, respectively).10–12 While the prevalence of obesity among women remained stable between the 1991 and 2000 surveys (25.1% and 23.8%, respectively), it increased in the 2008 survey to 26.0%.10–12 Despite this increase in the prevalence of obesity, the rate of diabetes has remained stable in Oman with no significant increase in trend among either gender. A similar analysis of data from the USA has shown doubling of both the incidence and prevalence of diabetes mellitus between 1990 to 2008; this increase subsequently plateaued between 2008 and 2012.21 The levelling off of both of these parameters is thought to be linked to the stabilisation of obesity rates in the USA.21 Second, increasing urbanisation will lead to a future increase in diabetes; 75% of the current Omani population live in urban areas as compared to 47% in 1980.22 Higher frequencies of T2DM and IGT were found in urban areas of Oman, such as Muscat (12% and 5.6%, respectively), compared to rural areas like the Musandam peninsula, which is over 400 km from Muscat (7.8% and 2.2%, respectively).23
The third indicator of an impending epidemic of T2DM and CVD in Oman is the proportion of the population aged 65 years and over. This proportion is expected to increase 10 times by the year 2035 (from 2.5% to 21%); this will also contribute to higher rates of diabetes.22 Finally, a high prevalence of IFG combined with a conversion rate of 5.6% per annum to diabetes and a high familial predisposition to diabetes is likely to aggravate the already high prevalence rates of this condition.24,25
In the present study, the incidence rate of T2DM among Omanis aged ≥20 years was 2.5 cases per 1,000 P-Y. High incidence rates of T2DM have been reported from South Korea and Taiwan (7.6 and 7.7 per 1,000 P-Y respectively),26,27 compared to Sweden (3.5 cases per 1,000 P-Y).28
Changes in the diagnostic criteria for diabetes usually have an impact on diabetes incidence and prevalence depending on the cut-off values adopted. In 1997, the ADA adopted new diagnostic criteria for diabetes, followed by similar changes by the WHO in 1999.16,17 However, such changes did not affect the current study as original data collected from the field were analysed based on both WHO and ADA diagnostic criteria.
The only study documenting the incidence of childhood T1DM in children aged 0–14 years in Oman was conducted by Soliman et al. over two years.29 The reported incidence rate was 2.45 and 2.62 per 100,000 P-Y in 1993 and 1994, respectively. The gender-specific incidence rates among boys and girls were 3.23 and 1.99 per 100,000 P-Y in 1993 and 2.91 and 1.95 per 100,000 P-Y in 1994, respectively. The age-specific incidence rates during these two years were higher in the 10–14-year-old age group (3.69 and 4.22 per 100,000 P-Y in 1993 and 1994, respectively) compared to those aged 5–9-year-old (2.32 and 2.79 per 100,000 P-Y) and those aged 0–4-year-old (1.54 and 0.97 per 100,000 P-Y). The same study also reported that the number of new cases was markedly higher in the relatively cooler months of the year (September to March).29 However, the reported incidence rate of T1DM in Omani children by Soliman et al. was lower than that reported in other Arabian Gulf states, such as Saudi Arabia and Kuwait (27.5 and 15.4 per 100,000 P-Y, respectively).30,31
The present study observed that approximately 30–60% of T2DM cases were undiagnosed in Oman. Similar or higher proportions have been reported from other Arab countries (75%, 48% and 62% in Tunisia, Saudi Arabia and Egypt, respectively).32 Studies from developed nations such as France, Portugal and Finland have reported the prevalence of UD to be 50%, 44% and 61%, respectively.32 In an effort to detect UD cases earlier and to reduce the burden of diabetes and other non-communicable diseases in Oman, the Ministry of Health initiated a National Screening Programme in 2006 inviting subjects aged ≥40 years to be screened for diabetes and other risk factors by attending their local primary healthcare centre after fasting overnight.33 Those who attended had their arterial blood pressure and weight measured and venous blood and urine samples collected. Results of the screening programme are shown in Table 4.33 In 2007, Al-Lawati et al. developed a simple diabetes risk score to screen for T2DM among adults aged ≥20 years.34 The tool contained specified scores for questions on age, waist circumference, BMI, family history of diabetes and current hypertension status. The sensitivity of the score was reported to be 78.6% and its specificity was 73.4%.34 The impact of both the screening programme and risk score have not yet been evaluated.
