Abstract
Background
Saliva is increasingly promoted as an alternative diagnostic bio-sample to blood; however its role in respiratory disease requires elucidation. Our aim was to investigate whether C-reactive protein (CRP), procalcitonin (PCT) and neutrophil elastase (NE) could be measured in unstimulated whole saliva, and to explore differences between COPD patients and controls with normal lung function. We also determined the relationship between these salivary biomarkers and self-reported COPD-relevant metrics.
Methods
Salivary CRP, PCT and NE levels were measured at each of 3 visits over a 14-day period alongside spirometry and a daily self-assessment dairy in 143 subjects: 20 never-smokers and 25 smokers with normal spirometry; 98 COPD patients [GOLD Stage I, 16; Stage II, 32; Stage III, 39; Stage IV, 11]. Twenty-two randomly selected subjects provided simultaneous blood samples.
Results
Levels of each salivary biomarker could distinguish between the above cohorts. Significant differences remained for salivary CRP and NE (p < 0.05) following adjustment for age, gender, sampling time, gum disease and total co-morbidities; but not for BMI except for salivary NE, which remained higher in smokers compared to non-smokers and stable COPD subjects (p < 0.001). Patients with acute COPD exacerbations had a median increase in all 3 salivary biomarkers (p < 0.001); CRP: median 5.74 ng/ml, [interquartile range (IQR) 2.86–12.25], PCT 0.38 ng/ml, [IQR 0.22–0.94], and NE 539 ng/ml, [IQR 112.25–1264]. In COPD patients, only salivary CRP and PCT levels correlated with breathing scores (r = 0.14, p < 0.02; r = 0.13, p < 0.03 respectively) and sputum features but not with activities of daily living. Salivary CRP and PCT concentrations strongly correlated with serum counterparts [r = 0.82, (95 % CI: 0.72–0.87), p < 0.001 by Spearman’s; and r = 0.53, (95 % CI: 0.33–0.69), p < 0.006 respectively]; salivary NE did not.
Conclusions
CRP, PCT and NE were reliably and reproducibly measured in saliva, providing clinically-relevant information on health status in COPD; additionally NE distinguished smoking status. All 3 salivary biomarkers increased during COPD exacerbations, with CRP and PCT correlating well with patient-derived clinical metrics. These results provide the conceptual basis for further development of saliva as a viable bio-sample in COPD monitoring and exacerbation management.
Electronic supplementary material
The online version of this article (doi:10.1186/s12931-015-0219-1) contains supplementary material, which is available to authorized users.
Keywords: Salivary biomarkers, C-reactive protein, Procalcitonin, Neutrophil elastase, COPD, COPD exacerbation, wellbeing parameters
Introduction
Saliva is increasingly used as a non-invasive easily accessible bio-sample for point-of-care diagnostics instead of blood [1, 2] to inform on infection [3–7], drugs [8] and disease states [9–18], including airways inflammation. Salivary eosinophil cationic protein can differentiate between asthmatic and healthy subjects [19]. Increased salivary CRP and haptoglobin levels are demonstrated in childhood allergic asthma [20]; raised salivary leukotriene levels differentiate aspirin-intolerant asthmatics from tolerant counterparts [21].
Biomarkers in various body fluids have been associated with Chronic Obstructive Pulmonary Disease (COPD) pathogenesis and clinical outcome [22, 23]. Serum and sputum CRP are elevated in COPD patients and healthy smokers [24, 25], with moderate inverse correlation of serum CRP to Forced Expiratory Volume in 1 s (FEV1) [26]. Serum CRP increases during exacerbations [27–32]; with high levels at 14 days post-exacerbation predicting re-exacerbation within 50 days and poor outcome [33]. Serum Procalcitonin (PCT) shows strong correlation to bacterial exacerbations [34], guiding antibiotic prescriptions [29, 35]. Neutrophil elastase (NE), mediator of airway pathogenesis [36, 37], is known to be elevated in smokers [38] and COPD patients [39], has a negative correlation with FEV1 in patients with expiratory volumes below 40 % predicted [40] and increases further during exacerbations [41].
The importance of CRP, PCT and NE in COPD has been clearly demonstrated. Yet despite the merits that saliva could offer to practical monitoring of COPD and its exacerbations, only two studies have explored its potential clinical role [42, 43]. The aim of our study was therefore to investigate levels of CRP, PCT and NE in unstimulated whole saliva using commercially-validated and modified enzyme-linked immunoassays (ELISA) and to determine differences between patients with COPD and controls with normal lung function. Target biomarkers were measured at 3 time points within a 14-day period. As smoking can influence steady-state biomarker levels [44], control groups included life-long never-smokers and current smokers. COPD data were analysed relative to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) stage (percentage predicted FEV1) [45], which alongside MRC scores and self-assessment scores provided information for correlations between target salivary biomarkers and COPD-relevant clinical metrics. For further validation, randomly chosen participants also provided simultaneous blood samples.
Materials & methods
Subject characteristics and study design
From January 2010 to March 2012, individuals were recruited consecutively from our research and outpatient clinic databases to one of 3 cohorts: life-long never-smokers (NS group); current smokers (S group; with > 20 pack years); or COPD, confirmed by spirometry according to GOLD criteria [45]. Patients with other respiratory disorders were excluded. All NS and S subjects had normal lung function. Participants were monitored over 14 days (3 visits, one week apart). At visit 1, demographic details were recorded (Table 1) (Additional file 1: Table S1); participants with any infection or unstable illness in the preceding 6 weeks were excluded. On each visit, the Medical Research Council (MRC) dyspnoea score was recorded [46], spirometry (Koko Legend, nSpire, USA) performed and unstimulated whole saliva collected (2 ml). Participants completed a daily self-assessment diary (Additional file 2) [47], incorporating scores on breathing, activities of daily living (ADL), sputum features and cough presence. In-between scheduled visits, patients were asked to contact the researchers on developing any change in symptoms. An exacerbation was defined as an increase in respiratory symptoms for two consecutive days, with at least two major symptoms (dyspnoea, sputum purulence, sputum volume) or a major plus a minor symptom (wheeze, cold, sore throat, cough) [48]. Randomly-selected subjects provided simultaneous saliva and blood samples. The study was approved by the local research ethics committee [REC project reference: 09/H1203/77]; all participants gave informed written consent.
Table 1.
