Abstract
Objectives:
Prescription rates of methylphenidate (MPH) are sharply rising in most Western countries. Although it has been reported that MPH has abuse potential, little is known about the prevalence of intravenous (IV) abuse of MPH. The aim of the study was to investigate the prevalence of IV MPH abuse among treatment-seeking IV substance abusers in Iceland.
Methods:
This is a descriptive population-based study using a semistructured interview assessing sociodemographics, substance abuse history, and the method of administration of 108 IV substance abusers. During 1 year, consecutively admitted adult inpatients with substance use disorder at any detoxification center in Iceland that reported any IV substance abuse in the past 30 days were invited to participate. Abuse was defined as nontherapeutic use of a substance to gain psychological or physiological effect.
Results:
Prevalence of any IV MPH abuse among participants was 88% in the last 30 days (95% confidence interval [CI], 0.82-0.94) and MPH was the most commonly abused substance (65%) and the preferred substance (63%). Around one third (30%) reported MPH as the first IV substance ever abused. However, among those reporting a shorter history than 10 years of IV abuse, 42% reported MPH as the first IV substance ever abused.
Conclusions:
This first nationwide study on IV abuse of MPH shows that it is common among treatment-seeking IV abusers in Iceland and suggests that MPH has high abuse potential. Therefore, both the use and possible abuse of MPH in those with high abuse potential should be monitored, especially in countries where MPH prescriptions rates are on the rise.
Keywords: detoxification, intravenous abuse, methylphenidate, prescription drugs, stimulants
Prescriptions of methylphenidate (MPH) for attention-deficit/hyperactivity disorder (ADHD) have been rising sharply in most Western countries during the past decade (Scheffler et al., 2007; Dalsgaard et al., 2012). This rise in MPH use has been particularly steep in Iceland. For 2 consecutive years (2010-2011), Iceland had a higher per capita prescription rates of MPH than the United States, which for several previous years had been reported to have among the highest prescription rate in the world per capita (Kaye & Dark, 2012; United Nations, 2012). In 2012, the consumption rate of MPH in Iceland was 14.8 defined daily doses per 1000 inhabitants per day versus 7.9 in the United States (United Nations, 2013).
This increase in MPH prescribing has been explained by the growing awareness and understanding of ADHD among both the public and the medical community (Castle et al., 2007; Riggs et al., 2011; Sigurjonsson, 2011; Kaye & Dark, 2012). Because of the high MPH prescription rate in Iceland, the Directorate of Health has restricted prescription privileges to psychiatrists, neurologists, and pediatricians (The Icelandic Ministry of Welfare, 2011).
Methylphenidate is a reuptake inhibitor that enhances both the effects of noradrenalin and dopamine in the central nervous system (Heal et al., 2009). Methylphenidate has similar pharmacological effects as better known substances with a high abuse potential such as cocaine and amphetamine. Methylphenidate has been shown to have similar drug-seeking reinforcing effects as cocaine and, therefore, concerns have been raised about its abuse potential (Wang et al., 1997; Kollins et al., 2001; Volkow et al., 2002; Kollins, 2003). However, the view in some reports (Volkow et al., 2002; Kollins, 2003) has been that MPH has less abuse potential than cocaine. This has been attributed to a relatively slow clearance rate from the brain and hence less likelihood of repeated administration and abuse of MPH.
Increased availability of MPH has indeed been followed by reports of nonintravenous abuse, particularly in countries where consumption levels are high (United Nations, 2012). Methylphenidate is typically abused by 2 subgroups. First, and more commonly reported, as a cognitive enhancer by students who want to boost their academic performance, and second, by abusers of other substances for recreational abuse (Teter et al., 2005; Wilens et al., 2008; Bagot & Kaminer, 2014). In a systemic review, Wilens and colleagues showed that the base rate of MPH abuse was about 5% to 35% in college-aged individuals (Wilens et al., 2008). However, in Iceland, the base rates of oral and nasal abuse are unknown.
Intravenous (IV) abuse of MPH has rarely been reported although its IV abuse potential was reported as early as in 1963 (McCormick & McNeel, 1963; Lucas & Weiss, 1971). Only a few case reports and one case series have been published on IV MPH abuse in which it has been indicated that medical and psychiatric complications such as depression, syncope, hallucinations, and paranoia are common consequences of such abuse (Lucas & Weiss, 1971; Wiley, 1971; Spensley & Rockwell, 1972; Parran & Jasinky, 1991).
