Abstract
The Unmet Needs Model states that problem behaviors of people with dementia result from unmet needs stemming from a decreased ability to communicate those needs and to provide for oneself. The purpose of this study is to describe the unmet needs of persons with dementia exhibiting behavior problems. Eighty-nine residents from 6 Maryland nursing homes with dementia were assessed by research assistants and nursing assistants for their unmet needs using multiple assessment tools. Three unmet needs per resident were identified on average, with informants rating boredom/sensory deprivation, loneliness/need for social interaction, and need for meaningful activity as the most prevalent needs. Discomfort was associated with higher levels of verbally agitated behaviors (e.g., complaining). Based on results and independent ratings of pain, the authors estimate notable under detection of discomfort and pain by both types of informants. The study demonstrates methodologies for uncovering unmet needs among persons with dementia and highlights the importance of developing programs that address those unmet needs, especially social and activity needs of nursing home residents. The detection of pain, and possibly that of discomfort, may require a different methodology.
Keywords: older persons, unmet needs model, nonpharmacological interventions
1. Introduction
Persons with dementia often exhibit inappropriate behaviors, which increases their suffering as well as the burden of caregivers (Cohen-Mansfield, 2001). These behaviors are addressed by both pharmacological and nonpharmacological treatments. There are several theoretical models regarding the etiology of inappropriate behaviors in persons with dementia, (Cohen-Mansfield, 2000b) and this paper will focus primarily on the Unmet Needs Model and its implications for the treatment and prevention of these behaviors.
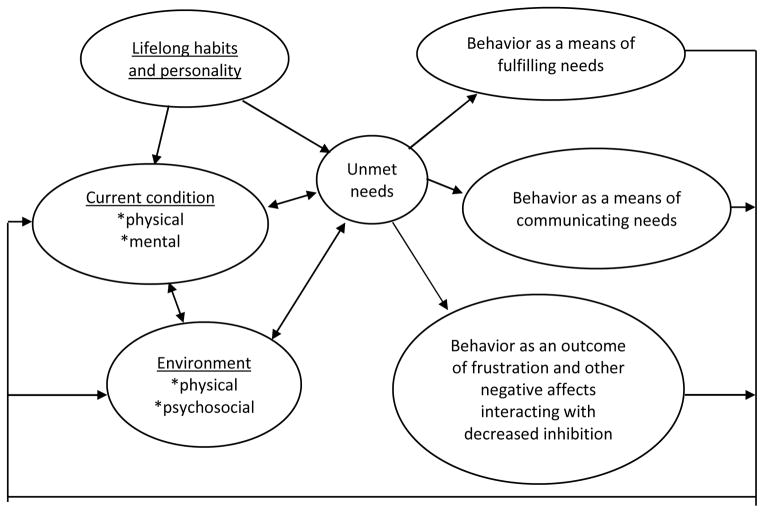
The Unmet Needs Model (Cohen-Mansfield and Werner, 1995; Cohen-Mansfield, 2000b) postulates that the dementia process results in a decreased ability to meet one’s needs because of an increasing difficulty in communicating these needs, and a decreased ability to provide for oneself (Hancock et al., 2006). The needs may pertain to pain/health/physical discomfort, mental discomfort, the need for social contacts, uncomfortable environmental conditions, or an inadequate level of stimulation. According to the Unmet Needs Model, problem behaviors result from an imbalance in the interaction between lifelong habits and personality, current physical and mental states, and less than optimal environmental conditions (Figure 1). Most of the unmet needs arise because of dementia-related impairments in both communication and the ability to utilize the environment appropriately to accommodate needs. The environment and caregivers, in turn, either do not provide for the needs or do so in a way that does not accommodate one’s preferences, habits, and disabilities. Consequently, agitated behaviors, such as pacing may act to alleviate boredom or repetitious vocalizations may be used to communicate the need. Prior studies have found relationships between certain behaviors and participants conditions and environments which support the notion of unmet needs. Specifically, those manifesting verbal\vocal behaviors were more likely to be displayed by persons who were rated as having pain, discomfort or being alone, whereas physically nonaggressive behaviors were more likely under normal environmental conditions when the people with dementia were not engaged with any activity (Cohen-Mansfield et al., 1990; Cohen-Mansfield and Werner, 1995; Sloane et al., 1997; Cohen-Mansfield, 2000a).
