Abstract
Dentin dysplasia is a rare disturbance of dentin formation characterized by normal enamel but atypical dentin formation with abnormal pupal morphology. The teeth appear clinically normal in morphologic appearance and color. The teeth characteristically exhibit extreme mobility and are commonly exfoliated prematurely. Radiograph shows obliteration of all pulp chambers, short, blunted and malformed or absent roots with periapical radiolucencies involving apparently intact tooth. This case is reported here because of its rarity along with the description of various clinical, radiological and histological features.
Keywords: Dentin dysplasia type I, pulpal obliteration, rootless teeth
INTRODUCTION
Dentin is a mineralized tissue constituting the body of a tooth, serving as a protective covering for the pulp and as a support for overlying enamel and cementum. Dentin dysplasia is an autosomal-dominant trait, affecting either the primary or both the primary and secondary dentitions for approximately one patient in every 100,000.[1,2] Dentin dysplasia was first reported in 1922 by Ballschmiedel who described six children in one family whose teeth had short, blunted roots with pulpal occlusion that he called “rootless teeth”. [3] Rushton[4] later described a similar condition in an individual without evidence of genetic inheritance and he termed as “dental dysplasia”. This condition is rarely encountered in dental practice. Generally, two main classes of dentin dysplasia are recognized based on clinical and radiographic appearance. Shields et al.,[5] proposed the classifications type I, or “dentin dysplasia,” and type II or “anomalous dysplasia of dentin.” Witkop[2] later described type I as “radicular dentin dysplasia” and type II as “coronal dentin dysplasia” to indicate the parts of the teeth that are primarily involved. Eastman et al., in 1977[6] and Ciola et al.,[7] in 1978 described two conditions for which they suggested the name “dentin dysplasia type III.” Ciola et al., case described radiographic findings characteristic of both dentin dysplasia type I and II and proposed type III classification in such cases. The case of Eastman et al., appears different from type I and type II, being focal rather than generalized. They described their case as focal odontoblastic dysplasia.
In type I (radicular) dentin dysplasia, both primary and permanent dentitions are affected, although the teeth are in normal morphologic appearance and color. The teeth characteristically exhibit extreme mobility and are commonly exfoliated prematurely. In type II (coronal), both the dentitions are affected; however, the deciduous teeth have a bluish or amber discoloration, while the permanent dentition appears normal. Primary teeth show total pulp obliteration and permanent teeth show thistle-tube pulp configuration and pulp stones in pulp chambers.[8]
Radiographically, in dentin dysplasia type I, the roots are sharp with conical, apical constrictions. Pre-eruptive pulpal obliteration occurs leading to a crescent-shaped pulpal remnant and total pulpal obliteration in the deciduous teeth.[9] In type II, the pulp chambers and root canals are shaped like a thistle tube with an accumulation of pulp stones with no periapical radiolucencies.
This article describes a rare case of dentin dysplasia type I in an 18-year-old female patient, highlighting the clinical, radiographic features of the defect and was confirmed by ground sectioning of the specimen and histopathologic examination.
CASE REPORT
An 18-year-old female patient reported to our department with the complaint of poor esthetic appearance due to missing upper and lower front teeth since 4 years and seeking prosthetic treatment. Patient gave no history of trauma and extractions in relation with the missing teeth. The patient reported that the teeth exfoliated due to loosening. The patient's medical history was not contributory. Family history revealed no such abnormality among other family members.
On intraoral examination [Figure 1] the morphologic appearance and color of the permanent teeth were normal. In maxillary arch, the missing teeth were from right canine region to left canine region and in mandibular arch, all the incisors were missing. There was generalized grade II and grade III mobility. Oral hygiene was poor and there were plaque and calculus deposits in all the quadrants. Restorations were present in left maxillary first molar and mandibular second molar.
Figure 1.

Intra oral photograph of a patient showing missing anterior teeth in both jaws with rest of the dentition exhibiting normal coronal color and morphology
Panoramic radiograph [Figure 2] revealed adequate enamel thickness on the cuspal tips of all the teeth. There was no root formation in most of the teeth while some of the teeth exhibited short, blunted and malformed roots of only a few millimeters with obliterated pulp chambers. The mandibular first left molar tooth had taurodontism like appearance. Well-defined periapical radiolucencies were present in association with the apex of the mandibular left first molar and right first and second molar.