Clinical experience shows an ongoing trend for IV MPH abuse in Iceland. In 2010, about 90% of all IV abusers (224 patients) who were admitted to the largest treatment center in Iceland had abused IV MPH (Sigurjonsson, 2011). It is imperative to record and report the IV abuse potential of common prescription medicines such as MPH. Clinicians treating ADHD must be aware of its abuse potential and government agencies that decide public policies be informed. The aim of this study was to investigate the prevalence of IV abuse of MPH among inpatients reporting any IV substance abuse that sought detoxification treatment in Iceland. Furthermore, to investigate whether IV MPH is abused more by Icelandic IV abusers than amphetamine, because prior reports from Iceland have shown that amphetamine has been the most common substance of choice among Icelandic IV abusers (SAA—National Center of Addiction Medicine, 2007).
MATERIALS AND METHODS
Study Design
A descriptive population-based cross-sectional study.
Participants and Setting
Consecutively admitted substance abusers for detoxification treatment that had abused substances intravenously in the past 30 days before admission were asked to participate in the study. Participants were recruited from all 3 detoxification centers in Iceland between March 31, 2012, and March 31, 2013. The detoxification centers were Mental Health Services at the National University Hospital, SAA—Vogur National Center of Addiction Medicine, and Hladgerdarkot. The Mental Health Services at the National University Hospital provide services for those suffering from substance abuse disorder and physical and mental complications and offer both acute and elective admissions. SAA—Vogur National Center of Addiction Medicine is the largest detoxification center in Iceland, providing services for subjects with substance abuse disorder who do not have symptoms of serious mental illness, and offers both acute and elective admissions. Hladgerdarkot, a privately run not-for-profit facility, offers only elective admissions.
The total population of Iceland is 325.671 (Statistic Iceland, 2014) and the total number of regular IV abusers of any substance in Iceland has been estimated to be between 400 and 550 (SAA—Vogur National Center of Addiction Medicine, 2010). During this 12-month period, 108 participants were recruited, representing approximately 20% of all active IV substance abusers in the Icelandic population.
Eligible participants were identified by employers at the 3 detoxification centers at admission through medical history and medical records. Each potential participant received an introduction letter about the study. Those willing to participate signed an informed consent and the interviewers were notified and arrived at the detoxification center within 2 days. All participants were interviewed face to face by 2 of the authors (G.D.B. and H.B.) in an assessment interview that usually lasted for half an hour. Those younger than 18 years, pregnant, suicidal, psychotic, manic, or physically too unstable to participate in the study were excluded. Very few patients, only 4 out of 53 (8%), of those invited to take part refused to do so at the main research site where most of the patients (45%) were recruited. The other 2 sites were unable to register those who refused participation for administrative reasons.
Instrument
A semistructured interview protocol was designed and used in the study because no current protocols are designed specifically for MPH abuse. No other additional sources for data collection were used. After recording sociodemographic data, participants were asked which licit and illicit substances (alcohol, cannabis, amphetamine, cocaine, crack-cocaine, MPH, heroin, opioids, benzodiazepam, ecstasy, hallucinogenic substances, pregabalin/gabapentin) they had abused, both IV and non-IV (oral and/or nasal) in the last 30 days and lifetime abuse. Moreover, what was their preferred IV substance and which substance they had most commonly abused during the past 1 month, what was the first IV substance they had ever abused, their age at first injection, previous substance abuse treatments, risk-seeking behavior, total length of abstinence, and whether they had ever been convicted of crimes or been sentenced to prison. Sociodemographics was defined on the basis of their highest level of education, type of housing, type of income, and employment status. Duration of abstinence was defined as the cumulative time of abstinence of any substance abuse except tobacco. Risk-seeking behavior included sharing needles, unprotected sex, and prostitution. Age of substance abuse onset was defined as the age when the participants stated that their substance abuse had become problematic for any substance except tobacco. Abuse was defined according to The Analgesic, Anesthetic, and Addiction Clinical Trials, Translation, Innovations, Opportunities, and Networks (ACTTION) recommendation: “Involves any intentional, nontherapeutic abuse of a drug product or substance, even once, for the purpose of achieving a desirable psychological or physiological effect” (Smith et al., 2013).
A question on which IV substance was first abused was added to the questionnaire after the study had commenced (n = 98). Only those participants who had abused IV MPH during the past 30 days answered the question why they had chosen IV MPH rather than other IV stimulants (n = 95).
Statistics
All data were coded, stored, and analyzed using SPSS 11 (PC; SPSS Inc., Chicago, Illinois). When comparing 2 continuous variables, a Student t test was used. Fisher exact test (2-tailed) was used to check for nonrandom associations for categorical variables in contingency tables. In all calculations, a 2-tailed P value < 0.05 was considered statistically significant.
Because the sample size is modest, the variables are more likely to follow an uneven distribution and standard deviations for some variables are close to the mean. Outliers were considered an important part of the sample and were not excluded. Both medians and means are therefore presented.
