Abstract
Actinomycosis is a chronic suppurative infection that can occur in the head and neck region. Though cervico-facial actinomycosis is well described, primary actinomycosis of the salivary gland is rare and can present as any other suppurative infection or can simulate malignancy. We hereby report a case of a young male with primary actinomycosis of submandibular gland, presenting as acute suppurative infection and diagnosed on histopathology.
Keywords: Actinomycosis, Actinomyces israelii, submandibular gland
INTRODUCTION
Although cervico-facial actinomycosis is well-described, primary actinomycosis of the salivary gland is rare. Actinomycosis was considered to be the commonest of all deep mycotic infections or mycetomas in the past.[1] However, now it is well-established that it is a granulomatous lesion characterized by chronic suppuration usually caused by Actinomyces israelii which is a gram positive, non-acid fast, anaerobic, commensal bacteria within the oral cavity (tonsillar crypts and tartar of teeth). Unlike most of the mycotic infections, actinomycosis is not an opportunistic infection and the portal of entry is not through inhalation.[2] It commonly affects the facial soft tissue although it can spread to adjacent, salivary gland, bone and skin of face and neck. Primary actinomycosis of the submandibular gland is very rare and can present as any other suppurative infection or can simulate malignancy.[3] We hereby report a case of a young male with primary actinomycosis of submandibular gland diagnosed on histopathology.
CASE REPORT
A 22-year-old male presented to The Surgical Emergency with a 4.5 × 3 cm rapidly progressive, firm, tender swelling in the right submandibular region. There were no discharging sinuses on the overlying skin. There was no history of fever, malaise, cough, breathlessness, hemoptysis, trauma, surgery, recent tooth extraction or dental infection. He was neither diabetic nor immunocompromised. The swelling was confined to the submandibular region only. Routine investigations including blood counts, erythrocyte sedimentation rate and chest X-ray were within normal limits except for mild eosinophilia in the peripheral blood. ELISA test for HIV antibody was negative. Surgical excision was planned with the clinical suspicion of acute suppurative infection and abscess formation. Submandibular gland with surrounding soft tissue was excised and sent for histopathological examination.
On gross examination the gland measured 4 × 3 ×3 cms. No abscess cavity could be identified [Figure 1]. Microscopic examination revealed dense chronic inflammatory infiltrate in the periductal region and in the normal glandular parenchyma with extensive lymphoid follicle formation. Within the ducts, micro-organisms with filamentous appearance were appreciated, compatible morphologically with Actinomyces colonies. Focal areas also exhibited mixture of acute and chronic inflammatory cells. No granulomas or fungal profiles were present. A diagnosis of actinomycosis of the right submandibular gland was made [Figures 2 and 3].
Figure 1.

Cut Section of submandibular gland shows yellowish discoloration. No abscess cavity identified
Figure 2.
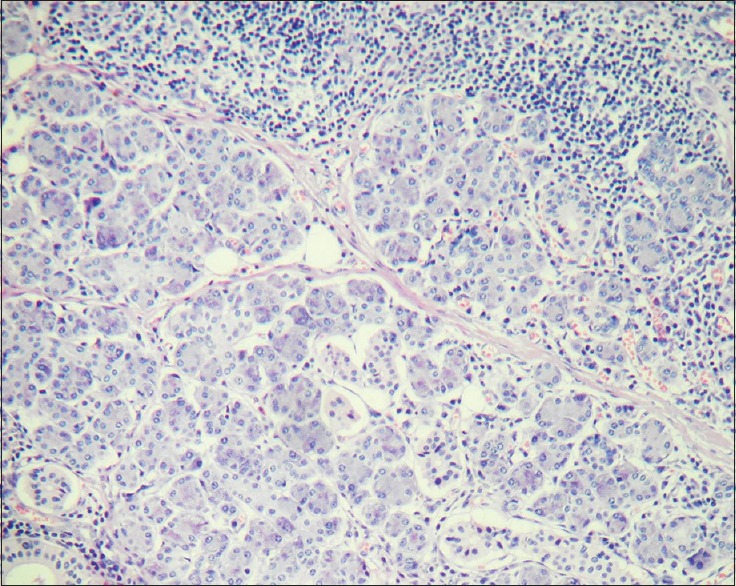
Photomicrograph showing dense chronic inflammatory infiltrate composed predominantly of lymphocytes in submandibular gland (H&E stain, x400)
Figure 3.
