Abstract
Background
Breastfeeding outcomes are often worse after cesarean section compared to vaginal childbirth.
Objectives
This study characterizes mothers’ breastfeeding intentions and their infant feeding experiences after cesarean childbirth.
Methods
Data are from 115 mothers on a postnatal unit in Northeast England during February 2006 to March 2009. Interviews were conducted an average of 1.5 days (range 1–6 days) after the women underwent unscheduled or scheduled cesarean.
Results
Thematic analysis of the data suggested breastfeeding was mostly considered the “right thing to do,” preferable, natural, and “supposedly healthier,” but tiring and painful. Advantages of supplementation involved more satiated infants, feeding ease, and longer sleep bouts. The need for “thinking about yourself” was part of cesarean recovery. Infrequent feeding was concerning but also enabled maternal rest. Other breastfeeding obstacles were maternal mobility limitations, positioning difficulties, and frustration at the need for assistance. Participants were confused about nocturnal infant wakings, leading many to determine that they had insufficient milk. Mothers were surprised that sub-clinically poor infant condition was common following cesarean section. Some breastfeeding difficulty stemmed from “mucus” expulsion that had to occur before the infants could be “interested” in feeding. Women who cited motivations for breastfeeding that included benefit to themselves were more likely to exclusively breastfeed on the postnatal unit after their cesareans than those who reported infant-only motivations.
Conclusions
For the majority of mothers, breastfeeding after a cesarean is affected by interrelated and compounding difficulties. Provision of more relational breastfeeding information may enable families to better anticipate early feeding experiences after cesarean section childbirth.
Keywords: cesarean section, breastfeeding, infant feeding, mothers, postpartum, support
Introduction
The publicized risks of cesarean childbirth do not currently include disruption to the maternal-infant feeding relationship, but breastfeeding outcomes are often lower in this population compared to those who undergo vaginal childbirth (McDonald et al., 2012; Prior et al., 2012; Biro et al., 2011). However, cesarean childbirth is not always associated with poorer breastfeeding outcomes (Bolling et al., 2007; Binns et al., 2006). Breastfeeding is a multi-faceted interaction between mothers, infants, those important to them, and their environment. Only recently have studies approached the topic of breastfeeding after cesarean section from the maternal perspective. Pérez-Ríos et al. (2008) suggest an amalgam of “aggravated health outcomes can compromise the mother’s ability to breastfeed” after cesarean childbirth while also “forcing mothers to concentrate more on their recovery, rather than on their baby’s [sic] nutritional needs” (p. 294).
Understanding and enabling breastfeeding is a public health priority because of the importance of human milk and lactation for health, family satisfaction, and economics (Renfrew et al., 2012). Better knowledge of the processes that contribute to breastfeeding outcomes after cesarean childbirth is needed to improve support for this population. The literature indicates that breastfeeding difficulty after cesarean section compared with vaginal delivery occurs for many reasons: later maternal-infant first contact (Hung and Berg, 2011; Rowe-Murray and Fisher, 2001); maternal postpartum emotional distress (Beck et al., 2011; Carlander et al., 2010); lower infant neurobehavior scores (Sakalidis et al., 2013); later breastfeeding initiation (Boccolini et al., 2011; Awi and Alikor, 2006); less maternal oxytocin and prolactin in response to suckling (Nissen et al., 1996); maternal physical pain (Karlström et al., 2007), less volume of milk transferred over the first few days (Evans et al., 2003); and delayed onset of lactogenesis II (Zhu et al., 2012; Dewey et al., 2003). Infant feeding cues can also be suppressed after cesarean childbirth due to lack of labor hormones (Jain and Eaton, 2006) and the influence of surgical anesthesia plus postpartum medications (Howie and McMullen, 2006).
Various researchers (Nolan and Lawrence, 2009; Rowe-Murray and Fisher, 2001) have called for a study of the relational impacts of cesarean section on infant feeding. Breastfeeding obstacles are often studied in relative isolation from one other, limiting the ability to appreciate how the experience of cesarean section delivery impacts infant and maternal capabilities. Objective: The purpose of this study was to explore maternal perspectives of mechanisms that contribute to early breastfeeding difficulty after cesarean childbirth as the experiences were unfolding.
Methods
Semi-structured, open-ended interviews were conducted with women who experienced cesarean childbirth (N=115).
Setting
The study setting was the postnatal unit of a tertiary-level National Health Service (NHS) hospital in Northeast England, which hosted approximately 5,400 births per year and was not Baby Friendly accredited. The cesarean section rate was 22%. This figure was consistent with childbirth in England (23% cesarean) at that time (Bolling et al., 2007).
Continuous rooming-in is standard on the postpartum unit for all healthy dyads at the study hospital. Infant feeding support was provided by midwives as a part of routine care. Mothers signaled for midwifery assistance by pushing a call button. Overnight visitors were prohibited, including women’s partners. There were two data collection periods. There was no change in the hospital breastfeeding policy or with provision of care across these times.
Participants
Study 1 was conducted from February to April 2006 and comprised participants who underwent either an unscheduled (n=48) or scheduled (n=27) cesarean section delivery. Study 2 was conducted from January to March 2009 and involved women who experienced scheduled, non-labor cesarean (n=40) as part of a randomized controlled trial that tested the effects of different types of postnatal unit bassinets on maternal-infant interactions (Authors, 2012). The interview schedule relevant to this analysis was identical in both research studies.
Procedures
Prior to commencing research, approval was obtained from the authors’ university, local healthcare authorities, and the NHS ethical review board. Inclusion criteria for both studies specified that mothers be at least 18 years of age at the time of enrollment, in good health, fluent in verbal and written English, and have experienced a cesarean. Informed consent was obtained from participants for both studies. Enrolled participants were allocated numerical codes to protect anonymity.
The first author, who was not hospital staff, conducted the face-to-face interviews with mothers. Interviews were completed on the postpartum ward between the day following delivery and discharge while no medical professionals were present. The average time of interview was 1.5 days after childbirth, with a range of study participation 1–6 days postpartum. Women’s partners were permitted to attend the interview, and their spontaneously offered comments were noted separately from participant responses.
