Abstract
Background
There is increasing interest in brief and very brief behaviour change interventions for physical activity as they are potentially scalable to the population level. However, few very brief interventions (VBIs) have been published, and evidence is lacking about their feasibility, acceptability and which ‘active ingredients’ (behaviour change techniques) would maximise their effectiveness. The aim of this research was to identify and develop promising VBIs for physical activity and test their feasibility and acceptability in the context of preventive health checks in primary care.
Methods
The process included two stages, guided by four criteria: effectiveness, feasibility, acceptability, and cost. In Stage 1, we used an iterative approach informed by systematic reviews, a scoping review of BCTs, team discussion, stakeholder consultation, a qualitative study, and cost estimation to guide the development of promising VBIs. In Stage 2, a feasibility study assessed the feasibility and acceptability of the short-listed VBIs, using tape-recordings and interviews with practitioners (n = 4) and patients (n = 68), to decide which VBIs merited further evaluation in a pilot trial.
Results
Four VBIs were short-listed: Motivational intervention; Action Planning intervention; Pedometer intervention; and Physical Activity Diary intervention. All were deliverable in around five minutes and were feasible and acceptable to participants and practitioners. Based on the results of interviews with practitioners and patients, techniques from the VBIs were combined into three new VBIs for further evaluation in a pilot trial.
Conclusions
Using a two-stage approach, in which we considered the practicability of VBIs (acceptability, feasibility and cost) alongside potential efficacy from the outset, we developed a short-list of four promising VBIs for physical activity and demonstrated that they were acceptable and feasible as part of a preventive health check in primary care.
Trial registration
Current Controlled Trials ISRCTN02863077. Registered 5 October 2012.
Electronic supplementary material
The online version of this article (doi:10.1186/s12889-015-1703-8) contains supplementary material, which is available to authorized users.
Keywords: Very brief interventions, Brief interventions, Physical activity, Behaviour change, Behaviour change techniques, Health Checks, Health promotion, Public health, Intervention development, Feasibility study
Background
Regular physical activity of moderate intensity (such as brisk walking, cycling and gardening) has significant benefits for both mental and physical health and can delay or prevent common chronic diseases such as heart disease, stroke and diabetes [1,2]. The UK government recommendations are for 30 minutes of moderate-intensity activity on at least five days per week. However, the majority of adults in the UK do not meet these recommendations [3]. Globally, physical inactivity is on the rise, adding to the burden of non-communicable diseases and affecting health worldwide [2]. There is a need for scalable, cost-effective interventions to enhance the adoption and maintenance of regular, everyday physical activity.
Recently, there has been a focus on developing brief and very brief behaviour change interventions targeting physical activity [4-6]. These have the potential to reach a large proportion of the adult population and could be delivered in routine or preventive primary care consultations, such as the National Health Service (NHS) health checks which target adults aged 40–74 adults [7]. Evidence shows that brief interventions (BIs) in primary care may increase physical activity in the short term [4-6,8]. However, definitions of BIs often include interventions that are too long for routine primary care consultations, with definitions ranging up to 30 [5] and 40 minutes [6]. Very brief interventions (VBIs), lasting no more than 5 minutes [5], could be delivered in most routine consultations. However, very few VBIs have been published and evidence for their effectiveness is weak and inconclusive [5]. Given the paucity of VBIs, little is known about which ‘active ingredients’ (behaviour change techniques (BCTs) [9]) would maximise their effectiveness. The UK Medical Research Council (MRC) guidance for the development and evaluation of complex interventions [10]. States that ‘best practice is to develop interventions systematically, using the best available evidence and appropriate theory, then to test them using a carefully phased approach’. Given the time constraints of VBIs, only a limited number of active ingredients can be included, whereas evidence may support a range of BCTs and hence a range of candidate interventions. Recent meta-analyses of physical activity interventions have shown that intention formation [11,12], self-monitoring [12-14], goal setting and review of behavioural goals [12] are effective BCTs, either alone or in combination [12]. However, the MRC framework does not provide guidance on criteria and methods to use when there are several candidate interventions. A simple approach would be to select the most effective intervention. However, candidate interventions are likely to differ in other ways that need consideration, e.g., the ease with which they can be delivered in routine practice, the extent of training required for health practitioners, intervention uptake and retention. In such instances, multiple criteria may be needed to short-list candidate interventions and decide which merit further evaluation.
We aimed to identify and develop promising VBIs for physical activity that could be delivered as part of routine NHS health checks in primary care and test their feasibility and acceptability. These health checks are delivered by a range of practitioners including nurses and health care assistants. They target adults between 40 and 74 years and include an assessment of vascular disease risk (e.g., type 2 diabetes, heart disease, kidney disease and stroke) [7] and therefore offer an ideal opportunity to promote physical activity among a large proportion of the adult population. Financial and time pressures are high in routine care, so interventions need to be cost-effective, feasible (e.g. can be delivered faithfully), and acceptable.
We used a two-stage approach to identify promising VBIs for physical activity, considering from the outset the practicability of the VBIs as well as their potential efficacy. Stage 1 was a development stage in which we combined evidence and expertise from multiple sources to develop a short-list of promising VBIs. In this stage the selection of BCTs was guided by evidence for their potential effectiveness, feasibility, acceptability and cost within the constraints of the target population, intervention providers, setting and target behaviour. Stage 2 was a feasibility study in which we assessed the feasibility and acceptability of the short-listed VBIs and decided which VBIs (or combinations of VBIs) should be carried forward for efficacy testing in a pilot trial.
Methods
Selection criteria
In both stages the selection of promising VBIs was guided by four criteria which the research team defined a priori:
Effectiveness: the VBI should have the potential to increase physical activity, as supported by evidence gathered.
Feasibility: a health practitioner should be able to deliver the VBI within 5 minutes as part of a health check. The VBI should also be feasible in other respects, e.g. fidelity of delivery, not requiring expensive equipment or extensive specialist training.
Acceptability: the VBI should be acceptable to both practitioners and patients.
Cost: the VBI should be low cost.
Initially, the research team defined a fifth criterion of the existence of a plausible mechanism of effect or theoretical basis, but this was dropped due to a lack of evidence in the behaviour change literature about mechanism of effect for most promising BCTs in this area [15].
