Abstract
Until recently, genetics was thought to play a minor role in the development of Parkinson’s disease (PD). Over the last decade, a number of genes that definitively cause PD have been identified, which has led to the generation of disease models based on pathogenic gene variants that recapitulate many features of the disease. These genetic studies have provided novel insight into potential mechanisms underlying the etiology of PD. This chapter will provide a profile of the genes conclusively linked to PD and will outline the mechanisms of PD pathogenesis implicated by genetic studies. Mitochondrial dysfunction, oxidative stress and impaired ubiquitin-proteasome system function are disease mechanisms that are particularly well supported by genetic studies and are therefore the focus of this chapter.
Introduction
Parkinson’s disease (PD) is the most common neurodegenerative movement disorder, affecting approximately 1% of the population at 65 years of age, increasing to 5% at 85 years (Van Den Eeden et al, 2003). Clinically, PD is characterized principally by symptoms of resting tremor, bradykinesia, rigidity and postural instability although additional dysfunction of non-motor systems is frequently present (Savitt et al., 2006). The primary symptoms, which together constitute Parkinsonism, arise from a profound degeneration and loss of dopaminergic neurons in the substantia nigra pars compacta, which leads to a marked depletion of the neurotransmitter dopamine in the striatum, a key region of the basal ganglia that regulates movement (Dauer and Przedborski, 2003).
Identifying a role for genetics in PD
Until the end of the twentieth century, PD was predominantly considered a non-genetic disease caused by environmental factors and aging (Farrer, 2006). This notion was propagated early-on by the emergence of Parkinsonism in survivors of the encephalitis epidemic that occurred from 1917–1928 (Poskanser and Schwab, 1963) and later fuelled by discoveries from epidemiological studies that Parkinsonism is associated with exposure to certain pesticides and to MPTP (1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine) via narcotic use (Langston et al., 1983; Elbaz and Moisan, 2008). A major contribution of heredity to development of the disease was thought unlikely due to epidemiological studies which indicated no effect of heritability on life-time risk of developing PD (Cookson et al., 2005). A role for genetics in PD was also not supported by cross-sectional twin studies that suggested low concordance rates in monozygotic and dizygotic twins (Ward et al., 1983; Martilla et al., 1988). This was despite the fact that since as early as the 1880’s, clinicians had been noting familial aggregation of Parkinsonism (Leroux, 1880; Gowers, 1900) and that numerous families inherited PD in a Mendelian fashion (Bell and Clark, 1926) suggesting a genetic contribution to disease. For example, studies on multiple populations in the mid-twentieth century indicated that the emergence of many cases of Parkinsonism were consistent with an autosomal dominant mode of inheritance (Allen, 1937; Mjones, 1949). Finally, over the last decade, linkage mapping studies have resulted in the identification of distinct genetic loci that definitively cause familial PD (Farrer, 2006). These discoveries have resulted in a paradigm shift in perceptions towards the contribution of genetics to PD that extend beyond early-onset familial disease, since variants in α-synuclein and leucine rich repeat kinase 2 (LRRK2) contribute to the lifetime risk of sporadic PD in the population (Cookson et al., 2005; Satake et al., 2009). Importantly, recent advances in the genetics of PD have led to cell and animal models of disease that promote our understanding of molecular pathways underlying the pathogenesis of PD (Dawson et al., 2002; Moore and Dawson, 2008). Although monogenic and sporadic forms of PD are not clinically or pathologically identical, they exhibit common core features such as Parkinsonism and loss of nigral dopamine neurons suggesting that they share common mechanisms of disease and that genetics should, therefore, provide clues to the etiology of sporadic PD (Cookson et al., 2005). The following section describes the genes that have been definitively linked to PD, the normal function of their gene products and how pathogenic mutations are thought to impact cell systems. This outline will form the basis for a subsequent discussion of how genetics has impacted our understanding of PD pathogenic mechanisms.
Dominantly Inherited Mutations
α-synuclein
Studies on a large family of Italian descent (the Contursi kindred) with apparent autosomal dominant PD, led to the discovery of a PD susceptibility locus on the long arm of chromosome 4 (Polymeropolous et al., 1996) that was later identified as the SNCA gene that encodes α-synuclein (Polymeropolous et al., 1997). The 209G>A (Ala53Thr) mutation found in this family was followed by the discovery of two further PD-associated SNCA missense mutations: 88G>C (Ala30Pro) (Kruger et al., 1998) and 188G>A (Glu46Lys) (Zarranz et al., 2004). Patients with SNCA point mutations typically develop prominent dementia and an earlier onset of Parkinsonism than in sporadic PD (Farrer, 2006). In addition to point mutations, duplication or triplication of SNCA have been found in kindreds with classic PD or sometimes, Parkinsonism with autonomic dysfunction and dementia (Singleton et al., 2003; Chartier-Harlin et al., 2004). The strong association between SNCA mutations or multiplications and PD suggests a central role for α-synuclein in PD pathogenesis (Moore et al., 2005). Furthermore, comparison of patients with duplications and triplications of SNCA reveals that age of onset is younger and disease progression faster with gene triplication (which results in an approximate doubling of plasma α-synuclein levels) (Farrer et al., 2004; Miller et al., 2004; Ross et al., 2008) suggesting that α-synuclein expression level and disease severity are related. This correlation between α-synuclein expression levels and PD susceptibility is further supported by studies in patients with sporadic PD in which allelic variability in regions of the SNCA promoter (especially the Rep1 region) is associated with risk of developing PD (Tan et al., 2000; Farrer et al., 2001; Pals et al., 2004), although this remains somewhat controversial (Spadafora et al., 2003; Tan et al., 2003; DeMarco et al., 2008).
α-Synuclein exists mainly as a 140 amino acid protein whose precise function is unknown (Moore et al., 2005). α-Synuclein is expressed in neurons throughout the mammalian nervous system where it resides predominantly at presynaptic terminals associated with vesicles and membranes (Kahle et al., 2000; Fortin et al., 2004; Bonini and Giasson, 2005). Interestingly, α-synuclein is natively unfolded in solution although it adopts an alpha-helical rich conformation when associated with membranes (Ferreon et al., 2009).
The precise function of α-synuclein is unclear, although its association with synaptic vesicles suggests a possible role in neurotransmission. Indeed, studies in yeast and mammalian systems suggest that α-synuclein may regulate synaptic vesicle trafficking via binding to lipids (Jenco et al., 1998; Outeiro and Lindquist, 2003; Nemani et al., 2010). A recent report describes a possible role for α-synuclein in assembly of the SNARE complex between vesicle and presynaptic membranes, which is crucial for priming and recycling of synaptic vesicles (Chandra et al., 2005; Bonini and Giasson, 2005). Deletion of the co-chaperone cysteine-string protein-α in mice results in neurodegeneration with underlying impairment in SNARE complex assembly (Chandra et al., 2005). The authors further report that transgenic expression of α-synuclein attenuates inhibition of SNARE complex formation and prevents neurodegeneration. Despite this, genetic knock-out studies in mice have indicated that the absence of α-synuclein has no significant effect on the pool size of recycling synaptic vesicles, synaptic plasticity or dopamine uptake and release from nerve terminals (Chandra et al., 2004) suggesting that α-synuclein may not be required for regulating synaptic vesicle release or uptake under normal conditions and may, instead, be protective following exposure to certain cell stressors.
Mutations and multiplications in the SNCA gene may cause PD through a gain-of-toxic-function mechanism as suggested by their dominant inheritance pattern. When mutated or at elevated concentrations, α-synuclein has a propensity to develop a β-sheet-rich structure that readily polymerizes into oligomers (Sharon et al., 2003) and higher-order aggregates such as fibrils (Conway et al., 1998) in cells, animal models and human brain (Lee et al., 2002; Outeiro et al., 2008; Sharon et al., 2003; Miller et al., 2004). Insoluble α-synuclein fibrils are a major component of hallmark PD inclusions called Lewy bodies and Lewy neurites, present in perikarya and neurites, respectively. In PD, Lewy bodies and neurites can be found in both dopaminergic and non-dopaminergic neurons of the brainstem and in the cortex (Farrer, 2006). Importantly, Lewy bodies are found in a number of neurodegenerative diseases involving SNCA mutations including PD, parkinsonism with dementia and dementia with Lewy bodies (MartÌ et al., 2003). This establishes a link between these diseases with distinct clinical features but shared pathology. Controversy exists as to whether Lewy bodies and neurites are a cause or consequence of PD, and some evidence suggests they might actually have a protective role by acting to sequester toxic α-synuclein oligomers (Tanaka et al., 2004; Olanow et al., 2004). Fueling this controversy are the findings that certain SNCA mutations (A53T and A30P) promote oligomerization but not fibrillization of α-synuclein and moreover that Lewy bodies are frequently absent from the brains of PD patients with genetic mutations (Conway et al., 2000; Gaig et al., 2007; Ahlskog, 2009). Accordingly, emerging evidence suggests that prefibrillar oligomers and protofibrils are the toxic species responsible for PD pathology (Conway et al., 2000; Goldberg and Lansbury, 2000, Masliah et al., 2000; Kayed et al., 2003; Danzer et al., 2007). α-Synuclein oligomers, akin to other amyloidogenic oligomers cause elevated Ca2+ influx into cells in vitro, possibly by altering membrane stability or permeability by forming membrane pores (Demuro et al., 2005; Danzer et al., 2007). Elevated intracellular Ca2+ levels may promote cellular toxicity through increased generation of reactive oxygen species and resultant oxidative damage.
Whether the pathogenic α-synuclein species is oligomeric, fibrillar or both, it is reasonably clear that aggregates of this protein are toxic in primary neuronal cultures (Xu et al., 2002; Tanaka et al., 2001; Zhou and Freed, 2005 Petrucelli et al., 2002), invertebrate animal models (Feany and Bender 2000; Park and Lee, 2006; periquet et al., 2007; Kuwahara et al., 2006; Lakso et al., 2003) and in rodent (St Martin et al., 2007; Lo Bianco et al., 2002) and non-human primate models involving viral vectors to deliver α-synuclein to the substantia nigra (Kirik et al., 2003; Yasuda et al., 2007). Aggregation may be promoted by numerous factors including mitochondrial complex I inhibitors paraquat and rotenone (Manning-Bog et al., 2002; Sherer et al., 2002; Sherer et al., 2003). Evidence linking exposure to these compounds with the occurrence of sporadic PD suggests a possible role for α-synuclein aggregates in sporadic disease. Additionally, oxidative and nitrative damage, which accumulate in the brains of many species including humans during aging, may promote aggregation of α-synuclein to toxic species (Ostrerova-Golts et al., 2000; Cole et al., 2005; Qin et al., 2007; Leong et al., 2009). Tyrosine nitration of α-synuclein is found in the PD brain and has been shown to accelerate α-synuclein aggregation in vitro (Giasson et al., 2000) by a mechanism that may include reduced efficiency of α-synuclein degradation by calpain I and 20S proteasome (Hodara et al., 2004). Lastly, the interaction of α-synuclein with other amyloidogenic proteins such as tau (Giasson et al., 2003) or amyloid-β (Masliah et al., 2001) may synergistically drive fibrillization of these proteins. For example, amyloid-β peptides were shown to promote intraneuronal α-synuclein aggregation in cell cultures and transgenic mice expressing both α-synuclein and amyloid-β neuronally developed more α-synuclein-immunoreactive inclusions than singly α-synuclein transgenic mice. These double transgenic mice also exhibited motor deficits and impaired learning and memory before mice expressing transgenic α-synuclein only (Masliah et al., 2001). A clear relevance of this stimulatory effect on α-synuclein aggregation applies to patients with clinical and pathological features of both PD and Alzheimer’s disease (e.g. those with the Lewy body variant of Alzheimer’s disease).
While α-synuclein is seen to undergo aggregation and post-translational modifications, and these events may lead to its toxicity to neurons, the effects of α-synuclein responsible for causing cell death are not yet clear. Nevertheless, several theories have been put forth to explain α-synuclein toxicity and are briefly outlined here. As already mentioned, α-synuclein oligomers can form pore-like structures and annular rings of α-synuclein were previously observed in brains of patients with multiple system atrophy, a synucleinopathy. Neural cells expressing mutant forms of α-synuclein (A53T and A30P) exhibited non-selective cation pores that increased both basal and depolarization-induced intracellular Ca2+ levels (Furukawa et al., 2006). Furthermore, cells expressing mutant α-synuclein were more sensitive to iron generated reactive oxygen species, unless treated with Ca2+-chelating agents, suggesting that elevated intracellular Ca2+ levels were responsible for the increased vulnerability of these cells to toxic insults. Given that a portion of α-synuclein has been observed to localize to mitochondrial membranes of dopamine neurons (Li et al., 2007; Nakamura et al., 2008), and the central involvement of mitochondria in PD pathogenesis, an obvious question is whether such pores form in mitochondrial membranes to promote mitochondrial dysfunction. Overexpression of α-synuclein in cells was reported to induce abnormal morphology and dysfunction of mitochondria together with increased oxidative stress (Hsu et al., 2000). Since there was little change in cell viability, this suggests that mitochondrial deficits were not secondary to cell death, but a direct consequence of α-synuclein overexpression.
