Abstract
Objectives:
To determine whether the tumor necrosis factor α inhibitor etanercept is well tolerated and obtain preliminary data on its safety in Alzheimer disease dementia.
Methods:
In a double-blind study, patients with mild to moderate Alzheimer disease dementia were randomized (1:1) to subcutaneous etanercept (50 mg) once weekly or identical placebo over a 24-week period. Tolerability and safety of this medication was recorded including secondary outcomes of cognition, global function, behavior, and systemic cytokine levels at baseline, 12 weeks, 24 weeks, and following a 4-week washout period. This trial is registered with EudraCT (2009-013400-31) and ClinicalTrials.gov (NCT01068353).
Results:
Forty-one participants (mean age 72.4 years; 61% men) were randomized to etanercept (n = 20) or placebo (n = 21). Etanercept was well tolerated; 90% of participants (18/20) completed the study compared with 71% (15/21) in the placebo group. Although infections were more common in the etanercept group, there were no serious adverse events or new safety concerns. While there were some interesting trends that favored etanercept, there were no statistically significant changes in cognition, behavior, or global function.
Conclusions:
This study showed that subcutaneous etanercept (50 mg/wk) was well tolerated in this small group of patients with Alzheimer disease dementia, but a larger more heterogeneous group needs to be tested before recommending its use for broader groups of patients.
Classification of evidence:
This study shows Class I evidence that weekly subcutaneous etanercept is well tolerated in Alzheimer disease dementia.
Acute and chronic systemic inflammation is characterized by the production of proinflammatory cytokines including tumor necrosis factor α (TNF-α) from immune cells. TNF-α has a role in systemic immune-to-brain communication by activating the central immune response.1 In humans, low levels of chronic systemic inflammation are associated with evidence of microglial activation.2 In animals, experimentally induced acute systemic inflammation results in an exaggerated central immune response leading to exacerbated neurodegeneration.3 In participants with Alzheimer disease (AD) dementia, we have shown that modestly increased serum TNF-α levels are associated with an increased rate of cognitive decline4 and an exaggeration of neuropsychiatric symptoms.5
Peer-reviewed published data on the use of the TNF-α inhibitor etanercept in AD dementia is limited to small open-label studies6–8 purporting to deliver etanercept centrally9 through a perispinal administration route. However, we have hypothesized that peripheral administration of a TNF-α inhibitor with high affinity and specificity could, if well tolerated and safe, have long-term beneficial cognitive and behavioral efficacy in an AD dementia population through inhibition of peripheral signaling to the brain.10 Peripheral administration of TNF-α inhibitors is licensed for a wide range of rheumatologic and skin conditions in the elderly but there are no randomized placebo-controlled trials (RPCTs) of these drugs in AD dementia that give comparative data regarding tolerability, safety, or its effects (beneficial or otherwise) on measures of clinical outcome. We report the findings of a double-blind, phase 2 RPCT examining the tolerability, safety, and clinical effects on secondary clinical psychometric measures of subcutaneous etanercept in a mild to moderate AD population.
METHODS
Standard protocol approvals, registrations, and participant consents.
The protocol and consent forms were approved by a multicenter research ethics committee (Southampton and South West Hampshire REC [A], reference number 10/H0502). All participants provided informed consent before screening procedures. The study was registered with EudraCT (2009-013400-31) and ClinicalTrials.gov (NCT01068353).
Study design and participants.
Safety and Tolerability of Etanercept in Alzheimer's Disease was an investigator-initiated, 24-week, single-center, phase 2, double-blind RPCT to assess the tolerability and safety of weekly 50 mg subcutaneous etanercept in participants with AD dementia including cognitive, behavioral, and functional outcomes.
The study was performed in accordance with the Declaration of Helsinki and the principles of Good Clinical Practice. An independent data and safety monitoring board monitored adverse events.
At screening, eligible participants had to be aged 55 years or older, be diagnosed with probable AD defined by the National Institute of Neurological and Communicative Disorders and Stroke–Alzheimer's Disease and Related Disorders Association criteria11 (diagnostic accuracy approximately 75%12,13), have a modified Hachinski Ischemic Scale score14 of less than 5 points, have a standardized Mini-Mental State Examination (sMMSE)15 score above 10 and below 27 points, have an informant spending at least 24 hours per week with the participant, and be capable of giving informed consent. Patients receiving a cholinesterase inhibitor, memantine, or antidepressant medication were required to have been on medication for a minimum period of 90 days before baseline. Patients with prior exposure to amyloid vaccines, monoclonal antibodies, or IV immunoglobulins for the treatment of AD were excluded. Patients with rheumatoid arthritis, psoriasis, psoriatic arthritis, or ankylosing spondylitis, or those taking anti–TNF-α agents, immunosuppressive drugs, and/or oral prednisone >10 mg/d within the past 90 days were excluded. Participants with known contraindications (active infections) or cautions (previous significant exposure to tuberculosis, herpes zoster, hepatitis B, heart failure [New York Heart Association grades 3 and 4], demyelination disorders, and active malignancy within past 5 years) to the use of etanercept were excluded.