Table 4:
Prevalence of risk factors among Omanis aged ≥40 years screened for selected non-communicable diseases in primary healthcare centres between 2008–2009*
| Risk factor | Prevalence in % | ||
|---|---|---|---|
| M (n = 15,115) | F (n = 24,861) | T (n = 39,976) | |
| Gender | 38 | 62 | 100 |
| BMI of ≥30 kg/m2 | 22 | 36 | 31 |
| Abnormal WC** | 54 | 76 | 68 |
| Pre-HTN† | 15 | 13 | 13 |
| HTN‡ | 22 | 19 | 20 |
| Pre-diabetes§ | 35 | 35 | 35 |
| Diabetes¶ | 10 | 7 | 8 |
| High cholesterol | 47 | 49 | 48 |
| eGFR of <90 mL/minute | 33 | 26 | 29 |
| eGFR of <60 mL/minute | 11 | 8 | 9 |
| eGFR of <30 mL/minute | 1 | 1 | 1 |
M = males; F = females; T = total; BMI = body mass index; WC = waist circumference; HTN = hypertension; eGFR = estimated glomerular filtration rate.
Data from Oman Ministry of Health. Operational and Management Guidelines for the National Non-Communicable Diseases Screening Program. Muscat, Oman: Ministry of Health, 2009.33
Defined as ≥94 cm for males and ≥80 cm for females.
Defined as systolic blood pressure (SBP) of ≥130 mmHg and <140 mmHg and/or diastolic blood pressure (DBP) of ≥85 mmHg and <90 mmHg.
Defined as SBP of ≥140 mmHg and/or DBP ≥ of 90 mmHg.
Defined as fasting plasma glucose (FPG) of ≥5.6 mmol/L and <7 mmol/L.
Defined as FPG of ≥7 mmol/L.
Current data from Omani Ministry of Health institutions indicate that 5% of all pregnant women are diagnosed with gestational diabetes mellitus (GDM).5 In addition, 14.3% of fetal deaths are attributed to diabetes during pregnancy.5 Dashora et al. reported testing 564 women attending an antenatal clinic at a secondary hospital for glucose intolerance using an OGTT.35 Results indicated that 20.2% of women had two hour post-load glucose levels of ≥7.8 mmol/L. Over 87% of cases of GDM in this study were diagnosed at the first antenatal visit (≤12 gestational weeks). Second (at 16–20 gestational weeks) and third OGTT (at 24–28 gestational weeks) results added additional information in only a minority of cases (10% and 2.5%, respectively).35 In another study investigating GDM, Barakat et al. reported that women in Oman with GDM were three times more likely to have a child with macrosomia (adjusted odds ratio [OR] = 3.03) and to have a Caesarean section delivery (adjusted OR = 2.7).36 Adjusted ORs for the same conditions were 7.2 and 4.4 for women with pregestational diabetes.
The prevalence of GDM depends on the type of test and the diagnostic cut-off values used. In Oman, the reported prevalence of GDM (20.2%) was similar to that reported from the United Arab Emirates (20.6%) and Qatar (19.0%), but higher than that reported from Bahrain (13.5%) and Saudi Arabia (12.5%).35,37 However, Oman’s only study investigating GDM was based in a regional hospital.35 Thus, a national study to further elucidate the epidemiology of GDM may be warranted. With Oman being a high prevalence country, screening for GDM earlier than usually recommended (for example, at the first trimester rather than at 24–28 gestational weeks) may prove beneficial in the light of recent data which show that women with hyperglycaemia have an increased risk of adverse maternal, fetal and neonatal outcomes even within ranges of glycaemia previously considered normal for pregnant women.35,38
Over the past four and a half decades, Oman has achieved conspicuous advances in the delivery of modern and free healthcare services to its entire population, including those living in remote areas. This has led to successful control and eradication of communicable diseases. On the other hand, the burden of non-communicable diseases, including diabetes, has increased.39 Despite this, information regarding how to prevent T2DM through lifestyle modifications is available.40 The public should be encouraged to adopt healthy lifestyles in order to prevent or delay T2DM and its complications. It is paramount that Omani health authorities pay greater attention to healthcare services that will result in reducing the burden of this condition in order to prevent or delay its complications and avert an impending epidemic.