Another potential mechanism of α-synuclein toxicity supported by the interaction of α-synuclein with synaptic vesicles is that increased or mutant α-synuclein expression interferes with synaptic neurotransmission. Wild type or A30P α-synuclein was shown to impair catecholamine release from chromaffin and PC12 cells associated with an accumulation of ‘docked’ vesicles at the presynaptic membrane (Larsen et al., 2006). Furthermore, α-synuclein overexpression to levels predicted to result from gene multiplication impaired neurotransmitter release in mice through a mechanism involving reduced size of the recycling vesicle pool (Nemani et al., 2010). Uptake of dopamine into synaptic vesicles may also be perturbed by α-synuclein. Mutant α-synuclein overexpression was reported to downregulate the vesicular monoamine transporter 2 which may lead to increased cytosolic levels of dopamine (lotharius et al., 2002). Pathogenic species of α-synuclein are not good substrates for proteasomal degradation and aggregates can directly bind to 20/26S proteasomal subunits inhibiting proteolytic activity (Snyder et al., 2003). α-Synuclein may also affect protein degradation through inhibiting lysosomal function (stefanis et al., 2001) and chaperone-mediated autophagy (Cuervo et al., 2004). Recent data suggests that chaperone-mediated autophagy is important in the regulation of the neuronal survival factor MEF2D (myocyte enhancer factor 2D) and that α-synuclein expression can disrupt this leading to cell death (Yang et al., 2009).
Hence, α-synuclein aggregates appear to exert toxic effects on numerous cell functions. The relative contributions of these effects to neuronal cell death is not well understood and may vary depending on cell type and other circumstances such as the type and amount of α-synuclein pathogenic species present. Teasing apart primary effects of α-synuclein toxicity from secondary will be important for identifying therapeutic targets for preventing cell death (Cookson, 2009).
Leucine-rich repeat kinase 2 (LRRK2)
Since the first identification of pathogenic LRRK2 mutations in 2004 (Paisan-Ruiz et al., 2004; Zimprich et al., 2004a; Zimprich et al., 2004b), mutations in this gene are now the most common known cause of familial PD worldwide (Webber and West, 2009). Autosomal dominantly inherited LRRK2 mutations exist in families from diverse ethnic backgrounds and mostly give rise to PD phenotypes that are highly similar to those of typical late-onset PD. This suggests that understanding the effects of mutant LRRK2 on disease pathogenesis has the potential to generate substantial insight into sporadic PD mechanisms. Interestingly, despite consistency of clinical phenotypes, LRRK2 mutant carriers can exhibit diverse neuropathology occasionally lacking Lewy bodies, even between individuals with the same mutation (Zimprich et al., 2004; Gaig et al., 2007).
LRRK2 encodes a large, 280 KDa protein with initial studies indicating potential roles in cytoskeletal dynamics, protein translation control, mitogen-activated protein kinase pathways, and apoptotic pathways. LRRK2 contains numerous domains, namely ankyrin-like repeats, leucine-rich repeats, COR (C-terminal of ROC) WD-40 domain and a catalytic GTPase/kinase region. Interestingly, LRRK2 kinase activity appears to require a functional GTP-ase domain (West et al., 2007) and possibly LRRK2 dimer formation (Sen et al., 2009). LRRK2 undergoes autophosphorylation and phosphorylates a number of protein substrates in vitro. Analysis of the human kinome indicates that the kinase domain of LRRK2 and its homolog LRRK1 are most similar in sequence to the receptor-interacting protein kinase and death-domain containing interleukin receptor-associated kinase families and to a lesser extent, MAP (mitogen-activated protein) kinase kinase kinases. Several of the most clear and common pathogenic mutations (G2019S, I2020T, R1441C/G) are found in the central catalytic region and may result in increased kinase activity in vitro (West et al., 2007) although it is important to note that not all PD-associated LRRK2 mutations increase kinase activity and only the G2019S mutation has consistently been found to increase kinase activity to date (Greggio and Cookson, 2009).
Much effort is currently focused on attempting to identify kinase substrates and pathogenic mechanisms linked to altered kinase activity. A role for LRRK2 in protein translation control has been put forth by the identification of the translational inhibitor 4E-BP (eukaryotic initiation factor 4E-binding protein) as a LRRK2 substrate both in vitro and in a Drosophila model (Imai et al., 2008; Tain et al., 2009). 4E-BP in its non-phosphorylated state interacts with eIF4E (eukaryotic initiation factor 4E), preventing activity of eIF4E within the protein translation machinery thereby inhibiting protein translation (Khalegpour et al., 1999). Phosphorylation of 4E-BP disrupts its interaction with eIF4E and stimuli that affect 4E-BP phosphorylation such as oxidative stress and activation of the mTOR (mammalian target of rapamycin) pathway can impact protein translation indicating that 4E-BP phosphorylation is associated with increased protein translation. Overexpression of human LRRK2 in mammalian cells or a Drosophila ortholog (dLRRK) in flies was shown to result in increased 4E-BP phosphorylation at two threonine sites (Thr37/Thr46) leading to secondary phosphorylation by additional kinases at other sites including Ser65/Thr70 (Imai et al., 2008). The authors also reported that RNAi-mediated silencing of LRRK2 in cells or loss-of-function dLRRK mutation in flies led to a decrease in 4E-BP phosphorylation at these sites supporting the possibility that 4E-BP is a kinase substrate of LRRK2. Finally, the authors showed that dopamine neuron pathology associated with dLRRK mutations was suppressed via overexpression of 4E-BP suggesting that increasing 4E-BP activity might attenuate PD pathology. Another recent study in Drosophila has strengthened a potential link between LRRK2, 4E-BP activity and PD pathology (Tain et al., 2009). Increased 4E-BP activity resulting from loss of dLRRK or administration of rapamycin was sufficient to suppress pathology in PINK1 (PTEN-induced putative kinase 1) and Parkin mutants raising the possibility that an involvement of general protein translation in PD pathology might be relevant to other PD-associated genes.
Another candidate substrate for LRRK2 kinase activity is moesin (Jaleel et al., 2007). Moesin is a member of the ERM (ezrin/radixin/meosin) protein family whose primary role is to anchor the cytoskeleton to the plasma membrane. Jaleel et al. found that Moesin could be phosphorylated by LRRK2 at Thr558 and to a lesser extent at Thr526. One caveat is moesin phosphorylation could only be observed after denaturating moesin via heating and even then, phosphate was minimally incorporated suggesting that moesin may be a weak kinase substrate of LRRK2. Despite this, a recent study on developing neurons supports the possibility that moesin is a LRRK2 substrate in vivo (Parisiadou et al., 2009). Phosphorylated ERM protein accumulated more in developing neurons from G2019S LRRK2 transgenic mice and less in LRRK2 knock-out mice than controls (Parisiadou et al., 2009). Furthermore, the extent of ERM phosphorylation correlated negatively with neurite outgrowth suggesting that LRRK2 mutations may perturb normal neuronal development.
Based on sequence similarity between LRRK2 and MAPKK kinases, which are involved in the MAPK signaling pathway and important to cellular stress responses, Gloeckner et al, recently used in vitro studies to probe MAPK kinases as potential substrates for LRRK2 kinase activity (Gloeckner et al., 2009). These studies revealed phosphorylation of MKK3, -4, -6 and -7 by LRRK2 and moreover, that PD-linked G2019S or I2020T mutations in LRRK2 exhibit increased phosphotransferase activity as well as enhanced autophosphorylation. Whether these changes are due to LRRK2 kinase activity is not clear since the authors did not use kinase-dead versions of LRRK2 as a control. Since phosphorylation of MAPK kinases within their activation loop is linked to increased downstream phosphorylation of c-Jun N-terminal kinase (JNK) and c-Jun, it might be expected that increased LRRK2 kinase activity would lead to higher phosphorylated JNK and/or c-Jun levels. However this is inconsistent with prior studies in cell system (West et al., 2007) in which LRRK2 overexpression does not appear to increase levels of phosphorylated JNK or c-Jun. Hence, the simplest explanation here is that there exists disparity between kinase activity observed in vitro and that found in intact cells.
For any putative LRRK2 kinase substrate identified in vitro, it will be imperative to determine its relevance as a substrate in vivo where conditions affecting protein localization, activity and structure are far more complicated. Moreover, since existing studies largely support an increase in kinase activity following certain mutations in LRRK2 (e.g. G2019S), it will be important to assess whether the phosphorylation of any putative substrate is enhanced in the presence of mutant LRRK2 relative to wild-type LRRK2.
Numerous studies show that expression of mutant LRRK2 causes cell death. Overexpression of mutant LRRK2 in primary neuronal cultures leads to rapid cell death possibly by apoptosis, while comparable expression of wild-type LRRK2 has only subtle effects on cell viability (Smith et al., 2005; Greggio et al., 2006; MacLeod et al., 2006; Smith et al., 2006; Iaccarino et al., 2007; West et al., 2007; Ho et al., 2009.). A proposed link between increased LRRK2 kinase activity and neuronal death in PD requires further investigation in vivo, although a dominant mode of inheritance (consistent with a toxic-gain-of-function) and preliminary studies in cell culture are supportive of this. Multiple investigators have discovered that pathogenic LRRK2 mutants engineered to ablate kinase activity are substantially less toxic in cultured cells than kinase-active counterparts (West et al., 2007; Gregio et al., 2006; Smith et al., 2006) indicating that kinase activity contributes to cellular toxicity. One caveat is that not all pathogenic LRRK2 mutations appear to result in elevated kinase activity based on measurements of autophosphorylation or generic kinase substrate phosphorylation. A possibility to consider here is that pathogenic LRRK2 mutations might alter kinase activity towards specific substrates that are key to LRRK2-mediated toxicity but not a universal increase in kinase activity to all substrates. Perhaps identification of true in vivo LRRK2 substrates will permit definitive assessment of the role of kinase activity in LRRK2-mediated PD pathogenesis. Despite considerable recent progress, much remains to be understood about the contribution of mutant LRRK2 to PD pathogenesis. Given the pervasiveness of these mutations in PD, unlocking these mysteries will surely have broad implications in understanding fundamental mechanisms of PD development and for therapeutic strategies aimed at LRRK2.
Recessive mutations
Compelling evidence implicates loss-of-function mutations in three genes; Parkin, PINK1 (PTEN-induced putative kinase 1) and DJ-1, in autosomal recessive PD and some sporadic cases (Dodson and Guo, 2007). Recent work has demonstrated key roles for all three gene products in preserving mitochondrial function and protecting against reactive oxygen species. This underscores the central role of mitochondrial dysfunction and oxidative stress in PD pathogenesis, reinforcing previous studies linking sporadic PD cases with mitochondrial poisons such as MPTP and paraquat. Recessively inherited mutations in a fourth gene, ATP13A2, are linked to Kufor-Rakeb syndrome, a pallidopyramidal syndrome featuring Parkinsonism together with behavioral and cognitive disorders (Najim al-Din et al., 1994). Large-scale association studies showed that ATP13A2 genetic variants do not segregate with PD within families indicating that these mutations likely do not contribute to disease risk (Vilarino-Guell et al., 2009).
Parkin
Mutations in Parkin were originally linked with autosomal recessive juvenile-onset Parkinsonism (AR-JP) in three unrelated Japanese families in 1997 (Kitada et al., 1998). Homozygous loss-of-function or compound heterozygous Parkin mutations account for approximately 50% of all familial early-onset cases of PD with point mutations being the most frequent genetic lesion, and deletions, duplications and exonic rearrangements also contributing to Parkin-linked PD (Mata et al., 2004). Although the majority of Parkin-associated PD is inherited in an autosomal recessive manner, there is some evidence to suggest that Parkin haploinsufficiency due to polymorphisms in the promoter or coding regions may associate with increased susceptibility to late-onset PD (Farrer, 2006). Clinically, patients with Parkin mutations are L-Dopa responsive and exhibit slower disease progression often accompanied by early-onset dystonia. Interestingly, Parkin-linked disease may be associated with an absence of Lewy body pathology, a finding that is inconsistent with these being causal in disease pathogenesis. However, Lewy body pathology is observed in some cases of Parkin-linked PD.