Missing Values
Missing values for participants who could not or were not able to answer some of the questions represented only 0.35% of all answers.
Ethics
The study was approved by the Icelandic Bioethics Committee (VSNb2012020009/03.15) and reported to the Icelandic Data Protection Authority (2012020272HGK/–). The information disclosed during the interview was confidential and did not affect current or future treatments and was not entered into the medical records. The participants could omit any question and withdraw at any time but no one did.
RESULTS
A total of 108 inpatients were interviewed, mean age was 33 years, and the majority were men (63%). As a group, the participants had a low educational attainment and a poor work attendance record, resulting in a high proportion receiving social benefits. The sociodemographic features of the sample are presented in Table 1. The sociodemographics did not differ significantly between treatment centers.
TABLE 1. Summary Data of Sociodemographics and Risk-Seeking Behavior of 108 Treatment-Seeking Patients Reporting Intravenous Substance Abuse in the Past 30 Days Before Inpatient Detoxification*.
| Characteristics | [mean (±SD)] or % (n) |
|---|---|
| Age | [33 (10.2)] |
| Male | 58 (63) |
| Marital status | |
| Single/separated/divorced | 76 (82) |
| Married/cohabiting | 24 (26) |
| Offsprings | 63 (68) |
| Education | |
| Finished primary school† | 57 (61) |
| Did not finish primary school | 23 (25) |
| Higher education than primary school | 20 (20) |
| Housing | |
| Homeless | 34 (37) |
| Own or rent an apartment | 25 (27) |
| Staying with a family member | 20 (22) |
| Council apartment | 18 (19) |
| Halfway house | 2 (2) |
| Other | 1 (1) |
| Social status | |
| Social welfare benefits | 82 (89) |
| Unemployment benefits | 9 (10) |
| No benefits | 8 (9) |
| Employment | |
| Disabled | 53 (57) |
| Unemployed | 35 (38) |
| Full- or part-time employment | 11 (12) |
| Risk-seeking behavior | |
| Unprotected sex during the past 30 days | 66 (70) |
| Shared needles during the past 30 days | 29 (31) |
| Prostitution during the past 30 days | 3 (3) |
| Other | |
| Convictions | 65 (70) |
| More than 10 detoxification treatments | 63 (68) |
| Imprisonments | 38 (41) |
*No significant differences were observed between treatment centers. Data are presented as % (n) or mean ± standard deviation (SD) as appropriate.
†Primary school is obligatory in Iceland from age 6 to 16 years. Council apartment: Housing provided by local social services.
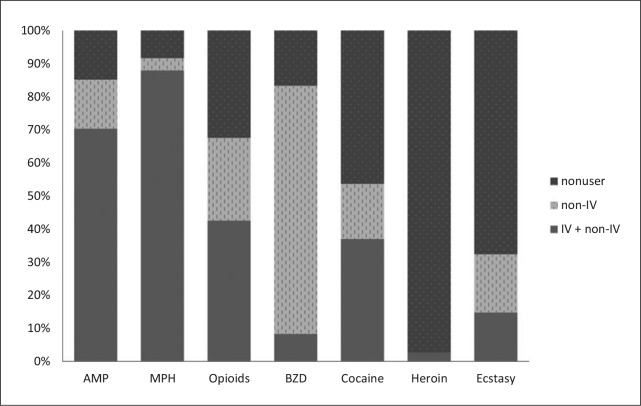
The vast majority of the 108 participants, 95 (88%; 95% confidence interval [CI], 0.82-0.94), reported having abused IV MPH in the past 30 days. There were no significant differences observed between males and females (P = 0.25). Amphetamine IV abuse was reported by 70% in the past 30 days and was significantly less common than IV MPH abuse (88%) in the same period (P = 0.004). No significant differences were observed in the prevalence of MPH IV abuse between the main research site, Landspitali University Hospital, and the other 2 detoxification centers (P = 0.77). All substances abused and route of administration among participants are shown in Figure 1. One participant reported abusing heroin exclusively IV, whereas all others who reported IV abuse also reported using a non-IV route.
FIGURE 1.
Substances abused IV and non-IV 30 days before admission of 108 participants. AMP indicates amphetamine; BZD, benzodiazepines; IV, intravenous; MPH, methylphenidate. One participant had abused only IV heroin and is included in the IV + non-IV group.
The mean age at the onset of substance abuse was 16 ± 4.5 years (median = 15 years, range 6-36 years). Mean age of first substance injection was 22.5 ± 7.3 years (median = 20 years, range 13-59 years). Most participants in the study had gone through many years of substance abuse with frequent inpatient detoxification treatments and a relatively short total duration of abstinence (Table 2).