Stage 1: Generation and development of a short-list of very brief interventions
Aims
-
(i)
To generate a short-list of promising VBIs to promote physical activity in primary care.
-
(ii)
To develop intervention and training procedures and materials for the short-listed VBIs.
(i) Generation of a short-list of promising VBIs
A short-list of promising VBIs was identified by the research team, using an iterative approach that combined evidence and expertise from multiple sources: systematic reviews, a scoping review of BCTs, team discussion, stakeholder consultation, a qualitative study, and estimation of resource cost. Figure 1 shows the sources of evidence and expertise that informed each of the four selection criteria. Each source of evidence is reported in turn below. In order to keep this stage manageable in terms of time, resources and proposed sample size, the short-list was limited a priori to a maximum of four interventions.
Figure 1.
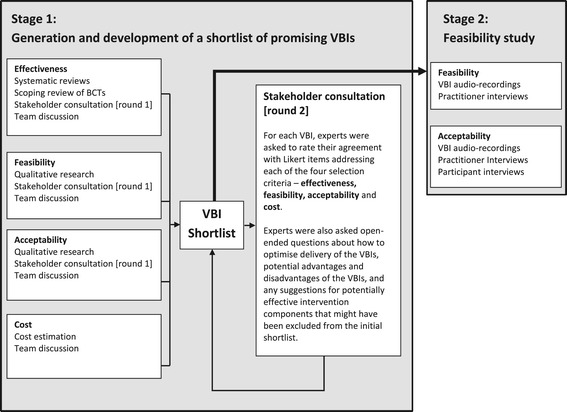
Sources of evidence informing the four selection criteria (effectiveness, feasibility, acceptability and cost).
Systematic reviews
Two systematic literature reviews were conducted by the research team. The first was a systematic review of reviews which aimed to identify what is known about brief and very brief interventions to promote physical activity in primary care in terms of their effectiveness, feasibility and acceptability [16]. The review was used to identify any promising interventions other than action planning and self-monitoring which had been identified a priori based on known evidence of their effectiveness. The second was a meta-analysis of the effects of pedometer use on daily physical activity among adults [17]. It was partially an update of earlier meta-analyses [13,14] but also aimed to identify BCTs other than self-monitoring in pedometer interventions.
Scoping review of BCTs
Promising BCTs that could be included in a VBI were identified from the Behaviour Change Technique Taxonomy Version 1 (BCTTv1) [9] by the research team. Evidence for the effectiveness of the BCTs identified was then extracted from systematic reviews or from primary studies when review level evidence was not available.
Stakeholder consultation [round 1]
We recruited a group of stakeholders with expertise in interventions to promote physical activity. They included academics, practitioners with experience in health service commissioning, health practitioners, and representatives of the public and patients (a panel of the local hospital). All stakeholders were asked to suggest interventions that they felt the study team should consider as promising very brief interventions to promote physical activity as part of an NHS health check. They were asked to bear in mind that the interventions should be deliverable in five minutes, and that they should be practical, feasible and acceptable to patients and practitioners [see Additional file 1 for more details].
Qualitative research
A qualitative researcher observed routine health check consultations in five practices to understand the content and process of delivery of health checks, and establish how VBIs could best be integrated within these consultations. The researcher also conducted face-to-face interviews with 51 patients to explore the potential effectiveness of a VBI and how it might be received by patients. Interviews followed an a priori topic guide, but a semi-structured approach was used to allow exploration of other relevant subjects if and when they arose [see Additional file 2 for the Patient Interview Topic Guide].
Cost estimation
The health economists in the research team estimated the set-up and running costs of self-monitoring and action planning interventions (defined a priori as promising VBIs) from studies included in systematic reviews of the effectiveness of interventions using self-monitoring [18] and implementation intentions (action planning) [11] to promote physical activity. They searched for any concurrent economic evaluations published as a part of the included trials, and this yielded one economic evaluation conducted alongside a pedometer-based intervention trial from which the cost of the intervention was estimated [19]. Resource use and cost were estimated based on intervention descriptions provided in the published studies [11,18,19]. Unit costs from standard published estimates [20] were applied to estimate set-up and running costs of the interventions.
Team discussion
The research team met monthly from December 2011 to September 2012 to review the evidence for the effectiveness, feasibility, acceptability and cost of promising components of VBIs, and generated a preliminary short-list of VBIs.
Stakeholder consultation [round 2]
At the end of stage 1, once a preliminary short-list of four VBIs had been generated, a one-page summary of the contents of each VBI was sent to a group of stakeholders. They consisted of four academics with expertise in behaviour change interventions (two of whom had participated in round 1), two practitioners with experience in service commissioning, two GPs and five nursing/allied professionals, and five PPI (Patient and Public Involvement) members. All were asked to complete seven questions about the potential effectiveness, feasibility, acceptability and cost of the proposed VBIs, measured on 5-point Likert-type scales. Stakeholders also answered open-ended questions about how to optimise delivery of the VBIs, potential advantages and disadvantages of the VBIs, and any suggestions for potentially effective intervention components that might have been omitted from the initial short-list [see Additional file 3 for full list of questions]. The research team reviewed the findings of this second stakeholder consultation and used them to decide on a final short-list of VBIs for the feasibility study.
(ii) Development of intervention and training procedures and materials for the short-listed VBIs
A member of the research team (SP) developed the intervention and training procedures and materials for each of the short-listed VBIs. Two researchers (SP, WH), one of whom had completed formal training in using the BCTTv1 and the second a member of the BCTTv1 team, independently coded the BCTs included in each VBI using BCTTv1 and resolved any disagreements.
The scripted intervention procedures for health practitioners and training procedures were piloted with seven members of the research team and five members of a PPI panel, to ensure that the procedures were clear and that the training could be completed in a reasonable time (three hours or less) and was feasible and acceptable in other respects.
Stage 2: Feasibility study of short-listed very brief interventions
Aims
The aims of the feasibility study were to:
-
(i)
Assess the fidelity, feasibility and acceptability of the short-listed VBIs identified in Stage 1 and optimise VBI procedures and materials.