Figure 2.

Panoramic radiograph shows no root formation in most of the teeth with total obliteration of the pulp chambers and periapical radiolucency in lower right mandibular first molar, left mandibular first and second molar
Although the patient had attained her physical maturity and was ready for definitive dental treatment but her physical, financial and psychological situations were important to be considered in selecting the final treatment plan. The following treatment plan was formulated for the patient. Dietary and oral hygiene instructions were given to the patient and extraction of the teeth that were mobile was advised along with the rehabilitation of the missing teeth with prosthesis.
The right maxillary first molar tooth was extracted and sent to Department of Oral Pathology and Microbiology. Clinical examination of the gross specimen [Figure 3] revealed an intact tooth. The tooth crown was of normal dimensions measuring around 7.5 mm but the roots were short and measured about 6 mm. The specimen was sectioned mesiodistally into halves. The mesiodistally cut tooth surface showed total obliteration of pulp chambers with dentin. One half of the cut tooth specimen was decalcified in 10% nitric acid and processed for hematoxylin-eosin (H and E) staining. Other half of the cut tooth specimen was used for preparing ground section.
Figure 3.
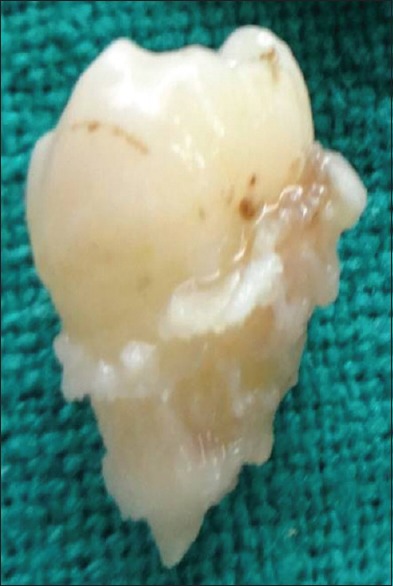
Gross specimen of permanent right maxillary first molar tooth
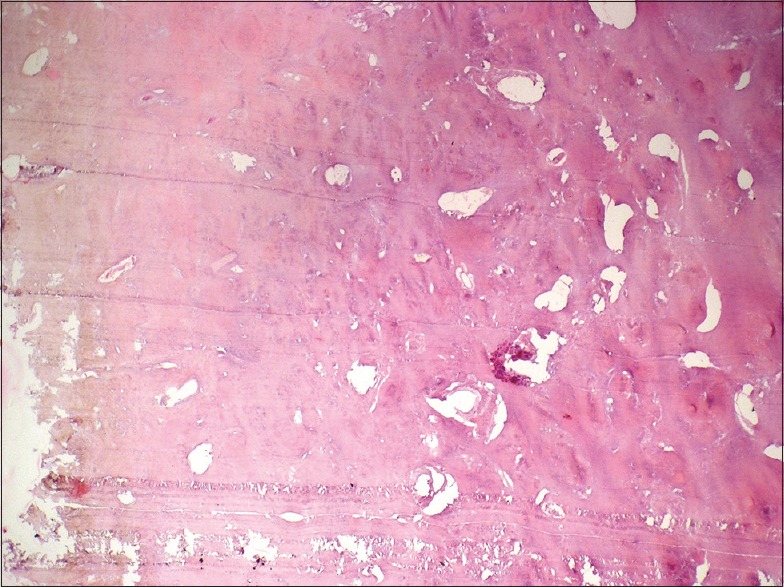
The ground section [Figure 4a and b] showed normal crown outline with normal enamel covering. A thin layer of superficial mantle dentin appeared but the pulp chamber was totally obliterated by an unusual calcified material consisting of atypical tubular dentin and osteodentin covered by thin discontinuous layer of cementum. Normal dentinal tubule formation appeared to have been blocked and the new dentin so formed around obstacle, gave rise to the characteristic appearance of “lava flow around the boulder” [Figure 5].
Figure 4.
