Abstract
Basal cell adenoma (BCA) is a rare benign epithelial tumor of the salivary gland, displaying monomorphic basaloid cells without a myxochondroid component, representing 1–3% of all salivary gland neoplasms seen predominantly in women over 50 years of age. It is uncommon in young adults. Cytodiagnosis of basaloid tumors chiefly basal cell adenoma of the salivary gland, is extremely challenging. The cytological differential diagnoses range from benign to malignant, neoplastic to non- neoplastic lesions. Histopathological examination is a must for definitive diagnosis, as these entities differ in prognosis and therapeutic aspects. We present a 22-years-old male with this uncommon diagnosis with a discussion on the role of cytological diagnosis. Fine needle aspiration cytology is a simple, minimally invasive method for the preoperative diagnosis of various types of neoplastic and non-neoplastic lesions. The knowledge of its pitfalls and limitations contributes to a more effective approach to treatment.
Keywords: Basal cell adenoma, basaloid tumor, basal cell adenocarcinoma, cytological diagnosis
INTRODUCTION
Basal cell adenomas are unique benign salivary gland tumors affecting women over 50 years of age comprising 1–3% of all salivary gland tumors.[1,2] Cytologically, they mimic several benign and malignant salivary and non-salivary gland tumors, warranting thorough histopathological examination. We describe basal cell adenoma in a young man with emphasis on cytological features and differential diagnoses.
CASE REPORT
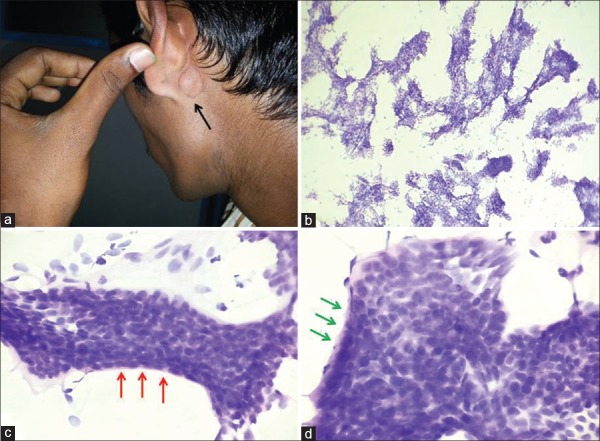
A 22-years-old man presented with a lump behind the left ear of 5 months duration. Clinical examination showed a nodule behind the left ear measuring 1.5 × 1.5 cm in size [Figure 1a]. There was no history of fever, weight loss, cough or tenderness. With a clinical diagnosis of salivary gland tumor, a fine needle aspiration was performed.
Figure 1.
(a) Clinical examination: Small nodule behind the left ear. Cytological smears showing (b) basaloid cells in nests sheets and trabeculae (PAP stain; ×100). (c) peripheral palisading of cells (red arrows) and bare nuclei in background (PAP, x400)); (d) basement membrane material around cell clusters (green arrows) (PAP, x400)
The aspiration yielded haphazardly arranged clusters and sheets of basaloid cells with scanty to moderate cytoplasm having round-oval benign nuclei with fine chromatin and indistinct nucleoli. Numerous bare nuclei were seen in the background. A thin peripheral ribbon of basement membrane material and peripheral palisading was present in some clusters. Squamous morules, hyaline globules, stromal elements, inflammatory cells, pleomorphism, mitoses and necrosis were absent [Figure 1b–d].
With a cytodiagnosis of basaloid neoplasm probably benign, excision of the lesion was suggested as several tumors like basal cell adenoma, basal cell adenocarcinoma, canalicular adenoma, cellular pleomorphic adenoma and solid variant of adenoid cystic carcinoma needed to be excluded in the differential diagnosis.