Interview questions were worded in a non-leading manner to solicit participant experiences and understandings. Although the principal interest of the study pertained to breastfeeding following cesarean section, this was purposefully not framed as an explicit focus. When participants occasionally asked if a specific question was directed at the impact of their cesarean, the investigator (First Author) replied that the research was about any factors the participant felt were important. Probes were used to elicit full accounts, and the interviewer wrote down participant responses to each question verbatim during the approximately thirty-minute interviews. A small gratuity was provided to participants in the form of gift cards.
Recruitment and interview responses
Seventy-five participants provided interview data in Study 1 and 40 participants provided interview data in Study 2. In Study 1, 101 women were approached on the postnatal ward; 15 declined participation, 5 expressed interest in participating but did not meet inclusion criteria, 5 were not enrolled due to timing conflicts, and 1 woman was withdrawn because she became unwell during the interview. Study 2 participants were recruited as part of the authors’ trial (2012); the main outcome of that study was behavioral observations collected through nocturnal filming on the postnatal unit. In Study 2, 77 of 134 (58%) eligible women approached face-to-face were enrolled into the study, along with 9 of 23 women (39%) who were approached via postal recruitment (Authors, 2012). The overall enrollment rate to those eligible was 86/157 = 55%.
The sample for this analysis is presented in Figure 1. Data from 115 women was utilized for the question about the factors that the decision of what to feed their infants.
Figure 1.
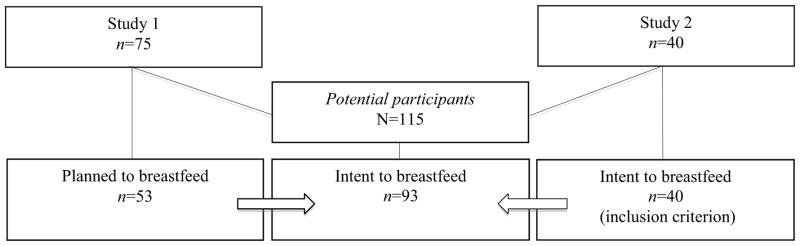
Sample recruitment.
Study questions on breastfeeding factors, descriptions of breastfeeding frequency, description of breastfeeding obstacles, breastfeeding exclusivity, and breastfeeding commitment are subsets of the 93 women who intended to breastfeed. The categories are illustrated by sample size in Table 1.
Table 1.
Interview responses on breastfeeding factors and experiences.
| Intent to breastfeed n=93 mothers | |
|---|---|
|
| |
| n | |
| Breastfeeding factors | 91 |
| - Breastfeeding benefit reported as being infant only factors | 45 |
| - Breastfeeding benefit reported as including maternal factors | 46 |
|
| |
| Postnatal unit breastfeeding frequency | 42 |
|
| |
| Hospital breastfeeding experiences | 85 |
|
| |
| Planned exclusive breastfeeding | 86 |
|
| |
| Breastfeeding commitment | 86 |
| - Breastfeeding outcome among those who reported infant only benefit | 40 |
| - Breastfeeding outcome among those who reported maternal benefit | 46 |
Analyses
Qualitative: Participant responses were read in their entirety to appreciate the mother’s story as a whole (Tesch, 1990). Data were then entered into a matrix format in response to the interview questions for ease of comparison. Responses were then coded to create thematic categories across all participants (Miles and Huberman, 1994; Wilkinson, 2004), which the authors identified and verified through an iterative process (Patton, 2002). Quantitative: Between group differences on maternal report of breastfeeding frequency and on breastfeeding commitment were tested using Fisher’s Exact tests. Statistical significance was determined at the p≤.05 level.
Participant demographics
Participants were mostly White, predominately first time mothers (range 0–6 previous deliveries), and aged between 18 to 41 years. Their infants were predominately healthy singletons and about half of them were female. Sample characteristics are reported in Table 2.
Table 2.
Participant demographics.
| Phase 1 N=75 mothers |
Phase 2 N=40 mothers |
|||
|---|---|---|---|---|
|
| ||||
| Median | Range | Median | Range | |
| Parity | 0 | 0–3 | 0 | 0–6 |
| Age in years | 29 | 18–41 | 34 | 23–41 |
| Education completed | Attended university | no GCSEs to Doctorate | University degree | no GCSEs to Doctorate |
| Gestational age in weeks + days | 39+3 | 30+3 – 42+6 | 39+1 | 37+4 – 41+1 |
| Apgar score at 5 minutes | 9 | 3–10 | 9 | 9–10 |
|
| ||||
| n | % | n | % | |
|
| ||||
| Previously had a cesarean section | 22 | 29.3 | 22 | 55.0 |
| Living with partner | 64 | 85.3 | 39 | 97.5 |
| Mother White European | 64 | 85.3 | 34 | 85.0 |
| Singleton | 68 | 90.7 | 40 | 100 |
| Infant female | 42 | 56.0 | 26 | 65.0 |
GCSE stands for General Certificate of Secondary Education. These exams are taken in the UK at the age of 16 years at the end of their compulsory high school education.
Findings
Infant feeding intentions and breastfeeding factors
About 71% of Study 1 participants (53 of 75) reported that they had intended to breastfeed. Most of these women planned to initially breastfeed exclusively. Intent to breastfeed was an inclusion criterion for Study 2 (40 of 40) (see Figure 1). In response to the postnatal interview question “what factors influenced this decision” some of the same variables were provided both for and against breastfeeding plans. Figure 2 illustrates the categories derived from the responses, such as maternal convenience. Breastfeeding intent was dominated by the ‘breast is best’ mantra of broad infant health benefits. Some participants spontaneously provided a more precise rationale reporting the advantages of breastfeeding were due to the composition of human milk and its protective effects on various infant outcomes. The mothers who also cited breastfeeding self-benefits reported a range of advantages including closeness with their infants, convenience, breastfeeding being ‘natural,’ breastfeeding as an emotionally rewarding experience, fulfilling expectations of family/friends, and cost effectiveness. No mother said she planned to breastfeed without mentioning infant benefit. Infant benefit without reference to maternal benefit was described by 49% (45 of 91) while the other half of participants, 51% (46 of 91), offered reasons that included benefits to themselves and the infant.
