Abstract
Background
Many clinicians believe that the results of revision ACL reconstruction compare unfavorably to primary ACL reconstruction. However, few prospective studies have evaluated revision ACL reconstruction using validated patient based metrics. This study was performed to evaluate and compare the results of revision ACL reconstruction and primary ACL reconstruction.
Methods
The MOON consortium is an NIH funded, hypothesis-driven, multi-center prospective cohort study of patients undergoing ACL reconstruction. All patients preoperatively complete a series of validated patient-oriented questionnaires. At scheduled 2-yr follow-up all patients are given the same series of questionnaires to complete. The study evaluated the results of two-year follow-up of revision ACL reconstruction performed in 2001. Parameters evaluated included Marx activity level, KOOS and IKDC scores.
Results
446 subjects met inclusion criteria; 2-year follow-up was obtained on 393 (88%). The cohort is 55% male, median age 22 yrs. There were 33 revision ACL reconstruction cases, for which follow-up was available for 29 (88%). Median baseline Marx (interquartile range) was 12 (8-16) and 12 (6-16) for the primary ACL reconstruction and revision ACL reconstruction groups respectively (p=0.81). At 2 yrs, median Marx was 9 (4-13) and 5 (0-10) for the primary ACL reconstruction and revision ACL reconstruction groups respectively (p=0.03). Median 2 year IKDC was 75.9 (revision) vs. 83.9 (primary) (p=0.003). Median KOOS subscale Knee Related Quality of Life (KRQOL) at 2 years was 62.5 (revision) vs. 75 (primary) (p<0.001), subscale Sports and Recreation was 75 (revision) and 85 (primary) (p=0.005), subscale Pain was 83.3 (revision) and 91.7 (primary) (p = 0.002).
Conclusions
Marx activity score declined at two-year follow-up in revision ACL reconstruction compared to primary ACL reconstruction. IKDC and KRQOL were significantly decreased in revision ACL reconstruction compared to primary ACL reconstruction at 2 year follow-up. Revision ACL reconstruction resulted in a significantly worse outcome as measured by these patient based measures at 2 years.
Keywords: Anterior Cruciate Ligament, Reconstruction, Outcomes
Introduction
Anterior cruciate ligament (ACL) reconstruction continues to be a commonly performed procedure.1-3 More than 200,000 ACL injuries are estimated to occur annually in the United States and more than 175,000 ACL reconstructions are performed each year.4,5 The initial cost of ACL reconstructions in the United States exceeds two billion dollars, and there is evidence that the number of these procedures is increasing.5,6 The past 20 years has resulted in significant advances in the surgical reconstruction of the ACL. With these advances has come increased expectations of outcome and currently many surgeons will describe a surgical reconstruction with a greater than 90% success rate.7 With these improved results has come the belief by patients that should problems develop a revision reconstruction can be performed with similar results to primary reconstructions. While high levels of evidence may be lacking it does not appear that any series of ACL revision reconstruction has met or exceeded the results of a series of primary reconstructions.8-10
The Multi-center Orthopedic Outcomes Network (Moon) has established a prospective longitudinal cohort to evaluate the results of ACL reconstruction including primary and revision patients. This allows us to compare and contrast the results of revision versus primary reconstruction in a series of patients collected during the same time frame by the same set of surgeons utilizing the same validated patient based outcome measures. Our hypothesis is that revision ACL reconstruction results in worse outcome as measured by patient based outcome measures specifically the Marx activity level, Knee Injury and Osteoarthritis Outcome Score (KOOS) subscales and International Knee Documentation Committee Subjective form (IKDC).
Methods
The MOON (Multicenter Orthopaedic Outcomes Network) consortium is an NIH-funded, hypothesis-driven, multi-center prospective cohort study of patients undergoing ACL reconstruction. Members of the MOON consortium began enrolling ACL reconstruction patients in a prospective protocol following Investigational Review Board approval was obtained from each of six sites (Washington University in St Louis, Vanderbilt University Sports Medicine, Cleveland Clinic Foundation, Ohio State University, University of Iowa, and Hospital for Special Surgery) by eight physicians (RWW, KPS, CK, ECM, AA, RDP, JTA, RGM).