Randomization and masking.
ACE Pharmaceuticals BV (Zeewolde, the Netherlands) manufactured the placebo and packaged both the study medication and placebo to ensure blinding. They used a computer to generate a simple random allocation sequence (1:1), stratified in blocks of 4, to ensure 20 patients in the treatment group (subcutaneous etanercept 50 mg) and 20 patients in the placebo group (water for injection). The investigators had no knowledge of the allocation sequence, which remained concealed throughout the study. ACE Pharmaceuticals loaded etanercept or placebo vials into serially numbered containers according to the allocation sequence. The loaded containers, and the interventions inside them, were identical in appearance and consistency to ensure concealment of the allocation sequence from the investigators. After successful screening, participants were assigned the container with the next available serial number in strict chronological order. Study drug was administered by weekly subcutaneous injection at home or in the clinic by study team health professionals who were blinded to treatment allocation.
Procedures.
Following consent, patients underwent a screening period including initial tuberculosis and infectious disease screen (i.e., a chest radiograph, tuberculin skin, and an interferon gamma release test). Participants fulfilling the inclusion and exclusion criteria received etanercept 50 mg or placebo subcutaneously once per week for 24 weeks. This was followed by a 4-week washout period in which no injections were given but in which blinding was maintained. Clinic visits took place at screening, baseline, week 12, week 24, and 4 weeks after the last study drug injection (week 28). Patients who withdrew from the study before scheduled clinic visits were seen within 1 week of withdrawal for an early termination visit. During these visits, adverse event monitoring and psychometric evaluation took place. Adverse events were recorded as definitely related, probably related, possibly related, unlikely to be related, or unrelated to the blinded study intervention. Patients experiencing a serious adverse event or recurrent infections were withdrawn from the study. Psychometric measures included the sMMSE,15 Alzheimer's Disease Assessment Scale–cognitive section (ADAS-cog),16 Bristol Activities of Daily Living Scale (BADLS),17 Clinical Global Impression–Improvement (CGI-I) scale,18 Cornell Scale for Depression in Dementia (Cornell),19 and the Neuropsychiatric Inventory (NPI).20
At screening, blood samples were taken for routine clinical laboratory assessments with additional measures of immunoglobulins, anti-nuclear antibody, anti-cardiolipin, and a midstream urine test for infection. Blood for DNA (principally for APOE ε4 analysis) was taken at baseline. APOE genotypes were determined by TaqMan genotyping of single nucleotide polymorphism (SNP) rs7412 and KASP genotyping of SNP rs429358. Blood for routine laboratory assessments and serum inflammatory markers were taken at baseline, week 12, week 24, and week 28 between 9 am and 12 noon. Serum samples for inflammatory markers were immediately placed on ice and stored within 2 hours at −80°C. Samples were analyzed blind to the treatment allocation using a V-PLEX assay (Meso Scale Discovery [MSD]). A protocol provided by MSD for custom assays was used with no major modifications. Five serum inflammatory markers were measured: TNF-α, interleukin (IL)-6, IL-10, IL-12p70, and C-reactive protein (CRP).
Outcomes.
The primary outcomes of the study were tolerability and safety. Tolerability was measured by compliance (number of injections given/number of planned injections) over the 24-week trial period. Associated safety was measured by the number of serious adverse events and adverse events during the study treatment period coded using the Medical Dictionary for Regulatory Activities (version 15.0) preferred term (http://www.meddra.org). A symptom checklist was used at each visit to probe for adverse events.
Secondary outcomes were differences in the change from baseline of the psychometric measures (sMMSE, ADAS-cog, BADLS, CGI-I, Cornell, and NPI) at 12 weeks and 24 weeks between intervention groups for observed cases and intention to treat–last observation carried forward (ITT-LOCF). In addition, emergent adverse events and psychometric changes following a 4-week washout phase were measured.
Statistical analysis.
