Abstract
Objective
To develop and validate a survey instrument designed to measure team dynamics in primary care.
Data Sources/Study Setting
We studied 1,080 physician and nonphysician health care professionals working at 18 primary care practices participating in a learning collaborative aimed at improving team-based care.
Study Design
We developed a conceptual model and administered a cross-sectional survey addressing team dynamics, and we assessed reliability and discriminant validity of survey factors and the overall survey's goodness-of-fit using structural equation modeling.
Data Collection
We administered the survey between September 2012 and March 2013.
Principal Findings
Overall response rate was 68 percent (732 respondents). Results support a seven-factor model of team dynamics, suggesting that conditions for team effectiveness, shared understanding, and three supportive processes are associated with acting and feeling like a team and, in turn, perceived team effectiveness. This model demonstrated adequate fit (goodness-of-fit index: 0.91), scale reliability (Cronbach's alphas: 0.71–0.91), and discriminant validity (average factor correlations: 0.49).
Conclusions
It is possible to measure primary care team dynamics reliably using a 29-item survey. This survey may be used in ambulatory settings to study teamwork and explore the effect of efforts to improve team-based care. Future studies should demonstrate the importance of team dynamics for markers of team effectiveness (e.g., work satisfaction, care quality, clinical outcomes).
Keywords: Survey, primary care, team dynamics, team effectiveness
There is increasing recognition that team-based approaches to delivering care in ambulatory settings may be critical for improving health care services and outcomes for patients. When patients require services of nurses, social workers, pharmacists, case managers, receptionists, or schedulers in addition to their primary care providers (e.g., physicians, nurse practitioners, and physician assistants), quality and value depend on the ability of these professionals to work together in a coordinated fashion. Prior research has associated team-based primary care with improved care for patients with specific diagnoses (e.g., diabetes and depression) (Lemieux-Charles and McGuire 2006). However, findings have been mixed, given differences in the way teams were designed and implemented. Nevertheless, team-based care has become a key tenet of efforts to transform primary care practices into patient-centered medical homes (PCMHs) (The Patient-Centered Primary Care Collaborative 2007; National Committee for Quality Assurance 2014), and stakeholders are considering how to structure payments to primary care teams as opposed to individual physicians (Blumenthal et al. 2013).
Despite heightened interest in improving teams and teamwork, little is known about how to assess team dynamics in ambulatory settings. While several survey instruments measure selected aspects of teamwork (e.g., conditions for team effectiveness), few tools comprehensively capture the team dynamics that evidence suggests may be valuable in ambulatory settings (Valentine, Nembhard, and Edmondson in press). Existing measures of teamwork are also either too specific (e.g., focused on geriatric care, targeted to nurses and physicians only) or not specific enough (i.e., thought applicable to any health care setting). Other surveys are designed for non-U.S. settings. Few surveys have measured, and even fewer have satisfied, standard psychometric criteria for validating surveys.
A survey instrument that measures ambulatory-based team dynamics is needed because teams in these settings face challenges that are less prominent in inpatient care: high rates of patient and provider turnover, wide variation in patient needs, a need for provider coordination within and beyond facility boundaries, and increasing expectations of primary care providers to engage patients in their care. Assessing team dynamics in ambulatory settings would enable identification of team dynamics most critical for desired health care outcomes, and this would make more targeted interventions possible.
To address this opportunity, we developed a novel survey that is grounded in an evidence-based conceptual model and draws on previous, psychometrically tested instruments. We administered the survey to all physician and nonphysician health care professionals caring for patients within 18 primary care practices in Massachusetts who are working to improve team-based care as part of a primary care learning collaborative.
In this paper, we begin by presenting our conceptual model for how to measure team dynamics in ambulatory settings. We then describe the development of the survey instrument, explore its psychometric properties, and discuss implications for the survey, future research, and its application in ambulatory care.
Conceptual Model of Primary Care Team Dynamics
Based on research about effective teaming in a variety of health care settings (Toseland, Palmer-Ganeles, and Chapman 1986; Heinemann et al. 1999; Hyer et al. 2000; Millward and Jeffries 2001; Gittell 2002; Leipzig et al. 2002; Lemieux-Charles and McGuire 2006; Nagpal et al. 2010; Schroder et al. 2011; Jesmin, Thind, and Sarma 2012), we developed a framework for team dynamics in primary care, which applies to ambulatory settings in general. We define effective team dynamics according to the following criteria: (1) team performance (i.e., the product of teamwork meets the expectations of those who use it); (2) member satisfaction (i.e., each team member's experience contributes to his or her personal well-being and development); and (3) team adaptation (i.e., the team experience enhances each member's capability to work and learn together in the future) (Nadler, Hackman, and Lawler 1979). Our conceptual model (Figure1a) posits that effective team performance begins with a set of enabling conditions that facilitate teaming. When present, these conditions promote shared understanding and supportive processes, which in turn encourage group members to act and feel like a team. When these conditions are met, group members will report that the care they deliver is more effective and efficient for both patients and professionals. Implied by our conceptual model—though not explored in this paper—is the belief that survey measures of team member perceptions will correspond with objective measures of team effectiveness.
Figure 1.
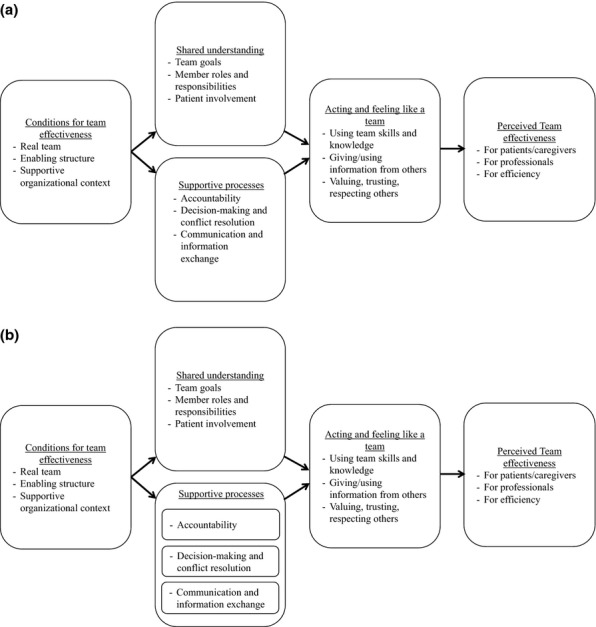
(a) Conceptual Model of Primary Care Team Dynamics Prior to Psychometric Assessment. (b) Modified Conceptual Model of Primary Care Team Dynamics
Note. (a) This model reflects the conceptual model of primary care team dynamics prior to psychometric assessment, which treats the three supportive processes as one factor. (b) This model reflects modifications made as a result of psychometric evaluation. Specifically, it treats the three supportive processes as separate factors.