Subject Demographics, Salivary Biomarker & Symptom Profiles
| Control Subjects (n = 45) | Stable COPD Subjects (n = 62) | P value | ||||||
|---|---|---|---|---|---|---|---|---|
| NS | S | I | II | III | IV | |||
| (n = 20) | (n = 25) | (n = 62) | (n = 12) | (n = 19) | (n = 25) | (n = 6) | ||
| Demographics | ||||||||
| Age, a years | 53 ± 17 | 42 ± 12 | 67 ± 7 | 65 ± 10 | 64 ± 8 | 68 ± 5 | 72 ± 4 | <0.001 |
| Gender, male (female) | 7 (13) | 17 (8) | 34 (28) | 4 (8) | 12 (7) | 13 (12) | 5 (1) | n/a |
| FEV1, a % predicted | 98.1 ± 3.7 | 99.7 ± 4.7 | 55.7 ± 22.0 | 90.4 ± 9.2 | 64.4 ± 7.6 | 44.1 ± 3.7 | 25.1 ± 4.2 | <0.001 |
| BMI, a (kg/m2) | 29.8 ± 3.6 | 25.4 ± 3.3 | 27.3 ± 7.8 | 28.0 ± 7.0 | 28.6 ± 2.6 | 27.3 ± 1.9 | 19.8 ± 3.6 | <0.379 |
| Co Morbidities | ||||||||
| Nil | 15 | 20 | 27 | 9 | 10 | 5 | 3 | n/a |
| Gum Disease | 2 | 0 | 1 | 0 | 0 | 1 | 0 | n/a |
| Cardiac | 3 | 3 | 31 | 2 | 7 | 19 | 3 | n/a |
| Type 2 Diabetes | 1 | 2 | 10 | 1 | 2 | 7 | 0 | n/a |
| Treatment | ||||||||
| B2 Agonists (Short Acting) | 9 | 19 | 25 | 6 | ||||
| B2 Agonists (Long Acting) | 8 | 16 | 25 | 6 | ||||
| Anticholinergic (Short Acting) | 1 | 2 | 3 | 0 | ||||
| Anticholinergic (Long Acting) | 3 | 8 | 18 | 5 | ||||
| Inhaled Steroid | 8 | 17 | 25 | 6 | ||||
| Oral Theophyllines | 0 | 1 | 7 | 2 | ||||
| Symptom & Sputum Metricsb | ||||||||
| MRC Score | 1.00, 0.25 | 1.00, 0.25 | 4.00, 1.67 | 3.00, 2.25 | 4.00, 1.50 | 5.00, 1.00 | 5.00, 0.00 | <0.001 |
| Breathing Score | 2.00, 1.00 | 2.00, 0.25 | 3.00, 0.00 | 3.00, 1.00 | 3.00, 0.00 | 3.00, 0.00 | 3.00, 0.75 | <0.001 |
| ADL Score | 1.00, 0.00 | 1.00, 0.00 | 3.00, 2.00 | 1.00, 2.00 | 3.00, 2.00 | 4.00, 2.33 | 3.00, 1.50 | <0.001 |
| Sputum Amount | 1.00, 0.00 | 1.00, 1.00 | 2.00, 2.00 | 1.50, 1.00 | 2.00, 1.84 | 3.00, 1.00 | 2.50, 2.50 | <0.001 |
| Sputum Texture | 1.00, 1.00 | 2.00, 0.00 | 2.00, 0.00 | 2.00, 0.50 | 2.00, 0.00 | 2.00, 0.00 | 2.00, 0.00 | <0.001 |
| Sputum Colour | 3.00, 0.00 | 3.00, 0.00 | 3.00, 1.00 | 3.00, 0.75 | 3.00, 0.83 | 3.00, 1.00 | 3.50, 1.00 | <0.001 |
| Salivary Biomarkers, b | ||||||||
| CRP, ng/ml | 0.89, 0.35 | 1.70, 1.07 | 1.66, 2.30 | 1.62, 1.36 | 2.44, 2.63 | 1.45, 2.34 | 2.34, 5.94 | <0.002 |
| PCT, ng/ml | 0.09, 0.03 | 0.13, 0.09 | 0.09, 0.04 | 0.10, 0.06 | 0.09, 0.04 | 0.09, 0.04 | 0.11, 0.03 | <0.012 |
| NE, ng/ml | 152, 96 | 408, 748 | 189, 508 | 227, 104 | 161, 491 | 189, 687 | 163, 181 | <0.001 |
I = GOLD stage I, II = GOLD stage II; III = GOLD stage III, IV = GOLD stage IV; ADL = Activity of Daily Living, COPD = Chronic Obstructive Pulmonary Disease; GOLD = Global Initiative for Chronic Obstructive Lung Disease; NS = healthy non-smoker; S = healthy smoker; FEV1 = Forced Expiratory Volume in 1 s; BMI = Body Mass Index; ex = ex-smokers; CRP = C-Reactive Protein; PCT = Procalcitonin; NE = Neutrophil Elastase. Data are presented as: a, Mean ± standard deviation; b, Median, inter-quartile range. Exacerbation frequency is divided into 3 groups: Group 1 = 1–3, Group 2 = 4–6, Group 3 = >6. P values represent the difference between controls and stable COPD subjects. No significant difference was found across COPD severity defined by GOLD for: Age, BMI, CRP, PCT, NE, Breathing Score, Sputum Texture and Sputum Colour: (p < 0.379; p < 0.403; p < 0.559; p < 0.946; p < 0.620; p < 0.127; p < 0.228; p < 0.824). FEV1 significantly decreased as COPD severity increased (p < 0.001), whilst MRC, ADL and Sputum Amount significantly increased: (p < 0.001; p < 0.002; p < 0.011 respectively)
Unstimulated whole saliva collection protocol
Participants were asked to abstain from alcohol for at least 12 h; fast for 2 h; refrain from brushing their teeth and smoking for 30 min, prior to providing saliva samples. Oral hygiene was checked and mucosal examination performed at each visit. All visit samples were collected at same time of day for each subject.
Immediately before collection participants rinsed their mouths with 10mls water; they then sat in an upright position, tilted their heads forward, and allowed saliva to pool in the mouth before passively drooling into an ice-cooled marked sterile tube (Nunc, Denmark) up-to a total of 2mls.
Collected saliva samples were transported on ice and stored at − 80 °C until analysis. Prior to analysis, thawed saliva was centrifuged at 3000 revolutions per minute (RPM) for 15 min. Sample measurements were undertaken within 3 months of storage; all biomarker assays were performed in duplicate. All saliva samples were tested for blood contamination using an 8-parameter urine dip test strip (Bayer AG, USA). Briefly, 10ul of saliva was aliquoted onto the reagent square for blood, with the colour change after 5 s being read on the key and documented.
Analysis of biomarkers in saliva
CRP was measured in 15ul of saliva using a salivary ELISA kit (Salimetrics Europe, UK) with a detection limit of 0.90 ng/ml; lower concentrations were assigned as 0.89 ng/ml.
Levels of PCT and NE in saliva were measured following in-house modification of commercially-available ELISAs [49].
Briefly, for adapting the VIDAS® BRAHMS PCT (bioMérieux, France) for use in saliva, pre-study experiments involved spiking saliva from non-smoker healthy subjects with PCT Control (provided by the manufacturer for assay calibration) in varying concentrations: 0.09–20 ng/ml. These spiked samples were analysed neat and in varying defined dilutions: 1:1, 1:2, 1:4, 1:8 using Phosphate Buffered Saline - Tween 20–0.05 % (PBS-T). Optimal recovery of PCT (85 %) at all concentrations occurred when saliva was diluted 1:2 in PBS-T. The manufacture’s test procedure for performing the assay was not altered. Thereafter, PCT was determined in 100ul of saliva diluted 1:2 in Phosphate Buffered Saline-Tween 20 − 0.05 % (PBS-T) using VIDAS® BRAHMS PCT (bioMérieux, France) with a detection limit of 0.10 ng/ml; lower concentrations were assigned as 0.09 ng/ml.
For adapting the PMN-Elastase ELISA Kit (Immundiagnostik AG, Germany) for use in saliva, we first spiked non-smoker healthy saliva with NE (provided by the manufacturer to calibrate the assay) in varying concentrations: 115–1000 ng/ml. These spiked samples were analysed in varying dilutions: 1:100, 1:200, 1:400, 1:800 using manufacturer-supplied ELISA wash buffer. Recovery of NE (90 %) was consistent across all 4 dilutions; for the study we elected to use a 1:200 dilution. The manufacture's test procedure for performing the assay was not altered. Thus, NE was measured in 7.0 ul of saliva diluted 1:200 in ELISA wash buffer using PMN-Elastase ELISA Kit (Immundiagnostik AG, Germany), with a detection limit of 70 ng/ml; lower concentrations were assigned as 69 ng/ml.
Analysis of biomarkers in blood
Peripheral blood was collected in supplement-free tubes and ethylene diaminetetra-acid vacutainer tubes (BD Bioscience, New Jersey, USA). Samples were then centrifuged at 2000 RPM for 15 min; retrieved serum was stored at 80 °C until analysis. Serum CRP was measured using ADVIA 2400 Chemistry System (Siemens AG, Germany) with detection limit of 0.3 mg/L. Serum PCT and NE were quantified using same assay kits as for saliva, but following manufacturers’ protocols. Serum levels were expressed as ng/ml except for CRP (mg/L). All assays were performed in duplicate.
Statistical analysis
Statistical analyses were performed using IBM SPSS Statistics Version 19 (SPSS Inc, IBM, USA). Parametric data are expressed as mean ± standard deviation (SD) and non-parametric as median, (inter-quartile range [IQR]). Between-group comparison was performed using Mann–Whitney U test, Kruskal-Wallis one-way analysis of variance (ANOVA) and for paired data, Wilcoxon Signed Ranks test. A Bonferroni Correction was applied when undertaking multiple comparison testing. Biomarker data were logarithmically transformed to allow Univariate Analysis and determination of covariate effect. Correlations were assessed by Spearman’s Rank correlation co-efficient (r). The reproducibility of salivary biomarker levels was explored using Bland-Altman plots expressing the change within a subject. A p value of <0.05 was considered significant.
Results
In total 143 individuals were recruited: 20 never-smokers (NS) and 25 current smokers, over 20 pack year history, (S) with normal lung function; 98 COPD patients (GOLD Stage I, 16; Stage II, 32; Stage III, 39; Stage IV, 11), all ex-smokers (>20 pack year history). Thirty-six COPD patients experienced an exacerbation during the course of the study; all controls remained clinically stable. Salivary CRP, PCT and NE were measured in all participants (Table 1) (Additional file 1: Table S1), with an intra-and inter-assay co-efficient of variances of <7 % and <12 % respectively for all 3 assays.