Parkin encodes a protein of 465 amino acids consisting of an N-terminal ubiquitin-like (UBL) domain, central linker region and a C-terminal RING domain containing two RING-finger domains (Moore et al., 2005). Parkin demonstrates E3 ubiquitin protein ligase activity, tagging protein lysine residues with ubiquitin. Attachment of Poly-ubiquitin chains to proteins via lysine K48 usually targets them for degradation via the 26S proteasome whereas monoubiquitylation and poly-ubiquitination through K48 or K63 can influence other pathways such as intraellular signaling, DNA repair, endocytosis, transcriptional regulation and protein trafficking (Mukhopadhyay et al., 2007; Sandebring et al., 2009).
While the majority of the Parkin pool is localized to the cytoplasm and vesicular structures (Shimura et al., 2000; kubo et al., 2001), a portion is found associated with the outer mitochondrial membrane (Darios et al., 2003). Several recent studies on Drosophila and mice have revealed a key role for Parkin in regulating mitochondrial function and protection against oxidative stress (Greene et al., 2003; Park et al., 2006; Yang et al., 2006; Deng et al., 2008; Palacino et al., 2004), which is discussed further in a subsequent section. Most mutations in Parkin appear to impair its E3 ligase activity or interactions with E2 enzymes such as UbcH7 and UbcH8 (Shimura et al., 2000; Zhang et al., 2000). Although it is not definitively known that loss of Parkin’s E3 ligase activity is sufficient for development of PD, a prominent hypothesis is that Parkin mutations lead to toxic accumulation of its substrates due to impaired ubiquitin-proteasome function (Dodson and Guo, 2007). Through extensive in vitro investigations, a number of putative Parkin substrates have been identified including the aminoacyl-tRNA synthase cofactor p38 (Corti et al., 2003), far upstream element-binding protein-1 (Ko et al., 2006) cyclin E (Staropoli et al., 2003), the parkin-associated endothelin receptor-like receptor (Pael-R) (Imai et al., 2001), synphilin-1 (Chung et al., 2001), synaptotagmin XI (Huynh et al., 2003), CDCrel-1 (Zhang et al., 2001) and alpha/beta-tubulin (Ren 2003). From this set, only the p38 subunit of aminoacyl tRNA synthase and far upstream element-binding protein-1 have been demonstrated to accumulate in the brains of both patients with Parkin mutations and Parkin-null mice (Ko et al., 2005; Ko et al., 2006) highlighting the importance of determining the authenticity of all other putative substrates in vivo. Further studies will also be required to determine the roles of these substrates in PD pathogenesis.
PINK1
A second locus for autosomal recessive early-onset Parkinsonism was discovered initially in a large Sicilian family mapped to the short-arm of chromosome 1p35-p36 (Valente et al., 2001) and later extended to eight additional families from four European countries (Valente et al., 2002). Subsequent work revealed that within this locus, mutations in PINK1 are linked to PD (Valente et al., 2004). Atypical clinical phenotypes have been reported in PINK1-linked PD, including dystonia, psychiatric disturbances and sleep benefit (Hatano et al., 2004; Tan and Dawson, 2006; Valente et al., 2004). PINK1 is a cytosolic and mitochondrially-localized protein kinase which contains an N-terminal mitochondrial targeting sequence followed by a predicted transmembrane domain, suggesting that PINK1 may be an integral transmembrane protein possibly in the mitochondrial inner membrane with which it closely associates (Silvestri et al., 2005). However, a recent study indicates that the kinase domain of PINK1 faces out into the cytosol (Zhou et al., 2008). Existing evidence from cell and animal models suggests that PINK1 is important for protection against cell death related to mitochondrial dysfunction and oxidative stress (Exner et al., 2007; Clark et al., 2006; Deng et al., 2008;, Hoepken et al., 2007; Wood-Kaczmar et al., 2008). Although several PD-associated mutations reduce PINK1 kinase activity, it is not clear whether loss of kinase activity is required for PD pathogenesis, since disease-associated mutations are found both within and outside of the kinase domain. It seems, however, that kinase activity is required for the protective function of PINK1 against pro-apoptotic agents since staurosporine-induced cell death was substantially reduced by wild type PINK1 overexpression whereas an equivalent increase in kinase-inactive PINK1 mutant had no protective effect (Petit et al., 2005). Additionally, recent in vivo data suggests that phosphorylation of the mitochondrial chaperone TRAP1 (TNF receptor-associated protein 1) by PINK1 is important for the protective action of PINK1 against oxidative stress-induced cell death (Pridgeon et al., 2007). The authors also reported that the ability of PINK1 to phosphorylate TRAP1 is impaired by PD-associated G309D, L347P and W437X PINK1 mutations suggesting a possible connection between these mutations, impaired PINK1 substrate phosphorylation and cell death. PINK1 was recently demonstrated to regulate mitochondrial Ca2+ efflux in mammalian neurons and loss of PINK1 was associated with mitochondrial Ca2+ overload and consequent respiration inhibition via increased reactive oxygen species generation and opening of the mitochondrial permeability transition pore (Ghandi et al., 2009).
DJ-1
Mutations in DJ-1 were originally associated with early-onset PD in 2003 (Bonifati et al., 2003) and are known to be very rare, accounting for less than 1% of early-onset cases. The DJ-1 protein is a member of the ThiJ/PfpI family of molecular chaperones that are induced by oxidative stress (Dodson and Guo, 2007). Consistent with this, DJ-1 deficiency in Drosophila increases cell death caused by ROS-generating species linked to PD in humans (Muelener et al., 2005). Additional studies revealed that a conserved cysteine residues in human (Canet-Aviles et al., 2004), mice (Andres-Mateos et al., 2007) and Drosophila (Meulener et al., 2006) DJ-1 is modified under conditions of oxidative stress and this modification is necessary for the protective effects of DJ-1. Furthermore, evidence in mice indicates that DJ-1 acts as an atypical peroxiredoxin-like peroxidase to scavenge H2O2 produced by mitochondria (Andres-Mateos et al., 2007). Accordingly, DJ-1 knock-out mice exhibit elevated mitochondrial H2O2 and reduced activity of mitochondrial aconitase activity levels although the pathological consequences of this are uncertain since there was an absence of dopaminergic neuron degeneration in these mice (Andres-Mateos et al., 2007). Hence, DJ-1 may act as a cellular redox-sensor, which becomes activated under oxidative conditions to provide protection against ROS-mediated damage. Numerous functions have been ascribed to DJ-1, including protease, transcriptional coactivator and molecular chaperone functions, although which of these, if any, contribute to its protective role in PD remains to be determined.
Impact of genetic research on understanding mechanisms of PD pathogenesis
Genetic studies over the last decade have resulted in the identification of pathogenic gene variants that underlie familial PD and in some cases contribute to the lifetime risk of developing sporadic PD. By linking these genes to PD and understanding the biological roles of the products they encode, a wealth of insight has been generated into mechanisms of PD pathogenesis. These pathogenic genes also yield understanding of possible relationships between PD and disorders with overlapping clinical or neuropathological features that may share common mechanisms. For example, neuronal α-synuclein accumulation often in Lewy bodies can be found in a number of neurodegenerative disease including PD, dementia with lewy bodies, multiple system atrophy and pure autonomic failure (Kramer and Schulz-Schaeffer, 2009; Goldstein and Sewell, 2009; Kövari et al., 2009) suggesting that α-synuclein aggregation is a common mechanism in these diseases. Genetic studies have in some instances corroborated pathogenic mechanisms indicated by environmental factors such as a central involvement of oxidative stress and mitochondrial dysfunction in PD etiology. Additionally, genetic studies have implicated protein mishandling due to dysfunction of the ubiquitin proteasome system in development of PD. Since perturbations in the ubiquitin proteasome system or mitochondrial function both lead to the same pathological outcome, i.e. loss of dopamine neurons and development of PD, it is likely that an important relationship exists between these functions that converges on dopamine neuron viability. The model presented in Figure 3 illustrates molecular pathways in PD pathogenesis implicated by genetic studies and how these pathways may be connected.
Mitochondrial dysfunction and oxidative stress
A role for mitochondrial dysfunction in PD pathogenesis is supported by studies on a number of gene products linked to PD. Knock-out studies in animals clearly indicate that two PD-linked genes, Parkin and PINK1, have key roles in preserving mitochondrial function and that loss-of-function mutations in these genes can lead to PD. Drosophila Parkin null mutants exhibit mitochondrial pathology marked by enlarged size and rarified cristae, as well as enhanced sensitivity to oxidative stress, apoptotic muscle degeneration, significant (albeit slight) degeneration of a subset of dopamine neurons and reduced life span (Greene et al., 2003; Pesah et al., 2004). Parkin null mice, which exhibit nigrostriatal deficits without nigral degeneration, do not have gross changes in striatal mitochondrial morphology but do experience mitochondrial dysfunction evidenced by reduced activity of multiple respiratory chain complexes along with decreased antioxidant capacity that results in increase oxidative damage (Palacino et al., 2004). Intriguingly, complete loss of PINK1 function in flies led to phenotypes that are highly similar to Parkin-null flies (Clark et al., 2006). The subtle neuronal death observed in PINK1 or Parkin mutants can be prevented by overexpression of antioxidants (Wang et al., 2006; Whitworth et al., 2005) supporting the contention that oxidative stress is important to PD pathology. Indeed, oxidative damage to cell macromolecules is consistently observed in the substantia nigra of PD patients (Jenner, 2003) and elevated reactive oxygen species generation may occur as a result of impaired respiratory chain function.
Several lines of evidence suggest a genetic interaction between PINK1 and Parkin. For example, overexpression of Parkin rescued all phenotypes resulting from PINK1 deficiency although a reciprocal rescue effect of PINK1 overexpression in Parkin mutants was not found (Park et al., 2006). Similarly, loss of mitochondrial potential, abnormal mitochondrial morphology and reduced cristae seen in HeLa cells with PINK1 deficits can be rescued by increased expression of wild-type but not PD-associated mutant Parkin (Exner et al., 2007). These lines of evidence have led to the hypothesis that Parkin acts downstream of PINK1 to preserve mitochondrial function (Dodson and Guo, 2007). Recent studies in Drosophila have suggested a possible link between PINK1, Parkin and mitochondrial function by demonstrating that both appear to regulate mitochondrial dynamics by either promoting fission or inhibiting fusion of the organelle (Poole et al., 2008; Deng et al., 2008). Genetic manipulations of the fly mitofusin homolog (Mfa), Opa1 (optic atrophy 1) or drp1 in favor of mitochondrial fission are sufficient to rescue mitochondrial pathology, cell death and muscle degeneration in Parkin or PINK1 mutants (Deng et al., 2008). However, these data and their relevance to human disease should be interpreted cautiously due to discrepancies in mitochondrial morphology abnormalities that exist between fly and mammalian model systems. Nonetheless, impaired mitochondrial respiration has been detected in peripheral tissues taken from human PD patients with PINK1 (Hoepken et al., 2007) or Parkin mutations (Muftuoglu et al., 2004) suggesting that the mitochondrial dysfunction observed in animal models may be relevant to human disease. Hence, considerable evidence supports a role for PINK1 and Parkin in protecting against cell death due to mitochondrial dysfunction and oxidative stress.
Mutations and multiplications in SNCA may also promote mitochondrial dysfunction leading to neuronal death. Mitochondrial pathology following MPTP exposure is exacerbated in α-synuclein transgenic mice (Song et al., 2004) and neuronal cells expressing mutant α-synuclein showed a selective increase in mitochondrial dysfunction and apoptotic cell death when treated with a proteasome inhibitor (Tanaka et al., 2001). Inhibition of the mitochondrial respiratory chain complex I, which is caused by pesticides and certain other environmental toxins, commonly leads to the accumulation of α-synuclein-positive inclusions suggesting that α-synuclein aggregation may be a consequence of mitochondrial dysfunction (Betarbet et al., 2000; Manning-Bog et al., 2002). Interestingly, α-synuclein knock-out mice are resistant to the toxic effects of MPTP on neurons while α-synuclein transgenic mice are more sensitive indicating that α-synuclein might be necessary for neuronal toxicity associated with impaired complex I activity (Dauer et al., 2002; Song et al., 2004). Taken together, this evidence suggests that α-synuclein, likely in aggregate form, may have a toxic role both in causing mitochondrial dysfunction and in the deleterious effects resulting from it. Future studies will hopefully elucidate the nature of the relationship between α-synuclein and mitochondrial dysfunction.