Figure 2.
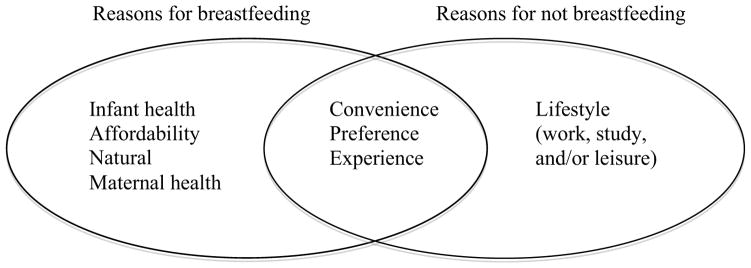
Maternally reported factors that influenced their prenatal feeding intentions.
The few women who discussed prenatal intent to supplement their milk with formula from birth (5 of 115) explained that the combination feeding strategy was intended to a) satiate their infants in the early postpartum period before their milk ‘came in,’ b) grant themselves more independence while providing some health benefits for their infants, or c) better enable to them to cope with the demands of breastfeeding. Multipara who had not previously breastfed but planned to do so during their latest pregnancy explained they felt that they had either not had the opportunity to breastfeed before, or they cited infant health as the reason for their changed approach to infant feeding. Few women said that they felt pressure to breastfeed, most perceived others as supportive, and all but one knew someone who had breastfed. Many were aware breastfeeding was encouraged, but felt that a mother needs to choose what is right in her circumstances. Maternal tiredness was specifically mentioned as a reason that family members did not support breastfeeding plans.
Maternal descriptions of breastfeeding frequency
In response to “how often have you been [breast]feeding, including during the nighttime,” women recounted their sessions in their own words. The participant descriptions were coded into categories reflecting infrequent, variable, or frequent breastfeeding. For example:
Infrequent: “In recovery, I tried about 3 times. Then did twice or so today…can’t do it.”
Variable: “Only fed twice on the first day…probably helped me actually. On the second day, I fed 4 or 5 times. Today it’s like don’t leave me mommy.”
Frequent: “Very [frequently]. I can’t count it.”
Overall, few participants (17%, 7 of 42) reported breastfeeding infrequently. The reported infrequent breastfeeding was associated with mothers who provided ‘infant-only’ reasons for breastfeeding intent (7 of 22) compared to the women who also cited self-advantages (0 of 20), p=.0092 (Fisher’s Exact test).
Maternal description of breastfeeding obstacles
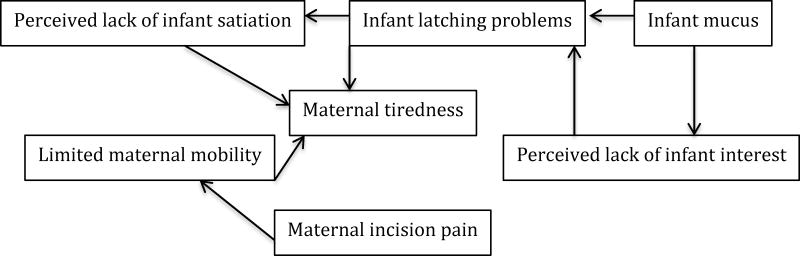
In response to “how has the [breast]feeding been going,” the majority of participants (71.8%, 61 of 85) reported at least one hindrance with breastfeeding during their postnatal hospital stay. Maternal obstacles were discussed by about half of the participants and slightly more reported at least one infant problem. The main breastfeeding problems were limited maternal mobility, maternal incision pain, maternal tiredness, infant mucus, perceived lack of infant interest, infant latching difficulty, and perceived lack of infant satiation. The interrelation of the thematic categories are presented in Figure 3.
Figure 3.
Maternally reported postnatal unit breastfeeding difficulties.
Participant discussions of breastfeeding difficulty revealed that obstacles were intertwined:
“The first night she [the newborn] was mucusy. She is having to bring all of that up first, so isn’t interested in feeding. She had to vomit up the mucus. I have to persevere even though I’m tired and want to sleep. At first, breastfeeding was awkward and clumsy. She [the baby] is getting the hang of it now…we’re working together more.”
“I was told because of not going into labor my milk didn’t start. If I hadn’t heard that I just would’ve thought it would be automatic. Because of that thought I’m probably not going to be able to [breastfeed]. I don’t want to try anymore…feel stressed and the baby has mucus. I’m disappointed that I couldn’t [breastfeed].”
Night-time was specifically mentioned as being more difficult for breastfeeding due to the absence of visitors to assist with infant care combined with mothers’ compromised mobility:
“I think that I had forgotten how debilitating it is [after a cesarean section] in the first 24 hours. I expected to be on my feet sooner…just remember things differently. Obviously, you’re not yourself for a few weeks. You forget how long it takes to get better. Just forget it’s major surgery. I will get help tonight with looking after them [twin newborns], ‘cause I can’t get up…felt bit let down by that [limited mobility]. Having to buzz [for midwifery assistance] is disappointing. You feel a bit helpless after cesarean. It’s night when you mainly need the help. Breastfeeding is quite tiring.”
“There’s no doubt that you need to think about yourself…you need to get enough sleep.”
The newborns’ physical condition was spontaneously mentioned as inhibiting breastfeeding. Mothers recounted that the midwives informed them only after delivery that newborns’ regurgitating ‘mucus’ was normal after cesarean:
“Her [the newborn’s] tummy feels full so she vomits a lot. Babies born by cesarean have mucus in them…she’s gradually expelling that.”
“She’s recovering from the cesarean section…is mucusy, sickly. It’s not giving her opportunities [to breastfeed] as much. She’s not taking any.”
The physiological mechanism for infants being unwell was understood differently among participants. They described poor infant condition as occurring due to the baby swallowing mucus and blood while in utero or when being delivered or not having the ‘mucus’ expelled via labor compressions.