Conditions for Team Effectiveness
Prior research demonstrates that teams are more likely to be effective when certain types of organizational conditions are present (Hackman 1987, 1990, 2002; Wageman 2001; Wageman, Hackman, and Lehman 2005). Our conceptual model focuses on three enabling conditions, which may vary substantially in primary care settings: (1) a “real”, that is, stable team; (2) clearly described responsibilities and predetermined norms; and (3) supportive rewards and incentives. Stable membership is helpful for teams because it promotes collective responsibility for a common purpose and facilitates collective learning over time. Clearly described responsibilities and predetermined norms increase the likelihood of effective teamwork because they clarify and encourage expected behaviors. Supportive rewards and incentives align financial or reputational rewards with the achievement of team-based (as opposed to individual) goals and hiring practices, training programs, and information systems, such that they promote teamwork and improvement. Our model does not explicitly focus on other enabling conditions, including team coaching (currently largely unavailable in primary care settings) and a compelling direction (we anticipate that medical professionals would report feeling compelled to act in patients’ best interests) (American Medical Association 2001; Snyder 2012). Together, the three conditions for team effectiveness create a foundation for the next two elements in our model.
Shared Understanding
Our model suggests that three characteristics increase a team's likelihood of developing a shared understanding about key aspects of the team: having members who (1) recognize themselves as part of the team, (2) receive formal and informal signals about what is expected, and (3) experience incentives and support for their participation. In primary care settings, we specifically expect shared understanding to emerge around issues like team goals (Lemieux-Charles and McGuire 2006; Senior and Swailes 2007; Klein et al. 2009; Schroder et al. 2011), member roles and responsibilities (Cannon-Bowers et al. 1995; Klein et al. 2009; Shuffler, DiazGranados, and Salas 2011), and patient engagement (Remmers et al. 2009; Stacey et al. 2011; Barry and Edgman-Levitan 2012; Harvey et al. 2012; Hibbard and Greene 2013; Hibbard, Greene, and Overton 2013; King and Moulton 2013). Shared goals motivate team members to act in keeping with overall work processes, which enables improved coordination (Saavedra, Earley, and Van Dyne 1993; Gittell 2000, 2002). A shared understanding of team member roles and responsibilities matters, particularly in the context of interprofessional teams like those in primary care, which frequently include doctors, nurses, medical assistants, and others (Suter et al. 2009). A shared understanding about patients’ active participation in decisions about their care, understanding of the care plan, and needs and preferences affects the way team members (which may, according to our survey, include patients themselves) interact with each other. Indeed, an inconsistent understanding about how to engage patients may result in team members delivering very different care, with potential for undermining team dynamics, patient experience, and clinical outcomes (Gandhi et al. 2003).
Supportive Processes
Our model emphasizes three processes that support teaming in primary care: accountability, conflict resolution, and communication and information exchange. Prior research has identified the need for teams to establish processes that foster responsibility and accountability for members’ actions (Weiss and Davis 1985; Baggs 1994). Accountability is important because perceived inequalities in team members’ share of work lead to conflict and dissatisfaction (Herzberg 1968). Ensuring that team members contribute their fair share, and holding individual members personally responsible for aspects of the team's task, promotes equity and willingness to exert effort on behalf of team goals (Latané, Williams, and Harkins 1979; Katzenbach and Smith 1993; Hill 2001).
Effective processes for conflict resolution are also critical for effective teamwork. A healthy amount of task conflict is desirable to explore problems thoroughly and generate novel solutions (Hill 1995, 2001; Bradford and Cohen 1998; Leonard-Barton and Swap 1999; Edmondson, Bohmer, and Pisano 2001; Garvin and Roberto 2001). However, too much task conflict can stress relationships and lead to negative dynamics. Productive conflict management requires a systematic way to refine and critique possible solutions and make decisions in a safe environment (Hill 1995; Eisenhardt, Kahwajy, and Bourgeois 1997; Edmondson, Bohmer, and Pisano 2001; Garvin and Roberto 2001). Explicitly framing decisions as a learning process can also reduce unproductive conflict (Argyris and Schön 1978).
Lastly, communication and information exchange are critical processes for supporting effective teamwork (Weiss and Davis 1985), as they allow the ongoing mutual adjustment that ensures safe and effective care (Thompson 1967). Communication breakdowns are the most common cause of medical errors and adverse events in medicine (The Joint Commission 2013). Teams need systematic approaches for communicating information clearly, comprehensibly, and reliably (Gandhi et al. 2005). Promoting knowledge integration when information is distributed among team members requires deliberate effort to encourage those with less formal authority to speak up (Gardner, Gino, and Staats 2012), especially when information is uniquely held (Stasser, Stewart, and Wittenbaum 1995).
Acting and Feeling Like a Team
Where the conditions for team effectiveness are present, members share an understanding about the team, and they engage in processes that support teaming, our model posits that members will learn to act and feel like a team. Acting like a team includes providing and using information from other team members who possess different skills and knowledge, such that they are working interdependently to accomplish tasks (Alexander et al. 2005). Feeling like a team means perceiving a collective identity, a “real team,” in which members experience a sense of belonging. Team-oriented feelings also include valuing, trusting, and respecting other group members’ perspectives and roles (Schroder et al. 2011).
Perceived Team Effectiveness
When team members act and feel like a team, the literature suggests that group members will perceive a higher level of team effectiveness (Millward and Jeffries 2001; Kozlowski and Ilgen 2006; Lemieux-Charles and McGuire 2006; Brennan et al. 2013). According to our conceptual model, team members may perceive a team to be successful in delivering highly effective and efficient care for patients and enhancing enthusiasm and interest among the professionals on the team (Heinemann et al. 1999; Hyer et al. 2000; Leipzig et al. 2002). Our model suggests that the conditions, understanding, processes, actions/feelings, and perceptions we have described will be positively associated with perceived team effectiveness (and ultimately with objective measures of team effectiveness) in primary care.
Methods
Instrument Development
We developed our survey in conjunction with a 2-year primary care learning collaborative at Harvard-affiliated practices called the Academic Innovations Collaborative (AIC) (Bitton et al. 2014). One of the key objectives of the AIC was for participating practices to establish “teams” (if they did not already have them) and improve team dynamics. We first reviewed proposals from primary care practices participating in the learning collaborative to understand how they envisioned developing team-based care within their practices. We also studied the proposed learning collaborative curriculum. In addition, we examined a variety of survey instruments, including those discussed in a recent systematic review of teamwork surveys in health care settings (Valentine, Nembhard, and Edmondson in press) and others suggested by investigators and learning collaborative members (Heinemann et al. 1999; Hyer et al. 2000; Leipzig et al. 2002; Mahoney and Turkovich 2010; National Committee for Quality Assurance 2011; Schroder et al. 2011). Of these, we selected 10 survey instruments whose content best reflected the constructs in our conceptual model. From these, we selected groups of items that best or uniquely reflected the dimensions in our model, retaining a comprehensive and nonredundant set of items. In selecting items to represent each factor, we chose among surveys rather than combining items from multiple surveys, maintaining original survey constructs as much as possible. We conducted a series of expert reviews and carried out cognitive interviews with attending physicians, nurses, and front desk staff to test targeted respondents’ understanding of survey items (e.g., comprehensibility for staff with high-school education levels or those who were nonnative-English speakers). On the basis of these interviews, we modified survey items mostly in minor ways (e.g., wrote items at the sixth grade literacy level). We also dropped items that interviewees suggested were not applicable in the context of ambulatory care (e.g., “I feel physically safe within this hospital environment”).
The administered survey included 31 items measuring the five factors represented in our conceptual model and four demographic items assessing respondent gender, age, race, and ethnicity. Except as noted, all items used a five-point Likert response scale, ranging from 1 = Strongly Disagree to 5 = Strongly Agree. Appendix SA2 describes the content and origin of each domain.