A prospective longitudinal cohort design was established to determine the demographics, associated injuries and outcome of revision ACL reconstruction. Patients preoperatively completed a questionnaire documenting demographics, injury mechanism, patient-based outcome measures, history of previous knee surgery and activity level. The attending surgeon completed a form documenting examination under anesthesia (EUA) and status and treatment of meniscal and articular cartilage injuries. Previous studies have demonstrated the group’s inter-relater agreement on meniscal and chondral pathology.11,12 The details of ACL reconstruction and rehabilitation milestones are recorded as previously described.13,14 A variety of reconstructive grafts was used among the participating surgeons. These included ipsilateral and contralateral autografts, and Achilles, patellar tendon, and soft tissue allografts. More detailed description of the surgeon documentation is detailed in previous studies.13,14
At two-year follow-up to patients are contacted and once again fill out the questionnaire and report any additional injuries and surgeries. Patient based outcome measures obtained by the questionnaire include the Knee Injury and Osteoarthritis Outcome Score (KOOS), International Knee Documentation Committee Subjective form (IKDC), and the Marx activity level score.
Results
Between January 1, 2002 and December 31, 2002, 446 patients met inclusion criteria for this study having had a unilateral primary or revision ACL reconstruction. Two-year follow-up was obtained on 393 (88%). After excluding those that had additional collateral ligament surgery (n=29), there were 364 subjects included in the analyses. Additional treatment of chondral and meniscal lesions was not excluded. The overall cohort is 55% male, median age 22 years. Thirty-eight revision ACL reconstructions were enrolled in the Moon prospective longitudinal cohort. At the time of enrollment, median age for these 38 patients was 26 (range, 16 to 49). There were 27 males and 11 females. Of the 38 revision cases, five were excluded due to concomitant collateral ligament surgery, leaving 33 revision ACL reconstruction patients meeting the inclusion criteria, and of these 29 (88%) were available for two-year follow-up. Twenty males and nine females participated in two-year follow-up.
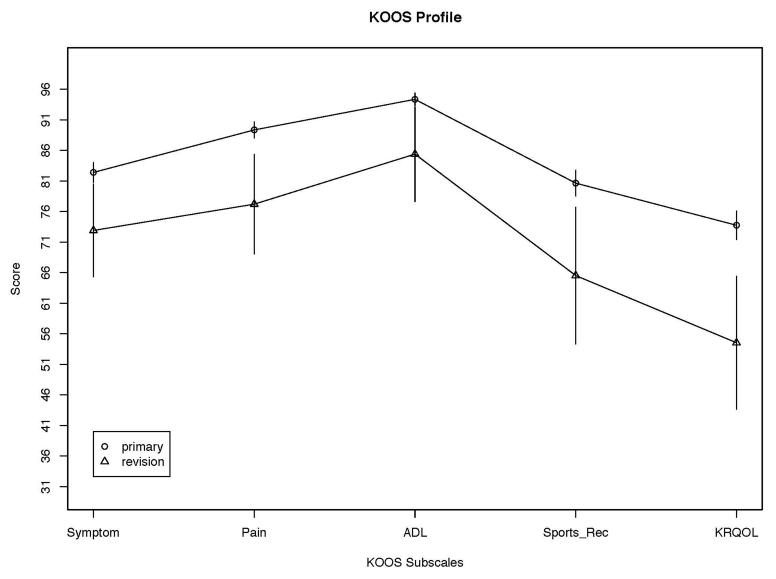
Median baseline Marx (interquartile range) was 12 (8-16) and 12 (6-16) for the primary ACL reconstruction and revision ACL reconstruction groups respectively (p=0.81). (Table 1) At 2 yrs, median Marx was 9 (4-13) and 5 (0-10) for the primary ACL reconstruction and revision ACL reconstruction groups respectively (p=0.03). Median 2 year IKDC was 75.9 (revision) vs. 83.9 (primary) (p=0.003). Median KOOS subscale Knee Related Quality of Life (KRQOL) at 2 years was 62.5 (revision) vs. 75 (primary) (p<0.001). (Figure 1) Median two-year KOOS subscale Sports and Recreation was 75 (revision) and 85 (primary) (p=0.005). Median two-year KOOS subscale Pain was 83.3 (revision) and 91.7 (primary) (p = 0.002). Median two-year KOOS subscale Symptoms was 78.6 (revision) and 85.7 (primary) (p = 0.008). Median two-year KOOS subscale ADLs 97.1 (revision) and 98.5 (primary) (p = 0.073).