Post-operative maternal pain and/or limited mobility were salient features of women’s breastfeeding experiences. Impeded access to infants due to maternal discomfort interrupted breastfeeding. For example, a mother said “the pain is restrictive” and it was hard to breastfeed because she could not easily maneuver herself. Another aspect was difficulty with the process of picking an infant up after cesarean childbirth because of the maternal incision wound. Some mothers “felt a bit useless” because breastfeeding was “very painful and very frustrating,” which is why they described only being able to “stand it for so long.” Maternal language was of relentless pain that caused “absolute agony.” One participant said that she felt like she was going to “rip open” and that her pain was not something you can “forget” or “switch off.”
Breastfeeding exclusivity
Among participants who reported prenatal intent to breastfeed, 73.3% (63 of 86) were exclusively doing so on the postnatal unit. Unplanned formula supplementation was described as easing the maternal ‘burden’ of breastfeeding. For experienced mothers, combination feeding of human and artificial milk “worked last time” which they would rather do than have the newborns “crying all night.” Some mothers used formula in an effort to settle their infants so that they could obtain more rest.
Breastfeeding commitment
Most of the breastfeeding women planned to continue providing their milk after hospital discharge (84.9%, 73 of 86). Mothers who reported motivations for breastfeeding that included benefits to themselves were significantly more likely to plan to breastfeed post-discharge compared to those who reported reasons for breastfeeding that referenced their infants only. Termination of breastfeeding in the hospital was reported by 11 of 40 ‘infant-only’ breastfeeding mothers versus 2 of 46 ‘included maternal’ breastfeeding mothers, p=.005 (Fisher’s exact test).
Discussion
This study documented maternal accounts of their breastfeeding intent and breastfeeding experiences following cesarean births. The findings extend knowledge on the challenges faced by the substantial population of mother-infant dyads who undergo cesarean section. Karlström et al. (2013) found that mothers encountered more breastfeeding complications after cesarean section compared to vaginal childbirth but the study did not detail the types of obstacles. Insight into mothers’ lived experiences are required for evidence-based breastfeeding support and ‘woman-centered’ care (Carolan, 2006).
In this study, maternal convenience, preference, and previous experience with feeding infants were offered by as reasons for breastfeeding by some women and by as reasons for formula feeding by others. This finding supports variation in what Lööf-Johanson et al. (2013) describe as the “life value” of breastfeeding. Infant feeding substance is part of mother-infant biopsychosocial relationships and, as such, may include both harmony and conflict with other meaningful aspects of life. We also found that infant health was the most commonly cited reason for breastfeeding, which was consistent with the breast as ‘best’ for baby finding by Burns et al. (2010). The distanced expressions of human milk advantages described by our participants could indicate that the women did not fully appreciate the differences between their milk and formula for infant health and development. About half of the women in this study also reported a range of self-benefits in their breastfeeding plans. The multiple factors for prenatal breastfeeding intent and the primary concentration on infant health were mirrored in English mothers as a whole during the study period (Bolling et al., 2007). Breastfeeding promotion may be more effective by not only emphasizing the range of maternal outcomes influenced by breastfeeding, but by also providing a concise explanation of the mechanisms by which human milk and lactation affect dyads’ health. Previous research found that women who express greater knowledge of breastfeeding benefits are more likely to intend, initiate, and sustain breastfeeding than others (Kornides and Kitsantas, 2013; Stuebe and Bonuck, 2011).
The women who had antenatal breastfeeding intentions but formula fed from birth described a low level of commitment combined with maternal tiredness. Fatigue and breastfeeding difficulties are both common physical problems reported by women in the early postpartum period (Rowlands and Reshaw, 2012). Mothers in this study said that their family members expressed concern that excess tiredness would occur as a consequence of breastfeeding. This expectation of burden may undermine what Avery et al. (2009) describe as the “confident commitment” needed for achieving breastfeeding goals. These researchers defined the theme of maternal process-efficacy in breastfeeding as understanding the physiological process of lactation, developing the breastfeeding relationship with their infants, and making breastfeeding ‘work’ despite obstacles. We found that breastfeeding after cesarean childbirth was hindered for many by maternal emotional stress from the interrelated obstacles of maternal incision pain, limited maternal mobility, latching difficulty, perceived lack of infant satiation, perceived lack of infant interest in breastfeeding, and infant mucus clearance. Furthermore, nighttime was specifically mentioned as being the most difficult for these breastfeeding mothers due to the lack of visitors permitted on the ward, hesitation of the women to summon midwives for assistance, and compounded maternal tiredness. Although most of these and other breastfeeding obstacles can be resolved, many mothers do not receive the postpartum guidance and support necessary to do so (Dewey, 2001). Our findings specifically call into question the policy of prohibiting, or otherwise impeding, the overnight presence of supportive partners or other family members on postpartum units.
Maternal description of infrequent breastfeeding was significantly associated with those who had reported infant-only reasons for their breastfeeding intent. Most of the mothers who reported infrequent breastfeeding were concerned about establishing breastfeeding and some felt “useless,” but this practice was presented as beneficial by some because it was perceived as enabling the women to obtain more sleep. Maternal accounts of relatively infrequent feedings can provide insight into why delayed onset of lactogenesis II and lower likelihood of regaining infant birth weight by the end of the first postpartum week is associated with cesarean childbirth (Dewey et al., 2003; Evans et al., 2003). This analysis is the first, to our knowledge, that investigated mothers’ reasons for their infant feeding plans as ‘infant-only’ or ‘included maternal’ benefit. Our findings on maternally reported breastfeeding frequency and breastfeeding termination prior to hospital discharge suggest that it may be helpful for future research to test whether such associations are replicated. Assessment tools such as the Infant Feedings Intentions Scale (Nommsen-Rivers & Dewey, 2009) could be modified to document whether mothers cite reasons related to themselves for their breastfeeding plans or not. Healthcare providers may benefit from knowing the factors that influence a mother’s plans to breastfeed, as those that do not include self-benefits may need additional support.