Biomarkers across health status
Only stable COPD patients (n = 62) were included in the between-group analyses. Salivary CRP differed between the 3 groups (p < 0.002 by ANOVA), with significant increase in COPD (median: 1.66 ng/ml; IQR: 2.55 ng/ml) compared to NS (0.89 ng/ml; 0.35 ng/ml, p < 0.001 by Mann Whitney U), but not to smokers (1.70 ng/ml; 1.07 ng/ml, p < 0.605). Smokers had higher salivary CRP than never-smokers (p < 0.001) (Fig. 1). These differences remained statistically significant (p < 0.05 by Univariate Analysis) following adjustment for age, gender, sampling time and total co-morbidities; but not for BMI (p < 0.402). The coefficient of variance for CRP variability within subjects was 13 %, 27 %, 15 % for NS, S and stable COPD respectively. The Bland‐Altman plot with upper and lower limits (1.96 Standard Deviation (SD)) combing all 3 groups (n = 107) showed good data consistency (difference between stable baseline values), with only 2 outliers (Fig. 2).
Fig. 1.
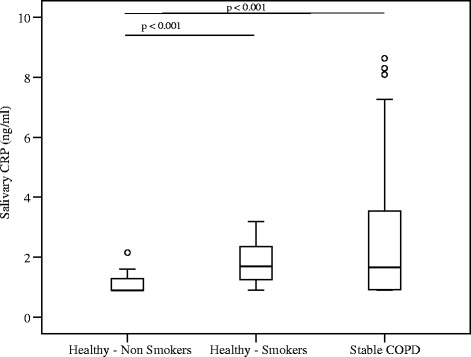
Salivary CRP levels from healthy non-smoker, healthy smokers and stable COPD subjects. The horizontal bar represents the median; the box length represents the interquartile range. Outliers are identified by o (1.5 x the interquartile range)
Fig. 2.
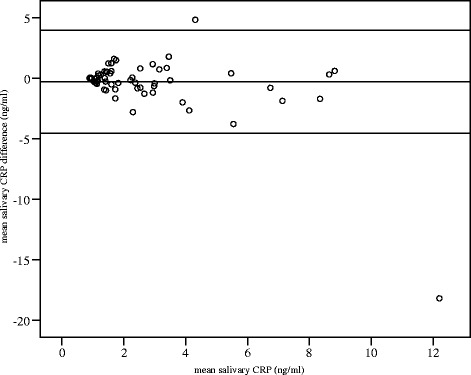
Bland-Altman plot of baseline salivary CRP levels across healthy non-smokers, health smokers and stable COPD. The upper and lower bars represent 1.96 Standard Deviations (SD) from the mean. Almost all replicates fell within the 95 % limits of agreement (difference between stable baseline values), with only 2 outliers
Salivary PCT differed between groups (p < 0.012). Salivary PCT was significantly elevated in smokers (0.13 ng/ml; 0.09 ng/ml) compared to NS (0.09 ng/ml; 0.03 ng/ml, p < 0.011) and COPD (0.09 ng/ml; 0.04 ng/ml, p < 0.01); but not between COPD and NS (p < 0.363) (Fig. 3). Following covariate adjustment, there was no significant difference (p < 0.564) between cohorts. Gender adjustment showed salivary PCT was generally lower in females, (0.11 vs. 0.14 ng/ml [males]: p < 0.05). The coefficient of variance for PCT variability within subjects was 19 %, 15 %, 14 % for NS, S and stable COPD respectively. The Bland‐Altman plot with upper and lower limits (1.96 SD) combing all 3 groups (n = 107) showed good data consistency, with only 4 outliers (Fig. 4).
Fig. 3.
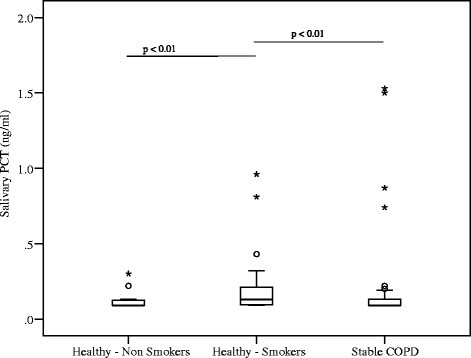
Salivary Procalcitonin (PCT) levels from healthy non-smokers, healthy smokers, stable COPD subjects. The horizontal bar represents the median; the box length represents the interquartile range. Outliers are identified by o (1.5 x the interquartile range) and * (3 x the interquartile range)
Fig. 4.
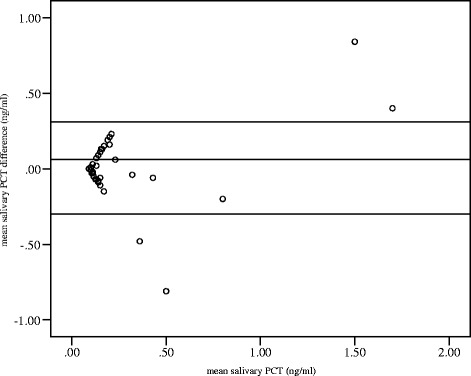
Bland-Altman plot of baseline salivary PCT levels across healthy non-smokers, health smokers and stable COPD. The upper and lower bars represent 1.96 Standard Deviations (SD) from the mean. Almost all replicates fell within the 95 % limits of agreement (difference between stable baseline values), with only 4 outliers
Differences in salivary NE were observed between cohorts (p < 0.001), irrespective of covariate adjustment (p < 0.011). Smokers had significantly raised NE (408 ng/ml; 748 ng/ml) compared to NS (152 ng/ml; 96 ng/ml, p < 0.001), and COPD patients (189 ng/ml; 508 ng/ml, p < 0.001); with no significant difference between NS and COPD (p < 0.235) (Fig. 5). Age appeared to affect salivary NE levels (p < 0.04), with around 60 ng/ml decline for every increasing decade in COPD patients, regardless of treatment. The coefficient of variance for NE variability within subjects was 32 %, 41 %, 37 % for NS, S and stable COPD respectively. The Bland‐Altman plot with upper and lower limits (1.96 SD) combing all 3 groups (n = 107) showed good consistency of data (difference between stable baseline values) with only 7 outliers (Fig. 6).
Fig. 5.
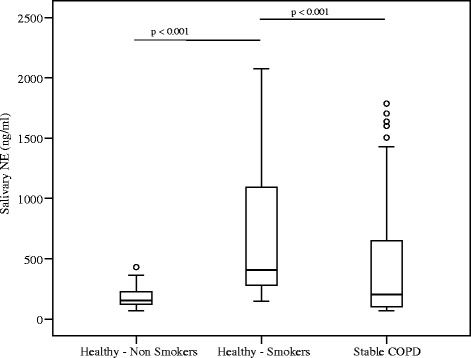
Salivary Neutrophil Elastase (NE) from healthy non-smokers, healthy smokers, stable COPD subjects. The horizontal bar represents the median; the box length represents the interquartile range. Outliers are identified by o (1.5 x the interquartile range)
Fig. 6.
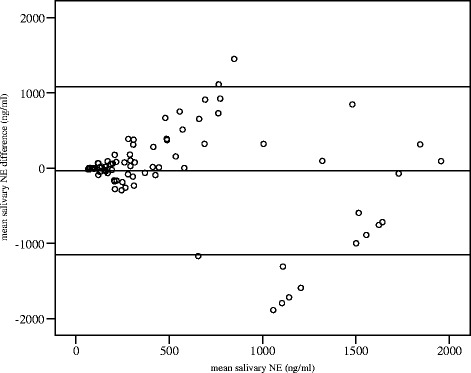
Bland-Altman plot of baseline salivary NE levels across healthy non-smokers, health smokers and stable COPD. The upper and lower bars represent 1.96 Standard Deviations (SD) from the mean. Almost all replicates fell within the 95 % limits of agreement (difference between stable baseline values), with only 7 outliers
No association was observed between salivary biomarkers and COPD severity, as determined by FEV1; CRP: p < 0.559; PCT: p < 0.946; NE: p < 0.620.
Subject-completed symptom scores
All participants completed a daily self-assessment symptom diary (Additional file 2), MRC scores significantly correlated with breathing scores (r = 0.55; 95 % Confidence Interval (CI): 0.34–0.70) and ADL (r = 0.47; 95 % CI: 0.25–0.64); p < 0.001 by Spearman’s.
Inter-group analysis demonstrated differences in all symptom scores between stable COPD, NS and S (p < 0.001). There was no significant difference between NS and S for any symptom metrics.
Analysis between salivary biomarkers and clinical metrics across participants (n = 143) revealed correlation of salivary CRP with ADL (r = 0.23, p < 0.02); sputum amount (r = 0.23, p < 0.02) and texture (r = 0.24, p < 0.02). Salivary PCT did not significantly correlate with any symptom. Salivary NE only correlated with MRC score (r = 0.29, p < 0.01).