TABLE 2. Self-Reported Substance Abuse History of 108 Participants.
| Variable | Mean ± SD | Median (Range) |
|---|---|---|
| Age of substance abuse onset, y* | 15.9 ± 4.5 | 15.0 (6.0-36.0) |
| Age of first IV substance abuse, y | 22.5 ± 7.3 | 20.0 (13.0-59.0) |
| Duration of IV substance abuse, y | 10.4 ± 9.5 | 7.0 (0.0-38.0) |
| Duration of MPH abuse, mo | 56.6 ± 59.8 | 36.0 (0.0-276.0) |
*Duration of abstinence was defined as the cumulative time of abstinence of any substance abuse except tobacco. Age of substance abuse onset was defined as age when the patient experienced substance abuse becoming problematic of any substance except tobacco.
†Duration of MPH abuse was defined as abusing MPH either non-IV or IV
IV, intravenous.
Altogether 99 (92%; 95% CI, 0.86-0.96) participants also reported having abused MPH non-IV in the past 30 days. In total, 85% and 68% of the sample reported non-IV abuse of amphetamine and prescription opioids, respectively.
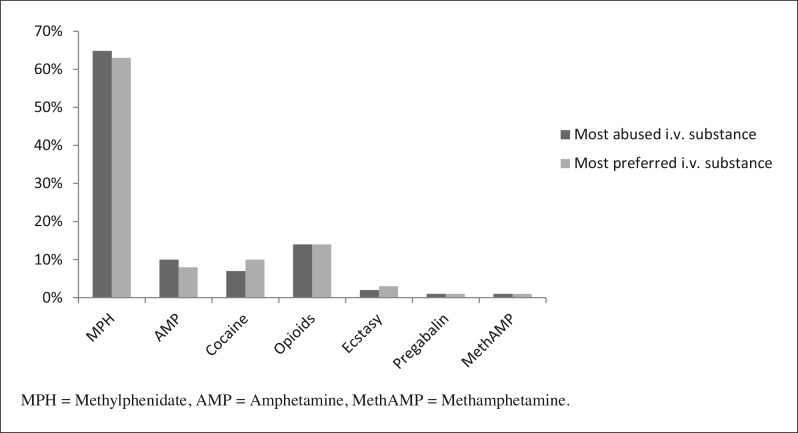
When participants were asked which IV substance they preferred and which substance they had abused most commonly during the past 30 days, MPH was both reported most frequently as the preferred IV substance (63%) and most commonly abused (65%, Fig. 2). Of those who reported MPH to be the most commonly substance abused (n = 70), 91% reported that MPH was also their preferred substance. Furthermore, it was the most frequently abused and preferred substance for both males (62% and 59%, respectively) and females (69% and 69%, respectively).
FIGURE 2.
Substances that 108 participants cited as their most commonly abused and preferred IV substance during the past 30 days. AMP indicates amphetamine; MethAMP, methamphetamine; MPH, methylphenidate.
The vast majority of participants had abused many substances during their lifetime. All those who reported IV abuse also reported some non-IV administration. Almost all participants (96%) had abused IV MPH, but additionally 3% reported non-IV abuse of MPH. Intravenous amphetamine abuse was reported by 94% and non-IV abuse by 5%. Furthermore, IV cocaine and opioids were abused roughly by 4 out of 5 participants (85% and 81%, respectively) and 14% of participants had abused those substances only non-IV during their lifetime. Intravenous abuse of ecstasy was reported by 70% and non-IV abuse by 26% of participants.
For most participants, stimulants were by far the most commonly reported first ever IV substance abused (n = 98, 85%), amphetamine (40%), followed by MPH (30%), cocaine (13%), and ecstasy (2%). Altogether 16 participants (15%) reported abusing only IV MPH. The proportion of individuals who reported MPH as their first IV substance was similar among polysubstance IV abusers and those using only MPH IV (P = 1.00).
As shown in Figure 3, the majority of the participants reported a preference for MPH compared with other IV stimulants. Participants were asked to detail their reasons for this preference. Knowing for certain what substance they were abusing (77%), a better intoxication effect (72%) and knowing the exact dose of abuse (72%) were the 3 main reasons for preferring MPH over other IV stimulants. Some 38% of the sample reported MPH to be more readily available, 22% said that MPH was cheaper and 12% reported that MPH had fewer side effects than other IV stimulants.
FIGURE 3.