The results of the current study highlight the current gaps in epidemiological knowledge and the need to update information regarding the incidence of T1DM. This may be done by investigating the accuracy of diabetes registers and examining ways to improve their utilisation in secondary and tertiary health institutions where the diagnosis of such cases occur. There is also a noticeable paucity of epidemiological data regarding the incidence and prevalence of T1DM in Oman, with the only available study dating back to two decades ago.29 As the incidence of this chronic disease is increasing worldwide, there is an urgent need to establish a national registry and to conduct further studies to monitor the magnitude of this condition to help plan for future healthcare services. Furthermore, no studies could be identified regarding the cost of diabetes in Oman. Thus, future work on determining the cost of diabetes to the Omani national health service would be vital.
The major strength of this study lies in the fact that all six surveys used for the data analysis were population-based with similar sampling methods and were thus representative and generalisable to the entire Omani population. However, the study has several limitations. First, in estimating the incidence of diabetes, an assumption of a full year of patient follow-up was made. This may have overestimated the incidence rate as some patients are censored during the study period (perhaps due to death, loss to follow-up, migration, etc.). Nonetheless, it is worthwhile noting that local health centre staff make enquiries regarding patients who do not follow-up their treatments and these patients are henceforth struck from the diabetes register which minimises this bias. Second, incidence rates are also likely to be underestimated as nearly 50% of diabetic subjects are undiagnosed; hence the true incidence is likely to be twice that reported. Third, incidence data on diabetes registers are not specifically collected to determine incidence rates. Their accuracy and completeness is often undetermined, especially in the absence of any evaluation of such registers.
Conclusion
There is a high prevalence of T2DM and, to a lesser extent, incidence of T2DM. Additionally, high proportions of UD cases were recorded in Oman. Health authorities need to prioritise detection, control and treatment strategies for this condition so that a future overwhelming epidemic of diabetes mellitus is averted in Oman. This may include encouraging the general population to adopt healthy lifestyles in order to prevent or delay T2DM and its related complications.
Footnotes
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
References
- 1.International Diabetes Federation IDF Diabetes Atlas: Sixth edition. From: www.idf.org/diabetesatlas/download-book Accessed: Nov 2014.
- 2.Mokdad AH, Jaber S, Aziz MI, AlBuhairan F, AlGhaithi A, AlHamad NM, et al. The state of health in the Arab world, 1990–2010: An analysis of the burden of diseases, injuries, and risk factors. Lancet. 2014;383:309–20. doi: 10.1016/S0140-6736(13)62189-3. [DOI] [PubMed] [Google Scholar]
- 3.The World Bank . Country and Lending Groups: Middle East and North Africa. From: data.worldbank.org/about/country-and-lending-groups#MENA Accessed: Nov 2014. [Google Scholar]
- 4.National Center for Statistics & Information Population. From: www.ncsi.gov.om/NCSI_Website/book/SYB2014/2-Population.pdf#search=“population” Accessed: Jul 2014.
- 5.Directorate General of Planning, Oman Ministry of Health Annual Health Report Muscat, Oman: Ministry of Health; 2000. –2012 [Google Scholar]
- 6.World Health Organization The World Health Report 2003: Shaping the future. From: www.who.int/whr/2003/en/ Accessed: Nov 2014.
- 7.Majeed A, El-Sayed AA, Khoja T, Alshamsan R, Millett C, Rawaf S. Diabetes in the Middle-East and North Africa: An update. Diabetes Res Clin Pract. 2014;103:218–22. doi: 10.1016/j.diabres.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 8.Institute for Health Metrics and Evaluation GBD Profile: Oman. From: www.healthdata.org/sites/default/files/files/country_profiles/GBD/ihme_gbd_country_report_oman.pdf Accessed: Nov 2013.
