Abstract
Background
The proportion of elderly patients beginning to undergo dialysis is increasing globally. Whether early referral (ER) of elderly patients is associated with favorable outcomes remains under debate. We investigated the influence of referral timing on the mortality of elderly patients.
Methods
We retrospectively assessed mortality in 820 patients aged ≥70 years with end-stage renal disease (ESRD) who initiated hemodialysis at a tertiary university hospital between 2000 and 2010. Mortality data was obtained from the time of dialysis initiation until December 2010. We assigned patients to one of two groups according to the time of their first encounters with nephrologists: ER (≥ 3 months) and late referral (LR; < 3 months).
Results
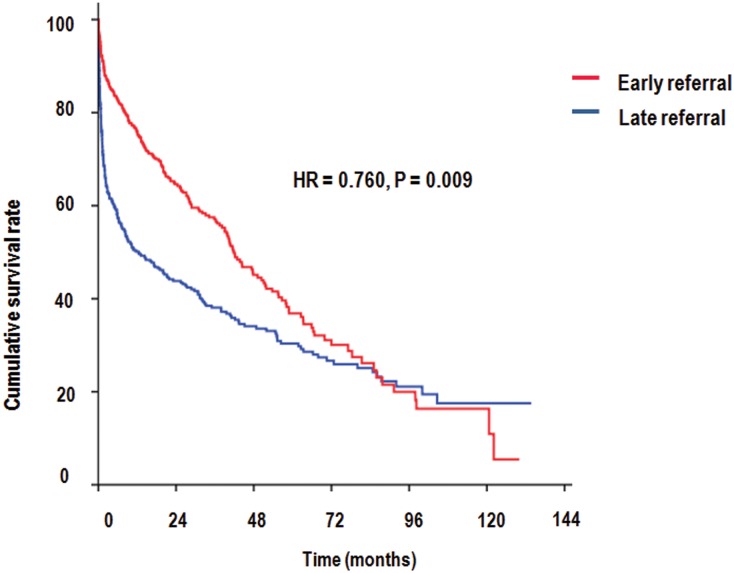
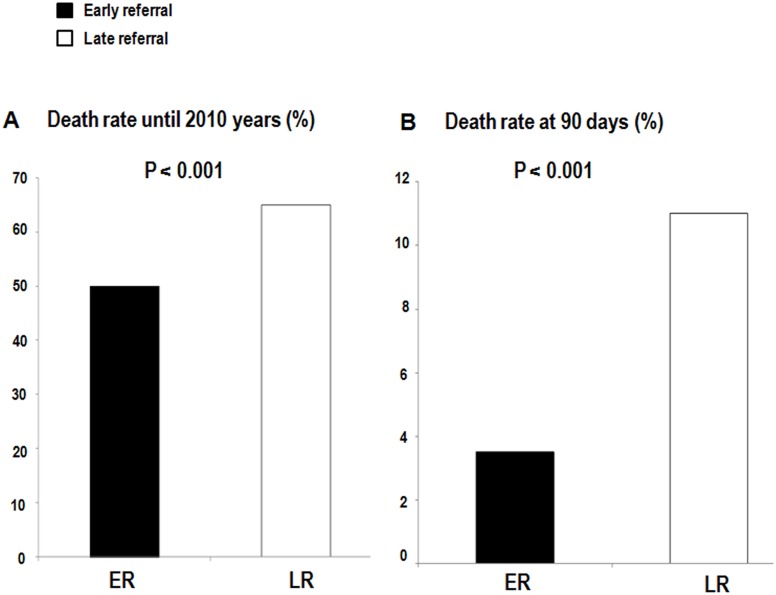
During a mean follow-up period of 25.1 months, the ER group showed a 24% reduced risk of long-term mortality relative to the LR group (HR = 0.760, P = 0.009). Rate of reduction in 90-day mortality for ER patients was 58% (HR = 0.422, P=0.012). However, the statistical significance of the difference in mortality rates between ER and LR group was not observed across age groups after 90 days. Old age, LR, central venous catheter, high white blood cell count and corrected Ca level, and lower levels of albumin, creatinine, hemoglobin, and sodium were significantly associated with increased risk of mortality.
Conclusions
Timely referral was also associated with reduced mortality in elderly ESRD patients who initiated hemodialysis. In particular, the initial 90-day mortality reduction in ER patients contributed to mortality differences during the follow-up period.