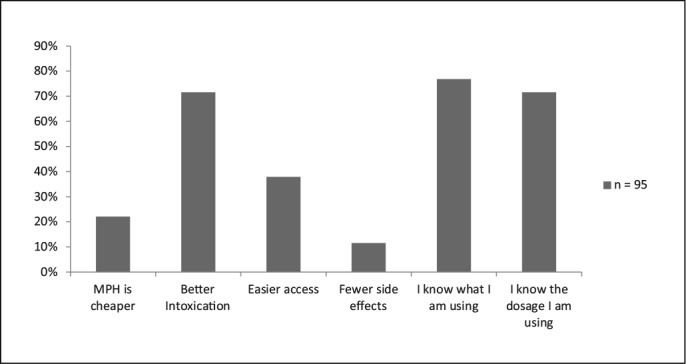
Reasons why IV abusers prefer IV MPH rather than other IV stimulants (n = 95). Only participants who had abused IV MPH in the last 30 days answered this question. Missing values range from 3% to 7%.
Participants who reported MPH as their first IV substance abused had a significantly shorter duration of IV substance abuse than those who reported other substances as their first IV substance (mean = 4.2 and 13.4 years, respectively; t = 6.3; n = 92; 95% CI, 6.26-12.03, P < 0.001). Four in 10 (42%) of those participants with a lifetime duration of IV substance abuse of 10 years or less reported MPH as their first IV substance abused as opposed to 30% in the whole sample. The vast majority, 60 (91%), most often purchased MPH illicitly, whereas 11 (17%) had received MPH prescriptions from health care professionals and 3 (5%) had purchased MPH abroad.
DISCUSSION
This is the first nationwide cross-sectional study that reports extensive IV abuse of MPH. The 108 participants had a low educational level and a limited work attendance similar to what has been reported in other IV substance abuse studies (Vlahov et al., 2004). In total, 88% of the participants reported having abused IV MPH at least once in the past 30 days before admission, and an even higher proportion, 92%, had abused non-IV MPH during the past 30 days. Methylphenidate was by far the most frequently abused substance, both IV and non-IV (Fig. 1). Furthermore, 63% reported that MPH was their IV substance of choice (Fig. 2).
Changes in IV substance abuse in Iceland
In Iceland, only 2 drugs are approved for the treatment of ADHD, MPH, and atomoxetine. A growing number of clinical cases of MPH abuse receiving detoxification in Iceland over the past decade indicate that MPH abuse has become relatively common in Iceland. The MPH abuse has gained increasing attention in the medical community and the media in the wake of rapidly increasing MPH prescriptions in recent years (Zoëga et al., 2009, 2011; Halldorsson, 2010). Traditionally, amphetamine had been the substance of choice among Icelandic IV abusers and it was frequently the first IV substance abused in the past according to annual reports (SAA—Vogur National Center of Addiction Medicine, 2007). However, in recent years there has been a steady shift toward IV abuse of MPH (SAA—Vogur National Center of Addiction Medicine, 2010).
In this study, overall 30% reported MPH as the first IV substance ever abused but among those who had commenced IV abuse within the past decade, 42% reported MPH as the first IV substance ever abused. Therefore, MPH was the most commonly reported first IV substance abused among those who were younger and had shorter duration of IV substance abuse. It is alarming that a prescription medicine commonly prescribed to children and adolescents but increasingly to adults has become the predominant substance of choice for new IV substance abusers in Iceland.
It is not clear why IV MPH abuse has become so common in Iceland. Such outbreaks of abuse of prescription substances have been reported in other countries and are by no means limited to Iceland. For instance, IV abuse of temazepam became problematic in the United Kingdom during the late 1980s (Strang et al., 1992). Furthermore, there is some evidence that the antipsychotic drug quetiapine may have an abuse potential (Klein-Schwartz et al., 2014). Another explanation could possibly be the increased awareness of ADHD as a disabling mental disorder in recent years and the relatively good access to psychiatrists in Iceland (Economics Co-operation & Development, 2011).