Figure 1.
Unmet needs model of problem behaviors. (c) Cohen-Mansfield, 2009.
Understanding unmet needs is central in formulating treatment plans for Nursing Home (NH) residents with dementia. Indeed, they form the basis for nonpharmacologic interventions for dementia (Bédard et al., 2011; Kolanowski et al., 2011; Cohen-Mansfield et al., 2012). Thus we examined unmet needs as perceived by Nursing Assistants (NAs) caring for the residents as well as Research Assistants (RAs) involved in implementing a nonpharmacological treatment program. As described in Cohen-Mansfield et al., (2012), the nonpharmacolocical interventions were tailored to participants’ needs. In response to need to alleviate loneliness, participants were presented with interventions such as simulated social stimuli such as a respite video or a lifelike baby doll, or one on one interaction. Those who had a need of relieving boredom were provided with stimuli that matched their past preferences such as reading materials or music. Those who had needs related to discomfort were helped directly with the specific source of discomfort, and an intervention could involve provision of care requested, such as responding to requests to be taken to one’s room. The specific research questions are:
What are the perceptions of unmet needs that contribute to behavior problems? What is the level of confidence in the determination of unmet needs?
How does RAs determination of unmet needs compare to that of NAs caring for the person?
-
How do the unmet needs relate to residents’ background information? The following hypotheses were examined:
The designation by the research assistant of pain relief as an unmet need will correlate positively with ratings of pain (assessed via the PAINE), and to negative affect (Cohen-Mansfield and Marx, 1993).
Unmet needs due to anxiety will be positively related to observed negative affect at baseline.
-
How do the unmet needs relate to the type of agitation manifested? Specific hypotheses are:
Social needs, pain, and discomfort will be related to verbally agitated behaviors (Cohen-Mansfield et al., 1990; Cohen-Mansfield and Werner, 1995; Sloane et al., 1997; Cohen- Mansfield, 2000a).
Boredom and need for stimulation will be related to physically nonaggressive agitated behaviors (Cohen-Mansfield, 2000a).
2. Methods
The current study describes the determination of unmet needs within the context of the treatment arm of a randomized placebo controlled repeated measures study of nonpharmacological intervention for behavior problems in persons with dementia (Cohen-Mansfield et al., 2012). The study was approved by the Institutional Review Board of the Charles E. Smith Life Communities and participants or closest relatives signed an informed consent.
2.1 Subjects
Participants were 89 NH residents (mean age=85.9) with a diagnosis of dementia, according to their medical chart, from 6 NHs in Maryland, USA. The inclusion criteria were: (a) The resident had been at the facility for at least three weeks so that nursing staff members knew the resident well enough to accurately assess him or her; (b) The resident had been identified by nursing staff as exhibiting either verbal agitation or physical non-aggressive agitation several times a day; and (c) The resident had a diagnosis of dementia. Exclusion criteria were: (a) A nursing staff member responsible for direct care of the resident judged him/her to have a life expectancy of less than 3 months due to obvious causes; (b) The resident had an accompanying diagnosis of bipolar disorder or schizophrenia; and (c) A score of 25 or higher on the Mini-Mental State Examination (MMSE; Folstein et al., 1975).
2.2 Procedure
For all study participants, informed consent was provided by the attorney in fact or the closest family member (Cohen-Mansfield et al., 1988). The ABMI observations and the MMSE were administered by trained RAs. After obtaining data on participants’ background, cognitive function, and medical status, baseline observations of agitation using the ABMI, (Cohen-Mansfield et al., 1989) on a Palm Pilot Zire™ were recorded. Direct observations were chosen because these are more objective and more accurate than other forms of assessment. Three minute observations of each participant were performed during three consecutive days for a total of 13 hours per day by several RAs. Each RA observed one resident at a time, and recorded one observation for each participant in every consecutive half-hour period. The PAINE was administered to each resident’s primary staff caregiver. Both the RAs and NAs assessed the participants’ unmet needs after the RAs completed the above assessments and the RAs conducted the intervention as described in Cohen-Mansfield et al., 2012.