Explanation for formula supplementation included satiating infants so that they would sleep more at night. This practice was perceived as reducing the mother’s need to move, which was painful after cesarean section. The Baby Friendly Hospital Initiative states that health care providers should not give infants food or drink other than human milk unless medically indicated (WHO and UNICEF, 2009). The World Health Organization (2006) also recommends that standard postpartum care include babies being within easy reach of their mothers, which [the Authors] (2012) suggest is not achieved by the stand-alone bassinets adjacent to maternal beds that are currently standard in hospitals. We determined that three-sided bassinets that attach to the maternal bedframe provide mothers with easier and safer access to infants. Furthermore, objective assessment of maternal sleep duration, sleep efficiency, and sleep fragmentation does not support the notion that supplementation or exclusive formula feeding promotes maternal sleep compared to exclusive breastfeeding (Montgomery-Downs et al., 2010). To the contrary, formula supplementation has been associated with poorer sleep in mothers compared to exclusively breastfeeding (Doan et al., 2007).
In our study, supplementation of formula on the postnatal unit was explained as providing the health benefits of mothers’ milk while also minimizing the time, frustration, and/or pain involved with infant feeding. Deviation from intended breastfeeding exclusivity did not seem to cause concern among some mothers, possibly due to them feeling it was necessary in their circumstances, but the practice was very upsetting to others. DaMonta et al. (2012) found that most women in their sample felt unprepared for the realities of early postpartum breastfeeding and that formula was often used in response to breastfeeding problems. Doan et al. (2007) caution, however, that medically unnecessary formula supplementation can sabotage the establishment of breastfeeding. Providing information on the health impact of breastfeeding needs to be balanced by adequate support to enable women and their infants to achieve the relationship. To achieve breastfeeding goals, women on postnatal units would benefit from working through infant feeding issues with relatable midwives (Dykes, 2005). Accurate information about the ability of women to lactate after non-labor childbirth is particularly important. In these cases, hospital staff can emphasize and facilitate frequent breastfeeding sessions.
Based on her research of British women’s experiences of breastfeeding in the hospital, Dykes (2006) concludes that the current system of postnatal care renders many families and caregivers unsatisfied. The frustration and guilt that she found among mothers when breastfeeding seemed unachievable were echoed by some of our participants, through their struggle to breastfeed during the night. Dykes (2006) argues that breastfeeding is largely positioned in public health in a manner that compartmentalizes the infant and the breast instead of revolving around the relational and physiological connectedness between the mother and child. Our findings on deviation from breastfeeding exclusivity during hospitalization support the suggestion by Dykes (2006) that exclusive breastfeeding is largely viewed as ideal but its achievement is uncertain because of the quantifiable nature of formula provision and its perceived superiority with infant satiation. If new mothers were aware that many of their peers have similar concerns as to whether their colostrum/milk is adequate and if their infant is behaving ‘normally,’ then individual perception of the need to provide formula may be diminished. This suggestion is supported by Tender et al.’s (2009) finding that mothers who attended a prenatal breastfeeding class were significantly less likely to supplement their breastfed infants while in the hospital compared to those who did not attend a class. Data on whether our participants attended a breastfeeding class were not collected, however antenatal breastfeeding classes were offered within the hospital. The role of antenatal classes on breastfeeding outcomes after cesarean section is an area for future research, as the Baby Friendly Hospital Initiative (BFHI) Step 2 includes the guideline of having a designated health care professional to assess local needs and train all health care staff caring for mothers and infants and the BFHI Step 3 recommends individualized education of breastfeeding management for women (Baby-Friendly USA, 2010).
A focused intervention to support women’s journey of establishing and maintaining breastfeeding would be to rephrase references to breastfeeding ‘on demand’ to ‘as the infant needs’ and ‘as your body needs.’ Replacement of the word ‘demand’ may eliminate notions of control, manipulation, or force and the language of ‘need’ fosters a broader perspective of both infant capability and lactation physiology (Burns et al., 2010). In England during the study period, breastfeeding mothers were more likely to change to exclusively formula feeding within two weeks of their infant’s birth if they experienced a lack of help or advice with their feeding problems compared with mothers who reported receiving support (Bolling et al., 2007). Our participants described formula supplementation as worthwhile to settle infants so that they would not be “crying all night.” Midwives have the opportunity to assist families in recognizing their interconnected breastfeeding obstacles and then mutually construct strategies to balance maternal recovery and exclusive breastfeeding.
Many women in our study were upset about being informed postnatally by midwives that (sub-clinically) poor infant condition was common after non-labor cesarean section. The physiological mechanisms for this were unclear to the mothers, indicating a need for consistent prenatal and postnatal explanation of the consequences to infants of non-labor birth. Conditions that have been considered sub-clinical are increasingly identified as impacting child health (Aryeetry et al., 2008; Wayse et al., 2004). Recognition that the hormonal milieu and physical stress of labor facilitate the fetal transition to extrauterine life (Sinha et al., 2011; Ramachadrappa and Jain, 2008; Jain and Eaton, 2006) may assist families in understanding post-cesarean morbidity, such as respiratory issues, and how these may impact on breastfeeding. Churchill et al. (2006) asked obstetricians to list the risks of cesarean section delivery that they routinely mention to women. Breastfeeding difficulty was not mentioned by any of the doctors in their sample. The United Kingdom National Institute for Clinical Health and Excellence guidance (2012) also does not include the possible impact on breastfeeding in the risk factors for cesarean section delivery, despite suggesting in the main text of the policy document that women who have a cesarean section “should be offered additional support to help them to start breastfeeding” (p. 24).
Most participants reported that they would to continue breastfeeding after hospital discharge, although the majority expressed plans that depended on infant weight gain, satiation, producing enough milk and “seeing how it goes.” These reasons mirrored the most common factors reported by mothers in England for stopping breastfeeding with the first week postpartum: baby not feeding properly, having insufficient milk and painful breast (Bolling et al., 2007). The contingent nature of our participants’ plans may reflect women’s concerns about the adequacy of their milk, the ability to lactate, and negotiation of the breastfeeding process. Mothers’ responses suggest that some of the women were confused and upset by their lack of understanding of both infant satiation and sleep behavior following cesarean section birth. Breastfeeding influences compounded one another, leading to network of support or a cycle of difficulty.