Table 1.
Outcomes stratified by Reconstruction Type
| N | primary N = 335 |
revision N = 29 |
Test Statistic | |
|---|---|---|---|---|
| Marx Activity Score | ||||
| Baseline Marx | 357 | 8.0 12.0 16.0 (11.2± 5.2) | 6.0 12.0 16.0 (10.4± 6.3) | F1,355 = 0.06, P = 0.805 |
| Marx at 2y | 364 | 4.0 9.0 13.0 ( 8.7± 5.5) | 0.0 5.0 10.0 ( 6.3± 6.0) | F1,362 = 4.72, P = 0.03 |
|
| ||||
| IKDC | ||||
| Baseline IKDC score | 359 | 40.2 52.9 65.5 (53.0±17.0) | 31.0 56.3 65.5 (52.7±20.8) | F1,357 = 0.02, P = 0.887 |
| IKDC score at 2y | 358 | 75.9 83.9 92.0 (81.5±14.7) | 54.0 75.9 86.2 (67.9±23.8) | F1,356 = 9.05, P = 0.003 |
|
| ||||
| KOOS KRQoL | ||||
| Baseline KOOS KRQoL | 364 | 18.8 37.5 50.0 (37.0±20.2) | 18.8 37.5 43.8 (36.6±23.8) | F1,362 = 0.18, P = 0.672 |
| KOOS KRQoL at 2y | 364 | 62.5 75.0 87.5 (73.8±21.8) | 37.5 62.5 75.0 (54.5±28.6) | F1,362 = 14.45, P<0.001 |
|
| ||||
| KOOS SptRec | ||||
| Baseline KOOS SptsRec | 350 | 25.0 50.0 75.0 (50.1±29.4) | 25 0 65.0 90.0 (57.9±34.0) | F1,348 = 1.94, P = 0.164 |
| KOOS SptsRec at 2y | 364 | 70.0 85.0 95.0 (80.6±19.7) | 50.0 75.0 85.0 (65.5±29.4) | F1,362 = 8.13, P = 0.005 |
|
| ||||
| KOOS Symptoms | ||||
| Baseline KOOS Symptoms | 362 | 571 67.9 82.1 (68.8±17.8) | 46.4 60.7 82.1 (64.2±22.5) | F1,360 = 1.1, P = 0.294 |
| KOOS Symptoms at 2y | 364 | 75.0 85.7 92.9 (82.4±15.3) | 60.7 78.6 85.7 (72.9±20.0) | F1,362 = 7.19, P = 0.008 |
|
| ||||
| KOOS ADL | ||||
| Baseline KOOS ADL | 359 | 73.9 88.2 95.6 ( 83.5±16.0) | 66.2 92.6 98.5 (81.8±20.3) | F1,357 = 0.08, P = 0.772 |
| KOOS ADL at 2y | 364 | 93.4 98.5 100.0 ( 94.4± 9.5) | 75.0 97.1 100.0 ( 85.4± 20.4) | F1,362 = 3.23, P = 0.073 |
|
| ||||
| KOOS Pain | ||||
| Baseline KOOS Pain | 363 | 61.1 77.8 88.9 (74.8±16.9) | 61.1 80.6 91.7 (73.4±22.5) | F1,361 = 0.02, P = 0.887 |
| KOOS Pain at 2y | 364 | 83.3 91.7 97.2 (89.4±12.3) | 66.7 83.3 94.4 (77.2±21.5) | F1,362 = 9.75, P = 0.002 |
a b c represent the lower quartile a, the median b, and the upper quartile c for continuous variables, x ± s represents X̄ ± 1 SD.
N is the number of non-missing values.
Test used:
Wilcoxon test
Figure 1.