-
(ii)
Decide which VBIs (or combinations of VBIs) to evaluate further in a pilot trial assessing fidelity, feasibility, acceptability and potential effects on objectively measured physical activity compared with the health check alone.
(i) Fidelity, feasibility and acceptability of VBI procedures and materials
Study design
The study was a feasibility study with a randomised design to assess the fidelity, feasibility and acceptability of the short-listed VBIs identified in Stage 1.
Randomisation
The order of the four arms was block randomised for each practice on a week by week basis, and participants were allocated to receive the intervention that was scheduled for delivery during the week of their health check appointment. This was done to ensure that the time and order of the interventions were balanced on average across practices and also to reduce cross-intervention contamination by making it easier for practitioners to focus on one VBI per week, rather than switching between four VBIs. The order of the intervention weeks was randomised for each practice and repeated until recruitment targets were reached for each practice. Participants were not aware of the intervention they were due to receive at the time of booking their appointment.
Setting
The study was conducted in three NHS general practices in urban areas in the east of England. The study was approved by the NRES Committee East of England - Cambridge Central (REC reference: 12/EE/0200), and research governance approval was obtained from NHS Cambridgeshire (Re: LO1183VBI).
Participants
Health practitioners (practice nurses (PNs) and health care assistants (HCAs)) responsible for delivering health checks were trained to deliver the four VBIs to patients eligible for an NHS health check. Patients were eligible if they were aged 40–74 years and not previously diagnosed with heart disease, stroke, diabetes, kidney disease or certain types of dementia. All patients invited for a health check during the recruitment period were invited to take part in the study. Current level of physical activity was not an inclusion criterion for the study as the VBIs were developed for delivery in a routine preventive consultation (the NHS Health Check) targeting all UK adults aged 40–74 years attending health checks, not just individuals who are currently insufficiently active.
Procedures
The practices sent letters to eligible patients, inviting them to take part in the study. Patients who wanted to take part in the study then contacted the practice to book an appointment for a health check at a time that was convenient for them. Participants received one of the four VBIs short-listed in Stage 1, which was delivered by the health practitioner at the end of the health check consultation.
Written consent for the study was obtained by the health practitioner at the start of the consultation. Participants were also asked for their consent to have the consultation audio-recorded. If the participant gave consent, the health check plus the VBI was audio-recorded. Following the consultation, participants were asked to participate in a short face-to-face interview with one of the research team members. A member of the research team also conducted face-to-face interviews with each practitioner at the end of the study.
Practitioner training in intervention delivery and study procedures
Two health practitioners from each practice who were responsible for delivering health checks underwent up to three hours of training to deliver the VBIs. Training and intervention procedures and materials were adapted iteratively.
Measures
Participant characteristics: The following demographic information was recorded on standardised forms by the health practitioner for each participant: age, gender, ethnicity, and occupation.
Feasibility: A coding framework was developed to assess practitioner adherence to the VBI procedures in terms of duration and fidelity. Two members of the research team listened independently to the VBI audio-recordings and completed the coding frame for each participant. They compared their ratings and any differences were resolved. VBI duration was defined as the length of time taken to deliver the VBI, excluding the rest of the health check consultation. VBI fidelity was defined as the presence (coded as 1) or absence (coded as 0) of VBI components (specific coding frame items) [see Additional file 4 for the fidelity items that made up each score] in the recording. Three fidelity scores were calculated for each VBI: (i) telling the participant the physical activity recommendations and giving feedback on their physical activity level (which was the same for all VBIs); (ii) delivery of specific intervention components (which were different for each ntervention, for example the Motivational VBI included a component related to the benefits of physical activity, and the Pedometer VBI included a component about how to use a pedometer to self-monitor physical activity); and (iii) overall fidelity (the sum of the first two scores). Feasibility of the VBIs was also assessed qualitatively from transcripts of semi-structured interviews with practitioners. A member of the research team (SP) read transcripts of the interviews and conducted a simple content analysis to determine: (i) practitioners’ views about the feasibility of delivering each VBI within 5 minutes as part of the HC; and (ii) whether practitioners found the VBIs easy to deliver.
Acceptability: Two members of the research team listened independently to the VBI audio-recordings and assessed participant engagement with the VBI on a five-point scale ranging from one (resistant) to five (enthusiastic), with a midpoint of three (ambivalent). They compared their ratings and any differences were resolved. Acceptability of the VBIs was also assessed qualitatively from transcripts of semi-structured interviews with participants and practitioners [see Additional file 5 for participant and practitioner interview topic guides]. A member of the research team (SP) read transcripts of the interviews and conducted a simple content analysis to determine: (i) whether the health check was an appropriate time to deliver the VBIs; (ii) whether VBIs differed in terms of acceptability to both participants and practitioners; (iii) whether anything could be improved about the VBIs.
(ii) Decision of which VBIs (or combinations of VBIs) to evaluate further in the pilot trial
Seven members of the research team (SS, WH, SP, KM, MB, LL, DM) met to review the findings of the feasibility study and select which VBIs or combination of VBIs to evaluate further in a pilot trial. VBI selection was guided by the findings about the acceptability and feasibility of each VBI. The group discussed the findings and reached a consensus.
Results
Stage 1: Generation and development of a short-list of very brief interventions
(i) Generation of a short-list of promising VBIs
Table 1 shows the findings of the systematic reviews, scoping review, stakeholder consultation, qualitative research and cost estimation. The systematic review of reviews identified ten physical activity intervention reviews (none of which focused explicitly on VBIs as defined by the current authors), and found that the few VBIs within those reviews were often poorly described [16]. Evidence for the effectiveness of VBIs and BIs was mixed, but did support the use of supplements (e.g. written materials) to brief advice [16]. The meta-analysis of pedometer use provided support for the use of pedometers as a promising VBI [17]. The scoping review of BCTs identified 17 BCTs that could feasibly be included in a low-cost, five-minute VBI (e.g. goal setting). Stakeholders in the first consultation identified eleven strategies that could be included in a VBI (e.g. tailoring). The qualitative research indicated that patients desired tailored advice about PA. Cost estimation revealed that the costs of self-monitoring and implementation intention (action planning) interventions were relatively low. Having reviewed the evidence from these different sources, the research team decided that all potential VBIs should include a 5-minute face-to-face discussion with the health care practitioner, including a discussion of current PA recommendations, and written materials for the participant. Four independent VBIs were identified as being potentially effective, feasible, acceptable and low cost: a Motivational intervention (VBI 1, focusing on identifying the personal benefits of PA and ways of increasing PA); an Action/Coping Planning intervention (VBI 2, focusing either on forming a specific plan of how to increase PA or on identifying potential barriers to maintaining PA and formulating a plan to overcome them); a Pedometer intervention (VBI 3, focusing on using a pedometer to monitor daily steps and reach a 10,000 steps/day goal); and a Physical Activity Diary intervention (VBI 4, focusing on weekly goal setting and self-monitoring of PA using a diary).