Separate sub-analysis on all COPD patients (n = 98) (Tables 2 and 3) (Additional file 3: Table S2 & Additional file 4: Table S3) demonstrated salivary CRP correlated with MRC score (r = 0.16, p < 0.01), breathing score (r = 0.14, p < 0.02) (Fig. 7a, 7b) sputum amount (r = 0.15, p < 0.01), texture (r = 0.13, p < 0.03) and colour (r = 0.32, p < 0.001). Salivary PCT correlated with breathing score (r = 0.13, p < 0.04) (Fig. 7c), sputum amount (r = 0.13, p < 0.03) and colour (r = 0.23, p < 0.001). Salivary NE did not correlate with any clinical features. Sputum amount and colour correlated with breathing (r = 0.34, p < 0.001) and ADL scores (r = 0.34, p < 0.001); texture correlated only with ADL (r = 0.24, p < 0.001) (Table 4) (Additional file 5: Table S4).
Table 2.
Correlations of All COPD Subjects (n = 98) Symptom Scores vs. Salivary Biomarker Levels
| Symptom Scores | |||
|---|---|---|---|
| Salivary Biomarkers | Breathing Score | ADL Score | MRC Score |
| CRP | r = 0.142, p <0.02 | r = 0.105, p <0.08 | r = 0.164, p <0.006 |
| PCT | r = 0.125, p <0.04 | r = 0.115, p <0.06 | r = 0.04, p <0.444 |
| NE | r = 0.105, p <0.082 | r = 0.028, p <0.647 | r = -0.074, p <0.222 |
COPD = Chronic Obstructive Pulmonary Disease; FEV1 = Forced Expiratory Volume in 1 s; MRC = Medical Research Council; ADL = Activity of Daily Living; CRP = C-Reactive Protein; PCT = Procalcitonin; NE = Neutrophil Elastase. Data are presented as the Spearman’s correlation coefficient: r value
Table 3.
Correlations of All COPD Subject (n = 98) Sputum Metrics vs. Salivary Biomarker Levels
| Sputum Metrics | |||
|---|---|---|---|
| Salivary Biomarkers | Sputum Amount | Sputum Texture | Sputum Colour |
| CRP | r = 0.148, p <0.013 | r = 0.130, p <0.032 | r = 0.324, p <0.001 |
| PCT | r = 0.130, p < 0.033 | r = 0.107, p < 0.078 | r = 0.229, p < 0.001 |
| NE | r = 0.075, p < 0.219 | r = -0.118, p < 0.051 | r = 0.068, p < 0.266 |
COPD = Chronic Obstructive Pulmonary Disease; FEV1 = Forced Expiratory Volume in 1 s; MRC = Medical Research Council; ADL = Activity of Daily Living; CRP = C-Reactive Protein; PCT = Procalcitonin; NE = Neutrophil Elastase. Data are presented as the Spearman’s correlation coefficient: r value
Fig. 7.
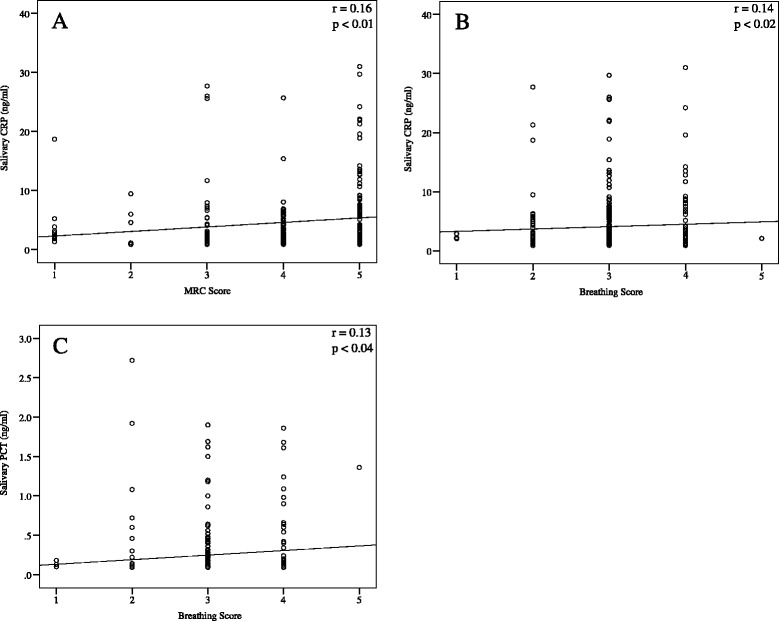
Scatter plot with a best fit line between COPD subject symptom scores and salivary biomarkers. a Salivary CRP vs. MRC score; b Salivary CRP vs. breathing score; c Salivary PCT vs. breathing score
Table 4.
Correlation of All COPD Subject (n = 98) Symptom Scores vs. Sputum Metrics
| Symptom Scores | |||
|---|---|---|---|
| Sputum Metrics | Breathing Score | ADL Score | MRC Score |
| Amount | r = 0.34, p < 0.001 | r = 0.34, p < 0.001 | r = 0.24, p < 0.001 |
| Texture | r = 0.07, p < 0.24 | r = 0.24, p < 0.001 | r = 0.31, p < 0.001 |
| Colour | r = 0.26, p < 0.001 | r = 0.19, p < 0.001 | r = 0.28, p < 0.001 |
COPD = Chronic Obstructive Pulmonary Disease; FEV1 = Forced Expiratory Volume in 1 s; MRC = Medical Research Council; ADL = Activity of Daily Living; CRP = C-Reactive Protein; PCT = Procalcitonin; NE = Neutrophil Elastase. Data are presented as the Spearman’s correlation coefficient: r value
COPD Stable vs. Exacerbation
Thirty-six COPD patients experienced an exacerbation at day 11 ± 3 (Table 5) (Additional file 6: Table S5). There was no difference in the median baseline exacerbation frequency (1–3 episodes per year) between these patients and those COPD patients that remained stable throughout the study. Comparison of their paired stable and pre-treatment exacerbation samples demonstrated significant elevation in all target salivary biomarkers at exacerbation (p < 0.001) (Figs. 8, 9, 10). Levels of CRP increased by 5.74 ng/ml (95 % CI: 3.72–11.47); PCT by 0.38 ng/ml, (95 % CI: 0.31–0.54) and NE by 539 ng/ml (95 % CI: 169–982); alongside a reduction in FEV1 (p < 0.001) and patient-recorded changes in sputum (amount: p < 0.001, texture: p < 0.05, colour: p < 0.001); ADL and breathing scores (p < 0.014 and p < 0.006 respectively) (Table 5) (Additional file 6: Table S5).
Table 5.
Same COPD Subjects in Stable and Exacerbation phase (n = 36) Demographics, Salivary Biomarker & Symptom Profiles
| Stable | Exacerbation | P value | |
|---|---|---|---|
| Demographics | |||
| Age, a years | 68 ± 9 | ||
| Gender, male (female) | 17 (19) | ||
| FEV1, a % predicted | 53 ± 23 | 48 ± 19 | < 0.001 |
| BMI, a (kg/m2) | 24.0 ± 6.3 | ||
| Co Morbidities | |||
| Nil | 5 | ||
| Gum Disease | 2 | ||
| Cardiac | 30 | ||
| Type 2 Diabetes | 4 | ||
| Treatment | |||
| B2 Agonists (Short Acting) | 35 | ||
| B2 Agonists (Long Acting) | 32 | ||
| Anticholinergic (Short Acting) | 5 | ||
| Anticholinergic (Long Acting) | 25 | ||
| Inhaled Steroid | 31 | ||
| Oral Theophyllines | 6 | ||
| Symptom & Sputum Metricsb | |||
| Increased Cough, n | 0 | 10 | < 0.001 |
| MRC Score | 5.00, 1.25 | 5.00, 1.25 | < 0.16 |
| Breathing Score | 3.00, 0.00 | 4.00, 1.00 | < 0.006 |
| ADL Score | 3.00, 1.00 | 4.00, 2.00 | < 0.014 |
| Sputum Amount | 2.00, 2.00 | 3.00, 2.25 | < 0.001 |
| Sputum Texture | 1.94, 0.33 | 2.06, 0.41 | < 0.001 |
| Sputum Colour | 3.00, 1.00 | 4.00, 0.41 | < 0.05 |
| Salivary Biomarkersb | |||
| CRP, ng/ml | 1.61, 1.10 | 7.35, 10.04 | < 0.001 |
| PCT, ng/ml | 0.09, 0.06 | 0.50, 0.71 | < 0.001 |
| NE, ng/ml | 128, 190 | 769, 1680 | < 0.001 |
COPD = Chronic Obstructive Pulmonary Disease; FEV1 = Forced Expiratory Volume in 1 s; BMI = Body Mass Index; ex = ex-smokers; MRC = Medical Research Council; ADL = Activity of Daily Living; CRP = C-Reactive Protein; PCT = Procalcitonin; NE = Neutrophil Elastase. Exacerbation frequency is divided into 3 groups: Group 1 = 1–3, Group 2 = 4–6, Group 3 = >6. Data are presented as: a, Mean ± standard deviation; b, Median, inter-quartile range. P values represent the difference between stable and exacerbation phases
Fig. 8.