Sample and Data Collection
The target population for this study consisted of 1,080 patient-facing health care professionals at 18 Harvard-affiliated primary care practices in Massachusetts participating in the AIC. We targeted this population using personnel lists obtained from each practice's Practice Manager. These lists contained information on each staff member's job title, description (including whether they interacted directly [e.g., reception] or indirectly [e.g., phone bank] with patients), and professional licenses, if applicable. We classified respondents into personnel types for comparing sample demographic characteristics. Though participating practices were affiliated with Harvard, they were diverse in setting (hospital-based vs. community-based), size (3–64 physicians), revenue sources (5–81 percent Medicaid, 7–40 percent Medicare), and patient demographics (ages 0 to >75 years, 15–95 percent non-white). They also varied in the type of primary care they provided (three pediatric practices, one internal medicine-pediatrics, two family medicine, and 12 internal medicine, including one with a geriatric program).
Between September 2012 and March 2013, we administered our survey electronically through subjects’ work emails. All Practice Managers sent an introductory email to their staff to notify them to expect our survey. We followed Practice Managers’ recommendations to determine specific timing for administering the initial survey (e.g., avoiding competing surveys) and reminders. Practice Managers promoted participation in our survey (e.g., through release time from clinical duties or required meetings). We also provided Practice Managers with token incentives (e.g., breakfast items) to help promote the survey.
For each practice, survey administration concluded when the practice reached or exceeded a 60 percent response or after 29 weeks following survey launch, whichever occurred first. The Institutional Review Board at the Harvard School of Public Health approved all research methods.
Statistical Analysis
First, we reverse-scored negatively worded items and assessed survey properties including item nonresponse, means, and variance. To determine the extent to which missing items would bias our results, we performed sensitivity analysis comparing results based on the original data to results based on a complete dataset generated by imputing missing values using stratified means. Results at each step in our analysis were robust to the dataset selected. In describing the sample, item means, and variance, we present results based on the original, nonimputed data.
Next, we used structural equation modeling (SEM) to perform two rounds of psychometric analysis. Given our strong conceptual model and the derivation of our items from previously validated instruments, rather than conducting a traditional exploratory factor analysis, we used SEM to test the fit of the survey data with our hypothesized model of primary care team dynamics (Byrne 2001). In doing so, we split our sample into randomly drawn halves, using the imputed dataset to maximize sample size. We used output from the first SEM, based on data from the first split-half sample, to identify minor ways of improving model fit by deleting items with factor loadings below 0.40 if they captured content similar to other items in the same factor and by adding covariances between items within factors if modification indices were 0.20 or higher (Byrne 2001). We also adjusted for spurious variance that can result when multiple scale scores come from a single survey by including a common latent factor (Podsakoff et al. 2003). Thus, our first SEM served an exploratory purpose. With the second split-half sample, we conducted a confirmatory factor analysis using SEM and accounting for common method bias to assess the goodness-of-fit of the final model derived from the initial SEM (Brown 2006). We assessed the robustness of the final model by comparing results based on the imputed data to results based on the original data, after list-wise deleting missing values.
We averaged items in each factor to create factor scores. We assessed factor reliability by computing Cronbach's alpha coefficients, which measure the internal consistency of the items comprising each scale. We also assessed the convergent and discriminant validity of the factors in our model by examining the strength of each item's correlation with its assigned scale and comparing it to its correlations with the remaining scales (Hays and Hayashi 1990).
We performed SEM using SPSS AMOS version 20 (Amos Development Corporation, Meadville, Pennsylvania, USA). All other analyses were performed using STATA 13.1 (StataCorp, College Station, Texas, USA).
Results
Response Rate
We received 732 responses for an overall response rate of 68 percent, ranging from 55 to 89 percent among practices. We excluded one observation with a value for age greater than 100, assuming this was a respondent's typographical error.
Sample Characteristics
Respondents were predominantly female (81 percent) (Table1). Approximately, one-third of respondents were 36–50 years old, and another third were older. Among respondents, 39 percent were physicians and 24 percent were administrative staff. More than half of respondents were non-Hispanic white (57 percent), and 21 percent were Hispanic. The split-half samples exhibited nonsignificant differences in distributions of demographic characteristics, suggesting randomization was successful.
Table 1.
Sample Demographics
| Total Sample | First Half-Sample | Second Half-Sample | ||||
|---|---|---|---|---|---|---|
| N | Percentage | N | Percentage | N | Percentage | |
| Total | 731 | 100 | 359 | 100 | 359 | 100 |
| Gender | ||||||
| Male | 130 | 17.78 | 59 | 16.43 | 69 | 19.22 |
| Female | 595 | 81.40 | 299 | 83.29 | 289 | 80.50 |
| Declined to answer | 6 | 0.82 | 1 | 0.28 | 1 | 0.28 |
| Age (years) | ||||||
| <30 | 72 | 9.85 | 40 | 11.14 | 31 | 8.64 |
| 30–35 | 122 | 16.69 | 61 | 16.99 | 61 | 16.99 |
| 36–50 | 234 | 32.01 | 107 | 29.81 | 123 | 34.26 |
| >50 | 251 | 34.34 | 131 | 36.49 | 117 | 35.59 |
| Declined to answer | 52 | 7.11 | 20 | 5.57 | 27 | 7.52 |
| Professional discipline | ||||||
| Physicians | ||||||
| Primary care | 267 | 36.53 | 134 | 37.33 | 130 | 36.21 |
| Specialist* | 18 | 2.46 | 9 | 2.51 | 7 | 1.95 |
| Nurses | ||||||
| Registered | 103 | 14.09 | 48 | 13.37 | 54 | 15.04 |
| Nurse†/Medical Assistant | 102 | 13.95 | 47 | 13.09 | 51 | 14.21 |
| Allied health | 66 | 9.03 | 33 | 9.19 | 31 | 8.64 |
| Administrative‡ | 175 | 23.94 | 88 | 24.51 | 86 | 23.96 |
| Declined to answer | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 |
| Race | ||||||
| White | 414 | 56.63 | 204 | 56.82 | 207 | 57.66 |
| Hispanic | 153 | 20.93 | 74 | 20.61 | 79 | 22.01 |
| Black | 65 | 8.89 | 34 | 9.47 | 28 | 7.80 |
| Asian/Pacific Islander | 42 | 5.75 | 22 | 6.13 | 19 | 5.29 |
| American Indian/Alaska Native | 3 | 0.41 | 1 | 0.28 | 2 | 0.56 |
| Other | 30 | 4.10 | 15 | 4.18 | 14 | 3.90 |
| Declined to answer | 24 | 3.28 | 9 | 2.51 | 10 | 2.79 |
Includes adolescent medicine physicians, behavioral medicine physicians, cardiologists, child and adolescent psychologists, child psychiatrists, obstetrician/gynecologists, psychiatrists, renal specialists, and urgent care physicians.
Includes licensed practical nurses (LPNs), nursing assistants, and nurse practitioners.
Includes Academic Innovations Collaborative practice project managers, administrative assistants, administrative coordinators, administrative directors, ambulatory billing coordinators, clinical research associates, community resource specialists, financial counselors, managed care coordinators, medical records staff, office managers, operations directors, practice managers, and receptionists.