Table 1.
Findings from Stage 1 systematic reviews, stakeholder consultation [round 1], qualitative research and cost estimation
| Systematic reviews | Scoping review of promising BCTs* | Stakeholder consultation [round 1] (N = 32) | Qualitative research | Cost estimation |
|---|---|---|---|---|
| Systematic review of reviews of brief interventions (BIs) : [16] | BCTs identified as potentially feasible, acceptable and effective: | Eleven strategies were identified by at least 5 out of 32 stakeholders: | Health check (HC) observations: | Self-monitoring interventions: |
| • Three BI reviews and seven general PA intervention reviews were included. No reviews focusing on VBIs were identified. | 1.1 Goal setting (behaviour) | 1. Information about behaviour-health link (n = 14); | • HC follows a strict template, and lasts approximately 10 minutes. | • Estimated cost of pedometer and consumables (e.g. patient information booklet; a PA diary) = £13.30. |
| • BIs ranged from 1–3 minutes to 30 minutes. Very few were VBIs (<5 minutes). | 1.2 Problem Solving | 2. Planning (n = 12); | • Questions about PA/exercise are minimal and vague, e.g. ‘how much exercise do you do?’ | • Estimated cost of nurse time = £8.66 (2010 prices). |
| • Majority of BIs and VBIs were delivered face to face, but were poorly defined in terms of active ingredients. | 1.4 Action Planning | 3. Tailoring (n = 11); | • Advice on PA not given in the vast majority of HCs observed. | • Total estimated cost = £21.96 per patient. |
| • Evidence favoured the use of supplements (e.g. written materials) to brief advice. | 1.5 Review behaviour goals(s) | 4. Signposting (n = 10); | Patient Interviews (n = 51): | Implementation Intentions (action planning) Interventions: |
| • Uncertainty about the effectiveness, feasibility and acceptability of BIs and VBIs that could be delivered in a routine primary care consultation. | 1.6 Discrepancy between current behaviour and goals | 5. Time management/ identify opportunities (n = 9); | • Patients wanted nurse to ask more detailed questions about their current PA. | • Estimated cost of consumables (e.g. printed material for patients; log books) = £2.30. |
| Meta-analysis of the effects of pedometer use on daily PA [17]: | 1.9 Commitment | 6. General encouragement (n = 7); | • Patients unclear about the definition of ‘exercise’ and ‘PA’. | • Estimated cost of nurse time = £8.66 (2010 prices). |
| • Pedometers are an effective intervention for increasing PA [pedometers increased steps by 2000 [11] to 2419 [10] steps per day. | 2.2 Feedback on behaviour | 7. Social support (n = 7); | • Many patients felt that they had not been given PA advice. | • Total estimated cost = £10.96 per patient. |
| 2.3 Self-monitoring of behaviour | 8. Exercise prescription/ referral (n = 6); | • Patients wanted tailored PA advice. | Conclusion: | |
| 3.1 Social support (unspecified) | 9. Goal-setting (n = 6); | • Patients felt that PA advice would be best given at a follow-up appointment (after HC results were fed back to them). | • The costs of self-monitoring and implementation intention interventions are relatively small, comprising initial consultations, stationery, and follow-up consultations to review patient progress. | |
| 4.1 Instruction on how to perform the behaviour | 10. Self-monitoring (n = 5); | • Patients felt that PA advice was not necessary if HC results indicated that they were ‘healthy’. | ||
| 5.1 Information about health consequences | 11. Provide instruction (n = 5) | Implications for a PA VBI: | ||
| 5.3 Information about social and environmental consequences | • There is a need for a VBI focusing on PA in the HC. | |||
| 5.4 Monitoring of emotional consequences | • A 5 minute VBI should fit into a HC. | |||
| 5.6 Information about emotional consequences | • Patients should be asked detailed questions about their current PA. | |||
| 8.7 Graded Tasks | • Patients should be made aware of the definition of PA (e.g. what counts as ‘moderate’ intensity). | |||
| 12.5 Adding objects to the environment | • PA advice should be tailored to the individual (e.g. their current activity, lifestyle, capability etc.) | |||
| 15.4 Self-talk | • PA advice should highlight the benefits of PA with less emphasis on PA as a treatment for a health problem. |
*Numbering refers to BCTTv1
Stakeholders from the second consultation rated all four VBIs from this preliminary short-list as being equally potentially effective, feasible, acceptable and low cost (see Table 2 and Figure 2). They also recommended: (i) including a follow-up consultation; (ii) emphasising everyday physical activities and that even small increases in PA can be beneficial; and (iii) removing the coping planning from VBI 2 as they felt that a five-minute consultation would not allow sufficient time to adequately problem solve any barriers to physical activity identified by participants.
Table 2.
Results of stakeholder consultation [round 2] (n = 18)
| Ratings of the effectiveness, feasibility, acceptability and cost items for the four short-listed VBIs: | Responses to open-ended questions about the four short-listed VBIs: |
|---|---|
| • There were no differences between VBIs in mean stakeholder ratings of the potential effectiveness, feasibility, acceptability and cost of the four short-listed VBIs (see Figure 2). | • Stakeholders felt that the proposed VBIs could, on the whole, be: deliverable in 5 minutes; acceptable; effective; and affordable. |
| • The mean rating of all seven items was very similar for all VBIs: | • No other potential VBIs or BCTs were identified that could be administered in a health check. |
| • VBI 1(Motivational) mean = 3.54 | • Twelve out of 18 stakeholders suggested incorporating some kind of follow-up session (e.g. telephone or face-to-face). |
| • VBI 2(Action planning) mean = 3.50 | • Five stakeholders suggested emphasising that everyday physical activities (e.g. gardening, brisk walking, etc.) count towards physical activity recommendations and that any increase is beneficial. |
| • VBI 3(Pedometer) mean = 3.57 | • Two academic stakeholders and one PPI panel member suggested removing the ‘coping planning’/problem solving component from VBI 2 (Action/Coping planning). |
| • VBI 4(Diary) mean = 3.67 |
Figure 2.