Ubiquitin-proteasome system impairment
Compelling evidence from genetic studies links ubiquitin-proteasome system (UPS) dysfunction to development of PD. Mutations in Parkin associated with the disease are widely believed to cause impairment of UPS function with consequent accumulation of potentially cytotoxic proteins that may result in death of dopamine neurons (Chung et al., 2001; Moore et al., 2005). In support of this, proteasome inhibitors are found to cause a number of phenotypes that closely recapitulate those in PD when injected into rats (McNaught et al., 2004) and genetic knock-out of a 26 proteasomal subunit in mice impairs ubiquitin-mediated protein degradation and leads to intraneuronal Lewy-like inclusion formation and substantial degeneration in the nigrostriatal pathway (Bedford et al., 2008). The accumulation of aggregated proteins such as α-synuclein in nigral neuron Lewy bodies in sporadic PD also indicates mishandling of protein turnover perhaps due to impaired UPS function. As previously mentioned, Lewy bodies are often absent in certain familial forms of PD suggesting that they may not be neuropathological in PD but are, instead, a hallmark of protein aggregation and therefore still supportive of a role for protein mishandling in PD pathology. Aggregated α-synuclein has been shown to strongly bind to and inhibit the 26S proteasome in vitro (Snyder et al., 2003) and overexpression of mutant α-synuclein in cells was observed to decrease proteasome function and cause selective toxicity to catecholaminergic neurons (Petrucelli et al., 2002). Interestingly, co-expression of Parkin was reported to reduce sensitivity of α-synuclein-expressing cells to proteasome inhibitors suggesting that Parkin protects against mutant α-synuclein-mediated toxicity. Similarly, overexpression of the molecular chaperone Hsp70 in flies (Auluck et al., 2002) or transgenic expression of the yeast chaperone Hsp104 in rats (Lo Bianco et al., 2008) prevents degeneration of dopamine neurons caused by expression of mutant α-synuclein indicating that chaperones function may protect against PD pathology related to α-synuclein. Consistent with this, Lewy bodies examined from postmortem human brain were found to contain molecular chaperones (Auluck et al., 2002), which may indicate that in the PD brain, these fail to effectively prevent protein aggregation at physiological levels. Further investigations assessing the ability of molecular chaperones to prevent neuronal toxicity associated with α-synuclein aggregation will hopefully lead to new therapeutic strategies for PD.
Conclusion
Although the majority of PD is sporadic, the discovery of rare familial forms of PD and subsequent identification of disease-causing mutations have provided extremely valuable tools to begin to understand the cellular network of dysfunction that ultimately results in neuronal demise and manifestation of disease phenotypes. Through the generation of cellular and small animal models expressing PD-linked genetic mutations, new insights into mechanisms of disease pathogenesis have been achieved. Further study will hopefully lead to new disease-modifying treatments for PD that will provide more then temporary symptomatic relief.
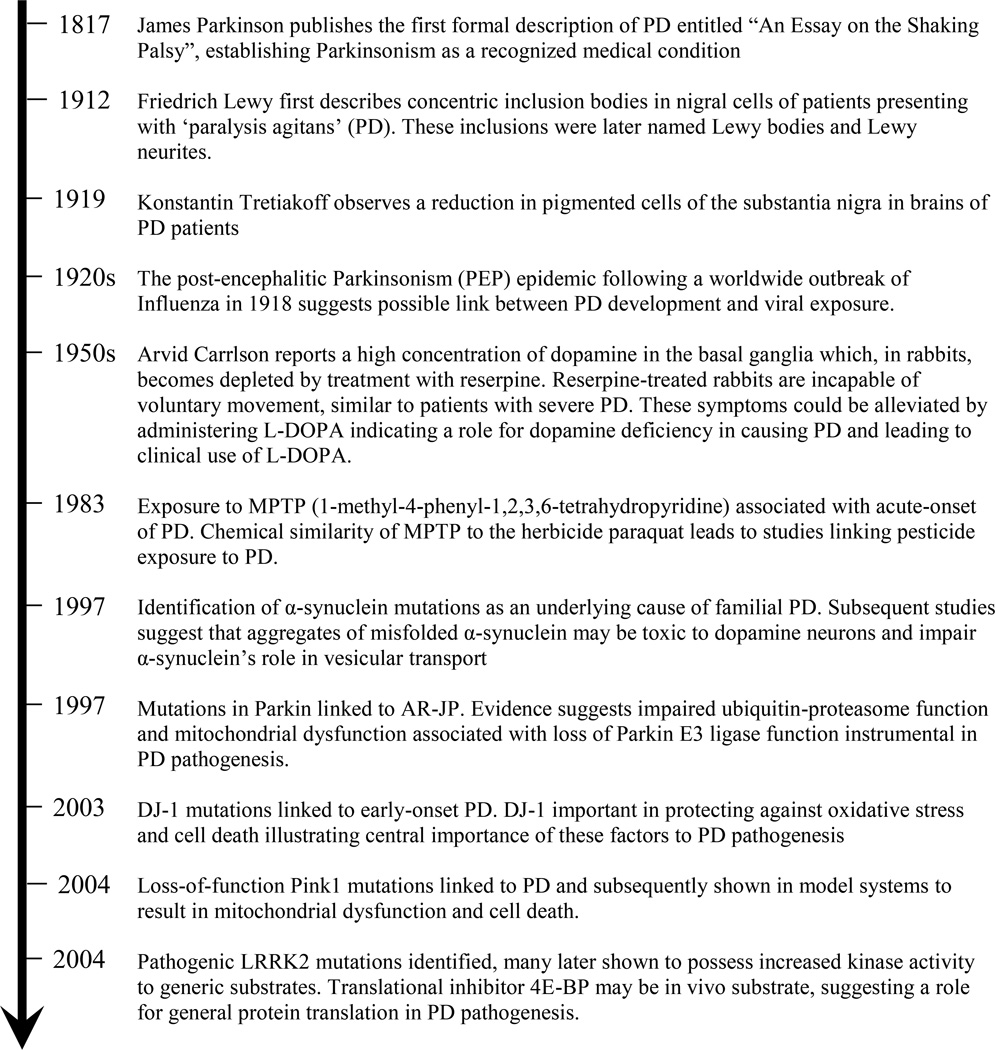
Figure 1. Timeline of key discoveries in PD pathogenesis.
Parkinson’s disease was first formally described in 1817 by James Parkinson. From then until the late twentieth century, advances were made in describing the pathological features of PD and in understanding possible causes of the disease, such as exposure to pesticides and MPTP. The recent discovery of multiple genetic causes of PD has generated insight into novel mechanisms of PD etiology. Studies using genetic models of PD will, no doubt, continue to advance our understanding of disease pathogenesis.
Figure 2. Pathogenic mechanisms implicated by genetic studies of PD.
This model links genetic mutations (autosomal recessive mutations in blue boxes and autosomal dominant mutations in purple boxes) to neurodegeneration via pathways involving mitochondrial dysfunction, oxidative stress and impaired ubiquitin-proteasome function. Loss-of-function mutations in PINK1 or Parkin cause PD possibly through a mechanism involving mitochondrial pathology and dysfunction. Deleterious effects of mitochondrial dysfunction include reduced ATP generation and oxidative stress due to elevated ROS generation. Loss of Parkin’s E3 ubiquitin ligase activity, may also lead to dopamine neuron toxicity via impaired ubiquitin-proteasome function and accumulation of Parkin’s substrates. Loss of DJ-1 antioxidant function may promote neuronal oxidative stress, as might reduced respiratory chain function and elevated intracellular calcium influx via pores created by α-synuclein oligomers. LRRK2 mutations might be linked to PD through altered protein translation further supporting a role for protein turnover in PD pathogenesis.
Table. Genes underlying familial PD.
Genes with variants that segregate with PD are listed. The inheritance pattern, typical age of disease-onset and characteristic phenotypes observed are described.
| Locus | Gene | Inheritance pattern |
Typical age of onset |
Phenotype characteristics |
|---|---|---|---|---|
| PARK1 and PARK4 | SNCA | Dominant | 24–65 | Parkinsonism (progression related to gene dose) with common dementia and autonomic dysfunction |
| PARK2 | Parkin | Recessive | 16–72 | Slow-progressing Parkinsonism |
| PARK6 | PINK1 | Recessive | 20–40 | Slow-progressing Parkinsonism |
| PARK7 | DJ1 | Recessive | 20–40 | Slow-progressing Parkinsonism sometimes with behavioral disturbances |
| PARK8 | LRRK2 | Dominant | 32–79 | Classic PD |
Acknowledgements
This work was supported by grants from NIH/NINDS P50 NS38377, NS054207. T.M.D. is the Leonard and Madlyn Abramson Professor in Neurodegenerative Diseases.
List of Abbreviations
- PD
Parkinson’s Disease
- SNARE
soluble NSF attachment protein receptors
- MEF2D
myocyte enhancer factor 2D
- LRRK2
leucine-rich repeat kinase 2
- eIF4E
eukaryotic initiation factor 4E
- 4E-BP
eukaryotic initiation factor 4E binding protein
- ERM
ezrin/radixin/meosin
- MAPK
mitogen-activated protein kinase
- MAPKK
mitogen-activated protein kinase kinase
- JNK
c-Jun N-terminal kinase
- PINK1
PTEN-induced putative kinase 1
- TRAP1
TNF receptor-associated protein 1
- MPTP
1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine
References
- Ahlskog JE. Parkin and PINK1 parkinsonism may represent nigral mitochondrial cytopathies distinct from Lewy body Parkinson's disease. Parkinsonism Relat Disord. 2009;15(10):721–727. doi: 10.1016/j.parkreldis.2009.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andres-Mateos E, Perier C, Zhang L, Blanchard-Fillion B, Greco TM, Thomas B, et al. DJ-1 gene deletion reveals that DJ-1 is an atypical peroxiredoxin-like peroxidase. Proc Natl Acad Sci U S A. 2007;104(37):14807–14812. doi: 10.1073/pnas.0703219104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen W. Inheritance of the shaking palsy. Archives of Internal Medicine. 1937;60:424–436. [Google Scholar]
- Auluck PK, Chan HY, Trojanowski JQ, Lee VM, Bonini NM. Chaperone suppression of alpha-synuclein toxicity in a Drosophila model for Parkinson's disease. Science. 2002;295(5556):865–868. doi: 10.1126/science.1067389. [DOI] [PubMed] [Google Scholar]
- Bedford L, Hay D, Devoy A, Paine S, Powe DG, Seth R, et al. Depletion of 26S proteasomes in mouse brain neurons causes neurodegeneration and Lewy-like inclusions resembling human pale bodies. J Neurosci. 2008;28(33):8189–8198. doi: 10.1523/JNEUROSCI.2218-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell J, Clark AJ. A pedigree of paralysis agitans. Annals of Eugenics. 1926;1:455–462. [Google Scholar]
- Betarbet R, Sherer TB, MacKenzie G, Garcia-Osuna M, Panov AV, Greenamyre JT. Chronic systemic pesticide exposure reproduces features of Parkinson's disease. Nat Neurosci. 2000;3(12):1301–1306. doi: 10.1038/81834. [DOI] [PubMed] [Google Scholar]
- Bonifati V, Rizzu P, van Baren MJ, Schaap O, Breedveld GJ, Krieger E, et al. Mutations in the DJ-1 gene associated with autosomal recessive early-onset parkinsonism. Science. 2003;299(5604):256–259. doi: 10.1126/science.1077209. [DOI] [PubMed] [Google Scholar]
- Bonini NM, Giasson BI. Snaring the function of alpha-synuclein. Cell. 2005;123(3):359–361. doi: 10.1016/j.cell.2005.10.017. [DOI] [PubMed] [Google Scholar]
- Canet-Aviles RM, Wilson MA, Miller DW, Ahmad R, McLendon C, Bandyopadhyay S, et al. The Parkinson's disease protein DJ-1 is neuroprotective due to cysteine-sulfinic acid-driven mitochondrial localization. Proc Natl Acad Sci U S A. 2004;101(24):9103–9108. doi: 10.1073/pnas.0402959101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandra S, Fornai F, Kwon HB, Yazdani U, Atasoy D, Liu X, et al. Double-knockout mice for alpha- and beta-synucleins: effect on synaptic functions. Proc Natl Acad Sci U S A. 2004;101(41):14966–14971. doi: 10.1073/pnas.0406283101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandra S, Gallardo G, Fernandez-Chacon R, Schluter OM, Sudhof TC. Alpha-synuclein cooperates with CSPalpha in preventing neurodegeneration. Cell. 2005;123(3):383–396. doi: 10.1016/j.cell.2005.09.028. [DOI] [PubMed] [Google Scholar]
- Chartier-Harlin MC, Kachergus J, Roumier C, Mouroux V, Douay X, Lincoln S, et al. Alpha-synuclein locus duplication as a cause of familial Parkinson's disease. Lancet. 2004;364(9440):1167–1169. doi: 10.1016/S0140-6736(04)17103-1. [DOI] [PubMed] [Google Scholar]
- Chung KK, Dawson VL, Dawson TM. The role of the ubiquitin-proteasomal pathway in Parkinson's disease and other neurodegenerative disorders. Trends Neurosci. 2001;24(11 Suppl):S7–S14. doi: 10.1016/s0166-2236(00)01998-6. [DOI] [PubMed] [Google Scholar]
- Chung KK, Zhang Y, Lim KL, Tanaka Y, Huang H, Gao J, et al. Parkin ubiquitinates the alpha-synuclein-interacting protein, synphilin-1: implications for Lewy-body formation in Parkinson disease. Nat Med. 2001;7(10):1144–1150. doi: 10.1038/nm1001-1144. [DOI] [PubMed] [Google Scholar]
- Clark IE, Dodson MW, Jiang C, Cao JH, Huh JR, Seol JH, et al. Drosophila pink1 is required for mitochondrial function and interacts genetically with parkin. Nature. 2006;441(7097):1162–1166. doi: 10.1038/nature04779. [DOI] [PubMed] [Google Scholar]