Introduction
The incidence and prevalence of end-stage renal disease (ESRD) have increased worldwide [1,2]. The proportion of elderly patients commencing dialysis is increasing globally [3,4]; however, sizeable variations exist and range from 16% to 40% geographically [5].
Timely referral to a nephrologist has long been recommended in patients with chronic kidney disease (CKD), because late referral (LR) is associated with increased mortality and morbidity and greater healthcare burden [6–8]. Elderly patients with ongoing debate about initiation of dialysis are at risk for experiencing delayed nephrology care [9,10]. While a few studies have reported that LR in the elderly was associated with high mortality rates [11,12], a recent study reported no material improvement in survival rates despite significant trends toward early referral (ER) [13]. Whether ER in the elderly is associated with favorable outcomes remains under debate. Therefore, we investigated predictors of referral timing and the influence of referral timing on the mortality of elderly patients undergoing incident hemodialysis.
Materials and Methods
Study population
We included 820 patients aged ≥70 years with ESRD who were receiving incident hemodialysis and had a baseline value of creatinine (Cr) at Seoul National University Hospital in Korea between 2000 and 2010. We excluded patients who were transferred from other chronic dialysis programs, those who experienced acute kidney injury, those for whom the timing of referral was unavailable, or those who underwent peritoneal dialysis as the treatment modality at any given time. This study was approved by the institutional review board of the Seoul National University Hospital (IRB number: H1107-092-370) with no written consent because patients records/information was anonymized and de-identified prior to analysis. All clinical investigations were conducted according to the 2008 Declaration of Helsinki and good clinical practice guidelines.
Measurements and definitions
Patients’ data were collected retrospectively via review of their electronic medical records. Dates of dialysis initiation were determined using electronic resources at Seoul National University Hospital and the ESRD registry committee of the Korean Society of Nephrology. We adopted a date as that of dialysis initiation when it was registered on two systems, and we thoroughly reviewed medical records when dates differed between the systems. ER and LR were defined according whether the patient’s first encounter with a nephrologist was more than or less than 3 months prior to the first time they were diagnosed with ESRD. Serum Cr values were measured using the alkaline picrate Jaffe kinetic method with an automatic analyzer (Toshiba-200FR, Tokyo, Japan). The estimated glomerular filtration rate (eGFR) was calculated using the Modification of Diet in Renal Disease study equation [14]. Presence of hypertension (HTN) at baseline was confirmed with systolic blood pressure (SBP) of ≥ 140 mmHg or diastolic blood pressure (DBP) of ≥ 90 mmHg during physical examination, a self-reported history of disease, or use of antihypertensive medication. Diabetes mellitus (DM) was confirmed with a glycated hemoglobin level of ≥ 6.5, a self-reported history of disease, or use of antihyperglycemic agents. Cardiovascular disease including angina pectoris (I20), acute myocardial infarction (I21), subsequent myocardial infarction (I22), certain current complications following acute myocardial infarction (I23), other acute ischemic heart disease (I24), chronic ischemic heart disease (I25), heart failure (I50), and cancer (C) at dialysis initiation were specified in the code of the International Classification of Disease, 10th Revision (ICD-10).
Outcome
We combined mortality data after dialysis initiation from Statistics Korea with our dataset, using each individual’s unique identifier. Post ESRD mortality data were obtained until December 2010 [15].
Statistical analysis
All analyses were conducted using SPSS Statistics V21.0 (IBM Corporation, Armonk, NY, USA). Continuous variables were presented as means ± SD values, and categorical variables were presented as proportions. Differences in continuous variables were analyzed using Student t-tests, while chi-square tests were used to analyze categorical variables. Correlation analysis was conducted using Spearman’s correlation analysis. The factors associated with ER were also evaluated via binary logistic regression. We compared the cumulative incidence of all-cause mortality between ER and LR groups via a log-rank test. Cox’s hazard proportion analysis was used to estimate the hazard ratios (HRs) for all-cause mortality. A logistic regression analysis was used to evaluate the risk of 90-day mortality according to the timing of nephrology referral. P < 0.05 was considered statistically significant.