KOOS Profile
Discussion
Our results demonstrate that revision ACL reconstruction results in a worse outcome than primary ACL reconstruction as measured by validated patient-based outcome measures. The differences demonstrated were both statistically and clinically significant. This occurred in a prospective longitudinal cohort performed by the same surgeons during the same time period utilizing the same measurement tools (Marx activity level, KOOS, and IKDC).
The Marx activity scale is a validated, quickly administered activity measure to use in addition to joint specific outcome measures and general health outcome measures.15 The Marx activity level was developed to assess functional activity rather than sport activity and to quantify the frequency of the activity. It consists of only four questions. The patient’s peak activity level over the past year is measured by these four questions assessing running, cutting, decelerating and pivoting. Items are scored from zero to four depending upon frequency performed from less than one time per month (0 points) to four or more times per week (four points). Thus, scores range from zero to 16. It has undergone validation testing in its development.15 At two-year follow-up median Marx activity level scores were 9 for primary reconstructions versus 5 for revision reconstructions. Unfortunately, additional studies have not been performed utilizing the Marx to determine a minimal clinically important difference in scores and thus we cannot unequivocally state that a difference of three points on the Marx activity level score represents a clinically significant difference. We speculate that a change in score of two points (more than a 10% of total possible score) is likely a clinically significant difference. The present study found a statistically significant difference between primary (Marx 9) and revision reconstructions (Marx 5) p= 0.03 at two year follow-up. in our study (p=0.009) a difference of 4 points represents a 33% change of a total score of 16, and while it probably represents a clinically significant difference further research is necessary.
Our study utilized the IKDC subjective form. The International Knee Documentation Committee (IKDC) was established in 1987 and developed a standardized outcome measure evaluating knee injuries and treatment first published in 1993. The Board of the American Orthopaedic Society for Sports Medicine (AOSSM) moved in 1997 to revise the form.16 The new subjective form consists of 18 questions. The raw scores are transformed to a zero to 100 scale.16 This new form has been validated for a variety of knee conditions including ligament and meniscus injuries.17,18 The minimal clinically important difference in scores has been determined and a change in score of 11.5 points on the 100 point scale represents a significant change.18 It can be used for a variety of ages and gender.19 Our revision median score was 75.9 vs. primary median score of 83.9. This represented a statistically different result but not clinically significant difference of IKDC scores.
The Knee Injury and Osteoarthritis Outcome Score (KOOS) was developed by Eva Roos as the first sport specific patient based outcome measure. Its goal was to assess outcome in the young and middle-aged athlete and included the WOMAC to assess osteoarthritis.20,21 The KOOS evaluates five dimensions measured separately: pain (nine items), symptoms (seven items), activities of daily living (17 items), sport and recreation function (five items), and knee related quality of life (four items).20 To assess osteoarthritis in the older individuals the 24 questions of the WOMAC were included.20 Each subscale is summed and transformed to a zero (worst possible) to 100 (best possible) score. Previous studies have determined that a change in score or difference in score of 8 points or greater represents a minimal clinically important difference.21
The KOOS has been used for the assessment of a variety of knee conditions including ACL reconstructions.22-26 The pain, sport and recreation and knee related quality of life subscales have been determined to be the most sensitive to a change in the condition of the knee. In our study knee related quality of life (KRQOL) demonstrated a difference of 12.5 points between revision and primary ACL reconstructions. Thus, this was a statistically and clinically significant worse outcome for revisions on the most sensitive KOOS subscale. The sports and recreation subscale difference was 10 points and represented a clinically significant difference and was statistically different between the two groups. The pain subscale difference was 8.4 points and probably represented a clinically significant difference and was statistically different between the two groups. All other subscales had differences less than 10 points and while statistically significant may not represent clinically significant differences. The Activities of Daily Living Score (ADL) as expected was virtually identical between primary and revision reconstructions [97.1 (revision) and 98.7 (primary)].