- Cole NB, Murphy DD, Lebowitz J, Di Noto L, Levine RL, Nussbaum RL. Metal-catalyzed oxidation of alpha-synuclein: helping to define the relationship between oligomers, protofibrils, and filaments. J Biol Chem. 2005;280(10):9678–9690. doi: 10.1074/jbc.M409946200. [DOI] [PubMed] [Google Scholar]
- Conway KA, Harper JD, Lansbury PT. Accelerated in vitro fibril formation by a mutant alpha-synuclein linked to early-onset Parkinson disease. Nat Med. 1998;4(11):1318–1320. doi: 10.1038/3311. [DOI] [PubMed] [Google Scholar]
- Conway KA, Lee SJ, Rochet JC, Ding TT, Williamson RE, Lansbury PT., Jr Acceleration of oligomerization, not fibrillization, is a shared property of both alpha-synuclein mutations linked to early-onset Parkinson's disease: implications for pathogenesis and therapy. Proc Natl Acad Sci U S A. 2000;97(2):571–576. doi: 10.1073/pnas.97.2.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cookson MR. alpha-Synuclein and neuronal cell death. Mol Neurodegener. 2009;4:9. doi: 10.1186/1750-1326-4-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cookson MR, Xiromerisiou G, Singleton A. How genetics research in Parkinson's disease is enhancing understanding of the common idiopathic forms of the disease. Curr Opin Neurol. 2005;18(6):706–711. doi: 10.1097/01.wco.0000186841.43505.e6. [DOI] [PubMed] [Google Scholar]
- Corti O, Hampe C, Koutnikova H, Darios F, Jacquier S, Prigent A, et al. The p38 subunit of the aminoacyl-tRNA synthetase complex is a Parkin substrate: linking protein biosynthesis and neurodegeneration. Hum Mol Genet. 2003;12(12):1427–1437. doi: 10.1093/hmg/ddg159. [DOI] [PubMed] [Google Scholar]
- Cuervo AM, Stefanis L, Fredenburg R, Lansbury PT, Sulzer D. Impaired degradation of mutant alpha-synuclein by chaperone-mediated autophagy. Science. 2004;305(5688):1292–1295. doi: 10.1126/science.1101738. [DOI] [PubMed] [Google Scholar]
- Danzer KM, Haasen D, Karow AR, Moussaud S, Habeck M, Giese A, et al. Different species of alpha-synuclein oligomers induce calcium influx and seeding. J Neurosci. 2007;27(34):9220–9232. doi: 10.1523/JNEUROSCI.2617-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darios F, Corti O, Lucking CB, Hampe C, Muriel MP, Abbas N, et al. Parkin prevents mitochondrial swelling and cytochrome c release in mitochondria-dependent cell death. Hum Mol Genet. 2003;12(5):517–526. doi: 10.1093/hmg/ddg044. [DOI] [PubMed] [Google Scholar]
- Dauer W, Kholodilov N, Vila M, Trillat AC, Goodchild R, Larsen KE, et al. Resistance of alpha -synuclein null mice to the parkinsonian neurotoxin MPTP. Proc Natl Acad Sci U S A. 2002;99(22):14524–14529. doi: 10.1073/pnas.172514599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dauer W, Przedborski S. Parkinson's disease: mechanisms and models. Neuron. 2003;39(6):889–909. doi: 10.1016/s0896-6273(03)00568-3. [DOI] [PubMed] [Google Scholar]
- Dawson T, Mandir A, Lee M. Animal models of PD: pieces of the same puzzle? Neuron. 2002;35(2):219–222. doi: 10.1016/s0896-6273(02)00780-8. [DOI] [PubMed] [Google Scholar]
- De Marco EV, Tarantino P, Rocca FE, Provenzano G, Civitelli D, De Luca V, et al. Alpha-synuclein promoter haplotypes and dementia in Parkinson's disease. Am J Med Genet B Neuropsychiatr Genet. 2008;147(3):403–407. doi: 10.1002/ajmg.b.30611. [DOI] [PubMed] [Google Scholar]
- Demuro A, Mina E, Kayed R, Milton SC, Parker I, Glabe CG. Calcium dysregulation and membrane disruption as a ubiquitous neurotoxic mechanism of soluble amyloid oligomers. J Biol Chem. 2005;280(17):17294–17300. doi: 10.1074/jbc.M500997200. [DOI] [PubMed] [Google Scholar]
- Deng H, Dodson MW, Huang H, Guo M. The Parkinson's disease genes pink1 and parkin promote mitochondrial fission and/or inhibit fusion in Drosophila. Proc Natl Acad Sci U S A. 2008;105(38):14503–14508. doi: 10.1073/pnas.0803998105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng H, Dodson MW, Huang H, Guo M. The Parkinson's disease genes pink1 and parkin promote mitochondrial fission and/or inhibit fusion in Drosophila. Proc Natl Acad Sci U S A. 2008;105(38):14503–14508. doi: 10.1073/pnas.0803998105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodson MW, Guo M. Pink1, Parkin, DJ-1 and mitochondrial dysfunction in Parkinson's disease. Curr Opin Neurobiol. 2007;17(3):331–337. doi: 10.1016/j.conb.2007.04.010. [DOI] [PubMed] [Google Scholar]
- Elbaz A, Moisan F. Update in the epidemiology of Parkinson's disease. Curr Opin Neurol. 2008;21(4):454–460. doi: 10.1097/WCO.0b013e3283050461. [DOI] [PubMed] [Google Scholar]
- Exner N, Treske B, Paquet D, Holmstrom K, Schiesling C, Gispert S, et al. Loss-of-function of human PINK1 results in mitochondrial pathology and can be rescued by parkin. J Neurosci. 2007;27(45):12413–12418. doi: 10.1523/JNEUROSCI.0719-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrer M, Kachergus J, Forno L, Lincoln S, Wang DS, Hulihan M, et al. Comparison of kindreds with parkinsonism and alpha-synuclein genomic multiplications. Ann Neurol. 2004;55(2):174–179. doi: 10.1002/ana.10846. [DOI] [PubMed] [Google Scholar]
- Farrer M, Maraganore DM, Lockhart P, Singleton A, Lesnick TG, de Andrade M, et al. alpha-Synuclein gene haplotypes are associated with Parkinson's disease. Hum Mol Genet. 2001;10(17):1847–1851. doi: 10.1093/hmg/10.17.1847. [DOI] [PubMed] [Google Scholar]
- Farrer MJ. Genetics of Parkinson disease: paradigm shifts and future prospects. Nat Rev Genet. 2006;7(4):306–318. doi: 10.1038/nrg1831. [DOI] [PubMed] [Google Scholar]
- Feany MB, Bender WW. A Drosophila model of Parkinson's disease. Nature. 2000;404(6776):394–398. doi: 10.1038/35006074. [DOI] [PubMed] [Google Scholar]
- Ferreon AC, Gambin Y, Lemke EA, Deniz AA. Interplay of alpha-synuclein binding and conformational switching probed by single-molecule fluorescence. Proc Natl Acad Sci U S A. 2009;106(14):5645–5650. doi: 10.1073/pnas.0809232106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortin DL, Troyer MD, Nakamura K, Kubo S, Anthony MD, Edwards RH. Lipid rafts mediate the synaptic localization of alpha-synuclein. J Neurosci. 2004;24(30):6715–6723. doi: 10.1523/JNEUROSCI.1594-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furukawa K, Matsuzaki-Kobayashi M, Hasegawa T, Kikuchi A, Sugeno N, Itoyama Y, et al. Plasma membrane ion permeability induced by mutant alpha-synuclein contributes to the degeneration of neural cells. J Neurochem. 2006;97(4):1071–1077. doi: 10.1111/j.1471-4159.2006.03803.x. [DOI] [PubMed] [Google Scholar]
- Gaig C, Marti MJ, Ezquerra M, Rey MJ, Cardozo A, Tolosa E. G2019S LRRK2 mutation causing Parkinson's disease without Lewy bodies. J Neurol Neurosurg Psychiatry. 2007;78(6):626–628. doi: 10.1136/jnnp.2006.107904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gandhi S, Wood-Kaczmar A, Yao Z, Plun-Favreau H, Deas E, Klupsch K, et al. PINK1-associated Parkinson's disease is caused by neuronal vulnerability to calcium-induced cell death. Mol Cell. 2009;33(5):627–638. doi: 10.1016/j.molcel.2009.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giasson BI, Duda JE, Murray IV, Chen Q, Souza JM, Hurtig HI, et al. Oxidative damage linked to neurodegeneration by selective alpha-synuclein nitration in synucleinopathy lesions. Science. 2000;290(5493):985–989. doi: 10.1126/science.290.5493.985. [DOI] [PubMed] [Google Scholar]
- Giasson BI, Forman MS, Higuchi M, Golbe LI, Graves CL, Kotzbauer PT, et al. Initiation and synergistic fibrillization of tau and alpha-synuclein. Science. 2003;300(5619):636–640. doi: 10.1126/science.1082324. [DOI] [PubMed] [Google Scholar]
- Gloeckner CJ, Schumacher A, Boldt K, Ueffing M. The Parkinson disease-associated protein kinase LRRK2 exhibits MAPKKK activity and phosphorylates MKK3/6 and MKK4/7, in vitro. J Neurochem. 2009;109(4):959–968. doi: 10.1111/j.1471-4159.2009.06024.x. [DOI] [PubMed] [Google Scholar]
- Goldberg MS, Lansbury PT., Jr Is there a cause-and-effect relationship between alpha-synuclein fibrillization and Parkinson's disease? Nat Cell Biol. 2000;2(7):E115–E119. doi: 10.1038/35017124. [DOI] [PubMed] [Google Scholar]
- Goldstein DS, Sewell L. Olfactory dysfunction in pure autonomic failure: Implications for the pathogenesis of Lewy body diseases. Parkinsonism Relat Disord. 2009;15(7):516–520. doi: 10.1016/j.parkreldis.2008.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gowers WR. Diseases of the Nerves and Spinal Cord. Philadelphia: Blakiston’s Son; 1900. A Manual of Diseases of the Nervous System. Volume I. [Google Scholar]
- Greene JC, Whitworth AJ, Kuo I, Andrews LA, Feany MB, Pallanck LJ. Mitochondrial pathology and apoptotic muscle degeneration in Drosophila parkin mutants. Proc Natl Acad Sci U S A. 2003;100(7):4078–4083. doi: 10.1073/pnas.0737556100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene JC, Whitworth AJ, Kuo I, Andrews LA, Feany MB, Pallanck LJ. Mitochondrial pathology and apoptotic muscle degeneration in Drosophila parkin mutants. Proc Natl Acad Sci U S A. 2003;100(7):4078–4083. doi: 10.1073/pnas.0737556100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greggio E, Cookson MR. Leucine-rich repeat kinase 2 mutations and Parkinson's disease: three questions. ASN Neuro. 2009;1(1) doi: 10.1042/AN20090007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greggio E, Jain S, Kingsbury A, Bandopadhyay R, Lewis P, Kaganovich A, et al. Kinase activity is required for the toxic effects of mutant LRRK2/dardarin. Neurobiol Dis. 2006;23(2):329–341. doi: 10.1016/j.nbd.2006.04.001. [DOI] [PubMed] [Google Scholar]
- Hatano Y, Li Y, Sato K, Asakawa S, Yamamura Y, Tomiyama H, et al. Novel PINK1 mutations in early-onset parkinsonism. Ann Neurol. 2004;56(3):424–427. doi: 10.1002/ana.20251. [DOI] [PubMed] [Google Scholar]
- Ho CC, Rideout HJ, Ribe E, Troy CM, Dauer WT. The Parkinson disease protein leucine-rich repeat kinase 2 transduces death signals via Fas-associated protein with death domain and caspase-8 in a cellular model of neurodegeneration. J Neurosci. 2009;29(4):1011–1016. doi: 10.1523/JNEUROSCI.5175-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodara R, Norris EH, Giasson BI, Mishizen-Eberz AJ, Lynch DR, Lee VM, et al. Functional consequences of alpha-synuclein tyrosine nitration: diminished binding to lipid vesicles and increased fibril formation. J Biol Chem. 2004;279(46):47746–47753. doi: 10.1074/jbc.M408906200. [DOI] [PubMed] [Google Scholar]