This study was powered to assess tolerability (dropout rates) of weekly etanercept 50-mg subcutaneous injections and to identify adverse events associated with poor tolerability in an AD dementia population. The study also aimed to inform a potential phase 3 study of the variance and mean differences in clinical outcome measures. To measure dropout such that a 95% confidence interval (CI) about the estimated rate had a margin of error of ±15%, normal approximation about a proportion showed that 36 to 41 participants would be required for a dropout rate commensurate with previous AD studies of between 29% and 41%.21,22 This sample size also fell between 24 and 50 recommended as necessary to estimate SDs for a future phase 3 study.23–25 Efficacy analyses were performed on observed cases, defined as all patients who received at least one dose of study medication, and who provided data at baseline, week 12, and week 24, and on ITT-LOCF cases, defined as all patients who received at least one dose of study medication, and had at least one postrandomization assessment. Study demographic characteristics, efficacy measure outcomes, and serum inflammatory proteins were assessed for normality using Q-Q plots. Changes in psychometric measures and serum inflammatory protein levels between the 2 intervention groups were measured by unpaired t test and linear regression for parametric variables or Mann–Whitney U test for nonparametric variables. Clinical psychometric outcomes were adjusted for baseline age, sex, and baseline psychometric score, and were conducted at p < 0.0017 significance to allow for 30 multiple comparisons.
RESULTS
Participant disposition.
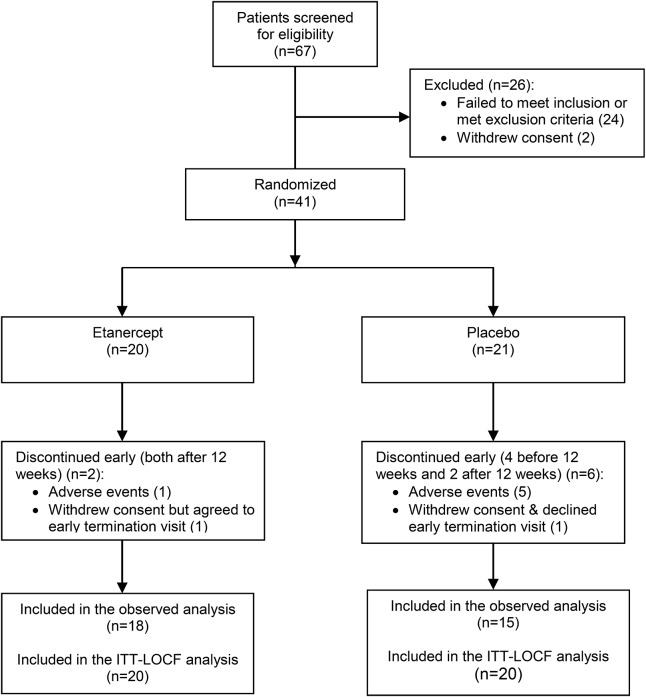
Participant disposition is detailed in figure 1. Between January 2011 and February 2013, a total of 67 patients were screened at the Memory Assessment and Research Centre, Southampton, UK, of whom 41 entered the study and were assigned to either etanercept or placebo. Reasons for screen failure included prior exposure to tuberculosis or latent tuberculosis (46% [12/26]), monoclonal gammopathy of unknown significance (12% [3/26]), MMSE screen failure (8% [2/26]), abnormal chest radiology (8% [2/26]), skin cancer (8% [2/26]), consent withdrawn before baseline (8% [2/26]), abdominal aortic aneurysm requiring surgery (4% [1/26]), clinically significant anemia (4% [1/26]), and lack of adequate informant time (4% [1/26]).
Figure 1. Trial profile.