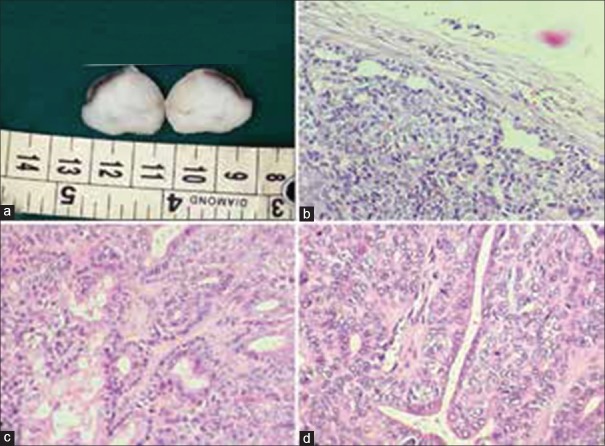
Intraoperatively, it was decided to limit the surgery to simple excision of nodule as the tumor was well encapsulated, lacked extensions outside the capsule and could be easily enucleated. The surgical specimen consisted of a nodular, well encapsulated, solid tumor measuring 2 × 1.5 cm with a homogenous lobulated cut surface [Figure 2a]. Histopathology showed a well-encapsulated benign tumor composed of uniform bland basaloid cells with round to oval nuclei and scant cytoplasm arranged in tubules, nests, trabeculae and sheets separated by collagenous non mucoid stroma. Peripheral palisading of cuboidal cells was observed in occasional tumor nests [Figure 2b and c]. The mitotic rate was 0–1/10 hpf. Capsular/vascular invasion, neurotropism, pleomorphism, necrosis and cystic change were absent. Multiple sections failed to reveal chondromyxoid stroma. Thus, a final diagnosis of basal cell adenoma, tubulo-trabecular type, was made.
Figure 2.
(a) Gross examination: Tumor with a solid homogenous grey-white lobulated cut surface. (b-d) Histological sections showing basaloid cells with uniform round-oval nuclei, eosinophilic cytoplasm and indistinct cytoplasmic borders arranged in tubulo-trabecular pattern separated by collagenous stroma and peripheral palisading within the nests. (H&E stain, (b) x200, (c) x400, (d) x400)
DISCUSSION
Basal cell adenoma is an uncommon benign basaloid salivary gland neoplasm rarely seen in the young.[1,2]
Cytologically small basaloid type of epithelial cells with bland oval nuclei, fine chromatin, indistinct nucleoli arranged in sheets, trabeculae and nests along with bare nuclei are seen. Two populations of cells may be seen; cells with larger nuclei and moderate cytoplasm and a second population with dark nuclei and scant cytoplasm. Peripheral palisading and amorphous homogenous basement membrane material around the nests and hyaline globules may be found. Chondromyxoid stromal component, atypia and necrosis are absent.[2,3,4,5,6,7]
Four histological patterns of basal cell adenoma are observed: Solid (sheets of basaloid cells separated by collagenous stroma), trabecular (nests and cords of basaloid cells separated by cellular stoma), tubular (glandular formations) and membranous (thick bands of hyaline material at the periphery of basaloid cells).[2] Peripheral palisading is a prominent feature within the nests. Mitoses are occasional. Capsular or vascular invasion, necrosis and chondroid matrix are absent.[1,3,4]
The differential diagnoses of’ basaloid neoplasm’ includes several benign and malignant tumors. Basal cell adenocarcinomas are low grade malignant tumors of the elderly with low risk of metastasis and recurrence and are hence treated by radical surgery. It is extremely difficult to differentiate them from basal cell adenoma cytomorphologically.[2] Histologically they show basaloid cells in sheets and trabeculae, mitotic activity of more than four per high power field,[1,8] nuclear pleomorphism, vascular and perineural invasion and infiltration of adjacent normal structures.[1] Absence of capsular invasion confirmed the diagnosis in our case on histopathological examination.
Immunohistochemistry (CK7, smooth muscle actin, Ki67) cannot distinguish between benign and malignant basaloid neoplasms.[1,8]
Canalicular adenomas mimic basal cell adenomas cytologically[2] but histologically show columnar epithelial cells in thin anastomosing cords with beaded pattern. They involve minor salivary glands of the oral cavity and have similar prognosis and therapeutic guidelines as basal cell adenomas.[1]
Cellular pleomorphic adenomas, (like the classical type) may recur after incomplete excision, requiring lobectomy.[1] Cytologically they show basaloid cells, fibrillary/myxoid material with spindled and plasmacytoid cells in the background.[2,4] Histological examination of the lesion is essential to identify the stromal component as myxoid material may be absent in cytological smears.[2]
Solid variants of adenoid cystic carcinomas require radical surgery and post-operative radiotherapy.[1] Cytologically, they show pleomorphism, increased mitosis, necrosis apart from basaloid cells and hyaline globules.[2,5,9] Histological evidence of vascular or perineural invasion, infiltration of adjacent normal structures and Ki 67 index of more than 5% differentiate them from basal cell adenoma.[1] Cytokeratin 5/6, p53, CD117, S100P protein and nuclear beta catenin are used to differentiate them from other basal cell neoplasms.[8,10]
Basaloid squamous cell carcinomas are aggressive tumors of the aerodigestive tract, treated by radical surgeries and radiotherapy or chemotherapy. Cytologically, they show basaloid cells with marked nuclear pleomorphism, necrosis, focal keratinization[2] and infiltrative growth on histology.[1] The index case lacked atypia and supportive histological features.