- Hoepken HH, Gispert S, Morales B, Wingerter O, Del Turco D, Mulsch A, et al. Mitochondrial dysfunction, peroxidation damage and changes in glutathione metabolism in PARK6. Neurobiol Dis. 2007;25(2):401–411. doi: 10.1016/j.nbd.2006.10.007. [DOI] [PubMed] [Google Scholar]
- Hsu LJ, Sagara Y, Arroyo A, Rockenstein E, Sisk A, Mallory M, et al. alpha-synuclein promotes mitochondrial deficit and oxidative stress. Am J Pathol. 2000;157(2):401–410. doi: 10.1016/s0002-9440(10)64553-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huynh DP, Scoles DR, Nguyen D, Pulst SM. The autosomal recessive juvenile Parkinson disease gene product, parkin, interacts with and ubiquitinates synaptotagmin XI. Hum Mol Genet. 2003;12(20):2587–2597. doi: 10.1093/hmg/ddg269. [DOI] [PubMed] [Google Scholar]
- Iaccarino C, Crosio C, Vitale C, Sanna G, Carri MT, Barone P. Apoptotic mechanisms in mutant LRRK2-mediated cell death. Hum Mol Genet. 2007;16(11):1319–1326. doi: 10.1093/hmg/ddm080. [DOI] [PubMed] [Google Scholar]
- Imai Y, Gehrke S, Wang HQ, Takahashi R, Hasegawa K, Oota E, et al. Phosphorylation of 4E-BP by LRRK2 affects the maintenance of dopaminergic neurons in Drosophila. Embo J. 2008;27(18):2432–2443. doi: 10.1038/emboj.2008.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai Y, Soda M, Inoue H, Hattori N, Mizuno Y, Takahashi R. An unfolded putative transmembrane polypeptide, which can lead to endoplasmic reticulum stress, is a substrate of Parkin. Cell. 2001;105(7):891–902. doi: 10.1016/s0092-8674(01)00407-x. [DOI] [PubMed] [Google Scholar]
- Jaleel M, Nichols RJ, Deak M, Campbell DG, Gillardon F, Knebel A, et al. LRRK2 phosphorylates moesin at threonine-558: characterization of how Parkinson's disease mutants affect kinase activity. Biochem J. 2007;405(2):307–317. doi: 10.1042/BJ20070209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenco JM, Rawlingson A, Daniels B, Morris AJ. Regulation of phospholipase D2: selective inhibition of mammalian phospholipase D isoenzymes by alpha- and beta-synucleins. Biochemistry. 1998;37(14):4901–4909. doi: 10.1021/bi972776r. [DOI] [PubMed] [Google Scholar]
- Jenner P. Oxidative stress in Parkinson's disease. Annals of Neurology. 2003;53(Supplemental. no. 3):S26–S36. doi: 10.1002/ana.10483. discussion S36-8. [DOI] [PubMed] [Google Scholar]
- Kahle PJ, Neumann M, Ozmen L, Muller V, Jacobsen H, Schindzielorz A, et al. Subcellular localization of wild-type and Parkinson's disease-associated mutant alpha -synuclein in human and transgenic mouse brain. J Neurosci. 2000;20(17):6365–6373. doi: 10.1523/JNEUROSCI.20-17-06365.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kayed R, Head E, Thompson JL, McIntire TM, Milton SC, Cotman CW, et al. Common structure of soluble amyloid oligomers implies common mechanism of pathogenesis. Science. 2003;300(5618):486–489. doi: 10.1126/science.1079469. [DOI] [PubMed] [Google Scholar]
- Khaleghpour K, Pyronnet S, Gingras AC, Sonenberg N. Translational homeostasis: eukaryotic translation initiation factor 4E control of 4E-binding protein 1 and p70 S6 kinase activities. Mol Cell Biol. 1999;19(6):4302–4310. doi: 10.1128/mcb.19.6.4302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirik D, Annett LE, Burger C, Muzyczka N, Mandel RJ, Bjorklund A. Nigrostriatal alpha-synucleinopathy induced by viral vector-mediated overexpression of human alpha-synuclein: a new primate model of Parkinson's disease. Proc Natl Acad Sci U S A. 2003;100(5):2884–2889. doi: 10.1073/pnas.0536383100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitada T, Asakawa S, Hattori N, Matsumine H, Yamamura Y, Minoshima S, et al. Mutations in the parkin gene cause autosomal recessive juvenile parkinsonism. Nature. 1998;392(6676):605–608. doi: 10.1038/33416. [DOI] [PubMed] [Google Scholar]
- Ko HS, Kim SW, Sriram SR, Dawson VL, Dawson TM. Identification of far upstream element-binding protein-1 as an authentic Parkin substrate. J Biol Chem. 2006;281(24):16193–16196. doi: 10.1074/jbc.C600041200. [DOI] [PubMed] [Google Scholar]
- Ko HS, von Coelln R, Sriram SR, Kim SW, Chung KK, Pletnikova O, et al. Accumulation of the authentic parkin substrate aminoacyl-tRNA synthetase cofactor, p38/JTV-1, leads to catecholaminergic cell death. J Neurosci. 2005;25(35):7968–7978. doi: 10.1523/JNEUROSCI.2172-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovari E, Horvath J, Bouras C. Neuropathology of Lewy body disorders. Brain Res Bull. 2009;80(4–5):203–210. doi: 10.1016/j.brainresbull.2009.06.018. [DOI] [PubMed] [Google Scholar]
- Kramer ML, Schulz-Schaeffer WJ. Presynaptic alpha-synuclein aggregates, not Lewy bodies, cause neurodegeneration in dementia with Lewy bodies. J Neurosci. 2007;27(6):1405–1410. doi: 10.1523/JNEUROSCI.4564-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruger R, Kuhn W, Muller T, Woitalla D, Graeber M, Kosel S, et al. Ala30Pro mutation in the gene encoding alpha-synuclein in Parkinson's disease. Nat Genet. 1998;18(2):106–108. doi: 10.1038/ng0298-106. [DOI] [PubMed] [Google Scholar]
- Kubo SI, Kitami T, Noda S, Shimura H, Uchiyama Y, Asakawa S, et al. Parkin is associated with cellular vesicles. J Neurochem. 2001;78(1):42–54. doi: 10.1046/j.1471-4159.2001.00364.x. [DOI] [PubMed] [Google Scholar]
- Kuwahara T, Koyama A, Gengyo-Ando K, Masuda M, Kowa H, Tsunoda M, et al. Familial Parkinson mutant alpha-synuclein causes dopamine neuron dysfunction in transgenic Caenorhabditis elegans. J Biol Chem. 2006;281(1):334–340. doi: 10.1074/jbc.M504860200. [DOI] [PubMed] [Google Scholar]
- Lakso M, Vartiainen S, Moilanen AM, Sirvio J, Thomas JH, Nass R, et al. Dopaminergic neuronal loss and motor deficits in Caenorhabditis elegans overexpressing human alpha-synuclein. J Neurochem. 2003;86(1):165–172. doi: 10.1046/j.1471-4159.2003.01809.x. [DOI] [PubMed] [Google Scholar]
- Langston JW, Ballard P, Tetrud JW, Irwin I. Chronic Parkinsonism in humans due to a product of meperidine-analog synthesis. Science. 1983;219(4587):979–980. doi: 10.1126/science.6823561. [DOI] [PubMed] [Google Scholar]
- Larsen KE, Schmitz Y, Troyer MD, Mosharov E, Dietrich P, Quazi AZ, et al. Alpha-synuclein overexpression in PC12 and chromaffin cells impairs catecholamine release by interfering with a late step in exocytosis. J Neurosci. 2006;26(46):11915–11922. doi: 10.1523/JNEUROSCI.3821-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee HJ, Choi C, Lee SJ. Membrane-bound alpha-synuclein has a high aggregation propensity and the ability to seed the aggregation of the cytosolic form. J Biol Chem. 2002;277(1):671–678. doi: 10.1074/jbc.M107045200. [DOI] [PubMed] [Google Scholar]
- Leong SL, Pham CL, Galatis D, Fodero-Tavoletti MT, Perez K, Hill AF, et al. Formation of dopamine-mediated alpha-synuclein-soluble oligomers requires methionine oxidation. Free Radic Biol Med. 2009;46(10):1328–1337. doi: 10.1016/j.freeradbiomed.2009.02.009. [DOI] [PubMed] [Google Scholar]
- Leroux P-D. Contribution à l’Étude des Causes de la Paralysie Agitante. Imprimeur de la Faculté de Mēdicine (In French) 1880 [Google Scholar]
- Li WW, Yang R, Guo JC, Ren HM, Zha XL, Cheng JS, et al. Localization of alpha-synuclein to mitochondria within midbrain of mice. Neuroreport. 2007;18(15):1543–1546. doi: 10.1097/WNR.0b013e3282f03db4. [DOI] [PubMed] [Google Scholar]
- Lo Bianco C, Ridet JL, Schneider BL, Deglon N, Aebischer P. alpha -Synucleinopathy and selective dopaminergic neuron loss in a rat lentiviral-based model of Parkinson's disease. Proc Natl Acad Sci U S A. 2002;99(16):10813–10818. doi: 10.1073/pnas.152339799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo Bianco C, Shorter J, Regulier E, Lashuel H, Iwatsubo T, Lindquist S, et al. Hsp104 antagonizes alpha-synuclein aggregation and reduces dopaminergic degeneration in a rat model of Parkinson disease. J Clin Invest. 2008;118(9):3087–3097. doi: 10.1172/JCI35781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lotharius J, Barg S, Wiekop P, Lundberg C, Raymon HK, Brundin P. Effect of mutant alpha-synuclein on dopamine homeostasis in a new human mesencephalic cell line. J Biol Chem. 2002;277(41):38884–38894. doi: 10.1074/jbc.M205518200. [DOI] [PubMed] [Google Scholar]
- MacLeod D, Dowman J, Hammond R, Leete T, Inoue K, Abeliovich A. The familial Parkinsonism gene LRRK2 regulates neurite process morphology. Neuron. 2006;52(4):587–593. doi: 10.1016/j.neuron.2006.10.008. [DOI] [PubMed] [Google Scholar]
- Manning-Bog AB, McCormack AL, Li J, Uversky VN, Fink AL, Di Monte DA. The herbicide paraquat causes up-regulation and aggregation of alpha-synuclein in mice: paraquat and alpha-synuclein. J Biol Chem. 2002;277(3):1641–1644. doi: 10.1074/jbc.C100560200. [DOI] [PubMed] [Google Scholar]
- Marti MJ, Tolosa E, Campdelacreu J. Clinical overview of the synucleinopathies. Mov Disord. 2003;18(Suppl 6):S21–S27. doi: 10.1002/mds.10559. [DOI] [PubMed] [Google Scholar]
- Marttila RJ, Kaprio J, Koskenvuo M, Rinne UK. Parkinson's disease in a nationwide twin cohort. Neurology. 1988;38(8):1217–1219. doi: 10.1212/wnl.38.8.1217. [DOI] [PubMed] [Google Scholar]
- Masliah E, Rockenstein E, Veinbergs I, Mallory M, Hashimoto M, Takeda A, et al. Dopaminergic loss and inclusion body formation in alpha-synuclein mice: implications for neurodegenerative disorders. Science. 2000;287(5456):1265–1269. doi: 10.1126/science.287.5456.1265. [DOI] [PubMed] [Google Scholar]
- Masliah E, Rockenstein E, Veinbergs I, Sagara Y, Mallory M, Hashimoto M, et al. beta-amyloid peptides enhance alpha-synuclein accumulation and neuronal deficits in a transgenic mouse model linking Alzheimer's disease and Parkinson's disease. Proc Natl Acad Sci U S A. 2001;98(21):12245–12250. doi: 10.1073/pnas.211412398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mata IF, Lockhart PJ, Farrer MJ. Parkin genetics: one model for Parkinson's disease. Hum Mol Genet. 2004;13(Spec No 1):R127–R133. doi: 10.1093/hmg/ddh089. [DOI] [PubMed] [Google Scholar]
- McNaught KS, Perl DP, Brownell AL, Olanow CW. Systemic exposure to proteasome inhibitors causes a progressive model of Parkinson's disease. Ann Neurol. 2004;56(1):149–162. doi: 10.1002/ana.20186. [DOI] [PubMed] [Google Scholar]