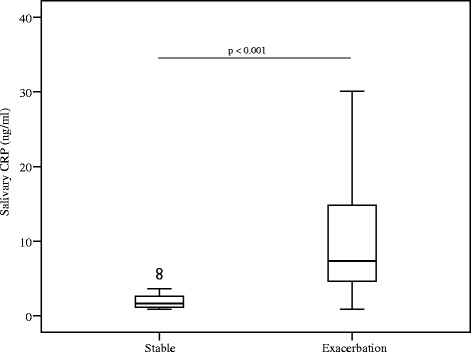
Salivary CRP levels from stable and the same COPD subjects during an exacerbation. The horizontal bar represents the median; the box length represents the interquartile range. Outliers are identified by o (1.5 x the interquartile range)
Fig. 9.
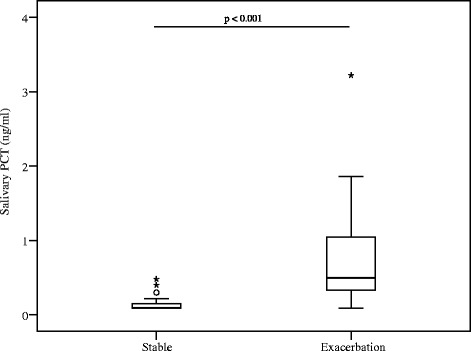
Salivary PCT levels from stable and the same COPD subjects during an exacerbation. The horizontal bar represents the median; the box length represents the interquartile range. Outliers are identified by o (1.5 x the interquartile range) and * (3 x the interquartile range)
Fig. 10.
Salivary NE levels from stable and the same COPD subjects during an exacerbation. The horizontal bar represents the median; the box length represents the interquartile range. Outliers are identified by o (1.5 x the interquartile range) and * (3 x the interquartile range)
Comparison of subject-matched saliva and serum biomarker levels
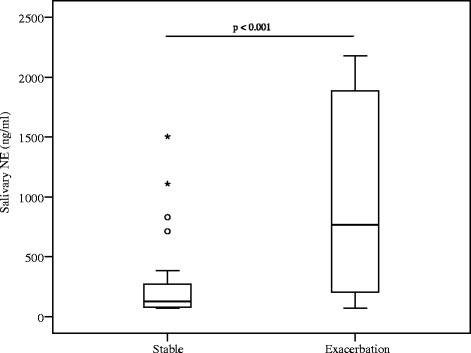
Relationships between saliva and serum biomarkers were studied in 22 randomly-selected subjects, providing a total of 66 paired saliva-serum samples. Salivary CRP was approximately 200 times lower than serum; salivary PCT and NE were about two-fold higher. Salivary CRP and PCT correlated with serum equivalents, r = 0.82, (95 % CI: 0.72–0.87), p < 0.001 by Spearman’s; and r = 0.53, (95 % CI: 0.33–0.69), p < 0.006 respectively (Fig. 11a, 11b). Salivary and serum NE did not correlate (r = −0.24, p < 0.25).
Fig. 11.
Scatter plot with a best fit line between same subject serum and salivary biomarkers. These subjects provided both serum and saliva samples on the same visit. a Salivary vs. serum CRP; b Salivary PCT vs. serum PCT; c Salivary PCT vs. serum CRP; d Salivary PCT vs. salivary CRP; e Salivary NE vs. salivary CRP; f Salivary NE vs. salivary PCT
Biomarker cross-analysis demonstrated salivary PCT correlated with serum and salivary CRP, r = 0.53, (95 % CI: 0.33–0.69), p < 0.006; and r = 0.73, (95 % CI: 0.59–0.83), p < 0.001 respectively (Fig. 11c, 11d). Salivary NE correlated with both salivary CRP, r = 0.45, (95 % CI: 0.23–0.63), p < 0.001, and salivary PCT, r = 0.58, (95 % CI: 0.39–0.72), p < 0.001 (Fig. 11e, 11f).
Discussion
As disease management shifts increasingly towards point-of-care, there is urgency to develop easier, less stressful sampling methods especially for monitoring chronic conditions. This is the first study to explore the potential role of salivary CRP, PCT and NE in COPD. Whilst a validated CRP saliva-based assay is available (Salimetrics®), we have also demonstrated that modification of existing body-fluid assays (PCT and NE) provides reproducible results for saliva [50].
Salivary biomarker targets in COPD patients of varying severity were compared to controls (never-smokers and smokers) under real world/working conditions; hence study participants with co-morbid conditions were included provided these were clinically stable at time of enrolment. To minimise across-cohort demographic variations and circadian influences, analysed measurements were then adjusted for potential covariate bias [51], including sampling times [52]. Non-smoker salivary CRP levels at 0.89 ng/ml (IQR 0.35 ng/ml) compared favourably to previous observations showing a healthy CRP range of 0.02–2.5 ng/ml in saliva [52–54]. Serum CRP has been shown to distinguish between COPD and controls [55], but not healthy smokers from non-smokers [24]. However no difference in salivary CRP was demonstrated between our study cohorts following all-covariate adjustment, possibly because our controls had relatively high BMIs; indeed significant differences emerged when adjustment excluded BMI. In support, strong correlations between serum CRP and BMI have been previously demonstrated [56]. Whilst correlations between serum CRP levels and FEV1 have been reported [26, 57], we found no association between salivary CRP and FEV1 in stable COPD; this possibly reflects the inhaled corticosteroid usage in our COPD patients [24].
We are the first to explore the presence of PCT in saliva. There was no difference in salivary PCT levels between stable COPD patients and healthy controls following covariate adjustment. This is not surprising as PCT is normally hardly detectable in blood (below 0.05 ng/ml) unless there is presence of bacterial infections and sepsis or following trauma [58]. In agreement with previous observations [38, 59] salivary NE was found to be higher in smokers, but not in stable COPD patients [60]; possibly because all study COPD patients were ex-smokers.
The observed increases in salivary CRP, PCT and NE during COPD exacerbations reflect the well-documented elevated CRP and PCT in blood [29, 57, 58] and NE in sputum [41, 59], and have clinical implications. Whilst salivary CRP (or any of the other analytes) may not be sufficiently sensitive for evaluating COPD risk and outcome, it could serve as a potential surrogate for determining exacerbation onset. However, evidence for CRP or any biomarker in isolation to confirm an exacerbation is minimal. On the other hand, our results give support to future development of single-platform immunodiagnostics for near-patient measurement of salivary CRP alongside other readily available biomarkers e.g., PCT to enable sufficient confidence for exacerbation prediction and stratified intervention.
Alongside such developments, we also need to improve understanding of the association between biomarker/physiological measurements and patient-reported outcomes (PRO) in COPD [61]. This is particularly crucial as no one parameter appears to be sufficiently sensitive or specific in monitoring disease status or predicting exacerbation onset. Our study reveals significant differences in self-assessed symptom scores and sputum metrics in COPD patients, similar to studies using SGRQ and CAT [62]. Furthermore, significant correlations were observed between salivary levels of CRP and PCT and breathing scores, with simultaneous changes occurring in both target analyte levels and patient-reported breathing and ADL assessments during exacerbations of COPD. As other PRO instruments have shown similar correlations [47, 63], it is likely that particular COPD symptoms will be shown to be driven by underlying inflammatory events, with those very severe COPD exacerbations requiring hospitalisation possibly exhibiting different clinical and inflammatory profiles [64].
Thus, biomarkers or symptoms in isolation will not be sensitive or specific enough to monitor longitudinal wellbeing in COPD, and combined bio-clinical profiling is essential, particularly if the long-term goal is to enable patient-led prediction of exacerbations and prompt intervention. Indeed, combining serum CRP with one increased major exacerbation symptom (dyspnoea, sputum volume or purulence) was found to be more sensitive than CRP alone in diagnosing exacerbations [30]. Of 36 biomarkers analysed, none were sensitive or specific enough to diagnose exacerbations without symptom assessment [30].
Most serum components are present in saliva, although compositional differences show that saliva is not a passive ultra-filtrate of serum [65]. Biomarkers can enter saliva by cellular diffusion or active transport, ultra-filtration within salivary glands and/or via the gingival sulcus [66]. The precise mechanisms explaining CRP, PCT and NE presence in saliva are unclear. Whilst blood contamination via micro-leakages, crevicular fluid overflow from micro-injuries or poor oral health is plausible, biomarker measurements in our study were not affected by adjustment for gum disease; samples also tested negative for blood.