As far as we know, MPH IV abuse has not yet surfaced as a major public health concern in other countries. This begs the question whether the drug scene in Iceland is in some respect unique or different from neighboring countries or whether this development arose simply because of the high prevalence of prescription and the increasing availability of MPH. If the latter is true, IV MPH abuse is also likely to become endemic in many other countries where prescriptions of MPH have been steadily increasing. Several facts argue against such explanations of MPH IV abuse in Iceland. First, with the exception of heroin, there is no scarcity of illegal drugs in Iceland, yet most of the study participants prefer MPH over other IV substances of abuse. The majority of participants also report that access to MPH is not better than that to other stimulants. Second, capital controls after the financial crisis in 2008 did not seem to push consumption suddenly toward prescription substances, because alarming signs of MPH abuse had already appeared several years before the crisis. Interestingly, there are no indications that the abuse of other prescription drugs, such as opioids, has been on the rise in Iceland between 2007 and 2012 (The Icelandic Directorate of Health, 2013). Third, only a minority of abusers reported that MPH is cheaper than other stimulants. The street prices of cannabis and amphetamine have remained relatively stable, whereas the price of MPH has, in fact, increased severalfold during the last 10 years, which is hard to explain in any other way than as a result of high demand for the substance (SAA—Vogur National Center of Addiction Medicine, 2013). Fourth, The Directorate of Health and the Ministry of Welfare in Iceland have recently increased surveillance and tightened regulations for MPH prescriptions to prevent the highly prevalent misuse and abuse of MPH but with limited results so far (The Icelandic Ministry of Welfare, 2011). For instance, only certain specialists can initiate MPH treatment (psychiatrists, child and adolescent psychiatrists, neurologists, and pediatricians). Furthermore, the Icelandic electronic prescription monitoring database has been made accessible for doctors by The Directorate of Health to enable doctors to monitor possible misuse and/or abuse. Last, and probably most importantly, the IV abusers report MPH as their preferred IV substance and the most commonly abused substance as well.
Study Limitations
The study sample consists of a heterogeneous group where some participants had had a long history of IV abuse, whereas others had relatively short periods of such abuse. Hence the data have uneven distribution and standard deviations for some variables (Table 2) are close to the mean. Furthermore, the exact number of IV abusers in Iceland is not known, but the estimated number is between 400 and 550 (SAA—Vogur National Center of Addiction Medicine, 2010). We managed to recruit up to one fifth of these but admittedly we have no means of knowing if and how treatment-seeking IV abusers may differ from those who are more reluctant to seek treatment with regard to IV abuse of MPH.
Study Strengths
This is a nationwide population-based study. Data collection took place at all detoxification centers in Iceland, thereby reducing the risk of referral and selection bias. Only 2 members of the study group gathered the data, thereby increasing uniformity of data collection. In Iceland, there is minimal gate keeping into detoxification treatment in all 3 inpatient centers for detoxification. These 3 facilities where all participants were recruited therefore provide an ideal setting to collect information from treatment-seeking IV abusers, a group generally difficult to recruit for research.
CONCLUSIONS
This study confirms that MPH has IV abuse potential and shows that MPH has become the most commonly abused IV substance in Iceland. This has happened in the wake of rapidly rising prescriptions over the past decade because of increasing demand for pharmaceutical treatment of ADHD. The results have grave implications, not only for Iceland, but also for other countries because this problem may possibly appear in countries where MPH prescriptions are on the rise and have become much more prevalent than before. Vigilance and close monitoring of the use and abuse of MPH are strongly recommended in our view.
Future Research
It is important to further verify and characterize the pattern of IV MPH abuse in Iceland and elsewhere. More research is needed, for instance, on whether some available forms of MPH formulations are more commonly abused or preferred to others by IV substance abusers. Future studies should also identify the effects of IV MPH abuse on morbidity and mortality. Finally, it is important to investigate the various intoxication parameters of different MPH formulations.
ACKNOWLEDGMENTS
We thank SAA—Vogur National Center of Addiction Medicine/medical clinics, Hladgerdarkot detoxification Centre, Brynjar Emilsson, Elín Hanna Jónsdóttir, and all the participants.
Ethical approval: This study was approved by The National Bioethics Committee (VSNb2012020009/03.15), Data Protection Authority (2012020272HGK/–) and The Bioethics Committee at the Landspitali University Hospital of Iceland (Tilv.16). Informed consent was given by all participants.
Footnotes
None of the authors have competing interests. G.D. Bjarnadottir did parts of this research during 4 months' leave from her clinical duties at Landspitali University Hospital. This study was conducted without any influence from the Hospital or other organizations. G. D. Bjarnadottir received a travel grant from the Nordic Psychiatric Association in June 2012. No other relationships or activities that could appear to have influenced the submitted work.
Author contribution: Bjarnadottir, Magnusson, Haraldsson, Steingrimsson, and Rafnar designed the study. Bjarnadottir and Bragadottir acquired the data. Bjarnadottir, Haraldsson, Rafnar, Steingrimsson, Sigurdsson, and Magnusson drafted the paper. Bjarnadottir, Magnusson, Haraldsson, Rafnar, Sigurdsson, Johannsson, and Steingrimsson take the responsibility for the integrity of the data and the accuracy of the data analysis. All authors have read and understand the Instructions for Authors. Bjarnadottir, Haraldsson, and Magnusson are guarantors and affirm that the manuscript is honest, accurate, and transparent and no important aspects of the study have been omitted and all discrepancies have been explained. All authors had access to the data, interpreted the data, critically revised the draft for important intellectual content, and gave final approval of the manuscript to be published. Bjarnadottir presented preliminary results at the European Psychiatry Congress in Nice, 2013.