2.3 Measurements
Background
Data regarding age, gender, ethnicity, and marital status were collected from each resident’s chart at the NH. Information from medical records included prescribed medications (including pain relievers and psychotropic drugs) and confirmation of the diagnosis of dementia as well as other medical diagnoses.
Cognitive functioning
The diagnosis of dementia was obtained from a physician or nurse practitioner. Cognitive status of the participants was assessed using the MMSE (Folstein et al., 1975). Scores ranged 0 (severe cognitive impairment) to 30 (normal cognitive functioning). Pain was assessed by the Pain Assessment In Elderly Persons (PAINE), consisting of a list of pain symptoms rated by direct caregivers (Cohen-Mansfield, 2006). Validity data are provided in (Cohen-Mansfield and Lipson, 2008).
Agitation
Direct observations were recorded via the Agitated Behaviors Mapping Instrument (ABMI; Cohen-Mansfield et al., 1989). An RA recorded the frequency of occurrence of 14 items describing problem behaviors, characterized as physical agitation (e.g., pacing), or verbal/vocal agitation (e.g., groaning). Inter-rater reliabilities regarding agitated behaviors previously averaged 0.93 (Cohen-Mansfield et al., 1989) and currently averaged 96% with Intra-Class Correlation (ICC) of 0.90.
Affect
Evaluation of positive and negative affect was based on direct observation and assessed via Lawton’s Modified Behavior Stream (LMBS; Lawton et al., 1996). Five different modes of affect were evaluated overall. Two were positive affect: pleasure and interest; three were negative affect: anger, anxiety, and sadness. Due to low frequencies of negative affect, the measures of anger, anxiety and sadness were combined to yield a mean score. Inter- rater agreement evaluations averaged 88% per emotional mode, with a range of 70%–99%, and an average ICC of 0.91.
Unmet Needs were assessed using the Type of Unmet Need Assessment (TUNA), developed by the authors. The TUNA includes 9 yes or no items describing types of unmet needs (Table 1). The discomfort need is subdivided into 12 yes or no items (Table 1). Participants are asked to circle the types of unmet needs that may affect the agitation of the NH resident. Overall confidence in unmet needs, specified in the TUNA, is rated on a 5-point scale ranging from 1 (“completely unsure”) to 5 (“completely confident”). Test–retest reliability was obtained for 41 NAs who completed the TUNA twice (with a mean of 14 days between TUNA administrations), resulting in an agreement rate of 85%. Research assistants were instructed to use all the information available to them (observations, assessments, etc.) in completing the TUNA. This included observations as to whether problem behavior increased under certain conditions (e.g., when the person was alone, when there were no activities, when the person seemed to be in an uncomfortable position). They also took into account their observations as to whether the problem behaviors diminished when interventions were addressing a potential need, for example, when the intervention included social exchange. Discomfort was ascertained either by observation (see Cohen-Mansfield et al., 2013), through interpretation of the participant’s verbal behavior, or via other means, such as the impact of intervention. In contrast to the RAs, the NAs were simply instructed to rely on their daily acquaintance with participants in completing the TUNA.
Table 1.