Results
Characteristics of patients according to timing of nephrology referral
The clinical characteristics of 820 elderly patients with incident hemodialysis are summarized in Table 1. Participants’ mean age and the mean follow-up duration were 76.3 years old and 25.1 months, respectively. Of the 820, 60.5% were men, 65.3% had diabetes, 98.3% had HTN, 36.2% had cardiovascular disease, and patients with ER group were reported in 52.4% of the subjects. Patients were assigned to one of two groups (ER and LR) according to the time of their first encounters with nephrologists. ER group had large proportions of cardiovascular disease and a central venous catheter (CVC) at initiation of dialysis, and had higher baseline Cr and albumin relative to LR group, whereas white blood cell (WBC) count, corrected Ca level, and phosphorous level were lower.
Table 1. Baseline characteristics of patients at initiation of dialysis according to the timing of nephrology referral.
| All 820 | Early referral 430 | Late referral 390 | P-value | |
|---|---|---|---|---|
| Male (%) | 496 (60.5) | 252 (58.6) | 244 (62.6) | 0.253 |
| Age, years | 76.3 ± 5.1 | 76.5 ± 5.3 | 76.2 ± 4.9 | 0.501 |
| Diabetes mellitus (%) | 523 (65.3) | 288 (67.3) | 235 (63.0) | 0.207 |
| Hypertension (%) | 803 (98.3) | 422 (98.4) | 381 (98.2) | 1.000 |
| Cardiovascular disease (%) | 297 (36.2) | 178 (41.4) | 119 (30.5) | 0.001 |
| Malignancy (%) | 109 (13.3) | 61 (14.2) | 48 (12.3) | 0.471 |
| Vascular access for the first dialysis * | <0.001 | |||
| AVF/AVG | 197 (187/10) | 150 (145/5) | 47 (42/5) | |
| CVC | 598 | 276 | 322 | |
| Systolic pressure (mmHg) | 130.8 ± 25.6 | 130.1 ± 25.7 | 131.6 ± 25.5 | 0.395 |
| Diastolic pressure (mmHg) | 73.4 ± 14.8 | 72.9 ± 15.0 | 74.1 ± 14.5 | 0.253 |
| Creatinine (mg/dL) | 6.02 ± 2.47 | 6.20 ± 2.35 | 5.83 ± 2.58 | 0.033 |
| eGFR (ml/min/1.73m 2 ) † | 10.48 ± 4.86 | 9.88 ± 4.37 | 11.15 ± 5.26 | <0.001 |
| WBC (/mm 3 ) | 9.4 ± 5.6 | 8.3 ± 4.2 | 10.7 ± 6.5 | <0.001 |
| Hemoglobin (g/dL) | 9.5 ± 1.7 | 9.5 ± 1.6 | 9.4 ± 1.7 | 0.483 |
| Albumin (g/dL) | 3.2 ± 0.6 | 3.4 ± 0.6 | 3.0 ± 0.6 | <0.001 |
| Corrected Ca (mg/dL) | 8.9 ± 0.8 | 8.8 ± 0.7 | 9.0 ± 0.9 | 0.003 |
| P (mg/dL) | 5.0 ± 1.7 | 4.9 ± 1.6 | 5.2 ± 1.9 | 0.012 |
| Follow up duration, months | 25.1 ± 28.1 | 27.5 ± 26.1 | 22.5 ± 30.0 | 0.012 |
Abbreviations: AVF, arteriovenous fistula; AVG, arteriovenous graft; CVC, central venous catheter; eGFR, estimated glomerular filtration rate; WBC, white blood cell
* Vascular access was analyzed in 795 patients because of unavailable data.
†eGFR was calculated using the Modification of Diet in Renal Disease study equation
Factors associated with early referral
Higher Cr (OR = 1.104, P = 0.007), higher albumin (OR = 2.087, P < 0.001), lower corrected Ca (OR = 0.769 P = 0.010) and lower phosphorous (OR = 0.902, P = 0.045), and arteriovenous fistula (AVF)/arteriovenous graft (AVG) rather than CVC (OR = 3.371, P < 0.001) were observed in the ER group relative to the LR group (Table 2).