REFERENCES
- Bagot KS, Kaminer Y. Efficacy of stimulants for cognitive enhancement in non–attention deficit hyperactivity disorder youth: a systemic review. Addiction 2014;109:547–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castle L, Aubert RE, Verbrugge RR, et al. Trends in medication treatment for ADHD. J Atten Disord 2007;10:335–342. [DOI] [PubMed] [Google Scholar]
- Dalsgaard S, Nielsen HS, Simonsen M. Five-fold increase in national prevalence rates of attention-deficit/hyperactivity disorder medications for children and adolescents with autism spectrum disorder, attention-deficit/hyperactivity disorder, and other psychiatric disorders: a Danish register-based study. J Adolesc Psychopharmacol 2012;23:432–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Economics Co-operation & Development: OECDiLibary statistics. Psychiatrists Per 100.000 Population, 2009 and Change Between 2000-2009. 2011. Available at: http://www.oecd-ilibrary.org/sites/health_glance-2011-en/03/06/index.html;jsessionid=2gq87b2juueg7.x-oecd-live-01?contentType&itemId=/content/chapter/health_glance-2011-25-en&containerItemId=%2Fcontent%2Fchapter%2Fhealth_glance-2011-25-en&accessItemIds=/content/book/health_glance-2011-en&mimeType=text/html&_csp_=43ca8945549e270ddddfd32e4873bba5 Archived at Webcite® at http://www.webcitation.org/6SWze4nay. Accessed September 12, 2014.
- Halldorsson M. Rítalín til góðs eða ills. [Ritalin for better or worse]. Laeknabladid 2010;96:519. [Icelandic] [DOI] [PubMed] [Google Scholar]
- Heal DJ, Cheetham SC, Smith SL. The neuropharmacology of ADHD drugs in vivo: insights on efficacy and safety. Neuropharmacology 2009;57:608–618. [DOI] [PubMed] [Google Scholar]
- Kaye S, Darke S. The diversion and misuse of pharmaceutical stimulants: what do we know and why should we care. Addiction 2012;107:467–477. [DOI] [PubMed] [Google Scholar]
- Klein-Schwartz W, Schwartz E, Anderson B, et al. Evaluation of quetiapine abuse and misabuse reported to poison centers. J Addict Med 2014;8:195–198. [DOI] [PubMed] [Google Scholar]
- Kollins SH. Comparing the abuse potential of methylphenidate versus other stimulants: a review of available evidence and relevance to the ADHD patient. J Clin Psychiatry 2003;64:14–18. [PubMed] [Google Scholar]
- Kollins SH, MacDonald EK, Rush CR. Assessing the abuse potential of methylphenidate in nonhuman and human subjects: a review. Pharmacol Biochem Behav 2001;68:611–627. [DOI] [PubMed] [Google Scholar]
- Lucas A, Weiss M. Methylphenidate hallucinosis. JAMA 1971;217:1079–1081. [PubMed] [Google Scholar]
- McCormick TJ, McNeel T. Acute psychosis and Ritalin abuse. Tex State J Med 1963; 59:99–100. [Google Scholar]
- Parran TV, Jasinski DR. Intravenous methylphenidate abuse. Prototype for prescription drug abuse. Arch Intern Med 1991;151:781–783. [PubMed] [Google Scholar]
- Riggs PD, Winhusen T, Davies RD, et al. Randomized controlled trial of osmotic-release methylphenidate with cognitive-behavioral therapy in adolescents with attention-deficit/hyperactivity disorder and substance use disorder. J Am Acad Child Adolesc Psychiatry 2011;50:903–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAA—Vogur National Center of Addiction Medicine. Annual Report. 2007. [Icelandic]. Available at: http://saa.is/Files/Skra_0022713.pdf, Archived at Webcite at http://www.webcitation.org/6O2dM8QWm. Accessed March 13, 2014.
- SAA—Vogur National Center of Addiction Medicine. Annu Rep. 2010. [Icelandic]. Available at: http://www.saa.is/Files/Skra_0042334.pdf, Archived at Webcite at http://www.webcitation.org/68Xoj1gVI. Accessed May 13, 2011.
- SAA—Vogur National Center of Addiction Medicine. 2013. [Icelandic]. Available at: http://www.saa.is/islenskivefurinn/samtokin/frettir/nr/178800/, Archived at Webcite® at http://www.webcitation.org/6O16cB2ZG. Accessed March 12, 2014.