- 9.Asfour MG, Samantray SK, Dua A, King H. Diabetes mellitus in the Sultanate of Oman. Diabet Med. 1991;8:76–80. doi: 10.1111/j.1464-5491.1991.tb01520.x. [DOI] [PubMed] [Google Scholar]
- 10.Asfour MG, Lambourne A, Soliman A, Al-Behlani S, Al-Asfoor D, Bold A, et al. High prevalence of diabetes mellitus and impaired glucose tolerance in the Sultanate of Oman: Results of the 1991 National Survey. Diabet Med. 1995;12:1122–5. doi: 10.1111/j.1464-5491.1995.tb00431.x. [DOI] [PubMed] [Google Scholar]
- 11.Al-Lawati JA, Al Riyami AM, Mohammed AJ, Jousilahti P. Increasing prevalence of diabetes mellitus in Oman. Diabet Med. 2002;19:954–7. doi: 10.1046/j.1464-5491.2002.00818.x. [DOI] [PubMed] [Google Scholar]
- 12.Al Riyami A, Elaty MA, Morsi M, Al Kharusi H, Al Shukaily W, Jaju S. Oman World Health Survey: Part 1 - Methodology, sociodemographic profile and epidemiology of non-communicable diseases in Oman. Oman Med J. 2012;27:425–43. [PMC free article] [PubMed] [Google Scholar]
- 13.Oman Ministry of Health . Summary Report of the Nizwa Healthy Lifestyle Project Survey 2001. Muscat, Oman: Ministry of Health; 2002. [Google Scholar]
- 14.Al-Siyabi H, Al-Anquodi Z, Al-Hinai H, Al-Hinai S. Nizwa Healthy Lifestyle Project Evaluation Report 2010. Ad Dakhiliyah, Oman: Ministry of Health; 2010. [Google Scholar]
- 15.Al-Farsi M, El-Melighy M, Mohammed S, Ali L. Healthy Lifestyle Study: Assessment of lifestyle risk factors among Sur city population Sur. Oman: Ministry of Health; 2006. [Google Scholar]
- 16.Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications: Part 1: Diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15:539–53. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 17.American Diabetes Association Standards of medical care in diabetes: 2014. Diabetes Care. 2014;37:S14–80. doi: 10.2337/dc14-S014. [DOI] [PubMed] [Google Scholar]
- 18.Segi M. Cancer mortality for selected sites in 24 countries (1950–57) Sendai, Japan: Department of Public Health, Tohuku University of Medicine; 1960. [Google Scholar]
- 19.Whiting DR, Guariguata L, Weil C, Shaw J. Idf diabetes atlas: Global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94:311–21. doi: 10.1016/j.diabres.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 20.Mabry R, Owen N, Eakin E. A national strategy for promoting physical activity in Oman: A call for action. Sultan Qaboos Univ Med J. 2014;14:e170–5. [PMC free article] [PubMed] [Google Scholar]
- 21.Geiss LS, Wang J, Cheng YJ, Thompson TJ, Barker L, Li Y, et al. Prevalence and incidence trends for diagnosed diabetes among adults aged 20 to 79 years, United States, 1980–2012. JAMA. 2014;312:1218–26. doi: 10.1001/jama.2014.11494. [DOI] [PubMed] [Google Scholar]
- 22.United Nations . World Population Prospects: The 2012 revision. From: esa.un.org/wpp/documentation/publications.htm Accessed: Nov 2014. [Google Scholar]
- 23.Al-Lawati JA, Mohammed AJ. Diabetes in Oman: Comparison of 1997 American Diabetes Association classification of diabetes mellitus with 1985 WHO classification. Ann Saudi Med. 2000;20:12–15. doi: 10.5144/0256-4947.2000.12. [DOI] [PubMed] [Google Scholar]