Table 2. Factors associated with early referral using multivariable logistic regression.
| Odds ratio | 95% CI | P-value | |
|---|---|---|---|
| Male/Female | 0.809 | 0.588–1.114 | 0.194 |
| Age at diagnosis | 1.031 | 1.000–1.063 | 0.050 |
| Creatinine (mg/dL), per 1- unit ↑ | 1.104 | 1.027–1.187 | 0.007 |
| Albumin (g/dL), per 1- unit ↑ | 2.087 | 1.598–2.725 | <0.001 |
| Corrected Ca (mg/dL), per 1- unit ↑ | 0.769 | 0.630–0.938 | 0.010 |
| P (mg/dL), per 1- unit ↑ | 0.902 | 0.816–0.998 | 0.045 |
| AVF+AVG/CVC for the first dialysis | 3.371 | 2.252–5.046 | <0.001 |
Abbreviations: AVF, arteriovenous fistula; AVG, arteriovenous graft; CVC, central venous catheter
Long-and short-term all-cause mortality according to the referral timing
During a mean follow-up period of 25.1 months, 213 patients (49.5%) in the ER group and 253 patients (64.9%) in the LR group, respectively, died (Figs 1 and 2A). In an adjusted model, the ER group displayed a 24% reduced risk of mortality relative to the LR group (HR = 0.760, P = 0.009) (Table 3). Old age, LR, CVC, high WBC count and corrected Ca level, and lower levels of albumin, Cr, hemoglobin, and sodium were significantly (P < 0.05) associated with increased risk of mortality (data not shown).
Fig 1. Kaplan—Meier curves for 820 patients with end stage renal disease who initiated hemodialysis during total follow-up period.
All-cause mortality rates according to the referral timing.
Fig 2. Death rate during total follow-up period (A) and at 90 days (B) according to referral timing.
Table 3. Effect of timing of nephrology referral on patient survival using multivariable cox proportional hazard model.
| Cox proportional hazard model | HR ER/LR | 95% CI | P-value |
|---|---|---|---|
| Total follow up ACM | 0.760 | 0.619–0.933 | 0.009 |
| 90-Day ACM | 0.422 | 0.215–0.828 | 0.012 |
| After 90-Day ACM | 1.156 | 0.879–1.521 | 0.301 |
Abbreviations: ER, early referral; LR, late referral; ACM, all-cause mortality Multivariable, adjusted for age, gender, diabetes mellitus, hypertension, serum creatinine, albumin, comorbidites including cardiovascular disease and malignancy, type of vascular access at the first dialysis
The overall 90-day mortality rates for patients with ESRD were 3.5% (15 of 430) in the ER group and 11% (43 of 390) in the LR group (Fig 2B). The ER group also demonstrated a reduced 90-day mortality rate relative to that of the LR group after adjustment for age, gender, DM, HTN, cardiovascular disease, malignancy, type of vascular access at the time of the first dialysis, WBC, albumin, and Cr (HR = 0.422, P = 0.012) However, after 90 days, the referral pattern was not associated with the mortality rates (Table 3). High WBC, presence of cardiovascular disease at start of dialysis were significantly (P < 0.05) associated with increased risk of mortality (data not shown).
Discussion
In this study of patients initiating dialysis between 2000 and 2010, 820 patients aged 70 years or older were included, and 52.4% presented early nephrology referral. We identified the factors associated ER and found ER also improved short-and long-term survival rates of the elderly.
The proportion of patients who received LR was higher in our study population compare to the 41% reported in a study conducted by Kim et al. showing an extended cutoff point for LR (LR < 1 year) [16]. In general, approximately 30% of patients globally [8,17], 34% of patients in the United States and United Kingdom, and approximately 23% of patients in Australasia [17] receive LR. The possible explanations for the difference observed in our study compared to others are as follows: The first reason may be that the study was performed in a large tertiary hospital in Korea, in which individuals are at higher risk of LR. The second possible reason is that there was no universal definition for nephrology referral timing in CKD patients. The definitions for LR timing were within 1 month [18], 3–4 months [19–27], 6 months [28,29], and 1 year [16]. Although some studies have questioned whether a cutoff time of 3 months within which to distinguish between LR and ER is adequate [16,30], the most broadly accepted definition of LR is the first encounter with a nephrologist within 3–4 months prior to ESRD diagnosis [8,17]. We adopted this period in this study.
The factors associated with ER were higher albumin and Cr levels, and higher frequency of AVF/AVG. With the exception of the finding that higher Cr level was observed in the ER group, our results for factors associated with ER were consistent with those of Arora et al [31].