O’Brien et al. (2009) present a ‘tool-box’ of coping strategies that women employed to support their breastfeeding. Results from their two interview studies in Australia were themes of: increasing breastfeeding knowledge; staying relaxed and ‘looking after yourself; the use of positive self-talk; challenging unhelpful beliefs; and problem solving. Similar themes of ‘looking after me’ and ‘managing the load’ were found by Taylor and Johnson (2010) as how women coped with postpartum fatigue. These researchers found that postpartum women most commonly used self-care strategies of sleeping/conserving energy instead of getting assistance or lowering their infant care expectations. In our study, ‘looking after oneself’ was justification for formula supplementation so that the mothers could try to get more sleep. Recent research in the UK found that most of the women who breastfed exclusively for the recommended 6 months described overcoming a variety of issues, including doubt about the effect of human milk on the development of infant sleep patterns (Brown and Lee, 2011). Participants in our study who encountered seemingly unassailable breastfeeding obstacles described the change as being best for both the infant (satiation) and themselves (recovery).
Limitations
The results of this study may not be generalizable to women who give birth in Baby Friendly accredited hospitals, in which hospital staff are trained to support breastfeeding through the 10 Steps to Breastfeeding Success (WHO and UNICEF, 2009). Women in other countries may experience unique breastfeeding challenges. However, the themes we documented are likely to be salient for many dyads after cesarean section childbirth. This study did not include women who had vaginal childbirth, so the findings are not a comparison of the influences of cesarean section on breastfeeding compared to the various types of vaginal birth. Declercq et al. (2009) suggest that to make informed choices about childbirth mode, families require realistic expectations about labor and postpartum pain. We would add that cesarean section childbirth should be presented in relation to how it may impact maternal-infant interactions, so that families can best prepare themselves for the postnatal experience.
Conclusions
Breastfeeding entails a maternal balance between self and infant care. From mothers’ perspectives, cesarean section childbirth led to physical impediments in accessing infants and the women reported confusion over infant physiological functioning and feeding cues. The findings suggest that maternal perception of whether the breastfeeding conveys benefits to themselves impacts early breastfeeding frequency and plans for breastfeeding after hospital discharge.
The results of this study indicate that maternal perception of ‘normal’ infant behavior, understanding of lactation physiology, perception of breastfeeding advantages, and the coping mechanisms that women adopt to counter early feeding obstacles may be important contributors to the duration of exclusive and any breastfeeding. Tailored prenatal and postnatal discussion of the trade-offs involved with breastfeeding and sleep practices after cesarean section childbirth may benefit families, so that they make informed and satisfying decisions. Deeper levels of understanding of the interconnected processes of childbirth and infant feeding may instigate more practical and effective support from healthcare providers and others who play a central role in breastfeeding processes. As more hospitals become Baby Friendly accredited, mothers may benefit beyond this standard of care by receiving anticipatory guidance and tailored support for the breastfeeding obstacles common to their circumstances.
Acknowledgments
This research was funded by the Parkes Foundation and the Owen F. Aldis Fund. The funding sources approved of the study design, but were not involved in data collection, analysis, writing, or publication. Kristin Tully is currently supported by the National Institute of Child Health and Human Development Training Grant, 5T32HD007376-22.
Footnotes
Conflict of interest statement
The authors declare that they have no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Kristin P. Tully, Center for Developmental Science, Associate, Carolina Global Breastfeeding Institute, University of North Carolina at Chapel Hill.
Helen L. Ball, Department of Anthropology, Fellow, Wolfson Research Institute for Health and Wellbeing, Durham University, Durham, United Kingdom.
References
- Aryeetry RNO, Marqis GS, Timms L, Lartey A, Brakohiapa L. Subclinical mastitis is common among Ghanan women lactating 3 to 4 months postpartum. Journal of Human Lactation. 2008;24:263–267. doi: 10.1177/0890334408316077. [DOI] [PubMed] [Google Scholar]
- Authors. Postnatal unit bassinet types when rooming-in after cesarean birth: implications for breastfeeding and infant safety. Journal of Human Lactation. 2012;28:495–505. doi: 10.1177/0890334412452932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avery A, Zimmerman K, Underwood PW, Magnus JH. Confident commitment is a key factor for sustained breastfeeding. Birth. 2009;36:141–148. doi: 10.1111/j.1523-536X.2009.00312.x. [DOI] [PubMed] [Google Scholar]
- Awi DD, Alikor EA. Barriers to timely initiation of breastfeeding among mothers of healthy full-term babies who deliver at the University of Port Harcourt Teaching Hospital. Nigerian Journal of Clinical Practice. 2006;9:57–64. [PubMed] [Google Scholar]
- Baby-Friendly USA. Guidelines and evaluation criteria for facilities seeking Baby-Friendly designation. Sandwich, MA: Baby-Friendly USA; 2010. [Accessed September 2013]. from http://www.babyfriendlyusa.org/get-started/the-guidelines-evaluation-criteria. [Google Scholar]