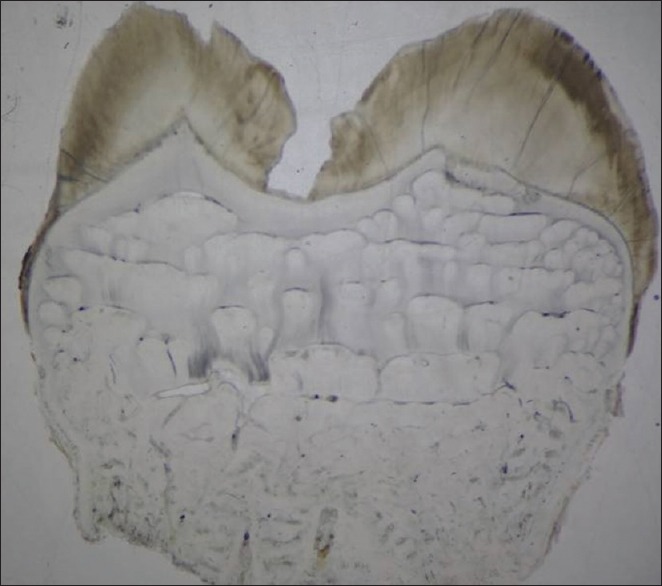
Stereomicroscopic view of ground section of permanent right maxillary first molar showing obliteration of pulp chamber with abnormal dentin formation (Ground section, x20)
Figure 5.
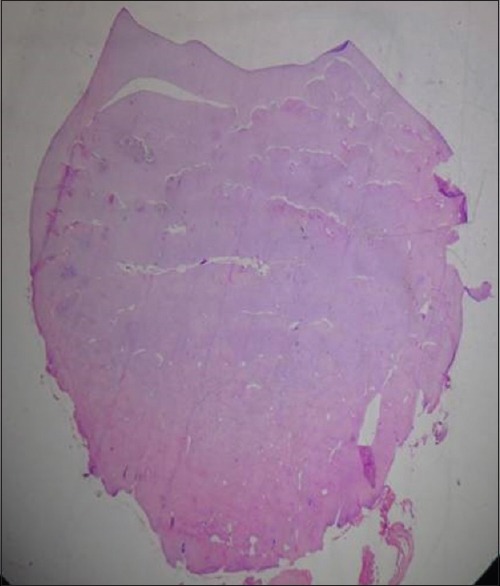
Stereomicroscopic view of hematoxylin-eosin stained permanent right maxillary first molar showing obliteration of pulp chamber with abnormal dentin formation (H&E stain, x20)
Histopathologic examination of the decalcified hematoxylin-eosin section [Figure 6] showed total obliteration of pulp that was filled with tubular dentin, osteodentin and irregular, globular masses of dentin [Figure 7 and 8]. A cluster of odontoblasts was seen within the globular masses of dentin.
Figure 6.

Photomicrograph of ground section showing polarized view of permanent maxillary first molar showing classic “lava flowing around boulders” appearance. (Polarizing microscopy, × 100)
Figure 7.
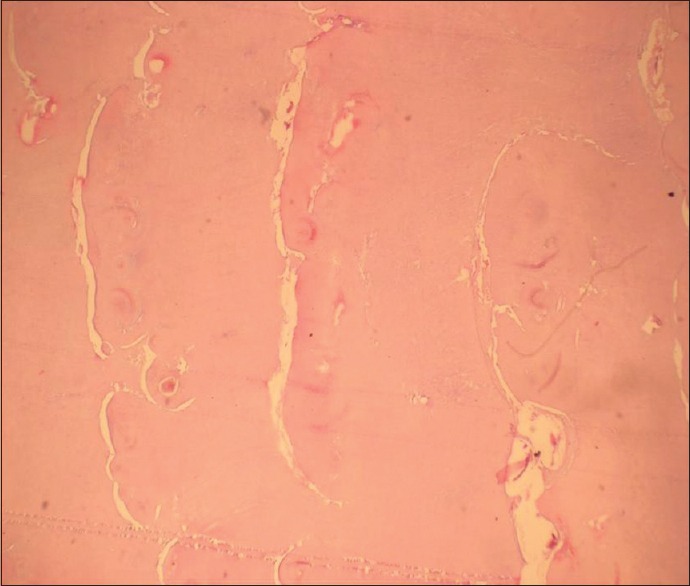
Photomicrograph showing decalcified section showing abnormal dentin formed around the obstacles (H&E stain, x100)
Figure 8.