Few revision ACL reconstruction studies have utilized validated patient-based outcome measures. In fact, no revision ACL reconstructions study has used Marx activity scores. The IKDC has been infrequently utilized. Our median IKDC score at two-year follow-up was 79.4. Recently Battaglia et al reported 95 revision ACL reconstructions at a mean follow-up of 72.7 months.9 The IKDC subjective scores for the patients they deemed excellent averaged 79.7, 63.1 in the fair group and 56.2 in the poor group. All of their groups on average scored lower than age matched norms. Fox et al in a retrospective case series of ACL revision reconstructions utilizing nonirradiated fresh frozen patellar tendon allograft evaluated outcome using a variety of patient based outcome measures.27 At a minimum of two-year follow-up (avg. 4.8 years) their IKDC mean score was 71. They reported KOOS subscales of pain, symptoms, and ADLs. KRQOL and sports and recreation subscales were not reported. Their mean pain score was 84, similar to our median score of 83.3. The symptoms subscale mean score was 77 compared to our 78.6. The ADL subscale mean for the Fox study was 91 versus 97.1 median score in our study.
Our study had a number of strengths and a few limitations. This represents one of the few studies utilizing prospective data. In addition, the ability to directly compare the results to a similar primary ACL reconstruction cohort collected at the same time by the same surgeons has previously not been available. Our follow-up is short at two years and additional length of follow up will be valuable. Despite a large cohort, less than 10% are revision ACL reconstructions. Thus, our study number is small. This precludes the ability to do multivariable analysis to determine predictors of outcome. Future studies such as those being performed by the Multi-center ACL Revision Study (MARS) group will be necessary to accumulate a cohort large enough to allow this more sophisticated analysis.
In conclusion the Marx activity score declined at two-year follow-up in revision ACL reconstruction compared to primary ACL reconstruction. IKDC and KOOS subscales KRQOL, sports and recreation and pain were significantly decreased in revision ACL reconstruction compared to primary ACL reconstruction at 2 year follow-up. Revision ACL reconstruction resulted in a significantly worse outcome as measured by these patient based measures at 2 years.
Bibliography
- 1.Johnson DL, Warner JJ. Diagnosis for anterior cruciate ligament surgery. Clin Sports Med. 1993;12:671–84. [PubMed] [Google Scholar]
- 2.Roos H, Ornell M, Gardsell P, Lohmander LS, Lindstrand A. Soccer after anterior cruciate ligament injury--an incompatible combination? A national survey of incidence and risk factors and a 7-year follow-up of 310 players. Acta Orthop Scand. 1995;66:107–12. doi: 10.3109/17453679508995501. [DOI] [PubMed] [Google Scholar]
- 3.Saperstein AL, Fetto JF. The anterior cruciate ligament-deficient knee: a diagnostic and therapeutic algorithm. Orthop Rev. 1992;21:1297–305. [PubMed] [Google Scholar]
- 4.Gottlob CA, Baker CL., Jr. Anterior cruciate ligament reconstruction: socioeconomic issues and cost effectiveness. Am J Orthop (Belle Mead NJ) 2000;29:472–6. [PubMed] [Google Scholar]
- 5.Gottlob CA, Baker CL, Jr., Pellissier JM, Colvin L. Cost effectiveness of anterior cruciate ligament reconstruction in young adults. Clin Orthop Relat Res. 1999:272–82. [PubMed] [Google Scholar]
- 6.Dunn WR, Lyman S, Lincoln AE, Amoroso PJ, Wickiewicz T, Marx RG. The effect of anterior cruciate ligament reconstruction on the risk of knee reinjury. Am J Sports Med. 2004;32:1906–14. doi: 10.1177/0363546504265006. [DOI] [PubMed] [Google Scholar]
- 7.Bach BR., Jr. ACL reconstruction: revisited, revised, reviewed. J Knee Surg. 2004;17:125–6. doi: 10.1055/s-0030-1248209. [DOI] [PubMed] [Google Scholar]
- 8.George MS, Dunn WR, Spindler KP. Current concepts review: revision anterior cruciate ligament reconstruction. Am J Sports Med. 2006;34:2026–37. doi: 10.1177/0363546506295026. [DOI] [PubMed] [Google Scholar]