- Beck CT, Gable RK, Sakala C, Declercq ER. Posttraumatic stress disorder in new mothers: results from a two-stage U.S. national survey. Birth. 2011;38:216–227. doi: 10.1111/j.1523-536X.2011.00475.x. [DOI] [PubMed] [Google Scholar]
- Binns CW, Gilchrist D, Woods B, Gracey B, Gracey M, Scott J, Smith H, Zhang M, Roberman B. Breastfeeding by Aboriginal mothers in Perth. Nutrition & Dietetics. 2006;63:8–14. [Google Scholar]
- Biro MA, Sutherland GA, Yelland JS, Hardy P, Brown SJ. In-hospital formula supplementation of breastfed babies: a population-based survey. Breastfeeding Medicine. 2011;38:302–310. doi: 10.1111/j.1523-536X.2011.00485.x. [DOI] [PubMed] [Google Scholar]
- Boccolini CS, Carvalho ML, Oliveira MI, Vasconcellos AG. Factor associated with breastfeeding in the first hour of life. Revista de Saúde Pública. 2011;45:69–76. doi: 10.1590/s0034-89102010005000051. [DOI] [PubMed] [Google Scholar]
- Bolling K, Grant C, Hamlyn B, Thornton A. Infant feeding survey 2005. London: The Information Centre; 2007. [Accessed March 2013]. at http://www.ic.nhs.uk/pubs/ifs2005. [Google Scholar]
- Brown A, Lee M. An exploration of the attitudes and experiences of mothers in the United Kingdom who chose to breastfeed exclusively for 6 months postpartum. Breastfeeding Medicine. 2011;6:197–204. doi: 10.1089/bfm.2010.0097. [DOI] [PubMed] [Google Scholar]
- Burns E, Schmied V, Sheehan A, Fenwick J. A meta-ethnographic synthesis of women’s experience of breastfeeding. Maternal & Child Nutrition. 2010;6:201–219. doi: 10.1111/j.1740-8709.2009.00209.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlander AK, Edman G, Christensson K, Andolf E, Wiklund I. Contact between mother, child and partner and attitudes towards breastfeeding in relation to mode of delivery. Sexual & Reproductive Healthcare. 2010;1:27–34. doi: 10.1016/j.srhc.2009.10.001. [DOI] [PubMed] [Google Scholar]
- Carolan M. Women’s stories of birth: a suitable form of research evidence? Women & Birth. 2006;19:65–71. doi: 10.1016/j.wombi.2006.06.003. [DOI] [PubMed] [Google Scholar]
- Churchill H, Savage W, Francome C. Caesarean birth in Britain: a book for health professionals and parents. Middlesex University Press; Middlesex, England: 2006. [Google Scholar]
- DaMota K, Bañuelos J, Goldbronn J, Vera-Beccera LE, Heinig MJ. Maternal request for in-hospital supplementation of healthy breastfed infants among low-income women. Journal of Human Lactation. 2012;28:476–482. doi: 10.1177/0890334412445299. [DOI] [PubMed] [Google Scholar]
- Declercq E, Labbok MH, Sakala C, O’Hara M. Hospital practices and women’s likelihood of fulfilling their intention to exclusively breastfeed. American Journal of Public Health. 2009;99:929–935. doi: 10.2105/AJPH.2008.135236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewey KG. Maternal and fetal stress are associated with impaired lactogenesis in humans. Journal of Nutrition. 2001;131:3012S–2015S. doi: 10.1093/jn/131.11.3012S. [DOI] [PubMed] [Google Scholar]
- Dewey KG, Nommsen-Rivers LA, Heinig J, Cohen RJ. Risk factors for suboptimal infant breastfeeding behavior, delayed onset of lactation, and excess neonatal weight loss. Pediatrics. 2003;112:607–619. doi: 10.1542/peds.112.3.607. [DOI] [PubMed] [Google Scholar]
- Doan T, Gardiner A, Gay CL, Lee KA. Breast-feeding increases sleep duration of new parents. Journal of Perinatal and Neonatal Nursing. 2007;21:200–206. doi: 10.1097/01.JPN.0000285809.36398.1b. [DOI] [PubMed] [Google Scholar]
- Dykes F. A critical ethnographic study of encounters between midwives and breast-feeding women in postnatal wards of England. Midwifery. 2005;21:241–252. doi: 10.1016/j.midw.2004.12.006. [DOI] [PubMed] [Google Scholar]
- Dykes F. Breastfeeding in hospital: mothers, midwives and the production line. Routledge; London: 2006. [Google Scholar]
- Evans KC, Evans RG, Ryoal R, Esterman AJ, James SL. Effect of cesarean section on breast milk transfer to the normal term newborn over the first week of life. Archives of Disease in Childhood – Fetal & Neonatal Edition. 2003;88:F380–F382. doi: 10.1136/fn.88.5.F380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forster DA, McLachlan HL. Women’s views and experiences of breast feeding: positive, negative or just good for the baby? Midwifery. 2010;26:16–125. doi: 10.1016/j.midw.2008.04.009. [DOI] [PubMed] [Google Scholar]
- Howie WO, McMullen PC. Breastfeeding problems following anesthetic administration. Journal of Perinatal Education. 2006;15:50–57. doi: 10.1624/105812406X119039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hung KJ, Berg O. Early skin-to-skin after cesarean to improve breastfeeding. The American Journal of Maternal Child Nursing. 2011;36:318–324. doi: 10.1097/NMC.0b013e3182266314. [DOI] [PubMed] [Google Scholar]
- Jain L, Eaton DC. Physiology of fetal lung fluid clearance and the effect of labor. Seminars in Perinatology. 2006;30:34–43. doi: 10.1053/j.semperi.2006.01.006. [DOI] [PubMed] [Google Scholar]
- Karlström A, Engström-Olofsson R, Norbergh KG, Sjöling M, Hildingsson I. Postoperative pain after cesarean birth affects breastfeeding and infant care. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2007;36:430–440. doi: 10.1111/j.1552-6909.2007.00160.x. [DOI] [PubMed] [Google Scholar]
- Kornides M, Kitsantas P. Evaluation of breastfeeding promotion, support, and knowledge of benefits on breastfeeding outcomes. Journal of Child Health Care. 2013 doi: 10.1177/1367493512461460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lööf-Johanson M, Foldevi M, Rudebeck CE. Breastfeeding as a specific value in women’s lives: the experiences and decisions of breastfeeding women. Breastfeeding Medicine. 2013;1:38–44. doi: 10.1089/bfm.2012.0008. [DOI] [PubMed] [Google Scholar]
- McDonald SD, Pullenayegum E, Chapman B, Vera C, Gilia L, Fusch C, Foster G. Prevalence and predictors of exclusive breastfeeding at hospital discharge. Obstetrics and Gynecology. 2012;119:1171–1179. doi: 10.1097/AOG.0b013e318256194b. [DOI] [PubMed] [Google Scholar]