Absence of inflammation in smears ruled out chronic sialadenitis. Cytologically, cutaneous cylindromas overlying the salivary glands show hyaline globules and basaloid cells, however they can be distinguished by careful clinical examination.
All variants of basal cell adenomas are treated by local excision or resection of involved lobe except the membranous type which requires extensive surgery due to increased recurrence rate (24%). Malignant transformation is rarely noted in the membranous type.[1] Our case was tubulo-trabecular type of basal cell adenoma and hence, restricting the surgery to excision of nodule was justified.
CONCLUSIONS
We present a unique case of basal cell adenoma of the parotid in a young male. Fine needle aspiration cytology is an inexpensive and sensitive tool useful in routine practice. However it has its own limitations. Cytologically, basal cell adenocarcinoma is indistinguishable from basal cell adenoma. Extensive histopathological examination of the capsule is crucial to distinguish them from one another. Hence, histopathology is mandatory for accurate diagnosis, tumor subtyping and correct surgical management. This case report aims to create awareness about the various cytological differentials of basaloid neoplasm, the pitfalls in cytodiagnosis of these tumors and their impact on management.
ACKNOWLEDGEMENT
We thank the department of Otorhinolaryngology for providing this case.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Barnes L, Eveson JW, Reichart P, Sidransky D. 10th ed. Lyon: IARC Press; 2005. World Health Organization Classification of Tumours. Pathology and genetics of head and neck tumours. [Google Scholar]
- 2.Orell RS, Sterrett GF. 5th ed. India: Churchill Livingstone, Elsevier Publications; 2012. Orell Sterrett's Fine Needle Aspiration Cytology. [Google Scholar]
- 3.Mukunyadzi P. Review of fine-needle aspiration cytology of salivary gland neoplasms, with emphasis on differential diagnosis. Am J Clin Pathol. 2002;118:S100–15. doi: 10.1309/WVVR-30E4-13TW-494D. [DOI] [PubMed] [Google Scholar]
- 4.Kotwal M, Gaikwad S, Patil R, Bobhate S. FNAC of salivary gland-A useful tool in preoperative diagnosis or a cytopathologist's riddle? J Cytol. 2007;24:85–8. [Google Scholar]
- 5.Singh A, Sharma R, Nema SK. Basal cell adenoma mimicking adenoid cystic carcinoma on FNAC- A case report. Int J Med Rev. 2014;2:166–8. [Google Scholar]
- 6.Gupta N, Bal A, Gupta AK, Rajwanshi A. Basal cell adenoma: A diagnostic dilemma on fine needle aspiration cytology. Diagn Cytopathol. 2011;39:913–6. doi: 10.1002/dc.21576. [DOI] [PubMed] [Google Scholar]
- 7.Midi A, Aydin O, Comunoglu C, Boyaci Z, Peker O. Basal cell adenoma of salivary gland; cytological features and differential diagnosis. 2009. [Last accessed on 2014 Sep 12]. p. 8. Available from: www.KBB.Forum.net .
- 8.Jung MJ, Roh JL, Choi SH, Nam SY, Kim SY, Lee SW, et al. Basal cell adenocarcinoma of the salivary gland: A morphological and immunohistochemical comparison with basal cell adenoma with and without capsular invasion. Diagn Pathol. 2013;8:171. doi: 10.1186/1746-1596-8-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jaso J, Malhotra R. Adenoid cystic carcinoma. Arch Pathol Lab Med. 2011;135:511–5. doi: 10.5858/2009-0527-RS.1. [DOI] [PubMed] [Google Scholar]
- 10.Kudoh M, Harada H, Sato Y, Omura K, Ishii Y. A case of basal cell adenoma of upper lip. Case Rep Med 2014;2014:795356. [Last accessed on 2015 Mar 27]. Available from: http;//dx.doi.org/10.1155/2014/795356 . [DOI] [PMC free article] [PubMed]