- 24.Nichols GA, Hillier TA, Brown JB. Progression from newly acquired impaired fasting glusose to type 2 diabetes. Diabetes Care. 2007;30:228–33. doi: 10.2337/dc06-1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Al-Sinani S, Al-Shafaee M, Al-Mamari A, Woodhouse N, Al-Shafie O, Hassan M, et al. Familial clustering of type 2 diabetes among Omanis. Oman Med J. 2014;29:51–4. doi: 10.5001/omj.2014.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim DJ. The epidemiology of diabetes in Korea. Diabetes Metab J. 2011;35:303–8. doi: 10.4093/dmj.2011.35.4.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chang CH, Shau WY, Jiang YD, Li HY, Chang TJ, Sheu WH, et al. Type 2 diabetes prevalence and incidence among adults in Taiwan during 1999–2004: A national health insurance data set study. Diabet Med. 2010;27:636–43. doi: 10.1111/j.1464-5491.2010.03007.x. [DOI] [PubMed] [Google Scholar]
- 28.Andersson T, Ahlbom A, Magnusson C, Carlsson S. Prevalence and incidence of diabetes in Stockholm County 1990–2010. PLoS One. 2014;9:e104033. doi: 10.1371/journal.pone.0104033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Soliman AT, al-Salmi IS, Asfour MG. Epidemiology of childhood insulin-dependent diabetes mellitus in the Sultanate of Oman. Diabet Med. 1996;13:582–6. doi: 10.1002/(SICI)1096-9136(199606)13:6<582::AIDDIA114>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 30.Abduljabbar MA, Aljubeh JM, Amalraj A, Cherian MP. Incidence trends of childhood type 1 diabetes in eastern Saudi Arabia. Saudi Med J. 2010;31:413–18. [PubMed] [Google Scholar]
- 31.Shaltout AA, Qabazard MA, Abdella NA, LaPorte RE, al Arouj M, Ben Nekhi A, et al. High incidence of childhood-onset IDDM in Kuwait: Kuwait Study Group of Diabetes in Childhood. Diabetes Care. 1995;18:923–7. doi: 10.2337/diacare.18.7.923. [DOI] [PubMed] [Google Scholar]
- 32.Beagley J, Guariguata L, Weil C, Motala AA. Global estimates of undiagnosed diabetes in adults. Diabetes Res Clin Pract. 2014;103:150–60. doi: 10.1016/j.diabres.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 33.Oman Ministry of Health . Operational and Management Guidelines for the National Non-Communicable Diseases Screening Program. Muscat, Oman: Ministry of Health; 2009. [Google Scholar]
- 34.Al-Lawati JA, Tuomilehto J. Diabetes risk score in Oman: A tool to identify prevalent type 2 diabetes among Arabs of the Middle East. Diabetes Res Clin Pract. 2007;77:438–44. doi: 10.1016/j.diabres.2007.01.013. [DOI] [PubMed] [Google Scholar]
- 35.Dashora U, Dashora V, Kennedy L. Two-hour 75-g oral glucose tolerance test early in pregnancy detects most cases of gestational diabetes. Diabetes Care. 2002;25:803. doi: 10.2337/diacare.25.4.803. [DOI] [PubMed] [Google Scholar]
- 36.Barakat MN, Youssef RM, Al-Lawati JA. Pregnancy outcomes of diabetic women: Charting Oman’s progress towards the goals of the Saint Vincent Declaration. Ann Saudi Med. 2010;30:265–70. doi: 10.4103/0256-4947.65253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bener A, Saleh NM, Al-Hamaq A. Prevalence of gestational diabetes and associated maternal and neonatal complications in a fast-developing community: Global comparisons. Int J Womens Health. 2011;3:367–73. doi: 10.2147/IJWH.S26094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.HAPO Study Cooperative Research Group. Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U, Coustan DR, et al. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008;358:1991–2002. doi: 10.1056/NEJMoa0707943. [DOI] [PubMed] [Google Scholar]
- 39.Al-Lawati JA, Mabry R, Mohammed AJ. Addressing the Threat of Chronic Diseases in Oman. Prev Chronic Dis. 2008;5:A99. [PMC free article] [PubMed] [Google Scholar]
- 40.Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Diabetes Prevention Program Research Group Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]