Photomicrograph of decalcified section showing osteodentin with empty lacunae devoid of osteocytes (H&E stain, x100)
Based on the clinical, radiographic, gross features and histological examination of the ground section and decalcified section, diagnosis of dentin dysplasia type I was made.
DISCUSSION
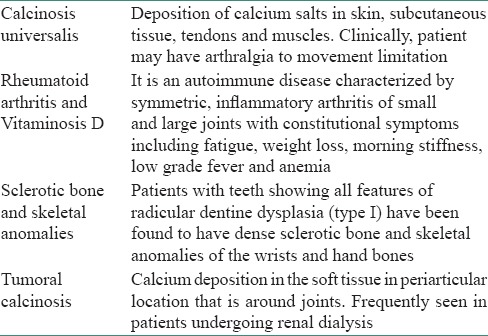
Dentin dysplasia is rarely seen in children, the occurrence is 1 in 100,000. There are some systemic disorders [Table 1] that are associated with dentin-dysplasia-like alterations but no such findings were found in this patient on general and radiological examination.[10,11] It is usually an autosomal dominant condition,[12] but in our patient there was no familial history of the disease, so she can be considered as a first generation sufferer. The etiology of dentin dysplasia type I remain speculative. Logan et al.,[13] proposed that the dental papilla is responsible for the abnormalities in root development. They suggested that multiple degenerative foci within the papilla become calcified, leading to reduced growth and final obliteration of the pulp space. Sauk et al., in a scanning electron microscope study, postulated that dentin dysplasia is a defect in the epithelial component of the developing tooth germ in which the invagination of the root sheath occurs too soon and, in a sequence of futile attempts to correct itself, results in a stunted root form with an unusual whorl-like pattern of dentin obliterating the pulp chambers.[14] Wesley et al.,[15] disagreed with this suggestion and proposed that the condition is caused by an abnormal interaction of odontoblasts with ameloblasts leading to abnormal differentiation and/or function of these odontoblasts. Witkop[16] suggested that the dysplasia results from epithelial cells from the sheath of Hertwig breaking off and migrating into dental papilla, where they induce odontoblast differentiation and dentin formation. Melnick et al.,[17] suggested that the abnormal root morphology is caused by abnormal differentiation and/or function of the odontoblasts. Clearly, the exact etiology of dentin dysplasia has yet to be explored.
Table 1.
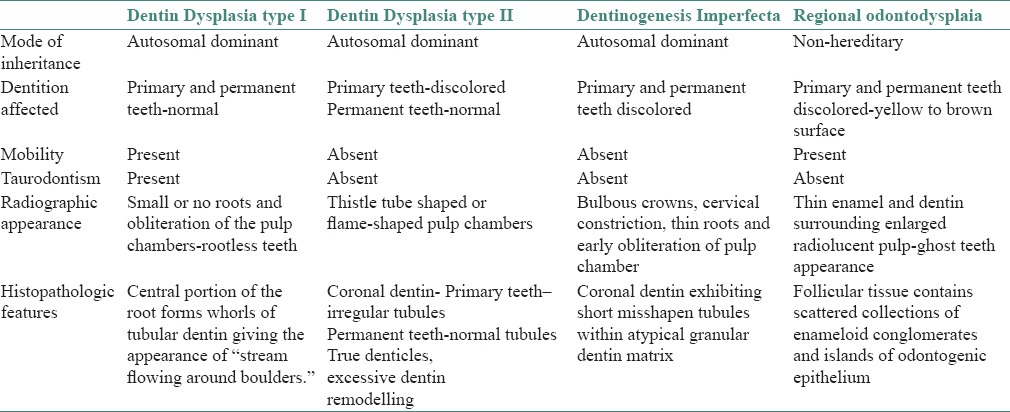
Dentin dysplasia type I should be differentiated from other conditions like dentin dysplasia type II, dentinogenesis imperfecta and odontodysplasia [Table 2].[11] In our patient, normal morphology of crown, short, blunted and malformed roots with pulpal obliteration and periapical radiolucency and ground section revealing “stream flowing around boulders” are characteristic for diagnosis of dentin dysplasia type I. There were no morphological variation in the dentition of our patient but there are reports that have suggested possible variations in the morphology of teeth affected by this type of dysplasia.[18,19]
Table 2.