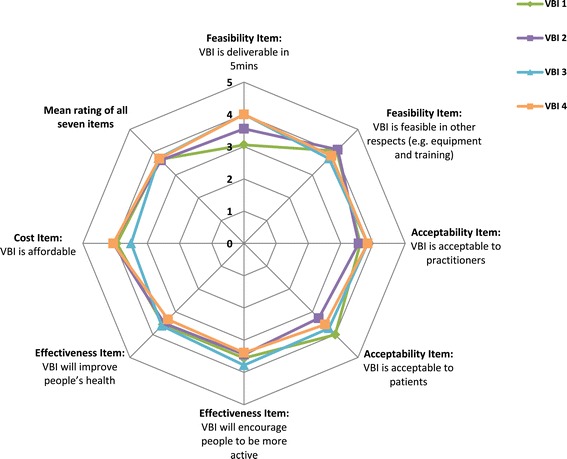
Stakeholders’ ratings of the potential effectiveness, feasibility, acceptability and cost of the four short-listed VBIs. Figure shows stakeholders’ mean ratings of agreement with seven items relating to the potential effectiveness, feasibility, acceptability and cost of the four short-listed VBIs. Agreement was rated on a 5-point scale ranging from 1 (Strongly disagree) to 5 (Strongly agree).
Following the second round of stakeholder consultation, the research team modified the preliminary short-list of VBIs according to the recommendations made by stakeholders. However, adding a follow-up session was considered to be unfeasible given the time and resource constraints of the NHS health checks. A detailed description of the final four VBIs short-listed for evaluation in the feasibility study can be found in Table 3, along with a list of component BCTs in each VBI.
Table 3.
Content and component BCTs of the four VBIs evaluated in the feasibility study
| General VBI content | ||||
|---|---|---|---|---|
| Face-to-face discussion content | Practitioner: | |||
| • Asks the participant if they are aware of the current PA recommendations. | ||||
| • Informs the participant that the recommendations are for a minimum of 30 minutes of moderate-intensity activity on 5 or more days of the week, and emphasises that moderate PA is any activity that raises heart rate, breathing or sweating and includes the activities of daily living. | ||||
| • Gives feedback on current PA and informs the participant of whether they are meeting the PA recommendations. | ||||
| VBI-specific content | ||||
| VBI 1 Motivational | VBI 2 Action planning | VBI 3 Pedometer | VBI 4 PA diary | |
| Face-to-face discussion content | Practitioner: | Practitioner: | Practitioner: | Practitioner: |
| • Asks the participant if they can think of any benefits of increasing their PA. | • Asks the participant if they can think of any easy and/or enjoyable ways of increasing their PA; | • Gives information about the 10,000 steps per day recommendation. | • Asks the participant if they can think of any easy and/or enjoyable ways of increasing their PA. | |
| • Asks the participant if they can think of any easy and/or enjoyable ways of increasing their PA. | • Encourages the participant to write an action plan for increasing their PA on the Action Planning sheet. | • Shows the participant how to use the pedometer. | • Explains how to use the diary to self-monitor PA. | |
| • Encourages the participant to monitor the number of steps walked each day. | • Encourages the participant to write a PA goal for the coming week. | |||
| Participant materials | Motivational booklet containing: | Action planning sheet containing: | Pedometer booklet containing: | PA diary containing: |
| • Information PA recommendations. | • Information on the UK government PA recommendations. | • Information on the UK government PA recommendations. | • Information on the UK government PA recommendations. | |
| • Information about the health, social, environmental and emotional benefits of PA. | • Instructions on how to write an action plan. | • Instructions on how to use the pedometer and how to self-monitor daily steps. | • Instructions on how to use the diary. | |
| • Questions about importance and confidence for increasing PA. | • An example of an action plan for PA. | Pedometer: | • An example of a completed diary. | |
| • Tips for increasing PA (e.g. positive self-talk, social support, information on local PA resources). | • Three blank templates for creating an action plan. | • A Yamax Digiwalker SW200. | • A four week diary. | |
| Component BCTs* | 1.1, 1.4, 2.2, 3.1, 5.1, 5.3, 5.6, 15.4 | 1.1, 1.4, 2.2 | 1.1, 1.4, 2.2, 2.3, 4.1, 12.5 | 1.1, 1.4, 2.2, 2.3, 5.4 |
*Numbering refers to BCTTv1: 1.1 Goal setting (behaviour); 1.4 Action Planning; 2.2 Feedback on behaviour; 2.3 Self-monitoring of behaviour; 3.1 Social support (unspecified); 4.1 Instruction on how to perform the behaviour; 5.1 Information about health consequences; 5.3 Information about social and environmental consequences; 5.6 Information about emotional consequences; 12.5 Adding objects to the environment; 15.4 Self-talk.
(ii) Development of intervention and training procedures and materials for the short-listed VBIs
VBI procedures
The following materials were developed for each VBI: (i) a detailed procedure which described how each component of the VBI should be delivered; (ii) a brief procedure which was a shortened version that practitioners could use as a prompt during the health check; (iii) an example script which gave an example of VBI delivery; and (iv) written materials for the participant.
Training procedures
A two-hour training session was developed, accompanied by a training manual. The training manual contained: (i) information about study aims and procedures; (ii) information about the importance of promoting physical activity among adults attending health checks; (iii) the detailed procedure, brief procedure, example script and participant materials for each VBI; and (iv) information about good communication principles to encourage behaviour change. The first round of practitioner training revealed that it was necessary to extend training time to three hours. Two researchers introduced the training manual and demonstrated each VBI in role-play. Each practitioner then practised delivering each VBI (role play) and was given feedback on their performance.