A reduced long-term mortality rate of 24% was observed in the ER group. In our data, a steeper slope of mortality was observed during the early-period (within 90-days) of dialysis and was remarkable in the LR group. After 90 days, the slope of mortality ran parallel between the ER and LR groups (Fig 1). To highlight the effect of referral timing on mortality within 90 days, we removed 90-day mortality data and calculated the mortality rate after 90 days. The 90-day mortality reduction in ER patients was 58% for patients aged 70 years or older; this reduction was greater than those observed during the total follow-up period. Furthermore, the statistical significance of the mortality differences after 90 days between the ER and LR groups was not observed across age groups. Therefore, mortality differences for the total follow-up period were related to the early-period (within-90 days) of dialysis. These results were consisted with a recent systematic review reporting that ER reduced mortality compared with LR, and differences in mortality at 5 years were correlated with the initial 0–3 month mortality rates [8]. In addition, some reports showed that patients who had undergone incident hemodialysis had the highest mortality in the first several months after dialysis initiation and pre-dialysis care was included as a modifiable risk factor [32–36]. In fact, previous studies reported that ER patients had higher survival rate in elderly patients as well as younger patients [12,16]. However, in the elderly, whether timing of referral is associated with long- and short-term (90-day) mortality has not been reported. Therefore, we emphasize the originality of this study in that timing of referral affects the early-period (90-day) mortality and long-term mortality of the elderly. LR group, higher WBC count, presence of cardiovascular disease at start of dialysis associated with short-term mortality. LR group, old age, CVC, higher WBC count and lower levels of albumin, hemoglobin, and sodium were significantly associated with increased risk of long-term mortality. Although we did not specifically explain the contributory causes of death in our data, it was inferred that acute complications during the early period of dialysis, including infection, vascular access, and cardiovascular events, could contribute to higher early mortality rates such as those reported in the U.S. Renal Data System [37]. Therefore, ER could lead to planned transition to ESRD by preventing acute complications and reducing mortality, which is also true in elderly patients.
In fact, previous studies showing the influence of the timing of referral on mortality rates have demonstrated negative results. Schmidt et al. reported no statistical difference in 4-month mortality between ER (>1 month) and LR [18]. In addition, Roubicek et al. showed that there were no differences in the 3-month, 1-year, or 5-year survival rates according to referral patterns (ER > 4 months) in 270 patients [21]. Wolfgang et al. reported no material improvement in 1-year survival rates despite significant trends toward ER in older patients [13]. There are several limitations to the studies showing negative results as follows: 1-month period before dialysis is too short to demonstrate the benefits of nephrological intervention, and the studies involved small study populations, and did not perform direct comparisons between ER and LR to evaluate survival outcomes but examined trends in 1-year survival rates over a decade in the elderly.
This study has several limitations. First, although favorable biochemical parameters for hemoglobin and albumin were postulated as the cause of improved survival rates, we cannot explain exactly which interventions, performed by nephrologists for the ER group, improved survival rates. Second, we did not adjust for medications.
In conclusion, timely referral was also associated with reduced mortality in the elderly with incident hemodialysis treatment; in particular, the initial 90-day mortality reduction in ER patients contributed to mortality differences observed for the total follow-up period.
Data Availability
All relevant data are within the paper.
Funding Statement
The authors have no support or funding to report.
References