ITT-LOCF = intention to treat–last observation carried forward.
Randomization phase.
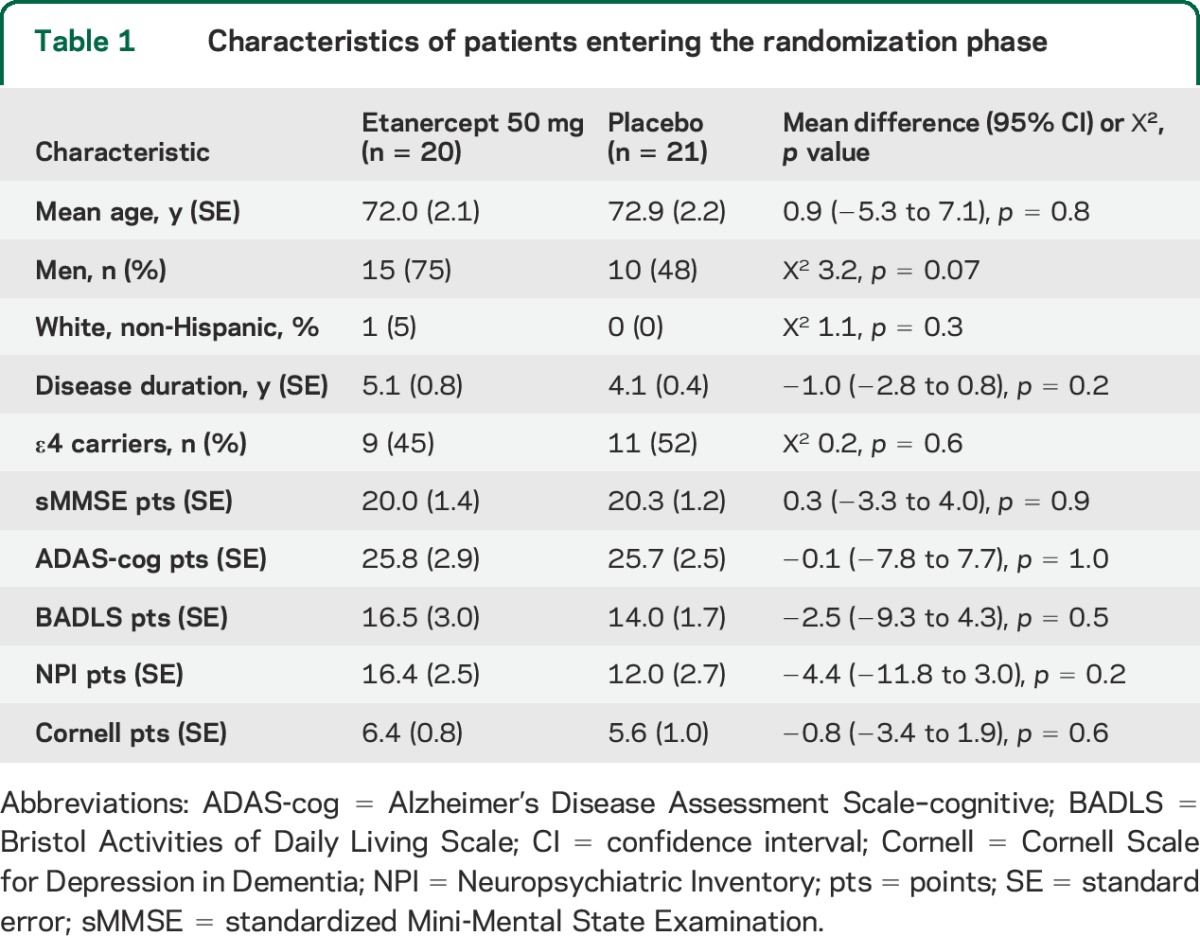
The mean age of the patients entering the study was 72.4 (SD 9.7) years, and the majority (61%) were men. Randomization of patients at baseline led to 2 treatment groups that were similar in demographic details, APOE ε4 carrier status, and psychometric test scores (p values in all cases >0.1 except sex, p = 0.07) (table 1). There was no significant difference between treatment groups in the frequency of participants taking a cholinesterase inhibitor (16/20 [80%] etanercept vs 18/21 [86%] placebo; Χ2 0.2, p = 0.6), memantine (3/20 [15%] etanercept vs 3/21 [14%] placebo; Χ2 0.004, p = 0.9), or antidepressant medication (7/20 [35%] etanercept vs 8/21 [38%] placebo; Χ2 0.01, p = 0.8).
Table 1.
Characteristics of patients entering the randomization phase
Tolerability and safety.
Compliance to medication was high over the 6-month trial period: overall median 100% (interquartile range [IQR] 87.5%–100%). There was no significant difference in the median compliance frequency between treatment groups (etanercept 100% [IQR 95.8%–100%] vs placebo 94% [IQR 62.5%–100%]; MWU p = 0.2). Eight participants (20%) (2 on etanercept and 6 on placebo) failed to complete the study following randomization. Of the 8 noncompleters, 4 participants (all taking placebo) failed to complete the study to 12 weeks, of whom one declined an early termination visit, and 4 participants (2 taking placebo and 2 taking etanercept) failed to complete the study to 24 weeks. Of the 2 noncompleters in the etanercept group, one participant contracted a chest infection and was withdrawn because of safety concerns and one participant withdrew consent because of drug delivery logistic problems. Of the 6 noncompleters in the placebo group, 5 participants were withdrawn because of safety concerns (one participant contracted a urinary tract infection, one developed a monoclonal gammopathy of unknown significance, one experienced blood in stools, one experienced worsening of behavioral symptoms, and one participant required an elective hip replacement). One participant withdrew consent because of family commitments.
The overall study completion was 81% (33/41). There was no statistical difference in the completion rates between those allocated to etanercept and those allocated to placebo (90% [18/20] from the etanercept group were completers vs 71% [15/21] from the placebo group; Fisher exact test, p = 0.2).