Stage 2: Feasibility study of short-listed very brief interventions
(i) Fidelity, feasibility and acceptability of VBI procedures and materials
Practitioners and participants
Six practitioners (one PN and five HCAs) from three primary care practices were trained to deliver the four VBIs. One practice with two trained HCAs withdrew from the study before the start of participant recruitment.
In total, 68 participants were recruited between September 2012 and March 2013 (n = 32 from the first practice and n = 36 from the second practice) and randomised to receive one of the four VBIs. Mean age was 52.9 years [SD 9.5 years], 50% were female, 93% were white British, 54% were employed and 24% were retired. Randomisation resulted in equally balanced groups, except for VBI 1, which had a slightly lower percentage (75%) of white British participants (see Table 4). Sixteen participants received the Motivational intervention (VBI 1), 17 the Action Planning intervention (VBI 2), 18 the Pedometer intervention (VBI 3), and 17 the Physical Activity Diary intervention (VBI 4). Fifty-eight participants (84%) gave consent for their health check and VBI to be audio-recorded. All participants gave consent to be interviewed by a researcher immediately after the health check.
Table 4.
Baseline characteristics of feasibility study participants (total sample and by intervention group)
| Variable | Whole sample | VBI 1 | VBI 2 | VBI 3 | VBI 4 |
|---|---|---|---|---|---|
| Motivational | Action planning | Pedometer | Physical activity diary | ||
| N | 68 | 16 | 17 | 18 | 17 |
| Age mean (SD) years | 52.9 (9.5) | 52.2 (9.3) | 56.2 (11.5) | 52.9 (9.2) | 50.7 (8.0) |
| Gender % female | 50 | 55 | 44 | 53 | 50 |
| Ethnicity % white British | 93 | 75 | 94 | 100 | 100 |
| Occupation % employed/% retired | 54%/24% | 50%/19% | 47%/35% | 61%/28% | 59%/12% |
Feasibility
VBI Duration: Mean delivery time ranged from 4 minutes and 7 seconds for the physical activity diary intervention to 5 minutes and 28 seconds for the action planning intervention (Table 5).
Table 5.
Mean VBI duration, fidelity scores and participant engagement for each very brief intervention
| Variable | VBI 1 | VBI 2 | VBI 3 | VBI 4 |
|---|---|---|---|---|
| Motivational | Action planning | Pedometer | Physical activity diary | |
| N (useable recordings) | 11 | 16 | 17 | 14 |
| VBI duration in minutes and seconds/mean (SD) | 5 m 10 s (1 m 54 s) | 4 m 52 s (1 m 08 s) | 5 m 28 s (1 m 33 s) | 4 m 07 s (1 m 01 s) |
| PA recommendations & feedback score*/mean (SD) | 6.3 (1.5) | 6.6 (1.3) | 7.1 (0.9) | 6.4 (2.1) |
| VBI-specific Score*/mean (SD) | 4.2 (1.7) | 4.2 (1.6) | 5.2 (1.5) | 4.2 (1.8) |
| Overall Fidelity Score**/mean (SD) | 10.5 (2.9) | 10.8 (2.4) | 12.3 (2.2) | 10.6 (3.3) |
| Participant engagement §/mean (SD) | 3.0 (0.6) | 3.3 (0.9) | 3.5 (0.7) | 3.1 (0.8) |
*Possible scores range from 0–8
**Possible scores range from 0–16
§Possible scores range from 1–5
VBI Fidelity: Mean values for the three fidelity scores are given in Table 5. Mean Overall Fidelity (which was the mean proportion of VBI components that were delivered) ranged from 10/16 for the Motivational VBI to 12/16 for the Pedometer VBI. The fidelity coding also revealed that no participant who received the Action Planning VBI wrote down an action plan during the consultation.
Practitioner (n = 4) interviews (lasting 25–45 minutes) revealed that practitioners felt that all VBIs could be delivered within 5 minutes as part of the HC. Practitioners also reported that they found the Pedometer VBI marginally easier to deliver than the other three VBIs, but that all VBIs were easy to deliver.
Acceptability
Participant engagement: Mean values of participant enthusiasm for each VBI are given in Table 5 and ranged from 3.0 in VBI 1 (Motivational) to 3.5 in VBI 4 (Pedometer).
Practitioner and participant interviews (lasting 5–15 minutes) revealed that all participants and practitioners reported that the health check was a good time to discuss PA and that all VBIs were acceptable to participants and practitioners. However, there were some differences in the acceptability of the VBIs as practitioners reported that the pedometer VBI appeared to be slightly more acceptable to participants, and participants who received VBI 1 (Motivational) or VBI 2 (Action Planning) more often reported that the VBI was tailored than participants who received VBI 3 (Pedometer) or VBI 4 (Physical Activity Diary); and (iii) Many participants who received VBI 2, VBI 3 or VBI 4 (but not VBI 1) reported that they would have liked to have been given more tips and ideas about how to increase PA, and participants who received VBI 4 (but not those who received VBIs 1, 2 or 3) reported that they would have liked a follow-up appointment to get feedback on their completed diary. Practitioners reported that they felt that the potential effectiveness and acceptability of each VBI was dependent on the individual participant’s needs, and that they wanted a choice about which VBI to deliver to each participant. For instance, the Pedometer VBI would be more effective and acceptable for participants who want to walk more, and the Motivational VBI for participants who are ambivalent about increasing their PA.
(ii) Decision of which VBIs (or combinations of VBIs) to evaluate further in a pilot trial
Following appraisal of the evidence, the research team reached a consensus that all four VBIs were deliverable in around five minutes as part of the NHS health check, were feasible in other aspects of delivery (for example, content fidelity) and practitioner training, and were acceptable to participants and practitioners. However, other key findings from the feasibility study led the researchers to conclude that combining techniques from the four VBIs might increase the potential effectiveness, feasibility and acceptability of the VBIs.
First, the qualitative study in stage 1 showed that participants wanted tailored PA advice, and the feasibility study showed that participants perceived the Motivational and Action Planning VBIs as tailored. However, no participant receiving the Action Planning VBI wrote an action plan during the consultation, and this might reduce its potential future impact. Therefore, the team decided to drop action planning as a standalone intervention and to integrate the technique in the written materials of the Motivational VBI.