- Scheffler RM, Hinshaw SP, Modrek S, et al. The global market for ADHD medications. Health Aff 2007;26:450–457. [DOI] [PubMed] [Google Scholar]
- Sigurjonsson H. Fjölgun HIV-smitaðra er áhyggjuefni—segir Valgerður Rúnarsdóttir á Vogi [Worrying increase in HIV infections—says Valgerdur Runarsdottir at Vogur Hospital]. Laeknabladid 2011;97:430–432. [Icelandic]. [Google Scholar]
- Smith SM, Dart CD, Katz NP, et al. Classification and definition of misuse, abuse, and related events in clinical trials: ACTTION systematic review and recommendations. PAIN® 2013;154:2287–2296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spensley J, Rockwell DA. Psychosis during methylphenidate abuse. N Engl J Med 1972; 286:880–881. [DOI] [PubMed] [Google Scholar]
- Statistic Iceland. Population by Sex and Age 1841–2014. 2014. Available at: http://www.hagstofa.is/?PageID=2593&src=https://rannsokn.hagstofa.is/pxis/Dialog/varval.asp?ma=MAN00101%26ti=Mannfj%F6ldi+eftir+kyni+og+aldri+1841%2D2013+%26path=../Database/mannfjoldi/Yfirlit/%26lang=3%26units=Fjöldi, Archived at Webcite® at http://www.webcitation.org/6O18dZbwB. Accessed March 12, 2014.
- Strang J, Seivewright N, Farrell M. Intravenous and other novel abuses of benzodiazepines: the opening of Pandora's box? [Editorial]. Br J Addict 1992;87:1373–1375. [DOI] [PubMed] [Google Scholar]
- Teter CJ, McCabe SE, Cranford JA, et al. Prevalence and motives for illicit abuse of prescription stimulants in an undergraduate student sample. J Am Coll Health 2005;53: 253–262. [DOI] [PubMed] [Google Scholar]
- The Icelandic Directorate of Health. The Prescription Database 2013. Iceland: The Icelandic Directorate of Health, 2013. [Google Scholar]
- The Icelandic Ministry of Welfare. Tillögur um aðgerðir til að stemma stigum við misnotkun Methýlfenídat-lyfja og annarra lyfseðilskyldra lyfja. [Recommendations for action to reduce the abuse of methylphenidate and other prescription drugs]. Iceland: The Icelandic Ministry of Welfare, 2011. Available at: http://www.velferdarraduneyti.is/media/ritogskyrslur2011/Tillogur-vinnuhops–metylfenidat.pdf, Archived at Webcite® at http://www.webcitation.org/6O10Ft6xo. Accessed March 13, 2014. [Google Scholar]
- United Nations: The International Narcotics Control Board. Annual Report. 2012. Available at: http://incb.org/documents/Publications/AnnualReports/AR2012/AR_2012_E.pdf, Archived at Webcite® at http://www.webcitation.org/6O2co1PA3. Accessed March 12, 2014.
- United Nations: The International Narcotics Control Board. Psychotropic Substances 2013: Statistics for 2012. 2013. Available at: http://www.incb.org/documents/Psychotropics/technical-publications/2013/en/5_Part_II_comments.pdf, Archived at Webcite® at http://www.webcitation.org/6SVjCtkuy. Accessed September 11, 2014.
- Vlahov D, Wang CL, Galai N, et al. Mortality risk among new onset injection drug abusers. Addiction 2004;99:946–954. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Fowler JS, Wang GJ, et al. Role of dopamine in the therapeutic and reinforcing effects of methylphenidate in humans: results from imaging studies. Eur Neuropsychopharmacol 2002;12:557–566. [DOI] [PubMed] [Google Scholar]
- Wang G-J, Volkow ND, Hitzemann RJ, et al. Behavioral and cardiovascular effects of intravenous methylphenidate in normal subjects and cocaine abusers. Eur Addict Res 1997;3:49–54. [Google Scholar]
- Wilens TE, Adler LA, Adams J, et al. Misuse and diversion of stimulants prescribed for ADHD: a systematic review of the literature. J Am Acad Child Adolesc Psychiatry 2008;47:21–31. [DOI] [PubMed] [Google Scholar]
- Wiley R. Abuse of methylphenidate (Ritalin). New Engl J Med 1971:285:464. [PubMed] [Google Scholar]
- Zoëga H, Baldursson G, Hrafnkelsson B, et al. Psychotropic drug use among Icelandic children: A nationwide population-based study. J Child Adoles Psychopharmacol 2009;19:757–764. [DOI] [PubMed] [Google Scholar]
- Zoëga H, Furu K, Halldórsson M, et al. Use of ADHD drugs in the Nordic countries: a population-based comparison study. Acta Psychiatr Scand 2011;123:360–367. [DOI] [PubMed] [Google Scholar]