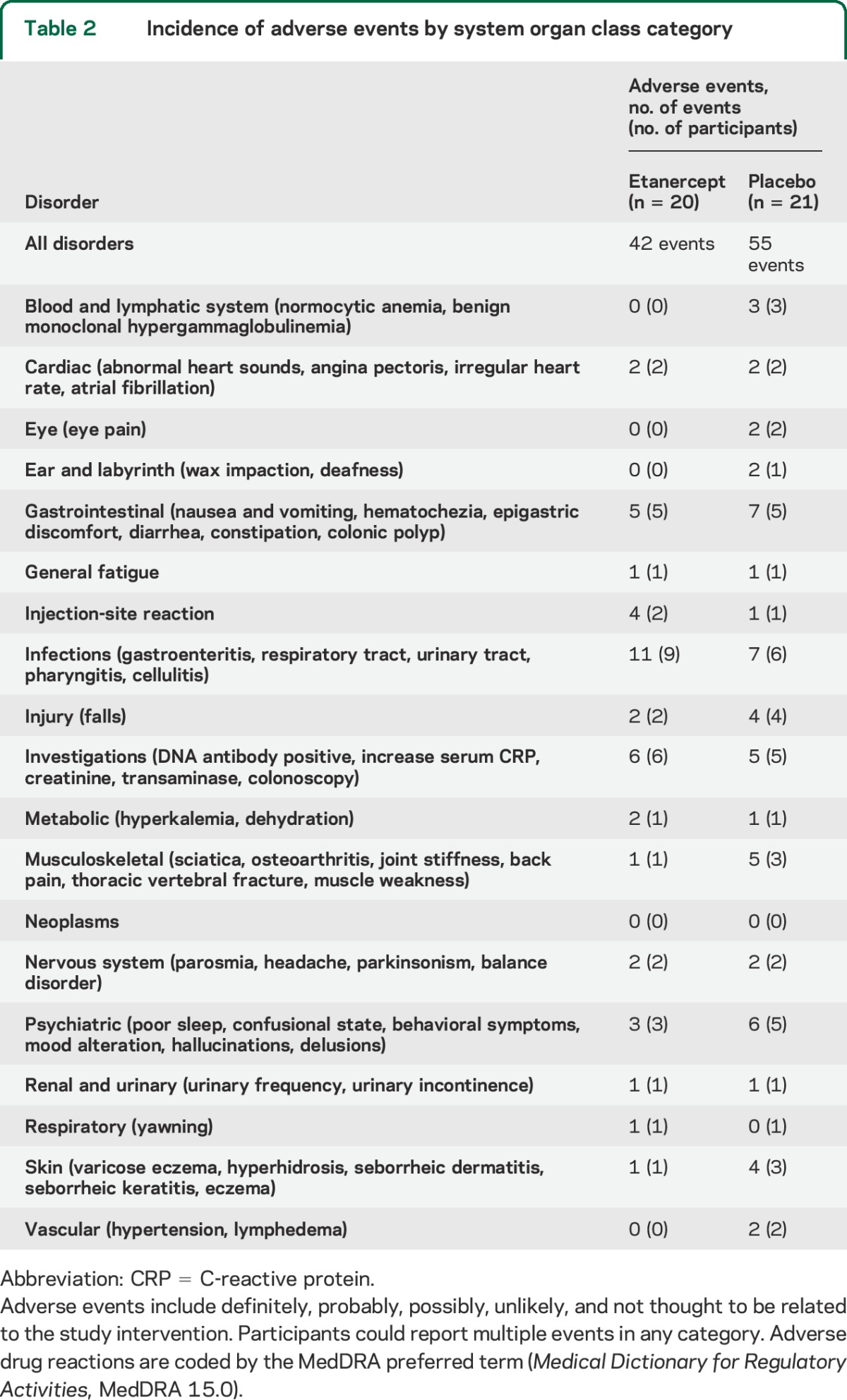
A total of 97 adverse events occurred during the 24-week randomization phase of the study with one serious adverse event (one participant in the placebo arm was admitted to hospital with a urinary tract infection). Adverse events grouped by system are summarized in table 2. There were 42 (43%) adverse events in 20 participants in the etanercept group and 55 (57%) in 21 participants in the placebo group. Infections, injection site reactions, and investigational abnormalities were present in a greater number of participants in the etanercept arm compared with the placebo arm but no statistical differences were found between groups (Χ2, all p > 0.1).
Table 2.
Incidence of adverse events by system organ class category
Secondary clinical outcomes.
Changes in psychometric scores for observed cases and ITT-LOCF at 12 and 24 weeks after randomization are shown in table 3 and figure 2. One participant randomized to placebo withdrew from the study at 4 weeks and declined an early termination assessment of clinical outcomes. Increases in psychometric scores from baseline indicate a worsening in outcomes except for the sMMSE for which an increase indicates an improvement. None of the clinical outcomes were statistically significant between treatment groups following Bonferroni correction.
Table 3.
Changes in psychometric scores 12 weeks and 24 weeks for observed and ITT-LOCF after randomization compared with baseline

Figure 2. Mean change in outcome scores (observed cases weeks 12 and 24) and ITT-LOCF (week 24) from baseline.