Both salivary CRP and PCT levels correlated with serum counterparts. Saliva-serum CRP correlations have been previously established [54, 67]. Although Ouellet-Morin et al. observed a moderate to strong association between saliva and serum CRP, lower correlations were found at serum CRP below 2.0 mg/L compared to higher CRP (≥2.0 mg/L) [67]. However, Punyadeera et al. demonstrated saliva to serum CRP correlation at concentrations above 5 mg/mL. Whilst these studies suggest that prediction of serum CRP from saliva CRP is more accurate at higher serum concentrations, our study demonstrated strong correlations at both low and high CRP levels. The only study on saliva to serum PCT relationship [68] showed no significant correlation between the two fluids; however saliva samples were stored at − 27 °C rather than the recommended − 80 °C [69].
No correlation was found between saliva and serum NE levels. Whilst one possible explanation could be localised NE production not manifesting systemically, this contradicts the observed moderate to strong correlation of salivary NE to both salivary CRP and PCT levels. An alternative explanation could be the rapid inactivation of NE in vivo [70], leading to comparatively slower inactivation in saliva than serum.
Some study limitations need to be considered. Although subjects had three assessments over 14 days, longitudinal studies are required to establish steady-state baselines for the target salivary analytes. These would offer precise correlations of biomarker changes to patient-reported outcomes, specifically in the important prodromal period leading to an exacerbation. Furthermore, as BMI-matched cohorts appear to influence salivary CRP between-group differences, BMI status may need consideration in future larger studies. Another possible shortfall is that our study did not specifically exclude for potential microbial airway colonisation in the COPD group, although we did ensure that participants were excluded in the event of any infection or unstable illness in the preceding 6 weeks to enrolment. We appreciate that the presence of lower airway bronchial colonisation can be associated with elevated serum CRP levels in stable COPD patients [71], and with increased exacerbation frequency [72]. In mitigation, we have provided separate analysis for the COPD subjects that underwent an exacerbation and for those who remained stable throughout the study; thus minimising bias on target biomarker level results. Furthermore, there was no difference in median exacerbation frequency between the exacerbation group and the stable group, which may indirectly indicate that airway microbial colonisation was not significantly different between the 2 groups.
Conclusions
We have established that levels of CRP, PCT and NE can be reliably and reproducibly measured in saliva, providing useful clinical information as blood. All 3 target salivary biomarkers increased during COPD exacerbations, with CRP and PCT correlating with patient-derived metrics. These findings provide the conceptual basis for the further development of salivary biomarkers, alongside PROs, for practical point-of-care monitoring of COPD and prediction of exacerbations.
Acknowledgment
This paper summarises independent research on ‘Development of a novel Saliva-based Point-Of-Care bioSensor for COPD: COPD-SPOC sensor’ funded by the National Institute for Health Research (NIHR) under its Invention for Innovation (i4i) Programme (Grant Reference Number II-FS-0109-11006). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Abbreviations
- ADL
Activities of Daily Living
- ANOVA
Analysis of variance
- BMI
Body Mass Index
- CAT
COPD Assessment Test
- CI
Confidence Interval
- COPD
Chronic Obstructive Pulmonary Disease
- CRP
C-Reactive Protein
- ELISA
Enzyme-linked immunoassay
- EXACT
Exacerbations of chronic pulmonary disease tool
- FEV1
Forced expiratory volume in 1 s
- GOLD
Global initiative for chronic Obstructive Lung Disease
- MRC
Medical Research Council
- NE
Neutrophil Elastase
- NS
Never-smokers (normal spirometry)
- PBS-T
Phosphate Buffered Salina - Tween
- PCT
Procalcitonin
- RPM
Revolutions per minute.
- S
Smokers (normal spirometry)
- SD
Standard Deviation
- SGRQ
St George's Respiratory Questionnaire
Additional files
Post Review. The subject demographics and salivary biomarker profiles for the healthy non-smokers, healthy smokers and stable COPD subjects (n = 107).
Wellbeing Diary & Life Impact Scores. The set of self-assessment questions on symptoms that was provided to and completed by each study subject.
Correlations of all COPD subjects (n = 98) symptom scores vs. salivary biomarker levels.
Correlations of all COPD subjects (n = 98) sputum metrics vs. salivary biomarker levels.
Correlations of all COPD subjects (n = 98) symptom scores vs. sputum metrics.
The subject demographics, salivary biomarker and symptom profiles for the same COPD subjects (n = 36) in stable and exacerbation phase.
Footnotes
Competing interests
The authors declare that they have no significant conflicts of interest with any companies/organisations whose products or services may be discussed in this article.
Authors’ contributions
MS oversaw all activities related to the conduct of the study and contributed to the study idea, and the discussion, writing and editing of the manuscript. NP contributed to the study idea, data collection, statistical analysis and the discussion, writing and editing of the manuscript. GT contributed to the study idea, discussion and editing of the manuscript. JB supervised all statistical analysis and contributed to the discussion of the results. NR contributed to the discussion and editing of the manuscript. All authors accepted the final version. All authors read and approved the final manuscript.
References
- 1.Sudhir S, Krueger K. Diagnostics other than blood. In: Wong DT, editor. Salivary diagnostics. Iowa: Wiley-Blackwell; 2008. pp. 94–103. [Google Scholar]
- 2.Denny P, Hagen FK, Hardt M, Liao L, Yan W, Arellanno M, et al. The proteomes of human parotid and submandibular/sublingual gland salivas collected as the ductal secretions. J Proteome Res. 2008;7(5):1994–2006. doi: 10.1021/pr700764j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gallo D, George JR, Fitchen JH, Goldstein AS, Hindahl MS. Evaluation of a system using oral mucosal transudate for HIV-1 antibody screening and confirmatory testing. J Am Med Assoc. 1997;277(3):254–8. doi: 10.1001/jama.1997.03540270080030. [DOI] [PubMed] [Google Scholar]
- 4.Thieme T, Yoshihara P, Piacentini S, Beller M. Clinical evaluation of oral fluid samples for diagnosis of viral-hepatatis. J Clin Microbiol. 1992;30(5):1076–9. doi: 10.1128/jcm.30.5.1076-1079.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li CF, Ha TZ, Ferguson DA, Chi DS, Zhao R, Patel NR, et al. A newly developed PCR assay of H-pylori in gastric biopsy, saliva, and faeces - evidence of high prevalence of H-pylori in saliva supports oral transmission. Dig Dis Sci. 1996;41(11):2142–9. doi: 10.1007/BF02071393. [DOI] [PubMed] [Google Scholar]
- 6.Ikuta K, Satoh Y, Hoshikawa Y, Sairenji T. Detection of Epstein-Barr virus in salivas and throat washings in healthy adults and children. Microbes Infect. 2000;2(2):115–20. doi: 10.1016/S1286-4579(00)00277-X. [DOI] [PubMed] [Google Scholar]
- 7.Blackbourn DJ, Lennette ET, Ambroziak J, Mourich DV, Levy JA. Human herpesvirus 8 detection in nasal secretions and saliva. J Infect Dis. 1998;177(1):213–6. doi: 10.1086/517356. [DOI] [PubMed] [Google Scholar]
- 8.Mandel ID. Salivary diagnosis: more than a lick and a promise. J Am Dent Assoc. 1993;124(1):85–7. doi: 10.14219/jada.archive.1993.0007. [DOI] [PubMed] [Google Scholar]
- 9.Raff H. Utility of salivary cortisol measurements in Cushing’s syndrome and adrenal insufficiency. J Clin Endocrinol Metab. 2009;94(10):3647–55. doi: 10.1210/jc.2009-1166. [DOI] [PubMed] [Google Scholar]
- 10.Miller CS, Foley JD, Bailey AL, Campell CL, Humphries RL, Christodoulides N, et al. Current developments in salivary diagnostics. Biomark Med. 2010;4(1):171–89. doi: 10.2217/bmm.09.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaufman E, Lamster IB. The diagnostic applications of saliva - a review. Crit Rev Oral Biol Med. 2002;13(2):197–212. doi: 10.1177/154411130201300209. [DOI] [PubMed] [Google Scholar]