- 1. Foley RN, Collins AJ (2007) End-stage renal disease in the United States: an update from the United States Renal Data System. J Am Soc Nephrol 18: 2644–2648. [DOI] [PubMed] [Google Scholar]
- 2. Stengel B, Billon S, Van Dijk PC, Jager KJ, Dekker FW, Simpson K, et al. (2003) Trends in the incidence of renal replacement therapy for end-stage renal disease in Europe, 1990–1999. Nephrol Dial Transplant 18: 1824–1833. [DOI] [PubMed] [Google Scholar]
- 3. Kurella M, Covinsky KE, Collins AJ, Chertow GM (2007) Octogenarians and nonagenarians starting dialysis in the United States. Ann Intern Med 146: 177–183. [DOI] [PubMed] [Google Scholar]
- 4. Krishnan M, Lok CE, Jassal SV (2002) Epidemiology and demographic aspects of treated end-stage renal disease in the elderly. Semin Dial 15: 79–83. [DOI] [PubMed] [Google Scholar]
- 5. Foote C, Ninomiya T, Gallagher M, Perkovic V, Cass A, McDonald SP, et al. (2012) Survival of elderly dialysis patients is predicted by both patient and practice characteristics. Nephrol Dial Transplant 27: 3581–3587. 10.1093/ndt/gfs096 [DOI] [PubMed] [Google Scholar]
- 6. Jungers P, Zingraff J, Page B, Albouze G, Hannedouche T, Man NK (1993) Detrimental effects of late referral in patients with chronic renal failure: a case-control study. Kidney Int Suppl 41: S170–173. [PubMed] [Google Scholar]
- 7. Astor BC, Eustace JA, Powe NR, Klag MJ, Sadler JH, Fink NE, et al. (2001) Timing of nephrologist referral and arteriovenous access use: the CHOICE Study. Am J Kidney Dis 38: 494–501. [DOI] [PubMed] [Google Scholar]
- 8. Smart NA, Titus TT (2011) Outcomes of early versus late nephrology referral in chronic kidney disease: a systematic review. Am J Med 124: 1073–1080 e1072 10.1016/j.amjmed.2011.04.026 [DOI] [PubMed] [Google Scholar]
- 9. Winkelmayer WC, Glynn RJ, Levin R, Owen WF Jr, Avorn J (2001) Determinants of delayed nephrologist referral in patients with chronic kidney disease. Am J Kidney Dis 38: 1178–1184. [DOI] [PubMed] [Google Scholar]
- 10. Carson RC, Juszczak M, Davenport A, Burns A (2009) Is maximum conservative management an equivalent treatment option to dialysis for elderly patients with significant comorbid disease? Clin J Am Soc Nephrol 4: 1611–1619. 10.2215/CJN.00510109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Schwenger V, Morath C, Hofmann A, Hoffmann O, Zeier M, Ritz E (2006) Late referral—a major cause of poor outcome in the very elderly dialysis patient. Nephrol Dial Transplant 21: 962–967. [DOI] [PubMed] [Google Scholar]
- 12. de Jager DJ, Voormolen N, Krediet RT, Dekker FW, Boeschoten EW, Grootendorst DC (2011) Association between time of referral and survival in the first year of dialysis in diabetics and the elderly. Nephrol Dial Transplant 26: 652–658. 10.1093/ndt/gfq438 [DOI] [PubMed] [Google Scholar]
- 13. Winkelmayer WC, Liu J, Chertow GM, Tamura MK (2011) Predialysis nephrology care of older patients approaching end-stage renal disease. Arch Intern Med 171: 1371–1378. 10.1001/archinternmed.2011.360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Levey AS, Coresh J, Greene T, Stevens LA, Zhang YL, Hendriksen S, et al. (2006) Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med 145: 247–254. [DOI] [PubMed] [Google Scholar]
- 15.Available: http://mdss.kostat.go.kr/mdssext/index.jsp?sso=ok.
- 16. Kim do H, Kim M, Kim H, Kim YL, Kang SW, Yang CW, et al. (2013) Early referral to a nephrologist improved patient survival: prospective cohort study for end-stage renal disease in Korea. PLoS One 8: e55323 10.1371/journal.pone.0055323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Foote C, Clayton PA, Johnson DW, Jardine M, Snelling P, Cass A (2014) Impact of estimated GFR reporting on late referral rates and practice patterns for end-stage kidney disease patients: a multilevel logistic regression analysis using the Australia and New Zealand Dialysis and Transplant Registry (ANZDATA). Am J Kidney Dis 64: 359–366. 10.1053/j.ajkd.2014.02.023 [DOI] [PubMed] [Google Scholar]
- 18. Schmidt RJ, Domico JR, Sorkin MI, Hobbs G (1998) Early referral and its impact on emergent first dialyses, health care costs, and outcome. Am J Kidney Dis 32: 278–283. [DOI] [PubMed] [Google Scholar]
- 19. Dogan E, Erkoc R, Sayarlioglu H, Durmus A, Topal C (2005) Effects of late referral to a nephrologist in patients with chronic renal failure. Nephrology (Carlton) 10: 516–519. [DOI] [PubMed] [Google Scholar]