ADAS-cog = Alzheimer's Disease Assessment Scale–cognitive; BADLS = Bristol Activities of Daily Living Scale; CGI-I = Clinical Global Impression–Improvement; Cornell = Cornell Scale for Depression in Dementia; ITT-LOCF = intention to treat–last observation carried forward; MMSE = standardized Mini-Mental State Examination; NPI = Neuropsychiatric Inventory.
Washout phase.
No serious adverse events occurred during the 4-week washout phase of the study. Six participants experienced a total of 7 adverse events: 3 adverse events (fall, upper respiratory tract infection, gastric irritation) in 3 participants taking etanercept previously and 4 adverse events (disturbed sleep, fall, constipation and fall) in 3 participants taking placebo previously.
Allowing for Bonferroni correction, there were no significant differences in the change of psychometric scores for the sMMSE, ADAS-cog, BADLS, NPI, Cornell, or CGI-I during the 4-week washout phase of the study between those participants previously taking etanercept compared with those previously taking placebo: sMMSE: etanercept −0.3 vs placebo −0.1 points (mean difference −0.2 points [95% CI 1.7 to −2.0]), p = 0.9; ADAS-cog: etanercept 1.3 vs placebo −4.2 points (mean difference 5.5 points [95% CI 9.0–2.0]), p = 0.003; BADLS: etanercept 2.4 vs placebo −1.7 points (mean difference 4.1 points [95% CI 7.0 to −1.4]), p = 0.004; NPI: etanercept −2.4 vs placebo −3.5 points (mean difference 1.1 points [95% CI 7.7 to −5.6]), p = 0.7; Cornell: etanercept −0.8 vs placebo −2.1 points (mean difference 1.2 points [95% CI 3.1 to −0.6]), p = 0.6; CGI-I: etanercept 0 vs placebo 0 points (mean difference 0 points [95% CI 0.7 to −0.8]), p = 1.0.
Serum inflammatory markers.
Serum was not available in one (placebo randomized) participant. Serum levels for TNF-α, IL-6, IL-10, IL-12p70, and CRP for all other participants completing the study (18 randomized to etanercept and 14 to placebo) are shown at baseline (week 0), week 12, week 24, and after the 4-week washout phase (week 28) in table e-1 on the Neurology® Web site at Neurology.org. At baseline, there were no statistical differences in serum TNF-α or IL-12 between the treatment and placebo groups. Following randomization, serum TNF-α was higher in the treatment compared with the placebo group at weeks 12 and 24 and was still significantly increased, although diminished, at week 28. Serum IL-12 was also higher in the treatment compared with the placebo group at week 12 but not significantly different from placebo at week 24 or week 28. At baseline, serum IL-10 was statistically lower in the treatment compared with the placebo group. Following randomization, serum IL-10 was no longer significantly different from placebo at week 12 or 24, but following withdrawal was lower in the treatment arm at week 28. There were no significant differences between the serum inflammatory markers IL-6 or CRP between the treatment and placebo groups at baseline or weeks 12, 24, and 28.
DISCUSSION
Of the 67 patients screened for this study, 26 failed to meet the inclusion or exclusion criteria. The 2-year recruitment period was the result of screening failures, the majority of which (n = 12 [46%]) were attributable to prior exposure to tuberculosis, of high frequency in the United Kingdom aged population,26 and to drug delivery delay following Pfizer's acquisition of Wyeth. Compliance was high over the 24-week trial period with no significant differences between treatment groups. Ninety percent of patients (18/20) completed the etanercept arm of the study. There were no serious adverse events in the etanercept arm. Adverse events, including infection rates and injection-site reactions, were in keeping with the known, and potentially serious, side effects of etanercept,27 but no new safety concerns were found regarding the use of etanercept in patients with AD dementia.
Whereas the psychometric changes in the placebo arm are in keeping with observed changes reported elsewhere in similar populations,28,29 the change in ADAS-cog was double than anticipated.4 While every attempt was made to improve internal validity by ensuring raters received the same psychometric rating training and, wherever possible, not change between visits, small numbers in the study cannot rule out the random allocation of a more rapidly declining group to the placebo arm and differences between groups should be viewed with caution. There was no statistical difference between the cognitive, functional, and behavioral assessments in the etanercept compared with the placebo group (or worsening following withdrawal) after Bonferroni correction. Serum TNF-α showed a marked increase in the etanercept-treated group compared with the placebo group, reflecting the increased half-life of the inert dimeric fusion protein after binding of TNF-α.30,31
The use of subcutaneous etanercept in this study is based on the hypothesis of modifying long-term, low-grade peripheral systemic inflammation,1,4,10,32 a different concept than the hypothesized rapid modification of central TNF-α through a periventricular approach,7 which has not been participant to an RPCT and remains highly controversial.33
The current study should not be seen to support the use of unlicensed subcutaneous etanercept for the treatment of AD dementia. Etanercept has recognized potentially serious adverse effects in the population,27 and independent validation is needed in a larger more heterogeneous AD dementia population to fully assess the long-term safety and clinical effects of this approach.