Survey Properties
Most survey responses were nonnegative, suggesting that on average respondents perceived a neutral to positive level of team dynamics in primary care in the first year of the learning collaborative (Table2). Mean scores for individual items ranged from 2.97 to 4.04 on a five-point scale, indicating opportunity for improvement in team dynamics measured by the survey. The item with the most positive response was “I regularly communicate with other members of my team.” The item with the least positive response was “My team has an effective process for conflict management.” Responses were also variable, with standard deviations for individual items of at least 0.73. The differences in average item score within participating practices also varied, by at least 0.4 SD and up to 1.4 SD.
Table 2.
Primary Care Team Dynamics Survey
| Factor Name | Item Number and Text | Mean | SD | Min.‡ | Max.‡ |
|---|---|---|---|---|---|
| Conditions for team effectiveness | 1. Membership on my team changes so frequently that we don't really have a team* | 3.58 | 1.07 | 2.76 | 4.28 |
| 2. My team has the right “mix” of members—a group of people who bring different clinical perspectives and experiences to the work | 3.66 | 0.96 | 3.29 | 4.08 | |
| 3. It is clear what is—and what is not—acceptable behavior on my team | 3.52 | 1.06 | 3.07 | 4.12 | |
| 4. Our practice recognizes and reinforces teams that perform well | 3.05 | 1.09 | 2.18 | 3.53 | |
| Shared understanding | 5. My team has goals that are clear, useful, and appropriate to my practice | 3.30 | 1.05 | 2.59 | 3.85 |
| 6. There is a real desire among team members to work collaboratively | 3.66 | 1.00 | 3.06 | 4.15 | |
| 7. If asked, I could explain some of the roles in the team and how they overlap† | 3.93 | 0.77 | 3.53 | 4.18 | |
| 8. If asked, I could explain every team member's role and how they overlap | 3.35 | 1.05 | 2.89 | 3.92 | |
| 9. My team encourages patients to be active participants in decisions about their care | 3.67 | 0.88 | 3.35 | 4.18 | |
| 10. My team does a good job of helping patients understand their care plan | 3.72 | 0.87 | 3.40 | 4.08 | |
| 11. The patient's needs and preferences are treated as an essential part of my team's decisions | 3.85 | 0.83 | 3.60 | 4.23 | |
| Processes for accountability | 12. Each team member shares accountability for team decisions and outcomes | 3.13 | 1.07 | 2.35 | 3.73 |
| Processes for communication and information exchange | 13. My team has developed effective strategies for sharing patient treatment goals among team members | 3.08 | 1.08 | 2.49 | 3.85 |
| 14. Relevant information about changes in patient status or care plan is reported to the appropriate team member in a timely manner | 3.34 | 1.02 | 2.93 | 3.81 | |
| 15. All team members effectively use the patient health record as a communication tool | 3.54 | 1.00 | 3.05 | 4.00 | |
| 16. My team addresses patients’ concerns effectively through team meetings and discussions | 3.20 | 1.17 | 2.60 | 4.04 | |
| 17. Team meetings provide an open, comfortable, safe place to discuss concerns | 3.55 | 1.06 | 2.80 | 4.13 | |
| Processes for conflict resolution | 18. When team members disagree, all points of view are considered before deciding on a solution | 3.32 | 1.04 | 2.43 | 3.92 |
| 19. My team has an effective process for conflict management | 2.97 | 1.03 | 2.27 | 3.43 | |
| Acting and feeling like a team | 20. Members of my team depend on each other for their special knowledge and expertise | 3.85 | 0.84 | 3.56 | 4.10 |
| 21. Overall, members of our team do a very good job of coordinating their different patient-related jobs and activities | 3.69 | 0.89 | 3.39 | 4.11 | |
| 22. I regularly communicate with other members of my team | 4.04 | 0.82 | 3.62 | 4.24 | |
| 23. Members of my team act upon the information I communicate to them | 3.95 | 0.73 | 3.68 | 4.20 | |
| 24. Members of my team show respect for each other's roles and expertise | 3.89 | 0.90 | 3.47 | 4.32 | |
| 25. Members of my team really trust each other's work and contributions related to patient care | 3.79 | 0.86 | 3.29 | 4.16 | |
| 26. On my team, physicians usually ask nonphysician team members for opinions about relevant aspects of patient care† | 3.30 | 0.99 | 2.59 | 4.08 | |
| Perceived team effectiveness | 27. The way my team members interact makes the delivery of care highly efficient | 3.13 | 1.07 | 2.71 | 3.82 |
| 28. The way my team members interact is very good for the quality of patient care | 3.40 | 1.00 | 2.94 | 4.12 | |
| 29. Working on a team like mine keeps members of my team enthusiastic and interested in their jobs | 3.21 | 1.04 | 2.41 | 4.04 | |
| 30. I feel integral to my team | 3.68 | 1.00 | 3.24 | 4.12 | |
| 31. I experience excellent teamwork with the members of my team | 3.42 | 1.00 | 2.94 | 4.04 |
Reverse-coded.
Excluded from final model.
Minima and maxima represent the range in average item score across participating primary care practices.
Psychometric Analysis
Using the first half-sample, SEM suggested excluding four of 31 items in three factors due to factor loadings less than 0.40 and the inclusion of a multitude of covariances between items within factors to improve model fit. This initial five-factor model demonstrated adequate fit on standard indices: goodness-of-fit index (GFI) of 0.91, adjusted GFI of 0.88, comparative fit index (CFI) of 0.96, root mean square residual (RMR) of 0.04, and root mean square error of approximation (RMSEA) of 0.05. Model fit is considered adequate when GFI>0.90, adjusted GFI>0.80, CFI>0.90, RMR<0.10, and RMSEA<0.08.
The pattern of factor loadings also suggested that a seven-factor model might better represent the underlying structure of our data than the five-factor model initially proposed. Such a modified model would differ from the original by dividing Supportive Processes into three distinct factors: (1) processes for accountability—one item; (2) processes for communication and information exchange—five items; and (3) processes for conflict resolution—two items. Conceptual distinctions among these three processes supported modifying the model in this way. Thus, we repeated the analyses above using the first half-sample and reverting to the original set of 31 survey items to explore the fit of a seven-factor model.1 Analysis with this adjusted model suggested the exclusion of two items (one from the shared understanding factor and the other from acting and feeling like a team) and a more limited number of item covariances (Figure2). This seven-factor model also had adequate fit on standard indices: GFI of 0.91, adjusted GFI of 0.87, CFI of 0.96, RMR of 0.04, and RMSEA of 0.04.
Figure 2.
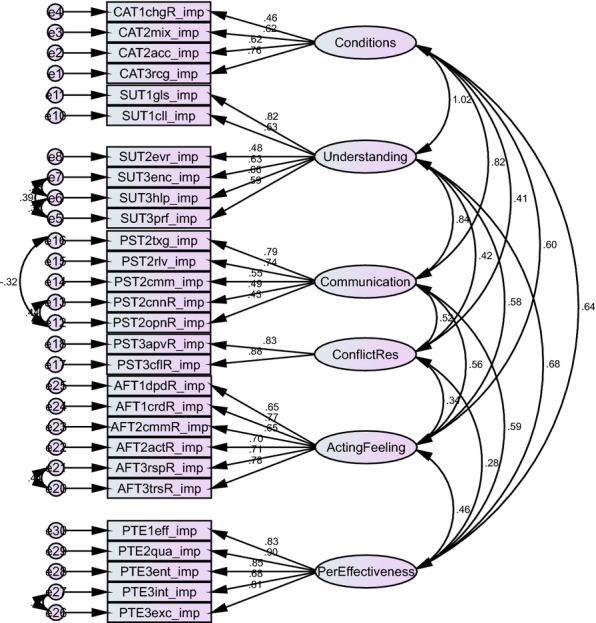
Diagram of Structural Equation Model with Standardized Factor Loadings
Note. Analysis conducted using the first split-half sample from the imputed dataset. Model excludes the single item measuring accountability.