- 9.Battaglia MJ, 2nd, Cordasco FA, Hannafin JA, et al. Results of revision anterior cruciate ligament surgery. Am J Sports Med. 2007;35:2057–66. doi: 10.1177/0363546507307391. [DOI] [PubMed] [Google Scholar]
- 10.Wright RW, Dunn WR, Amendola A, et al. Anterior cruciate ligament revision reconstruction: two-year results from the MOON cohort. J Knee Surg. 2007;20:308–11. doi: 10.1055/s-0030-1248066. [DOI] [PubMed] [Google Scholar]
- 11.Dunn WR, Wolf BR, Amendola A, et al. Multirater agreement of arthroscopic meniscal lesions. Am J Sports Med. 2004;32:1937–40. doi: 10.1177/0363546504264586. [DOI] [PubMed] [Google Scholar]
- 12.Marx RG, Connor J, Lyman S, et al. Multirater agreement of arthroscopic grading of knee articular cartilage. Am J Sports Med. 2005;33:1654–7. doi: 10.1177/0363546505275129. [DOI] [PubMed] [Google Scholar]
- 13.Spindler KP, Warren TA, Callison JC, Jr., Secic M, Fleisch SB, Wright RW. Clinical outcome at a minimum of five years after reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am. 2005;87:1673–9. doi: 10.2106/JBJS.D.01842. [DOI] [PubMed] [Google Scholar]
- 14.Wright RW, Dunn WR, Amendola A, et al. Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: a prospective MOON cohort study. Am J Sports Med. 2007;35:1131–4. doi: 10.1177/0363546507301318. [DOI] [PubMed] [Google Scholar]
- 15.Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29:213–8. doi: 10.1177/03635465010290021601. [DOI] [PubMed] [Google Scholar]
- 16.Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29:600–13. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- 17.Irrgang JJ, Anderson AF. Development and validation of health-related quality of life measures for the knee. Clin Orthop Relat Res. 2002:95–109. doi: 10.1097/00003086-200209000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Irrgang JJ, Anderson AF, Boland AL, et al. Responsiveness of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med. 2006;34:1567–73. doi: 10.1177/0363546506288855. [DOI] [PubMed] [Google Scholar]
- 19.Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ. The International Knee Documentation Committee Subjective Knee Evaluation Form: normative data. Am J Sports Med. 2006;34:128–35. doi: 10.1177/0363546505280214. [DOI] [PubMed] [Google Scholar]
- 20.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)--development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28:88–96. doi: 10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
- 21.Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1:64. doi: 10.1186/1477-7525-1-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roos EM, Roos HP, Ekdahl C, Lohmander LS. Knee injury and Osteoarthritis Outcome Score (KOOS)--validation of a Swedish version. Scand J Med Sci Sports. 1998;8:439–48. doi: 10.1111/j.1600-0838.1998.tb00465.x. [DOI] [PubMed] [Google Scholar]
- 23.Roos EM, Roos HP, Ryd L, Lohmander LS. Substantial disability 3 months after arthroscopic partial meniscectomy: A prospective study of patient-relevant outcomes. Arthroscopy. 2000;16:619–26. doi: 10.1053/jars.2000.4818. [DOI] [PubMed] [Google Scholar]
- 24.Englund M, Roos EM, Lohmander LS. Impact of type of meniscal tear on radiographic and symptomatic knee osteoarthritis: a sixteen-year followup of meniscectomy with matched controls. Arthritis Rheum. 2003;48:2178–87. doi: 10.1002/art.11088. [DOI] [PubMed] [Google Scholar]
- 25.Roos EM, Ostenberg A, Roos H, Ekdahl C, Lohmander LS. Long-term outcome of meniscectomy: symptoms, function, and performance tests in patients with or without radiographic osteoarthritis compared to matched controls. Osteoarthritis Cartilage. 2001;9:316–24. doi: 10.1053/joca.2000.0391. [DOI] [PubMed] [Google Scholar]
- 26.W-Dahl A, Toksvig-Larsen S, Roos EM. A 2-year prospective study of patient-relevant outcomes in patients operated on for knee osteoarthritis with tibial osteotomy. BMC Musculoskelet Disord. 2005;6:18. doi: 10.1186/1471-2474-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fox JA, Pierce M, Bojchuk J, Hayden J, Bush-Joseph CA, Bach BR., Jr. Revision anterior cruciate ligament reconstruction with nonirradiated fresh-frozen patellar tendon allograft. Arthroscopy. 2004;20:787–94. doi: 10.1016/j.arthro.2004.07.019. [DOI] [PubMed] [Google Scholar]