Percent of unmet needs of 89 nursing home residents with dementia
| Informant
|
Authors’ estimate | ||
|---|---|---|---|
| Research Assistant | Nursing Assistant | ||
|
| |||
| % with need | |||
| Type of unmet need | |||
| Loneliness/need for social interaction | 68.5 | 48.3 | 70 |
| Boredom/sensory deprivation | 70.8 | 50.6 | 75 |
| Need for meaningful activity | 59.6 | 46.1 | 60 |
| Discomfort | 32.6 | 37.1 | 51 |
| Anxiety/need for relaxation | 23.6 | 25.8 | 26 |
| Need for control | 11.2 | 19.1 | 19 |
| Pain | 8.0 | 10.1 | 55 |
| Other unmet need | 3.4a | 5.6b | 8 |
| No need | 1.1 | 6.7 | 0 |
| Type of discomfort | |||
| Need to go to the bathroom | 9.0 | 6.7 | 13 |
| Uncomfortable seating position | 6.7 | 1.1 | 8 |
| Fatigue | 7.9 | 4.5 | 11 |
| Hunger | 4.5 | 4.5 | 8 |
| Thirst | 4.5 | 2.2 | 6 |
| Discomfort caused by behavior of another resident(s) | 3.4 | 3.4 | 4 |
| Need to change underwear | 2.2 | 1.1 | 2 |
| Restraints | 1.1 | 2.2 | 3 |
| Constipation | 1.1 | 4.5 | 6 |
| Feeling cold | 1.1 | 1.1 | 2 |
| Feeling hot | 0.0 | 0.0 | 0 |
| Other discomfort | 6.7c | 18.0d | |
wants to go home; wants to sleep in own room; disease
needs attention, presence of unwanted person, turning TV off, needs to go out, needs to go outside-see family
itching, discomfort related to having to prop legs up, discomfort related to back, uncomfortable body position, stomach problems
itching, diaper-related discomfort, contractures, noise, discomfort related to body parts and functions (back, leg, knee, stomach, breathing, sore foot, neuropathy in feet, muscles, teeth, scrotum)
2.4 Statistical analyses
TUNA responses were tabulated for the RA and the NA. We then examined the frequencies and means of the ratings of confidence in the determination of unmet needs. For the 2nd research question, we compared the assessment by the NA with that of the RA using chi square and kappa. For the 3rd and 4th research questions, we compared those with and without an unmet need based on the RAs reports using chi-square and Mann-Whitney nonparametric analyses. In the presentation of results, p-values are 2-sided unless reported in response to a specific hypothesis.
3. Results
Of the 89 NH residents under study, 73% were female, 81% were Caucasian, and over half (60.7%) were widowed. The mean MMSE score was 7.6. Each participant received an average of 9 medications, and all of the participants received analgesics.
3.1 The perceptions of unmet needs contributing to behavior problems, and the level of confidence in the determination of unmet needs
The prevalence of unmet needs based on perceptions of RAs (who observed residents and also implemented nonpharmacologic interventions) and NAs (front-line caregivers) are presented in Table 1. The most common needs were loneliness/need for social contact and boredom/sensory deprivation, noted for about two thirds of the sample by RAs and for approximately half by NAs, followed by the need for a meaningful activity, which was noted for around half the sample by both sources. Discomfort was noted as an unmet need for about one third of the sample and included many types of needs including the need to use the bathroom (most commonly) and uncomfortable seating positions (Table 1). RAs reported an average of 2.9 unmet needs per participant (range 0–7, s.d.=1.3) and NAs reported an average of 2.6 unmet needs per participant (range 0–6, s.d.=1.4).
Informants felt quite confident with their ratings. On a scale of 1 (completely unsure) to 5 (completely confident), RAs marked 52% of their ratings with ‘4’, 34% with ‘3’, and 14% with ‘5’. While the ratings of NAs produced a somewhat different distribution (NAs ratings of 3, 4, and 5 were given to 36%, 31% and 27% of the sample, respectively with another 5% ratings of 2 and 1% rating 1), the average rating of confidence was identical for both RAs and NAs (mean=3.78).
3.2 A comparison of RAs and NAs determination of unmet needs
The agreement rate between RAs and NAs averaged 86% for all types of needs, and kappas averaged .25. Based on our examination of the results, this indicates high agreement when most of the residents do not exhibit the need, but much lower agreement when determining which residents actually experience a specific unmet need.