- Meulener M, Whitworth AJ, Armstrong-Gold CE, Rizzu P, Heutink P, Wes PD, et al. Drosophila DJ-1 mutants are selectively sensitive to environmental toxins associated with Parkinson's disease. Curr Biol. 2005;15(17):1572–1577. doi: 10.1016/j.cub.2005.07.064. [DOI] [PubMed] [Google Scholar]
- Meulener MC, Xu K, Thomson L, Ischiropoulos H, Bonini NM. Mutational analysis of DJ-1 in Drosophila implicates functional inactivation by oxidative damage and aging. Proc Natl Acad Sci U S A. 2006;103(33):12517–12522. doi: 10.1073/pnas.0601891103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mjones H. Paralysis Agitans. A clinical and genetic study. Acta. Psychiatrica et Neurologica Scandinavica. 1949;(Supplemental. 54):1–195. [Google Scholar]
- Miller DW, Hague SM, Clarimon J, Baptista M, Gwinn-Hardy K, Cookson MR, et al. Alpha-synuclein in blood and brain from familial Parkinson disease with SNCA locus triplication. Neurology. 2004;62(10):1835–1838. doi: 10.1212/01.wnl.0000127517.33208.f4. [DOI] [PubMed] [Google Scholar]
- Moore DJ, Dawson TM. Value of genetic models in understanding the cause and mechanisms of Parkinson's disease. Curr Neurol Neurosci Rep. 2008;8(4):288–296. doi: 10.1007/s11910-008-0045-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore DJ, West AB, Dawson VL, Dawson TM. Molecular pathophysiology of Parkinson's disease. Annu Rev Neurosci. 2005;28:57–87. doi: 10.1146/annurev.neuro.28.061604.135718. [DOI] [PubMed] [Google Scholar]
- Muftuoglu M, Elibol B, Dalmizrak O, Ercan A, Kulaksiz G, Ogus H, et al. Mitochondrial complex I and IV activities in leukocytes from patients with parkin mutations. Mov Disord. 2004;19(5):544–548. doi: 10.1002/mds.10695. [DOI] [PubMed] [Google Scholar]
- Mukhopadhyay D, Riezman H. Proteasome-independent functions of ubiquitin in endocytosis and signaling. Science. 2007;315(5809):201–205. doi: 10.1126/science.1127085. [DOI] [PubMed] [Google Scholar]
- Najim al-Din AS, Wriekat A, Mubaidin A, Dasouki M, Hiari M. Pallido-pyramidal degeneration, supranuclear upgaze paresis and dementia: Kufor-Rakeb syndrome. Acta Neurol Scand. 1994;89(5):347–352. doi: 10.1111/j.1600-0404.1994.tb02645.x. [DOI] [PubMed] [Google Scholar]
- Nakamura K, Nemani VM, Wallender EK, Kaehlcke K, Ott M, Edwards RH. Optical reporters for the conformation of alpha-synuclein reveal a specific interaction with mitochondria. J Neurosci. 2008;28(47):12305–12317. doi: 10.1523/JNEUROSCI.3088-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nemani VM, Lu W, Berge V, Nakamura K, Onoa B, Lee MK, et al. Increased expression of alpha-synuclein reduces neurotransmitter release by inhibiting synaptic vesicle reclustering after endocytosis. Neuron. 65(1):66–79. doi: 10.1016/j.neuron.2009.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olanow CW, Perl DP, DeMartino GN, McNaught KS. Lewy-body formation is an aggresome-related process: a hypothesis. Lancet Neurol. 2004;3(8):496–503. doi: 10.1016/S1474-4422(04)00827-0. [DOI] [PubMed] [Google Scholar]
- Oshiro N, Fukata Y, Kaibuchi K. Phosphorylation of moesin by rho-associated kinase (Rho-kinase) plays a crucial role in the formation of microvilli-like structures. J Biol Chem. 1998;273(52):34663–34666. doi: 10.1074/jbc.273.52.34663. [DOI] [PubMed] [Google Scholar]
- Ostrerova-Golts N, Petrucelli L, Hardy J, Lee JM, Farer M, Wolozin B. The A53T alpha-synuclein mutation increases iron-dependent aggregation and toxicity. J Neurosci. 2000;20(16):6048–6054. doi: 10.1523/JNEUROSCI.20-16-06048.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Outeiro TF, Lindquist S. Yeast cells provide insight into alpha-synuclein biology and pathobiology. Science. 2003;302(5651):1772–1775. doi: 10.1126/science.1090439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Outeiro TF, Putcha P, Tetzlaff JE, Spoelgen R, Koker M, Carvalho F, et al. Formation of toxic oligomeric alpha-synuclein species in living cells. PLoS One. 2008;3(4):e1867. doi: 10.1371/journal.pone.0001867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paisan-Ruiz C, Jain S, Evans EW, Gilks WP, Simon J, van der Brug M, et al. Cloning of the gene containing mutations that cause PARK8-linked Parkinson's disease. Neuron. 2004;44(4):595–600. doi: 10.1016/j.neuron.2004.10.023. [DOI] [PubMed] [Google Scholar]
- Palacino JJ, Sagi D, Goldberg MS, Krauss S, Motz C, Wacker M, et al. Mitochondrial dysfunction and oxidative damage in parkin-deficient mice. J Biol Chem. 2004;279(18):18614–18622. doi: 10.1074/jbc.M401135200. [DOI] [PubMed] [Google Scholar]
- Pals P, Lincoln S, Manning J, Heckman M, Skipper L, Hulihan M, et al. alpha-Synuclein promoter confers susceptibility to Parkinson's disease. Ann Neurol. 2004;56(4):591–595. doi: 10.1002/ana.20268. [DOI] [PubMed] [Google Scholar]
- Park J, Lee SB, Lee S, Kim Y, Song S, Kim S, et al. Mitochondrial dysfunction in Drosophila PINK1 mutants is complemented by parkin. Nature. 2006;441(7097):1157–1161. doi: 10.1038/nature04788. [DOI] [PubMed] [Google Scholar]
- Park SS, Lee D. Selective loss of dopaminergic neurons and formation of Lewy body-like aggregations in alpha-synuclein transgenic fly neuronal cultures. Eur J Neurosci. 2006;23(11):2908–2914. doi: 10.1111/j.1460-9568.2006.04844.x. [DOI] [PubMed] [Google Scholar]
- Periquet M, Fulga T, Myllykangas L, Schlossmacher MG, Feany MB. Aggregated alpha-synuclein mediates dopaminergic neurotoxicity in vivo. J Neurosci. 2007;27(12):3338–3346. doi: 10.1523/JNEUROSCI.0285-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pesah Y, Pham T, Burgess H, Middlebrooks B, Verstreken P, Zhou Y, et al. Drosophila parkin mutants have decreased mass and cell size and increased sensitivity to oxygen radical stress. Development. 2004;131(9):2183–2194. doi: 10.1242/dev.01095. [DOI] [PubMed] [Google Scholar]
- Petit A, Kawarai T, Paitel E, Sanjo N, Maj M, Scheid M, et al. Wild-type PINK1 prevents basal and induced neuronal apoptosis, a protective effect abrogated by Parkinson disease-related mutations. J Biol Chem. 2005;280(40):34025–34032. doi: 10.1074/jbc.M505143200. [DOI] [PubMed] [Google Scholar]
- Petrucelli L, O'Farrell C, Lockhart PJ, Baptista M, Kehoe K, Vink L, et al. Parkin protects against the toxicity associated with mutant alpha-synuclein: proteasome dysfunction selectively affects catecholaminergic neurons. Neuron. 2002;36(6):1007–1019. doi: 10.1016/s0896-6273(02)01125-x. [DOI] [PubMed] [Google Scholar]
- Polymeropoulos MH, Higgins JJ, Golbe LI, Johnson WG, Ide SE, Di Iorio G, et al. Mapping of a gene for Parkinson's disease to chromosome 4q21-q23. Science. 1996;274(5290):1197–1199. doi: 10.1126/science.274.5290.1197. [DOI] [PubMed] [Google Scholar]
- Polymeropoulos MH, Lavedan C, Leroy E, Ide SE, Dehejia A, Dutra A, et al. Mutation in the alpha-synuclein gene identified in families with Parkinson's disease. Science. 1997;276(5321):2045–2047. doi: 10.1126/science.276.5321.2045. [DOI] [PubMed] [Google Scholar]
- Poole AC, Thomas RE, Andrews LA, McBride HM, Whitworth AJ, Pallanck LJ. The PINK1/Parkin pathway regulates mitochondrial morphology. Proc Natl Acad Sci U S A. 2008;105(5):1638–1643. doi: 10.1073/pnas.0709336105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poskanzer DC, Schwab RS. Cohort Analysis of Parkinson's Syndrome: Evidence for a Single Etiology Related to Subclinical Infection About 1920. J Chronic Dis. 1963;16:961–973. doi: 10.1016/0021-9681(63)90098-5. [DOI] [PubMed] [Google Scholar]
- Pridgeon JW, Olzmann JA, Chin LS, Li L. PINK1 protects against oxidative stress by phosphorylating mitochondrial chaperone TRAP1. PLoS Biol. 2007;5(7):e172. doi: 10.1371/journal.pbio.0050172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin Z, Hu D, Han S, Reaney SH, Di Monte DA, Fink AL. Effect of 4-hydroxy-2-nonenal modification on alpha-synuclein aggregation. J Biol Chem. 2007;282(8):5862–5870. doi: 10.1074/jbc.M608126200. [DOI] [PubMed] [Google Scholar]
- Ren Y, Zhao J, Feng J. Parkin binds to alpha/beta tubulin and increases their ubiquitination and degradation. J Neurosci. 2003;23(8):3316–3324. doi: 10.1523/JNEUROSCI.23-08-03316.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross OA, Braithwaite AT, Skipper LM, Kachergus J, Hulihan MM, Middleton FA, et al. Genomic investigation of alpha-synuclein multiplication and parkinsonism. Ann Neurol. 2008;63(6):743–750. doi: 10.1002/ana.21380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandebring A, Dehvari N, Perez-Manso M, Thomas KJ, Karpilovski E, Cookson MR, et al. Parkin deficiency disrupts calcium homeostasis by modulating phospholipase C signalling. Febs J. 2009;276(18):5041–5052. doi: 10.1111/j.1742-4658.2009.07201.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satake W, Nakabayashi Y, Mizuta I, Hirota Y, Ito C, Kubo M, et al. Genome-wide association study identifies common variants at four loci as genetic risk factors for Parkinson's disease. Nat Genet. 2009;41(12):1303–1307. doi: 10.1038/ng.485. [DOI] [PubMed] [Google Scholar]
- Savitt JM, Dawson VL, Dawson TM. Diagnosis and treatment of Parkinson disease: molecules to medicine. J Clin Invest. 2006;116(7):1744–1754. doi: 10.1172/JCI29178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sen S, Webber PJ, West AB. Dependence of leucine-rich repeat kinase 2 (LRRK2) kinase activity on dimerization. J Biol Chem. 2009;284(52):36346–36356. doi: 10.1074/jbc.M109.025437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharon R, Bar-Joseph I, Frosch MP, Walsh DM, Hamilton JA, Selkoe DJ. The formation of highly soluble oligomers of alpha-synuclein is regulated by fatty acids and enhanced in Parkinson's disease. Neuron. 2003;37(4):583–595. doi: 10.1016/s0896-6273(03)00024-2. [DOI] [PubMed] [Google Scholar]
- Sherer TB, Betarbet R, Stout AK, Lund S, Baptista M, Panov AV, et al. An in vitro model of Parkinson's disease: linking mitochondrial impairment to altered alpha-synuclein metabolism and oxidative damage. J Neurosci. 2002;22(16):7006–7015. doi: 10.1523/JNEUROSCI.22-16-07006.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherer TB, Betarbet R, Testa CM, Seo BB, Richardson JR, Kim JH, et al. Mechanism of toxicity in rotenone models of Parkinson's disease. J Neurosci. 2003;23(34):10756–10764. doi: 10.1523/JNEUROSCI.23-34-10756.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimura H, Hattori N, Kubo S, Mizuno Y, Asakawa S, Minoshima S, et al. Familial Parkinson disease gene product, parkin, is a ubiquitin-protein ligase. Nat Genet. 2000;25(3):302–305. doi: 10.1038/77060. [DOI] [PubMed] [Google Scholar]