- 20. Kazmi WH, Obrador GT, Khan SS, Pereira BJ, Kausz AT (2004) Late nephrology referral and mortality among patients with end-stage renal disease: a propensity score analysis. Nephrol Dial Transplant 19: 1808–1814. [DOI] [PubMed] [Google Scholar]
- 21. Roubicek C, Brunet P, Huiart L, Thirion X, Leonetti F, Dussol B, et al. (2000) Timing of nephrology referral: influence on mortality and morbidity. Am J Kidney Dis 36: 35–41. [DOI] [PubMed] [Google Scholar]
- 22. Stoves J, Bartlett CN, Newstead CG (2001) Specialist follow up of patients before end stage renal failure and its relationship to survival on dialysis. Postgrad Med J 77: 586–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Winkelmayer WC, Owen WF Jr, Levin R, Avorn J (2003) A propensity analysis of late versus early nephrologist referral and mortality on dialysis. J Am Soc Nephrol 14: 486–492. [DOI] [PubMed] [Google Scholar]
- 24. Cass A, Cunningham J, Arnold PC, Snelling P, Wang Z, Hoy W (2002) Delayed referral to a nephrologist: outcomes among patients who survive at least one year on dialysis. Med J Aust 177: 135–138. [DOI] [PubMed] [Google Scholar]
- 25. Ellis PA, Reddy V, Bari N, Cairns HS (1998) Late referral of end-stage renal failure. QJM 91: 727–732. [DOI] [PubMed] [Google Scholar]
- 26. Hoffmann M, Binaut R, Maisonneuve N, Bacri JL, Fleury D, Vanhille P, et al. (2006) [Patterns of nephrology referral and predialysis management of patients with chronic kidney disease]. Nephrol Ther 2: 15–23. [DOI] [PubMed] [Google Scholar]
- 27. Stack AG (2003) Impact of timing of nephrology referral and pre-ESRD care on mortality risk among new ESRD patients in the United States. Am J Kidney Dis 41: 310–318. [DOI] [PubMed] [Google Scholar]
- 28. Jungers P, Joly D, Nguyen-Khoa T, Mothu N, Bassilios N, Grunfeld JP (2006) [Continued late referral of patients with chronic kidney disease. Causes, consequences, and approaches to improvement]. Presse Med 35: 17–22. [DOI] [PubMed] [Google Scholar]
- 29. Gallego E, Lopez A, Lorenzo I, Lopez E, Llamas F, Illescas ML, et al. (2003) [Influence of early or late referral to nephrologist over morbidity and mortality in hemodialysis]. Nefrologia 23: 234–242. [PubMed] [Google Scholar]
- 30. Quaglia M, Canavese C, Stratta P (2011) Early nephrology referral: how early is early enough? Arch Intern Med 171: 2065–2066; author reply 2067. 10.1001/archinternmed.2011.585 [DOI] [PubMed] [Google Scholar]
- 31. Arora P, Obrador GT, Ruthazer R, Kausz AT, Meyer KB, Jenuleson CS, et al. (1999) Prevalence, predictors, and consequences of late nephrology referral at a tertiary care center. J Am Soc Nephrol 10: 1281–1286. [DOI] [PubMed] [Google Scholar]
- 32. Bradbury BD, Fissell RB, Albert JM, Anthony MS, Critchlow CW, Pisoni RL, et al. (2007) Predictors of early mortality among incident US hemodialysis patients in the Dialysis Outcomes and Practice Patterns Study (DOPPS). Clin J Am Soc Nephrol 2: 89–99. [DOI] [PubMed] [Google Scholar]
- 33. Chan KE, Maddux FW, Tolkoff-Rubin N, Karumanchi SA, Thadhani R, Hakim RM (2011) Early outcomes among those initiating chronic dialysis in the United States. Clin J Am Soc Nephrol 6: 2642–2649. 10.2215/CJN.03680411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lukowsky LR, Kheifets L, Arah OA, Nissenson AR, Kalantar-Zadeh K (2012) Patterns and predictors of early mortality in incident hemodialysis patients: new insights. Am J Nephrol 35: 548–558. 10.1159/000338673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. McQuillan R, Trpeski L, Fenton S, Lok CE (2012) Modifiable risk factors for early mortality on hemodialysis. Int J Nephrol 2012: 435736 10.1155/2012/435736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Perl J, Wald R, McFarlane P, Bargman JM, Vonesh E, Na Y, et al. (2011) Hemodialysis vascular access modifies the association between dialysis modality and survival. J Am Soc Nephrol 22: 1113–1121. 10.1681/ASN.2010111155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Collins AJ, Foley RN, Gilbertson DT, Chen SC (2009) The state of chronic kidney disease, ESRD, and morbidity and mortality in the first year of dialysis. Clin J Am Soc Nephrol 4 Suppl 1: S5–11. 10.2215/CJN.05980809 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.