In the second half-sample, we examined this seven-factor model, including the 29 remaining items, interfactor item covariances, and accounting for common method bias. We again obtained adequate fit on standard indices: GFI of 0.88, adjusted GFI of 0.83, CFI of 0.94, RMR of 0.05, and RMSEA of 0.06.
We further assessed the robustness of our empirically derived, seven-factor model by comparing results based on the imputed data to those derived from the same analysis using data with no imputed values. In this instance, observations missing any data were list-wise deleted (n = 94). All indices were robust to this analysis; this modified model achieved similar fit: GFI of 0.91, adjusted GFI of 0.88, CFI of 0.95, RMR of 0.04, and RMSEA of 0.05.
Scale means, standard deviations, correlation among scales, and Cronbach's alpha coefficients (estimating scale internal consistency at the individual level of analysis) are included in Table3. Mean scores for the seven factors (including the single-item independent measure of accountability) ranged from 3.09 for processes for accountability to 3.83 for acting and feeling like a team (based on the first half-sample). All six multi-item factors demonstrated adequate reliability using standard criteria, ranging from 0.71 to 0.91. Correlations among factors were relatively high, averaging 0.49. This was particularly true for the relationship between shared understanding and conditions for team effectiveness (r = 0.73). However, all correlations among factors were lower than the corresponding alpha coefficients, suggesting the factors measured related, yet distinct team dynamics.
Table 3.
Survey Properties
| First Half-Sample | Second Half-Sample | Factor Correlations, Total Sample | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | α | Mean | SD | α | 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
| 1. Conditions for team effectiveness | 3.42 | 0.77 | 0.71 | 3.49 | 0.78 | 0.75 | 1 | ||||||
| 2. Shared understanding | 3.59 | 0.67 | 0.83 | 3.58 | 0.70 | 0.83 | 0.73 | 1 | |||||
| 3. Processes for accountability | 3.09 | 1.10 | —* | 3.16 | 1.04 | —* | 0.59 | 0.64 | 1 | ||||
| 4. Processes for communication and information exchange | 3.33 | 0.81 | 0.81 | 3.34 | 0.74 | 0.78 | 0.60 | 0.66 | 0.64 | 1 | |||
| 5. Processes for conflict resolution | 3.12 | 0.93 | 0.80 | 3.16 | 0.92 | 0.82 | 0.37 | 0.39 | 0.37 | 0.57 | 1 | ||
| 6. Acting and feeling like a team | 3.83 | 0.65 | 0.87 | 3.90 | 0.66 | 0.88 | 0.47 | 0.49 | 0.37 | 0.45 | 0.43 | 1 | |
| 7. Perceived team effectiveness | 3.31 | 0.89 | 0.90 | 3.41 | 0.86 | 0.91 | 0.54 | 0.56 | 0.44 | 0.47 | 0.28 | 0.38 | 1 |
Note Analysis conducted using imputed dataset.
Cronbach's alpha is not reported because scale is based on a single item.
To assess the extent to which our measures could inform practice-level comparisons, we calculated four complementary measures of within-group agreement for each of the seven factors in our final model: the median rwg (the degree to which individual responses within a practice are interchangeable), the F-statistic from a one-way ANOVA (the extent to which responses differ between individuals at different practices), and two forms of intraclass correlation: ICC(1) (an estimate of the reliability of one individual's assessment of the practice mean) and ICC(2) (an overall estimate of the reliability of practice means). Assessed with an average sample size of 40 respondents per practice, the median rwg ranged from 0.23 to 0.75, with two of the seven factors having a median rwg greater than the suggested threshold of 0.70 (James, Demaree, and Wolf 1984). Each F-statistic was highly significant (p < .01), all values of ICC(1) were positive, and values of ICC(2) ranged from 0.58 to 0.81, with all above the suggested threshold of 0.50 (Klein and Kozlowski 2000). Collectively, these results suggest that survey domains may be aggregated to assess team dynamics at the practice level, with the caveat that individual responses within a practice may not be highly interchangeable. We used the Spearman–Brown prophecy formula to solve for the number of respondents needed to obtain practice-level reliability of 0.70 (Hays et al. 1999). This yielded sample size requirements for each of the seven factors ranging from 26 to 62.
Discussion
In recent years, team dynamics have become increasingly important in ambulatory settings to manage and coordinate care for patients with multiple comorbidities and to curb costs. Health care providers—even those working within the same practice—need to exchange critical information and coordinate efforts with one another. Thus, being able to measure and improve team dynamics in ambulatory settings will be integral to the development and promotion of PCMHs and Accountable Care Organizations. Notably, the National Committee for Quality Assurance (NCQA) recently designated team-based care as a “must-pass” criterion for PCMH recognition (NCQA 2014).
We developed an evidence-based conceptual model of primary care team dynamics and validated a survey instrument designed to measure team dynamics in ambulatory settings. Our findings suggest it is possible to reliably measure primary care team dynamics using a 29-item survey. Survey items represent a model that includes seven dynamically interacting factors (Figure1b). Certain conditions increase shared understanding and specific processes that support teamwork. These promote acting and feeling like a team, which is related to team member perceptions of team effectiveness.
The first factor, conditions for team effectiveness, includes four items that assess whether the team has stable membership, an enabling structure, and a supportive organizational context. Shared understanding, our second factor, includes seven survey items that assess the extent to which the team has collective goals, a clear delineation of member roles and responsibilities, and patient involvement. Our psychometric analysis suggested three separate processes support teamwork in primary care: processes for accountability measured with a single item; processes for communication and information exchange represented by five items probing communication that regularly occurs in primary care; and processes for conflict resolution, consisting of two items. Acting and feeling like a team, the sixth factor, includes seven items measuring the extent to which team members have learned to use team skills and knowledge effectively; share and use information from others; and value, trust, and respect other members of the team. The last factor uses five items to assess perceived team effectiveness, the extent to which members view the team as effective in delivering effective, efficient care, and in enhancing enthusiasm and interest among team members.
Empirical support for the survey instrument is strong. With only minor modifications to our original conceptual framework, goodness-of-fit measures supported the hypothesized model. Evidence for scale reliability is also excellent, with all scales demonstrating Cronbach's alpha coefficients exceeding conventional thresholds (Nunnally and Bernstein 1994). In addition, correlation patterns provide validation of satisfactory discrimination among factors, although not unexpectedly this analysis also reveals strong relationships among factors.
This survey instrument is the first, to our knowledge, that comprehensively assesses team dynamics in ambulatory settings. Unlike most other survey instruments designed for use in health care settings, it is also designed to be administered to a wide range of health care professionals, including nonphysician health care professionals such as medical assistants, nursing assistants, and receptionists.