- Miles MB, Huberman AM. Qualitative data analysis: An expanded sourcebook. 2. Thousand Oaks, CA: Sage; 1994. [Google Scholar]
- Montgomery-Downs HE, Clawges HM, Santy EE. Infant feeding methods and maternal sleep and daytime functioning. Pediatrics. 2010;126:e1562–e1568. doi: 10.1542/peds.2010-1269. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Clinical Excellence. [Accessed March 2013];Caesarean Section (update). Clinical Guideline CG132. 2012 at http://guidance.nice.org.uk/CG132. [PubMed]
- Nissen E, Uvnäs-Moberg K, Svensson K, Stock S, Widström AM, Winberg J. Different patterns of oxytocin, prolactin but not cortisol release during breastfeeding in women delivered by caesarean section or by the vaginal route. Early Human Development. 1996;45:103–118. doi: 10.1016/0378-3782(96)01725-2. [DOI] [PubMed] [Google Scholar]
- Nolan A, Lawrence C. A pilot study of a nursing intervention protocol to minimize maternal-infant separation after cesarean birth. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2009;38:430–442. doi: 10.1111/j.1552-6909.2009.01039.x. [DOI] [PubMed] [Google Scholar]
- Nommsen-Rivers LA, Dewey KG. Development and validation of the infant feeding intentions scale. Maternal & Child Health Journal. 2009;13:334–342. doi: 10.1007/s10995-008-0356-y. [DOI] [PubMed] [Google Scholar]
- O’Brien ML, Buikstra E, Fallon T, Hegney D. Strategies for success: a toolbox of coping strategies used by breastfeeding women. Journal of Clinical Nursing. 2009;18:1574–1582. doi: 10.1111/j.1365-2702.2008.02667.x. [DOI] [PubMed] [Google Scholar]
- Patton MQ. Qualitative research and evaluation methods. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Pérez-Ríos N, Ramos-Valencia G, Ortiz AP. Cesarean delivery as a barrier for breastfeeding initiation: the Puerto Rican experience. Journal of Human Lactation. 2008;24:293–302. doi: 10.1177/0890334408316078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prior E, Santhakumaran S, Gale C, Philipps LH, Modi N, Hyde MJ. Breastfeeding after cesarean delivery: a systematic review and meta-analysis of world literature. American Journal of Clinical Nutrition. 2012;95:1113–1135. doi: 10.3945/ajcn.111.030254. [DOI] [PubMed] [Google Scholar]
- Ramachadrappa A, Jain L. Elective cesarean section: its impact on neonatal respiratory outcome. Clinics in Perinatology. 2008;35:373–393. doi: 10.1016/j.clp.2008.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renfrew MJ, Pokhrel S, Quigley M, McCormick F, Fox-Rushby J, Dodds R, Duffy S, Trueman Williams A. Preventing diseases and saving resources: the potential contribution of increasing breastfeeding rates in the UK. UNICEF; UK: 2012. [Accessed July 2013]. at http://www.unicef.org.uk/Documents/Baby_Friendly/Research/Preventing_disease_saving_resources.pdf. [Google Scholar]
- Rowe-Murray HJ, Fisher JRW. Operative intervention in delivery is associated with compromised early mother-infant interaction. British Journal of Obstetrics& Gynaecology. 2001;108:1068–1075. doi: 10.1111/j.1471-0528.2001.00242.x. [DOI] [PubMed] [Google Scholar]
- Sakalidis VS, Williams TM, Hepworth AR, Garbin CP, Hartmann PE, Paech MJ, Al-Tamimi Y, Geddes DT. A comparison of early sucking dynamics during breastfeeding after cesarean section and vaginal birth. Breastfeeding Medicine. 2013;8:79–85. doi: 10.1089/bfm.2012.0018. [DOI] [PubMed] [Google Scholar]
- Sinha A, Bewley A, McIntosh T. Myth: babies would choose prelabour caesarean section. Seminars in Fetal & Neonatal Medicine. 2011;16:247–253. doi: 10.1016/j.siny.2011.03.003. [DOI] [PubMed] [Google Scholar]
- Stuebe AM, Bonuck K. What predicts intent to breastfeed exclusively? Breastfeeding knowledge, attitudes, and beliefs in a diverse urban population. Breastfeeding Medicine. 2011;6:413–420. doi: 10.1089/bfm.2010.0088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor J, Johnson M. How women manage fatigue after childbirth. Midwifery. 2010;26:367–375. doi: 10.1016/j.midw.2008.07.004. [DOI] [PubMed] [Google Scholar]
- Tender JAF, Janakiram J, Arce E, Mason R, Jordan T, Marsh J, Kin S, Jianping H, Moon RY. Reasons for in-hospital formula supplementation of breastfed infants from low-income families. Journal of Human Lactation. 2009;25:11–17. doi: 10.1177/0890334408325821. [DOI] [PubMed] [Google Scholar]
- Tesch R. Qualitative research, analysis types and software tools. New York, NY: Falmer Press; 1990. [Google Scholar]
- Wayse W, Yousafzai A, Mogale K, Filteau S. Association of subclinical vitamin D deficiency with severe acute lower respiratory infection in Indian children under 5 y. European Journal of Clinical Nutrition. 2004;58:563–567. doi: 10.1038/sj.ejcn.1601845. [DOI] [PubMed] [Google Scholar]
- Wilkinson S. Focus group research. In: Silverman D, editor. Qualitative research: theory, method and practice. 2. Sage Publications; London: 2004. pp. 177–199. [Google Scholar]
- World Health Organization. Pregnancy, childbirth, postpartum and newborn care: a guide for essential practice. Geneva: World Health Organization; 2006. [Accessed July 2013]. at http://whqlibdoc.who.int/publications/2006/924159084X_eng.pdf. [PubMed] [Google Scholar]
- World Health Organization [WHO] and United Nations International Children Fund [UNICEF] Baby-Friendly Hospital Initiative: revised, updated and expanded for integrated care. WHO and UNICEF; Geneva, Switzerland: 2009. [Accessed July 2013]. at http://whqlibdoc.who.int/publications/2009/9789241594967_eng.pdf. [PubMed] [Google Scholar]
- Zhu P, Hao J, Jiang X, Huang K, Tao F. New insight into onset of lactation: mediating the negative effect of multiple perinatal biopsychosocial stress on breastfeeding duration. Breastfeeding Medicine. 2012;8:151–158. doi: 10.1089/bfm.2012.0010. [DOI] [PMC free article] [PubMed] [Google Scholar]