- Silvestri L, Caputo V, Bellacchio E, Atorino L, Dallapiccola B, Valente EM, et al. Mitochondrial import and enzymatic activity of PINK1 mutants associated to recessive parkinsonism. Hum Mol Genet. 2005;14(22):3477–3492. doi: 10.1093/hmg/ddi377. [DOI] [PubMed] [Google Scholar]
- Singleton AB, Farrer M, Johnson J, Singleton A, Hague S, Kachergus J, et al. alpha-Synuclein locus triplication causes Parkinson's disease. Science. 2003;302(5646):841. doi: 10.1126/science.1090278. [DOI] [PubMed] [Google Scholar]
- Smith WW, Pei Z, Jiang H, Dawson VL, Dawson TM, Ross CA. Kinase activity of mutant LRRK2 mediates neuronal toxicity. Nat Neurosci. 2006;9(10):1231–1233. doi: 10.1038/nn1776. [DOI] [PubMed] [Google Scholar]
- Smith WW, Pei Z, Jiang H, Moore DJ, Liang Y, West AB, et al. Leucine-rich repeat kinase 2 (LRRK2) interacts with parkin, and mutant LRRK2 induces neuronal degeneration. Proc Natl Acad Sci U S A. 2005;102(51):18676–18681. doi: 10.1073/pnas.0508052102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder H, Mensah K, Theisler C, Lee J, Matouschek A, Wolozin B. Aggregated and monomeric alpha-synuclein bind to the S6' proteasomal protein and inhibit proteasomal function. J Biol Chem. 2003;278(14):11753–11759. doi: 10.1074/jbc.M208641200. [DOI] [PubMed] [Google Scholar]
- Song DD, Shults CW, Sisk A, Rockenstein E, Masliah E. Enhanced substantia nigra mitochondrial pathology in human alpha-synuclein transgenic mice after treatment with MPTP. Exp Neurol. 2004;186(2):158–172. doi: 10.1016/S0014-4886(03)00342-X. [DOI] [PubMed] [Google Scholar]
- Spadafora P, Annesi G, Pasqua AA, Serra P, Ciro Candiano IC, Carrideo S, et al. NACP-REP1 polymorphism is not involved in Parkinson's disease: a case-control study in a population sample from southern Italy. Neurosci Lett. 2003;351(2):75–78. doi: 10.1016/s0304-3940(03)00859-0. [DOI] [PubMed] [Google Scholar]
- St Martin JL, Klucken J, Outeiro TF, Nguyen P, Keller-McGandy C, Cantuti-Castelvetri I, et al. Dopaminergic neuron loss and up-regulation of chaperone protein mRNA induced by targeted over-expression of alpha-synuclein in mouse substantia nigra. J Neurochem. 2007;100(6):1449–1457. doi: 10.1111/j.1471-4159.2006.04310.x. [DOI] [PubMed] [Google Scholar]
- Staropoli JF, McDermott C, Martinat C, Schulman B, Demireva E, Abeliovich A. Parkin is a component of an SCF-like ubiquitin ligase complex and protects postmitotic neurons from kainate excitotoxicity. Neuron. 2003;37(5):735–749. doi: 10.1016/s0896-6273(03)00084-9. [DOI] [PubMed] [Google Scholar]
- Stefanis L, Larsen KE, Rideout HJ, Sulzer D, Greene LA. Expression of A53T mutant but not wild-type alpha-synuclein in PC12 cells induces alterations of the ubiquitin-dependent degradation system, loss of dopamine release, and autophagic cell death. J Neurosci. 2001;21(24):9549–9560. doi: 10.1523/JNEUROSCI.21-24-09549.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tain LS, Mortiboys H, Tao RN, Ziviani E, Bandmann O, Whitworth AJ. Rapamycin activation of 4E-BP prevents parkinsonian dopaminergic neuron loss. Nat Neurosci. 2009;12(9):1129–1135. doi: 10.1038/nn.2372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan EK, Matsuura T, Nagamitsu S, Khajavi M, Jankovic J, Ashizawa T. Polymorphism of NACP-Rep1 in Parkinson's disease: an etiologic link with essential tremor? Neurology. 2000;54(5):1195–1198. doi: 10.1212/wnl.54.5.1195. [DOI] [PubMed] [Google Scholar]
- Tan EK, Tan C, Shen H, Chai A, Lum SY, Teoh ML, et al. Alpha synuclein promoter and risk of Parkinson's disease: microsatellite and allelic size variability. Neurosci Lett. 2003;336(1):70–72. doi: 10.1016/s0304-3940(02)01178-3. [DOI] [PubMed] [Google Scholar]
- Tan JM, Dawson TM. Parkin blushed by PINK1. Neuron. 2006;50(4):527–529. doi: 10.1016/j.neuron.2006.05.003. [DOI] [PubMed] [Google Scholar]
- Tanaka M, Kim YM, Lee G, Junn E, Iwatsubo T, Mouradian MM. Aggresomes formed by alpha-synuclein and synphilin-1 are cytoprotective. J Biol Chem. 2004;279(6):4625–4631. doi: 10.1074/jbc.M310994200. [DOI] [PubMed] [Google Scholar]
- Tanaka Y, Engelender S, Igarashi S, Rao RK, Wanner T, Tanzi RE, et al. Inducible expression of mutant alpha-synuclein decreases proteasome activity and increases sensitivity to mitochondria-dependent apoptosis. Hum Mol Genet. 2001;10(9):919–926. doi: 10.1093/hmg/10.9.919. [DOI] [PubMed] [Google Scholar]
- Valente EM, Abou-Sleiman PM, Caputo V, Muqit MM, Harvey K, Gispert S, et al. Hereditary early-onset Parkinson's disease caused by mutations in PINK1. Science. 2004;304(5674):1158–1160. doi: 10.1126/science.1096284. [DOI] [PubMed] [Google Scholar]
- Valente EM, Bentivoglio AR, Dixon PH, Ferraris A, Ialongo T, Frontali M, et al. Localization of a novel locus for autosomal recessive early-onset parkinsonism, PARK6, on human chromosome 1p35-p36. Am J Hum Genet. 2001;68(4):895–900. doi: 10.1086/319522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valente EM, Brancati F, Ferraris A, Graham EA, Davis MB, Breteler MM, et al. PARK6-linked parkinsonism occurs in several European families. Ann Neurol. 2002;51(1):14–18. [PubMed] [Google Scholar]
- Van Den Eeden SK, Tanner CM, Bernstein AL, Fross RD, Leimpeter A, Bloch DA, et al. Incidence of Parkinson's disease: variation by age, gender, and race/ethnicity. Am J Epidemiol. 2003;157(11):1015–1022. doi: 10.1093/aje/kwg068. [DOI] [PubMed] [Google Scholar]
- Vilarino-Guell C, Soto AI, Lincoln SJ, Ben Yahmed S, Kefi M, Heckman MG, et al. ATP13A2 variability in Parkinson disease. Hum Mutat. 2009;30(3):406–410. doi: 10.1002/humu.20877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D, Qian L, Xiong H, Liu J, Neckameyer WS, Oldham S, et al. Antioxidants protect PINK1-dependent dopaminergic neurons in Drosophila. Proc Natl Acad Sci U S A. 2006;103(36):13520–13525. doi: 10.1073/pnas.0604661103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward CD, Duvoisin RC, Ince SE, Nutt JD, Eldridge R, Calne DB. Parkinson's disease in 65 pairs of twins and in a set of quadruplets. Neurology. 1983;33(7):815–824. doi: 10.1212/wnl.33.7.815. [DOI] [PubMed] [Google Scholar]
- Webber PJ, West AB. LRRK2 in Parkinson's disease: function in cells and neurodegeneration. Febs J. 2009;276(22):6436–6444. doi: 10.1111/j.1742-4658.2009.07342.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West AB, Moore DJ, Choi C, Andrabi SA, Li X, Dikeman D, et al. Parkinson's disease-associated mutations in LRRK2 link enhanced GTP-binding and kinase activities to neuronal toxicity. Hum Mol Genet. 2007;16(2):223–232. doi: 10.1093/hmg/ddl471. [DOI] [PubMed] [Google Scholar]
- Whitworth AJ, Theodore DA, Greene JC, Benes H, Wes PD, Pallanck LJ. Increased glutathione S-transferase activity rescues dopaminergic neuron loss in a Drosophila model of Parkinson's disease. Proc Natl Acad Sci U S A. 2005;102(22):8024–8029. doi: 10.1073/pnas.0501078102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood-Kaczmar A, Gandhi S, Yao Z, Abramov AY, Miljan EA, Keen G, et al. PINK1 is necessary for long term survival and mitochondrial function in human dopaminergic neurons. PLoS One. 2008;3(6):e2455. doi: 10.1371/journal.pone.0002455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu J, Kao SY, Lee FJ, Song W, Jin LW, Yankner BA. Dopamine-dependent neurotoxicity of alpha-synuclein: a mechanism for selective neurodegeneration in Parkinson disease. Nat Med. 2002;8(6):600–606. doi: 10.1038/nm0602-600. [DOI] [PubMed] [Google Scholar]
- Yang Q, She H, Gearing M, Colla E, Lee M, Shacka JJ, et al. Regulation of neuronal survival factor MEF2D by chaperone-mediated autophagy. Science. 2009;323(5910):124–127. doi: 10.1126/science.1166088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y, Gehrke S, Haque ME, Imai Y, Kosek J, Yang L, et al. Inactivation of Drosophila DJ-1 leads to impairments of oxidative stress response and phosphatidylinositol 3-kinase/Akt signaling. Proc Natl Acad Sci U S A. 2005;102(38):13670–13675. doi: 10.1073/pnas.0504610102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y, Gehrke S, Imai Y, Huang Z, Ouyang Y, Wang JW, et al. Mitochondrial pathology and muscle and dopaminergic neuron degeneration caused by inactivation of Drosophila Pink1 is rescued by Parkin. Proc Natl Acad Sci U S A. 2006;103(28):10793–10798. doi: 10.1073/pnas.0602493103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yasuda T, Miyachi S, Kitagawa R, Wada K, Nihira T, Ren YR, et al. Neuronal specificity of alpha-synuclein toxicity and effect of Parkin co-expression in primates. Neuroscience. 2007;144(2):743–753. doi: 10.1016/j.neuroscience.2006.09.052. [DOI] [PubMed] [Google Scholar]
- Zarranz JJ, Alegre J, Gomez-Esteban JC, Lezcano E, Ros R, Ampuero I, et al. The new mutation, E46K, of alpha-synuclein causes Parkinson and Lewy body dementia. Ann Neurol. 2004;55(2):164–173. doi: 10.1002/ana.10795. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Gao J, Chung KK, Huang H, Dawson VL, Dawson TM. Parkin functions as an E2-dependent ubiquitin- protein ligase and promotes the degradation of the synaptic vesicle-associated protein, CDCrel-1. Proc Natl Acad Sci U S A. 2000;97(24):13354–13359. doi: 10.1073/pnas.240347797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou C, Huang Y, Shao Y, May J, Prou D, Perier C, et al. The kinase domain of mitochondrial PINK1 faces the cytoplasm. Proc Natl Acad Sci U S A. 2008;105(33):12022–12027. doi: 10.1073/pnas.0802814105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou W, Freed CR. DJ-1 up-regulates glutathione synthesis during oxidative stress and inhibits A53T alpha-synuclein toxicity. J Biol Chem. 2005;280(52):43150–43158. doi: 10.1074/jbc.M507124200. [DOI] [PubMed] [Google Scholar]
- Zimprich A, Biskup S, Leitner P, Lichtner P, Farrer M, Lincoln S, et al. Mutations in LRRK2 cause autosomal-dominant parkinsonism with pleomorphic pathology. Neuron. 2004;44(4):601–607. doi: 10.1016/j.neuron.2004.11.005. [DOI] [PubMed] [Google Scholar]
- Zimprich A, Muller-Myhsok B, Farrer M, Leitner P, Sharma M, Hulihan M, et al. The PARK8 locus in autosomal dominant parkinsonism: confirmation of linkage and further delineation of the disease-containing interval. Am J Hum Genet. 2004;74(1):11–19. doi: 10.1086/380647. [DOI] [PMC free article] [PubMed] [Google Scholar]