Nevertheless, our testing of the Primary Care Team Dynamics survey has limitations. First, our final sample of 731 individuals was adequate, but not large relative to the number of dimensions in our conceptual model (Brown 2006; Hair et al. 1998), and the overall response rate of 68 percent was high (Jepson et al. 2005), but still leaves room for selection bias. Survey respondents and nonrespondents may have differed systematically in ways that impacted their team dynamics. However, analyses comparing the responses of early and late responders do not reveal significant differences, suggesting that nonresponse bias may not significantly affect interpretation of results. Second, our conceptual model may be incomplete. For the sake of parsimony, we excluded intervening processes (e.g., processes for learning within teams). Researchers may consider further developing the survey instrument by complementing it with scales that capture such processes. Third, like many surveys, responses may be subject to social desirability bias. We modified survey items to minimize this potential, but cannot rule out the possibility of an effect. Fourth, although our conceptual model asserts directionality, we are unable to ascertain the directionality of related constructs because our data come from a cross-sectional survey administration. Future research should seek to determine empirically the directionality of constructs. Finally, in this paper, we did not examine the relationship of survey measures to objective measures of team effectiveness, such as career satisfaction, care quality, and clinical outcomes. Future research should seek to validate the Primary Care Team Dynamics survey in this way.
Because of the critical role that team-based care plays in recent U.S. efforts to transform primary care practices to become PCMHs, more specific primary care-focused tools that evaluate team dynamics are needed to enable organizations to understand where they are succeeding and where they need more work (Margolius 2013). The Primary Care Team Dynamics survey is currently ready for use in a research or exploratory context. Additional research should generate information about the reliability of the survey in other contexts, its responsiveness to interventions to improve team performance, and the relationship between survey constructs and team outcomes. In future studies, the Primary Care Team Dynamics survey may be useful in understanding the level of team dynamics in primary care practices, evaluating differences in perceptions among team members in different roles, and measuring the impact of interventions that seek to establish care teams and improve team dynamics in primary care practices.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This research was supported by a grant from the Harvard Medical School Center for Primary Care. The authors acknowledge the Center for Primary Care and all members of the primary care practices participating in the Academic Innovations Collaborative (AIC) for their support of the survey. The funding source played no role in the analysis, interpretation, writing of the manuscript, or the decision to submit it for publication.
Disclosures: None.
Disclaimers: None.
Footnotes
Because one of the factors was measured by a single item, and the structural equation modeling approach does not allow for single-item factors in the analysis, we treated the “processes for accountability” factor as an independent measure of accountability. Thus, the diagram of the structural equation model in Figure2 includes only six factors.
Supporting Information
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Appendix SA2: Contents and Origin of Survey Domains.
References
- Alexander JA, Lichtenstein R, Jinnett K, Wells R, Zazzali J. Liu D. Cross-Functional Team Processes and Patient Functional Improvement. Health Services Research. 2005;40(5):1335–55. doi: 10.1111/j.1475-6773.2005.00418.x. doi: 10.1111/j.1475-6773.2005.00418.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Medical Association. Principles of Medical Ethics. 2001. . “ ” [accessed on September 22, 2013]. Available at http://www.ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics/principles-medical-ethics.page. [Google Scholar]
- Argyris C. Schön DA. Organizational Learning: A Theory of Action Perspective. Addison-Wesley Series on Organization Development. Reading, MA: Addison-Wesley Pub. Co; 1978. [Google Scholar]
- Baggs JG. Development of an Instrument to Measure Collaboration and Satisfaction about Care Decisions. Journal of Advanced Nursing. 1994;20(1):176–82. doi: 10.1046/j.1365-2648.1994.20010176.x. doi: 10.1046/j.1365-2648.1994.20010176.x. [DOI] [PubMed] [Google Scholar]
- Barry MJ. Edgman-Levitan S. Shared Decision Making-Pinnacle of Patient-Centered Care. New England Journal of Medicine. 2012;366(9):780–1. doi: 10.1056/NEJMp1109283. doi: 10.1056/NEJMp1109283. [DOI] [PubMed] [Google Scholar]
- Bitton A, Ellner A, Pabo E, Stout S, Sugarman J, Sevin C, Goodell K, Bassett JS. Phillips RS. Launching the Harvard Medical School Academic Innovations Collaborative: Transforming Primary Care Practice and Education. Academic Medicine. 2014;89(9):1239–44. doi: 10.1097/ACM.0000000000000410. [DOI] [PubMed] [Google Scholar]
- Blumenthal DM, Song Z, Jena AB. Ferris TG. Guidance for Structuring Team-Based Incentives in Healthcare. American Journal of Managed Care. 2013;19(2):e64–70. [PMC free article] [PubMed] [Google Scholar]
- Bradford DL. Cohen AR. Power up: Transforming Organizations through Shared Leadership. New York: John Wiley & Sons; 1998. [Google Scholar]
- Brennan SE, Bosch M, Buchan H. Green SE. Measuring Team Factors Thought to Influence the Success of Quality Improvement in Primary Care: A Systematic Review of Instruments. Implementation Science. 2013;8(1):20. doi: 10.1186/1748-5908-8-20. doi: 10.1186/1748-5908-8-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA. Confirmatory Factor Analysis for Applied Research. Methodology in the Social Sciences. New York: Guilford; 2006. [Google Scholar]
- Byrne BM. Structural Equation Modeling with AMOS: Basic Concepts, Applications, and Programming. Multivariate Applications Series. Mahwah, NJ: Lawrence Erlbaum Associates; 2001. [Google Scholar]
- Cannon-Bowers JA, Tannenbaum SI, Salas E. Volpe CE. Defining Team Competencies and Establishing Team Training Requirements. In: Guzzo R, Salas E, editors; Team Effectiveness and Decision Making in Organizations. San Francisco, CA: Jossey-Bass; 1995. pp. 333–80. , edited by , and . “ .”. [Google Scholar]