- 12.Tishler M, Yaron I, Raz A, Meyer FA, Yaron M. Salivary eicosanoid concentration in patients with Sjogren’s syndrome. Ann Rheum Dis. 1996;55(3):202–4. doi: 10.1136/ard.55.3.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hanemaaijer R, Visser H, Knottinen YT, Koolwijk P, Verheijen JH. A novel and simple immunocapture assay for determination of gelatinase-B (MMP-9) activities in biological fluids: Saliva from patients with Sjogren's syndrome contain increased latent and active gelatinase-B levels. Matrix Biol. 1998;17(8–9):657–65. doi: 10.1016/S0945-053X(98)90116-0. [DOI] [PubMed] [Google Scholar]
- 14.Sugimoto M, Wong DT, Hirayama A, Soga T, Tormita M. Capillary electrophoresis mass spectrometry-based saliva metabolomics identified oral, breast and pancreatic cancer-specific profiles. Metabolomics. 2010;6(1):78–95. doi: 10.1007/s11306-009-0178-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hu S, Arellano M, Boontheung P, Wang J, Zhou H, Jiang J, et al. Salivary proteomics for oral cancer biomarker discovery. Clin Cancer Res. 2008;14(19):6246–52. doi: 10.1158/1078-0432.CCR-07-5037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xiao H, Zhang L, Zhou H, Lee JM, Garon EB, Wong DT. Proteomic analysis of human saliva from lung cancer patients using Two-dimensional difference Gel electrophoresis and mass spectrometry. Mol Cell Proteomics. 2012;11(2):1–12. doi: 10.1074/mcp.M111.012112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang L, Xiao H, Zhou H, Santiago S, Lee JM, Garon EB, et al. Development of transcriptomic biomarker signature in human saliva to detect lung cancer. Cell Mol Life Sci. 2012;69(19):3341–50. doi: 10.1007/s00018-012-1027-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Floriano PN, Christodoulides N, Miller CS, Ebersole JL, Spertus J, Rose BG, et al. Use of saliva-based nano-biochip tests for acute myocardial infarction at the point of care: a feasibility study. Clin Chem. 2009;55(8):1530–8. doi: 10.1373/clinchem.2008.117713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schmekel B, Ahlner J, Malmstrom M, Venge P. Eosinophil cationic protein (ECP) in saliva: a new marker of disease activity in bronchial asthma. Respir Med. 2001;95(8):670–5. doi: 10.1053/rmed.2001.1123. [DOI] [PubMed] [Google Scholar]
- 20.Rao NL, Shetty S, D'Souza J, Prasad RM, Vishal B, Shariff MH, et al. Saliva C-reactive protein levels in patients with acute urticaria. Biomed Res. 2011;22(1):90–2. [Google Scholar]
- 21.Gaber F, Daham K, Higashi A, Higashi N, Gülich A, Delin I, et al. Increased levels of cysteinyl-leukotrienes in saliva, induced sputum, urine and blood from patients with aspirin-intolerant asthma. Thorax. 2008;63(12):1076–82. doi: 10.1136/thx.2008.101196. [DOI] [PubMed] [Google Scholar]
- 22.Barnes PJ, Chowdhury B, Khaaritonov SA, Magnussen H, Page CP, Postma D, et al. Pulmonary biomarkers in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2006;174(1):6–14. doi: 10.1164/rccm.200510-1659PP. [DOI] [PubMed] [Google Scholar]
- 23.Koutsokera A, Kostikas K, Nicod LP, Fitting JW. Pulmonary biomarkers in COPD Exacerbations: a systematic review. Respir Res. 2013;14(1):111. doi: 10.1186/1465-9921-14-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pinto-Plata VM, Mullerova H, Toso JF, Feudjo-Tepie M, Soriano JB, Vessey RS, et al. C-reactive protein in patients with COPD, control smokers and non-smokers. Thorax. 2006;61(1):23–8. doi: 10.1136/thx.2005.042200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.He ZH, Chen Y, Chen P, Wu GB, Cai S. Local inflammation occurs before systemic inflammation in patients with COPD. Respirology. 2010;15(3):478–84. doi: 10.1111/j.1440-1843.2010.01709.x. [DOI] [PubMed] [Google Scholar]
- 26.de Torres JP, Cordoba-Lanus E, Lopez-Aguilar C, de Fuentes Muros M, De Garcini Montejo A, Aguirre-Jaime A, et al. C-reactive protein levels and clinically important predictive outcomes in stable COPD patients. Eur Respir J. 2006;27(5):902–7. doi: 10.1183/09031936.06.00109605. [DOI] [PubMed] [Google Scholar]
- 27.Rohde G, Borg I, Wiethege A, Kauth M, Jerzinowski S, An Duong Dinh T, et al. Inflammatory response in acute viral exacerbations of COPD. Infection. 2008;36(5):427–33. doi: 10.1007/s15010-008-7327-5. [DOI] [PubMed] [Google Scholar]
- 28.Bircan A, Gokirmak M, Kilic O, Ozturk O, Akkaya A. C-reactive protein levels in patients with chronic obstructive pulmonary disease: role of infection. Med Princ Pract. 2008;17(3):202–8. doi: 10.1159/000117793. [DOI] [PubMed] [Google Scholar]
- 29.Stolz D, Christ-Crain M, Morgenthaler NG, Leuppi J, Miedinger D, Bingisser R, et al. Copeptin, C-reactive protein and procalcitonin as prognostic biomarkers in acute exacerbation of COPD. Chest. 2007;131(4):1058–67. doi: 10.1378/chest.06-2336. [DOI] [PubMed] [Google Scholar]
- 30.Hurst JR, Donaldson GC, Perera WR, Wilkinson TM, Bilello JA, Hagan GW, et al. Use of plasma biomarkers at exacerbation of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2006;174(8):867–74. doi: 10.1164/rccm.200604-506OC. [DOI] [PubMed] [Google Scholar]
- 31.Malo O, Sauleda J, Busquets X, Miralles C, Agusti AG, Noguera A. Systemic inflammation during exacerbations of chronic obstructive pulmonary disease. Arch Bronconeumol. 2002;38(4):172–6. doi: 10.1016/S0300-2896(02)75184-3. [DOI] [PubMed] [Google Scholar]
- 32.Dev D, Wallace E, Sankaran R, Cunniffe J, Govan JR, Wathen CG, et al. Value of C-reactive protein measurements in exacerbations of chronic obstructive pulmonary disease. Respir Med. 1998;92(4):664–7. doi: 10.1016/S0954-6111(98)90515-7. [DOI] [PubMed] [Google Scholar]
- 33.Perera WR, Hurst JR, Wilkinson TM, Sapsford RJ, Müllerova H, Donaldson GC, et al. Inflammatory changes, recovery and recurrence at COPD exacerbation. Eur Respir J. 2007;29(3):527–34. doi: 10.1183/09031936.00092506. [DOI] [PubMed] [Google Scholar]
- 34.Lacoma A, Prat C, Andreo F, Lores L, Ruiz-Manzano J, Ausina V, et al. Value of procalcitonin, C-reactive protein, and neopterin in exacerbations of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2011;6:157–69. doi: 10.2147/COPD.S16070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Christ-Crain M, Jaccard-Stolz D, Bingisser R, Gencay MM, Huber PR, Tamm M, et al. Effect of procalcitonin-guided treatment on antibiotic use and outcome in lower respiratory tract infections: cluster-randomised, single-blinded intervention trial. Lancet. 2004;363(9409):600–7. doi: 10.1016/S0140-6736(04)15591-8. [DOI] [PubMed] [Google Scholar]
- 36.Hill AT, Bayley D, Stockley RA. The interrelationship of sputum inflammatory markers in patients with chronic bronchitis. Am J Respir Crit Care Med. 1999;160(3):893–8. doi: 10.1164/ajrccm.160.3.9901091. [DOI] [PubMed] [Google Scholar]
- 37.Hoenderdos K, Condliffe A. The neutrophil in chronic obstructive pulmonary disease. Am J Respir Cell Mol Biol. 2013;48(5):531–9. doi: 10.1165/rcmb.2012-0492TR. [DOI] [PubMed] [Google Scholar]
- 38.Weitz JI, Crowley KA, Landman SL, Lipman BI, Yu J. Increased neutrophil elastase activity in cigarette smokers. Ann Intern Med. 1987;107(5):680–2. doi: 10.7326/0003-4819-107-5-680. [DOI] [PubMed] [Google Scholar]
- 39.Vlahos R, Wark PAB, Anderson GP, Bozinovski S. Glucocorticosteroids differentially regulate MMP-9 and neutrophil elastase in COPD. PLoS One. 2012;7(3):e33277. doi: 10.1371/journal.pone.0033277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bizeto L, Mazzoli AB, Ribeiro M, Stelmach R, Cukier A, Nunes MPT. Interrelationship between serum and sputum inflammatory mediators in chronic obstructive pulmonary disease. Braz J Med Biol Res. 2008;41(3):193–8. doi: 10.1590/S0100-879X2008005000010. [DOI] [PubMed] [Google Scholar]
- 41.Ilumets H, Rytilä PH, Sovijärvi AR, Tervahartiala T, Myllärniemi M, Sorsa TA, et al. Transient elevation of neutrophil proteinases in induced sputum during COPD exacerbation. Scand J Clin Lab Invest. 2008;68(7):618–23. doi: 10.1080/00365510801983773. [DOI] [PubMed] [Google Scholar]
- 42.Yigla M, Berkovich Y, Nagler RM. Oxidative stress indices in COPD–broncho-alveolar lavage and salivary analysis. Arch Oral Biol. 2007;52(1):36–43. doi: 10.1016/j.archoralbio.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 43.Ji J, von Scheele I, Bergstrom J, Billing B, Dahlen B, Lantz AS, et al. Compartment differences of inflammatory activity in chronic obstructive pulmonary disease. Respir Res. 2014;15. [DOI] [PMC free article] [PubMed]
- 44.Cazzola M, MacNee W, Martinez FJ, Rabe KF, Franciosi LG, Barnes PJ, et al. Outcomes for COPD pharmacological trials: from lung function to biomarkers. Eur Respir J. 2008;31(2):416–68. doi: 10.1183/09031936.00099306. [DOI] [PubMed] [Google Scholar]
- 45.Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: revised 2014. http://www.goldcopd.com/uploads/users/files/GOLD_Report_2014_Oct30.pdf. Accessed 01 Nov 2014.