Supplementary Material
ACKNOWLEDGMENT
The authors thank study personnel at the Memory Assessment and Research Centre who were involved in administration, drug delivery, venesection, and sample preparation including Lyn Davies, Suzanne Dodge, Isobel Lewsey, Margaret Nicholls, Ceri Rayner, Rebecca Sussams, and Annette Stevens. The authors also thank NIHR DenDRoN for support and all patients and carers who took part in this study.
GLOSSARY
- AD
Alzheimer disease
- ADAS-cog
Alzheimer's Disease Assessment Scale–cognitive
- BADLS
Bristol Activities of Daily Living Scale
- CGI-I
Clinical Global Impression–Improvement
- CI
confidence interval
- CRP
C-reactive protein
- IL
interleukin
- IQR
interquartile range
- ITT-LOCF
intention to treat–last observation carried forward
- NPI
Neuropsychiatric Inventory
- RPCT
randomized placebo-controlled trial
- sMMSE
standardized Mini-Mental State Examination
- TNF-α
tumor necrosis factor α
Footnotes
Supplemental data at Neurology.org
AUTHOR CONTRIBUTIONS
J.B. made a substantial contribution to the design of the work, the acquisition and interpretation of the data, drafting the work, and reviewing it for important intellectual content. L.B. made a substantial contribution to the design of the work, the acquisition of the data, and reviewing it for important intellectual content. V.H., J.T., U.P., R.S., S.S., R.R., R.T. made a substantial contribution to the acquisition of the data and reviewing it for important intellectual content. P.P., V.H.P., D.C., B.M. made a substantial contribution to the interpretation of the data and reviewing it for important intellectual content. C.H. made a substantial contribution to the conception of the study, the design of the work, the acquisition and interpretation of the data, drafting the work, and reviewing it for important intellectual content. All authors had full access to all of the data in the study and C.H. had final responsibility for the decision to submit for publication.
STUDY FUNDING
This study was funded as an independent investigator-initiated grant awarded by Pfizer Pharmaceuticals to Prof. Clive Holmes.
DISCLOSURE
J. Butchart, L. Brook, V. Hopkins, J. Teeling, U. Püntener, D. Culliford, R. Sharples, S. Sharif, B. McFarlane, R. Raybould, R. Thomas, P. Passmore, and V. Perry report no disclosures relevant to the manuscript. C. Holmes reports receiving an independent investigator-initiated grant from Pfizer to fund this study. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Perry VH, Cunningham C, Holmes C. Systemic infections and inflammation affect chronic neurodegeneration. Nat Rev Immunol 2007;7:161–167. [DOI] [PubMed] [Google Scholar]
- 2.Drake C, Boutin H, Jones MS, et al. Brain inflammation is induced by co-morbidities and risk factors for stroke. Brain Behav Immun 2011;25:1113–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cunningham C, Wilcockson DC, Campion S, Lunnon K, Perry VH. Central and systemic endotoxin challenges exacerbate the local inflammatory response and increase neuronal death during chronic neurodegeneration. J Neurosci 2005;25:9275–9284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Holmes C, Cunningham C, Zotova E, et al. Systemic inflammation and disease progression in Alzheimer disease. Neurology 2009;73:768–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holmes C, Cunningham C, Zotova E, Culliford D, Perry VH. Proinflammatory cytokines, sickness behavior, and Alzheimer disease. Neurology 2011;77:212–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tobinick E, Gross H, Weinberger A, Cohen H. TNF-alpha modulation for treatment of Alzheimer's disease: a 6-month pilot study. MedGenMed 2006;8:25. [PMC free article] [PubMed] [Google Scholar]
- 7.Tobinick EL, Gross H. Rapid cognitive improvement in Alzheimer's disease following perispinal etanercept administration. J Neuroinflammation 2008;5:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tobinick EL, Gross H. Rapid improvement in verbal fluency and aphasia following perispinal etanercept in Alzheimer's disease. BMC Neurol 2008;8:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tobinick EL, Chen K, Chen X. Rapid intracerebroventricular delivery of Cu-DOTA-etanercept after peripheral administration demonstrated by PET imaging. BMC Res Notes 2009;2:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Perry VH, Holmes C. Microglial priming in neurodegenerative disease. Nat Rev Neurol 2014;10:217–224. [DOI] [PubMed] [Google Scholar]