Difference between dentin dysplasia type I, II, dentinogenesis imperfect and regional odontodysplasia[11]
Management of patients with dentin dysplasia has posed several problems to the dentists. Extraction has been suggested as a treatment alternative for teeth with pulp necrosis and periapical abscess. Endodontic treatment is contraindicated in teeth with total obliteration of root canals and pulp chambers.[20] Another approach for the treatment of teeth with dentin dysplasia has included peri-apical surgery and retrograde filling, which is recommended in teeth with long roots.[21,22] Follow-up and routine conservative treatment is another choice of treatment plan in dentin dysplasia.[21] Orthodontic treatment is suggested; however, further resorption of the roots, loosening of teeth and premature exfoliation may occur due to the resistance of the short roots to the orthodontic forces.[23] Successful oral rehabilitation with complete denture after extraction of all teeth and curettage of cysts has also been proposed.[24] Since these patients usually have early exfoliation of the teeth and consequently, maxillomandibular bony atrophy, treatment with a combination of onlay bone grafting and a sinus lift technique to accomplish implant placement can be used successfully.[25]
CONCLUSION
Dentin dysplasia type I is an unusual abnormality of dentin which leads to premature exfoliation of the teeth. The treatment of children with dentin dysplasia aims in effective preventive care as because of the early loss of teeth due to shortened roots and periodontitis. So, meticulous oral hygiene measures and dietary instructions must be established and maintained for the retention of teeth to help children have natural teeth as long as possible. In this regard, dentist has an important role in early diagnosis of this disorder and in guiding patients in the selection of measures to prolong the retention of affected teeth.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Kim JW, Simmer JP. Hereditary dentin defects. J Dent Res. 2007;86:392–9. doi: 10.1177/154405910708600502. [DOI] [PubMed] [Google Scholar]
- 2.Witkop CJ., Jr Hereditary defects of dentin. Dent Clin North Am. 1975;19:25–45. [PubMed] [Google Scholar]
- 3.Chamberlain BB, Hayward JR. Management of dentin dysplasia and facial disharmony. Spec Care Dentist. 1983 May-Jun;3:113–6. doi: 10.1111/j.1754-4505.1983.tb01615.x. [DOI] [PubMed] [Google Scholar]
- 4.Rushton MA. A case of dentin dysplasia. Guys Hosp Rep. 1939;89:369–73. [Google Scholar]
- 5.Shields ED, Bixler D, e1-Kafrawy AM. A proposed classification for heritable human dentine defects with a description of a new entity. Arch Oral Biol. 1973;18:543–53. doi: 10.1016/0003-9969(73)90075-7. [DOI] [PubMed] [Google Scholar]
- 6.Eastman JR, Melnick M, Goldblatt LI. Focal odontoblastic dysplasia: Dentin dysplasia type III. Oral Surg Oral Med Oral Pathol. 1977;44:909–14. doi: 10.1016/0030-4220(77)90035-4. [DOI] [PubMed] [Google Scholar]
- 7.Ciola B, Bahn SL, Goviea GL. Radiographic manifestation of an unusual combination of type I and type II dentin dysplasia. Oral Surg Oral Med Oral Pathol. 1978;45:317–22. doi: 10.1016/0030-4220(78)90101-9. [DOI] [PubMed] [Google Scholar]
- 8.Burkes EJ, Jr, Aquilino SA, Bost ME. Dentin dysplasia II. J Endod. 1979;5:277–81. doi: 10.1016/S0099-2399(79)80175-2. [DOI] [PubMed] [Google Scholar]