- 46.Fletcher CM. Standardized questionnaire on respiratory symptoms: a statement prepared and approved by the MRC committee on the aetiology of chronic bronchitis. Br Med J. 1960;2:1665. [Google Scholar]
- 47.Patel N, Jones P, Adamson V, Spiteri M, Kinmond K. Chronic obstructive pulmonary disease Patients’ experiences of an enhanced self-management model of care. Qual Health Res. 2015 doi: 10.1177/1049732315573013. [DOI] [PubMed] [Google Scholar]
- 48.Mackay AJ, Donaldson GC, Patel ARC, Singh R, Kowlessar B, Wedzicha JA. Detection and severity grading of COPD exacerbations using the exacerbations of chronic pulmonary disease tool (EXACT) Eur Respir J. 2014;43(3):735–44. doi: 10.1183/09031936.00110913. [DOI] [PubMed] [Google Scholar]
- 49.Jaedicke KM, Taylor JJ, Preshaw PM. Validation and quality control of ELISAs for the use with human saliva samples. J Immunol Methods. 2012;377(1–2):62–5. doi: 10.1016/j.jim.2012.01.010. [DOI] [PubMed] [Google Scholar]
- 50.Lipton CR, Dautlick JX, Grothaus CD, Hunst PL, Magin KM, Mihaliak CA, et al. Guidelines for the validation and use of immunoassays for determination of introduced proteins in biotechnology enhanced crops and derived food ingredients. Food Agric Immunol. 2000;12(2):153–64. doi: 10.1080/095401000404094. [DOI] [Google Scholar]
- 51.Janes H, Pepe MS. Adjusting for covariates in studies of diagnostic, screening, or prognostic markers: an old concept in a new setting. Am J Epidemiol. 2008;168(1):89–97. doi: 10.1093/aje/kwn099. [DOI] [PubMed] [Google Scholar]
- 52.Izawa S, Miki K, Liu XX, Ogawa N. The diurnal patterns of salivary interleukin-6 and C-reactive protein in healthy young adults. Brain Behav Immun. 2013;27:38–41. doi: 10.1016/j.bbi.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 53.Topkas E, Keith P, Dimeski G, Cooper-White J, Punyadeera C. Evaluation of saliva collection devices for the analysis of proteins. Clin Chim Acta. 2012;413(13–14):1066–70. doi: 10.1016/j.cca.2012.02.020. [DOI] [PubMed] [Google Scholar]
- 54.Punyadeera C, Dimeski G, Kostner K, Beyerlein P, Cooper-White J. One-step homogeneous C-reactive protein assay for saliva. J Immunol Methods. 2011;373(1–2):19–25. doi: 10.1016/j.jim.2011.07.013. [DOI] [PubMed] [Google Scholar]
- 55.Gan WQ, Man SFP, Senthilselvan A, Sin DD. Association between chronic obstructive pulmonary disease and systemic inflammation: a systematic review and a meta-analysis. Thorax. 2004;59(7):574–80. doi: 10.1136/thx.2003.019588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Choi J, Joseph L, Pilote L. Obesity and C-reactive protein in various populations: a systematic review and meta-analysis. Obes Rev. 2013;14(3):232–44. doi: 10.1111/obr.12003. [DOI] [PubMed] [Google Scholar]
- 57.Broekhuizen R, Wouters EFM, Creutzberg EC, Schols AMWJ. Raised CRP levels mark metabolic and functional impairment in advanced COPD. Thorax. 2006;61(1):17–22. doi: 10.1136/thx.2005.041996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Uzzan B, Cohen R, Nicolas P, Cucherat M, Perret GY. Procalcitonin as a diagnostic test for sepsis in critically ill adults and after surgery or trauma: a systematic review and meta-analysis. Crit Care Med. 2006;34(7):1996–2003. doi: 10.1097/01.CCM.0000226413.54364.36. [DOI] [PubMed] [Google Scholar]
- 59.Ozcaka O, Bicakci N, Pussinen P, Sorsa T, Kose T, Buduneli N. Smoking and matrix metalloproteinases, neutrophil elastase and myeloperoxidase in chronic periodontitis. Oral Dis. 2011;17(1):68–76. doi: 10.1111/j.1601-0825.2010.01705.x. [DOI] [PubMed] [Google Scholar]
- 60.Higashimoto Y, Yamagata Y, Taya S, Iwata T, Okada M, Ishiguchi T, et al. Systemic inflammation in chronic obstructive pulmonary disease and asthma: similarities and differences. Respirology. 2008;13(1):128–33. doi: 10.1111/j.1440-1843.2007.01170.x. [DOI] [PubMed] [Google Scholar]
- 61.Paladini L, Hodder R, Cecchini I, Bellia V, Incaalzi RA. The MRC dyspnoea scale by telephone interview to monitor health status in elderly COPD patients. Respir Med. 2010;104(7):1027–34. doi: 10.1016/j.rmed.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 62.Nishimura K, Mitsuma S, Kobayashi A, Yanagida M, Nakayasu K, Hasegawa Y, et al. COPD and disease-specific health status in a working population. Respir Res. 2013;14(1):61. doi: 10.1186/1465-9921-14-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tu YH, Zhang Y, Fei GH. Utility of the CAT in the therapy assessment of COPD exacerbations in China. BMC Pulm Med. 2014;14:42. doi: 10.1186/1471-2466-14-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Huerta A, Crisafulli E, Menéndez R, Martínez R, Soler N, Guerrero M, et al. Pneumonic and nonpneumonic exacerbations of COPD: inflammatory response and clinical characteristics. Chest. 2013;144(4):1134–42. doi: 10.1378/chest.13-0488. [DOI] [PubMed] [Google Scholar]
- 65.Rehak NN, Cecco SA, Csako G. Biochemical composition and electrolyte balance of “unstimulated” whole human saliva. Clin Chem Lab Med. 2000;38(4):335–43. doi: 10.1515/CCLM.2000.049. [DOI] [PubMed] [Google Scholar]
- 66.Spielmann N, Wong DT. Saliva: diagnostics and therapeutic perspectives. Oral Dis. 2011;17(4):345–54. doi: 10.1111/j.1601-0825.2010.01773.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ouellet-Morin I, Danese A, Williams B, Arseneault L. Validation of a high-sensitivity assay for C-reactive protein in human saliva. Brain Behav Immun. 2011;25(4):640–6. doi: 10.1016/j.bbi.2010.12.020. [DOI] [PubMed] [Google Scholar]
- 68.Bassim CW, Redman RS, DeNucci DJ, Becker KL, Nylen ES. Salivary procalcitonin and periodontitis in diabetes. J Dent Res. 2008;87(7):630–4. doi: 10.1177/154405910808700707. [DOI] [PubMed] [Google Scholar]
- 69.Slavkin HC. Toward molecularly based diagnostics for the oral cavity. J Am Dent Assoc. 1998;129(8):1138–43. doi: 10.14219/jada.archive.1998.0390. [DOI] [PubMed] [Google Scholar]
- 70.Carter RI, Ungurs MJ, Mumford RA, Stockley RA. A alpha-Val (360): a marker of neutrophil elastase and COPD disease activity. Eur Respir J. 2013;41(1):31–8. doi: 10.1183/09031936.00197411. [DOI] [PubMed] [Google Scholar]
- 71.Marin A, Garcia-Aymerich J, Sauleda J, Belda J, Millares L, Garcia-Nunez M, et al. Effect of Bronchial Colonisation on Airway and Systemic Inflammation in Stable COPD. COPD. 2012;9(2):121–30. doi: 10.3109/15412555.2011.636407. [DOI] [PubMed] [Google Scholar]
- 72.Patel IS, Seemungal TAR, Wilks M, Llyd-Owen SJ, Donaldson GC, Wedzicha JA. Relationship between bacterial colonisation and the frequency, character, and severity of COPD exacerbations. Thorax. 2002;57(9):759–64. doi: 10.1136/thorax.57.9.759. [DOI] [PMC free article] [PubMed] [Google Scholar]