- Edmondson AC, Bohmer RM. Pisano GP. Speeding Up Team Learning. Harvard Business Review. 2001;79(9):125–32. [Google Scholar]
- Eisenhardt KM, Kahwajy JL. Bourgeois LJ. Conflict and Strategic Choice: How Top Management Teams Disagree. California Management Review. 1997;39(2):42–62. [Google Scholar]
- Gandhi TK, Graydon-Baker E, Barnes JN, Neppl C, Stapinski C, Silverman J, Churchill W, Johnson P. Gustafson M. Creating an Integrated Patient Safety Team. Joint Commission Journal on Quality and Safety. 2003;29(8):383–90. doi: 10.1016/s1549-3741(03)29046-8. [DOI] [PubMed] [Google Scholar]
- Gandhi TK, Graydon-Baker E, Huber CN, Whittemore AD. Gustafson M. Closing the Loop: Follow-Up and Feedback in a Patient Safety Program. Joint Commission Journal on Quality and Safety. 2005;31(11):614–21. doi: 10.1016/s1553-7250(05)31079-8. [DOI] [PubMed] [Google Scholar]
- Gardner HK, Gino F. Staats BR. Dynamically Integrating Knowledge in Teams: Transforming Resources into Performance. Academy of Management Journal. 2012;55(4):998–1022. doi: 10.5465/amj.2010.0604. [Google Scholar]
- Garvin DA. Roberto MA. What You Don't Know about Making Decisions. Harvard Business Review. 2001;79(8):108–19. [PubMed] [Google Scholar]
- Gittell JH. Organizing Work to Support Relational Coordination. International Journal of Human Resource Management. 2000;11(3):517–39. doi: 10.1080/095851900339747. [Google Scholar]
- Gittell JH. Coordinating Mechanisms in Care Provider Groups: Relational Coordination as a Mediator and Input Uncertainty as a Moderator of Performance Effects. Management Science. 2002;48(11):1408–26. [Google Scholar]
- Hackman JR. The Design of Work Teams. In: Lorsch JW, editor. Handbook of Organizational Behavior. Englewood Cliffs, NJ: Prentice-Hall; 1987. pp. 315–42. [Google Scholar]
- Hackman JR. Groups That Work (and Those That Don't): Creating Conditions for Effective Teamwork. Jossey-Bass Management Series. San Francisco, CA: Jossey-Bass; 1990. [Google Scholar]
- Hackman JR. Leading Teams: Setting the Stage for Great Performances. Boston: Harvard Business Press; 2002. [Google Scholar]
- Hair JF, Anderson RE, Tatham RL. Black WC. Multivariate Data Analysis. 5th Edition. Upper Saddle River, NJ: Prentice Hall; 1998. [Google Scholar]
- Harvey L, Fowles JB, Xi M. Terry P. When Activation Changes, What Else Changes? The Relationship between Change in Patient Activation Measure (PAM) and Employees’ Health Status and Health Behaviors. Patient Education and Counseling. 2012;88(2):338–43. doi: 10.1016/j.pec.2012.02.005. doi: 10.1016/j.pec.2012.02.005. [DOI] [PubMed] [Google Scholar]
- Hays RD. Hayashi T. Beyond Internal Consistency Reliability: Rationale and User's Guide for Multitrait Analysis Program on the Microcomputer. Behavior Research Methods, Instruments, and Computers. 1990;22(2):167–75. doi: 10.3758/BF03203140. [Google Scholar]
- Hays RD, Shaul JA, Williams VS, Lubalin JS, Harris-Kojetin LD, Sweeny SF. Cleary PD. Psychometric Properties of the CAHPS 1.0 Survey Measures. Consumer Assessment of Health Plans Study. Medical Care. 1999;37(3 Suppl):MS22–31. doi: 10.1097/00005650-199903001-00003. [DOI] [PubMed] [Google Scholar]
- Heinemann GD, Schmitt MH, Farrell MP. Brallier SA. Development of an Attitudes toward Health Care Teams Scale. Evaluation and the Health Professions. 1999;22(1):123–42. doi: 10.1177/01632789922034202. doi: 10.1177/01632789922034202. [DOI] [PubMed] [Google Scholar]
- Herzberg F. One More Time: How Do You Motivate Employees? Harvard Business Review. 1968;46(1):53–62. [PubMed] [Google Scholar]
- Hibbard JH. Greene J. What the Evidence Shows about Patient Activation: Better Health Outcomes and Care Experiences; Fewer Data on Costs. Health Affairs. 2013;32(2):207–14. doi: 10.1377/hlthaff.2012.1061. doi: 10.1377/hlthaff.2012.1061. [DOI] [PubMed] [Google Scholar]
- Hibbard JH, Greene J. Overton V. Patients with Lower Activation Associated with Higher Costs; Delivery Systems Should Know Their Patients’ ‘Scores’. Health Affairs. 2013;32(2):216–22. doi: 10.1377/hlthaff.2012.1064. doi: 10.1377/hlthaff.2012.1064. [DOI] [PubMed] [Google Scholar]
- Hill LA. Managing Your Team. Harvard Business School Background Note; 1995. pp. 494–081. [Google Scholar]
- Hill LA. M Farkas. A Note on Team Process. Harvard Business School Background Note: 2001. pp. 402–032. [Google Scholar]
- Hyer K, Fairchild S, Abraham I, Mezey M. Fulmer T. Measuring Attitudes Related to Interdisciplinary Training: Revisiting the Heinemann, Schmitt and Farrell ‘Attitudes toward Health Care Teams’ Scale. Journal of Interprofessional Care. 2000;14(3):249–58. doi: 10.1080/jic.14.3.249.258. [Google Scholar]
- James LR, Demaree RG. Wolf G. Estimating within-Group Interrater Reliability with and without Response Bias. Journal of Applied Psychology. 1984;69(1):85–98. doi: 10.1037/0021-9010.69.1.85. [Google Scholar]
- Jepson C, Asch DA, Hershey JC. Ubel PA. In a Mailed Physician Survey, Questionnaire Length Had a Threshold Effect on Response Rate. Journal of Clinical Epidemiology. 2005;58(1):103–5. doi: 10.1016/j.jclinepi.2004.06.004. doi: 10.1016/j.jclinepi.2004.06.004. [DOI] [PubMed] [Google Scholar]
- Jesmin S, Thind A. Sarma S. Does Team-Based Primary Health Care Improve Patients’ Perception of Outcomes? Evidence from the 2007-08 Canadian Survey of Experiences with Primary Health. Health Policy. 2012;105(1):71–83. doi: 10.1016/j.healthpol.2012.01.008. doi: 10.1016/j.healthpol.2012.01.008. [DOI] [PubMed] [Google Scholar]
- The Joint Commission. Improving Transitions of Care: Hand-off Communications. 2013. . “ .” [accessed on September 5, 2013]. Available at http://www.centerfortransforminghealthcare.org/assets/4/6/CTH_Hand-off_commun_set_final_2010.pdf. [Google Scholar]
- Katzenbach JR. Smith DK. The Discipline of Teams. Harvard Business Review. 1993;71(2):111–20. [PubMed] [Google Scholar]
- King J. Moulton B. Group Health's Participation in a Shared Decision-Making Demonstration Yielded Lessons, Such as Role of Culture Change. Health Affairs. 2013;32(2):294–302. doi: 10.1377/hlthaff.2012.1067. doi: 10.1377/hlthaff.2012.1067. [DOI] [PubMed] [Google Scholar]
- Klein KJ. Kozlowski SWJ. Multilevel Theory, Research, and Methods in Organizations. San Francisco, CA: Jossey-Bass; 2000. [Google Scholar]
- Klein C, DiazGranados D, Salas E, Le H, Burke CS, Lyons R. Goodwin GF. Does Team Building Work? Small Group Research. 2009;40(2):181–222. doi: 10.1177/1046496408328821. [Google Scholar]
- Kozlowski SWJ. Ilgen DR. Enhancing the Effectiveness of Work Groups and Teams. Psychological Science in the Public Interest. 2006;7(3):77–124. doi: 10.1111/j.1529-1006.2006.00030.x. doi: 10.1111/j.1529-1006.2006.00030.x. [DOI] [PubMed] [Google Scholar]