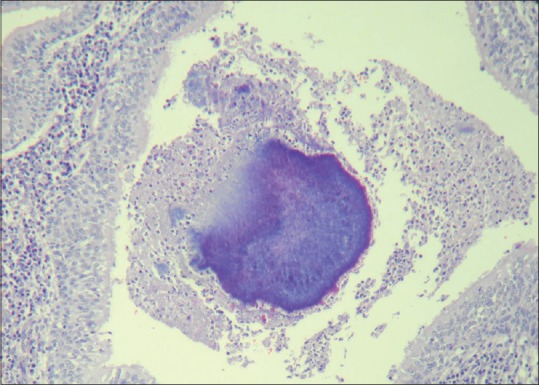
Photomicrograph showing colonies of Actinomyces in the duct of the submandibular gland. (H&E stain, x400)
DISCUSSION
Actinomycosis is a chronic, suppurative infection that can occur in the head and neck region. It is a potential microbial contaminant of head and neck surgery and may complicate a major surgical oncologic head and neck procedure. There is a male prevalence in young adults (3:1). The disease is characterized by an abscess formation surrounded by a granulomatous inflammatory reaction. The present case is also of a young male with a similar presentation.[4,5]
Actinomyces is a commensal and normal inhabitant of the human oral cavity and gastro-enteric tract. Cervicofacial actinomycosis is the most common manifestation, comprising 50–70% of reported cases. Infection typically occurs following oral surgery or in patients with poor dental hygiene. This form of actinomycosis is characterized in the initial stages by soft-tissue swelling of the perimandibular area. The infection in humans may occur due to procedures like dental manipulation, dental extractions, poor oral hygiene or maxillo-facial trauma. In the present case no such history was present therefore clinical diagnosis was difficult and urgent surgical intervention was done. The clinical diagnosis is difficult to establish because the onset and duration of the disease are not specific and a wide range of differential diagnoses have to be considered. Laboratory investigations can reveal anemia, mild leukocytosis and elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) levels. Organism cultures can be prepared from draining sinuses, deep needle aspirate or biopsy specimens. Cultures should be placed immediately under anaerobic conditions and incubated for 48 hours or longer; the isolation and definitive identification of actinomycetes may require 2–3 weeks. A Gram-stained smear of the specimen may demonstrate the presence of beaded, branched, gram-positive filamentous rods, suggesting the diagnosis of actinomycosis. Nucleic acid probes and polymerase chain reaction (PCR) methods are being developed for more rapid and more definite diagnosis.[6,7,8]
Histopathology of the biopsy specimen can be performed for definite demonstration of organism. In this case, surgical excision was performed as a consequence of the acute presentation of the disease and the histopathological examination lead to the final diagnosis though culture studies were not performed.[9,10,11]
When the actinomycosis infection is circumscribed, it is diagnosed early and is not associated with draining fistulas, medical treatment is preferred to surgery. However surgery clearly was the choice in this case.
The clinical appearance of cervico-facial actinomycosis is variable and may mimic malignant lesions or other chronic diseases, such as chronic granulomatous infections and inflammatory disease. There are no specific methods to prevent cervicofacial actinomycosis.