3.3 Unmet needs in relation to residents’ background information
RA’s designation of the unmet need of pain was associated with significantly better cognitive function as tapped by the MMSE (z=2.16, p=.03), significantly higher levels of negative affect at baseline (z=2.21, p=.027), and higher scores on the PAINE (z=1.76. p=.039, one-tailed; one-tailed tests used to examine one sided hypotheses). Residents rated as having anxiety/need for relaxation by the RA had significantly higher ratings of verbal agitation (z=2.04, p=.041), and negative affect (z=2. 60, p=.009).
3.4 Unmet needs in relation to the type of agitation manifested
Participants who were rated by RAs as having a loneliness need had significantly higher ratings of verbal agitation (Mann-Whitney test, z=1.70, p=.045, one-tailed – used based on the hypothesis) than those not designated as having this need, but there was no difference between the groups in physical agitation. Discomfort was related to better cognitive function (MMSE, z=2.56, p=.01), greater pain (PAINE, z=2.07, p=.039), higher levels of negative affect at baseline (z=1.96, p=.05), higher levels of manifesting verbally agitated behaviors of constant requests for attention (z=1.93. p=.027, one-tailed), complaining (z=2.92, p=.004), and screaming (z=2.28, p=.02). Discomfort was not significantly associated with the ratings of the category of verbal behaviors.
Participants who were rated as having an unmet need which is related to boredom and sensory deprivation displayed somewhat higher levels of physical nonaggressive behaviors (mean ranks of 47.1 for those rated as having the need and 39.9 for those rated as not having it, z=1.20, p=.11, one-tailed). However, this difference did not reach statistical significance.
Upon reviewing the analyses described above, it became clear that the ratings of unmet needs by RAs and by NAs may actually represent an underestimation of the residents’ true needs, which led to reinterpreting the results and developing improved estimates for the prevalence of unmet needs. These authors’ estimates are an analysis based on the following premises: Regarding pain, the finding that pain was significantly related to cognitive function led us to believe that the raters of the present study were subject to the same bias found in most studies of pain in persons with dementia; that is, those who can express pain are likely to be identified, whereas those who cannot express pain remain under diagnosed (Cohen-Mansfield, 2005; Cohen-Mansfield and Lipson, 2002). For this reason, the PAINE data was used for the estimate rather than the reports of RAs or NAs, as this assessment has been shown to be superior to others for the detection of pain in this population (Cohen-Mansfield and Lipson, 2008). Discomfort was also significantly related to better cognitive function, suggesting that discomfort was under detected among participants with a severe cognitive decline. To account for this, the revised estimates for the specific types of discomfort were derived by combining the reports of nursing and RAs, i.e., accepting either report as valid indication of such discomfort. For social and activity needs, we chose to use only the RA’s evaluation since the RA, unlike the overextended nursing staff, was able to give undivided attention to a resident’s response to social/activity opportunities; that is, an RA could learn if an unmet need had indeed been present by observing resident improvement following introduction of the social and activity solutions designed to meet that need. For the need of control, we chose only the NA ratings for the revised estimate as we had observed that nursing staff labeled a resident as “resisting care” if the resident expressed a preferred time or alternate venue for care delivery, thus manifesting his/her need for control of his/her daily life. The percentages of residents with each unmet need, as determined by the revised estimate, are presented in the authors’ estimate column in Table 1. The following unmet needs were found for over half of the residents: loneliness/need for social contact, boredom, need for meaningful activity, pain, and discomfort. Moreover, each study participant was rated as having at least one unmet need.
4. Discussion
This is the first paper to delineate the unmet needs of agitated NH residents with dementia, revealing an average of 3 unmet needs per resident. Results show a high prevalence of unmet needs, particularly for needs pertaining to loneliness/need for social contact, boredom, need for meaningful activity, and discomfort. The extent of unmet needs in these NH residents, according to the revised estimate (Table 1), is alarming and in our opinion, calls for immediate action.