Second, practitioners reported that they found the Pedometer VBI marginally easier to deliver than the other VBIs and also felt that this VBI was more acceptable to participants. However, participants who received the Pedometer VBI wanted more tips and ideas of how to increase PA. Consequently, the team decided to retain the Pedometer VBI with the addition of the tips and ideas from the written materials of the Motivational VBI.
Third, many participants who received the Physical Activity Diary VBI reported that they would have liked a follow-up appointment to get feedback on their completed diary. Because a follow-up appointment would not meet the definition of a very brief intervention, and as participants who received the other three VBIs did not mention a follow-up session, the research team decided to drop the physical activity diary as a standalone intervention and to incorporate the physical activity diary into the Motivational and Pedometer VBIs.
Finally, practitioners reported that they felt that the potential effectiveness and acceptability of each VBI was dependent on the individual participant’s needs and that they wanted a choice about which VBI to deliver to each participant. Although multiple VBIs will be tested in a future pilot trial, the aim of the pilot trial will be to select a single intervention for evaluation in an RCT. The team therefore decided that offering a choice of VBIs was not feasible and instead decided to combine a larger range of techniques within a single VBI.
To accommodate the above findings, the research team decided to combine the four VBIs into three VBIs to be taken forward for further evaluation in a large pilot trial:
The Motivational VBI was amended to include an action planning sheet and a physical activity diary for goal-setting and self-monitoring of physical activity.
The Pedometer VBI was amended to include tips and ideas for increasing daily steps, as well as a step chart (akin to a physical activity diary) for goal-setting and self-monitoring of daily steps.
The amended Motivational and Pedometer VBIs (1 and 2 above) were combined into a single VBI so that it included a wider range of techniques.
Discussion
We identified and developed very brief interventions (VBIs) for physical activity that could be delivered in preventive consultations (NHS health checks). Using a two-stage approach we identified and developed four promising and well-characterised VBIs for physical activity. The feasibility study showed that all four VBIs could be delivered in approximately five minutes as part of the health check, could be delivered with moderate to good fidelity, and were acceptable to participants and practitioners. We found that combining techniques from the four VBIs might increase their potential effectiveness, feasibility and acceptability, and therefore selected a combined Motivational/Pedometer VBI alongside a Motivational and Pedometer VBI alone, respectively, for further evaluation in a pilot trial. The pilot trial will examine their potential efficacy for increasing objective and self-reported physical activity, feasibility (including delivery time and fidelity) and acceptability to participants and practitioners.
Although participants and practitioners found all four VBIs acceptable, the fidelity assessment showed that on average participants were ambivalent to somewhat enthusiastic about the VBIs. However, by definition opportunities for active engagement were limited to five minutes, participants had positive views about the VBIs immediately after their delivery, and the interviews or audio-recordings of consultations did not suggest how participant engagement could be increased.
Current literature supports their use of brief interventions [4-6,8] and favours the use of supplements (e.g. written materials) to brief advice [16], but highlights uncertainty about the effectiveness, feasibility and acceptability of very brief interventions [4-6,16]. We focused on selecting and developing very brief interventions (VBIs) that could be delivered in a preventive health check and defined a VBI as any intervention consisting of a single session lasting no more than 5 minutes. Our findings have advanced the evidence base about VBIs for physical activity, where very few VBIs existed with poorly described active ingredients [16]. We identified four promising, well-characterised VBIs and showed that all four VBIs are feasible and acceptable when delivered by health care practitioners as part of a preventive consultation.
Our study had a number of strengths. First, selecting BCTs based on evidence for their potential effectiveness, feasibility, acceptability and cost enabled us to develop a number of promising VBIs, given the lack of evidence about how to select BCTs to target theoretical constructs [15]. Second, this approach enabled the development of VBIs that were practicable as well as potentially effective. Finally, we developed and tested multiple VBIs simultaneously, rather than a best-bet VBI only.
Key challenges of using our approach were deciding which criteria should be used to select interventions, what evidence should be collected to inform those criteria, and whether and how criteria should be weighted when short-listing interventions. We identified four key selection criteria (effectiveness, feasibility, acceptability and cost) at the outset, and used an iterative approach to combine evidence and expertise from multiple sources. We decided that, given the primary care context, feasibility and acceptability should be considered to be of equal importance as effectiveness and cost. Future research may identify other criteria depending on context, behaviour and target group, e.g. the potential to reduce health inequalities, and might also develop a more refined approach to weighting criteria.
Finally, this approach was also challenging in terms of the practicalities of evaluating several interventions in the context of routine primary care. For example, it increased the burden on practitioners, who were trained in four VBIs within limited time, and had to randomise delivery of each VBI. We addressed the latter by randomising VBI delivery by week rather than by participant, and produced a brief script for each VBI to guide delivery. Future research may identify other ways to deal with these challenges, such as clustering by practice or practitioner, though it is likely that this would increase the sample size significantly.
We recommend that anyone using this approach to intervention development defines a priori: key selection criteria (tailored to context, target population and target behaviour); the evidence needed to inform those criteria; and the method for weighting/combining the criteria. We also recommend that the practical challenges posed by combining multiple sources of evidence and testing multiple interventions simultaneously are considered at the outset when deciding how many interventions to shortlist and evaluate further.
Conclusions
Using a two-stage approach, in which we considered the practicability of VBIs (acceptability, feasibility and cost) as well as potential efficacy from the outset, we developed and tested the feasibility of four promising VBIs for physical activity and demonstrated that all were acceptable and feasible as part of routine preventive health checks in primary care.
Acknowledgements
This study was conducted on behalf of the Very Brief Interventions Programme team (see http://www.phpc.cam.ac.uk/pcu/research/research-projects-list/vbi/vbi-research-team/ for team members). We thank study participants, participating GP practice teams and practitioners who delivered the interventions; Laura Lamming and Dan Mason for leading the systematic reviews; the programme management team (Simon Griffin and Ann Louise Kinmonth); the qualitative research team (Simon Cohn and Philip Miles); all individuals who took part in our stakeholder consultations for their contributions to the development of the interventions; Richard Parker and Toby Prevost for their advice on study design and statistical guidance; the East of England Primary Care Research Network (Kim Fell) for their help with practice recruitment. This paper presents independent research funded by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research Programme (Grant Reference Number RP-PG-0608-10079). The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. The funder had no role in study design, data collection, data analysis, data interpretation, the writing of the manuscript, and decision to submit the manuscript for publication.