Maintenance of good oral hygiene and appropriate plaque removal can limit the tendency of Actinomyces to establish dense colonization and subclinical infection.[12,13]
Actinomyces are usually susceptible to several antibiotics like penicillins, chloremphenicol, tetracycline, clindamycin, streptomycin and cephalosporins. The patient in the present case was put on tetracycline and was asymptomatic on follow up after 2 weeks.[7,14]
CONCLUSION
Actinomycosis of submandibular gland is rare. The unusual presentation like the present case may make diagnosis difficult. In the absence of microbiological cultures histopathology is essential in diagnosis.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Vera-Alvarez J, Marigil-Gomez M, Abscal-Agorreta M. Fine needle aspiration cytology of cervicofacial actinomycosis. Acta Cytol. 1993;37:109–11. [PubMed] [Google Scholar]
- 2.Schaal KP, Lee HJ. Actinomycete infections in humans: A review. Gene. 1992;115:201–11. doi: 10.1016/0378-1119(92)90560-c. [DOI] [PubMed] [Google Scholar]
- 3.Das DK, Gulati A, Bhatt NC, Mandal AK, Khan VA, Bhambhani S. Fine needle aspiration cytology of oral and pharyngeal lesions. A study of 45 cases. Acta Cytol. 1993;37:333–42. [PubMed] [Google Scholar]
- 4.Weese WC, Smith IM. A study of 57 cases of actinomycosis over a 36-year period. Arch Intern Med. 1975;135:1562–8. [PubMed] [Google Scholar]
- 5.Sa’do B, Yoshiura K, Yuasa K, Ariji Y, Kanda S, Oka M, et al. Multimodality imaging of cervicofacial actinomycosis. Oral Surg Oral Med Oral Pathol. 1993;76:772–82. doi: 10.1016/0030-4220(93)90051-5. [DOI] [PubMed] [Google Scholar]
- 6.Moniruddin AB, Begum H, Nahar K. Actinomycosis-An update. Med Today. 2010;22:43–7. [Google Scholar]
- 7.Bennhoff DF. Actinomycosis: Diagnostic and therapeutic considerations and a review of 32 cases. Laryngoscope. 1984;94:1198–217. doi: 10.1288/00005537-198409000-00013. [DOI] [PubMed] [Google Scholar]
- 8.Kwartker JA, Limaye A. Cervicofacial actinomycosis: pathologic quiz case. Arch Otolaryngol Head Neck Surg. 1989;115:524–4. [PubMed] [Google Scholar]
- 9.Smego RA, Foglia G. Actinomycosis. State of the art clinical article. Clin Infect Dis. 1998;26:1255–61. doi: 10.1086/516337. [DOI] [PubMed] [Google Scholar]
- 10.Stenhouse D, MacDonald DG, MacFarlane TW. Cervico-facial and intra-oral actinomycosis: A 5-year retrospective study. Br J Oral Surg. 1975;13:172–82. doi: 10.1016/0007-117x(75)90006-2. [DOI] [PubMed] [Google Scholar]
- 11.Gaffney RJ, Walsh MA. Cervicofacial actinomycosis: An unusual cause of submandibular swelling. J Laryngol Otol. 1993;107:1169–70. doi: 10.1017/s0022215100125587. [DOI] [PubMed] [Google Scholar]
- 12.Chiang CW, Chang YL, Lou PJ. Actinomycosis imitating nasopharyngeal carcinoma. Ann Otol Rhinol Laryngol. 2000;109:605–7. doi: 10.1177/000348940010900614. [DOI] [PubMed] [Google Scholar]
- 13.Belmont MJ, Behar PM, Wax MK. Atypical presentations of actinomycosis. Head Neck. 1999;21:264–8. doi: 10.1002/(sici)1097-0347(199905)21:3<264::aid-hed12>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 14.Stewart AE, Palma JR, Amsberry JK. Cervicofacial actinomycosis. Otolaryngol Head Neck Surg. 2005;132:957–9. doi: 10.1016/j.otohns.2004.07.008. [DOI] [PubMed] [Google Scholar]