A high prevalence of unmet needs relating to social contact and meaningful activities was found. This finding corroborates previous findings in persons with dementia of a need for being useful/giving meaning to life, enjoyment of activities, and social contact, which have been rated as psychological domains judged to be important to the quality of life of persons with dementia (see Schölzel-Dorenbos et al., 2010). In this way, finding meaningful activities is imperative for promoting quality of life and reducing agitated behaviors. Activities interpreted as meaningful by residents relate to their past values, beliefs, interests and routines, and psychological needs and are experienced as enjoyable (Schölzel-Dorenbos et al., 2010).
The modest agreement between RAs and NAs regarding the determination of unmet needs attests to the difficulty of determining such needs in a population with a severe cognitive impairment. We believe this result stems from the different perspectives of these informants. Whereas the RAs focused on social and activity needs and their fulfillment, the NAs were more concerned with physical needs and often had more information of this type (e.g., constipation as an unmet need) to draw from when completing the TUNA. Unmet needs represent an internal construct that cannot be assessed by self-report, yet is crucial for proper treatment. Accordingly, this finding demonstrates the value of the subjective assessment of unmet needs and reinforces the need to use multiple informants (Chung, 2006) (such as activity therapists, social workers, relatives and NAs) who focus on different aspects of needs. An alternative is to provide a comprehensive training about unmet needs to all professionals, which could prompt all to focus on the different needs independently of their profession. In addition, the above finding highlights the need for a comprehensive assessment of unmet needs using quantitative measurements (Cohen-Mansfield et al., 2013), observations (Cohen-Mansfield et al., 2012), and trial and error protocols. Finally, the promotion of an ongoing dialogue and discussion among the different sources of information is warranted.
One of the challenges with assessing nursing home residents by nursing assistants is staff turnover. This has been shown to pose a barrier to quality of care (Trinkoff et al., 2013; Lerner et al., 2014). It is likely to affect nursing assistants’ ability to provide a thorough evaluation of unmet needs via the TUNA and should therefore be taken into account in future research.
The version of TUNA presented in this paper is a first step towards developing a nomenclature of unmet needs. The TUNA is the consolidation of findings from prior literature, our observations of NH residents over the years, and a small pilot study. That pilot tackled problems of categorizing unmet needs in order to develop categories and suggested, for example, combining the categories of boredom and need for sensory stimulation, since differentiation between these proved difficult.
Validity of the TUNA was examined by analyzing relationships between unmet needs and independently derived measures of the same needs or behaviors. Findings included significant associations between an unmet need of pain and higher scores on the PAINE, and between having anxiety/need or relaxation and negative affect. Thus, the hypotheses relating to the 3rd research question were generally supported. In regard to the hypotheses relating to the 4th research question pertaining to the relationship between unmet needs and type of agitation, the relationships between loneliness and verbal agitation and between pain and verbal agitation were supported by the findings. Significant relationships between discomfort and specific types of verbal agitation were found, but not with the category as a whole. The fact that one relationship, that between boredom and physical agitation, emerged as a trend rather than a statistically significant result is most likely due to too small of a sample size.
Yet, other challenges relating to the current nomenclature remain. For instance, while one would expect that boredom would be rather close to the need for meaningful activities, as has been found in other studies (Cohen-Mansfield, 2001; Cohen-Mansfield et al., 2009; Kolanowski et al., 2011), data from this study suggest otherwise. Cross tabulating ratings for both of these unmet needs shows that RAs identified only one or the other of these needs, rather than both, 39% of the time; the corresponding rate for NAs was 66% indicating that informants found these two needs to be different. Similarly, there was considerable overlap between the categories of pain and discomfort, yet the ratings were different. Finally, a closer look needs to be taken at issues raised in the categories of Other unmet needs and Other needs pertaining to discomfort (see Table 1) in order to define additional categories not yet available in the TUNA. Future versions of the TUNA should further refine the nomenclature.