Abbreviations
- BI
Brief intervention
- PA
Physical activity
- VBI
Very brief intervention
- BCT
Behaviour change technique
- BCTTv1
Behaviour change technique taxonomy version 1
- HC
Health check
- PN
Practice nurse
- HCA
Health care assistant
- NHS
National Health Service
- MRC
Medical Research Council
Additional files
Stakeholder Consultation [Round 1].
Qualitative Research Patient Interview Topic Guide.
Table of Likert-type Items and Open-ended questions from the Stakeholder Consultation [Round 2].
Fidelity Coding Items.
Participant and Practitioner Interview Topic Guides.
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
All authors contributed to the development of the interventions, led by WH and SS. SP, KM and MB collected the data used in the feasibility study. All authors were involved in analysing and interpreting the data. SP and WH drafted the manuscript. All authors read, contributed to and approved the final manuscript.
Contributor Information
Sally Pears, Email: sp643@medschl.cam.ac.uk.
Katie Morton, Email: km576@medschl.cam.ac.uk.
Maaike Bijker, Email: mab91@medschl.cam.ac.uk.
Stephen Sutton, Email: srs34@medschl.cam.ac.uk.
Wendy Hardeman, Email: wh207@medschl.cam.ac.uk.
References
- 1.World Health Organization. Global recommendations on physical activity for health. 2010. http://whqlibdoc.who.int/publications/2010/9789241599979_eng.pdf. Accessed 2 April 2015. [PubMed]
- 2.Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Lancet Physical Activity Series Working Group. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380(9838):219–29. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chaudhury M, Esliger D. Accelerometry in adults. In: Craig R, Mindell J, Hirani V, editors. Health Survey for England 2008: Physical activity and fitness, 1. London: National Centre for Social Research; 2008. pp. 61–88. [Google Scholar]
- 4.National Institute for Health and Care Excellence. Physical activity: brief advice for adults in primary care. NICE public health guidance 44. 2013. https://www.nice.org.uk/guidance/ph44. Accessed 2 April 2015.
- 5.Campbell F, Blank L, Messina J, Day M, Wood HB, Payne N et al. Physical activity: Brief advice for adults in primary care. Published Online First. 2012. [http://www.nice.org.uk/guidance/ph44/resources/physical-activity-brief-advice-for-adults-in-primary-care-review-of-effectiveness-and-barriers-and-facilitators2]
- 6.NICE Public Health Collaborative Centre - Physical Activity. A rapid review of the effectiveness of brief interventions in primary care to promote physical activity in adults. 2006. https://www.nice.org.uk/guidance/ph2/evidence/brief-interventions-review-25-jan-20062. Accessed 2 April 2015.
- 7.Public Health England. NHS Health Check implementation review and action plan. 2013. https://www.gov.uk/government/publications/nhs-health-check-implementation-review-and-action-plan on_review_and_action_plan.pdf. Accessed 2 April 2015.
- 8.Orrow G, Kinmonth AL, Sanderson S, Sutton S. Effectiveness of physical activity promotion based in primary care: systematic review and meta-analysis of randomised controlled trials. BMJ. 2012;344 doi: 10.1136/bmj.e1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behaviour change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behaviour change interventions. Ann Behav Med. 2013;46(1):81–95. doi: 10.1007/s12160-013-9486-6. [DOI] [PubMed] [Google Scholar]
- 10.Craig N, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337:a1655. doi: 10.1136/bmj.a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Belanger-Gravel A, Godin G, Amireault S. A meta-analytic review of the effect of implementation intentions on physical activity. Health Psychology Review. 2013;7:23–54. doi: 10.1080/17437199.2011.560095. [DOI] [PubMed] [Google Scholar]
- 12.Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol. 2009;28(6):690–701. doi: 10.1037/a0016136. [DOI] [PubMed] [Google Scholar]
- 13.Bravata DM, Smith-Spangler C, Sundaram V, Gienger AL, Lin N, Lewis R, et al. Using pedometers to increase physical activity and improve health: A systematic review. JAMA. 2007;298:2296–304. doi: 10.1001/jama.298.19.2296. [DOI] [PubMed] [Google Scholar]
- 14.Kang M, Marshall SJ, Barreira TV, Lee JO. Effect of pedometer-based physical activity interventions: a meta-analysis. Res Q Exerc Sport. 2009;80(3):648–55. doi: 10.1080/02701367.2009.10599604. [DOI] [PubMed] [Google Scholar]
- 15.Michie S, Johnston M. Theories and techniques of behaviour change: Developing a cumulative science of behaviour change. Health Psych Rev. 2012;6(1):1–6. doi: 10.1080/17437199.2012.654964. [DOI] [Google Scholar]
- 16.Lamming L, Mason D, Wilson E, Singh GCV, Sutton S, Hardeman W. Very brief interventions to increase physical activity: a systematic review of reviews. Psychol Health. 2012;27:76. [Google Scholar]
- 17.Mason D, Lamming L, Wilson E, Singh GCV, Pears S, Morton K, et al. The effectiveness and cost-effectiveness of pedometers to increase physical activity: a systematic review and meta-analysis. Psychol Health. 2012;27:85–6. [Google Scholar]
- 18.Fair A. The Role of Self-Monitoring in Increasing Physical Activity. PhD Thesis. University of Cambridge, Department of Public Health and Primary Care; 2011.
- 19.Shaw R, Fenwick E, Baker G, McAdam C, Fitzsimons C, Mutrie N. ‘Pedometers cost buttons’: the feasibility of implementing a pedometer based walking programme within the community. BMC Public Health. 2011;11:200. doi: 10.1186/1471-2458-11-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Curtis L. Unit Costs of Health and Social Care 2011. Canterbury: Personal Social Services Research Unit, University of Kent; 2007. [Google Scholar]