- Latané B, Williams K. Harkins S. Many Hands Make Light the Work: The Causes and Consequences of Social Loafing. Journal of Personality and Social Psychology. 1979;37(6):822–32. doi: 10.1037/0022-3514.37.6.822. [Google Scholar]
- Leipzig RM, Hyer K, Ek K, Wallenstein S, Vezina ML, Fairchild S, Cassel CK. Howe JL. Attitudes toward Working on Interdisciplinary Healthcare Teams: A Comparison by Discipline. Journal of the American Geriatrics Society. 2002;50(6):1141–8. doi: 10.1046/j.1532-5415.2002.50274.x. [DOI] [PubMed] [Google Scholar]
- Lemieux-Charles L. McGuire WL. What Do We Know about Health Care Team Effectiveness? A Review of the Literature. Medical Care Research and Review. 2006;63(3):263–300. doi: 10.1177/1077558706287003. doi: 10.1177/1077558706287003. [DOI] [PubMed] [Google Scholar]
- Leonard-Barton DA. Swap WC. When Sparks Fly: Igniting Creativity in Groups. Boston: Harvard Business School Press; 1999. [Google Scholar]
- Mahoney B. Turkovich C. The Team Development Measure. [accessed on October 16, 2013]. Available at: 2010. http://www.peacehealth.org/about-peacehealth/medical-professionals/eugene-springfield-cottage-grove/team-measure/Pages/measure.aspx. [Google Scholar]
- Margolius D. Less Tinkering, More Transforming: How to Build Successful Patient-Centered Medical Homes. Journal of the American Medical Association Internal Medicine. 2013;173(18):1702–3. doi: 10.1001/jamainternmed.2013.8964. doi: 10.1001/jamainternmed.2013.9241.5. [DOI] [PubMed] [Google Scholar]
- Millward LJ. Jeffries N. The Team Survey: A Tool for Health Care Team Development. Journal of Advanced Nursing. 2001;35(2):276–87. doi: 10.1046/j.1365-2648.2001.01844.x. [DOI] [PubMed] [Google Scholar]
- Nadler D, Hackman JR. Lawler EE. Managing Organizational Behavior. Boston: Little, Brown and Company; 1979. [Google Scholar]
- Nagpal K, Vats A, Lamb B, Ashrafian H, Sevdalis N, Vincent C. Moorthy K. Information Transfer and Communication in Surgery: A Systematic Review. Annals of Surgery. 2010;252(2):225–39. doi: 10.1097/SLA.0b013e3181e495c2. doi: 10.1097/SLA.0b013e3181e495c2. [DOI] [PubMed] [Google Scholar]
- National Committee for Quality Assurance. 2011 PCMH Standards and Guidelines. 2011. [Google Scholar]
- National Committee for Quality Assurance. 2014 PCMH Standards and Guidelines. 2014. [Google Scholar]
- Nunnally J. Bernstein I. Psychometric Theory. New York: McGraw-Hill; 1994. [Google Scholar]
- The Patient-Centered Primary Care Collaborative. 2007. “ Joint Principles of the Patient Centered Medical Home ” [accessed on September 3, 2013]. Available at http://www.aafp.org/dam/AAFP/documents/practice_management/pcmh/initiatives/PCMHJoint.pdf.
- Podsakoff PM, MacKenzie SB, Lee J-Y. Podsakoff NP. Common Method Biases in Behavioral Research: A Critical Review of the Literature and Recommended Remedies. Journal of Applied Psychology. 2003;88(5):879–903. doi: 10.1037/0021-9010.88.5.879. doi: 10.1037/0021-9010.88.5.879. [DOI] [PubMed] [Google Scholar]
- Remmers C, Hibbard J, Mosen DM, Wagenfield M, Hoye RE. Jones C. Is Patient Activation Associated with Future Health Outcomes and Healthcare Utilization among Patients with Diabetes? Journal of Ambulatory Care Management. 2009;32(4):320–7. doi: 10.1097/JAC.0b013e3181ba6e77. doi: 10.1097/JAC.0b013e3181ba6e77. [DOI] [PubMed] [Google Scholar]
- Saavedra R, Earley PC. Van Dyne L. Complex Interdependence in Task-Performing Groups. Journal of Applied Psychology. 1993;78(1):61–72. doi: 10.1037/0021-9010.78.1.61. [Google Scholar]
- Schroder C, Medves J, Paterson M, Byrnes V, Chapman C, O'Riordan A, Pichora D. Kelly C. Development and Pilot Testing of the Collaborative Practice Assessment Tool. Journal of Interprofessional Care. 2011;25(3):189–95. doi: 10.3109/13561820.2010.532620. doi: 10.3109/13561820.2010.532620. [DOI] [PubMed] [Google Scholar]
- Senior B. Swailes S. Inside Management Teams: Developing a Teamwork Survey Instrument. British Journal of Management. 2007;18:138–53. doi: 10.1111/j.1467-8551.2006.00507x. [Google Scholar]
- Shuffler ML, DiazGranados D. Salas E. There's a Science for That: Team Development Interventions in Organizations. Current Directions in Psychological Science. 2011;20(6):365–72. doi: 10.1177/0963721411422054. [Google Scholar]
- Snyder L. American College of Physicians Ethics Manual: Sixth Edition. Annals of Internal Medicine. 2012;156(1 Pt 2):73–104. doi: 10.7326/0003-4819-156-1-201201031-00001. doi: 10.7326/0003-4819-156-1-201201031-00001. [DOI] [PubMed] [Google Scholar]
- Stacey D, Bennett CL, Barry MJ, Col NF, Eden KB, Holmes-Rovner M, Llewellyn-Thomas H, Lyddiatt A, Légaré F. Thomson R. Decision Aids for People Facing Health Treatment or Screening Decisions. Cochrane Database of Systematic Reviews. 2011;10:CD001431. doi: 10.1002/14651858.CD001431.pub3. doi: 10.1002/14651858.CD001431.pub3. [DOI] [PubMed] [Google Scholar]
- Stasser G, Stewart DD. Wittenbaum GM. Expert Roles and Information Exchange during Discussion: The Importance of Knowing Who Knows What. Journal of Experimental Social Psychology. 1995;31(3):244–65. doi: 10.1006/jesp.1995.1012. [Google Scholar]
- Suter E, Arndt J, Arthur N, Parboosingh J, Taylor E. Deutschlander S. Role Understanding and Effective Communication as Core Competencies for Collaborative Practice. Journal of Interprofessional Care. 2009;23(1):41–51. doi: 10.1080/13561820802338579. doi: 10.1080/13561820802338579. [DOI] [PubMed] [Google Scholar]
- Thompson JD. Organizations in Action: Social Science Bases of Administrative Theory. New York: McGraw-Hill; 1967. [Google Scholar]
- Toseland RW, Palmer-Ganeles J. Chapman D. Teamwork in Psychiatric Settings. Social Work. 1986;31(1):46–52. doi: 10.1093/sw/31.1.46. [DOI] [PubMed] [Google Scholar]
- Valentine MA, Nembhard IM. Edmondson AC. Measuring Teamwork in Health Care Settings: A Review of Survey Instruments. Medical Care. doi: 10.1097/MLR.0b013e31827feef6. In press. “ .” . doi: 10.1097/MLR.0b013e31827feef6. [DOI] [PubMed] [Google Scholar]
- Wageman R. How Leaders Foster Self-Managing Team Effectiveness: Design Choices versus Hands-On Coaching. Organization Science. 2001;12(5):559–77. doi: 10.1287/orsc.12.5.559.10094. [Google Scholar]
- Wageman R, Hackman JR. Lehman E. Team Diagnostic Survey: Development of an Instrument. Journal of Applied Behavioral Science. 2005;41(4):373–98. doi: 10.1177/0021886305281984. [Google Scholar]
- Weiss SJ. Davis HP. Validity and Reliability of the Collaborative Practice Scales. Nursing Research. 1985;34(5):299–305. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Appendix SA2: Contents and Origin of Survey Domains.