The determination of unmet needs is a basis for developing intervention and prevention programs to meet those needs, thereby leading to improvement in the quality of life of NH residents with dementia. This study can therefore be seen as a template for developing such programs. It highlights the crucial importance of developing programs that address social and activity needs of NH residents as well as the urgent need to improve detection and treatment of physical needs that result in pain and discomfort. The specific nature of the identified discomfort needs make these particularly amenable to improvement efforts. Thus, the findings could be used to enhance person-centered care and quality of care in nursing homes. Further studies to develop and implement programs to address unmet needs in the NH environment are necessary to promote effective interventions.
Research Highlights.
On average, three unmet needs were identified per nursing home resident
The most common were needs for stimulation and for meaningful and social activities
The paper presents a methodology for the determination of unmet needs
Acknowledgments
Funding: This study was supported by National Institutes of Health grant 2 R01 AG010172-10A2 and by the Minerva-Stiftung Foundation Grant number 31583295000, 80539. There was no involvement in conducting the research and/or preparation of the article.
Footnotes
Conflicts of Interest: The authors have no actual or potential conflicts of interest to disclose.
Contributors: All authors have approved the final article.
Jiska Cohen-Mansfield directed the study and was involved and contributed to the data collection, data analysis and interpretation of data and write up.
Maha Dakheel-Ali was involved in data collection and data analysis
Marcia S. Marx contributed to the conceptualization of the study and was involved in the interpretation of data and write-up.
Khin Thein was involved in the coordination of data collection, data collection and data checks and organization.
Natalie G. Regier was involved in data collection and the write-up of the paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bédard A, Landreville P, Voyer P, Verreault R, Vézina J. Reducing verbal agitation in people with dementia: evaluation of an intervention based on the satisfaction of basic needs. Aging & Mental Health. 2011;15:855–865. doi: 10.1080/13607863.2011.569480. [DOI] [PubMed] [Google Scholar]
- Chung J. Care needs assessment of older Chinese individuals with dementia of Hong Kong. Aging & Mental Health. 2006;10:631–637. doi: 10.1080/13607860600650532. [DOI] [PubMed] [Google Scholar]
- Cohen-Mansfield J. Nonpharmacological management of behavioral problems in persons with dementia: the TREA model. Alzheimers Care Today. 2000a;1:22–34. [Google Scholar]
- Cohen-Mansfield J. Theoretical frameworks for behavioral problems in dementia. Alzheimers Care Today. 2000b;1:8–21. [Google Scholar]
- Cohen-Mansfield J. Nonpharmacologic interventions for inappropriate behaviors in dementia: a review, summary, and critique. American Journal of Geriatric Psychiatry. 2001;9:361–381. [PubMed] [Google Scholar]
- Cohen-Mansfield J. Nursing staff members assessments of pain in cognitively impaired nursing home residents. Pain Management Nursing. 2005;6:68–75. doi: 10.1016/j.pmn.2005.05.002. [DOI] [PubMed] [Google Scholar]
- Cohen-Mansfield J. Pain assessment in noncommunicative elderly persons-PAINE. Clinical Journal of Pain. 2006;22:569–575. doi: 10.1097/01.ajp.0000210899.83096.0b. [DOI] [PubMed] [Google Scholar]
- Cohen-Mansfield J, Billig N, Lipson S, Rosenthal AS, Pawlson LG. Medical correlates of agitation in nursing home residents. Gerontology. 1990;36:150–158. doi: 10.1159/000213191. [DOI] [PubMed] [Google Scholar]