- 9.Barron MJ, McDonnell ST, Mackie I, Dixon MJ. Hereditary dentine disorders: Dentinogenesis imperfecta and dentine dysplasia. Orphanet J Rare Dis. 2008;3:31. doi: 10.1186/1750-1172-3-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morris ME, Augsburger RH. Dentine dysplasia with sclerotic bone and skeletal anomalies inherited as an autosomal dominant trait. A new syndrome. Oral Surg Oral Med. Oral Pathol. 1977;43:267. doi: 10.1016/0030-4220(77)90163-3. [DOI] [PubMed] [Google Scholar]
- 11.Neville B, Damm D, Allen C, Bouquot J, Bouquot J. Abnormalities of teeth. 2nd ed. Philadelphia: Saunders Elsevier; 2005. Oral and Maxillofacial Pathology; pp. 94–101. [Google Scholar]
- 12.Greenberg M, Glick M, Ship J. Immunologic Diseases. In: Atkinson JC, Imanguli MM, Challacombe S, editors. Burkett's oral medicine. 11th ed. Ontario, Canada: BC Decker Inc; 2008. pp. 453–6. [Google Scholar]
- 13.Logan J, Becks H, Silverman S, Jr, Pinborg JJ. Dentinal dysplasia. Oral Surg Oral Med Oral Pathol. 1962;15:317–33. doi: 10.1016/0030-4220(62)90113-5. [DOI] [PubMed] [Google Scholar]
- 14.Sauk JJ, Jr, Lyon HW, Trowbridge HO, Witkop CJ., Jr An electron optic analysis and explanation for the etiology of dentinal dysplasia. Oral Surg Oral Med Oral Pathol. 1972;33:763–71. doi: 10.1016/0030-4220(72)90444-6. [DOI] [PubMed] [Google Scholar]
- 15.Wesley RK, Wysocki GP, Mintz SM, Jackson J. Dentin dysplasia type I. Clinical, morphologic, and genetic studies of a case. Oral Surg Oral Med Oral Pathol. 1976;41:516–24. doi: 10.1016/0030-4220(76)90279-6. [DOI] [PubMed] [Google Scholar]
- 16.Witkop CJ., Jr Amelogenesis imperfecta, dentinogenesis imperfecta and dentin dysplasia revisited: Problems in classification. J Oral Pathol. 1988;17:547–53. doi: 10.1111/j.1600-0714.1988.tb01332.x. [DOI] [PubMed] [Google Scholar]
- 17.Melnick M, Levin LS, Brady J. Dentin dysplasia type I: A scanning electron microscopic analysis of the primary dentition. Oral Surg Oral Med Oral Pathol. 1980;50:335–40. doi: 10.1016/0030-4220(80)90418-1. [DOI] [PubMed] [Google Scholar]
- 18.Elzay RP, Robinson CT. Dentinal dysplasia. Report of a case. Oral Surg Oral Med Oral Pathol. 1967;23:338–42. doi: 10.1016/0030-4220(67)90146-6. [DOI] [PubMed] [Google Scholar]
- 19.Ozer L, Karasu H, Aras K, Tokman B, Ersoy E. Dentin dysplasia type I: Report of atypical cases in the permanent and mixed dentitions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:85–90. doi: 10.1016/j.tripleo.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 20.Steidler NE, Radden BG, Reade PC. Dentinal dysplasia: A clinicopathological study of eight cases and review of the literature. Br J Oral Maxillofac Surg. 1984;22:274–86. doi: 10.1016/0266-4356(84)90084-6. [DOI] [PubMed] [Google Scholar]
- 21.Ravanshad S, Khayat A. Endodontic therapy on a dentition exhibiting multiple periapical radiolucencies associated with dentinal dysplasia Type 1. Aust Endod J. 2006;32:40–2. doi: 10.1111/j.1747-4477.2006.00008.x. [DOI] [PubMed] [Google Scholar]
- 22.Ansari G, Reid JS. Dentinal dysplasia type I: Review of the literature and report of a family. ASDC J Dent Child. 1997;64:429–34. [PubMed] [Google Scholar]
- 23.Witkop CJ. Clinical aspects of dental anomalies. Int Dent J. 1976;26:378–90. [PubMed] [Google Scholar]
- 24.Neumann F, Wurfel F, Mundt T. Dentin dysplasia type I--a case report. Ann Anat. 1999;181:138–40. doi: 10.1016/S0940-9602(99)80120-4. [DOI] [PubMed] [Google Scholar]
- 25.Muñoz-Guerra MF, Naval-Gías L, Escorial V, Sastre-Pérez J. Dentin dysplasia type I treated with onlay bone grafting, sinus augmentation and osseointegrated implants. Implant Dent. 2006;15:248–53. doi: 10.1097/01.id.0000234638.60877.1b. [DOI] [PubMed] [Google Scholar]