- 11.McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology 1984;34:939–944. [DOI] [PubMed] [Google Scholar]
- 12.Lim A, Tsuang D, Kukull W, et al. Clinico-neuropathological correlation of Alzheimer's disease in a community-based series. J Am Geriatr Soc 1999;47:564–569. [DOI] [PubMed] [Google Scholar]
- 13.Holmes C, Cairns N, Lantos P, Mann A. Validity of current clinical criteria for Alzheimer's disease, vascular dementia and dementia with Lewy bodies. Br J Psychiatry 1999;174:45–50. [DOI] [PubMed] [Google Scholar]
- 14.Hachinski VC, Iliff LD, Zilhka E, et al. Cerebral blood flow in dementia. Arch Neurol 1975;32:632–637. [DOI] [PubMed] [Google Scholar]
- 15.Molloy DW, Standish TI. A guide to the standardized Mini-Mental State Examination. Int Psychogeriatr 1997;9(suppl 1):87–94; discussion 143–150. [DOI] [PubMed] [Google Scholar]
- 16.Rosen WG, Mohs RC, Davis KL. A new rating scale for Alzheimer's disease. Am J Psychiatry 1984;141:1356–1364. [DOI] [PubMed] [Google Scholar]
- 17.Bucks RS, Ashworth DL, Wilcock GK, Siegfried K. Assessment of activities of daily living in dementia: development of the Bristol Activities of Daily Living Scale. Age Ageing 1996;25:113–120. [DOI] [PubMed] [Google Scholar]
- 18.Guy W. Clinical Global Impressions (CGI) Scale. In: Rush J; American Psychiatric Association. Task Force for the Handbook of Psychiatric Measures. Handbook of Psychiatric Measures. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 19.Alexopoulos GS, Abrams RC, Young RC, Shamoian CA. Cornell Scale for Depression in Dementia. Biol Psychiatry 1988;23:271–284. [DOI] [PubMed] [Google Scholar]
- 20.Cummings JL. The neuropsychiatric inventory: assessing psychopathology in dementia patients. Neurology 1997;48(5 suppl 6):S10–S16. [DOI] [PubMed] [Google Scholar]
- 21.Birks J. Cholinesterase inhibitors for Alzheimer's disease. Cochrane Database Syst Rev 2006;(1):CD005593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tabet N, Feldman H. Indomethacin for the treatment of Alzheimer's disease patients. Cochrane Database Syst Rev 2002;(2):CD003673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Browne RH. On the use of a pilot sample for sample size determination. Stat Med 1995;14:1933–1940. [DOI] [PubMed] [Google Scholar]
- 24.Sim J, Lewis M. The size of a pilot study for a clinical trial should be calculated in relation to considerations of precision and efficiency. J Clin Epidemiol 2012;65:301–308. [DOI] [PubMed] [Google Scholar]
- 25.Julious SA. Sample size of 12 per group rule of thumb for a pilot study. Pharm Stat 2005;4:287–291. [Google Scholar]
- 26.British Thoracic Society Standards of Care Committee. BTS recommendations for assessing risk and for managing Mycobacterium tuberculosis infection and disease in patients due to start anti-TNF-alpha treatment. Thorax 2005;60:800–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Summary of product characteristics (ENBREL). Available at: http://www.medicines.org.uk/emc/medicine/3343/SPC/Enbrel+25+mg+powder+and+solvent+for+solution+for+injection/. Accessed January 29, 2015.
- 28.McGuinness B, O'Hare J, Craig D, Bullock R, Malouf R, Passmore P. Statins for the treatment of dementia. Cochrane Database Syst Rev 2010;(8):CD007514. [DOI] [PubMed] [Google Scholar]
- 29.Howard R, Phillips P, Johnson T, et al. Determining the minimum clinically important differences for outcomes in the DOMINO trial. Int J Geriatr Psychiatry 2011;26:812–817. [DOI] [PubMed] [Google Scholar]
- 30.Schulz M, Dotzlaw H, Neeck G. Ankylosing spondylitis and rheumatoid arthritis: serum levels of TNF-alpha and its soluble receptors during the course of therapy with etanercept and infliximab. Biomed Res Int 2014;2014:675108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Madhusudan S, Muthuramalingam SR, Braybrooke JP, et al. Study of etanercept, a tumor necrosis factor-alpha inhibitor, in recurrent ovarian cancer. J Clin Oncol 2005;23:5950–5959. [DOI] [PubMed] [Google Scholar]
- 32.Holmes C, Butchart J. Systemic inflammation and Alzheimer's disease. Biochem Soc Trans 2011;39:898–901. [DOI] [PubMed] [Google Scholar]
- 33.Novella S. Enbrel for Stroke and Alzheimer's: Science Based Medicine. 2014. Available at: http://www.sciencebasedmedicine.org/enbrel-for-stroke-and-alzheimers/. Accessed January 29, 2015. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.