- Cohen-Mansfield J, Dakheel-Ali M, Marx MS. Engagement in persons with dementia: the concept and its measurement. American Journal of Geriatric Psychiatry. 2009;17:299–307. doi: 10.1097/JGP.0b013e31818f3a52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen-Mansfield J, Kerin P, Pawlson G, Lipson S, Holdridge K. Informed consent for research in a nursing home: processes and issues. The Gerontologist. 1988;28:355–360. doi: 10.1093/geront/28.3.355. [DOI] [PubMed] [Google Scholar]
- Cohen-Mansfield J, Lipson S. Pain in cognitively impaired nursing home residents: how well are physicians diagnosing it? Journal of the American Geriatrics Society. 2002;50:1039–1044. doi: 10.1046/j.1532-5415.2002.50258.x. [DOI] [PubMed] [Google Scholar]
- Cohen-Mansfield J, Lipson S. The utility of pain assessment for analgesic use in persons with dementia. Pain. 2008;134:16–23. doi: 10.1016/j.pain.2007.03.023. [DOI] [PubMed] [Google Scholar]
- Cohen-Mansfield J, Marx MS. Pain and depression in the nursing home: corroborating results. Journals of Gerontology. 1993;48:96–97. doi: 10.1093/geronj/48.2.p96. [DOI] [PubMed] [Google Scholar]
- Cohen-Mansfield J, Thein K, Marx MS, Dakheel-Ali M, Freedman L. Efficacy of nonpharmacologic interventions for agitation in advanced dementia: a randomized, placebo-controlled trial. Journal of Clinical Psychiatry. 2012;73:1255–1261. doi: 10.4088/JCP.12m07918. [DOI] [PubMed] [Google Scholar]
- Cohen-Mansfield J, Thein K, Marx MS, Dakheel-Ali M, Jensen B. Sources of discomfort in persons with dementia. JAMA Internal Medicine. 2013;173:1378–1379. doi: 10.1001/jamainternmed.2013.6483. [DOI] [PubMed] [Google Scholar]
- Cohen-Mansfield J, Werner P. Environmental influences on agitation: an integrative summary of an observational study. American Journal of Alzheimers Disease & Other Dementias. 1995;10:32–39. [Google Scholar]
- Cohen-Mansfield J, Werner P, Marx MS. An observational study of agitation in agitated nursing home residents. International Psychogeriatrics. 1989;1:153–165. doi: 10.1017/s1041610289000165. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Hancock GA, Woods B, Challis D, Orrell M. The needs of older people with dementia in residential care. International Journal of Geriatric Psychiatry. 2006;21:43–49. doi: 10.1002/gps.1421. [DOI] [PubMed] [Google Scholar]
- Kolanowski A, Litaker M, Buettner L, Moeller J, Costa PT., Jr A randomized clinical trial of theory-based activities for the behavioral symptoms of dementia in nursing home residents. Journal of American Geriatrics Society. 2011;59:1032–1041. doi: 10.1111/j.1532-5415.2011.03449.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawton MP, Van Haitsma K, Klapper J. Observed affect in nursing home residents with Alzheimer’s disease. Journals of Gerontology Series B. 1996;51:3–14. doi: 10.1093/geronb/51b.1.p3. [DOI] [PubMed] [Google Scholar]
- Lerner NB, Johantgen M, Trinkoff AM, Storr CL, Han K. Are nursing home survey deficiencies higher in facilities with greater staff turnover. Journal of the American Medical Directors Association. 2014;15:102–107. doi: 10.1016/j.jamda.2013.09.003. [DOI] [PubMed] [Google Scholar]
- Schölzel-Dorenbos CJ, Meeuwsen EJ, Olde Rikkert MG. Integrating unmet needs into dementia health-related quality of life research and care: introduction of the hierarchy model of needs in dementia. Aging & Mental Health. 2010;14:113–119. doi: 10.1080/13607860903046495. [DOI] [PubMed] [Google Scholar]
- Sloane PD, Davidson S, Buckwalter K, Lindsey BA, Ayers S, Lenker V, Burgio LD. Management of the patient with disruptive vocalization. The Gerontologist. 1997;37:675–682. doi: 10.1093/geront/37.5.675. [DOI] [PubMed] [Google Scholar]
- Trinkoff AM, Han K, Storr CL, Lerner N, Johantgen M, Gartrell K. Turnover, staffing, skill mix, and resident outcomes in a national sample of US nursing homes. Journal of Nursing Administration. 2013;43:630–636. doi: 10.1097/NNA.0000000000000004. [DOI] [PubMed] [Google Scholar]